Abstract
Objective:
The objective was to develop a disability-based metric for motor vehicle crash (MVC) upper and lower extremity injuries and compare functional outcomes between children and adults.
Methods:
Disability risk (DR) was quantified using Functional Independence Measure (FIM) scores within the National Trauma Data Bank–Research Data System for the top 95% most frequently occurring Abbreviated Injury Scale (AIS) 3 extremity injuries (22 unique injuries). Pediatric (7–18 years), young adult (19–45 years), middle-aged (46–65 years), and older adult (66+ years) MVC occupants with an FIM score and at least one of the 22 extremity injuries were included. DR was calculated for each injury as the proportion of occupants who were disabled of those sustaining the injury. A maximum AIS-adjusted disability risk (DRMAIS) was also calculated for each injury, excluding occupants with AIS 4+ co-injuries.
Results:
Locomotion impairment was the most frequent disability type across all ages. DR and DRMAIS of the extremity injuries ranged from 0.06 to 1.00 (6%–100% disability risk). Disability risk increased with age, with DRMAIS increasing from 25.9% ± 8.6% (mean ± SD) in pediatric subjects to 30.4% ± 6.3% in young adults, 39.5% ± 6.6% in middle-aged adults, and 60.5 ± 13.3% in older adults. DRMAIS for upper extremity fractures differed significantly between age groups, with higher disability in older adults, followed by middle-aged adults. DRMAIS for pelvis, hip, shaft, knee, and other lower extremity fractures differed significantly between age groups, with older adult DRMAIS being significantly higher for each fracture type. DRMAIS for hip and lower extremity shaft fractures was also significantly higher in middle-aged occupants compared to pediatric and young adult occupants. The maximum AIS-adjusted mortality risk (MRMAIS, proportion of fatalities among occupants sustaining an MAIS 3 injury) was not correlated with DRMAIS for extremity injuries in pediatric, young adult, middle-aged, and older adult occupants (all R2 < 0.01). Disability associated with each extremity injury was higher than mortality risk.
Conclusions:
Older adults had significantly greater disability for MVC extremity injuries. Lower disability rates in children may stem from their increased physiological capacity for bone healing and relative lack of bone disease. The disability metrics developed can supplement AIS and other severity-based metrics by accounting for the age-specific functional implications of MVC extremity injuries.
Keywords: Upper extremity, lower extremity, disability, children, older adults, fracture
Introduction
Motor vehicle crashes (MVCs) remain a leading cause of death and disability across the age spectrum. Mortality and disability risk of a given injury can vary based on occupant age (Weaver et al. 2013; Doud et al. 2015; Schoell et al. 2016; Doud et al. 2017; Schoell et al. 2018). Though mortality among pediatric patients is typically lower than that among adults, nonfatal injuries cause varying levels of short-and long-term disability (Schoell et al. 2016, 2018). Pediatric disability can range from 0% to 43% for MVC injuries (Doud et al. 2017), which is critical given the potential loss of quality life years if permanent disability presents during childhood.
Reporting disability in children is challenging depending on their age and ability to answer questions (Willis et al. 2006). The Abbreviated Injury Scale (AIS) was developed to determine injury survivability, not quality of life, but is currently used to infer the latter (Read et al. 2004). Functional Independence Measure (FIM) scores can be a beneficial supplement to AIS in quantifying disability associated with injuries (Schoell et al. 2016, 2018).
Pediatric bone physiology is quite different from that of adults, allowing for greater capacity to heal (Ho-Fung et al. 2017). Adults, particularly older adults, have greater mortality, morbidity, and comorbidity after extremity injuries (MacKenzie and Bosse 2006; Herron et al. 2017). Thus, disability after injury to the extremities likely varies with age, and quantifying this disability has implications for improving treatment and quality of life. This study’s objective was to develop a disability-based metric for upper and lower extremity injuries and to compare functional outcomes between children, young adults, middle-aged adults, and older adults.
Methods
Extremity injuries
The top 95% most frequently occurring AIS 3 upper and lower extremity injuries resulting from MVCs were identified using NASS-CDS years 2000–2011. These years were used for a larger study examining the mortality, time sensitivity, predictability, and disability due to MVC injuries in children and adults (Doud et al. 2015, 2017; Stitzel et al. 2016). NASS-CDS contains a representative, random sample of thousands of minor to fatal tow-away crashes in the United States. Unlike prior studies (Schoell et al. 2016, 2018), AIS 3 extremity injuries were the focus because AIS 1–2 injuries are less likely to have diminished functional outcomes, and AIS 4–6 injuries were not among the top 95% most common extremity injuries in NASS-CDS. We were interested in disability rates for frequent extremity injuries; thus, both disabling and nondisabling injuries resulting from MVCs were assessed and we focused on the most frequent AIS 3 extremity injuries to obtain adequate sample sizes.
MVC occupants were stratified into 4 age groups: Pediatric (7–18 years), young adult (19–45 years), middle-aged adult (46–65 years), and older adult (66+ years). The pediatric group encompasses the full age range in which FIM scores are validated (Winthrop et al. 2005). Sixty-five years is a common threshold for defining older adults. The age range 19–65 years was divided relatively equally to define young and middle-aged adult groups. The top 95% most frequent AIS 3 extremity injuries for each of these age groups consisted of 22 injuries (unique AIS codes; see Table A1, online supplement).
Disability risk
To quantify disability risk associated with MVC extremity injuries, the National Trauma Data Bank–Research Data Set (NTDB-RDS) was used. NTDB-RDS is the most complete database of discharged trauma patients in the United States. MVC cases were selected from NTDB-RDS (v.7.1; 2008) based on International Classification of Diseases, Ninth Revision (ICD-9) external cause of injury codes 810–819 with 0 or 1 postdots. A mapping approach was utilized to map each ICD-9 injury code to a corresponding AIS code (Barnard et al. 2013). Disability was classified with the FIM instrument, which provides a uniform measurement of disability based on the International Classification of Impairment, Disabilities, and Handicaps (Uniform Data System for Medical Rehabilitation 2014). This instrument typically contains 18 items (13 motor; 5 cognitive) with scores from 1 to 7. The FIM score is designed to be reassessed as progress is made and the score translates to the number of hours required to assist with personal care living (Uniform Data System for Medical Rehabilitation 2014). NTDB-RDS contains an abridged FIM version with 3 items (self-feed; locomotion; verbal expression) graded from 1 (full functional dependence) to 4 (full functional independence) at the time of patient discharge. FIM is validated for children ≥7 years (Winthrop et al. 2005) and is reliable across raters, settings, and patients (Ottenbacher et al. 1996). Utilizing the FIM scale within NTDB-RDS, each occupant in the pediatric, young adult, middle-aged, and older adult groups was classified as disabled or not disabled. An FIM score of 1 or 2 (full functional/modified dependence) on any of the 3 items (self-feed; locomotion; verbal expression) classified occupants as disabled.
For each of the top 95% most frequent AIS 3 extremity injuries, disability risk (DR) was calculated using Eq. (1).
| (1) |
To account for the impact of more severe associated co-injuries, a Maximum AIS (MAIS)-adjusted DR (DRMAIS) was also calculated for each injury where occupants with more severe co-injuries (AIS 4+) were excluded (Eq. (2)). In addition, MAIS-adjusted mortality risk (MRMAIS) reported for these injuries and age groups in prior studies was compared to DRMAIS to assess the mortality impact of an injury (Weaver et al. 2013; Doud et al. 2015).
| (2) |
The DR and DRMAIS could range from 0 to 1 (0%–100% disability risk). Linear regression was used to compare disability risk between age groups and with mortality risk. One-way analysis of variance and pairwise comparisons (Student’s t tests) were used to examine group differences in disability risk between age groups, body regions (upper versus lower extremity), and fracture locations (e.g., upper extremity, pelvis, hip, shaft, knee) with α = .05. Statistical analyses were performed using IBM SPSS v.25 (IBM Corp., Armonk, NY) and JMP Pro 13.0 (SAS Institute, Cary, NC).
Results
Disability risk
MVC occupants who were alive at discharge, 7 years of age and older, possessing an AIS-coded extremity injury included 37,707 pediatric, 94,405 young adult, 83,616 middle-aged adult, and 25,439 older adult occupants. FIM scores were available for 54.4% of these occupants (n = 131,042), including 20,006 (15.3%) pediatric, 51,248 (39.1%) young adult, 45,777 (34.9%) middle-aged adult, and 14,011 (10.7%) older adult occupants. Classifying extremity disability through the FIM scores found that 17.6% of pediatric (n = 3,531), 17.8% of young adult (n = 9,108), 23.2% of middle-aged adult (n = 10,635), and 38.1% of older adult (n = 5,335) occupants were disabled.
Focusing on the 22 AIS 3 extremity injuries on the top 95% list, the samples of MVC occupants who were alive at discharge and 7 years of age and older included 14,988 pediatric, 40,700 young adult, 38,163 middle-aged adult, and 10,400 older adult occupants. FIM scores were available for over half of the occupants in each of the age groups, leaving a total sample size of 56,706 for analyses (pediatric: 7,996[14.1%], young adult: 22,352 [39.4%], middle-aged adult: 20,748 [36.6%], older adult: 5,610 [9.9%]). Classifying disability through the FIM scores revealed that 33.1% of pediatric (n = 2,643), 33.4% of young adult (n = 7,475), 43.8% of middle-aged adult (n = 9,079), and 60.3% of older adult (n = 3,383) occupants were disabled. Thus, the 22 injuries that are the focus of this article comprised 78.9% of all disabled occupants with extremity injuries (pediatric: 74.9%, young adult: 82.1%, middle-aged adult: 85.4%, and older adult: 63.4%).
The most frequent type of disability (FIM component) for each age group was locomotion impairment alone (see Table A2, online supplement). Locomotion impairment was still the most common disability when stratifying each age group by upper versus lower extremity injury. The second most frequent disability for upper and lower extremity injuries was a combination of locomotion and self-feeding disability among middle-aged and older adults and a combination of all 3 disabilities (locomotion; self-feeding; verbal expression) in the pediatric and young adult groups.
Adjusted disability risk (DRMAIS)
After excluding occupants with AIS 4+ injuries, 11,417 pediatric, 30,890 young adult, 28,336 middle-aged adult, and 7,554 older adult occupants were included in the DRMAIS calculation. FIM scores were available for over half of the occupants in each age group (pediatric: 6,093 [14.3%], young adult: 17,007 [39.8%], middle-aged: 15,504 [36.3%], and older adult: 4,088 [9.6%]). Classification of disability using FIM scores revealed that 25.6% of pediatric (n = 1,561), 27.5% of young adult (n = 4,683), 38.4% of middle-aged adult (n = 5,953), and 55.4% of older adult (n = 2,263) occupants were disabled.
The most frequent type of disability for each age group was locomotion impairment alone followed by a combination of self-feeding and locomotion impairment (see Table A3, online supplement). Locomotion impairment was still the most common disability when stratifying each age group by upper versus lower extremity injury. The second most frequent disability for upper extremity or lower extremity injury across the age groups was the combination of self-feeding and locomotion impairment, except in the pediatric upper extremity injury group, where the second most common disability was solely self-feeding impairment.
DR and DRMAIS by age
DR and DRMAIS for AIS 3 extremity injuries ranged from0.06 to 1.00 (6%–100%). The mean and standard deviation DR and DRMAIS values with interquartile ranges (IQRs) for the AIS 3 extremity injuries on the top 95% lists for each age group are reported in Table 1. DR and DRMAIS increased with age.
Table 1.
Sample size, mean, standard deviation, and median DR and MAIS-adjusted disability risk (DRMAIS) with IQRs for top 95% AIS 3 extremity injuries in each age group.
| DR (%) | DRMAIS (%) | |||||
|---|---|---|---|---|---|---|
| Age group | N | Mean ± SD | IQR | N | Mean ± SD | IQR |
| Pediatric, 7–18 years | 7,996 | 32.9 ± 9.8 | 28.7–39.6 | 6,093 | 25.9 ± 8.6 | 20.5–30.7 |
| Young adult, 19–45 years | 22,352 | 35.9 ± 6.3 | 30.9–38.9 | 17,007 | 30.4 ± 6.3 | 26.0–33.9 |
| Middle-aged, 46–65 years | 20,748 | 45.0 ± 6.5 | 39.6–47.7 | 15,504 | 39.5 ± 6.6 | 34.3–43.6 |
| Older adult, 66+ years | 5,610 | 64.9 ± 12.2 | 59.7–70.3 | 4,088 | 60.5 ± 13.1 | 53.8–65.8 |
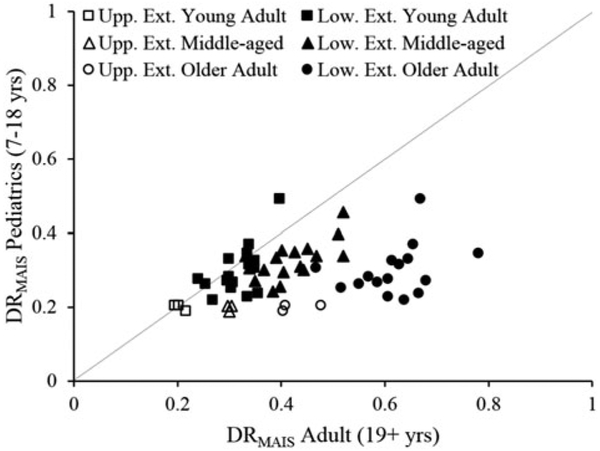
Overall, DRMAIS of the pediatric population was moderately correlated with DRMAIS of young (R2 0.52), middl-eaged (R2 = 0.52), and older (R2 = 0.24) adults. In general, DRMAIS was lower in the pediatric population compared to adults as indicated by most injuries falling below the equivalency line in Figure 1.
Figure 1.
DRMAIS for AIS 3 extremity injuries for pediatric versus adult occupants. DRMAIS for each injury in the pediatric group is plotted against the DRMAIS of that injury for the young adult, middle-aged, and older adult age groups. The equivalency line is plotted as a dashed line.
DRMAIS by age and body region
Subanalyses were performed with DRMAIS because it better describes disability by excluding interference of occupants with more severe injuries in other body regions. Disability risk across each age group was evaluated for upper and lower extremity fractures, excluding amputation, crush, and ligament injuries (AIS711000.3; 713000.3; 840406.3).
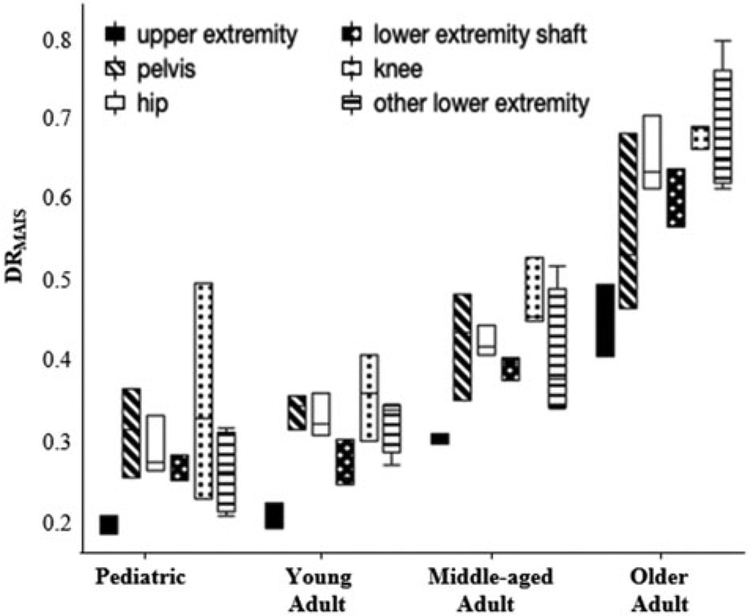
DRMAIS for upper extremity fractures (humerus, radius, ulna) differed between age groups (P < .001), with higher disability in older adults, followed by middle-aged adults (Figure 2). Pair-wise comparisons revealed differences in upper extremity fracture DRMAIS between all age groups (P≤ .002), except for the pediatric versus young adult comparison.
Figure 2.
DRMAIS by age group for upper extremity, pelvis, hip, lower extremity shaft, knee, and other lower extremity fractures. Disability is greatest for older adults and lowest for pediatric patients.
DRMAIS for pelvis, hip (femoral head, neck, intertrochanteric), lower extremity shaft (femur, subtrochanteric, tibia), knee (condylar and supracondylar femur and tibia), and other lower extremity fractures (malleolar and other lower extremity not further specified femur, tibia, and fibula fractures) differed between age groups (all P < .011; Figure 2). Pair-wise comparisons for pelvis, hip, shaft, knee, and other lower extremity fractures revealed that older adult DRMAIS was higher for these lower extremity fracture types, when compared to each of the younger age groups (all P < .047). Hip and lower extremity shaft fracture DRMAIS were also higher in middle-aged occupants compared to pediatric and young adult occupants (P < .011), and DRMAIS for other lower extremity fractures was higher in middle-aged occupants compared to pediatric occupants (P = .010). The remaining pair-wise comparisons were not statistically significant.
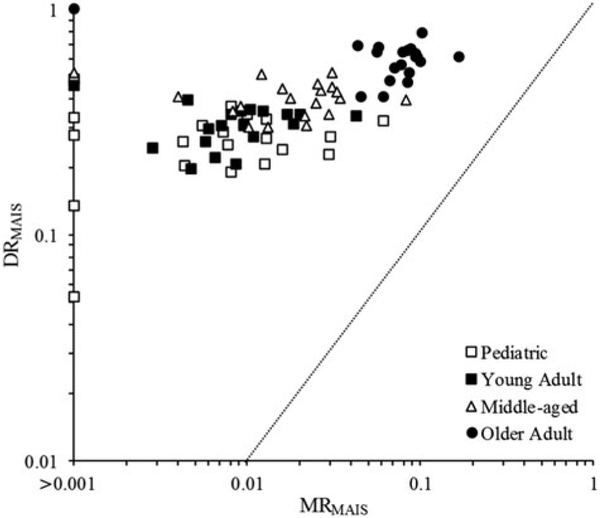
DRMAIS correlation with MRMAIS
The relationship between DRMAIS and MRMAIS was examined for extremity injuries in pediatric and adult occupants (Figure 3); MRMAIS metrics are fully described elsewhere (Weaver et al. 2013; Doud et al. 2015). All extremity injuries in the pediatric population had an MRMAIS <6.5%, with DRMAIS ranging from 6% to 48%. All extremity injuries in adults had an MRMAIS < 10%, except for femur fractures not further specified (MRMAIS = 17%); DRMAIS for adults overall ranged from 19% to 100%. Older adults generally had higher associated mortality and disability for these extremity injuries, with MRMAIS ranging from 0% to 17% and DRMAIS ranging from 39% to 100%. DRMAIS for extremity injuries was not correlated with MRMAIS in pediatric, young adult, middle-aged, and older adult occupants (all R2 ≤ 0.01).
Figure 3.
MAIS-adjusted disability risk (DRMAIS) versus MAIS-adjusted mortality risk (MRMAIS) for the top 95% AIS 3 extremity injuries by age group. The equivalency line is plotted as a dashed line.
Discussion
MVC-induced extremity injuries can result in varying levels of mortality and morbidity. Combining mortality and AIS severity information with disability and functional outcomes allows for better characterization of the severity of injuries, especially if they have low mortality rates. In this study, a disability metric—DR and DRMAIS—was quantified for the 22 most common AIS 3 MVC-induced extremity injuries across the pediatric, young adult, middle-aged, and older adult populations using FIM scores from the NTDB-RDS.
Disability risk increased with age, with older adults having a greater DR and DRMAIS than the pediatric, young adult, and middle-aged groups. Further analysis of disability and comparison of functional outcomes across the groups was conducted using DRMAIS because it is a better estimate of disability of an individual injury by excluding AIS 4+ co-injuries.
DRMAIS and MRMAIS were compared to observe differences in disability and mortality across the pediatric and adult populations. Both pediatric and adult populations revealed wide variability in disability for extremity injuries with an overall low mortality. DRMAIS for upper extremity, pelvis, hip, lower extremity shaft, knee, and other lower extremity fractures was higher in older adults. Other studies support these findings of adults, and particularly older adults, having greater morbidity and comorbidity following orthopedic trauma (MacKenzie and Bosse 2006; Herron et al. 2017). Older adults have increasing risk of fracture secondary to osteoporosis; notably, hip fractures increase mortality in older adults (Zanker and Duque 2018). In addition, aging-related muscle loss and sarcopenia increase the risk of injury and decrease the ability to recover. This deficit is compounded given that increased immobility leads to a loss of muscle mass and increased risk of injury. Compared to the pediatric to middle-aged populations, older adults’ rehabilitation and functionality are more likely to be affected because of their decreased physiologic reserve (Suetta et al. 2009). One study assessing the effect of 2-week lower limb immobilization on muscle fiber function found no difference in baseline composition of muscle fibers of older versus younger adults but found decreased calcium sensitivity (force generation) after immobilization in some muscle isoforms of older adults (Hvid et al. 2011). Similarly, Suetta et al. (2009) compared older versus younger adults during 2-week immobilization followed by 4 weeks of retraining and reported comparatively reduced muscle activation in older adults after immobilization and decreased gains in muscle volume and architecture (Suetta et al. 2009). Osteoporosis and sarcopenia often present jointly (“osteosarcopenia”), and low muscle strength is associated with poorer postfracture outcomes (Zanker and Duque 2018).
Bone healing in children includes accelerated periosteal new bone formation compared to adults, as well as continued growth plate gains. In contrast to the osteopenia and osteoporosis prevalent in older adult bone physiology, pediatric bone physiology is in a state of bone mass accrual. The peak of bone mass occurs at 25–30 years of age and thereafter starts to decline (Zanker and Duque 2018). Thus, it is not surprising that pediatric occupants tended to have lower disability compared to adults, which may be due to an increased capacity for healing following orthopedic trauma (Ho-Fung et al. 2017).
The ability to accurately identify who needs further therapy holds importance across all ages. A study of rehabilitation effects in pediatric patients found that only the most severely injured were referred for therapy and that their improvement was notable; however, more pediatric patients are likely to benefit if not only the most severely injured undergo therapy (Zonfrillo et al. 2013). Pediatric patients’ disabilities can be difficult to quantify and have greater temporal implications because of their greater remaining life span. More research is needed to accurately identify those who will benefit from rehabilitation.
The functional outcomes and subsequent disability relate to the severity of the injury, but existing metrics such as AIS severity, Injury Impairment Scale (IIS), Functional Capacity Index (FCI), and the predictive form of the FCI (pFCI) do not always correlate well with disability outcomes (MacKenzie et al. 1996; Barnes and Morris 2009; Palmer et al. 2017). All of the aforementioned metrics were established for individual AIS codes using expert consensus methods. The IIS is an ordinal score ranging from 0 (no impairment) to 6 (impairment precludes any useful function) based on 6 health dimensions; however, it has not been widely adopted or validated (Barnes and Morris 2009). The FCI was developed to map the residual disability that is present 1 year postinjury based on 10 health dimensions using a 0–100 scale corresponding to no impairment to maximal impairment (MacKenzie et al. 1996). Discrimination of observed impairment following lower extremity injury was only moderately better for FCI compared to AIS or IIS. Validation data showed that the proportion of lower extremity fracture patients with 1-year postinjury impairment was 13% (FCI 0), 16% (FCI 1–20), 19% (FCI 21–40 and 41–60), and 25% (61–80). The pFCI is a predictive ordinal score ranging from 1 (maximum impairment) to 5 (no impairment) that is derived from the FCI scores, which also showed moderate ability to predict postinjury impairment in patients with lower extremity injuries (Barnes and Morris 2009). FCI and pFCI are governed by 4 assumptions: That the injured patient (1) survived, (2) is 18–34 years old with no prior comorbidities, (3) received timely and appropriate acute care and rehabilitation, and (4) sustained only one injury. These assumptions do not apply broadly to the trauma population, which includes individuals of all ages with multiple injuries whose triage and treatment pathways vary. This supports the need for a disability metric such as DRMAIS that is derived from trauma data for specific age groups, which also controls for more severe co-injuries.
A limitation is that NTDB is a convenience sample—it consists solely of data submitted by participating hospitals and it is not a population database and therefore may not be generalizable. In addition, patients who are dead upon arrival are excluded from NTDB (Barnard et al. 2013); this is therefore a possible confounder to the overall reported mortality rates. We focused on the most common AIS 3 injuries sustained in all types of MVCs in the NASS-CDS analysis, so crash characteristics were not controlled for in the selection of injuries to study and are not included in the NTDB. The use of AIS as a selection criterion may limit the ability to study disability as an independent factor, and future studies could select injuries based on the ICD coding lexicon or the most common disabling injuries. Another consideration is that FIM scores were available for only 54% of the patients identified for inclusion in the study, and the remainder of the patients were excluded because they were missing these data. Based on database content, we could assess only 22 injuries with nonuniform injury pattern distribution across the life span. In addition, occupants <7 years old were excluded, and defining different age ranges for the groups could change the study results. These limitations could introduce some bias in disability and injury distribution of the population.
Although NTDB only collects FIM at time of discharge from the hospital, this is an important time frame to understand functionality as patients re-enter society. Another limitation is that pre-injury health status, preexisting comorbidities, and need for surgical intervention were not considered. These circumstances could affect subsequent outcomes and complications and thereby disability status. For example, accurately documenting disability in situ with psychological sequalae (i.e., depression, PTSD) has been found to delay recovery (Read et al. 2004; MacKenzie and Bosse 2006). In addition, the ability of pediatric patients and, by extension, adults to rehabilitate after significant injury is impaired by concomitant brain injury and was not assessed in this study (Zonfrillo et al. 2014). It is important for future efforts to include these factors for additional study and to integrate these into comprehensive treatment and management plans in the future.
In conclusion, this study demonstrates that there are age-related differences in disability risk and outcomes following MVC extremity injury. Overall, disability risk for upper and lower extremity injuries increased with age, with older adults having significantly greater overall disability than each of the other age groups. These differences highlight the effect on risk of morbidity over human development. DR and DRMAIS can supplement AIS and other severity-based metrics by accounting for the functional implications of MVC extremity injuries. Understanding age-related differences to extremity injury outcomes could also influence future age-specific modifications to AIS and postinjury impairment metrics such as IIS and FCI.
The content reproduced from the NTDB remains the full and exclusive copyrighted property of the American College of Surgeons. The American College of Surgeons is not responsible for any claims arising from works based on the original data, text, tables, or figures.
Supplementary Material
Acknowledgments
We thank Samantha Schoell and Andrea Doud for their assistance with the data analysis. The authors acknowledge the National Science Foundation (NSF) Center for Child Injury Prevention Studies at the Children’s Hospital of Philadelphia (CHOP) Industry Advisory Board (IAB) members for their support, valuable input, and advice. The views presented are those of the authors and not necessarily the views of CHOP, the NSF, the IAB members, or the NIH.
Funding
The authors acknowledge the National Science Foundation (NSF) Center for Child Injury Prevention Studies at the Children’s Hospital of Philadelphia (CHOP) for sponsoring this study (1034593). This publication was also supported by the National Institutes of Health (NIH), Eunice Kennedy Shriver National Institute of Child Health and Human Development (K08HD073241), and National Institute on Aging (K25AG058804).
Footnotes
Supplemental data for this article can be accessed on the publisher’s website.
References
- Barnard RT, Loftis KL, Martin RS, Stitzel JD. 2013. Development of a robust mapping between AIS 2+ and ICD-9 injury codes. Accid Anal Prev. 52:133–143. [DOI] [PubMed] [Google Scholar]
- Barnes J, Morris A. 2009. A study of impairing injuries in real world crashes using the Injury Impairment Scale (IIS) and the predicted Functional Capacity Index (PFCI-AIS). Ann Adv Automot Med. 53: 195–205. [PMC free article] [PubMed] [Google Scholar]
- Doud AN, Schoell SL, Weaver AA, Talton JW, Barnard RT, Petty JK, Stitzel JD. 2017. Disability risk in pediatric motor vehicle crash occupants. J Trauma Acute Care Surg. 82(5):933–938. May [DOI] [PubMed] [Google Scholar]
- Doud AN, Weaver AA, Talton JW, Barnard RT, Schoell SL, Petty JK, Stitzel JD. 2015. Mortality risk in pediatric motor vehicle crash occupants: accounting for developmental stage and challenging abbreviated injury scale metrics. Traffic Inj Prev. 16(Sup2): S201–S208. [DOI] [PubMed] [Google Scholar]
- Herron J, Hutchinson R, Lecky F, Bouamra O, Edwards A, Woodford M, Eardley WGP. 2017. The impact of age on major orthopaedic trauma: an analysis of the United Kingdom Trauma Audit Research Network database. Bone Joint J. 99-B(12): 1677–1680. December [DOI] [PubMed] [Google Scholar]
- Ho-Fung VM, Zapala MA, Lee EY. 2017. Musculoskeletal traumatic injuries in children: characteristic imaging findings and mimickers. Radiol Clin North Am. 55(4):785–802. [DOI] [PubMed] [Google Scholar]
- Hvid LG, Ortenblad N, Aagaard P, Kjaer M, Suetta C. 2011. Effects of ageing on single muscle fibre contractile function following short-term immobilisation. J Physiol. 589(19):4745–4757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKenzie EJ, Bosse MJ. 2006. Factors influencing outcome following limb-threatening lower limb trauma: lessons learned from the Lower Extremity Assessment Project (LEAP). J Am Acad Orthop Surg. 14(Suppl):S205–S210. [DOI] [PubMed] [Google Scholar]
- MacKenzie EJ, Damiano A, Miller T, Luchter S. 1996. The development of the Functional Capacity Index. J Trauma. 41(5):799–807. [DOI] [PubMed] [Google Scholar]
- Ottenbacher KJ, Hsu Y, Granger CV, Fiedler RC. 1996. The reliability of the functional independence measure: a quantitative review. Arch Phys Med Rehabil. 77(12):1226–1232. [DOI] [PubMed] [Google Scholar]
- Palmer CS, Cameron PA, Gabbe BJ. 2017. A review of the revised Functional Capacity Index as a predictor of 12 month outcomes following injury. Injury. 48(3):591–598. [DOI] [PubMed] [Google Scholar]
- Read KM, Kufera JA, Dischinger PC, Kerns TJ, Ho SM, Burgess AR, Burch CA. 2004. Life-altering outcomes after lower extremity injury sustained in motor vehicle crashes. J Trauma. 57(4): 815–823. [DOI] [PubMed] [Google Scholar]
- Schoell SL, Weaver AA, Talton JW, Baker G, Doud AN, Barnard RT, Stitzel JD, Zonfrillo MR. 2016. Functional outcomes of motor vehicle crash head injuries in pediatric and adult occupants. Traffic Inj Prev. 17(sup1):27–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schoell SL, Weaver AA, Talton JW, Barnard RT, Baker G, Stitzel JD, Zonfrillo MR. 2018. Functional outcomes of motor vehicle crash thoracic injuries in pediatric and adult occupants. Traffic Inj Prev. 19(3):280–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stitzel JD, Weaver AA, Talton JW, Barnard RT, Schoell SL, Doud AN, Martin RS, Meredith JW. 2016. An injury severity-, time sensitivity-, and predictability-based advanced automatic crash notification algorithm improves motor vehicle crash occupant triage. J Am Coll Surg. 222(6):1211–1219 e1216. [DOI] [PubMed] [Google Scholar]
- Suetta C, Hvid LG, Justesen L, Christensen U, Neergaard K, Simonsen L, Ortenblad N, Magnusson SP, Kjaer M, Aagaard P, et al. 2009. Effects of aging on human skeletal muscle after immobilization and retraining. J Appl Physiol (1985). 107(4):1172–1180. [DOI] [PubMed] [Google Scholar]
- Uniform Data System for Medical Rehabilitation. 2014. The FIM instrument: its background, structure, and usefulness. Buffalo: UDSMR. [Google Scholar]
- Weaver AA, Barnard RT, Kilgo PD, Martin RS, Stitzel JD. 2013. Mortality-based quantification of injury severity for frequently occurring motor vehicle crash injuries. Ann Adv Automot Med. 57: 235–246. [PMC free article] [PubMed] [Google Scholar]
- Willis CD, Gabbe BJ, Butt W, Cameron PA. 2006. Assessing outcomes in paediatric trauma populations. Injury. 37(12):1185–1196. [DOI] [PubMed] [Google Scholar]
- Winthrop AL, Brasel KJ, Stahovic L, Paulson J, Schneeberger B, Kuhn EM. 2005. Quality of life and functional outcome after pediatric trauma. J Trauma. 58(3):468–464. discussion 473- [DOI] [PubMed] [Google Scholar]
- Zanker J, Duque G. 2018. Osteoporosis in older persons: old and new players. J Am Geriatr Soc. 67(4):831–840. [DOI] [PubMed] [Google Scholar]
- Zonfrillo MR, Durbin DR, Winston FK, Zhang X, Stineman MG. 2014. Residual cognitive disability after completion of inpatient rehabilitation among injured children. J Pediatr. 164(1): 130–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zonfrillo MR, Durbin DR, Winston FK, Zhao H, Stineman MG. 2013. Physical disability after injury-related inpatient rehabilitation in children. Pediatrics. 131(1):e206–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.