Abstract
Aim: Infertility is defined as failure to achieve a clinical pregnancy after 12 months or more of regular unprotected sexual intercourse. It is a major crisis, triggering psychological stress for most people, and can cause many negative psychological reactions. This study aimed to explore the effects of group counseling sessions by a cognitive approach on infertile women’s stress.
Materials and methods: In this study, 50 infertile women who were referred to an infertility center were selected using convenient sampling. The selected participants were randomly assigned to two groups: experimental and control. First, the Newton Infertility Stress questionnaire was filled as a pre-test by both groups. The control group had no counseling, while the experimental group received 10 sessions of group counseling in the field of stress management and controlling irrational thoughts about infertility during a two-week period. After this time, both groups completed the same questionnaire again and the obtained data were analyzed.
Results: In this study, a significant difference in the mean score of all five aspects of the infertility specific total stress questionnaire and that of total stress after counseling (P = 0.002) was found between the experimental and control groups.
Conclusion: The study showed the effects of group counseling by a participatory approach on infertility specific stress
Keywords:group counseling, infertility, infertility specific distress, reproductive health collaborative model.
INTRODUCTION
Infertility is defined as failure to achieve a clinical pregnancy after 12 months or more of regular unprotected sexual intercourse (without using any contraceptive method) (1). The literature reports that about 50 to 80 million people worldwide suffer from some form of infertility, with one in every six couples facing this problem globally (2). Infertility is observed in 15 percent of spouses who desire to have children (3). According to recent research studies of Avicenna Research Institute (ARI), which is affiliated to ACECR, the prevalence of infertility is 20.2% in Iran (4).
For many, infertility is a major crisis and a psychological stress factor that can cause emotional stress and various negative psychological reactions, including depression, mixed anxiety-depressive disorder, worry, anger, shame, jealousy, loneliness, despair, low self-esteem, emotional instability, feelings of sexual inadequacy, sexual dysfunction and reduced sexual satisfaction (5, 6).
According to studies, infertility can have many psychological consequences. The fact that a person cannot follow the reproduction process and have a child naturally like other normal people is one of the most bitter experiences of life, and the psychological and social context can enhance its importance and make it a psychological crisis. The sense of inability in reproduction and common social reaction towards this group of people in society underlie a major part of mental pressure for this group (7). Infertility diagnosis challenges the infertile couples’ expectations of life, because infertility is an unwanted and unplanned stress factor and many couples do not have the knowledge and skills for its proper management (8, 9).
Abbey et al believe that infertility leads to low self-esteem and self-control and increased interpersonal conflicts in infertile couples; besides, the stress of infertility has detrimental effects on the quality of life, which are stronger in women than men (10).
Abbey et al believe that infertility leads to low self-esteem and self-control and increased interpersonal conflicts in infertile couples; besides, the stress of infertility has detrimental effects on the quality of life, which are stronger in women than men (10).
Infertility stress includes the interaction between the physical conditions causing infertility and medical interventions, other people’s reactions, and the individual’s psychological characteristics, and it may remain for years and relapse with any diagnostic or therapeutic intervention (5). According to a research by Malsted et al, 80% of infertile couples who had experienced a divorce described infertility stress higher and more severe than that of divorce (13).
The intervention is based on a stress management technique and its main objective is to increase the person’s ability to cope with stress, fostering appropriate coping strategies among clients. This means that the person rehabilitates and strengthens both psychologically and in terms of psychological mechanisms. There are multiple stress control intervention techniques, including relaxation, abdominal breathing, biofeedback, medication, counseling, meditation, behavior therapy, sleeping, exercise, etc (14).
There are several ways to cope with the psychological reactions of infertility. Myers and Wark suggest a cognitive-behavioral approach is the most appropriate way to treat these couples, being tailored to their needs (15). Miller also believes that cognitive and behavioral therapies should always be the first step in the treatment of infertile couples (16).
According to the cognitive approach, what upsets people are not these events, but the person’s mindset, resulting from his/her beliefs, schemas and attitude, which affects the way information is processed and results in excitements and individual responses. Therefore, it appears that the individual’s beliefs and mindset about the problem of infertility forms the type and severity of the concerns. So, it is reasonable to be able to improve the disturbing mindset and beliefs of an individual by taking advantage of the principles and techniques of cognitive-behavioral approaches (17).
A century ago, group counseling was founded on principles of assisting patients to improve their health and well-being when struggling with serious medical conditions, which has come full circle to assisting infertility patients. Research has shown that infertility group treatment was both effective and cost-efficient. Despite differences in approach, setting, leadership, treatment disorders or focus, group counseling helps people adapt, adjust, and/or modify their behavior to improve well-being. The theoretical framework of Yalom’s curative factors applies to a variety of infertility counseling groups, especially instillation of hope, universality, cohesion, information sharing, and catharsis. Mental health professionals running infertility counseling groups need to be aware of clinical issues, including group structure, development, membership, confidentiality, and common themes. Therapeutic interventions in infertility group counseling include cognitive-behavioral, emotive-interactional, psycho-educational, technology- mediated, and staff groups (8).
Considering the importance of infertile couples’ mental health, further research studies should emphasize the need for consultation during infertility treatment. To this end, the present study has used a counseling centered intervention and cognitive approach to plan group counseling sessions for infertile women, measuring its impact on infertile women’s specific stress.
METHODOLOGY
In this study, 50 infertile women aged 20 to 45, with at least one year of infertility, referred to Kosar Infertility Center in Urmia during the fall of 2017 and met the study requirements, were selected using a convenient sampling method. More than 100 of the referred women were evaluated by interview, but only 50 of them met the necessary requirements and were included in the study. Subsequently, the study goals were explained to all participants and their informed consent was obtained. Then, subjects were randomly divided into two equal groups, with 25 participants each, an all were given an envelope numbered 1 or 2. Women who received a number 1 envelope were assigned to the intervention group and those who received a number 2 envelope, to the control group.
Inclusion criteria were as follows: Iranian nationality, residence in Urmia, primary infertility, not having an adopted child, not having medical diseases, not having mental-neurological diseases, not using any psychiatric medications, having not experienced any traumatic events such as death of a close relative, not having a family quarrel in the last month, not being employed or having received any education in the field of medical sciences and psychology. Exclusion criteria included unwillingness to cooperate, pregnancy, having experienced a traumatic event such as death of a loved one.
Instruments included general research information form, Newton’s infertility stress questionnaire, record forms for participation in counseling sessions and home practicing of relaxation techniques.
The general research information form consisted of three parts: A) demographic data (age, education, spouse’s education, employment status, marriage duration, family composition); B) infertility information (duration of infertility, cause of infertility, duration of treatment, types of treatments used, attempt to cure, hope for successful treatment, the cost of treatment); and C) psychological information (the individual’s feeling towards the problem of infertility).
The 46-item Newton’s infertility stress questionnaire is a tool designed in 1999 by Newton, which is used to measure the perceived stress of infertility in infertile individuals. It consists of five subtests, including social concerns, sexual concerns, relationship concerns, the need to become parents, and rejection of life without children.
Newton used Cronbach’s alpha coefficient to check the reliability of the test and each subtest was reported as follows: 0.87 for social issues, 0.77 for sexual issues, 0.82 for communication, 0.80 for rejection of childless lifestyle, 0.84 for need to be a parent, and 0.93 for total stress. Validity and reliability of the questionnaire in Iran has been checked by Alizadeh (2004). Cronbach’s alpha coefficient has been estimated 0.78 for social issues, 0.77 for sexual issues, 0.78 for communication, 0.75 for rejection of childless lifestyle, 0.84 for need to be a parent, and 0.91 for total stress (18).
Once the Ethics Committee of the University approved the study and the letter of introduction of Nursing and Midwifery (UMSU.REC.1393.185) was provided to the Kosar Infertility Center, sampling was done based on inclusion criteria. Due to the long duration of treatment (approximately Counseling on Infertile Women’s Stress 366 Maedica A Journal of Clinical Medicine, Volume 14, No. 4, 2019 2.5 months) and because the control group could communicate with the experimental group, the intervention period was divided into two parts in order to prevent any potential information spreading among participants.
Firstly, Newton’s infertility stress questionnaire has been completed by the control group once as a pre-test and then again after two weeks. The control group was reduced to 23 subjects because two of the 25 participants did not cooperate in the post-test. Then, treatment was administered to the experimental group. The control group had not received any counseling.
Knowing that the standard number of people in group counseling should be between 3 to 15 people to ensure intervention effectiveness, the group was divided into two groups of 12 and 13 people, respectively.
The experimental group received 10 sessions of group counseling in Kosar hospital, in the physiological childbirth class. The procedures were as follows: two sessions of sterility counseling on infertility, changing and correcting misconceptions and offering the required solutions by a fellowship of infertility and the researcher, six sessions of group counseling on stress management, and problem solving skill and controlling irrational thoughts about infertility, which were held in three sessions with one week interval and conducted by a PhD in psychology and the study researcher, as described below.
The first session was dedicated to welcome the clients and introduce the treatment. In the second and third sessions, participants were trained to identify their automatic thoughts; the impact of exercise performed by patients on their body expressions, thoughts and feelings, the effects of psychological treatment on disease, and the role of psychological factors on emotions and sensory experiences were discussed. Afterwards, identifying negative thoughts was taught and homework was assigned. In the fourth session, evaluation of automatic thoughts and alternative responses were discussed. Also, the previous session was reviewed before performing muscle relaxation and deep breathing which lasted for 10 minutes. Subsequently, replacing rational thoughts with irrational thoughts was practiced and patients were asked about the effects of positive and negative thoughts on their feelings and they were encouraged to discuss about them. At the end of the session, homework was assigned. The researcher dedicated the fifth and sixth sessions to coping self-talk, written emotional disclosure, assertive communication and two sessions of reproductive health on menstrual cycle, pregnancy diagnosis, pregnancy, and sexual health. The duration of each session was 90 minutes and all sessions were held with one-week intervals.
At the end of each session, the researcher administered a 15-minute relaxation exercise, using Jacobson relaxation technique (including discontinuous tightening and relaxing movements of body muscles from lower limbs towards upper limbs). Participants have been also trained and provided with the educational pamphlet and a CD of relaxation and its home practice record form, so that they could perform it at home and record the required information.
Two weeks after the intervention, Newton’s infertility stress questionnaire was filled by the experimental group again. The collected data were explored using SPSS software version 16 in two parts, descriptive and inferential statistics, which were analyzed using descriptive statistics and independent t-test, respectively.
RESULTS
The descriptive statistics of the studied groups are shown in Table 1 and Figures 1 and 2. There was a significant difference between the groups based on one way ANOVA test. Tukey post hoc test showed that there was a significant difference among the four groups: between CPP-ACP paste and laser (p < 0.0001), CPP-ACP laser and paste-laser (p <0.0001), CPP-ACP paste and CPP-ACP laser-paste (p < 0.0001), control and CPP-ACP paste (p < 0.0001), and control and CPP-ACP laser-paste (p < 0.0001). This test showed that there was no significant difference between control and laser groups (p = 0.99).
DISCUSSION
The participants in both groups were homogeneous in terms of overall study profile. Independent samples t-test and chi-square were used to analyze quantitative and qualitative variables. Results did not show any significant difference in demographic and familial variables (age, duration of marriage, individual’s education, spouse’s education, employment status, combining life) between the two groups. Both groups were homogenous in terms of demographic and familial variables before the study.
Independent samples t-test and chi-square were used to analyze quantitative and qualitative variables of characteristics related to infertility (information on infertility, for diagnosis and treatment of infertility time, number of IUI and IVF, cause and treatment of infertility, hope for successful treatment, economic costs). The results did not show any significant difference between the two groups. Both groups were homogenous in terms of characteristics related to infertility before the study.
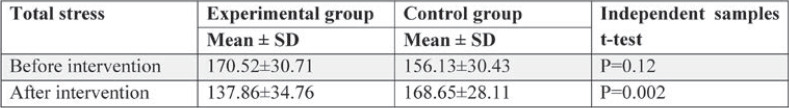
Regarding the main goals of the study, results showed that before treatment, mean scores of stress in the experimental and control groups Counseling on Infertile Women’s Stress Maedica A Journal of Clinical Medicine, Volume 14, No. 4, 2019 367 were 170.52±30.71 and 156.13±30.43, respectively, which was not statistically significant (p=0.12). Both groups were homogeneous in terms of overall stress levels at the beginning of the study. However, the mean post-treatment scores in the experimental and control groups were 137.86±34.76 and 168.65±28.11, respectively. The results of independent samples t-test showed that there was a significant difference between the experimental and control groups after treatment (P = 0.002), which highlighted that counseling centered treatment had an impact on reducing the total stress of infertile women in the experimental group (Table 1).
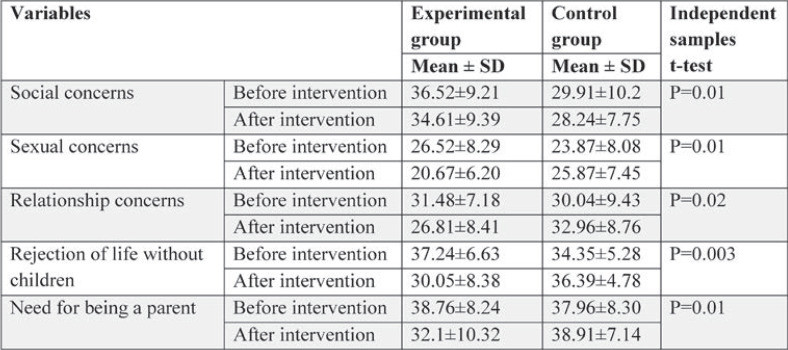
experimental group (Table 1). In this study, the mean scores of all five aspects of the infertility specific total stress questionnaire in the experimental and control groups were compared, showing a significant difference between the two groups in social concerns, sexual concerns, relationship concerns, rejection of life without children, and need for being a parent (Table 2).
According to our findings, the mean posttreatment scores of “social concerns” in the experimental and control groups were 28.24±7.75 and 36.61±9.39, respectively. The results of independent samples t-test showed a significant difference between the two groups after treatment (P = 0.01).
The average differences in “sexual concerns” between the experimental and control groups were 20.67±6.20 and 25.78±7.45, respectively. The results of independent samples t-test revealed a significant post-treatment difference between the experimental and control groups (P = 0.01).
The average score in “communication concerns” was 26.81±8.41 in the experimental group and 96.32±8.76 in the control group. Independent samples t-test showed a significant difference between the two groups in terms of “communication concerns”, indicating a reduced stress in communication issues in the experimental group (P = 0.02).
The average scores in “rejection of life without children” was 30.05±8.38 in the experimental group and 36.39±4.78 in the control group. The results of independent samples t-test showed a significant difference between the two groups in “rejection of life without children”, indicating a decline in stress of life without children in the experimental group (P = 0.003).
The average scores of “need to become a parent” in the experimental and control groups were 32.1±10.32 and 38.91±7.14, respectively. The results of independent samples t-test showed that there was a significant post-treatment difference between the two groups (P = 0.01).
DISCUSSION
The results of the present study showed that group counseling with a participatory approach had been effective on reducing infertility specific stress in various aspects such as social concerns, sexual concerns, relationship concerns, worries and fears of rejection of life without children, and concerns related to the need for becoming a parent.
In this study, the difference in average scores of “social concerns” before and after treatment had a significant difference (P = 0.01). Thus, treatment was effective in reducing community concerns of participants in the experimental group. In a study conducted by Casino (19), it was found that the group receiving online psychological treatment showed a significant reduction in the score related to the social aspect of Newton infertility stress questionnaire in comparison to the control group, which is in line with the results of our study. In the study of Latifnejad et al (20), treatment was given as an individual counseling to women undergoing IVF treatment, and a statistically significant difference was observed in social concerns between the control group and experimental group, which is in accordance with our findings. Also, in the Latifnejad et al, the mean difference of scores for “community concerns” was 8.2, while in our research it was 2; a possible explanation for this higher reduction obtained by us may be the influence of the collaborative approach to counseling. Given that group counseling is an interpersonal dynamic process that focuses on conscious thoughts and behavior, therapeutic function, desire to reality, abreaction and mutual trust, care, understanding, acceptance and support functions, collaboration allows participants to share their own capabilities and benefit from each other’s skills.
Also, group counseling enables participants to form a social network with other members that act as a basis for changing the environment; thus, group provides the safest place for talking about things they cannot say to others and abreaction. This was one of the influential factors in this study.
According to the findings of current study, there was a significant difference in the scores of “sexual concerns” before and after treatment, the intervention leading to an improvement in sexual concerns of the experimental group. The study of Peterson et al (2007) reported a high sexual stress in infertile women before treatment and showed that men and women who reported a greater subjective and autonomic anxiety at the onset of treatment may have increased levels of sexual infertility stress. For couples whose treatments are unsuccessful, increases in anxiety and sexual infertility stress may be exacerbated (21), which is consistent with the results of this study. Although there are few studies which specifically examine the link between relationship factors and sexual infertility stress, a prospective longitudinal study found that six months after unsuccessful IVF treatments, men and women showed greater dissatisfaction in their sexual relationship than couples who achieved a pregnancy (22). In another study by Rpocary (23), both fertile and infertile groups were compared during the pregnancy period, happening naturally in fertile women and by help of assisted reproductive technology in infertile women. Women who had used assisted reproductive technology experienced lower sexual satisfaction when faced with stressful situations. The probable reason for the difference between the results of Rpocary’s study and those of our study is the participants’ pregnancy, since pregnancy itself is one of the factors affecting sexual satisfaction and in women who have become pregnant with assisted reproductive technology, fear of harm to the fetus and miscarriage is higher than in those who get pregnant naturally. However, participants in the present study were only infertile women.
According to our results, the average scores of communication concerns in the experimental group were reduced by treatment, which has led to an improved communication among participants.
In a study published in 2003, Lee investigated the impact of treatment on the psychological responses of infertile women undergoing IVF treatment and noticed that poor interpersonal relationships in the experimental group had improved, which was also found by us in the present study (5).
In the study conducted by Latifnejad et al, no significant difference was observed between the mean scores of “social concerns” before and after treatment (20), which is not consistent with our results. This difference may be due to cognitivebehavioral group therapy present in this experi- Counseling on Infertile Women’s Stress Maedica A Journal of Clinical Medicine, Volume 14, No. 4, 2019 369 ment. Diagnosis of infertility challenges infertile couples’ expectations of life because infertility is an unwanted and unplanned stressful factor and many couples do not have enough knowledge and skills to properly manage it. In our study as well as in other studies, infertile women using cognitive-behavioral techniques actually use some sorts of behavior to cognitively reconstruct the problem in stressful situations and thus enjoy better mental health; there was a significant difference between the two study groups in depression and anxiety after the final session of intervention. Cognitive behavioral stress management significantly decreased the rate of depression and anxiety in the experimental group (24).
In the present study, there was a significant difference between the mean scores of “concerns of acceptance of lifestyle without children” and “need to become a parent” before and after treatment, the intervention leading to a reduction of participants’ concerns. In Latifnejad’s study (20) there was a significant difference in the “need to become a parent” between the experimental and control groups, but not also in the “rejection of lifestyle without children”, which may be due to the uncooperative approach used in that research, while in the present study, cooperative and cognitive- behavioral approaches have been also taken into account besides the participatory approach.
Lymns et al. reported that the body-mind group, almost similarly to cognitive and behavioral approaches, can reduce the tension and desire to have children in infertile couples (25). According to the cognitive approach, it is not these events that upset people but the individuals’ mindset, which is the result of personal beliefs, schema and attitude, affecting the way the information is processed and causing individual responses and excitements. Therefore, it appears that individuals’ beliefs and way of thinking about the problem of infertility forms the type and intensity of the concerns (26).
Another important point that should be mentioned in justifying treatment effectiveness in the present study is the effect of psychological support in a “Group”. Considering the fact that infertile people feel alone and consider their problem to be unique, being also unable to express their feelings and talk about personal problems to most people, group therapy develops a sense of empathy among them and they realize that their problem is not unique to them. In addition, meeting people in these groups provides infertile couples with the opportunity to share their experiences and expand their own coping strategies.
According to the findings, there was a significant difference between the mean differences in infertility specific total stress scores between the two groups (P=0.002). The findings of Silvia Mayumi et al. (2011) and Alizadeh (2004) indicate that the total infertility stress in infertile women was high before treatment (18, 27). In the study conducted by Latifnejad, the total infertility stress had dropped at the end of the research (20), which is consistent with our findings. The results of the studies carried out by Sexton (2010) and Casino (2008) suggest that online treatment for coping with infertility stress decreased general stress symptoms in infertile women, but there was no significant difference between the two groups in terms of perceived infertility stress (19, 28). Since we used a face to face treatment, it appears that the confounding factors in our study were less than in studies carried out by Sexton and Casino, which were performed online. Besides, counseling was provided by a team composed of a master of counseling in gynecology, a PhD in Educational Psychology, and an infertility fellowship, and it seems that the participatory approach to counseling, on one hand, and group counseling, on the other hand, affected the results of the study.
The present study investigated the effects of group counseling with a participatory approach on infertility specific stress. As indicated by our findings, psychological disorders exacerbate the problems with their vicious cycle. With the help of group counseling sessions, infertile individuals can strengthen their family bonds by taking the advantage of desired marital satisfaction and a life without stress and worries. Obviously, the existence of resources and cooperation between gynecologists, midwifery counselors and psychologists in infertility clinics plays an important role in reducing the problems of infertile people.
CONCLUSION
The results of this study showed that group counseling was effective in reducing stress in infertile women.
Conflict of interests: none declared
Financial support: This work was financially supported by the Research Deputy of Urmia University of Medical Sciences.
Ethics Committee approval: The study was approved by the Ethics Committee of Urmia University of Medical Sciences (approval number: UMSU.REC.1393.185).
Author contributions: conception and design – Ordoni avval Zahra, Rabiepoor Soheila; data analysis and interpretation – Yas Atefeh, Behroozilak Tahereh, Arefi Marzieh; manuscript draft – Ordoni avval Zahra, Rabiepoor Soheila, Yas Atefeh; critical revision of the manuscript –Ordoni avval Zahra, Rabiepoor Soheila, Behroozilak Tahereh, Arefi Marzieh, Yas Atefeh; final approval of the manuscript – Ordoni avval Zahra, Rabiepoor Soheila, Yas Atefeh.
TABLE 1.
Comparison of total stress scores between control and experimental groups before and after intervention in infertile women
TABLE 2.
Comparison of mean scores of specific infertility stress between experimental and control groups before and after intervention
Contributor Information
Ordoni Avval ZAHRA, Midwifery Counseling, Golestan Health Center, Golestan University of Medical Sciences, Gorgan, Iran.
Rabiepoor SOHEILA, Reproductive Health Research Center & Midwifery Department, Urmia University of Medical Sciences, Urmia, Iran.
Behroozilak TAHEREH, Infertility Fellowship, Urmia University of Medical Sciences, Urmia, Iran.
Arefi MARZIEH, Psychology Department, Islamic Azad University of Urmia, Urmia, Iran.
Yas ATEFEH, Midwifery Counseling, Urmia University of Medical Sciences, Urmia, Iran.
References
- 1.Berek JS, Hillard PJA. Berek & Novak, Gynecology, 15th ed, Tehran: Artin teb. 2012.
- 2.Kalkhoran LF, Bahrami H, Farrokhi NA, et al. Comparing anxiety, depression and sexual life satisfaction in two groups of fertile and infertile women in Tehran. Journal of Reproduction & Infertility. 2011;2:157–163. [Google Scholar]
- 3.Boivin J, Bunting L, Collins JA, Nygren KG. International estimates of infertility prevalence and treatment-seeking: potential need and demand for infertility medical care. Human Reproduction. 2007;6:1506–1512. doi: 10.1093/humrep/dem046. [DOI] [PubMed] [Google Scholar]
- 4.Safarinejad MR. Infertility among couples in a population‐based study in Iran: prevalence and associated risk factors. International journal of andrology. 2007;6:1506–1512. doi: 10.1111/j.1365-2605.2007.00764.x. [DOI] [PubMed] [Google Scholar]
- 5.Lee S-H. Effects of Using a Nursing Crisis Intervention Program on Psychosocial Responses and Coping Strategies of Infertile Women DuringIn VitroFertilization. Journal of Nursing Research. 2003;3:197–208. doi: 10.1097/01.jnr.0000347636.95347.f8. [DOI] [PubMed] [Google Scholar]
- 6.Sadock B. Synopsis of Psychiatry: Behavioral Sciences. Clinical Psychiatry, 9th ed (translated by Pourafkari N), Tehran, lran, Shahrab Publishers. Journal of Nursing Research. 2000. p. 55.
- 7.Haririan HR MY, Aghajanloo A. Prevalence of depression and contributing factors of depression in the infertile women referred to Kosar Infertility Center. Obstet Gynecol Infertil. 2010;2:45–50. [Google Scholar]
- 8.Covington SN, Burns LH. Infertility counseling: A comprehensive handbook for clinicians. Cambridge University Press. 2006.
- 9.Peterson BDNC, Rosen KH, Skaggs GE. Coping processes of couples experiencing infertility. Fam Relat. 2006;2:335–342. [Google Scholar]
- 10.Benyamini Y, Gozlan M, Kokia E. Variability in the difficulties experienced by women undergoing infertility treatments. Fertility and Sterility. 2005;2:275–283. doi: 10.1016/j.fertnstert.2004.10.014. [DOI] [PubMed] [Google Scholar]
- 11.Taylor E. The stress of infertility. Human Ecology Forum. Cornell University, Human Ecology. 1995.
- 12.Abbey A, Andrews FM, Halman LJ. Infertility and subjective well-being: the mediating roles of self-esteem, internal control, and interpersonal conflict. Journal of Marriage and Family. 1992;54:408–417. [Google Scholar]
- 13.Hjelmstedt A, Widström AM, Wramsby H, et al. Personality factors and emotional responses to pregnancy among IVF couples in early pregnancy: a comparative study. Acta Obstetricia et Gynecologica Scandinavica. 2003;2:152–161. doi: 10.1034/j.1600-0412.2003.00040.x. [DOI] [PubMed] [Google Scholar]
- 14.Watkins KJ, Baldo TD. The infertility experience: Biopsychosocial effects and suggestions for counselors. Journal of Counseling & Development. 2004;4:394–402. [Google Scholar]
- 15.Karaca A, Yavuzcan A, Batmaz S, et al. The Effect of Cognitive Behavioral Group Therapy on Infertility Stress, General Health, and Negative Cognitions: A Randomized Controlled Trial. Journal of Rational-Emotive & Cognitive-Behavior Therapy. 2019. pp. 1–20.
- 16.Noorbala A, Ramezanzadeh F, Malakafzali H, et al. Effectiveness of psychiatric interventions on depression rate in infertile couples referred to Vali-Asr. Hakim Research Journal. 2008;4:17–26. [Google Scholar]
- 17.Smith JA, Smith AH. Treating Faith‐Based Infertile Couples Using Cognitive‐Behavioral Counseling Strategies: A Preliminary Investigation. Counseling and Values. 2004;1:48–63. [Google Scholar]
- 18.Alizadeh T. Stress associated with self-control source. Journal of Reproduction Infertility. 2004. pp. 194–204.
- 19.Cousineau TM, Green TC, Corsini E, et al. Online psychoeducational support for infertile women: a randomized controlled trial. Human Reproduction. 2008;3:554–566. doi: 10.1093/humrep/dem306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Latifnejad L, Rasolzadeh M, Mousavifar N, Modarres M. The effect of collaborative counseling on perceived infertility-related stress in infertile women undergoing IVF. Journal of Mashhad. 2010;3:21–26. [Google Scholar]
- 21.Peterson BD, Newton CR, Feingold T. Anxiety and sexual stress in men and women undergoing infertility treatment. Fertility and Sterility. 2007;4:911–914. doi: 10.1016/j.fertnstert.2006.12.023. [DOI] [PubMed] [Google Scholar]
- 22.Slade P, Emery J, Lieberman B. A prospective, longitudinal study of emotions and relationships in in-vitro fertilization treatment. Human Reproduction.(Oxford, England) 1997;1:183–190. doi: 10.1093/humrep/12.1.183. [DOI] [PubMed] [Google Scholar]
- 23.Repokari LPR, Unkila-Kallio L, Vilska S, Poikkeus P, et al. Infertility treatment and marital relationships: a 1-year prospective study among successfully treated ART couples and their controls. Hum Reprod. 2007;5:81–91. doi: 10.1093/humrep/dem013. [DOI] [PubMed] [Google Scholar]
- 24.Hamid N. The effectiveness of stress management on depression, anxiety and fertilization of infertile women. Article (in Persian) J Behav Sci. 2011;1:55–60. [Google Scholar]
- 25.Lemmens G, Vervaeke M, Enzlin P, et al. Coping with infertility: a body–mind group intervention programme for infertile couples. Human Reproduction. 2004;8:1917–1923. doi: 10.1093/humrep/deh323. [DOI] [PubMed] [Google Scholar]
- 26.Abdolahi HM, Ghojazadeh M, Abdi S, et al. Effect of cognitive behavioral therapy on anxiety and depression of infertile women: A meta–analysis. Asian Pacific Journal of Reproduction. 2019;6:251. [Google Scholar]
- 27.Gradvohl SMO, Osis MJD, Makuch MY. Stress of men and women seeking treatment for infertility. Revista Brasileira de Ginecologia e Obstetrícia. 2013;6:255–261. doi: 10.1590/s0100-72032013000600004. [DOI] [PubMed] [Google Scholar]
- 28.Sexton MB, Byrd MR, O’Donohue WT, Jacobs NN. Web-based treatment for infertility-related psychological distress. Archives of Women’s Mental Health. 2010;4:347–358. doi: 10.1007/s00737-009-0142-x. [DOI] [PubMed] [Google Scholar]