Abstract
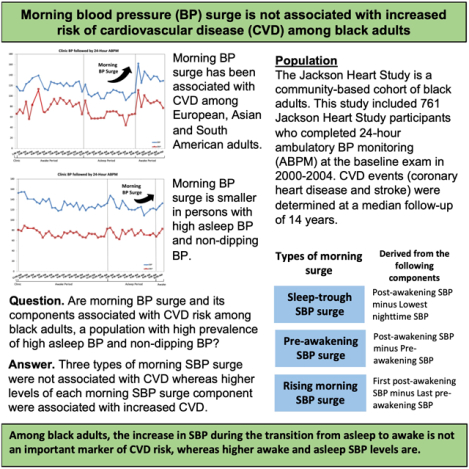
The cardiovascular disease (CVD) and mortality risk associated with morning blood pressure (BP) surge and its components among black adults, a population with high BP during the asleep period, is unknown. We studied Jackson Heart Study participants who completed 24-hour ambulatory BP monitoring at the baseline exam in 2000–2004 (n=761). The sleep-trough morning surge was calculated as the mean two-hour post-awakening systolic BP (SBP) minus the lowest nighttime SBP, pre-awakening morning surge as mean two-hour post-awakening SBP minus mean two-hour pre-awakening SBP, and rising morning surge as the first post-awakening SBP minus the last pre-awakening SBP. The primary outcome was the occurrence of CVD events including the composite of coronary heart disease or stroke. Over a median follow-up of 14.0 years, there were 74 CVD (coronary heart disease or stroke) events and 144 deaths. Higher tertiles of sleep-trough, pre-awakening, and rising SBP surge were not associated with CVD risk after multivariable adjustment. In contrast, the highest tertile of the individual components of morning surge including post-awakening SBP (tertiles 2 and 3 versus 1: hazard ratio [95% CI] 1.58 [0.71–3.53] and 4.04 [1.91–8.52], respectively), lowest nighttime SBP (1.29 [0.59–2.84] and 2.87 [1.41–5.83]), pre-awakening SBP (1.26 [0.57–2.80] and 2.79 [1.32–5.93]), first post-awakening SBP (1.60 [0.73–3.51] and 2.93 [1.40–6.16]), and last pre-awakening SBP (1.23 [0.57–2.68] and 2.99 [1.46–6.12]) was associated with increased CVD risk after multivariable adjustment. Among black adults, the components of morning SBP surge, but not morning SBP surge itself, were associated with increased CVD risk.
Keywords: morning surge, African American, outcomes, cardiovascular disease, all-cause mortality
GRAPHICAL ABSTRACT
INTRODUCTION
Blood pressure (BP) typically follows a diurnal pattern wherein the levels are lowest while asleep.1 An increase in BP over the transition from being asleep to awake is called the morning BP surge.1 Using BP measurements on ambulatory BP monitoring (ABPM), several definitions of morning BP surge have been examined including sleep-trough morning surge, pre-awakening morning surge and rising morning surge (Table 1).1 In some but not all prior studies, higher morning BP surge has been associated with an increased risk for cardiovascular disease (CVD) events and all-cause mortality.2–6
Table 1.
Definitions for each type of morning blood pressure surge and each component of the types of morning surge.
| Type of morning BP surge | Definition of morning BP surge and each morning BP surge component |
|---|---|
| Sleep-trough morning BP surge | Post-awakening BP (mean BP in the two hours after awakening) minus Lowest nighttime BP (mean of the lowest BP during sleep as well as the measurement before and after the lowest BP measurement) |
| Pre-awakening morning BP surge | Post-awakening BP (mean BP in the two hours after awakening) minus Pre-awakening BP (mean BP in the two hours before awakening) |
| Rising morning BP surge | First post-awakening BP (the one BP measurement immediately after awakening) minus Last pre-awakening BP (the one BP measurement immediately before awakening) |
Each type of morning surge and the components can be calculated for systolic BP and separately, diastolic BP.
BP: blood pressure.
In prior US-based studies, 50% to 60% of black adults had nocturnal hypertension, defined by asleep systolic BP (SBP) ≥ 120 mm Hg or asleep diastolic BP (DBP) ≥ 70 mm Hg.7, 8 Also, 40% to 70% of black participants had non-dipping SBP, defined by a sleep-to-awake SBP ratio <10%.7, 8 The high prevalence of nocturnal hypertension and non-dipping BP among blacks may result in a small morning surge. As the distribution of the morning BP surge may be smaller among black adults compared with other race/ethnic groups, it is unclear if morning BP surge is associated with an increased risk for CVD and mortality in this population.
In this study, we determined the associations of three types of morning BP surge (i.e. sleep-trough, pre-awakening, and rising BP morning surge) and, separately, the components that make up each morning surge type with CVD events and all-cause mortality. We also examined the rate of surge (i.e., slope of the morning BP) with CVD events and all-cause mortality.1, 9 To accomplish these aims, we analyzed data from the Jackson Heart Study (JHS), a community-based cohort comprised exclusively of black adults.
METHODS
Requests to access JHS data from qualified researchers trained in human subject confidentiality protocols may be submitted to BioLINCC, the NHLBI repository (https://biolincc.nhlbi.nih.gov/home/). Alternatively, investigators may submit manuscript proposals to the JHS at https://www.jacksonheartstudy.org. Statistical code is available from the corresponding author.
Study population
The JHS enrolled 5,306 community-dwelling black adults ≥20 years old between 2000 and 2004 from the Atherosclerosis Risk in the Community (ARIC) study site in Jackson, Mississippi, and a representative sample of urban and rural Jackson, Mississippi metropolitan tri-county (Hinds, Madison and Rankin counties) area residents, volunteers, randomly contacted individuals and family members of participants.10, 11 The current analysis was restricted to participants (n=1,148) who underwent ABPM at the baseline exam. For the analysis wherein the slope of morning surge was the exposure, we included participants with self-reported awake and asleep times, and a complete ABPM recording (defined below) (n=917). For the analyses examining the types and components of morning surge, the population was further restricted to 761 participants with at least three SBP and DBP measurements in the two hours before awakening (i.e., pre-awakening SBP and DBP) and three SBP and DBP measurements in the two hours after awakening (i.e., post-awakening SBP and DBP). The JHS was approved by the institutional review boards of the University of Mississippi Medical Center, Jackson State University, and Tougaloo College. All participants provided written informed consent.
Data collection
Self-reported information on socio-demographic factors, health behaviors and prior diagnosed co-morbid conditions were collected by trained staff during an in-home interview at baseline. Height, weight and clinic BP were measured, blood and urine samples were collected and the names of prescription and over the counter medications taken in the two weeks prior to the study visit were recorded by trained staff during a study examination at the JHS clinic. Clinic BP was measured twice with a random-zero sphygmomanometer using a standardized protocol, and the average of the two clinic BP measurements was calculated. The clinic BP measurements were calibrated to a semi-automated oscillometric device using data from 2115 participants who had simultaneous BP measurement on both devices using a Y-connector.12 Detailed definitions for the variables used in the analyses are provided in the Supplemental Methods. Participants were invited to complete ABPM following the study visit.
Ambulatory blood pressure monitoring
A Spacelabs model 90207 ABPM device was fitted on participants’ non-dominant arm. The device was programmed to measure BP every 20 minutes and participants returned to the clinic and the device was removed approximately 24 hours later. Participants also were asked to write down in a diary the times they went to sleep and awakened while performing ABPM. ABPM recordings were considered complete if there were ≥10 awake and ≥5 asleep SBP and DBP measurements.13, 14 Using all of the SBP and DBP measurements recorded, mean 24-hour systolic and diastolic SBP and DBP, respectively, were computed.15 Percentage SBP and DBP decline were defined as one minus the ratio of mean asleep-to-awake SBP and DBP multiplied by 100.15 Reverse SBP dipping, non-dipping SBP, SBP dipping, and extreme SBP dipping were defined as percentage SBP decline < 0%, 0% to < 10%, 10% to < 20%, and ≥ 20%, respectively. As shown in Table 1, for SBP and separately DBP, three types of morning surge, which have been examined in prior studies, were calculated using different components. Sleep-trough morning surge was calculated as mean BP in the two hours after awakening (i.e., post-awakening) minus the lowest nighttime BP measurement (i.e., mean of the lowest BP during sleep as well as the measurement before and after the lowest BP measurement). Pre-awakening morning surge was calculated as mean BP in the two hours post-awakening minus mean BP in the two hours before awakening. Rising morning BP surge was calculated as the first post-awakening BP measurement minus the last pre-awakening BP measurement. For SBP and separately DBP, to calculate the slope of BP surge, the participant-specific ambulatory BP pattern was estimated using a linear mixed model. Fixed effects in the model included a fifth degree orthogonal polynomial that captured variation in BP, over the 24-hour monitoring period. Random effects in the model included a participant-specific intercept and a third degree polynomial that permitted each participant’s ambulatory BP pattern to deviate from the population BP pattern.
Outcomes
The primary outcome was the occurrence of CVD events including the composite of coronary heart disease or stroke defined as non-carotid embolic or thrombotic brain infarction, brain hemorrhage or subarachnoid hemorrhage. All-cause mortality was a secondary outcome. As previously described, potential CVD events and vital status were assessed by annually contacting living participants or their proxies via telephone.16 Also, specific diagnoses were obtained for JHS participants from the discharge lists of Jackson, Mississippi tri-county area hospitals discharge lists. Death certificates were requested from the Mississippi State Department of Health as needed. Identification of a CVD-related hospitalization or death resulted in medical records being retrieved, abstracted, and adjudicated by trained physicians. Definite or probable CVD events and all-cause mortality were available through December 31, 2014.
Statistical analysis
The analyses for SBP described below were also performed for DBP. The distributions of participants’ sleep-trough, pre-awakening and rising morning SBP surge were plotted in a histogram using 5 mmHg increments. Characteristics were calculated among participants overall and grouped into tertiles of each type of morning surge (i.e., sleep-trough, pre-awakening and rising morning SBP surge). Cox proportional hazards regression with cause-specific hazards to calculate hazard ratios (HR) for CVD events, accounting for the competing risk of death, was used. The HRs for CVD events associated with tertiles 2 and 3 versus tertile 1 of each type of morning surge were determined. An initial model included adjustment for age, sex, less than a high school education, body mass index (BMI), and current smoking (Model 1). A second model included the variables in Model 1 and diabetes, reduced estimated glomerular filtration rate (eGFR), albuminuria, sleep duration, antihypertensive medication use and clinic SBP (Model 2). Additional adjustment included the variables in Model 2 and mean 24-hour SBP (Model 3). HR for CVD events associated with tertiles 2 and 3 versus tertile 1 of the slope of morning SBP surge was also calculated. For analyses of morning DBP surge, we adjusted for mean 24-hour DBP rather than mean 24-hour SBP in Models 3. A linear association across the higher tertiles of each type, and the slope, of morning surge associated with CVD events was calculated by modelling a three level variable for the tertiles as a continuous exposure. Identical analyses were conducted to calculate the association between the components of each type of morning surge (i.e., post-awakening, lowest nighttime, pre-awakening, first post-awakening and last pre-awakening SBP) and CVD events. Adjustment included the variables in Model 1 and Model 2 as described above. Additional adjustment for mean 24-hour SBP (i.e. Model 3) was not performed as the components of morning SBP surge are also components of 24-hour BP. All analyses were repeated for the secondary outcome of all-cause mortality.
In a sensitivity analysis, the HRs for CVD events associated with higher levels of morning SBP surge, expressed as a continuous variable and reflecting a standard deviation increase in each type of morning surge, were determined in adjusted models. The HRs for CVD events associated with one standard deviation increase in the components of each type of morning SBP surge was also determined in adjusted models.
Finally, the distribution of each type of morning surge in JHS participants was compared to the distribution in Europeans, Asian and South American populations reported in prior published studies evaluating the association of morning BP surge with clinical outcomes including CVD.2, 4–6, 17–19
Multiple imputation with chained equations was applied to create 10 data sets with missing values replaced by plausible estimates.20 Results from each data set were pooled using Rubin’s rules. P-values <0.05 were considered statistically significant. All analyses were conducted using SAS 9.4 (Cary, NC) and R version ≥3.6.0.
RESULTS
Participant characteristics
Participant characteristics are reported for the overall population and by tertile of each type of morning SBP surge in Table 2. Sleep-trough, pre-awakening and rising SBP morning surge were each normally distributed (Supplemental Figure S1).
Table 2.
Participant characteristics overall and by tertiles of each type of morning systolic blood pressure surge (n=761).
| Characteristic | Overall | Tertiles for each type of morning SBP surge | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Sleep-trough morning SBP surge | Pre-awakening morning SBP surge | Rising morning SBP surge | ||||||||
| 1 (lowest) |
2 | 3 (highest) |
1 (lowest) |
2 | 3 (highest) |
1 (lowest) |
2 | 3 (highest) |
||
| n=761 | n=253 | n=255 | n=253 | n=253 | n=254 | n=254 | n=245 | n=268 | n=248 | |
| Minimum to maximum morning surge, mmHg | − | −21.7 to <12.1 | 12.1 to <21.3 | 21.3 to 48.0 | −25.2 to <2.2 | 2.2 to <10.9 | 10.9 to 37.3 | −46.0 to <−2.0 | −2.0 to <7.0 | 7.0 to 43.0 |
| Age, years | 58.7 (10.9) | 58.1 (11.5) | 58.1 (11.1) | 59.8 (10.0) | 60.8 (11.0) | 58.0 (11.0) | 57.2 (10.4) | 59.9 (10.8) | 58.4 (11.2) | 57.7 (10.6) |
| Male sex | 245 (32.2%) | 83 (32.8%) | 86 (33.7%) | 76 (30.0%) | 66 (26.1%) | 87 (34.3%) | 92 (36.2%) | 68 (27.8%) | 99 (36.9%) | 78 (31.5%) |
| Less than a high school education | 139 (18.3%) | 47 (18.6%) | 47 (18.5%) | 45 (17.9%) | 57 (22.5%) | 40 (15.8%) | 42 (16.6%) | 44 (18.0%) | 48 (18.0%) | 47 (19.0%) |
| Body mass index, kg/m2 | 30.8 (6.3) | 31.7 (7.0) | 30.6 (6.4) | 30.0 (5.3) | 32.2 (6.8) | 30.7 (6.3) | 29.4 (5.4) | 31.4 (6.7) | 30.6 (6.4) | 30.3 (5.7) |
| Current smoker | 76 (10.0%) | 25 (9.9%) | 22 (8.6%) | 29 (11.5%) | 22 (8.7%) | 27 (10.6%) | 27 (10.6%) | 21 (8.6%) | 25 (9.3%) | 30 (12.1%) |
| Diabetes | 209 (27.6%) | 73 (29.0%) | 67 (26.6%) | 69 (27.4%) | 81 (32.4%) | 59 (23.4%) | 69 (27.2%) | 74 (30.3%) | 69 (26.0%) | 66 (26.7%) |
| Reduced eGFR | 82 (10.8%) | 30 (11.9%) | 28 (11.1%) | 24 (9.5%) | 37 (14.8%) | 28 (11.1%) | 17 (6.7%) | 34 (14.0%) | 21 (7.9%) | 27 (10.9%) |
| Albuminuria | 63 (10.5%) | 27 (12.9%) | 16 (8.2%) | 20 (10.4%) | 32 (15.4%) | 11 (5.8%) | 20 (10.0%) | 23 (11.4%) | 20 (9.9%) | 20 (10.3%) |
| Sleep duration, hours | 8.2 (1.7) | 7.9 (1.8) | 8.3 (1.7) | 8.5 (1.6) | 8.4 (1.8) | 8.3 (1.6) | 8.1 (1.7) | 8.2 (1.8) | 8.2 (1.7) | 8.3 (1.7) |
| Antihypertensive medication use | 424 (57.1%) | 135 (55.3%) | 142 (57.3%) | 147 (58.8%) | 158 (64.8%) | 130 (52.6%) | 136 (54.2%) | 147 (62.0%) | 149 (57.3%) | 128 (52.2%) |
| SBP, mmHg | ||||||||||
| Clinic | 127 (16.1) | 126 (15.2) | 126 (14.8) | 129 (18.0) | 129 (15.1) | 125 (16.0) | 128 (16.9) | 128 (15.5) | 127 (15.5) | 127 (17.3) |
| Daytime | 130 (13.6) | 127 (12.9) | 130 (13.6) | 132 (13.8) | 130 (13.6) | 127 (12.9) | 132 (14.0) | 131 (13.7) | 128 (12.5) | 130 (14.6) |
| Nighttime | 121 (15.5) | 124 (15.9) | 122 (15.3) | 119 (15.0) | 128 (16.1) | 119 (14.2) | 117 (14.0) | 125 (16.3) | 120 (13.7) | 119 (15.9) |
| 24-hour | 127 (13.8) | 126 (13.6) | 127 (13.9) | 127 (13.9) | 129 (14.1) | 124 (13.1) | 127 (13.8) | 129 (14.0) | 125 (12.5) | 126 (14.7) |
| DBP, mmHg | ||||||||||
| Clinic | 74.2 (8.6) | 74.0 (8.7) | 74.2 (8.2) | 74.3 (9.0) | 74.1 (8.4) | 73.5 (8.6) | 74.9 (8.9) | 73.5 (8.8) | 74.7 (8.9) | 74.2 (8.2) |
| Daytime | 78.1 (9.3) | 76.6 (9.6) | 78.8 (8.8) | 78.8 (9.4) | 77.2 (9.7) | 76.9 (8.6) | 80.1 (9.3) | 77.5 (9.6) | 78.4 (9.1) | 78.3 (9.2) |
| Nighttime | 68.8 (9.5) | 70.6 (10.3) | 69.6 (8.7) | 66.2 (8.7) | 72.0 (10.1) | 67.8 (8.6) | 66.6 (8.8) | 69.8 (9.9) | 69.5 (9.1) | 66.9 (9.1) |
| 24-hour | 74.6 (9.0) | 74.4 (9.5) | 75.4 (8.4) | 74.0 (8.9) | 75.2 (9.5) | 73.5 (8.3) | 75.2 (9.0) | 74.7 (9.3) | 75.1 (8.8) | 74.1 (8.9) |
| Percentage SBP decline, % | 6.5 (6.7) | 2.6 (6.2) | 6.5 (4.9) | 10.2 (6.7) | 1.6 (6.3) | 6.4 (4.7) | 11.3 (5.2) | 4.1 (7.3) | 6.5 (5.6) | 8.7 (6.5) |
| Percentage DBP decline, % | 11.7 (8.0) | 7.8 (7.8) | 11.6 (6.6) | 15.8 (7.5) | 6.7 (7.2) | 11.6 (6.6) | 16.8 (6.8) | 9.7 (8.3) | 11.1 (7.1) | 14.3 (7.9) |
| BP dipping status | ||||||||||
| Reverse SBP dipping | 118 (15.5%) | 78 (30.8%) | 27 (10.6%) | 13 (5.1%) | 90 (35.6%) | 25 (9.8%) | 3 (1.2%) | 60 (24.5%) | 32 (11.9%) | 26 (10.5%) |
| Non-dipping SBP | 430 (56.5%) | 155 (61.3%) | 169 (66.3%) | 106 (41.9%) | 151 (59.7%) | 175 (68.9%) | 104 (40.9%) | 146 (59.6%) | 166 (61.9%) | 118 (47.6%) |
| SBP dipping | 197 (25.9%) | 20 (7.9%) | 58 (22.7%) | 119 (47.0%) | 12 (4.7%) | 54 (21.3%) | 131 (51.6%) | 36 (14.7%) | 68 (25.4%) | 93 (37.5%) |
| Extreme SBP dipping | 16 (2.1%) | 0 (0.0%) | 1 (0.4%) | 15 (5.9%) | 0 (0.0%) | 0 (0.0%) | 16 (6.3%) | 3 (1.2%) | 2 (0.7%) | 11 (4.4%) |
The numbers in the table are mean (standard deviation) or percentage.
eGFR: estimated glomerular filtration rate.
SBP: systolic blood pressure.
DBP: diastolic blood pressure.
Associations of the types of morning surge with CVD events and all-cause mortality
There were 74 CVD events and 144 deaths over a median follow-up of 14.0 years. There was no evidence of an association between higher tertiles of sleep-trough morning SBP surge and increased CVD risk after adjustment for age, sex, less than a high school education, BMI, and current smoking in Model 1 (p-trend=0.609), after adjustment for the variables in Model 1 plus diabetes, reduced eGFR, albuminuria, sleep duration, antihypertensive medication use, and clinic SBP in Model 2 (p-trend=0.469), and additional adjustment for mean 24-hour SBP in Model 3 (p-trend=0.530; Table 3). There was also no evidence of an association of higher tertiles of pre-awakening or rising morning SBP surge with CVD risk in any of the adjusted models. Higher tertiles of sleep-trough, pre-awakening, and rising morning SBP surge were also not associated with all-cause mortality in any of the adjusted models (Supplemental Table S1).
Table 3.
Hazard ratios for cardiovascular disease events associated with each type of morning systolic blood pressure surge (n=761).
| Type of morning SBP surge | N events/N participants | Hazard ratio (95% confidence interval) | ||
|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | ||
| Sleep-trough morning SBP surge (range), mmHg | ||||
| Tertile 1 (−21.7 to < 12.1) | 23/253 | 1 (reference) | 1 (reference) | 1 (reference) |
| Tertile 2 (12.1 to < 21.3) | 24/255 | 1.16 (0.65–2.06) | 1.25 (0.69–2.28) | 1.11 (0.61–2.02) |
| Tertile 3 (21.3 to 48.0) | 27/253 | 1.16 (0.66–2.04) | 1.25 (0.69–2.24) | 1.21 (0.67–2.16) |
| P-trend | − | 0.609 | 0.469 | 0.530 |
| Pre-awakening morning SBP surge (range), mmHg | ||||
| Tertile 1 (−25.2 to < 2.2) | 31/253 | 1(reference) | 1(reference) | 1(reference) |
| Tertile 2 (2.2 to < 10.9) | 17/254 | 0.59 (0.33–1.08) | 0.68 (0.37–1.27) | 0.77 (0.42–1.43) |
| Tertile 3 (10.9 to 37.3) | 26/254 | 1.04 (0.60–1.80) | 1.11 (0.64–1.92) | 1.18 (0.68–2.07) |
| P-trend | − | 0.959 | 0.778 | 0.607 |
| Rising morning SBP surge (range), mmHg | ||||
| Tertile 1 (−46.0 to < −2.0) | 26/245 | 1(reference) | 1(reference) | 1(reference) |
| Tertile 2 (−2.0 to < 7.0) | 22/268 | 0.79 (0.44–1.41) | 0.80 (0.45–1.44) | 0.92 (0.51–1.68) |
| Tertile 3 (7.0 to 43.0) | 26/248 | 1.03 (0.59–1.78) | 0.98 (0.56–1.73) | 1.05 (0.60–1.84) |
| P-trend | − | 0.939 | 0.956 | 0.873 |
SBP: systolic blood pressure.
The hazard ratios for cardiovascular disease are adjusted for the competing risk of death.
Model 1: Adjustment for age, sex, less than a high school education, body mass index and current smoking status.
Model 2: Adjustment for the variables in model 1 and diabetes status, estimated glomerular filtration rate < 60 mL/min/1.73 m2, albumin to creatinine ratio > 30 mg/g, sleep duration, antihypertensive medication use and clinic systolic blood pressure.
Model 3: Adjustment for the variables in model 2 and 24-hour systolic blood pressure.
There was no evidence of associations of higher tertiles of sleep-trough morning DBP surge, pre-awakening morning DBP surge, and rising morning DBP surge with CVD risk, and separately, all-cause mortality in any of the adjusted models (Supplemental Table S2).
Associations of the components of morning surge with CVD events and all-cause mortality
There was a graded increasing risk for CVD events across higher tertiles of post-awakening, lowest nighttime, pre-awakening, first post-awakening and last pre-awakening components of SBP morning surge in each adjusted model (Table 4). Higher tertiles of the components of SBP morning surge were not associated with all-cause mortality in a fully adjusted model (Model 2; Supplemental Table S3).
Table 4.
Hazard ratios for cardiovascular disease events associated with each component of morning systolic blood pressure surge (n=761).
| Morning SBP surge component | N events/N participants | Hazard ratio (95% confidence interval) | |
|---|---|---|---|
| Model 1 | Model 2 | ||
| Post-awakening SBP (range), mmHg | |||
| Tertile 1 (86.0 to <121.6) | 10/251 | 1 (reference) | 1 (reference) |
| Tertile 2 (121.6 to <135.0) | 17/259 | 1.47 (0.67–3.22) | 1.58 (0.71–3.53) |
| Tertile 3 (135.0 to 197.3) | 47/251 | 3.80 (1.91–7.55) | 4.04 (1.91–8.52) |
| P-trend | − | <0.001 | <0.001 |
| Lowest nighttime SBP (range), mmHg | |||
| Tertile 1 (64.0 to < 97.0) | 11/255 | 1 (reference) | 1 (reference) |
| Tertile 2 (97.0 to <109.0) | 16/242 | 1.39 (0.64–3.04) | 1.29 (0.59–2.84) |
| Tertile 3 (109.0 to 170.0) | 47/264 | 3.30 (1.69–6.45) | 2.87 (1.41–5.83) |
| P-trend | − | <0.001 | 0.001 |
| Pre-awakening SBP (range), mmHg | |||
| Tertile 1 (89.7 to <114.3) | 10/253 | 1 (reference) | 1 (reference) |
| Tertile 2 (114.3 to <128.3) | 18/255 | 1.29 (0.58–2.84) | 1.26 (0.57–2.80) |
| Tertile 3 (128.3 to 194.7) | 46/253 | 3.14 (1.55–6.37) | 2.79 (1.32–5.93) |
| P-trend | − | <0.001 | 0.002 |
| First post-awakening SBP (range), mmHg | |||
| Tertile 1 (84.0 to <119.0) | 10/254 | 1 (reference) | 1 (reference) |
| Tertile 2 (119.0 to <135.0) | 18/251 | 1.61 (0.74–3.51) | 1.60 (0.73–3.51) |
| Tertile 3 (135.0 to 195.0) | 46/256 | 3.30 (1.64–6.62) | 2.93 (1.40–6.16) |
| P-trend | − | <0.001 | 0.003 |
| Last pre-awakening SBP (range), mmHg | |||
| Tertile 1 (75.0 to <115.0) | 11/254 | 1 (reference) | 1 (reference) |
| Tertile 2 (115.0 to <131.0) | 17/246 | 1.35 (0.63–2.91) | 1.23 (0.57–2.68) |
| Tertile 3 (131.0 to 200.0) | 46/261 | 3.19 (1.62–6.28) | 2.99 (1.46–6.12) |
| P-trend | − | <0.001 | <0.001 |
SBP: systolic blood pressure.
The hazard ratios for cardiovascular disease are adjusted for the competing risk of death.
Model 1: Adjustment for age, sex, less than a high school education, body mass index and current smoking status.
Model 2: Adjustment for the variables in model 1 and diabetes status, estimated glomerular filtration rate < 60 mL/min/1.73 m2, albumin to creatinine ratio > 30 mg/g, sleep duration, antihypertensive medication use, and clinic systolic blood pressure.
Higher tertiles of post-awakening DBP were associated with higher CVD risk (Supplemental Table S4). There were no evidence of associations of the other morning DBP surge components with CVD risk. None of the components of morning DBP surge were associated with all-cause mortality.
Rate of increase in morning surge with CVD events and all-cause mortality
There was no evidence that a higher rate of increase in morning SBP and DBP surge was associated with CVD or all-cause mortality in any of the adjusted models (Table 5, Supplemental Table S5 and Supplemental Table S6).
Table 5.
Hazard ratios for cardiovascular disease events associated with the slope of morning systolic blood pressure surge (n=917).
| Slope of morning SBP surge (range), mmHg/hour | N events/N participants | Hazard ratio (95% confidence interval) | ||
|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | ||
| Tertile 1 (−8.3 to < −1.8) | 24/305 | 1 (reference) | 1 (reference) | 1 (reference) |
| Tertile 2 (−1.8 to < −0.2) | 26/306 | 1.13 (0.65–1.98) | 1.20 (0.69–2.11) | 1.14 (0.65–1.99) |
| Tertile 3 (−0.2 to 9.6) | 41/306 | 1.57 (0.94–2.62) | 1.43 (0.85–2.43) | 1.33 (0.78–2.27) |
| P-trend | − | 0.077 | 0.180 | 0.286 |
SBP: systolic blood pressure.
The hazard ratios for cardiovascular disease are adjusted for the competing risk of death.
Model 1: Adjustment for age, sex, less than a high school education, body mass index and current smoking status.
Model 2: Adjustment for the variables in model 1 and diabetes status, estimated glomerular filtration rate < 60 mL/min/1.73 m2, albumin to creatinine ratio > 30 mg/g, sleep duration, antihypertensive medication use and clinic systolic blood pressure.
Model 3: Adjustment for the variables in model 2 and 24-hour systolic blood pressure.
Sensitivity analysis
There were no evidence of associations of sleep-trough morning SBP surge, pre-awakening morning SBP surge, and rising morning SBP surge, when modeled as continuous variables, with CVD risk (Supplemental Table S7). In contrast, higher post-awakening, lowest nighttime, pre-awakening, first post-awakening and last pre-awakening components of SBP morning surge, when modeled as continuous variables, were each associated with increased CVD risk (Supplemental Table S8).
Comparison with prior studies
A smaller percentage of participants in the current study had a higher morning SBP surge when compared to their counterparts from prior studies (Table 6). For example, no participants in the current study were in the top decile of sleep-trough morning SBP surge using the threshold (>55 mm Hg) from a 2003 study by Kario et al.2 Also, 2.9% of participants in the current study were in the top quintile of pre-awakening SBP surge using the threshold (>25 mm Hg) from a 2006 study by Metoki et al.4 Finally, no participants in the current study were in the top decile of rising SBP morning surge using the threshold (≥40 mm Hg) from a 2011 study by Israel et al.17
Table 6.
Summary of the distribution of each type of morning systolic blood pressure surge in prior studies and the current study.
| Type of morning SBP surge | Author, year | Country of origin for study participants (n participants) |
Distribution and thresholds for morning SBP surge, mmHg | Proportion of participants characterized by the thresholds for morning surge, % | |
|---|---|---|---|---|---|
| Prior study | Current study among black from the Jackson Heart Study | ||||
| Current study | |||||
| Sleep-trough SBP surge | Booth, 2019 (current study) |
United States (n=761 blacks) |
Tertile 1 −21.7 to < 12.1 | NA | 33.3% |
| Tertile 2: 12.1 to < 21.3 | 33.3% | ||||
| Tertile 3: 21.3 to 48.0 | 33.3% | ||||
| Pre-awakening SBP surge | Tertile 1: −25.2 to < 2.2 | NA | 33.3% | ||
| Tertile 2: 2.2 to < 10.9 | 33.3% | ||||
| Tertile 3: 10.9 to 37.3 | 33.3% | ||||
| Rising SBP surge | Tertile 1: −46.0 to < −2.0 | NA | 33.3% | ||
| Tertile 2: −2.0 to < 7.0 | 33.3% | ||||
| Tertile 3: 7.0 to 43.0 | 33.3% | ||||
| Prior studies | |||||
| Sleep-trough SBP surge | Kario, 20032 | Japan (n=519) |
> 55 (i.e., top decile) |
10% | 0.0% |
| Metoki, 20064 | Ohasama, Iwate Prefecture, Japan (n=1430) |
Quintile 1: < 16 | Quintile 1: 20% | 47.4% | |
| Quintile 2: 16 to 23 | Quintile 2: 20% | 24.7% | |||
| Quintile 3: NR | Quintile 3: 20% | NA | |||
| Quintile 4: NR | Quintile 4: 20% | NA | |||
| Quintile 5: ≥ 40 | Quintile 5: 20% | 2.9% | |||
| Amici, 20095 | Italy (n=42) |
≥ 34 (i.e., top tertile) |
33.3% | 7.1% | |
| Li, 20106 | Europe, Asia and South America: IDACO (n=5645) |
≥ 37 (i.e., top decile) |
10% | 4.6% | |
| >20.9 | NR | 34.7% | |||
| Verdecchia, 201218 | Italy: Progetto Ipertensione Umbria Monitoraggio Ambulatoriale Study (n=3012) |
Quartile 1: ≤ 19.5 | Quartile 1: 25% | 60.8% | |
| Quartile 2: 19.5 to ≤ 27.5 | Quartile 2: 25% | 22.9% | |||
| Quartile 3: 27.5 to ≤ 36 | Quartile 3: 25% | 11.4% | |||
| Quartile 4: > 36 | Quartile 4: 25% | 4.9% | |||
| Pre-awakening SBP surge | Metoki, 20064 | Ohasama, Iwate Prefecture, Japan (n=1430) |
Quintile 1: < 3 | Quintile 1: 20% | 35.7% |
| Quintile 2: 3 to ≤ 11 | Quintile 2: 20% | 31.0% | |||
| Quintile 3: 11 to ≤ 17 | Quintile 3: 20% | 19.4% | |||
| Quintile 4: 17 to ≤ 25 | Quintile 4: 20% | 10.1% | |||
| Quintile 5: > 25 | Quintile 5: 20% | 3.7% | |||
| Li, 20106 | Europe, Asia and South America: IDACO (n=5645) |
≥ 28 (i.e., top decile) |
10% | 2.5% | |
| >21.5 | NR | 5.7% | |||
| Verdecchia, 201218 | Italy: Progetto Ipertensione Umbria Monitoraggio Ambulatoriale Study (n=3012) |
Quartile 1: ≤ 9.5 | Quartile 1: 25% | 61.8% | |
| Quartile 2: > 9.5 to ≤ 17.5 | Quartile 2: 25% | 25.5% | |||
| Quartile 3: > 17.5 to ≤ 27.5 | Quartile 3: 25% | 10.0% | |||
| Quartile 4: >27.5 | Quartile 4: 25% | 2.8% | |||
| Cocchina, 201919 | Italy (n=1073) |
> 27 (i.e. top decile) |
10% | 3.2% | |
| Rising SBP surge | Israel, 201117 | Israel (n=2627) |
≥ 40 (i.e., top decile) |
10% | 0.0% |
SBP: systolic blood pressure.
NA: not applicable
NR: not reported.
IDACO: International Database of Ambulatory BP in relation to Cardiovascular Outcome
DISCUSSION
In this prospective community-based cohort study of black adults, higher tertiles of sleep-trough, pre-awakening, and rising morning SBP and DBP surge were not associated with CVD. In contrast, higher tertiles of the components of SBP morning surge including post-awakening SBP, lowest nighttime SBP, pre-awakening SBP, first post-awakening SBP, and last pre-awakening SBP were each associated with increased CVD risk. Higher tertiles of post-awakening DBP were associated with higher CVD risk. Finally, higher tertiles of morning SBP and DBP surge and their components were not associated with all-cause mortality.
An association between morning BP surge and CVD and mortality has been reported in some, but not all, studies.3, 6, 17, 18, 21 For example, an analysis of the IDACO study that included 5645 Europeans, Asians and South Americans, the multivariable adjusted HR (95% CI) for CVD and mortality in those with sleep-trough SBP surge ≥37 versus <37 mmHg was 1.30 (1.06–1.60) and 1.32 (1.09–1.59), respectively, and pre-awakening SBP surge ≥28 versus <28 mmHg was 1.45 (1.17–1.80) and 1.23 (1.00–1.51), respectively.6 In contrast, among 3012 Italian adults, increased sleep-trough morning SBP surge was associated with a lower risk of CVD events: the HR (95% CI) for CVD associated with sleep-trough morning SBP surge >36 versus ≤19.5 mmHg was 0.60 (0.41–0.88) and pre-awakening morning SBP surge >27.5 versus ≤9.5 mmHg was 0.58 (0.38–0.89).18 Further, higher sleep-trough and pre-awakening morning SBP surge were not associated with mortality in 2627 Israeli adults.17 A systematic review and meta-analysis of 17 studies demonstrated sleep-trough morning SBP surge >36 versus ≤36 mmHg and pre-awakening morning SBP surge >27.5 versus ≤27.5 mm Hg were not associated with CVD (HR [95% CI]: 0.90 [0.42–1.91] for sleep-trough morning SBP surge and HR [95% CI]: 0.94 [0.39–2.28] for pre-awakening morning SBP surge) and mortality (HR [95% CI]: 1.24 [1.00–1.54] for sleep-trough morning SBP surge and HR [95% CI]: 1.09 [0.77–1.54] for pre-awakening morning SBP surge).21 While sleep-trough and pre-awakening morning surge have been more commonly investigated in prior studies, higher rising morning SBP surge was associated with CVD events in a study of 507 adults in Bordeaux, France.3
Two factors may have contributed to some studies reporting an association between higher morning BP surge and outcomes while others did not. First, there was no consistent approach across the individual studies in the types of morning BP surge examined and the threshold definitions used to define high morning BP surge. Second, prior studies did not consistently adjust for 24-hour BP.5, 22 In the current study, there were no associations between morning SBP surge, defined as tertiles, with CVD and all-cause mortality after multivariable adjustment including 24-hour SBP. No association was present regardless of the definition of morning surge used. Although sleep-trough, pre-awakening and rising SBP surge were normally distributed in the current study of black adults, the distributions were narrower, indicating less inter-individual variance, compared with prior studies. These data support our hypothesis that black adults, a population with a high prevalence of high BP while asleep, have a substantially smaller morning BP surge compared with non-black populations, thereby attenuating any association between morning BP surge and CVD events in black adults.7
In addition to examining three types of morning BP surge, we evaluated the association of the components of each type of morning BP surge with CVD events and all-cause mortality. Higher levels of the components of morning SBP surge including post-awakening SBP, lowest nighttime SBP, pre-awakening SBP, first post-awakening SBP, and last pre-awakening SBP were each associated with increased CVD risk in multivariable adjusted models. These findings suggest that the components (i.e. BP levels) rather than morning BP surge provide important information on the risk of CVD events among black adults.
The current study has several strengths. The JHS is a community-based study comprised exclusively of black adults, a population with a high risk for premature CVD and premature mortality.23 Also, the JHS is one of the largest community-based prospective studies conducted in the US that performed ABPM. The comprehensive data collection in the JHS permitted adjustment for numerous potential confounders. CVD events and all-cause mortality, identified by actively following participants, were adjudicated following a standardized approach. However, there are also potential limitations. Only a subgroup of JHS participants completed ABPM. There were differences in characteristics of JHS participants who did and did not complete ABPM at their baseline visit.24 There is no reason to expect that this would impact the internal validity or generalizability of the current study. As only 74 CVD events occurred during follow-up, the study may be underpowered to detect an association between morning surge and CVD events. Sleep and wake times were self-reported. There is a possibility that these times were misreported by some participants resulting in potential errors in the estimates of morning BP surge. Finally, ABPM was only performed a single time. Given the limited reproducibility of morning surge,25 participants may have been misclassified which would bias the results towards the null.
Supplementary Material
Perspectives.
The distribution of the morning BP surge was smaller in black adults in the current study, compared with non-black adults from prior studies. While higher morning SBP and DBP surge on ABPM were not associated with CVD risk, the components of morning SBP and DBP surge were associated with CVD risk. These findings suggest that among black adults, the change in BP during the asleep to awake transition period is not associated with CVD risk. In contrast, the average BP levels while awake and asleep are more important markers of CVD risk.
NOVELTY AND SIGNIFICANCE.
What is New?
A larger morning BP surge has been associated with increased CVD risk among Asian, European and South American adults.
This study examined the CVD risk associated with morning surge among black adults.
What is Relevant?
The high prevalence of nocturnal hypertension and non-dipping BP among black adults may result in a small morning surge, thereby attenuating any association between morning BP surge and CVD events.
Summary
Among black adults in the Jackson Heart Study, three types of morning SBP surge (sleep-trough, pre-awakening, and rising morning SBP surge) were not associated with increased CVD risk.
In contrast, the components of morning SBP surge including post-awakening SBP, lowest nighttime SBP, pre-awakening SBP, first post-awakening SBP, last pre-awakening SBP were each associated with increased CVD risk.
Therefore, average BP levels while awake and asleep are more important markers of CVD risk among black adults.
SOURCES OF FUNDING
The Jackson Heart Study (JHS) is supported and conducted in collaboration with Jackson State University (HHSN268201800013I), Tougaloo College (HHSN268201800014I), the Mississippi State Department of Health (HHSN268201800015I/HHSN26800001) and the University of Mississippi Medical Center (HHSN268201800010I, HHSN268201800011I and HHSN268201800012I) contracts from the National Heart, Lung, and Blood Institute (NHLBI) and the National Institute for Minority Health and Health Disparities (NIMHD). The authors also wish to thank the staffs and participants of the JHS.
JNBII received research support through grant 15SFRN2390002 from the American Heart Association.
BCJ received research support through grant 15SFRN2390002 from the American Heart Association and grant R01 HL117323 from the NHLBI.
MA received research support through KL2TR001874 from the NIH.
MS did not report receiving research support.
MB received support through 5K23HL125939-03 from the NIH/NHLBI.
PM received research support through grant 15SFRN2390002 from the American Heart Association and R01HL117323 from the NIH/NHLBI.
DS received research support through grant 15SFRN2390002 from the American Heart Association and grant R01HL117323 and K24-HL125704 from the NIH/NHLBI.
Footnotes
DISCLOSURES
PM receives an institutional grant from Amgen Inc. unrelated to the topic of the current manuscript. There are no other potential conflicts of interest.
REFERENCES
- 1.Kario K Morning surge in blood pressure and cardiovascular risk: evidence and perspectives. Hypertension. 2010;56:765–73. [DOI] [PubMed] [Google Scholar]
- 2.Kario K, Pickering TG, Umeda Y, Hoshide S, Hoshide Y, Morinari M, Murata M, Kuroda T, Schwartz JE, Shimada K. Morning surge in blood pressure as a predictor of silent and clinical cerebrovascular disease in elderly hypertensives: a prospective study. Circulation. 2003;107:1401–6. [DOI] [PubMed] [Google Scholar]
- 3.Gosse P, Lasserre R, Minifie C, Lemetayer P, Clementy J. Blood pressure surge on rising. J Hypertens. 2004;22:1113–8. [DOI] [PubMed] [Google Scholar]
- 4.Metoki H, Ohkubo T, Kikuya M, Asayama K, Obara T, Hashimoto J, Totsune K, Hoshi H, Satoh H, Imai Y. Prognostic significance for stroke of a morning pressor surge and a nocturnal blood pressure decline: the Ohasama study. Hypertension. 2006;47:149–54. [DOI] [PubMed] [Google Scholar]
- 5.Amici A, Cicconetti P, Sagrafoli C, Baratta A, Passador P, Pecci T, Tassan G, Verrusio W, Marigliano V, Cacciafesta M. Exaggerated morning blood pressure surge and cardiovascular events. A 5-year longitudinal study in normotensive and well-controlled hypertensive elderly. Arch Gerontol Geriatr. 2009;49:e105–9. [DOI] [PubMed] [Google Scholar]
- 6.Li Y, Thijs L, Hansen TW, Kikuya M, Boggia J, Richart T, Metoki H, Ohkubo T, Torp-Pedersen C, Kuznetsova T, Stolarz-Skrzypek K, Tikhonoff V, Malyutina S, Casiglia E, Nikitin Y, Sandoya E, Kawecka-Jaszcz K, Ibsen H, Imai Y, Wang J, Staessen JA, International Database on Ambulatory Blood Pressure Monitoring in Relation to Cardiovascular Outcomes I. Prognostic value of the morning blood pressure surge in 5645 subjects from 8 populations. Hypertension. 2010;55:1040–8. [DOI] [PubMed] [Google Scholar]
- 7.Thomas SJ, Booth JN 3rd, Bromfield SG, Seals SR, Spruill TM, Ogedegbe G, Kidambi S, Shimbo D, Calhoun D, Muntner P. Clinic and ambulatory blood pressure in a population-based sample of African Americans: the Jackson Heart Study. J Am Soc Hypertens. 2017;11:204–212 e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Booth JN, Anstey DE, Bello NA, Jaeger BC, Pugliese DN, Thomas SJ, Deng L, Shikany JM, Lloyd-Jones D, Schwartz JE, Lewis CE, Shimbo D, Muntner P. Race and sex differences in asleep blood pressure: The Coronary Artery Risk Development in Young Adults (CARDIA) study. J Clin Hypertens (Greenwich). 2019;21:184–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Parati G, Vrijens B, Vincze G. Analysis and interpretation of 24-h blood pressure profiles: appropriate mathematical models may yield deeper understanding. Am J Hypertens. 2008;21:123–5; discussion 127–9. [DOI] [PubMed] [Google Scholar]
- 10.Fuqua SR, Wyatt SB, Andrew ME, Sarpong DF, Henderson FR, Cunningham MF, Taylor HA Jr. Recruiting African-American research participation in the Jackson Heart Study: methods, response rates, and sample description. Ethn Dis. 2005;15:S6–18-29. [PubMed] [Google Scholar]
- 11.Wilson JG, Rotimi CN, Ekunwe L, Royal CD, Crump ME, Wyatt SB, Steffes MW, Adeyemo A, Zhou J, Taylor HA Jr., Jaquish C. Study design for genetic analysis in the Jackson Heart Study. Ethn Dis. 2005;15:S6–30-37. [PubMed] [Google Scholar]
- 12.Seals SR, Colantonio LD, Tingle JV, Shimbo D, Correa A, Griswold ME, Muntner P. Calibration of blood pressure measurements in the Jackson Heart Study. Blood Press Monit. 2019;24:130–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thijs L, Hansen TW, Kikuya M, Bjorklund-Bodegard K, Li Y, Dolan E, Tikhonoff V, Seidlerova J, Kuznetsova T, Stolarz K, Bianchi M, Richart T, Casiglia E, Malyutina S, Filipovsky J, Kawecka-Jaszcz K, Nikitin Y, Ohkubo T, Sandoya E, Wang J, Torp-Pedersen C, Lind L, Ibsen H, Imai Y, Staessen JA, O’Brien E, Investigators I. The International Database of Ambulatory Blood Pressure in relation to Cardiovascular Outcome (IDACO): protocol and research perspectives. Blood Press Monit. 2007;12:255–62. [DOI] [PubMed] [Google Scholar]
- 14.Bromfield SG, Booth JN 3rd, Loop MS, Schwartz JE, Seals SR, Thomas SJ, Min YI, Ogedegbe G, Shimbo D, Muntner P. Evaluating different criteria for defining a complete ambulatory blood pressure monitoring recording: data from the Jackson Heart Study. Blood Press Monit. 2018;23:103–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.O’Brien E, Parati G, Stergiou G, Asmar R, Beilin L, Bilo G, Clement D, de la Sierra A, de Leeuw P, Dolan E, Fagard R, Graves J, Head GA, Imai Y, Kario K, Lurbe E, Mallion JM, Mancia G, Mengden T, Myers M, Ogedegbe G, Ohkubo T, Omboni S, Palatini P, Redon J, Ruilope LM, Shennan A, Staessen JA, vanMontfrans G, Verdecchia P, Waeber B, Wang J, Zanchetti A, Zhang Y, European Society of Hypertension Working Group on Blood Pressure M. European society of hypertension position paper on ambulatory blood pressure monitoring. J Hypertens. 2013;31:1731–68. [DOI] [PubMed] [Google Scholar]
- 16.Keku E, Rosamond W, Taylor HA Jr., Garrison R, Wyatt SB, Richard M, Jenkins B, Reeves L, Sarpong D. Cardiovascular disease event classification in the Jackson Heart Study: methods and procedures. Ethn Dis. 2005;15:S6–62-70. [PubMed] [Google Scholar]
- 17.Israel S, Israel A, Ben-Dov IZ, Bursztyn M. The morning blood pressure surge and all-cause mortality in patients referred for ambulatory blood pressure monitoring. Am J Hypertens. 2011;24:796–801. [DOI] [PubMed] [Google Scholar]
- 18.Verdecchia P, Angeli F, Mazzotta G, Garofoli M, Ramundo E, Gentile G, Ambrosio G, Reboldi G. Day-night dip and early-morning surge in blood pressure in hypertension: prognostic implications. Hypertension. 2012;60:34–42. [DOI] [PubMed] [Google Scholar]
- 19.Coccina F, Pierdomenico AM, Cuccurullo C, Vitulli P, Pizzicannella J, Cipollone F, Pierdomenico SD. Prognostic value of morning surge of blood pressure in middle-aged treated hypertensive patients. J Clin Hypertens (Greenwich). 2019;21:904–910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.White IR, Royston P, Wood AM. Multiple imputation using chained equations: Issues and guidance for practice. Stat Med. 2011;30:377–99. [DOI] [PubMed] [Google Scholar]
- 21.Sheppard JP, Hodgkinson J, Riley R, Martin U, Bayliss S, McManus RJ. Prognostic significance of the morning blood pressure surge in clinical practice: a systematic review. Am J Hypertens. 2015;28:30–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Iqbal P, Stevenson L. Cardiovascular outcomes in patients with normal and abnormal 24-hour ambulatory blood pressure monitoring. Int J Hypertens. 2010;2011:786912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, Chiuve SE, Cushman M, Delling FN, Deo R, de Ferranti SD, Ferguson JF, Fornage M, Gillespie C, Isasi CR, Jimenez MC, Jordan LC, Judd SE, Lackland D, Lichtman JH, Lisabeth L, Liu S, Longenecker CT, Lutsey PL, Mackey JS, Matchar DB, Matsushita K, Mussolino ME, Nasir K, O’Flaherty M, Palaniappan LP, Pandey A, Pandey DK, Reeves MJ, Ritchey MD, Rodriguez CJ, Roth GA, Rosamond WD, Sampson UKA, Satou GM, Shah SH, Spartano NL, Tirschwell DL, Tsao CW, Voeks JH, Willey JZ, Wilkins JT, Wu JH, Alger HM, Wong SS, Muntner P, American Heart Association Council on E, Prevention Statistics C, Stroke Statistics S. Heart Disease and Stroke Statistics-2018 Update: A Report From the American Heart Association. Circulation. 2018;137:e67–e492. [DOI] [PubMed] [Google Scholar]
- 24.Diaz KM, Veerabhadrappa P, Brown MD, Whited MC, Dubbert PM, Hickson DA. Prevalence, Determinants, and Clinical Significance of Masked Hypertension in a Population-Based Sample of African Americans: The Jackson Heart Study. Am J Hypertens. 2015;28:900–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wizner B, Dechering DG, Thijs L, Atkins N, Fagard R, O’Brien E, de Leeuw PW, Parati G, Palatini P, Clement D, Grodzicki T, Kario K, Staessen JA. Short-term and long-term repeatability of the morning blood pressure in older patients with isolated systolic hypertension. J Hypertens. 2008;26:1328–35. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


