Abstract
Purpose of review
Polluting industries are more likely to be located in low income communities of color who also experience greater social stressors that may make them more vulnerable than others to the health impacts of toxic chemical exposures. We describe recent developments in assessing pollutant exposures and health threats posed by industrial facilities using or releasing synthetic chemicals to nearby communities in the U.S.
Recent findings
More people are living near oil and gas development due to the expansion of unconventional extraction techniques as well as near industrial animal operations, both with suggestive evidence of increased exposure to hazardous pollutants and adverse health effects. Legacy contamination continues to adversely impact a new generation of residents in fenceline communities, with recent studies documenting exposures to toxic metals and poly- and perfluoroakyl substances (PFASs). Researchers are also giving consideration to acute exposures resulting from inadvertent industrial chemical releases, including those resulting from extreme weather events linked to climate change. Natural experiments of industrial closures or clean ups provide compelling evidence that exposures from industry harm the health of nearby residents.
Summary
New and legacy industries, coupled with climate change, present unique health risks to communities living near industry due to the release of toxic chemicals. Cumulative impacts from multiple stressors faced by environmental justice communities may amplify these adverse effects.
Keywords: Environmental justice, climate justice, oil and gas development, industrial pollution, natural technological disasters
Introduction
Synthetic chemical compounds have drastically transformed many human activities, such as through the production of food, consumer products and energy. As tens of thousands of new chemicals have been synthesized, highly unequal patterns of exposure to pollution waste streams has resulted with communities living on the fenceline of such industries being particularly at risk of harmful exposures [1]. The past four decades have brought to light the role of policies, land-use decisions, regulations, and market-based forces in contributing to social inequalities in residential proximity to industry and resultant exposures to harmful chemicals that disproportionately impact low-income communities of color [2].
Even as toxic exposures and associated health risks have been on the decline nationally, such reductions have been less evident in low-income communities and communities of color [3] [4]. In many cases, these fenceline industries are un- or under-regulated and the surrounding communities often have less access to resources for conducting research into the relationships between industry, environmental quality, and health conditions [5]. Facing environmental hazards, community organizations and the environmental justice movement have turned to gathering data in the face of government inaction or industry denial about chemical exposures [6]. In many cases, primary or secondary data demonstrating the presence of harmful pollutants in the environment near industry has been insufficient to prompt regulatory or policy action; rather, it has also been necessary to demonstrate people’s exposure and that exposures causes adverse health effects [6, 5]. However, linking local industrial pollution with environmental health impacts presents unique challenges. For example, while advancements in biomonitoring have enabled better estimation of human exposures to synthetic chemicals, attributing those exposures to a local industry is difficult, particularly in environmental justice communities because they often are subject to multiple sources of pollution. Epidemiological studies in fenceline communities must confront power limitations due to small sample sizes and issues of confounding, since fenceline communities are typically also low socioeconomic status and struggling with social as well as environmental stressors to health.
In this paper, we review recent environmental health literature regarding communities living in close proximity to industrial pollution sources and advancements in the field, focusing on studies in the United States (U.S.). We searched for original articles published in the last 3 years that included hazardous point sources of man-made chemicals and measured a health (or biomarker) endpoint among residents living in close proximity. For purposes of this review, our emphasis was on hazardous facilities that use or emit synthetic chemicals. Literature from the past three years fitting these criteria were review and synthesized based on commonalities and methods. We summarize recent evidence that the expansion of oil and gas extraction has resulted in chemical exposures to nearby communities that may be impacting health. Similarly, the growth industrial animal operations (e.g. hogs, dairies, poultry) has been associated with adverse health impacts in nearby, largely rural communities. We also find that legacy contaminants from other industries continue to impact a new generation due to a lack of adequate clean up. Finally, we find that accidental industrial releases are becoming of greater concern with the increase in extreme weather events due to climate change, with implications for harmful chemical exposures in nearby communities. We also review several recent studies that have used a “natural experiment” design to compellingly demonstrate the health impacts of industry on fenceline communities, overcoming some of the challenges in quantifying the health impacts of exposures related to local industry.
Oil and Gas Extraction
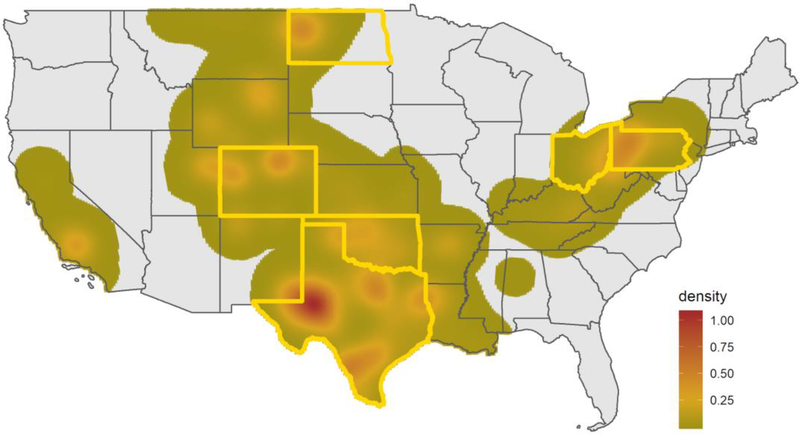
Extraction of petroleum has been a longstanding concern in communities. Recently, the U.S. has seen a rapid proliferation of oil and natural gas (ONG) extraction activity, sparking research into the potential health impacts [7] [8]. Over the past decade, oil production has nearly doubled while natural gas production rose 50% reversing a longstanding decline in production [9]. This has been made possible, in part, by advancements in high volume hydraulic fracturing techniques (“fracking”) that involve the injection of fluids, sands and chemical additives into wells to reduce friction, decrease drill time or stimulate production [10]. Chemicals used in fracking include carcinogens, mutagens, reproductive and developmental toxins, and endocrine disruptors, and these compounds can enter the nearby environment through spills, leaks, volatilization and disposal of wastewater, but in general are poorly characterized in terms of transport through and persistence in the environment [11] [12]. A review of unconventional oil and gas spills, identified 6600 spills in 4 states from 2005–2014, with wastewater, crude oil, drilling waste, and hydraulic fracturing fluid as the materials most frequently spilled [13]. An estimated 17.4 million people that live near (<1600 m) an active oil or gas extraction site [14], the majority of whom are in rural communities (Figure 1). This presents unique challenges to environmental health research on oil and gas extraction as baseline environmental monitoring data is often not available in rural areas, and small population sizes limit the statistical power of epidemiologic studies. At the same time, rural communities are more likely to be reliant on unregulated groundwater sources - and thus more vulnerable to chemical contamination of drinking water associated with underground drilling and wastewater injection. One recent community-based study in Ohio found that living near wells was associated with higher detection rates and concentrations of drinking water contaminants coupled with more reported health symptoms [15].
Figure 1.
Density of productive oil and gas wells completed between January 1, 2005 and December 31, 2018 in the continental U.S., with states in which recent health studies have been conducted highlighted. Data source: DrillingInfo
In addition to potential new pathways of exposure to toxic chemicals, populations living in regions with oil and gas development may experience increased exposure to traffic and construction-related pollution, noise, crime, psychosocial stress, as well as community disruption from the rapid influx of workers resulting in cumulative impacts [16]. For example, drilling has been associated with increase truck traffic and noise [17] that likely contributes to sleep disturbance, annoyance, and increased stress for those living nearby [18] [19]. New approaches are being used to better characterize changes to environmental quality near ONG operations. Community monitoring networks, leveraging low-cost monitors offer new opportunities to assess local air quality near active oil and gas operations [20]. Such real-time monitoring can provide long-term data and capture episodic peaks commonly associated with ONG development [21]. Researchers have also leveraged satellite data to characterize flaring, or the combustion of petroleum products into the open atmosphere, in regions with oil and gas development, demonstrating that this largely unreported activity may be an important health concern for nearby residents [22]. Personal exposure monitoring, using silicon passive samplers in a community-driven study, found significantly higher levels of polycyclic aromatic hydrocarbons (PAHs) among residents near active natural gas sites in rural Ohio compared to those living farther away [23].
The first publications regarding body burden of chemicals among women near unconventional ONG sites showed higher levels of urinary biomarkers of benzene as well as manganese, barium, aluminum and strontium among pregnant women living near ONG sites as compared to the general Canadian population [24] [25]. Median levels of contaminants were generally higher among the indigenous when compared with the non-indigenous participants.
To date, researchers have largely relied on assessing health impacts near oil and gas development, such as birth outcomes or hospitalization, using secondary data. Earlier research has leveraged administrative birth records to assess the associations between proximity to extraction sites and adverse birth outcomes, such as pre-term birth and low birth weight [26] [27] [28] [29]. While the results are not consistent across all studies, there is suggestive evidence of an association with increased risk of pre-term birth in the most highly drilled regions. In other cases, the effects of natural gas drilling on low birth weight were found to be larger among children living in neighborhoods of lower socioeconomic status [26]. Studies in rural Oklahoma and Colorado found an increased prevalence of neural tube defects among infants born to mother living near drilling [30] [28]. Hospitalizations, which reflect acute illness or serious exacerbations of chronic disease, have been used to assess potential health effects at a population scale. Elevated incidence of hospitalization among residents in non-urban counties in Pennsylvania (PA) with respect to higher intensity of drilling activity has been observed for pediatric asthma [31] and for genitourinary problems of non-elderly adult women [32]. New efforts to examine the relationship between natural gas development and mental health of residents using a mailed Patient Health Questionnaire-8 and electronic health records has found an association between depression symptoms in adults living near the highest level of drilling activity in northeastern PA [33].
Small studies are underway to collect physiological measurements in communities living near ONG operations. In CO, measurements of augmentation index, systolic and diastolic blood pressure, and plasma concentrations of interleukin (IL)-1β, IL-6, IL-8 and tumor necrosis factor alpha (TNF-α) was collected among 97 adult participants. Researchers found preliminary evidence of adverse cardiovascular impacts, including higher augmentation index and blood pressure, among adults near the most drilling activity in this cross-sectional community study [34]. In most cases, however, studies have not yet sought to identify the biological mechanisms by which emissions from ONG lead to the observed elevation in adverse health effects.
The rapid expansion of ONG development coupled with the rurality of most populations that are affected are challenges to fully measure the impacts on population health and understand the ONG-related exposure pathways and biological mechanisms of greatest importance. Oil and gas drilling are often comprised of multiple small-scale operators and dispersed across a region. The distributions and types of rural pollution are typically not well characterized, nor are the population-level health characteristics in these regions [35]. Despite these challenges, ONG development remains an active and important area of research, particularly as early studies have demonstrated evidence of harmful exposures and health impacts. The need for additional research is also underscored by the fact that the populations impacted by ONG development may also experience rural, economic, participatory, and/or distributive injustices that result in greater vulnerability to risks associated with the environmental and health consequences [36].
Industrial Animal Production
The rise of industrial-scale agriculture in the U.S. has led to the release of numerous biological and chemical pollutants that threaten environmental quality and public health [37–40]. These operations are usually sited in rural areas has been a long-standing concerns of neighbors who report health problems related to airborne emissions, odors, open waste pits and spray fields [41, 42]. In North Carolina, industrial hog facilities are disproportionately permitted near communities of color [43] and a recent analysis of disease-specific mortality data concluded that communities located near industrial hog facilities had higher all-cause and infant mortality, mortality due to anemia, kidney disease, tuberculosis, and septicemia [44]. Recent studies have added to a growing body of literature in the U.S. on acute and chronic respiratory health effects among residents living near industrial animal operations. Among rural adults in Wisconsin, decreased lung function and increased prevalence of asthma and allegories was higher among residents living near (<3 miles) from an industrial animal operations compared to those living far (> 5 miles) [45]. Asthmatic residents living within 3 miles of a hog, dairy or veal operation in Pennsylvania had an increased risk of exacerbations, as measured by oral corticosteroid medication orders and asthma hospitalizations, compared to those living farther away [46]. A similar finding was observed among predominantly Hispanic asthmatic children living near dairies and exposed to outdoor ammonia pollution associated with industrial dairy operations in Washington state [47]. Researchers observed that residing closer to more and larger poultry operations was associated with community acquired pneumonia, the first study of its kind in the US [48]. The epidemiological literature is increasingly addressing more types of industrial animal operations like dairies and poultry, building upon decades of research near industrial hog operations. While the majority of studies utilize cross-sectional designs, a few are beginning to integrate prospective longitudinal studies designs along with source-tracking of pollution source, that may better help establishing causality [47, 38, 49].
Legacy Industrial Pollution
Health disparities related to proximity to industrial corridors across the U.S. that are home to existing and legacy chemical manufacturing and metal plating, finishing, or recycling industries continue to be a source of community concerns and research interest. The economic landscape in these neighborhoods often involves a symbiotic relationship with industry, yet limited access to health care facilities, lack of green space and government divestment [50]. Metalworking facilities are associated with elevated releases of lead (Pb), arsenic (As), cadmium (Cd), manganese (Mn), hexavalent chromium (Cr6) and other toxicants [51]. Elevated road dust concentrations of Mn and Pb were identified around a steel facility at levels of concern for human health. The research demonstrates that metal pollution is still pervasive in road sediment and parks, even though the amount of industrial productivity at the facility has rapidly declined over time [52, 53]. Proximity to a legacy smelting facility together with soil lead levels was associated with higher blood lead levels in children in a majority people of color town in Colorado [54]. Using a community-driven approach, early life exposures to lead were estimated using teeth biomarkers among Latinx children living the whole lives near a secondary lead-acid battery smelter [55]. The results demonstrate an approach to measure exposure retrospectively and suggest that prenatal and early life exposure to toxic metals is associated with legacy soil contamination in an urban community near a smelter. Further there is evidence that environmental injustice is vertically transmitted from mothers to their unborn children, and that this burden is disproportionately borne by disadvantaged communities. This community-academic collaboration worked to increase awareness and support local community power to transform the debate on battery smelter facilities and legacy lead contamination across the state of California [56]. This included extensive soil remediation and a new state fund dedicated to the removal of lead-contaminated soil for communities where lead smelters have operated.[57] In another community-based participatory research study, the relationship between manganese exposure, largely attributed to a hazardous waste incinerator, and child cognition was assessed using biomarkers. Increasing hair manganese concentration was significantly and inversely associated with child cognition [58].
Poly- and perfluoroalkyl substances (PFASs) have emerged as another chemical class of major concern for communities living near manufacturers or industrial end-users. These fluorinated organic compounds have potential multi-generational impacts due to the widespread use of these anthropogenic chemicals in industrial processes and commercial products, their long persistence in the environment, high detection frequencies in human biomonitoring studies, and the evidence of developmental, immune, metabolic, and endocrine disruption in human and animal studies [59]. Although the manufacturing of certain PFASs has been phased out, there remain concerns regarding the production of closely related congeners, and numerous known and unknown PFASs continue to be introduced to the marketplace [60]. Much of what we know about the health impacts of PFASs stem from epidemiological studies conducted in a highly exposed community near the Parkersburg, West Virginia Washington Works Teflon manufacturing plant, which contaminated local drinking water supplies [61]. These studies found evidence linking PFAS exposure to testicular and kidney cancer, thyroid disease, ulcerative colitis, high cholesterol, and pregnancy-induced hypertension [62]. Few studies have been conducted in other fenceline communities in the U.S. Elevated levels of PFAS in serum and urine samples from residents were also found near a PFAS manufacturing site that discharged wastewater into a drinking water source in Alabama [63]. The number of industrial sites that manufacture PFASs, military fire training areas, and wastewater treatment plants were found to all be significant predictors PFAS concentrations in U.S. drinking water, suggesting elevated exposure among populations living near these sites [64].
Natural and technological disasters
While earlier environmental justice scholarship built a robust evidence base for social inequalities in chronic exposures related to the citing of industrial and other hazardous land uses, a growing body of work has also considered more acute exposures associated with accidental releases at industrial sites. For example, Remy et al. (2019) compared emergency department visits and hospital admissions during the 4 weeks after and 4 weeks prior to two major chemical release events at the Chevron refinery in Richmond, California. The larger of these events, occurring in 2012, resulted in a 3.7-fold increase in the number of people seeking care at emergency departments from zip codes closest to the refinery, with the visits for numerous sensory/nervous system conditions (migraine headaches, eye conditions, and dizziness), asthma, upper and lower respiratory conditions, chest pain, and non-medical related poisonings being elevated [65]. The most impacted zip codes closer to the refinery had a much higher proportion of residents of color than those farther away (76% vs. 45%). Court-ordered examinations of randomly-selected plaintiffs who sued Chevron after the smaller 2007 chemical release showed that half of patients had new or worsened chronic respiratory conditions five years after that event, suggesting major accidental chemical releases from refineries can have significant long-term health impacts.
Another series of retrospective studies examined health impacts to residents near the British Petroleum refinery in Texas City, Texas following a 2010 flaring event that lasted 40 days and resulted in the release of several hundred thousand pounds of toxic chemicals including benzene. Like Richmond, Texas City is a highly industrialized city with high rates of poverty and a population that is majority people of color (primarily Hispanic and African American). Researchers found evidence of altered markers of hematological and hepatic function among residents living downwind of the refinery roughly 2–14 months after the incident, compared to unexposed patients identified from medical records living 30–40 miles away [66]. Residents downwind of the refinery also reported a range of symptoms of illness, with neurological and upper respiratory symptoms being the most common, and had urinary phenol concentrations - a marker of benzene exposure - that increased with residential proximity to the refinery [67]. Attribution of these symptoms to the chemical release is however limited since this study lacked baseline data or a comparison population.
Increasing attention is also being given to so-called “natural technological” or “cascading” disasters in which natural disasters result in technological malfunctions or failures, releasing hazardous materials [68]. This line of research suggests communities living near industrial sites may be increasingly subject to harmful unintentional chemical releases because of extreme weather events associated with climate change (Table 1). For example, during Hurricane Harvey in 2017, 46 industrial sites released a reported 4.6 million pounds of excess emissions during pre-emptive shutdowns, startups, leaks, or explosions [69], and multiple Superfund sites remained underwater for days [70]. Based on pre-hurricane household dust and post-hurricane soil samples from 25 homes in the Manchester neighborhood of Houston, Texas - which hosts 21 facilities that report to the Environmental Protection Agency’s Toxic Release Inventory within a one-mile radius - Horney et al. (2018) concluded that floodwaters likely geographically re-distributed polycyclic aromatic hydrocarbons (PAHs) originating from combustion sources [71]. Flooding events are also likely to result in chemical releases from active and legacy industrial sites. For example, concentrations of heavy metals in stream water from the Greater Houston Area after Hurricane Harvey were higher than pre-storm samples despite greater dilution due to the flooding, and associated with the presence of industrialized areas [72]. Analysis of lake sediment samples before and after Hurricane Florence in 2018 revealed significantly elevated coal ash contaminants in lake sediments adjacent to coal ash storage sites in North Carolina that mobilized into the lake ecological system [73]. Finally, in the only study we are aware of to assess hazardous chemical releases in the aftermath of Hurricane Maria, Subramanian and colleagues found elevated ambient concentrations of sulfur dioxide, carbon monoxide, and black carbon concentrations in San Juan, Puerto Rico’s air due to the widespread reliance on generators for electricity [74].
Table 1.
Example recent extreme weather events that resulted in excess chemical contaminant releases in communities near industry.
| Storm (year) | U.S. areas affected | Partial list of industrial sites in affected areas | Reported excess chemical releases |
|---|---|---|---|
| Hurricanes Katrina and Rita (2005) | U.S. Gulf Coast | ■ 54 Superfund sites in AL, LA, MS and TX [75, 76] ■ 23 facilities reporting to the Toxic Release Inventory in New Orleans, LA [77] |
■ 10 onshore oil spills totaling 8 million gallons, including the Murphy oil spill at the Meraux Refinery (LA) that impacted approximately 1,800 homes [78] ■ 166 reported releases of hazardous substances from industry in LA and TX, primarily due to emergency shut downs and start-ups [79] |
| Hurricanes Gustav and Ike (2008) | U.S. Gulf Coast | ■ 45 Superfund sites in LA and TX [80] | ■ Elevated arsenic concentrations in soils, possibly originating from decommissioned industrial sites in Galveston, TX [81] |
| Hurricane / Superstorm Sandy (2012) | 24 U.S. states in the Southeast, Mid-Atlantic, Midwest, and New England | ■ 247 Superfund sites in NY and NJ [82] | ■ 3 spills totaling 400,000 gallons of biodiesel, oil, and diesel from refineries along the Arthur Kill in NJ [83] |
| Hurricane Harvey(2017) | Southeast TX | ■ 13 of 41 Superfund site inundated in Houston, TX [84] | ■ Excess emissions of 4.6 million pounds of hazardous chemicals from 46 facilities across 13 counties[69] ■ Arkema chemical plant explosions require evacuation of residents in Crosby, TX [85] |
| Hurricanes Irma and Maria (2017) | U.S. Southeast, U.S. Virgin Islands, Puerto Rico | ■ 168 Superfund sites in FL, GA, AL, and SC [86] ■ 17 Superfund sites in PR [87] |
■ Elevated air pollution due to reliance on generators ■ Reliance on untested drinking water sources ■ Coal ash releases from landfill sites in Guayamas and Peñuelas, PR [88] |
| Hurricane Florence (2018) | NC, SC, GA, TN | ■ 113 Superfund sites [89] | ■ Releases of coal ash [73, 90] ■ Flooding of waste lagoons from concentrated animal feeding operations [90] |
In general, assessment of post-disaster chemical exposures is logistically challenging and hindered by the fact that baseline data is often lacking, funding is rarely immediately available, and study protocols for human subject’s data collection must typically already be in place prior to the disaster to facilitate rapid field data collection [71]. Nevertheless, climate change and the increasing number of people living near industrial sites requires environmental health scientists to consider novel pathways of exposure to hazardous chemicals due to natural technological disasters. Modelling approaches and community-based environmental monitoring efforts can also inform adaptation planning and emergency response efforts to protect health prior to disaster events by determining the areas of greatest exposure risk due to the location of industrial facilities in disaster prone areas [91, 92].
Leveraging industrial closures as natural experiments
Several recent studies have used the retirement or cleanup of industrial sites as “natural experiments” to assess the impacts on exposures and the health benefits associated with their closure. This study design provides compelling evidence of causal effects of industrial exposure on the health of nearby residents because natural experiments are arguably the best approximation of a randomized trial of environmental exposures. For example, using a difference-in-difference approach to account for secular trends in the preterm birth rate over time, Casey and colleagues were able to demonstrate that the retirement of oil and coal power plants in California was associated with a substantial reduction in the prevalence of preterm birth, with larger reductions in women living closer to the plant [93]. The effects were strongest among black women, suggesting that power plant closures may help address persistent existing health disparities. Additionally, these researchers found that fertility rates among nearby populations increased after the retirements of these same power plants [94]. Similarly, the closure of an oil refinery near Toronto, Canada resulted in a reduction in air pollutants as well as respiratory- related hospitalizations from the Oakville community closest to the refinery [95]. Cold-season respiratory hospitalizations in Oakville fell by 2.2 cases per thousand persons per year (approximately 180 total hospitalizations for the year) and the reduction in visits persisted for the subsequent 7 year after the refinery closed, a trend not seen across the larger urban area. This further suggests that closure of local industrial sites can have immediate and long-lasting health benefits for the nearby community. While limited to population-level data, recent research also suggests that mortality rates are declining as a result of remediation of legacy contamination sites related to smelter and mining activities in rural Montana that created millions of cubic meters of mine waste [96]. Although individual-level inference is limited given the ecological approach, the time trend analysis indicates that while mortality in counties with high concentrations of mine waste remains elevated compared to the state as a whole, deaths from cancer and neurological conditions decreased post remediation.
Conclusion
New and legacy industries, coupled with climate change, present unique health risks to communities living near industry as a result of exposures to toxicants. Both rural and inner city America are typically understood as sites of concentrated poverty, dumping grounds for locally unwanted land uses [97] and continue to be a focus for research on industrial exposures. Exposure to toxic pollution and stress related to fear of potential chemical or climate disasters may increase the health burden on these fenceline communities. These hazards are amplified by other negative socioeconomic and health factors, including higher rates of chronic diseases, lack of access to healthy foods, substandard housing, and stress from racism, poverty, unemployment, and crime. As extreme weather events become increasingly frequent, exposure and health disparities faced by fenceline communities are anticipated to amplify as a result of climate change. These communities not only face additional burdens due to potential toxic releases, but often do not have the social or financial resources to mitigate their exposures.
In this context, the identification of environmental hazards and human exposures in fenceline communities remains highly valuable information for self-protection, pollution prevention, and remediation, issues that are all of concern in communities facing environmental injustice. Such research can fill gaps in government data available at a local level, draw attention to disproportionate exposures to environmental hazards that were being denied by polluters or overlooked by regulators, and garner credibility for action to reduce environmental health disparities. In many cases, it is insufficient to show that pollutants exist in the environment: it may also be necessary to demonstrate people’s exposure to such pollutants and that exposure causes adverse health effects. As a result, the burden of scientific proof of environmental harm falls on affected communities, not polluters. Credible science that assesses exposure to toxic chemicals, especially in situations of a specific industrial source of pollution affecting a community, is critical for informing appropriate public health and policy responses [98].
While assessing health impacts due to chemical exposures in communities adjacent to industrial activities is challenging due to the common lack of baseline environmental monitoring and small sample size issues for epidemiologic studies, recent advancements in the literature have used innovative strategies including community-engaged research, biomonitoring, and natural experiments to help elucidate these links. Emerging technologies such as low-cost air pollution sensors, passive silicone-based samplers, and non-targeted analysis methods to detect novel chemical compounds in environmental media and human bodies hold promise for improving our understanding of exposures near industrial sources of pollution going forward. In addition, novel methodological approaches for assessing the cumulative impacts of multiple chemical exposures and social stressors to health remains a key research need to inform decision-making that improves health in environmental justice communities.
Finally, while only a few of the studies we reviewed directly involved impacted communities in the research, community engagement has been an important hallmark of much of the work in this field. Prior studies related to traffic, goods movements, refineries, and industrial agriculture illustrate how community-based participatory research approaches strengthen the scientific process and help to ensure research findings are leveraged to bring about regulatory action or policy change that protects community health [5, 99, 100]. An important component of environmental justice research going forward should therefore be the continued emphasis on involving community members in identifying environmental health concerns in need of investigation, collaborating with scientists in the conduct of the research, and translating research findings into action, including advocacy for policy change.
Acknowledgements
The authors thank Khang Chau at the University of Southern California for assistance in creating Figure 1.
Compliance with Ethics Guidelines
Conflict of Interest
Dr. Johnston was funded, in part, by the National Institute of Environmental Health Sciences (#5P30ES007048). Dr. Cushing reports that this work was partially funded by the JPB Foundation Environmental Health Fellowship.
Footnotes
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of a an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
References
- 1.Collins MB, Munoz I, JaJa J. Linking ‘toxic outliers’ to environmental justice communities. Environmental Research Letters. 2016;11(1):015004. doi: 10.1088/1748-9326/11/1/015004. [DOI] [Google Scholar]
- 2.Banzhaf S, Ma L, Timmins C. Environmental justice: The economics of race, place, and pollution. Journal of Economic Perspectives. 2019;33(1):185–208. [PubMed] [Google Scholar]
- 3.Cushing L, Faust J, August LM, Cendak R, Wieland W, Alexeeff G. Racial/Ethnic Disparities in Cumulative Environmental Health Impacts in California: Evidence From a Statewide Environmental Justice Screening Tool (CalEnviroScreen 1.1). American journal of public health. 2015;105(11):2341–8. doi: 10.2105/AJPH.2015.302643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mikati I, Benson AF, Luben TJ, Sacks JD, Richmond-Bryant J. Disparities in Distribution of Particulate Matter Emission Sources by Race and Poverty Status. Am J Public Health. 2018;108(4):480–5. doi: 10.2105/ajph.2017.304297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wing S, Horton RA, Muhammad N, Grant GR, Tajik M, Thu K. Integrating epidemiology, education, and organizing for environmental justice: community health effects of industrial hog operations. American Journal of Public Health. 2008;98(8):1390–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.O’Rourke D, Macey GP. Community environmental policing: Assessing new strategies of public participation in environmental regulation. Journal of Policy Analysis and Management. 2003;22(3):383–414. [Google Scholar]
- 7.Shonkoff SB, Hays J, Finkel ML. Environmental Public Health Dimensions of Shale and Tight Gas Development. Environ Health Perspect. 2014;122(8):787–95. doi: 10.1289/ehp.1307866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Johnston JE, Lim E, Roh H. Impact of upstream oil extraction and environmental public health: A review of the evidence. Sci Total Environ. 2019;657:187–99. doi: 10.1016/j.scitotenv.2018.11.483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Administration UEI. Crude Oil Production: US Department of Energy2018. [Google Scholar]
- 10.Colborn T, Kwiatkowski C, Schultz K, Bachran M. Natural gas operations from a public health perspective. Human and Ecological Risk Assessment: An International Journal. 2011;17(5):1039–56. [Google Scholar]
- 11.Stringfellow WT, Camarillo MK, Domen JK, Sandelin WL, Varadharajan C, Jordan PD et al. Identifying chemicals of concern in hydraulic fracturing fluids used for oil production. Environ Pollut. 2017;220(Pt A):413–20. doi: 10.1016/j.envpol.2016.09.082. [DOI] [PubMed] [Google Scholar]
- 12.Kassotis CD, Iwanowicz LR, Akob DM, Cozzarelli IM, Mumford AC, Orem WH et al. Endocrine disrupting activities of surface water associated with a West Virginia oil and gas industry wastewater disposal site. Science of The Total Environment. 2016;557-558:901–10. doi: 10.1016/j.scitotenv.2016.03.113. [DOI] [PubMed] [Google Scholar]
- 13.Maloney KO, Baruch-Mordo S, Patterson LA, Nicot JP, Entrekin SA, Fargione JE et al. Unconventional oil and gas spills: Materials, volumes, and risks to surface waters in four states of the U.S. Sci Total Environ. 2017;581-582:369–77. doi: 10.1016/j.scitotenv.2016.12.142. [DOI] [PubMed] [Google Scholar]
- 14.Czolowski ED, Santoro RL, Srebotnjak T, Shonkoff SBC. Toward Consistent Methodology to Quantify Populations in Proximity to Oil and Gas Development: A National Spatial Analysis and Review. Environ Health Perspect. 2017;125(8):086004. doi: 10.1289/ehp1535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Elliott EG, Ma X, Leaderer BP, McKay LA, Pedersen CJ, Wang C et al. A community-based evaluation of proximity to unconventional oil and gas wells, drinking water contaminants, and health symptoms in Ohio. Environ Res. 2018;167:550–7. doi: 10.1016/j.envres.2018.08.022. [DOI] [PubMed] [Google Scholar]
- 16.Adgate JL, Goldstein BD, McKenzie LM. Potential public health hazards, exposures and health effects from unconventional natural gas development. Environmental science & technology. 2014;48(15):8307–20. doi: 10.1021/es404621d. [DOI] [PubMed] [Google Scholar]
- 17.Blair BD, Brindley S, Dinkeloo E, McKenzie LM, Adgate JL. Residential noise from nearby oil and gas well construction and drilling. J Expo Sci Environ Epidemiol. 2018;28(6):538–47. doi: 10.1038/s41370-018-0039-8. [DOI] [PubMed] [Google Scholar]
- 18.Allshouse WB, McKenzie LM, Barton K, Brindley S, Adgate JL. Community Noise and Air Pollution Exposure During the Development of a Multi-Well Oil and Gas Pad. Environmental science & technology. 2019. [DOI] [PubMed] [Google Scholar]
- 19.Richburg CM, Slagley J. Noise concerns of residents living in close proximity to hydraulic fracturing sites in Southwest Pennsylvania. Public health nursing (Boston, Mass). 2019;36(1):3–10. doi: 10.1111/phn.12540. [DOI] [PubMed] [Google Scholar]
- 20.Collier-Oxandale A, Hannigan MP, Casey JG, Piedrahita R, Ortega J, Halliday H et al. Assessing a low-cost methane sensor quantification system for use in complex rural and urban environments. Atmos Meas Tech Discuss. 2018:1–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Garcia-Gonzales DA, Shonkoff SBC, Hays J, Jerrett M. Hazardous Air Pollutants Associated with Upstream Oil and Natural Gas Development: A Critical Synthesis of Current Peer-Reviewed Literature. Annual Review of Public Health. 2019;40(1):283–304. doi: 10.1146/annurev-publhealth-040218-043715. [DOI] [PubMed] [Google Scholar]
- 22.Franklin M, Chau K, Cushing LJ, Johnston JE. Characterizing Flaring from Unconventional Oil and Gas Operations in South Texas Using Satellite Observations. Environ Sci Technol. 2019;53(4):2220–8. doi: 10.1021/acs.est.8b05355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Paulik LB, Hobbie KA, Rohlman D, Smith BW, Scott RP, Kincl L et al. Environmental and individual PAH exposures near rural natural gas extraction. Environ Pollut. 2018;241:397–405. doi: 10.1016/j.envpol.2018.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Caron-Beaudoin É, Valter N, Chevrier J, Ayotte P, Frohlich K, Verner M-A. Gestational exposure to volatile organic compounds (VOCs) in Northeastern British Columbia, Canada: A pilot study Environment international. 2018;110:131–8. [DOI] [PubMed] [Google Scholar]
- 25.Caron-Beaudoin É, Bouchard M, Wendling G, Barroso A, Bouchard MF, Ayotte P et al. Urinary and hair concentrations of trace metals in pregnant women from Northeastern British Columbia, Canada: a pilot study. Journal of Exposure Science & Environmental Epidemiology. 2019. doi: 10.1038/s41370-019-0144-3. [DOI] [PubMed] [Google Scholar]
- 26.Hill EL. Shale gas development and infant health: Evidence from Pennsylvania. Journal of Health Economics. 2018;61:134–50. doi: 10.1016/j.jhealeco.2018.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stacy SL, Brink LL, Larkin JC, Sadovsky Y, Goldstein BD, Pitt BR et al. Perinatal outcomes and unconventional natural gas operations in Southwest Pennsylvania. PloS one. 2015;10(6):e0126425–e. doi: 10.1371/journal.pone.0126425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McKenzie LM, Guo R, Witter RZ, Savitz Da, Newman LS, Adgate JL. Birth Outcomes and Maternal Residential Proximity to Natural Gas Development in Rural Colorado. Environmental Health Perspectives. 2014(4):412–7. doi: 10.1289/ehp.1306722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Walker Whitworth K, Kaye Marshall A, Symanski E. Drilling and production activity related to unconventional gas development and severity of preterm birth. Environmental health perspectives. 2018;126(3):037006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Janitz AE, Dao HD, Campbell JE, Stoner JA, Peck JD. The association between natural gas well activity and specific congenital anomalies in Oklahoma, 1997–2009. Environment international. 2019;122:381–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Willis MD, Jusko TA, Halterman JS, Hill EL. Unconventional natural gas development and pediatric asthma hospitalizations in Pennsylvania. Environmental research. 2018;166:402–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Denham A, Willis M, Zavez A, Hill E. Unconventional natural gas development and hospitalizations: evidence from Pennsylvania, United States, 2003–2014. Public health. 2019;168:17–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Casey JA, Wilcox HC, Hirsch AG, Pollak J, Schwartz BS. Associations of unconventional natural gas development with depression symptoms and disordered sleep in Pennsylvania. Scientific reports. 2018;8(1):11375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.McKenzie LM, Crooks J, Peel JL, Blair BD, Brindley S, Allshouse WB et al. Relationships between indicators of cardiovascular disease and intensity of oil and natural gas activity in Northeastern Colorado. Environmental research. 2019;170:56–64.• First publication to take physiological measurements of residents near fracking sites and assess cardiovascular outcomes.
- 35.Kelly-Reif K, Wing S. Urban-rural exploitation: An underappreciated dimension of environmental injustice. Journal of Rural Studies. 2016;47:350–8. doi: 10.1016/j.jrurstud.2016.03.010. [DOI] [Google Scholar]
- 36.McKenzie LM, Allshouse WB, Burke T, Blair BD, Adgate JL. Population Size, Growth, and Environmental Justice Near Oil and Gas Wells in Colorado. Environmental Science & Technology. 2016:acs.est.6b04391–acs.est.6b. doi: 10.1021/acs.est.6b04391. [DOI] [PubMed] [Google Scholar]
- 37.Schinasi L, Horton RA, Guidry VT, Wing S, Marshall SW, Morland KB. Air pollution, lung function, and physical symptoms in communities near concentrated swine feeding operations. Epidemiology. 2011;22(2):208-. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Guidry VT, Kinlaw AC, Johnston J, Hall D, Wing S. Hydrogen sulfide concentrations at three middle schools near industrial livestock facilities. Journal of Exposure Science and Environmental Epidemiology. 2017;27(2):167. [DOI] [PubMed] [Google Scholar]
- 39.Hatcher SM, Rhodes SM, Stewart JR, Silbergeld E, Pisanic N, Larsen J et al. The Prevalence of Antibiotic-Resistant Staphylococcus aureus Nasal Carriage among Industrial Hog Operation Workers, Community Residents, and Children Living in Their Households: North Carolina, USA. Environ Health Perspect. 2017;125(4):560–9. doi: 10.1289/ehp35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Casey JA, Kim BF, Larsen J, Price LB, Nachman KE. Industrial food animal production and community health. Current environmental health reports. 2015;2(3):259–71. [DOI] [PubMed] [Google Scholar]
- 41.Cole D, Todd L, Wing S. Concentrated swine feeding operations and public health: a review of occupational and community health effects. Environmental health perspectives. 2000;108(8):685-. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wing S, Wolf S. Intensive livestock operations, health, and quality of life among eastern North Carolina residents. Environmental health perspectives. 2000;108(3):233-. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wing S, Cole D, Grant G. Environmental injustice in North Carolina’s hog industry. Environmental health perspectives. 2000;108(3):225–31. doi:sc271_5_1835 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kravchenko J, Rhew SH, Akushevich I, Agarwal P, Lyerly HK. Mortality and Health Outcomes in North Carolina Communities Located in Close Proximity to Hog Concentrated Animal Feeding Operations. N C Med J. 2018;79(5):278–88. doi: 10.18043/ncm.79.5.278. [DOI] [PubMed] [Google Scholar]
- 45.Schultz AA, Peppard P, Gangnon RE, Malecki KMC. Residential proximity to concentrated animal feeding operations and allergic and respiratory disease. Environment International. 2019;130:104911. doi: 10.1016/j.envint.2019.104911. [DOI] [PubMed] [Google Scholar]
- 46.Rasmussen SG, Casey JA, Bandeen-Roche K, Schwartz BS. Proximity to Industrial Food Animal Production and Asthma Exacerbations in Pennsylvania, 2005–2012. International journal of environmental research and public health. 2017;14(4):362. doi: 10.3390/ijerph14040362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Loftus C, Afsharinejad Z, Sampson P, Vedal S, Torres E, Arias G et al. Estimated time-varying exposures to air emissions from animal feeding operations and childhood asthma. International Journal of Hygiene and Environmental Health. 2019. doi: 10.1016/j.ijheh.2019.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Poulsen MN, Pollak J, Sills DL, Casey JA, Nachman KE, Cosgrove SE et al. High-density poultry operations and community-acquired pneumonia in Pennsylvania. Environmental Epidemiology. 2018;2(2):e013. doi: 10.1097/ee9.0000000000000013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Heaney CD, Myers K, Wing S, Hall D, Baron D, Stewart JR. Source tracking swine fecal waste in surface water proximal to swine concentrated animal feeding operations. Science of the total environment. 2015;511:676–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Allen S, Fanucchi MV, McCormick LC, Zierold KM. The Search for Environmental Justice: The Story of North Birmingham. International Journal of Environmental Research and Public Health. 2019;16(12):2117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kimbrough DE, Steele NL, Suffet I. Off-Site Forensic Determination of Airborne Elemental Emissions by Multi-Media Analysis: A Case Study at Two Seconday Lead Smelters. Environmental Science & Technology. 1996;30(12):3649-. [DOI] [PubMed] [Google Scholar]
- 52.Dietrich M, Huling J, Krekeler MPS. Metal pollution investigation of Goldman Park, Middletown Ohio: Evidence for steel and coal pollution in a high child use setting. Science of The Total Environment. 2018;618:1350–62. doi: 10.1016/j.scitotenv.2017.09.246. [DOI] [PubMed] [Google Scholar]
- 53.Dietrich M, Wolfe A, Burke M, Krekeler MPS. The first pollution investigation of road sediment in Gary, Indiana: Anthropogenic metals and possible health implications for a socioeconomically disadvantaged area. Environ Int. 2019;128:175–92. doi: 10.1016/j.envint.2019.04.042. [DOI] [PubMed] [Google Scholar]
- 54.Diawara MM, Shrestha S, Carsella J, Farmer S. Smelting Remains a Public Health Risk Nearly a Century Later: A Case Study in Pueblo, Colorado, USA. International journal of environmental research and public health. 2018;15(5):932. doi: 10.3390/ijerph15050932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Johnston JE, Franklin M, Roh H, Austin C, Arora M. Lead and Arsenic in Shed Deciduous Teeth of Children Living Near a Lead-Acid Battery Smelter. Environmental Science & Technology. 2019. doi: 10.1021/acs.est.9b00429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Johnston JE, Lopez m, Gribble MO, Gutschow W, Austin C, Arora M. A Collaborative Approach to Assess Legacy Pollution in Communities Near a Lead-Acid Battery Smelter: The “Truth Fairy” Project. Health Education & Behavior. 2019;46(1_suppl):71S–80S. doi: 10.1177/1090198119859406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Johnston JE, Hricko A. Industrial Lead Poisoning in Los Angeles: Anatomy of a Public Health Failure. Environmental Justice. 2017;10(5):162–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Haynes EN, Sucharew H, Hilbert TJ, Kuhnell P, Spencer A, Newman NC et al. Impact of air manganese on child neurodevelopment in East Liverpool, Ohio. Neurotoxicology. 2018;64:94–102. doi: 10.1016/j.neuro.2017.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Center for Disease Control and Prevention. Fourth national report on human exposure to environmental chemicals, updated tables, February 2015. Atlanta: US Department of Health and Human Services 2015:91–105. [Google Scholar]
- 60.Sun M, Arevalo E, Strynar M, Lindstrom A, Richardson M, Kearns B et al. Legacy and Emerging Perfluoroalkyl Substances Are Important Drinking Water Contaminants in the Cape Fear River Watershed of North Carolina. Environmental Science & Technology Letters. 2016;3(12):415–9. doi: 10.1021/acs.estlett.6b00398. [DOI] [Google Scholar]
- 61.C8 Science Panel. C8 Science Panel Homepage. 2005. [Google Scholar]
- 62.Khalil N, Lee M, Steenland K. Epidemiological Findings. In: DeWitt JC, editor. Toxicological Effects of Perfluoroalkyl and Polyfluoroalkyl Substances Cham: Springer International Publishing; 2015. p. 305–35. [Google Scholar]
- 63.Worley RR, Moore SM, Tierney BC, Ye X, Calafat AM, Campbell S et al. Per- and polyfluoroalkyl substances in human serum and urine samples from a residentially exposed community. Environment International. 2017;106:135–43. doi: 10.1016/j.envint.2017.06.007.•• Assessment of multiple PFAS compounds in residents of an environmental justice communitied due to a nearby manufacturing site’s impact on drinking water sources.
- 64.Hu XC, Andrews DQ, Lindstrom AB, Bruton TA, Schaider LA, Grandjean P et al. Detection of Poly- and Perfluoroalkyl Substances (PFASs) in U.S. Drinking Water Linked to Industrial Sites, Military Fire Training Areas, and Wastewater Treatment Plants. Environmental science & technology letters. 2016;3(10):344–50. doi: 10.1021/acs.estlett.6b00260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Remy LL, Clay T, Byers V, Rosenfeld PE. Hospital, health, and community burden after oil refinery fires, Richmond, California 2007 and 2012. Environ Health. 2019;18(1):48. doi: 10.1186/s12940-019-0484-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.D’Andrea MA, Reddy GK. Detrimental Health Effects of Benzene Exposure in Adults After a Flaring Disaster at the BP Refinery Plant in Texas City. Disaster medicine and public health preparedness. 2016;10(2):233–9. doi: 10.1017/dmp.2015.160. [DOI] [PubMed] [Google Scholar]
- 67.D’Andrea MA, Reddy GK. Adverse Health Complaints of Adults Exposed to Benzene After a Flaring Disaster at the BP Refinery Facility in Texas City, Texas. Disaster medicine and public health preparedness. 2018;12(2):232–40. doi: 10.1017/dmp.2017.59. [DOI] [PubMed] [Google Scholar]
- 68.Young S, Balluz L, Malilay J. Natural and technologic hazardous material releases during and after natural disasters: a review. Science of the total environment. 2004;322(1–3):3–20. [DOI] [PubMed] [Google Scholar]
- 69.Nicole W Wristbands for Research: Using Wearable Sensors to Collect Exposure Data after Hurricane Harvey. Environmental Health Perspectives. 2018;126(4):042001. doi:doi: 10.1289/EHP3131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Christine Cardinal MPH J, Yue Xie M. Implications of Hurricane Harvey on Environmental Public Health in Harris County, Texas. Journal of Environmental Health. 2018;81(2):24–32. [Google Scholar]
- 71.Horney JA, Casillas GA, Baker E, Stone KW, Kirsch KR, Camargo K et al. Comparing residential contamination in a Houston environmental justice neighborhood before and after Hurricane Harvey. PloS one. 2018;13(2):e0192660.• Community-engaged research demostrates that polycyclic aromatic hydrocarbon contaminants linked to combustion were geographically redistributed by flooding during Hurricane Harvey in a heavy industrialized neighborhood of Houston.
- 72.Kiaghadi A, Rifai HS. Physical, Chemical, and Microbial Quality of Floodwaters in Houston Following Hurricane Harvey. Environ Sci Technol. 2019;53(9):4832–40. doi: 10.1021/acs.est.9b00792. [DOI] [PubMed] [Google Scholar]
- 73.Vengosh A, Cowan EA, Coyte RM, Kondash AJ, Wang Z, Brandt JE et al. Evidence for unmonitored coal ash spills in Sutton Lake, North Carolina: Implications for contamination of lake ecosystems. Sci Total Environ. 2019;686:1090–103. doi: 10.1016/j.scitotenv.2019.05.188. [DOI] [PubMed] [Google Scholar]
- 74.Subramanian R, Ellis A, Torres-Delgado E, Tanzer R, Malings C, Rivera F et al. Air Quality in Puerto Rico in the Aftermath of Hurricane Maria: A Case Study on the Use of Lower Cost Air Quality Monitors. ACS Earth and Space Chemistry. 2018;2(11):1179–86. doi: 10.1021/acsearthspacechem.8b00079.• While reference monitors were offline, the authors used low cost air quality monitors to characterize increased air pollution due to reliance on back up generators in the aftermath of Hurricane Maria.
- 75.Agency USEP. Summary of Assessments at Superfund National Priority List Sites. Washginton, DC: 2016. https://archive.epa.gov/katrina/web/html/superfund.html Accessed July 10 2019. [Google Scholar]
- 76.Santella N, Steinberg LJ, Sengul H. Petroleum and Hazardous Material Releases from Industrial Facilities Associated with Hurricane Katrina. Risk Analysis. 2010;30(4):635–49. doi: 10.1111/j.1539-6924.2010.01390.x. [DOI] [PubMed] [Google Scholar]
- 77.Reible DD, Haas CN, Pardue JH, Walsh WJ. Toxic and contaminant concerns generated by Hurricane Katrina. American Society of Civil Engineers; 2006. [Google Scholar]
- 78.Manuel J In Katrina’s Wake. Environmental health perspectives. 2006;114(1):A32–A9. doi: 10.1289/ehp.114-a32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Ruckart PZ, Orr MF, Lanier K, Koehler A. Hazardous substances releases associated with Hurricanes Katrina and Rita in industrial settings, Louisiana and Texas. Journal of Hazardous Materials. 2008;159(1):53–7. doi: 10.1016/j.jhazmat.2007.07.124. [DOI] [PubMed] [Google Scholar]
- 80.Lester S, Rabe A. Superfund: In the Eye of the Storm. Falls Church, Virginia: Center for Health, Environment & Justice2010. [Google Scholar]
- 81.Lubick N Natural disasters: arsenic spike from Ike. Environmental health perspectives. 2009;117(7):A294–A. doi: 10.1289/ehp.117-a294a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Agency USEP. Historical Information About the Response. 2016. https://archive.epa.gov/region02/sandy/web/html/history.html. [Google Scholar]
- 83.Wilson RP. Hurricane Sandy: Environmental Impact and Agency Efforts. Environmental Claims Journal. 2014;26(2):126–56. doi: 10.1080/10406026.2014.868741. [DOI] [Google Scholar]
- 84.Environmental US Protection Agency OotA. EPA Response To The AP’s Misleading Story. 2017. [Google Scholar]
- 85.Dempsey M, Carpenter J. Arkema documents: Planning, mechanical failures led to Harvey chemical fires. Houston Chronicle. 2017. November 15, 2017. [Google Scholar]
- 86.Agency USEP. Evaluation of Remedy Resilience at Superfund NPL and SAA Sites In: Management OoLaE, editor. Washington, DC2018. [Google Scholar]
- 87.Garcia-Lopez GA. The Multiple Layers of Environmental Injustice in Contexts of (Un)natural Disasters: The Case of Puerto Rico Post-Hurricane Maria. Environmental Justice. 2018;11(3):101–8. doi: 10.1089/env.2017.0045.•• Critical assessment of multiple burdens on communities after Hurricane Maria and inequities in the recovery efforts.
- 88.Rice K Hurricane María Has Renewed Puerto Rico’s Fight Against Coal Ash. HuffPost. 2018. August 17, 2018. [Google Scholar]
- 89.Agency USEP. National Priorities List Sites Assessed after Hurricane Florence. Washington, DC2018. [Google Scholar]
- 90.Bruggers J In Florence’s Floodwater: Sewage, Coal Ash and Hog Waste Lagoon Spills. Inside Climate News. 2018. September 18, 2019. [Google Scholar]
- 91.Stafford SL, Renaud AD. Measuring the Potential for Toxic Exposure from Storm Surge and Sea-Level Rise: Analysis of Coastal Virginia. Natural Hazards Review. 2019;20(1):04018024. doi:doi:10.1061/(ASCE)NH.1527–6996.0000315. [Google Scholar]
- 92.Jaime M, Camilo OJ, Eddie B, Ryan C, F CC, Erika M et al. Fugitive Chemicals and Environmental Justice: A Model for Environmental Monitoring Following Climate-Related Disasters. Environmental Justice. 2018;11(3):95–100. doi: 10.1089/env.2017.0044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Casey JA, Karasek D, Ogburn EL, Goin DE, Dang K, Braveman PA et al. Retirements of Coal and Oil Power Plants in California: Association With Reduced Preterm Birth Among Populations Nearby. American Journal of Epidemiology. 2018;187(8):1586–94. doi: 10.1093/aje/kwy110.•• Leverages a natural experiment study design to show the improvements to health of fenceline communities after the closure of power plants.
- 94.Casey JA, Gemmill A, Karasek D, Ogburn EL, Goin DE, Morello-Frosch R. Increase in fertility following coal and oil power plant retirements in California. Environmental Health. 2018;17(1):44. doi: 10.1186/s12940-018-0388-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Burr WS, Dales R, Liu L, Stieb D, Smith-Doiron M, Jovic B et al. The Oakville Oil Refinery Closure and Its Influence on Local Hospitalizations: A Natural Experiment on Sulfur Dioxide. Int J Environ Res Public Health. 2018;15(9). doi: 10.3390/ijerph15092029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Davis B, McDermott S, McCarter M, Ortaglia A. Population-based mortality data suggests remediation is modestly effective in two Montana Superfund counties. Environ Geochem Health. 2019;41(2):803–16. doi: 10.1007/s10653-018-0175-z. [DOI] [PubMed] [Google Scholar]
- 97.Lichter DT, Brown DL. Rural America in an urban society: Changing spatial and social boundaries. Annual review of sociology. 2011;37:565–92. [Google Scholar]
- 98.Brugge D, Patricia H. Hynes. Community Research in Environmental Health: Studies in Science, Advocacy, and Ethics. Aldershot, Hants, Eng.: Ashgate; 2005. [Google Scholar]
- 99.Petersen D, Minkler M, Vásquez VB, Baden AC. Community-Based Participatory Research as a Tool for Policy Change: A Case Study of the Southern California Environmental Justice Collaborative. Review of Policy Research. 2006;23(2):339–54. doi: 10.1111/j.1541-1338.2006.00204.x. [DOI] [Google Scholar]
- 100.Balazs CL, Morello-Frosch R. The Three Rs : How Community-Based Participatory and Reach of Science. Environemental Justice. 2013;6(1):9–16. doi: 10.1089/env.2012.0017. [DOI] [PMC free article] [PubMed] [Google Scholar]