Abstract
Background:
The aims of the study were to understand sleep problems and their effects in advanced cancer patients and spousal and intimate partner caregivers and to examine the directionality of the link between patients’ and caregivers’ sleep problems.
Methods:
Fifty-four advanced cancer patients and their spousal and intimate partners were administered a battery of questionnaires that included the Pittsburgh Sleep Quality Index and the Center for Epidemiological Studies at the patients’ cancer diagnosis and at 2, 4, and 6 months after diagnosis.
Results:
Patients’ and caregivers’ sleep duration was significantly related. Using cross-lagged panel analyses, caregivers’ sleep quality significantly predicted patients’ sleep quality and patients’ sleep quality subsequently predicted caregivers’ sleep quality. Patients’ sleep latency significantly was found to significantly predict caregivers’ sleep latency.
Conclusion:
Patients diagnosed with cancer and their intimate partners have poor sleep quality and sleep patterns are related.
Keywords: Cancer, Sleep quality, Caregiver, Sleep latency, Sleep problem
Introduction
Sleep symptoms are common in patients with cancer. Although studies of cancer patients often include the assessment of individual symptoms of insomnia rather than full diagnostic criteria, prevalence rates of sleep disturbances are consistently high (59–79%)1–3. Rates of insomnia and subclinical symptoms and of insomnia in patients with cancer appear to be at least two to three times higher than in the general population2. Longitudinal studies have found that sleep problems such as insomnia often begin or worsen during cancer treatment, and follow a chronic course in up to 95% patients2. The rate of sleep problems also rises in more advanced cancer patients (85%), whose significant symptom burdens and uncontrolled physical symptoms can contribute to poor sleep quality4.
Sleep plays a vital role in physical and psychological health, and inadequate sleep may further compound illness and impair recovery4. Chronic sleep problems can have negative effects on outcomes as diverse as quality of life, physical symptoms, adherence to treatments, interpersonal relationships, accidents and falls, pro-inflammatory cytokines, and healthcare utilization1,5–11. Among cancer patients, sleep disturbance is associated with aberrant patterns of cortisol secretion, which in turn can impair the cellular immunity responsible for mounting a defense against tumors3.
Intimate partners are frequently the primary caregivers for cancer patients, often providing around-the-clock care and incurring physical, emotional, and financial burden12,13. Most research on the sleep of intimate partner caregivers has been conducted in caregivers of patients with dementia. However, recent studies have also shown high rate of sleep problems among intimate partner caregivers of patients with cancer14–16. A systematic review of ten sleep studies found at least 72% of caregivers reported moderate to severe sleep disturbance17. Intimate partner caregivers also reported significantly greater sleep problems compared to the general population18. Specifically, problems with insomnia, sleep latency, wake after sleep onset (WASO), night awakenings, and daytime fatigue are common among intimate partner caregivers of cancer patients19. Despite the high prevalence of sleep problems, some findings suggest caregivers may underestimate the extent of their problem. Sleep measured across a 10-week span showed caregivers reported an average of 6.05 hours of sleep a night, yet objective assessment indicated an average sleep duration of only 4.83 hours a night14. A qualitative study of caregivers of advanced cancer patients found caregivers minimized the significance of their sleep problems20. Carney and colleagues measured sleep using actigraphy and found that cancer patients and their caregivers had approximately 18 awakenings, each lasting 3–4 minutes, over the course of the night21. These findings are consistent with a study of 60 caregivers of advanced cancer patients, in which 90% had sleep fragmentation22. However, it is still not clear that if the severity of the sleep fragmentation in cancer caregivers is different from the general population.
Sleep problems can lead to negative mental and physical health outcomes among cancer caregivers. For instance, sleep problems have been associated with increased depression, poorer coping, lower optimism, less mastery, and higher neuroticism among caregivers12,23. Specifically, sleep fragmentation can lead to excessive daytime sleepiness, cognitive impairment and mood disorders24,25, and has also been associated with metabolic syndrome, diabetes, and increased risk of cardiovascular disease (CVD)26–29. These risks may be compounded by the fact that many caregivers must provide care for months or even years. Carter found that caregivers of advanced cancer patients reported providing care an average of 16 hours of care per day for two years. Of these caregivers, 95% reported severe sleep problems with moderate-severe daytime impairment14.
While sleep problems are common and have negative consequences for both patients and caregivers, little is known about how these problems differ among partners, or how sleep in one partner may affect sleep in the other. Two separate studies found that 40–50% of cancer patients and caregivers reported sleep problems21,22. The primary difference between cancer patients and intimate partner caregivers was that patients had more frequent awakenings and used significantly more sleep aids than their intimate partner21. Cancer patients also reported poorer sleep efficiency compared to caregivers, but sleep, rest and wake and activity parameters were highly correlated among partners. A recent study found that interdependence in couples’ sleep (sleep-wake concordance) is associated with CVD risk, raising the possibility that dyadic sleep patterns may also affect health outcomes in cancer patients30. Further research is needed to compare intimate partner sleep patterns in cancer patients and their caregivers versus the general population.
Sleep disturbance in cancer patients is a crucial area of clinical and research focus, as sleep loss can affect one’s physical and emotional health. These factors can impact the caregivers’ ability to safely and effectively perform caregiving duties. Further research is needed to examine the extent and nature of sleep problems in cancer caregivers, as well as explore potential demographic and emotional predictors to identify those cancer caregivers at a higher risk for developing sleep problems. To address the gap in cancer caregivers’ sleep research, this study aimed to: (1) describe the sleep problems of advanced cancer spousal and intimate partner caregivers, (2) investigate the association between sleep problems and depression in advanced cancer patients and intimate partner caregivers, and (3) examine the directionality of the link between patients’ and their caregivers’ sleep problems.
Methods
Design and Participants
We conducted a prospective observational study in patients with cancer and their intimate partners. The Liver Cancer Center evaluates and treats patients with advanced cancers related to the hepatobiliary-pancreatic system. Patients and intimate partners were enrolled between January 2008 to June 2012 (K07CA118576). Patients were required to have a biopsy or radiographic-proven diagnosis of cancer affecting the hepatobiliary or pancreatic system. Additional inclusion and exclusion criteria for patients and intimate partners were: (1) age 21 years or older; (2) fluent in English, and (3) no evidence of thought disorder, hallucinations, or delusions.
Instruments
Sociodemographic, Disease, and Treatment Specific Factors
Sociodemographic data including patients’ age, gender, BMI, race, ethnicity, religious preference, educational level, occupation, income, and health insurance status were collected on a self-reported questionnaire designed specifically for this study. Disease-specific and treatment-related information including diagnosis, presence or absence of cirrhosis, maximum tumor size, number of lesions, vascularity of lesions, and vascular invasion was gathered from the patients’ electronic medical record. Survival was measured from the time of diagnosis of cancer until death.
Sleep
The Pittsburgh Sleep Quality Index (PSQI) is an 18-item self-rated questionnaire which assesses sleep quality and disturbance over a one-month time interval31. The PSQI was used to describe sleep problems in seven components: sleep duration, sleep disturbances, sleep latency (≥30 minutes indicates poor latency), daytime dysfunction, sleep efficiency (time asleep divided by time spent in bed, <85% indicates poor efficiency), subjective sleep quality, and use of sleep medication. Each component is scored on a 0–3 scale. The seven component scores are summed to yield a global score of ranging from 0–21 (higher scores indicate worse sleep quality and scores greater than 5 indicate poor sleep quality)31. Acceptable measures of internal consistency (Cronbach α=0.83), test-retest reliability (r=0.85, p<0.001), and validity using clinical interview and polysomnographic (Hotelling’s TL = 2.62, p < 0.001), have been reported for the PSQI31.
Depressive Symptoms
The Center for Epidemiologic Studies-Depression (CES-D) is a 20-item self-report questionnaire designed to assess depressive symptoms. Each item is answered on a four-point scale by reporting weekly frequency of depressive symptoms (“rarely,” ”some days,” ”occasionally,” ”most days”)32. The CES-D has a range of 0 to 60 for the summed item scores32. A total score of 16 or greater represents depressive symptoms in the clinical range32. The CES-D has demonstrated adequate construct validity with higher scores among cancer patients than healthy adults prior to treatment (p<0.05) and midway through treatment (p<0.001); positive correlation with the Profile of Mood States-Fatigues and the State-Trait Anxiety Inventory-Anxiety and negative correlations with the Mental Health Summary Scale of the Short Form-36 (p < 0.001 for all correlations)33. It is also found to have acceptable reliability (α=0.89) and test-retest reliability (r=0.57, p<0.001) in cancer patients33.
Procedure
The study was approved by the University of Pittsburgh Institutional Review Board prior to the enrollment of patients. Patients were referred to the study team by their attending physician. If the patient agreed to speak to the study team, study staff would explain the risks and benefits of the study and obtain informed consent from the patient prior to administering the questionnaires.
Data Analysis
All data were entered, verified and analyzed with SPSS version 25 (IBM Corp, Armonk, NY). Descriptive statistics were performed to obtain measures of central tendency, distribution, and percentages for each variable. Kendal tau-c coefficients were computed to assess agreement between patients and caregivers sleep problems at each time point. Next, the longitudinal relationships among patient and caregivers sleep problems were examined by constructing four constrained cross-lagged panel models using EQS software (version 6.2, Multivariate Software, Inc.). The panel design allowed for the estimation of autocorrelations (correlations between the same variables measured at different times) and cross-lagged correlations (correlations between different variables measured at different times)34. Model fit was assessed using goodness of fit indices, including root mean square error of approximation (RMSEA; values ≤ .07 were considered appropriate); standardized root mean square residual (SRMSR; values ≤.08 were considered good fit); and the comparative fit index (CFI; values ≥ .95 were considered good fit)35. Cross-lagged panel analyses were used to examine relationships in patient and caregivers’ sleep quality, latency, and duration over time. Analyses were conducted with EQS (Multivariate Software, Inc., version 6.2) using maximum likelihood estimation.
Results
Sociodemographic characteristics of 54 advanced cancer patients and their intimate partner are shown in Table 1. The majority of the patients were male (65%), Caucasian (80%) and the mean age was 62 (SD=11). The majority of patients were diagnosed with hepatocellular or cholangiocarcinoma (67%) and most were treated with regional chemotherapy or radiation (76%). The family caregivers were primarily female (71%), Caucasian (91%), and had a mean age of 55 (SD=12) years. Forty-three percent of intimate partner caregivers were working full or part-time and 24% of patients were employed.
Table 1:
Sociodemographic Characteristics of Patients and Caregivers
| Caregivers | Patients | |
|---|---|---|
| N=54 | N=54 | |
| Gender (n, %) | ||
| Male | 15 (29) | 35 (65) |
| Female | 39 (71) | 19 (35) |
| Age (mean, SD) | 55 (12) | 62 (11) |
| Race (n, %) | ||
| Caucasian | 49 (91) | 43 (80) |
| Non-Caucasian | 5 (9) | 11 (20) |
| Marital Status | ||
| Married (n, %) | 38 (73) | 38 (70) |
| Cohabitating or Significant Other | 16 (27) | 16 (27) |
| Educational Level (n, %) | ||
| Less than High School | 2 (4) | 3 (6) |
| Completed High School | 15 (28) | 31 (58) |
| College | 37 (68) | 15 (28) |
| Employed (n, %) | 23 (43) | 13 (24) |
| Diagnosis | --- | |
| Hepatocellular or Cholangio Carcinoma | --- | 36 (67) |
| Colorectal with liver metastases | --- | 6 (11) |
| Other | --- | 12 (22) |
| Treatment | --- | |
| Regional chemo/90Y (radiation) | --- | 41 (76) |
| Radiofrequency Ablation/Resection | --- | 13 (24) |
Sleep of Advanced Cancer Patients
The patients reported a mean sleep duration of 6.47 hours (SD=2.1) and an average sleep latency of 21.9 minutes (SD=25.9); 12% reported a sleep latency of >30 minutes three or more times per week. Sixty-four percent of patients reported taking a sleep aid in the past month and 8.1 percent reported taking a sleep aid three or more times per week. Patients reported a mean sleep efficiency of 85.6%. (Table 2)
Table 2:
Kendall’s Tau-c coefficients for patients and caregivers at each time point.
| PSQI Component | Time 1 | Time 2 | Time 3 | Time 4 |
|---|---|---|---|---|
| Global Sleep Quality | .18 | −.25 | .12 | .31 |
| Duration | .28** | .27 | .11 | .15 |
| Daytime Dysfunction | −.05 | .12 | −.17 | .02 |
| Latency | .01 | −.24 | −.12 | −.11 |
| Disturbance | −.02 | −.03 | .18 | .12 |
p<.05
p<.01
p<.001
Sleep of Spousal or Intimate Partner Caregivers
Caregivers reported on average sleeping 6.0 hours per night (SD=2.1; range 1–9 hours) and a mean sleep latency of 24 minutes (SD=21.8); 27% reported a sleep latency of greater than 30 minutes. Thirty percent of family caregivers reported using a sleep aid in the last week and 22% of caregivers reported using a sleep aid more than 3 times per week. Caregivers reported a mean sleep efficiency of 83%.
Concordance between Cancer Patients and Spousal/Intimate Partner Caregivers Sleep Problems
Kendall’s tau-c was performed to examine the concordance between 54 patient and family caregivers with regard to the components of the PSQI. Patient and intimate partner sleep duration were significantly related [Kendall’s tau-c=0.301, p=0.02]. The patient and intimate partner agreement for the PSQI Daytime Dysfunction was not significant [Kendall’s tau-c=0.027, p=0.86]. The patient and intimate partners’ sleep latency also was not significantly related at diagnosis [Kendall’s tau-c=0.115, p=0.458], however, patients and intimate partner had approximately the same latency (patients 29.9; SD=25.9 minutes and =24.0; SD=21.8 minutes). The use of medication between the patients and intimate partner was not significant [Kendall’s tau-c=0.182, p=0.119]. A total of 30% of intimate partner reported using a sleep aid within the last week and 22% of intimate partner reported using a sleep aid more than 3 times per week.
Patients’ and Caregivers’ Sleep Problems: Who is Disturbing Whom?
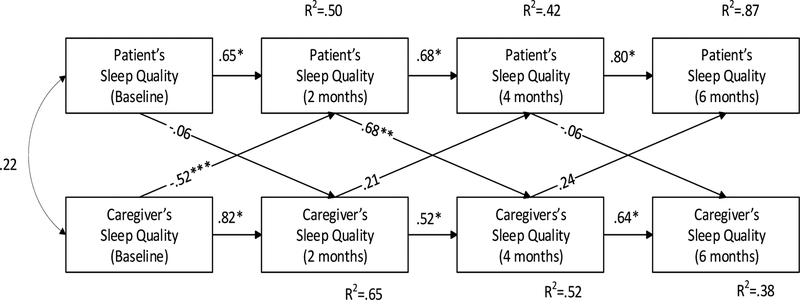
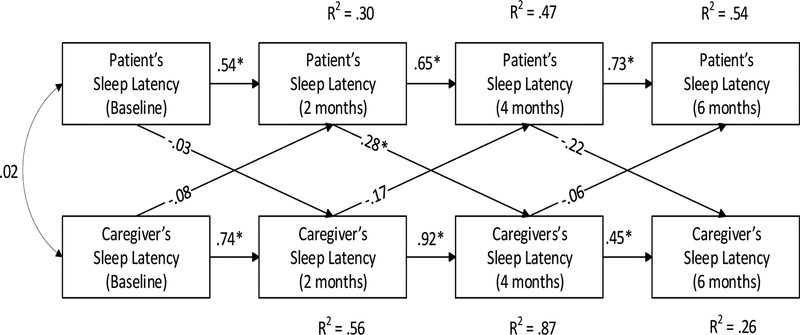
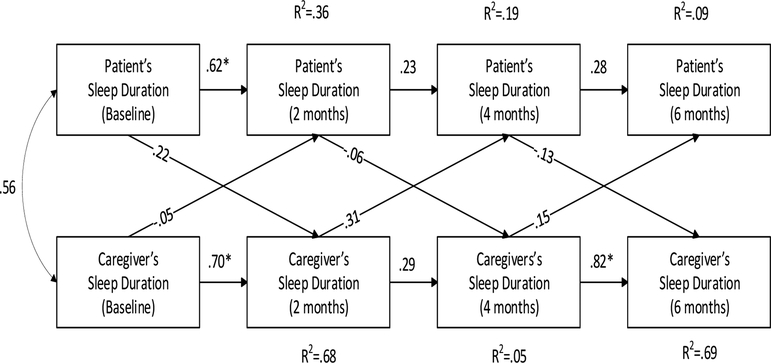
Using cross-lagged panel analyses, partners’ sleep quality significantly predicted patients’ sleep quality (r=0.52, p<0.001) from baseline to the 2-month evaluation; patients’ sleep quality then significantly predicted partners’ sleep quality from the 2 months to the 4-month evaluation (r=0.68, p=0.01). Similarly, patients’ sleep latency significantly predicted partners’ sleep latency from 2 to 4 months (r=0.28, p=0.05). Although sleep duration was highly correlated between patients and partners between baseline to 6-months, neither patients’ nor partners’ sleep duration significantly predicted the other’s.
Sleep and Depression
No significant relationships were found between the caregivers’ sleep parameters on the PSQI and depression. Sleep duration [F(1,26)=0.646, p=0.533], sleep latency [F(1,25)=1.824, p=0.184], and sleep quality [F(1,26)=0.681, p=0.573] were not related to depressive symptoms. Similarly, we did not observe significant relationships between sleep duration [F(1,19)=1.543, p=0.242], sleep latency [F(1,18)=0.546, p=0.590], or sleep quality [F(1,19)=0.715, p=0.557] and depressive symptoms in the advanced cancer patients.
Discussion
Consistent with previous studies14,36–38, our study found that sleep problems, such as poor sleep quality and short sleep duration, were common among cancer patients and their intimate partner caregivers. We observed short sleep duration for patients and caregivers that is less than the recommended seven hours per night of sleep39. Further, since self-report often overestimates the duration of sleep compared to actigraphy40, the hours of sleep estimated by patients and caregivers in this study are likely overestimated. Inconsistent with prior research, intimate partner caregivers had shorter sleep duration, longer sleep latency, and poorer sleep efficiency compared to their loved ones diagnosed with cancer21. Additionally, cancer caregivers reported a higher frequency of using sleep aids.
Poor sleep in patients with cancer has been increasingly tied to increased risk of psychological symptoms and mortality. For instance, Palesh has recently found a link between sleep efficiency and increased mortality in a sample of patients diagnosed with breast cancer41,42. We also found a curvilinear relationship between sleep duration and mortality. Further studies are needed to examine whether treatment of sleep problems improves symptoms and survival in the context of cancer4.
Similarly, sleep problems in cancer caregivers should not be neglected and will need further investigation as they may explain caregivers’ increased risk of CVD. Several large epidemiological studies have shown a link between caregiving and increased risk for CVD43–45, but the mechanisms underlying this link have not been elucidated. A recent meta-analysis found that insomnia is associated with a 45% increased risk of developing and dying from CVD46,47. Risk factors for CVD also include metabolic abnormalities (e.g., low high-density lipoprotein and high levels of triglycerides and glucose levels)46 and sleep problems are precisely found to be one of the significant predictors of the development of metabolic abnormalities48–50. Sleep fragmentation, poor sleep efficiency and quality, and insomnia have been associated with increased risk of developing metabolic syndrome, diabetes, and CVD in the general population27,29,51. Thus, sleep problems may be one pathway that links caregiving and development of the CVD.
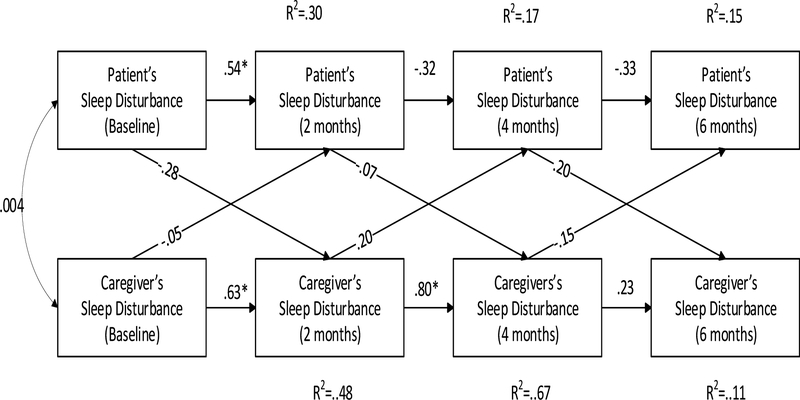
Prior research has investigated demographic, genetics, and psychosocial predictors of poor caregiver sleep quality. Few studies have addressed whether partners affect each other’s sleep quality. For example, a cross-sectional study of cancer caregivers found less functional coping, mastery, neuroticism, and depression predicted sleep problems36, and a longitudinal study of cancer patients and caregivers identified age and genotype as predictors of both baseline sleep disturbances and subsequent trajectories52. A study on Parkinson’s disease patients and their caregiving partners also found a relationship between spouses’ and patients’ self-perceived sleep, but this cross-sectional study could not address directionality53. Few studies have assessed sleep over time, particularly in dyads. We found agreements between patients and family caregivers in sleep quality, sleep duration, sleep latency and the use of sleep aids. Although limited, we observed some bidirectional relationships between patients’ and caregivers’ sleep patterns. One of the partner’s sleep quality and sleep latency predicted the other partners at two months’ intervals. This suggests that if one of the partners has sleep disturbance, the other partner is affected.
Although the current study has provided insight to cancer patients and caregivers’ sleep problems and bidirectional association, there are several potential limitations. First, the sample size is small, but the study begins to show trends that may be important for future study. Second, we collected only self-reported sleep data, which might underestimate sleep disturbance compared to actigraphy. Third, the patients in this study were diagnosed with advanced cancers (stage III and IV) and were primarily male and Caucasian. A more diverse sample with regard to types and stages of cancer, gender, and race is recommended.
Even with the acknowledged limitations, this study presents pragmatic implications for future sleep research on cancer patients and caregivers. To our knowledge, this is the first prospective study examining the link between cancer patients and their caregivers’ sleep problems. Specifically, it investigated four different major parameters of sleep and followed up for six months to explore the relationship of each of them between cancer patients and their caregivers, which provided sufficient evidence on the similar sleep patterns and bi-directional relationship. In addition, this study is an important supplement to the cancer caregiver sleep research.
The results from the current study together with the findings discussed above suggest that clinical trials testing dyadic sleep interventions are warranted. Targeted interventions may improve sleep and mental health outcomes on a short-term basis and serve as a prevention tool for reducing the risk of long-term poor mental and physical health outcomes in cancer patients and intimate partner caregivers.
Future research can advance the current projects in two directions. First, effective interventions specifically targeted to cancer patients and caregivers are warranted to help improve outcomes. There are only a few options for treatment for cancer patient population and their caregivers. In our study, we found that caregivers use sleep aids to minimize the negative effects of sleep problem, but sleep aids’ sedative effects impact the caregiver’s ability to respond to the needs of the patient during the night15. Treatment of the intimate partners sleep problems, either through the downstream treatment of the patient or dyadic treatment, may improve sleep, quality of life, and potentially the health of the caregiver. Currently, cognitive behavioral therapy is widely applied to treating sleep disorders with cancer patients and that can significantly improve subjective sleep outcomes in patients with cancer54. Mindfulness-based stress reduction was also tested as a sleep intervention to treat cancer patient55,56. A multi model psychological sleep management program combining relaxation techniques, sleep hygiene, cognitive techniques, and advice in stimulus control technique was found effective in enhancing various sleep parameters and well-being of cancer patients57. There are even fewer studies discussed sleep intervention for cancer caregivers. However, dyadic treatment of sleep, rather than individual treatment with either the cancer patient or caregiver, could potentially establish a more sustainable, healthy sleep pattern based on our study result that one of the partner’s sleep problem will affect the other. Studies also found the sleep of partners has been shown to improve when the identified person with sleep problems was treated58.
Second, prospective studies with more racially diverse samples, longer follow up, and use of actigraphy are warranted to further confirm the reliability and validity of the bidirectional relationship in sleep patterns between cancer patients and caregivers. Prior studies found that the sleep of partners improves when the identified person with sleep problems was treated; however, not all parameters of sleep show improvement58. Further research is needed to understand the sleep patterns of cancer patients and their intimate partners to develop effective dyadic sleep interventions. Given that some of the correlations and nuanced changes in sleep patterns are not easy to detect, a design with more precise and objective measurements looking at sleep at a micro level will allow for more sophisticated analyses. A recent study found couples had higher concordance in sleep-wake patterns throughout the night using actigraphy to measure minute-by-minute sleep for ten days59. This method could be one possibility to further explore the dyadic sleep pattern in the future.
Figure 1:
Cross-lagged panel analyses of patient and caregiver sleep quality
Figure 2:
Cross-lagged panel analyses of patient and caregiver sleep latency
Figure 3:
Cross-lagged panel analyses of patient and caregiver sleep duration
Figure 4:
Cross-lagged panel analyses of patient and caregiver sleep disturbance
Table 3:
| PSQI Component | χ2 | SRMSR | CFI |
|---|---|---|---|
| Global Sleep Quality | 141.44, df=28, p<.001 | .019 | .98 |
| Duration | 105.90, df=28, p<.001 | .064 | .92 |
| Latency | 118.38, df=28, p<.001 | .048 | .93 |
| Disturbance | 67.34, df=28, p=.013 | .012 | .95 |
Funding:
This study was funded by National Cancer Institute (Grant number K07CA118576; R21CA127046)
Footnotes
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
Conflict of interest: All the authors stated there was no conflict of interest.
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent: Informed consent was obtained from all individual participants included in the study.
Contributor Information
Qi Chen, University of Pittsburgh, Department of Surgery.
Lauren Terhorst, University of Pittsburgh, Department of Occupational Therapy and Health and Community Systems.
Amy Lowery-Allison, University of Pittsburgh, Department of Medicine.
Hannah Cheng, University of Pittsburgh, Department of Surgery
Allan Tsung, University of Pittsburgh, Department of Surgery.
Mikhaila Layshock, University of Pittsburgh, Department of Surgery.
Daniel J. Buysse, University of Pittsburgh, Department of Psychiatry and Clinical and Translational Science
David A. Geller, University of Pittsburgh, Department of Surgery
James W. Marsh, University of Pittsburgh, Department of Surgery
Yisi Wang, University of Pittsburgh, Department of Surgery.
Jennifer. L. Steel, University of Pittsburgh, Department of Surgery, Psychiatry, and Psychology
References:
- 1.Davidson JR, MacLean AW, Brundage MD, Schulze KJSs, medicine. Sleep disturbance in cancer patients. 2002;54(9):1309–1321. [DOI] [PubMed] [Google Scholar]
- 2.Savard J, Morin CMJJoco. Insomnia in the context of cancer: a review of a neglected problem. 2001;19(3):895–908. [DOI] [PubMed] [Google Scholar]
- 3.Theobald DEJCC. Cancer pain, fatigue, distress, and insomnia in cancer patients. 2004;6(1):S15–S21. [DOI] [PubMed] [Google Scholar]
- 4.Collins KP, Geller DA, Antoni M, et al. Sleep duration is associated with survival in advanced cancer patients. 2017;32:208–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Berger AJTO. Treating fatigue in cancer patients. 2003;8(Supplement 1):10–14. [DOI] [PubMed] [Google Scholar]
- 6.Bjørngaard JH, Bjerkeset O, Romundstad P, Gunnell DJS. Sleeping problems and suicide in 75,000 Norwegian adults: a 20 year follow-up of the HUNT I study. 2011;34(9):1155–1159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Engstrom CA, Strohl RA, Rose L, Lewandowski L, Stefanek MEJCn. Sleep alterations in cancer patients. 1999;22(2):143–148. [DOI] [PubMed] [Google Scholar]
- 8.Kochar J, Fredman L, Stone KL, Cauley JA, Society SoOFJJotAG. Sleep problems in elderly women caregivers depend on the level of depressive symptoms: Results of the Caregiver–Study of Osteoporotic Fractures. 2007;55(12):2003–2009. [DOI] [PubMed] [Google Scholar]
- 9.Manabe K, Matsui T, Yamaya M, et al. Sleep patterns and mortality among elderly patients in a geriatric hospital. 2000;46(6):318–322. [DOI] [PubMed] [Google Scholar]
- 10.Manocchia M, Keller S, Ware JEJQolr. Sleep problems, health-related quality of life, work functioning and health care utilization among the chronically ill. 2001;10(4):331–345. [DOI] [PubMed] [Google Scholar]
- 11.Palesh O, Peppone L, Innominato PF, et al. Prevalence, putative mechanisms, and current management of sleep problems during chemotherapy for cancer. 2012;4:151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Northouse L, Williams A-l, Given B, McCorkle RJJoCO. Psychosocial care for family caregivers of patients with cancer. 2012;30(11):1227–1234. [DOI] [PubMed] [Google Scholar]
- 13.Pellegrino R, Formica V, Portarena I, et al. Caregiver distress in the early phases of cancer. 2010;30(11):4657–4663. [PubMed] [Google Scholar]
- 14.Carter PA, Chang BLJCn. Sleep and depression in cancer caregivers. 2000;23(6):410–415. [DOI] [PubMed] [Google Scholar]
- 15.Carter PAJCn. Family caregivers’ sleep loss and depression over time. 2003;26(4):253–259. [DOI] [PubMed] [Google Scholar]
- 16.Stenberg U, Ruland CM, Miaskowski CJPo. Review of the literature on the effects of caring for a patient with cancer. 2010;19(10):1013–1025. [DOI] [PubMed] [Google Scholar]
- 17.Maltby KF, Sanderson CR, Lobb EA, Phillips JLJP, care s. Sleep disturbances in caregivers of patients with advanced cancer: A systematic review. 2017;15(1):125–140. [DOI] [PubMed] [Google Scholar]
- 18.Zhang Q, Yao D, Yang J, Zhou YJPo. Factors influencing sleep disturbances among spouse caregivers of cancer patients in Northeast China. 2014;9(10):e108614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kotronoulas G, Wengstrom Y, Kearney NJCn. Sleep patterns and sleep-impairing factors of persons providing informal care for people with cancer: a critical review of the literature. 2013;36(1):E1–E15. [DOI] [PubMed] [Google Scholar]
- 20.Hearson B, McClement SJIjopn. Sleep disturbance in family caregivers of patients with advanced cancer. 2007;13(10):495–501. [DOI] [PubMed] [Google Scholar]
- 21.Carney S, Koetters T, Cho M, et al. Differences in sleep disturbance parameters between oncology outpatients and their family caregivers. 2011;29(8):1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gibbins J, McCoubrie R, Kendrick AH, et al. Sleep-wake disturbances in patients with advanced cancer and their family carers. 2009;38(6):860–870. [DOI] [PubMed] [Google Scholar]
- 23.Carter PA, Acton GJJJogn. Personality and coping: predictors of depression and sleep problems among caregivers of individuals who have cancer. 2006;32(2):45–53. [DOI] [PubMed] [Google Scholar]
- 24.Martin SE, Engleman HM, Deary IJ, Douglas NJJAjor, medicine cc. The effect of sleep fragmentation on daytime function. 1996;153(4):1328–1332. [DOI] [PubMed] [Google Scholar]
- 25.Stepanski EJ, Perlis MLJJoPR. Behavioral sleep medicine: An emerging subspecialty in health psychology and sleep medicine. 2000;49(5):343–347. [DOI] [PubMed] [Google Scholar]
- 26.Mullington JM, Hinze-Selch D, Pollmächer TJAotNYAoS. Mediators of inflammation and their interaction with sleep. 2001;933(1):201–210. [DOI] [PubMed] [Google Scholar]
- 27.Mullington JM, Haack M, Toth M, Serrador JM, Meier-Ewert HKJPicd. Cardiovascular, inflammatory, and metabolic consequences of sleep deprivation. 2009;51(4):294–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mullington JM, Simpson NS, Meier-Ewert HK, Haack MJBp, endocrinology rC, metabolism. Sleep loss and inflammation. 2010;24(5):775–784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vgontzas AN, Liao D, Bixler EO, Chrousos GP, Vela-Bueno AJS. Insomnia with objective short sleep duration is associated with a high risk for hypertension. 2009;32(4):491–497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gunn HE, Buysse DJ, Matthews KA, Kline CE, Cribbet MR, Troxel WM. Sleep-Wake Concordance in Couples Is Inversely Associated With Cardiovascular Disease Risk Markers. Sleep. 2016;40(1):zsw028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. May 1989;28(2):193–213. [DOI] [PubMed] [Google Scholar]
- 32.Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1(3):385–401. [Google Scholar]
- 33.Hann D, Winter K, Jacobsen P. Measurement of depressive symptoms in cancer patients: evaluation of the Center for Epidemiological Studies Depression Scale (CES-D). Journal of psychosomatic research. 1999;46(5):437–443. [DOI] [PubMed] [Google Scholar]
- 34.Kenny DAJPb. Cross-lagged panel correlation: A test for spuriousness. 1975;82(6):887. [Google Scholar]
- 35.Lt Hu, Bentler PMJSemamj. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. 1999;6(1):1–55. [Google Scholar]
- 36.Carter PAJCn. A brief behavioral sleep intervention for family caregivers of persons with cancer. 2006;29(2):95–103. [DOI] [PubMed] [Google Scholar]
- 37.McCurry SM, Logsdon RG, Teri L, Vitiello MVJSmr. Sleep disturbances in caregivers of persons with dementia: contributing factors and treatment implications. 2007;11(2):143–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nijboer C, Triemstra M, Tempelaar R, Sanderman R, van den Bos GAJC. Determinants of caregiving experiences and mental health of partners of cancer patients. 1999;86(4):577–588. [DOI] [PubMed] [Google Scholar]
- 39.Hirshkowitz M, Whiton K, Albert SM, et al. National Sleep Foundation’s sleep time duration recommendations: methodology and results summary. Sleep health. 2015;1(1):40–43. [DOI] [PubMed] [Google Scholar]
- 40.Lauderdale DS, Knutson KL, Yan LL, Liu K, Rathouz PJJE. Self-reported and measured sleep duration: how similar are they? 2008;19(6):838–845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kakizaki M, Kuriyama S, Sone T, et al. Sleep duration and the risk of breast cancer: the Ohsaki Cohort Study. 2008;99(9):1502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Palesh O, Aldridge-Gerry A, Zeitzer JM, et al. Actigraphy-measured sleep disruption as a predictor of survival among women with advanced breast cancer. 2014;37(5):837–842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ji J, Zöller B, Sundquist K, Sundquist JJC. Increased risks of coronary heart disease and stroke among spousal caregivers of cancer patients. 2012:CIRCULATIONAHA. 111.057018. [DOI] [PubMed] [Google Scholar]
- 44.Lee S, Colditz GA, Berkman LF, Kawachi IJAjopm. Caregiving and risk of coronary heart disease in US women: a prospective study. 2003;24(2):113–119. [DOI] [PubMed] [Google Scholar]
- 45.Schulz R, Beach SRJJ. Caregiving as a risk factor for mortality: the Caregiver Health Effects Study. 1999;282(23):2215–2219. [DOI] [PubMed] [Google Scholar]
- 46.Cappuccio FP, Cooper D, D’elia L, Strazzullo P, Miller MAJEhj. Sleep duration predicts cardiovascular outcomes: a systematic review and meta-analysis of prospective studies. 2011;32(12):1484–1492. [DOI] [PubMed] [Google Scholar]
- 47.Cappuccio FP, Cooper D, D’elia L, Strazzullo P, Miller MA Sleep duration predicts cardiovascular outcomes: a systematic review and meta-analysis of prospective studies. European Heart Journal. 2011;32(12):1484–1492. [DOI] [PubMed] [Google Scholar]
- 48.Gottlieb DJ, Punjabi NM, Newman AB, et al. Association of sleep time with diabetes mellitus and impaired glucose tolerance. 2005;165(8):863–867. [DOI] [PubMed] [Google Scholar]
- 49.Gottlieb DJ, Redline S, Nieto FJ, et al. Association of usual sleep duration with hypertension: the Sleep Heart Health Study. 2006;29(8):1009–1014. [DOI] [PubMed] [Google Scholar]
- 50.Troxel WM, Buysse DJ, Matthews KA, et al. Sleep symptoms predict the development of the metabolic syndrome. 2010;33(12):1633–1640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Fernandez-Mendoza J, Vgontzas AN, Liao D, et al. Insomnia with objective short sleep duration and incident hypertension: the Penn State Cohort. 2012;60(4):929–935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Miaskowski C, Dodd M, Lee K, et al. Preliminary evidence of an association between a functional interleukin-6 polymorphism and fatigue and sleep disturbance in oncology patients and their family caregivers. 2010;40(4):531–544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Happe S, Berger KJA, Ageing. The association between caregiver burden and sleep disturbances in partners of patients with Parkinson’s disease. 2002;31(5):349–354. [DOI] [PubMed] [Google Scholar]
- 54.Garland SN, Johnson JA, Savard J, et al. Sleeping well with cancer: a systematic review of cognitive behavioral therapy for insomnia in cancer patients. 2014;10:1113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Carlson LE, Tamagawa R, Stephen J, Drysdale E, Zhong L, Speca MJPO. Randomized-controlled trial of mindfulness-based cancer recovery versus supportive expressive group therapy among distressed breast cancer survivors (MINDSET): long-term follow-up results. 2016;25(7):750–759. [DOI] [PubMed] [Google Scholar]
- 56.Shapiro SL, Bootzin RR, Figueredo AJ, Lopez AM, Schwartz GEJJopr. The efficacy of mindfulness-based stress reduction in the treatment of sleep disturbance in women with breast cancer: an exploratory study. 2003;54(1):85–91. [DOI] [PubMed] [Google Scholar]
- 57.Simeit R, Deck R, Conta-Marx BJSciC. Sleep management training for cancer patients with insomnia. 2004;12(3):176–183. [DOI] [PubMed] [Google Scholar]
- 58.McArdle N, Kingshott R, Engleman H, Mackay T, Douglas NJT. Partners of patients with sleep apnoea/hypopnoea syndrome: effect of CPAP treatment on sleep quality and quality of life. 2001;56(7):513–518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Gunn HE, Buysse DJ, Hasler BP, Begley A, Troxel WMJS. Sleep concordance in couples is associated with relationship characteristics. 2015;38(6):933–939. [DOI] [PMC free article] [PubMed] [Google Scholar]