Abstract
In the Decade of Nutrition, food must be reconsidered.
The main objective of our research was to establish if there are any correlations between ultraprocessed food consumption and increased asthma prevalence or other respiratory outcomes. Meanwhille, it will be an important step to design some lifestyle recommendations with direct benefits for asthma treatment. NOVA system for food classification is a new concept addressing food quality.
Ultraprocessed food, made entirely from substances derived from food and additives, that includes other sources of nutrients and energy, is not usually used in culinary preparation. How asthma outcomes are influenced by Western diet that contains a lot of processed food and what benefits could arise from the Mediterranean diet are subjects for interesting studies.
Substantial correlations have been established between unhealthy diets, especially Western diet, ultraprocessed foods and food allergies and asthma pathogenesis and control.
NOVA clasification of processing foods and dietary inflammatory index are helpful tools in early identifying of correct dietary approach in asthma.
More research in nutrition recommendations for asthma patients must be done and practical guidelines in nutritional interventions are future steps.
Keywords:ultraprocessed food, Mediterranean diet, Western diet, asthma outcomes, dietary inflammatory index, NOVA system for food classification.
INTRODUCTION
We are now in the Decade of Nutrition (1), as it was designated by the UN Supporting Sustainable Development Goals for 2016-2025. Food must be reconsidered in order to know whether it will bring an additional benefit for well-being and health or some aspects of nutrients and processing can promote diseases.
Asthma, a chronique inflammatory disease characterised by wheezing, dispneea and cough due to airways obstruction, is affecting 230 million persons worldwide and 30 million people in Europe (2). Allergic asthma is highly frequent, and environmental changes represent a key factor in increasing allergies (3).
Food allergies are estimated to affect 10.8% of all US inhabitants (4), and their frequency is increasing in direct relation with Western style adoption (5).
Western diet (WD) (6), meaning the dietary pattern characterised by consumption of highly processed food, highly refined carbohydrates, high-fat, especially highly saturated fat, highly processed meat and overconsumtion of salt. This dietary pattern is usually hypercaloric and is associated with a low level of physical activity and sedentarism, leading to obesity.
Mediterranean diet (MD) (7), used by people living near the Mediterranean Sea, is rich in olive oil, fish, fruits, vegetables and nuts, together with a high fiber content. It is recognized to be a diet with many health benefits, which will be further described here.
The main objective of our research is to establish whether ultra-processed food (UPF) could be related to an increased asthma prevalence and to design some lifestyle recommendations that may be beneficial for asthma development, based on current scientific evidence.
The new developed NOVA system for food classification is effectively addressing the quality of diets. This system is based on food processing (1).
Ultra-processed products are manufactured and promoted as attractive, hyper-pallatable, easy to be consumed anywhere and in any occasion. Due to spectaculous and intensive marketing efforts, they often promote overconsumption. But could all these ultra-processed foods pose a risk to the general population? Or could it influence the pathogenesis of some diseases?
The concept of ultra-processing was developed by the University of Sao Paulo and it was explained for the first time in Public Health Nutrition in 2009 (8).
Food processing could explain the relationship between food, nutrition, health and disease.
Concept definition
“The most important factor now, when considering food, nutrition and public health, is not nutrients, and is not foods, so much as what is done to foodstuffs and nutrients originally contained in them before they are purchased and consumed. That is to say, the issue is food processing – or, to be more precise, the nature, extent and purpose of processing, and what happens to food and to us as a result of processing” (8).
The meaning of processing is in relation to industrial formulations that could be manufactured from natural nutrients derived from food or obtained by synthesis from other organic or anorganic sources. How can these ultra-processed foods be described? They contain a small percentage of whole food, they are usually ready to be consumed and have a high content of salt, sugar, fats, while being depleted of proteins, fibers or bioactive compounds (1).
NOVA classification for processed food (1)
Unprocessed or minimally processed foods are either home made or cooked in small restaurants. Edible parts of plants and animals and fungi, algae and water are unprocessed foods. Minimally processed food is a natural food altered by some processes of removal of inedible parts by crushing, grinding, refrigerating, chilling, freezing, pasteurization, fermentation, drying and vacuum packaging. These processes will preserve natural food, improving storage, safety and making them more pleasant for consumption.
Processed culinary ingredients are defined by substances derived from group 1 or directly from nature and changed by pressing, refining, grinding, milling, or drying, all these processes being designed to make durable products that will be used at home to prepare, cook group 1 foods and to prepare enjoyable handmade dishes and meals. They will not be consumed by themselves, but in combination with group 1.
Processed foods (for example, canned fish, bottled vegetables, cheeses, fresh bread) are prepared by adding oil, sugar, salt or other substances from group 2 to group 1 via various types of processes such as preservation, cooking or non-alcoholic fermentation (for bread and cheese). This group includes versions of group 1.
Ultra-processed foods are formulations made mainly or entirely from substances derived from different foods and additives with a small percentage of group 1. Importantly, they incorporate other sources of nutrients and energy, which are not normally used in culinary preparations; some are extracted from foods but others are derived from further processig of food constituents. Classes of food additives that can be found in UPF are those initiating or enhancing sensorial qualities of food or changing unpalatable aspects – for example, colours, non-sugar sweeteners, carbonating, firming, emulsifiers. Processes used in this type of food include hydrolisation, hydro- Asthma and Ultra-Processed Food 404 Maedica A Journal of Clinical Medicine, Volume 14, No. 4, 2019 genation, or pre-processing for frying, which do not have domestic equivalents.
NOVA – in practical use
Beside assesing changes in dietary patterns, the socio-economic distribution, NOVA is important to evaluate the association between consumption of UPF and obesity (9-11), dyslipidemias (12) and metabolic syndrome (13).
Meanwhile, the impact of nutritional interventions will be evaluated.
NOVA has been used to evaluate the impact of ultra-processed products on the quality of diets (14, 15).
Incidence of hypertension and obesity was evaluated in relation to UPF consumption (16, 17).
The main issue with UPF is that these types of foods displace unprocessed or minimally processed foods.
Diets during lifecycle – potential role in asthma (18)
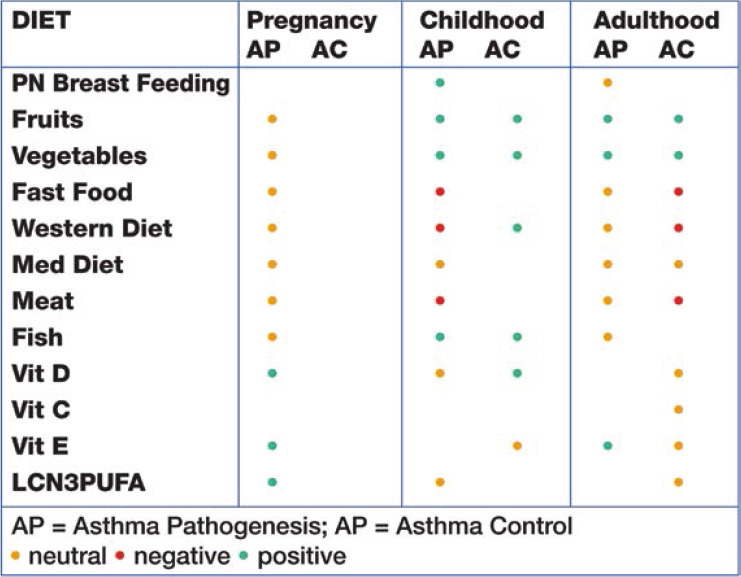
Dietary patterns (foods and nutrients) and exposure period (prebirth, childhood, adult) play a role in the asthma pathogenesis and progression (Table 1).
Pregnancy period – a decreased maternal intake of vitamins E and D, Zinc, fruits and vegetables is correlated with asthma development in childhood.
Childhood – generally named processed food: fast food, WD and processed meat consumption in childhood have been shown to be associated with asthma development later in adult life; vitamins A, D, and E, Zinc, fruits, vegetables, and MD have protective effects against asthma evolution.
Adulthood – adult asthma control is negatively influenced by fast food consumption in childhood; also, WD adoption in adulthood is correlated with less asthma control.
Clinical evidence – ultra-procesed food and respiratory outcomes (Brasilian study) (19) (18)
A large retrospective study, involving 109104 Brasilian adolescents, found a positive association between UPF and asthma. The assessment of UPF consumption was done by a questionnaire that evaluated the previous seven days consumption of UPF based on a score from 0 to 42, showing that the higher the intake, the higher the score. The weekly consumption of salty or sweet biscuits, packaged snacks, ultraprocessed meats, sweets or candies and soft drinks was divided into three groups: 0-2, 3-4 and >5 days/week. The score was calculated by adding partial scores according to the weekly intake of each of the mentioned products.
Self reported symptoms on asthma and wheezing in the previous 12 months have been recorded. In conclusion, this study found that ultraprocessed food consumption was positively correlated with asthma and wheezing in Brasilian adolescents (19).
Specific evidence in asthma: processed meat
Another study, performed on 971 adult participants, reported worsening asthma symptoms correlated with proccesed meat intake. The effect was indirectly mediated by BMI.
In conclusion, over time (seven year-follow-up), processed meat intake is associated with increased asthma symptoms for more than four servings/week compared to less than one serving/ week. These results expand the previously proven effects of diets in adult asthma (20).
Dietary inflammatory index and asthma
Increasing asthma prevalence in the latest years could be associated with diets. A lower diet quality together with an increasing use of processed Asthma and Ultra-Processed Food TABLE 1. Diet role during life stages in asthma (18) Maedica A Journal of Clinical Medicine, Volume 14, No. 4, 2019 405 foods may be the promoter of a pro-inflammatory environment. Reversible airflow obstruction, the signature in asthma, a chronic inflammatory disease, is accompanied by wheezing, cough and breathlessness. Beside genetic or environmental factors, more and more dietary factors are incriminated to contribute to asthma progression.
Dietary inflammatory index (DII) is a new validated concept that was tested to describe the inflammatory potential of different diets (21).
A study published by Lisa Wood (21) calculated the DII from food frequency questionnaires and identified that the DII score was higher for people with asthma vs controls. This could indicate that subjects had pro-inflammatory diets. FEV1 is significantly associated with the DII score. Each unit increase from the DII score is associated with 3.44 times decrease in FEV1. What is the conclusion from these findings? Tipically, people with asthma have a pro-inflammatory diet, which may worsen their disease parameters. Lifestyle measures, together with a healthy diet recommendation could be a good strategy in improving asthma outcomes.
A promoter of a pro-inflammatory environment could be the WD pattern (1). Characterised by a consumption of highly refined carbohydrates and saturated fats, WD is worsening asthma (22). A study on 46 subjects, for 14 weeks, with a nutritional intervention based on antioxidant foods decreased the clinically significant inflammatory markers in asthma (IL6, C reactive protein, TNF-alfa) as well as asthma exacerbations (22).
Lifestyle interventions in asthma – a good strategy for improvement of asthma outcomes
Specific lifestyle interventions for pulmonary diseases are not yet developed, compared to other chronic diseases. Adapting proofs from other chronic disease interventions and assessing their efficacy on specific asthma outcomes could lead to a fast development of lifestyle medicine designed for pulmonary diseases.
The primary research focus should be to adapt and understand how actual lifestyle interventions work in asthma in order to close the gap for knowledge in pulmonary lifestyle medicine.
In asthma, lifestyle interventions must consider the potential for implementation and use valuable information for clinical practice based on evidence-based guidelines (23).
Lifestyle in asthma – a summary of evidence-based recommendations (24)
Nutrition science is increasingly recommending healthy dietary patterns rather than different foods or nutrients. More attention to practical guidelines was given in chronic disease prevention, asthma being just a nascent field (23).
Important scientific research has been performed and provided concrete scientific proofs for dietary patterns with a positive influence on FEV1, exacerbations or wheezing, leading to strong recommendations for asthma patients:
- High consumption of fruits and vegetables (21);
- The MD, which is rich in fish, olive oil, nuts, fruits and vegetables, but adapted to an individual’s caloric need, is highly recommended, with proven benefits in asthma;
- In obese asthma patients, a weight loss of 5-10% could significantly improve asthma control (24);
- Exercise in asthma will bring additional benefits to asthma control, although it is still not clear whether the positive impact is the direct effect of exercise or is rather related to a greater weight loss benefit, especially in obese asthma patients (25).
A systematic review and meta-analysis was performed to assess the effect of exercise training (EXT) on the quality of life (QOL), bronchial hyperresponsiveness (BHR), exercise induced bronchoconstriction (EIB), lung function and exercise capacity. The meta-analysis included 17 studies (25) on a total number of 599 patients, which showed a significant improvement of QOL (17%), BHR (53%) EIB (9%) and FEV1 (3%) compared to controls.
EXT is improving asthma symptoms, exercise capacity (due to changes in airway hyperreactivity) and QOL through lung function improvement and airway hyperreactivity.
Prospective medical nutrition therapy in asthma (26) should consider:
- addressing food triggers
- correcting energetic intake levels and adjusting nutritional deficiencies
- limiting fatty food ingestion and encouraging portion control
- avoiding allergenic proteins from food
- avoiding sulfits, tartrazin, that are used in processed foods and could become triggers for asthma exacerbations.
CONCLUSIONS AND FUTURE DIRECTIONS
Affecting millions of people worldwide, asthma is an important healthcare issue.
Lifestyle changes that could improve the QoL of patients with asthma and obesity are under research (27-32), but so far, this approach is not recognized and studied to its full potential.
Substantial correlations have been established between unhealthy diets, especially WD, UPF and food allergies and asthma pathogenesis and control.
NOVA clasification of processing foods and the dietary inflamatory index (33) are helpful tools for early identification of a correct dietary approach in asthma (34-36).
More research in nutrition recommendations for asthma patients must be performed and practical guidelines in asthma nutritional interventions are future steps.
Further pragmatic studies analysing the impact of a comprehensive model of weight loss intervention, with behavioral modifications, physical activity and dietary changes on symptoms, pulmonary function, airway hyperreactiviy and exacerbations in asthma, mainly for adults with comorbidities such as asthma and obesity. Obesity is a risk factor and a comorbidity for asthma, being the result of an unhealthy diet and physical inactivity. It can be described as „obese asthma’’‚ a multiphenotypic disease of multifactorial origin (37-39).
More and more, the complex relation between asthma and obesity, based on inflammatory common mechanisms, should be better understood. Asthma in obese people is correlated with a lower QoL and increased healthcare access, due to an impaired response to standard asthma therapy (40-46).
Important studies are correlating obesity with impaired response to cortisosteroid therapy in asthma, which is leading to higher and higher doses, and obviously, to secondary effects (47-50).
A better management of asthma requires new medical and environmental strategies that will contribute to reduce the prevalence of this important chronic disease.
Conflict of interests: none declared.
Financial support: none declared.
TABLE 1.
Diet role during life stages in asthma (18)
Contributor Information
Anca HANCU, Lotus-Med Clinic, Bucharest, Romania.
Florin MIHALTAN, „Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania.
Gabriela RADULIAN, „Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania.
References
- 1.Monteiro CA, Cannon G, Moubarac J-C, et al. The UN Decade of Nutrition, the NOVA food classification and the trouble with ultra-processing, Public Health Nutrition. 2018;1:5–17. doi: 10.1017/S1368980017000234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.European Lung White Book. www.erswhitebook.org, Chapter 21, p. 138.
- 3.Takano H, Inone KI. Environmental pollution and allergies. J Toxicol Pathology. 2017;30:193–199. doi: 10.1293/tox.2017-0028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gupta R. JAMA Netw Open. 2019.
- 5.Julia V, Macia L, Dombrowicz D. The impact of diet on asthma and allergic diseases. Nature Reviews Immunology. 2015;15:308–322. doi: 10.1038/nri3830. [DOI] [PubMed] [Google Scholar]
- 6.Brigham EP, Kolahdooz F, Hansel N, et al. Association between Western diet pattern and adult asthma: a focused review. Ann Allergy Asthma Immunol. 2015;4:273–280. doi: 10.1016/j.anai.2014.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Davis C, Bryan J, Hodgson J, Murphy K. Definition of the Mediterranean Diet; a Literature Review. Nutrients. 2015;11:9139–9153. doi: 10.3390/nu7115459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Monteiro CA. Nutrition and health. The issue is not food, nor nutrients, so much as processing. Public Health Nutr. 2009;12:729–731. doi: 10.1017/S1368980009005291. [DOI] [PubMed] [Google Scholar]
- 9.Louzada ML, Martins AP, Canella DS, et al. Ultra-processed foods and the nutritional dietary profile in Brazil. Rev Saude Publica. 2015;49:38. doi: 10.1590/S0034-8910.2015049006132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Barcelos GT, Rauber F, Vitolo MR. Processed and ultra-processed food products and nutrient intake in children. Rev Cienc Saude. 2014;7:155–161. [Google Scholar]
- 11.Bielemann R, Santos Motta J, Minten G, et al. Consumption of ultra-processed foods and their impact on the diet of young adults. Rev Saude Publica. 2015;49:28. doi: 10.1590/S0034-8910.2015049005572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rauber F, Campagnolo P, Hoffman D et al. Consumption of ultra-processed food products and its effects on children’s lipid profiles: a longitudinal study. Nutr Metab Cardiovasc Dis. 2015;25:116–122. doi: 10.1016/j.numecd.2014.08.001. [DOI] [PubMed] [Google Scholar]
- 13.Tavares L, Fonseca S, Garcia Rosa L, et al. Relationship between ultra-processed foods and metabolic syndrome in adolescents from a Brazilian family doctor program. Public Health Nutr. 2012;15:82–87. doi: 10.1017/S1368980011001571. [DOI] [PubMed] [Google Scholar]
- 14.Crovetto M, Uauy R, Martins AP, et al. Household availability of ready-to-consume food and drink products in Chile: impact on nutritional quality of the diet. Rev Med Chile. 2014;142:850–858. doi: 10.4067/S0034-98872014000700005. [DOI] [PubMed] [Google Scholar]
- 15.Cediel G, Reyes M, Louzada MLC, et al. Contribution of ultra-processed foods to total energy and added sugars in Chilean diet. Public Health Nutr. 2017. [DOI] [PMC free article] [PubMed]
- 16.Mendonça R, Pimenta A, Gea A, et al. Ultra-processed foods consumption and risk of overweight/ obesity: the SUN cohort study. Am J Clin Nutr. 2016;104:433–440. doi: 10.3945/ajcn.116.135004. [DOI] [PubMed] [Google Scholar]
- 17.Mendonça R, Lopes A, Pimenta A, et al. Ultraprocessed food consumption and the incidence of hypertension in a Mediterranean cohort: the Seguimiento Universidad de Navarra Project. Am J Hypertens 2016(Epublication ahead of print version). [DOI] [PubMed]
- 18.Guilleminault L, Williams EJ, Scott HA, et al. Diet and Asthma: Is It Time to Adapt Our Message? Nutrients. 2017;11:1227. doi: 10.3390/nu9111227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Melo B, Rezende L, Machado P, et al. Ultra-processed products and asthma Associations of ultra-processed food and drink products with asthma and wheezing among Brazilian adolescents. Pediatr Allergy Immunol. 2018;5:504–511. doi: 10.1111/pai.12911. [DOI] [PubMed] [Google Scholar]
- 20.Li Z, Rava M, Bédard A, et al. Cured meat intake is associated with worsening asthma symptoms. Thorax. 2017;3:206–212. doi: 10.1136/thoraxjnl-2016-208375. [DOI] [PubMed] [Google Scholar]
- 21.Lisa Wood et al. Dietary inflammatory index is related to asthma risk, lung function and systemic inflammation in asthma. Clin Exp Allergy. 2015;45(1):177–183. doi: 10.1111/cea.12323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Young RP, Hopkins RJ. Is the “Western Diet” a New Smoking Gun for Chronic Obstructive Pulmonary Disease? Ann Am Thorac Soc. 2018;6:662–663. doi: 10.1513/AnnalsATS.201802-131ED. [DOI] [PubMed] [Google Scholar]
- 23.Nyenhuis S, Dixon AE, Ma J. Impact of Lifestyle Interventions Targeting Healthy Diet, Physical Activity and Weight Loss on Asthma in Adults: What is the evidence? Allergy Clin Immunol Pract. 2018;3:751–763. doi: 10.1016/j.jaip.2017.10.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dixon AE, Holguin F. Diet and Metabolism in the Evolution of Asthma and Obesity. Clin Chest Med. 2019;1:97–106. doi: 10.1016/j.ccm.2018.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Eichenberger PA, Diener SN, Kofmehl R, Spengler CM. Effects of Exercise Training on Airway Hyperreactivity in Asthma: A Systematic Review and Meta-Analysis. Sports Med. 2013;11:1157–1170. doi: 10.1007/s40279-013-0077-2. [DOI] [PubMed] [Google Scholar]
- 26.Mahan LK, Raymond JL. Krause’s Food & the Nutrition Care Process. 14th edition 2016, p 688.
- 27.Adeniyi FB, Young T. Weight loss interventions for chronic asthma. C. ochrane Database Syst Rev. 2012;7:CD009339. doi: 10.1002/14651858.CD009339.pub2. [DOI] [PubMed] [Google Scholar]
- 28.Carson KV, et al. Physical training for asthma. Cochrane Database Syst Rev. 2013;9:CD001116. doi: 10.1002/14651858.CD001116.pub4. [DOI] [PubMed] [Google Scholar]
- 29.Marcus BH, et al. Physical activity intervention studies: what we know and what we need to know: a scientific statement from the American Heart Association Council on Nutrition, Physical Activity, and Metabolism (Subcommittee on Physical Activity); Council on Cardiovascular Disease in the Young; and the Interdisciplinary Working Group on Quality of Care and Outcomes Research. Circulation. 2006;24:2739–2752. doi: 10.1161/CIRCULATIONAHA.106.179683. [DOI] [PubMed] [Google Scholar]
- 30.Baranowski T, Anderson C, Carmack C. Mediating variable framework in physical activity interventions. How are we doing? How might we do better? Am J Prev Med. 1998;4:266–297. doi: 10.1016/s0749-3797(98)00080-4. [DOI] [PubMed] [Google Scholar]
- 31.National Asthma Education and Prevention Program. Expert Panel Report 3 (EPR 3): Guidelines for the. Diagnosis and Management of Asthma.National Institutes of Health; Bethesda, MD: 2007.
- 32.Boulet LP, et al. Effect of bariatric surgery on airway response and lung function in obese subjects with asthma. Respir Med. 2012;5:651–660. doi: 10.1016/j.rmed.2011.12.012. [DOI] [PubMed] [Google Scholar]
- 33.Wood LG,Gibson PG. Dietary factors lead to innate immune activation in asthma. Pharmacol Ther. 2009;1:37–53. doi: 10.1016/j.pharmthera.2009.03.015. [DOI] [PubMed] [Google Scholar]
- 34.Wood LG, Attia J, McElduff P, et al. Assessment of dietary fat intake and innate immune activation as risk factors for impaired lung function. Eur J Clin Nutr. 2010;8:818–825. doi: 10.1038/ejcn.2010.68. [DOI] [PubMed] [Google Scholar]
- 35.Olafsdottir IS, Gislason T, Thjodleifsson B, et al. C reactive protein levels are increased in non-allergic but not allergic asthma: a multicentre epidemiological study. Thorax. 2005;60:451–454. doi: 10.1136/thx.2004.035774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Takemura M, Matsumoto H, Niimi A, et al. High sensitivity C reactive protein in asthma. Eur Respir J. 2006;5:908–912. doi: 10.1183/09031936.06.00114405. [DOI] [PubMed] [Google Scholar]
- 37.Dixon AE, et al. An official American Thoracic Society Workshop report: obesity and asthma. Proceedings of the American Thoracic Society. 2010;5:325–335. doi: 10.1513/pats.200903-013ST. [DOI] [PubMed] [Google Scholar]
- 38.Sutherland ER. Linking obesity and asthma. Annals of the New York Academy of Sciences. 2014;1:31–41. doi: 10.1111/nyas.12357. [DOI] [PubMed] [Google Scholar]
- 39.Baffi CW, Winnica DE, Holguin F. Asthma and obesity: mechanisms and clinical implications. Asthma Res Pract. 2015;1:1. doi: 10.1186/s40733-015-0001-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Avallone KM, McLeish AC. Asthma and aerobic exercise: a review of the empirical literature. J Asthma. 2013;2:109–116. doi: 10.3109/02770903.2012.759963. [DOI] [PubMed] [Google Scholar]
- 41.Dogra S, Baker J. Physical activity and health in Canadian asthmatics. J Asthma. 2006;10:795–799. doi: 10.1080/02770900601034304. [DOI] [PubMed] [Google Scholar]
- 42.Bacon SL, et al. Association between patterns of leisure time physical activity and asthma control in adult patients. BMJ Open Respiratory Research. 2015;1:e000083. doi: 10.1136/bmjresp-2015-000083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Matthews CE, et al. Physical activity, sedentary behavior, and cause-specific mortality in black and white adults in the Southern Community Cohort Study. Am J Epidemiol. 2014;4:394–405. doi: 10.1093/aje/kwu142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cohen SS, et al. Sedentary and physically active behavior patterns among low-income African-American and white adults living in the southeastern United States. PLoS One. 2013;4:e59975. doi: 10.1371/journal.pone.0059975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Doggett N, Dogra S. Physical inactivity and television-viewing time among Aboriginal adults with asthma: a cross-sectional analysis of the Aboriginal Peoples Survey. Health Promot Chronic Dis Prev Can. 2015;3:54–61. doi: 10.24095/hpcdp.35.3.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Barros R, et al. Adherence to the Mediterranean diet and fresh fruit intake are associated with improved asthma control. Allergy. 2008;7:917–923. doi: 10.1111/j.1398-9995.2008.01665.x. [DOI] [PubMed] [Google Scholar]
- 47.Baffi CW, Winnica DE, Holguin F. Asthma and obesity: mechanisms and clinical implications. Asthma Res Pract. 2015;1:1. doi: 10.1186/s40733-015-0001-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sutherland ER, et al. Body mass and glucocorticoid response in asthma. American Journal of Respiratory and Critical Care Medicine. 2008;7:682–687. doi: 10.1164/rccm.200801-076OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Peters-Golden M, et al. Influence of body mass index on the response to asthma controller agents. European Respiratory Journal. 2006;3:495–503. doi: 10.1183/09031936.06.00077205. [DOI] [PubMed] [Google Scholar]
- 50.Adeniyi FB, Young T. Weight loss interventions for chronic asthma. Cochrane Database Syst Rev. 2012;7:CD009339. doi: 10.1002/14651858.CD009339.pub2. [DOI] [PubMed] [Google Scholar]