Abstract
Children with autism spectrum disorder (ASD) are reported to have greater levels of anger rumination than typically developing children. This study examined anger rumination in children with ASD in comparison to children with disruptive behavior disorder without ASD. We also tested if anger rumination is associated with aggression and the core ASD symptoms of restricted and repetitive behaviors (RRBs). This study included three groups of children aged 8–16 years: 63 had ASD (ASD group), 79 had disruptive behavior disorder (DB group), and 40 healthy controls (HC). ASD and DB groups showed greater anger rumination relative to the HC group. Anger rumination was associated with RRBs in children with ASD, suggesting the link to core ASD symptoms.
Keywords: Anger rumination, Autism spectrum disorder, Aggression, Emotion regulation, Restricted and repetitive behaviors
Anger rumination is a cognitive-emotional process that refers to the tendency to dwell on frustrating experiences and to recall past anger experiences (Sukhodolsky et al. 2001). More broadly, rumination also represents a maladaptive form of emotion processing that entails remaining focused on the stressor through repetitive and passive dwelling upon distress, past mistakes, regrets, and one’s shortcomings (Nolen-Hoeksema 1991; Nolen-Hoeksema et al. 2008). Further, rumination may preclude the use of adaptive emotion regulation strategies such as cognitive reappraisal and problem solving (Connor-Smith et al. 2000; Nolen-Hoeksema et al. 2008). Although rumination is associated with anxiety and depression (Aldao et al. 2010), there is also evidence that rumination may be a factor in other forms of maladaptive behaviors including disruptive behaviors such as anger/irritability and aggression (Aldao et al. 2016; McLaughlin et al. 2014; Nolen-Hoeksema and Watkins 2011).
Autism spectrum disorder (ASD) is characterized by defi-cits in social communication and interaction, and restricted, repetitive patterns of behavior (RRBs) (American Psychiatric Association 2013). However, over 50% of children with ASD have co-occurring disruptive behavior disorders and/or internalizing disorders (Lecavalier et al. 2019; Sukhodolsky et al. 2008) that cause substantial distress and impair functioning. In addition to concomitant disorders, children and adults with ASD also exhibit elevated levels of rumination relative to typically developing controls (Crane et al. 2011; Mazefsky et al. 2014; Patel et al. 2017). While studies have investigated anger rumination in children without ASD (Smith et al. 2016), the mechanisms of anger rumination in children with ASD has not been well-studied.
Similar to results in non-ASD populations (Aldao et al. 2010), associations between rumination and internalizing symptoms of anxiety and depression were also found in children (Mazefsky et al. 2014; Patel et al. 2017; Pouw et al. 2013) and adults (Crane et al. 2011; Gotham et al. 2014; Keenan et al. 2017) with ASD. Two recent studies reported an association between anger rumination, core ASD symptoms, and disruptive behaviors (Patel et al. 2017; Pugliese et al. 2015). However, only one study to date (Patel et al. 2017) examined anger-focused rumination in a sample of children with ASD and reported greater levels of anger rumination in children with ASD relative to typically developing children. Another study examined anger rumination in young adults in the general population and showed that anger rumination was associated with anxiety symptoms and disruptive behaviors; that is, symptoms of social anxiety predicted greater anger rumination, which was associated with increased levels of disruptive behaviors (Pugliese et al. 2015). Relevant to the current study, the ASD symptom of perseveration was found to augment the relationship between anger-focused rumination and disruptive behaviors (Pugliese et al. 2015). Together, these studies provide pre-liminary evidence of an increased tendency to engage in anger-focused rumination in ASD and its possible association with ASD core symptoms. Given the high prevalence of co-occurring disruptive behavior in ASD (Lecavalier et al. 2019; Mazurek et al. 2013), a better understanding of the mechanisms underlying anger rumination in ASD may contribute to the development of novel treatments or inform existing clinical interventions addressing disruptive behaviors as well as emotion regulation (Mazefsky and White 2014). However, no studies to date have investigated patterns of anger rumination in children with ASD relative to children with disruptive behavior disorders. Therefore, the present study examines anger rumination in a sample of well-characterized children with ASD compared to children with disruptive behavior disorders without ASD and to matched typically developing controls.
In addition, associations between anger rumination and aggressive behavior was reported in both adults (Denson et al. 2011; White and Turner 2014) and children (Harmon et al. 2017; Smith et al. 2016) without ASD. Children with disruptive behavior disorders were also found to have higher levels of anger rumination than typically developing controls (Smith et al. 2016). Given the high prevalence of individuals with ASD who also meet criteria for comorbid psychiatric disorders, particularly disruptive behavior disorders (Lecavalier et al. 2019; Leyfer et al. 2006; Simonoff et al. 2008; van Steensel et al. 2013), it is important to examine if anger rumination in ASD is associated with symptoms related to disruptive behavior such as aggression. Thus, we also tested if aggressive behavior is associated with anger rumination in children with ASD.
Restricted and repetitive behavior and lack of flexibility have been hypothesized to contribute to emotion dysregulation in children with ASD (Mazefsky et al. 2013). Studies have noted hyper-focus on upsetting events (Crane et al. 2011) and correlation of anger rumination with core ASD symptoms (Patel et al. 2017; Pugliese et al. 2015). In our clinical work, we have also observed that children with ASD, when asked to describe a situation that made them angry during cognitive-behavioral therapy (CBT), often reported events from the distant past and became visibly upset when recalling the frustrating elements of these events (Sukhodolsky and Scahill 2012). Some children with ASD appeared as if they were re-experiencing anger felt when the upsetting situation had actually happened. This clinical observation was reminiscent of the construct of anger rumination, described by Sukhodolsky et al. (2001), that is measured by items such as “memories of certain events from the past still make me angry.” We reasoned that rumination in general, as a cognitive process of over-focusing on negative emotions, is associated with the core ASD symptoms of RRBs including insistence on sameness, inflexible adherence to routines, rigidity of thinking, and perseveration. For example, depressive rumination was associated with perseveration in young adults (Keenan et al. 2017) and adults with ASD (Gotham et al. 2014). However, no studies to date examined the association between ASD symptoms of RRBs and anger rumination. Thus, we tested the association of anger rumination with RRBs in children with and without ASD and varying levels of disruptive behavior.
In the present study, we examined anger rumination in well-characterized samples of children aged 8–16 with and without ASD and clinically significant levels of disruptive behavior. Our primary aim was to examine levels of anger rumination in three groups of children: ASD, Disruptive Behavior without ASD (DB group), and typically developing healthy controls (HC) matched on age, gender, and IQ. We predicted that children with ASD would show greater levels of anger rumination compared to HC children. In the context of a paucity of prior studies directly comparing anger rumination in children with ASD and children with disruptive behavior disorders, we hypothesized that there would be differences in anger rumination between the ASD and DB groups. We restricted the main analyses to the three largest samples (ASD, DB without ASD, and HC) to provide the most statistical power. However, because the focus of this study centered on anger rumination in ASD, ASD subgroups were also formed for post hoc analyses to examine differences in anger rumination in children with ASD with and without co-occurring disruptive behavior. Children with ASD were divided into two groups based on the presence of co-occurring disruptive behavior disorder. Regarding these ASD subgroups, we expected that children with ASD-plus-disruptive-behavior (ASD/DB+ subgroup) would show greater levels of anger rumination compared to children with ASD-without-disruptive-behavior (ASD/DB− subgroup). Our second aim was to test correlates of anger rumination (i.e., gender, aggression, and RRBs). We expected anger rumination to be associated with aggression and RRBs.
Methods
Participants and Procedures
Three groups of children aged 8–16 years were included: 63 verbally fluent children with ASD (ASD group); 79 children with disruptive behavior disorders without ASD (DB group); and 44 typically developing healthy controls (HC group) matched for age, gender, and IQ. Demographic and clinical characterization data for participants are shown in Table 1. Participants with ASD had a DSM-5-de-fined ASD diagnosis that was confirmed with the Autism Diagnostic Interview-Revised (ADI-R) (Le Couteur et al. 2003) and Autism Diagnostic Observation Schedule-2nd edition (ADOS-2) (Lord et al. 2012) administered by an expert clinician trained to research reliability.
Table 1.
Participant demographics and clinical characteristics
| Variable | Total sample | ASD subgroups based on disruptive behavior (DB) | |||||
|---|---|---|---|---|---|---|---|
| Healthy controls n = 44 |
Disruptive behavior n = 79 |
ASD n = 63 |
p value | With DB (ASD/DB+) n = 22 |
Without DB (ASD/DB−) n = 41 |
p value | |
| Age, years (SD) | 12.3 (1.8) | 11.7 (2.1) | 12.4 (1.9) | .09 | 12.5 (2) | 12.3 (1.9) | .74 |
| Male (n, %) | 29 (65.9) | 54 (68.4) | 47 (74.6) | .58 | 17 (77.3) | 30 (73.2) | .72 |
| Mean IQa (SD) | 111.3 (10) | 105.8 (13.7) | 104.9 (19.1) | .07 | 103.7 (16.8) | 105.6 (20.3) | .71 |
| Race (n, %) | .13 | .09 | |||||
| White | 28 (63.6) | 58 (73.4) | 54 (85.7) | 18 (81.8) | 36 (87.8) | ||
| Black | 9 (20.5) | 11 (13.9) | 2 (3.2) | 2 (9.1) | 0 | ||
| Asian/Pacific Islander | 1 (2.3) | 1 (1.3) | 1 (1.6) | 1 (4.5) | 0 | ||
| American Indian/Alaska Native | 0 | 2 (2.5) | 0 | 0 | 0 | ||
| Other/more than one race | 6 (13.6) | 7 (8.9) | 6 (9.5) | 1 (4.5) | 5 (12.2) | ||
| Ethnicity (n, %) | .45 | .41 | |||||
| Hispanic | 5 (11.4) | 14 (17.7) | 7 (11.1) | 1 (4.5) | 6 (14.6) | ||
| Non-Hispanic | 39 (88.6) | 65 (82.3) | 55 (88.7) | 21 (95.5) | 35 (85.4) | ||
| Mean CBCL aggression T score (SD) | 50.5 (1.8) | 75.3 (7.2) | 60.8 (11.2) | < .001bc | 72.9 (8.6) | 54.4 (5.8) | < .001b |
| Mean RPQ aggression total score (SD) | 2.5 (2.2) | 19.5 (6.7) | 10.1 (7.9) | < .001bc | 17.5 (7.8) | 6.1 (4.3) | < .001b |
| Mean SRS-2 total T score (SD) | 45 (5.7) | 62.3 (10.6) | 73.5 (9.5) | < .001bd | 79.2 (7.6) | 70.5 (9.2) | < .001b |
| Social communication interaction scale | 45 (7.7) | 63.1 (10.3) | 73.3 (9.8) | < .001bd | 78.5 (8.1) | 70.4 (9.6) | .001b |
| Restricted and repetitive behaviors scale | 43.8 (3.8) | 58.4 (11.2) | 71.9 (10.8) | < .001bd | 79.4 (7.7) | 67.9 (10.2) | < .001b |
| Mean ADOS-2 module 3 total score (SD) | 13.2 (4.2) | 15.2 (4.1) | 12.1 (3.9) | .005b | |||
| Social affect scale | 10.7 (3.7) | 11.9 (3.4) | 9.9 (3.7) | .04b | |||
| Restricted and repetitive behaviors scale | 2.6 (1.7) | 3.3 (1.7) | 2.2 (1.6) | .01b | |||
| Mean ADI-R subscale scores (SD) | |||||||
| Social interaction | 19.5 (5.3) | 20.2 (5.4) | 19.2 (5.2) | .47 | |||
| Communication | 15.3 (3.8) | 15.5 (3.5) | 15.2 (3.9) | .76 | |||
| DSM-5 diagnosis (n, %) | |||||||
| Oppositional defiant disorder | 56 (70.9) | 22 (28.2) | < .001b | 22 (100) | 0 | < .001b | |
| Conduct disorder | 3 (3.8) | 0 | .25 | 0 | 0 | ||
| Disruptive behavior disorder NOS | 4 (5.1) | 0 | .13 | 0 | 0 | ||
| Disruptive mood dysregulation disorder | 17 (21.5) | 0 | < .001b | 0 | 0 | ||
| Attention-deficit/hyperactivity disorder | 60 (75.9) | 35 (55.6) | .01b | 19 (86.4) | 16 (39) | < .001b | |
| Anxiety disorder | 19 (24.1) | 33 (52.4) | .001b | 9 (40.9) | 24 (58.5) | .18 | |
| Depressive disorder | 5 (6.3) | 3 (4.8) | 1 | 0 | 3 (7.3) | .54 | |
| Currently taking medication (n, %) | 34 (43) | 29 (46) | < .001b | 16 (72.7) | 13 (31.7) | .002b | |
| Type of medication (n, %) | |||||||
| Stimulants | 25 (31.6) | 12 (19) | .09 | 7 (31.8) | 5 (12.2) | .09 | |
| Non-stimulants | 15 (19) | 9 (14.3) | .46 | 7 (31.8) | 2 (4.9) | .006b | |
| Antidepressant | 9 (11.4) | 11 (17.5) | .30 | 6 (27.3) | 5 (12.2) | .17 | |
| Neuroleptics | 7 (8.9) | 5 (7.9) | .84 | 4 (18.2) | 1 (2.4) | .04b | |
| Mood stabilizers | 0 | 3 (4.8) | .09 | 3 (13.6) | 0 | .04b | |
| Benzodiazepines | 0 | 2 (3.2) | .19 | 2 (9.1) | 0 | .12 | |
Disruptive behavior group refers to children with disruptive behavior disorder without ASD
ASD/DB+, autism spectrum disorder with co-occurring disruptive behavior disorder; ASD/DB−, autism spectrum disorder without disruptive behavior disorder; ADI-R, autism diagnostic interview-revised; ADOS-2, autism diagnostic observation schedule-2nd edition; CBCL, child behavior checklist; RPQ, reactive–proactive aggression questionnaire; SRS-2, social responsiveness scale-second edition
Full-scale IQ measured by the Wechsler abbreviated scale of intelligence (Wechsler 1997) or the differential ability scales-II (Elliott 2007)
Significant group differences at p < 0.05, Bonferroni corrected, except for Chi square test for categorical variables and independent samples T test
ASD > healthy controls; disruptive behavior > healthy controls; disruptive behavior > ASD
ASD > healthy controls; ASD > disruptive behavior; disruptive behavior > healthy controls
All children received a comprehensive diagnostic evaluation that included the Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL) (Kaufman et al. 2016) or the Anxiety Disorders Interview Schedule for Children and Parents (ADIS-C/P) (Silverman and Albano 1996), which are structured interviews with excellent reliability that were conducted with parent and child by an expert clinician to establish main DSM-5 diagnoses. Full scale IQ was evaluated with the Wechsler Abbreviated Scale of Intelligence (WASI) (Wechsler 1997) or the Differential Ability Scales-II (Elliott 2007). Parents and children completed diagnostic evaluations (K-SADS-PL or ADIS) and IQ assessments (WASI or DAS-II) depending on the study that they were enrolled in. Parents and children also completed a battery of self-report measures that was facilitated by a research assistant to ensure understanding and answer any questions. Parents completed demographics and medical history forms.
Children with disruptive behavior were required to meet a cut-off criterion of a T score ≥ 65 on the Aggressive Behavior scale of the parent-rated child behavior checklist (CBCL), a well-established measure of child psychopathology (Achenbach and Rescorla 2001). This score is 1.5 standard deviation units above the mean in the standardization sample and represents a cut-off for a clinically significant level of aggression. The Aggressive Behavior scale includes 16-items reflecting inappropriate anger outbursts as well as verbal and physical aggression. To recruit a representative sample of children with disruptive behavior, children were included in this study regardless of co-occurring psychiatric diagnoses or treatment with psychotropic medication. HC participants were required to have no current or past history of psychiatric disorders and a CBCL-aggression T-score below 55. For post hoc analyses of anger rumination differences within the ASD group, children with ASD were divided into two groups based on the presence or absence of co-occurring disruptive behavior disorder (ASD/DB+ and ASD/DB− groups, respectively), which was based on diagnostic assessments (K-SADS-PL, ADIS).
Children with ASD and children with disruptive behavior disorders participated in clinical trials of behavior therapy at the Yale Child Study Center. This paper combined baseline data from two studies in order to examine anger rumination in children with ASD. Healthy control participants were recruited from the community via advertisements, flyers, and brochures. Each participant’s parent provided informed consent according to specifications by the institutional review board at the Yale University School of Medicine. Each child provided assent.
Measures
The anger rumination scale (ARS)(Sukhodolsky et al. 2001) is a 19-item self-report measure assessing the cognitive processes related to feelings of anger as well as the tendency to think about current anger-provoking situations and to recall past anger episodes. Each item is rated on a 4-point Likert scale of 1 (almost never), 2 (sometimes), 3 (often), and 4 (almost always). The ARS has four subscales including: anger afterthoughts, thoughts of revenge, angry memories, and understanding of causes. The first two subscales (anger afterthoughts and thoughts of revenge) correspond to thinking about a recent episode or recalling and getting angry about a distant episode. The last two subscales (angry memories and understanding of causes) correspond to thinking about causes of an anger episode in order to achieve a meaningful understanding of the anger episode. Higher scores on the ARS indicate a greater level of anger rumination. Within the current sample, high internal reliability was observed for the ARS in the total sample (α = 0.89) and within the ASD (α = 0.88) and DB (α = 0.89) groups. We report mean values and standard deviation on the ARS subscales for descriptive purposes (Table 2). However, due to the sample size of the study, we only use the ARS total score in the analyses.
Table 2.
Between-group differences in anger rumination
| Variable | Total sample | ASD subgroups based on disruptive behavior (DB) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| ASD n = 63 |
Disruptive behavior n = 79 |
Healthy controls n = 44 |
F | p value | η2 | ASD/DB+ n = 22 |
ASD/DB− n = 41 |
p value | |
| ARS total, mean (SD) | 34.7 (8.7) | 36.7 (10) | 29.8 (8.2) | 8.00 | < .001ab | .08 | 37.8 (7.4) | 32.9 (8.9) | .03a |
| Angry afterthoughts, mean (SD) | 10.4 (3.3) | 10.9 (3.4) | 8.6 (3.0) | 7.15 | .001ab | .07 | 11.4 (3.1) | 9.9 (3.3) | .08 |
| Thoughts of revenge, mean (SD) | 6.8 (2.4) | 7.3 (2.8) | 5.7 (2.3) | 5.14 | .007ac | .05 | 7.5 (2.6) | 6.4 (2.2) | .08 |
| Angry memories, mean (SD) | 9.2 (2.6) | 10.2 (3.2) | 8.3 (2.8) | 5.68 | .004ac | .06 | 10.1 (2.5) | 8.7 (2.6) | .03a |
| Understanding causes, mean (SD) | 8.2 (2.3) | 8.4 (2.8) | 7.2 (2.5) | 3.31 | .039ac | .04 | 8.7 (2.1) | 7.9 (2.4) | .15 |
Degrees of freedom = 2 for ANOVA. Means for ARS subscales are provided for descriptive purposes. The ARS total score is used for all group-level and multiple regression analyses. Disruptive behavior group refers to children with disruptive behavior disorder without ASD
ARS, anger rumination scale; ASD/DB+, autism spectrum disorder with co-occurring disruptive behavior disorder; ASD/DB−, autism spectrum disorder without disruptive behavior disorder; ASD, autism spectrum disorder
Significant group differences at p < 0.05, Bonferroni corrected, except for independent samples T-test
ASD > healthy controls; disruptive behavior > healthy controls
Disruptive behavior > healthy controls
The social responsiveness scale-second edition (SRS-2) (Constantino 2005) is a 65-item scale that measures symptoms associated with ASD. Items are rated on a 4-point scale from “not true” to “almost always true” by the child’s parent or teacher. In the current study, the parent version for children ages 4–18 years was used. Higher scores on the SRS-2 indicate greater social impairment. Total raw scores for the restricted and repetitive behavior (RRB) subscale were used for analyses in this study. High internal reliability was observed for the SRS-2 RRB subscale within the total sample (α = 0.89) and within the ASD (α = 0.80) and DB (α = 0.78) groups.
The ADOS-2 (Lord et al. 2012) is a standardized, semi-structured observational assessment that elicits social interaction, language use, and restricted and repetitive behaviors and circumscribed interests. The ADOS-2 yields two subscale scores of social affect and restricted and repetitive behaviors as well as algorithm-based classifications of autism/autism spectrum or non-spectrum disorder. Item scores are on a scale of 0–2, with higher scores indicating greater severity of symptoms. Module 3 (intended for fluent speakers) was administered to participants in the current study.
The reactive–proactive aggression questionnaire (RPQ) (Raine et al. 2006) is a 23-item parent-report scale that measures aggression on a 3-point Likert scale. Twelve items index proactive aggression (e.g., “Had fights with others to show who was on top”) and 11 items index reactive aggression (e.g., “Reacted angrily when provoked by others”). Because proactive and reactive aggression subscales were highly correlated in this sample (r = 0.78), the RPQ Aggression Total score was used as a continuous measure of aggression in the analyses. Internal consistency for the RPQ was high for the total sample (α = .93) and for the ASD (α = .92) and DB (α = .84) groups.
Statistical analyses
Our primary aim was to examine levels of anger rumination between the three groups of children (ASD, DB, and HC groups). Statistical analyses were conducted with SPSS v24. The differences in levels of anger rumination in children with ASD relative to samples of children with disruptive behavior disorder (DB group) and HC participants were examined using a one-way ANOVA with a statistical thresh-old of significance set at p < .05 and Bonferroni corrected for multiple comparisons.
Our second aim was to test the association between anger rumination, RRBs and aggression. Thus, we examined zero-order correlations between ARS and other study variables using Pearson correlations. Next, a hierarchical multiple regression was conducted to assess the predictive utility of various potential predictors of anger rumination in five steps. First, gender was entered as a dichotomously coded variable (0 = boys and 1 = girls) to control for possible differences in gender. Next, diagnostic group was entered and dichotomously coded for ASD diagnosis (0 = no and 1 = yes) to understand potential contributions of ASD to anger rumination as well as to examine the interactions between diagnostic group, aggression, and RRBs in predicting anger rumination. In the third step, RPQ aggression total score was entered. In the fourth step, we added SRS-2 RRB subscale scores to examine the association between RRBs and rumination over and beyond other predictors. Finally, interactions were entered in the fifth step that included: ASD diagnosis × RPQ Aggression Total, and ASD diagnosis × SRS-2 RRB. Continuous variables were centered to the mean before creating these interaction terms. Alpha was set at p < .05 for the multiple regression analysis.
Results
Presentation of Anger Rumination
Our hypotheses centered on differences in anger rumination in children with ASD (n = 63) compared to children with disruptive behavior disorder without ASD (n = 79) and HC participants. Results of a one-way ANOVA conducted across the three groups (ASD vs. DB vs. HC) revealed that there was a significant difference in anger rumination (F2, 183 = 8.0, p = .001). Post hoc tests revealed that children with ASD showed significantly greater levels of anger rumination relative to HC children (p = .02), but similar levels of anger rumination as the DB group (p = .54) (see Table 2 and Fig. 1). Children in the DB group showed greater levels of anger rumination relative to HC participants (p < .001).
Fig. 1.
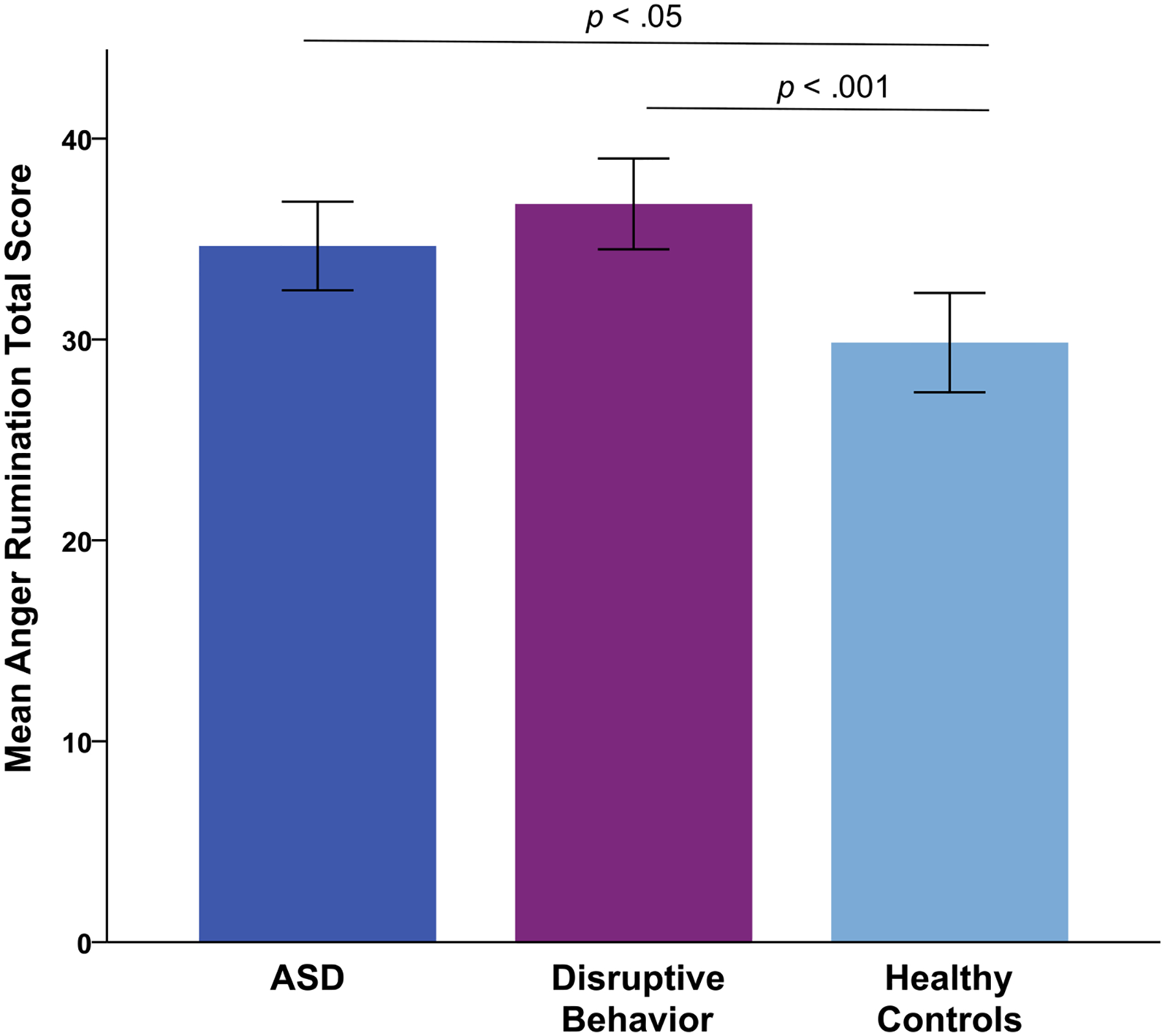
Mean levels of anger rumination across the combined ASD group in comparison to children with disruptive behavior disorders without ASD and healthy controls. Children with ASD (n = 63) showed greater levels of anger rumination relative to healthy control children (n = 44). However, levels of anger rumination were similar between children with ASD and children with disruptive behavior disorders without ASD (n = 79). The figure shows mean anger rumination scale total scores (y-axis). Disruptive behavior group refers to children with disruptive behavior disorders without ASD. Standard error is represented in error bars
We also examined differences in anger rumination in subgroups of children with ASD with and without co-occurring disruptive behavior. Planned post hoc tests were conducted after dividing the total sample of children with ASD into two subgroups based on the presence or absence of co-occurring disruptive behavior: ASD/DB+ (n = 22) and ASD/DB− (n = 41) groups, respectively. Independent samples t tests revealed that children with ASD/DB+ showed significantly greater levels of anger rumination relative to children with ASD/DB− (p = .03) (Table 2).
We also report between-group differences for the ARS subscales for descriptive purposes. Results of one-way ANOVAs revealed significant differences between the three groups for angry afterthoughts (F2, 183 = 7.2, p = .001), thoughts of revenge (F2, 183 = 5.14, p = .007), angry memories (F2, 183 = 5.68, p = .004), and understanding causes (F2, 183 = 3.31, p = .039) (see Table 2). Post hoc tests revealed that children with ASD showed levels of angry afterthoughts that were similar to the DB group (p > .5), but significantly greater than the HC group (p = .01). Children with ASD did not differ significantly from the HC group for thoughts of revenge, angry memories, and understanding causes scales. However, the DB group showed significantly greater levels of angry afterthoughts, thoughts of revenge, angry memories, and understanding causes relative to the HC group (all p < .03). The effect size η2 for these comparisons varied from 0.04 to 0.08, which can be interpreted as small to medium effects.
Correlations Between Study Variables
In the total sample of participants (N = 186), anger rumination yielded significant positive correlations with RRBs and aggression (Table 3). There were no significant correlations between anger rumination and age, gender, or full-scale IQ. In the sample of children with ASD (n = 63), anger rumination was positively correlated with RRBs. For the DB group (n = 79), there were no significant correlations between anger rumination and other variables. Correlations between anger rumination and predictors did not exceed .37, suggesting low risks of multicollinearity.
Table 3.
Correlations of anger rumination with demographic and clinical characteristics
| Assessment variable | Age | Gender | IQ | SRS-2 SCI | SRS-2 RRB | RPQ aggression total |
|---|---|---|---|---|---|---|
| Anger rumination scale total score | ||||||
| All participants (n = 186) | 0.01 | − 0.11 | − 0.11 | 0.13 | 0.16* | 0.22** |
| ASD group (n = 63) | 0.09 | − 0.15 | − 0.06 | 0.08 | 0.37** | 0.21 |
| Disruptive behavior group (n = 79) | 0.03 | − 0.08 | − 0.04 | − 0.09 | − 0.15 | − 0.14 |
Significant correlations are indicated in bold. Correlations are presented for the combined ASD group. Disruptive behavior group refers to children with disruptive behavior disorder without ASD.
p < .05,
p < .01
ASD, autism spectrum disorder group combined; RPQ, reactive–proactive aggression questionnaire; SRS-2 RRB, social responsiveness scale-second edition restricted and repetitive behaviors scale; SRS-2 SCI, social responsiveness scale-second edition social communication interaction scale
Multiple Regression Analyses
We then tested whether anger rumination was associated with aggression and RRBs. Using a dimensional approach, a multiple regression analysis was conducted across the total sample (N = 186). Model results from the multiple regression analysis are presented in Table 4. Step 1 indicated that child gender did not significantly predict anger rumination. In Step 2, ASD diagnosis did not predict anger rumination. In Step 3, aggression made a significant independent contribution to the model predicting anger rumination. Further, adding aggression into the model in Step 3 significantly increased the proportion of explained variance (R2 change .04, p = .003) from .1 to 4%. Step 4 showed that RRBs did not significantly predict anger rumination over and beyond other variables and aggression did not remain a significant predictor. Importantly, Step 5 showed that aggression and the interaction between ASD diagnosis and RRBs contributed significantly to the prediction of anger rumination. That is, for children with ASD, high levels of RRBs were related to high levels of anger rumination, but not for children without ASD (Fig. 2). The interaction between ASD diagnosis and aggression did not contribute significantly to the model predicting anger rumination. Note, controlling for age and IQ did not alter the results. The final model accounted for 5.6% of the variance in anger rumination.
Table 4.
Hierarchical regression results predicting anger rumination in the total sample
| Variable | B | SE B | β | p |
|---|---|---|---|---|
| Step 1. F1,184 = 2.27, p = .134; adjusted R2= .007, R2 change = .01, p = .134 | ||||
| Constant | 35.09 | 0.83 | ||
| Gender | − 2.28 | 1.52 | − 0.11 | .134 |
| Step 2. F2,183 = 1.14 p = .322; adjusted R2= .001, R2 change = 0, p = .886 | ||||
| Constant | 35.01 | 0.99 | ||
| Gender | − 2.27 | 1.52 | − 0.11 | .139 |
| ASD diagnosis | 0.21 | 1.48 | 0.01 | .886 |
| Step 3. F3,182 = 3.83, p = .011; adjusted R2= .044, R2 change = .047, p = .003 | ||||
| Constant | 34.69 | 0.98 | ||
| Gender | − 2.07 | 1.49 | − 0.10 | .169 |
| ASD diagnosis | 0.97 | 1.47 | 0.05 | .509 |
| RPQ aggression total score | 0.22 | 0.07 | 0.22 | .003 |
| Step 4. F4,181 = 3.04, p = .019; adjusted R2= .042, R2 change = .004, p = .412 | ||||
| Constant | 35.13 | 1.11 | ||
| Gender | − 2.01 | 1.499 | − 0.09 | .181 |
| ASD diagnosis | − 0.37 | 2.194 | − 0.02 | .867 |
| RPQ aggression total score | 0.17 | 0.09 | 0.17 | .073 |
| SRS-2 RRB score | 0.11 | 0.13 | 0.09 | .412 |
| Step 5. F6,179 = 2.82, p = .012; adjusted R2= .056, R2 change = .023, p = .106 | ||||
| Constant | 34.24 | 1.18 | ||
| Gender | − 2.08 | 1.49 | − 0.10 | .165 |
| ASD diagnosis | − 2.46 | 2.41 | − 0.12 | .308 |
| RPQ aggression total score | 0.27 | 0.11 | 0.27 | .016 |
| SRS-2 RRB score | − 0.12 | 0.17 | − 0.09 | .511 |
| ASD diagnosis × RPQ aggression total score | − 0.29 | 0.22 | − 0.15 | .174 |
| ASD diagnosis × SRS-2 RRB score | 0.60 | 0.28 | 0.32 | .034 |
Significant results are indicated in bold. ASD diagnosis variable represents children in the total sample with a diagnosis of ASD based on the ADOS-2 and ADI-R. Continuous variables are centered to the mean
ASD, autism spectrum disorder; RPQ, reactive–proactive aggression questionnaire; SRS-2 RRB, social responsiveness scale-second edition restricted and repetitive behaviors scale
Fig. 2.
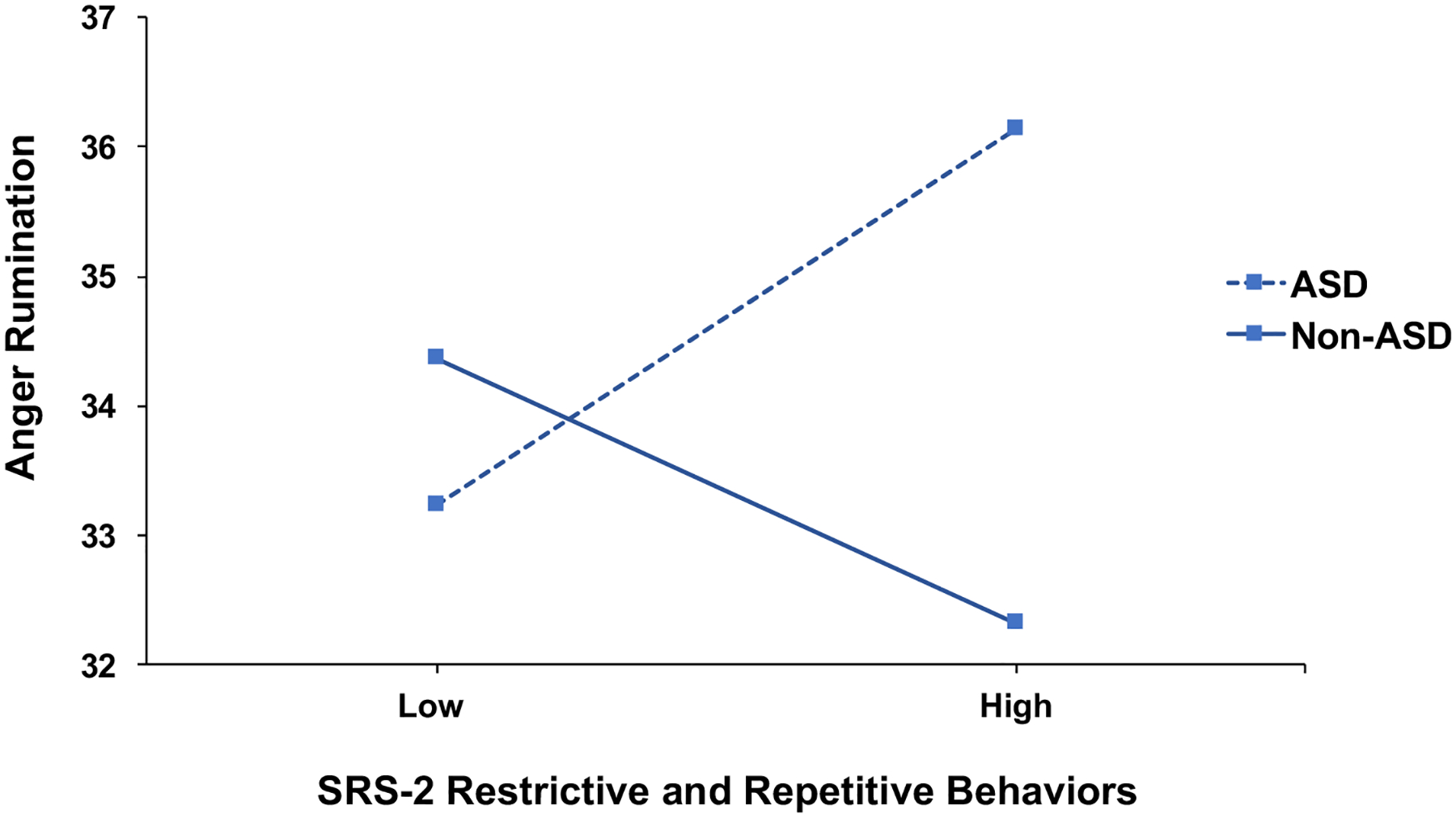
Interaction between ASD diagnosis and restricted and repetitive behaviors is associated with anger rumination in the total sample (N = 186). Restrictive and repetitive behaviors are measured using the social responsiveness scale-second edition (SRS-2) restricted and repetitive behaviors scale. Anger rumination is measured using the Anger Rumination Scale total score. The model controls for gender, aggression using the reactive–proactive aggression questionnaire total score, and the interaction between ASD diagnosis and aggression. High and low levels of restrictive and repetitive behaviors were dichotomized using a median split for visualization purposes. The total sample of participants includes children with ASD (n = 63), children with disruptive behavior disorder without ASD (n = 79), and healthy controls (n = 44)
To further explore the association between RRBs and aggression in predicting anger rumination in children with ASD, an additional linear regression restricted to children with ASD (n = 63) was conducted modeling RRBs and aggression simultaneously. RRBs (β = .48, p = .017), but not aggression (β = − .03, p = .87), was found to be a significant predictor of anger rumination across the sample of children with ASD (Fig. 3).
Fig. 3.
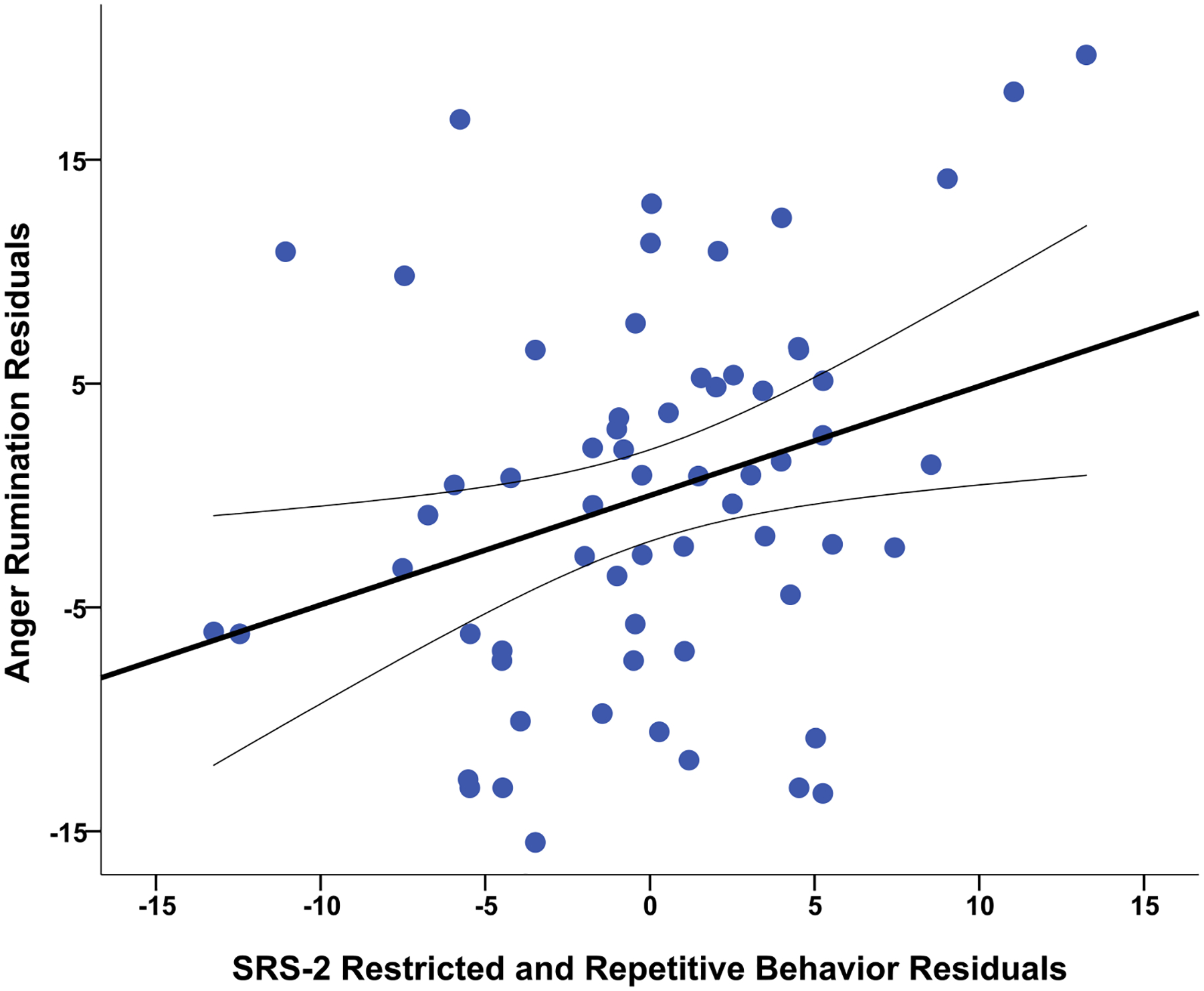
Results of a linear regression across the combined ASD group (n = 63). The residual plot shows the association between anger rumination and restricted, repetitive behaviors (RRBs) across the ASD group when both the social responsiveness scale-second edition RRB score and reactive–proactive aggression questionnaire total score were modelled simultaneously while controlling for gender. The anger rumination scale total score is used for analyses
Discussion
In the current study, we investigated anger rumination and its association with disruptive behavior and core ASD symptoms of RRBs in children with ASD. To our knowledge, this is the first study to examine anger rumination in well-characterized samples of children with ASD with varying levels of disruptive behaviors compared to children with disruptive behavior disorders without ASD. The primary aim of the study was to test if levels of anger rumination differed between children with and without ASD and co-occurring disruptive behavior and HC participants. Consistent with our expectations, children with ASD showed significantly greater levels of anger rumination relative to HC children. Our finding of greater rumination in the ASD group relative to the HC group is consistent with earlier studies (Crane et al. 2011; Gotham et al. 2014; Patel et al. 2017), which could suggest a greater tendency to engage in maladaptive cognitive regulatory patterns in ASD (Mazefsky et al. 2014). Alternatively, greater levels of rumination in the ASD group could also indicate that rumination is related to core ASD symptoms of RRBs such as perseveration, rigidity of thought, and insistence on sameness (Mazefsky et al. 2012). Our findings of greater anger rumination in the DB group compared to HC participants is consistent with studies in non-ASD populations that report associations between rumination and disruptive behaviors (Harmon et al. 2017; McLaughlin et al. 2014; Pugliese et al. 2015; Smith et al. 2016; Sukhodolsky et al. 2001). Additionally, levels of anger rumination were similar between the ASD and DB groups, which may suggest a shared underlying mechanism of emotion impairments across disorders. Further, these findings of similar patterns of rumination between clinically distinct disorders (ASD and DB groups) may lend support to rumination as a transdiagnostic process common across disorders (Aldao et al. 2016). Interestingly, the ASD/DB+ subgroup showed greater levels of anger rumination compared to the ASD/DB− subgroup, which is consistent with studies of non-ASD populations indicating higher anger rumination in youth with disruptive behavior disorders (Harmon et al. 2017; Smith et al. 2016). However, future studies with larger samples of children with ASD with and without co-occurring disruptive behavior disorders should examine anger-focused rumination to disentangle the overlap of ASD symptoms and disruptive behaviors, which could contribute to identifying differences among subgroups of children with ASD. A better understanding of anger rumination in ASD may also support the development of clinical interventions targeting rumination through acquisition of adaptive emotion regulatory strategies and improving a broad range of symptoms, such as disruptive behaviors.
Our second aim was to test whether anger rumination was associated with aggression and RRBs. Using a regression-based approach to model aggressive behavior and RRBs dimensionally, we found that the interaction between ASD diagnosis and RRBs was significant in predicting anger rumination, suggesting that the presence of an ASD diagnosis and high levels of RRBs is related to anger rumination. This finding is consistent with studies reporting an association between rumination and ASD symptoms of RRBs such as insistence on sameness and perseveration (Gotham et al. 2014; Pugliese et al. 2015). However, a recent study of adults in the general population did not find an association between sadness-focused rumination and perseveration using a self-report measure of ASD symptoms (Keenan et al. 2017). Our finding of an association between anger rumination and RRBs in ASD is noteworthy because RRBs such as rigidity of thinking, insistence on sameness, and perseveration are part of the constellation of core ASD symptoms and could predispose children with ASD to engage in rumination through greater difficulty in disengaging from perseverative, ruminative thoughts focused on the stressor (Mazefsky et al. 2012). On the other hand, it is also possible that impairments in emotional reactivity and regulation coupled with RRBs in ASD may impede the use of adaptive and voluntary emotion regulation strategies such as cognitive reappraisal and problem solving (Jahromi et al. 2012; Mazefsky et al. 2013, 2014; Rieffe et al. 2011). However, given the correlational nature of our study, directionality and causality cannot be inferred from these associations.
While aggression was positively correlated with anger rumination in correlations in the total sample, the interaction between ASD diagnosis and aggression did not emerge as a significant predictor of anger rumination. It is possible that because the sample size was relatively small for children with ASD and co-occurring disruptive behavior (ASD/DB+ subgroup, n = 22) compared to the DB group (n = 79), our ASD sample could have been underpowered to detect effects of aggression and ASD diagnosis in the regression model. Alternatively, the lack of a significant interaction with diagnostic category may lend support to the use of a dimensional framework to understand the contributions of aggression and emotion dysregulation more broadly in predicting anger rumination in ASD (Ibrahim and Sukhodolsky 2018). However, a recent longitudinal study of rumination showed that the developmental trajectory of worry and rumination predicted increased levels of disruptive behaviors in children with ASD (Bos et al. 2018). It should be noted, however, that Bos et al. (2018) used a broad measure of rumination that assessed worry and the tendency to dwell on a problem, and the sample consisted of only boys. Given that emotion regulation impairments are common in ASD including reliance on involuntary maladaptive strategies such as suppression and rumination rather than adaptive emotion regulation processes such as cognitive reappraisal or problem solving (Mazefsky et al. 2014; Samson et al. 2015a, b), it is possible that the tendency to engage in anger rumination may be related to emotion dysregulation in ASD. Further, the overlap between anger rumination, emotion dysregulation, and RRBs could predispose children with ASD to a heightened risk for disruptive behaviors. However, causal conclusions cannot be made based on the cross-sectional design of the current study. Future studies with larger samples and longitudinal designs are needed to dissociate the role of disruptive behaviors, particularly aggression, in predicting anger rumination in children with ASD.
The present study has limitations that should be considered when interpreting these findings. First, the sample size of the ASD/DB+ subgroup was small, particularly relative to the ASD/DB− subgroup. However, the total sample of children with ASD was well-matched on age, IQ and gender with the DB and HC groups. There were also no significant differences in age, IQ, or gender between the ASD/DB+ and ASD/DB− subgroups. Nonetheless, replication of results with larger samples is needed. In addition, our sample was not sufficiently powered for a more nuanced analysis of anger rumination between the ASD/DB+ and DB without ASD groups. An exploratory post hoc test indicated no significant difference in levels of anger rumination between the ASD/DB+ and DB groups (p = .628), but it is possible that anger rumination may have different underlying mechanisms in different diagnostic groups. Thus, studies are needed with larger samples sufficiently powered to compare anger rumination in children with ASD/DB+ to children with disruptive behavior disorders without ASD to understand the overlap between core ASD symptoms and disruptive behaviors in predicting anger rumination. Further, our sample did not include children with trauma or posttraumatic stress disorder (PTSD). Given the increased prevalence of trauma in children with ASD (Haruvi-Lamdan et al. 2017; Kerns et al. 2015) and the role that rumination may play in strengthening the association between PTSD symptoms and anger (Olatunji et al. 2010; Orth et al. 2008; Spinhoven et al. 2015), future studies are needed that examine the effects of co-occurring trauma in ASD, such as maltreatment and bullying, and its relationship with anger rumination and core ASD symptoms. Second, we used a cross-sectional design, which limits the capacity to assess directionality in the associations between study variables or predictability. Future studies using longitudinal designs will be important to understand anger rumination and its associations with other correlates, such as measures of emotion control. Third, the strength of correlations between the study variables was weak and the final regression model predicted 5% of the variance in anger rumination. This suggests that additional factors should also be explored as predictors of anger rumination in children with ASD such as other clinical and demographic factors. Additionally, this study focused on anger-related rumination and it will important for future studies to investigate potential positive emotion-focused cognitive processing such as reminiscence (Elias et al. 2015; Meléndez Moral et al. 2015; Westerhof et al. 2010) and recall of positive autobiographical memories (Gadeikis et al. 2017; Kovacs et al. 2015) in ASD. Future studies may examine whether perseverative tendencies of individuals with ASD may be associated with or could be deployed in interventions for anxiety and depression that are focused on recall of positive autobiographic memories. Finally, this study consisted of predominately boys and it will be important to understand gender differences and anger rumination in girls with ASD.
In conclusion, anger rumination in children with ASD was associated with RRBs. To our knowledge, the current study is the first to investigate anger rumination and its association with RRBs in a clinical sample of children with ASD relative to children with disruptive behavior disorders. Children with ASD showed greater levels of anger rumination relative to HC children, but similar levels to a clinical comparison group of children with disruptive behavior disorders without ASD. In addition, we examined anger rumination between subgroups of children with ASD/DB+ and ASD/DB−, which is a first step in understanding the correlates of rumination in distinct clinical subgroups of children with ASD. Children with ASD/DB+ showed higher levels of anger rumination compared to children with ASD/DB−, which could indicate distinct underlying mechanisms of rumination in children with ASD and co-occurring disruptive behavior. Further, a greater tendency to engage in rumination in ASD could be related to emotion regulation impairments and may confer a greater risk of disruptive behaviors. Therefore, a better understanding of rumination in ASD could support the development of novel clinical interventions as well as inform existing treatments to address negatively valenced rumination.
Acknowledgments
This work was supported by NIMH Grant R01MH101514 (D.G.S.) and NICHD Grant R01HD083881 (D.G.S.). K.I. and C.K. are Fellows of the Translational Developmental Neuroscience Training Program (T32 MH18268) directed by Dr. Michael Crowley. We thank Drs. Pamela Ventola and Megan Tudor for subject characterization assessments, and Ms. Emilie Bertschinger and Ms. Tess Gladstone for study coordination.
Footnotes
Conflict of interest Dr. Sukhodolsky receives royalties from Guilford Press for a treatment manual on CBT for anger and aggression in children. Other authors (K.I., C.K., C.L.M., A.A., L.G., and K.C.) have no biomedical financial interests or potential conflicts of interest to declare related to this present study.
Ethical Approval All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent Informed consent was obtained from all individual participants included in the study.
Publisher’s Note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Achenbach TM, & Rescorla LA (2001). Manual for the ASEBA school-age forms & profiles. Burlington, VT: University of Ver-mont, Research Center for Children, Youth, and Families. [Google Scholar]
- Aldao A, Gee DG, De Los Reyes A, & Seager I (2016). Emotion regulation as a transdiagnostic factor in the development of internalizing and externalizing psychopathology: Current and future directions. Development and Psychopathology, 28, 927–946. 10.1017/s0954579416000638. [DOI] [PubMed] [Google Scholar]
- Aldao A, Nolen-Hoeksema S, & Schweizer S (2010). Emotion-regulation strategies across psychopathology: A meta-analytic review. Clinical Psychology Review, 30, 217–237. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author. [Google Scholar]
- Bos MG, Diamantopoulou S, Stockmann L, Begeer S, & Rieffe C (2018). Emotion control predicts internalizing and externalizing behavior problems in boys with and without an autism spectrum disorder. Journal of Autism and Developmental Disorders, 48, 2727–2739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connor-Smith JK, Compas BE, Wadsworth ME, Thomsen AH, & Saltzman H (2000). Responses to stress in adolescence: Measurement of coping and involuntary stress responses. Journal of Consulting and Clinical Psychology, 68, 976. [PubMed] [Google Scholar]
- Constantino JN (2005). Social responsiveness scale (SRS). Los Angeles: Western Psychological Services. [Google Scholar]
- Crane L, Goddard L, & Pring L (2011). Autobiographical memory in adults with autism spectrum disorder: The role of depressed mood, rumination, working memory and theory of mind. Autism, 17, 205–219. 10.1177/1362361311418690. [DOI] [PubMed] [Google Scholar]
- Denson TF, Pedersen WC, Friese M, Hahm A, & Roberts L (2011). Understanding impulsive aggression: Angry rumination and reduced self-control capacity are mechanisms underlying the provocation-aggression relationship. Personality and Social Psychology Bulletin, 37, 850–862. [DOI] [PubMed] [Google Scholar]
- Elias SMS, Neville C, & Scott T (2015). The effectiveness of group reminiscence therapy for loneliness, anxiety and depression in older adults in long-term care: A systematic review. Geriatric Nursing, 36, 372–380. [DOI] [PubMed] [Google Scholar]
- Elliott CD (2007). The differential abilities scales, second edition (DAS-II). San Antonio, TX: Pearson Education Inc. [Google Scholar]
- Gadeikis D, Bos N, Schweizer S, Murphy F, & Dunn B (2017). Engaging in an experiential processing mode increases positive emotional response during recall of pleasant autobiographical memories. Behaviour Research and Therapy, 92, 68–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gotham K, Bishop SL, Brunwasser S, & Lord C (2014). Rumination and perceived impairment associated with depressive symptoms in a verbal adolescent–adult ASD sample. Autism Research, 7, 381–391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harmon SL, Stephens HF, Repper KK, Driscoll KA, & Kistner JA (2017). Children’s rumination to sadness and anger: Implications for the development of depression and aggression. Journal of Clinical Child & Adolescent Psychology. 10.1080/15374416.2017.1359788. [DOI] [PubMed] [Google Scholar]
- Haruvi-Lamdan N, Horesh D, & Golan O (2017). PTSD and autism spectrum disorder: Co-morbidity, gaps in research, and potential shared mechanisms. Psychological Trauma, 1, 1 10.1037/tra0000298. [DOI] [PubMed] [Google Scholar]
- Ibrahim K, & Sukhodolsky DG (2018). RDoC and autism In Volkmar F (Ed.), Encyclopedia of autism spectrum disorders. Mahwah, NJ: Springer. [Google Scholar]
- Jahromi LB, Meek SE, & Ober-Reynolds S (2012). Emotion regulation in the context of frustration in children with high functioning autism and their typical peers. Journal of Child Psychology and Psychiatry and Allied Disciplines, 53, 1250–1258. 10.1111/j.1469-7610.2012.02560.x. [DOI] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Axelson D, Perepletchikova F, Brent D, & Ryan N (2016). Schedule for affective disorders and schizophrenia for school aged children: Present and lifetime version for DSM-5 (K-SADS-PL). Retrieved from https://www.pediatricbipolar.pitt.edu/resources/instruments.
- Keenan EG, Gotham K, & Lerner MD (2017). Hooked on a feeling: Repetitive cognition and internalizing symptomatology in relation to autism spectrum symptomatology. Autism. 10.1177/1362361317709603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerns CM, Newschaffer CJ, & Berkowitz SJ (2015). Traumatic childhood events and autism spectrum disorder. Journal of Autism and Developmental Disorders, 45, 3475–3486. [DOI] [PubMed] [Google Scholar]
- Kovacs M, et al. (2015). Mood repair via attention refocusing or recall of positive autobiographical memories by adolescents with pediatric-onset major depression. Journal of Child Psychology and Psychiatry, 56, 1108–1117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Couteur A, Lord C, & Rutter M (2003). The autism diagnostic interview-revised (ADI-R). Los Angeles, CA: Western Psychological Services. [Google Scholar]
- Lecavalier L, et al. (2019). An exploration of concomitant psychiatric disorders in children with autism spectrum disorder. Comprehensive Psychiatry, 88, 57–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leyfer OT, et al. (2006). Comorbid psychiatric disorders in children with autism: Interview development and rates of disorders. Journal of Autism and Developmental Disorders, 36, 849–861. 10.1007/s10803-006-0123-0. [DOI] [PubMed] [Google Scholar]
- Lord C, Rutter M, DiLavore PC, & Risi S (2012). Autism diagnostic observation schedule—second edition (ADOS-2). Los Angeles, CA: Western Psychological Services. [Google Scholar]
- Mazefsky CA, Borue X, Day TN, & Minshew NJ (2014). Emotion regulation patterns in adolescents with high-functioning autism spectrum disorder: Comparison to typically developing adolescents and association with psychiatric symptoms. Autism Research, 7, 344–354. 10.1002/aur.1366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazefsky CA, Pelphrey KA, & Dahl RE (2012). The need for a broader approach to emotion regulation research in autism. Child Development Perspectives, 6, 92–97. 10.1111/j.1750-8606.2011.00229.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazefsky CA, & White SW (2014). Emotion regulation. Concepts & practice in autism spectrum disorder. Child and Adolescent Psychiatric Clinics of North America, 23, 15–24. 10.1016/j.chc.2013.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazefsky CA, et al. (2013). The role of emotion regulation in autism spectrum disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 52, 679–688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazurek MO, Kanne SM, & Wodka EL (2013). Physical aggression in children and adolescents with autism spectrum disorders. Research in Autism Spectrum Disorders, 7, 455–465. [Google Scholar]
- McLaughlin KA, Aldao A, Wisco BE, & Hilt LM (2014). Rumination as a transdiagnostic factor underlying transitions between internalizing symptoms and aggressive behavior in early adolescents. Journal of Abnormal Psychology, 123, 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meléndez Moral JC, Fortuna Terrero FB, Sales Galan A, & Mayordomo Rodríguez T (2015). Effect of integrative reminiscence therapy on depression, well-being, integrity, self-esteem, and life satisfaction in older adults. The Journal of Positive Psychology, 10, 240–247. [Google Scholar]
- Nolen-Hoeksema S (1991). Responses to depression and their effects on the duration of depressive episodes. Journal of Abnormal Psychology, 100, 569. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, & Watkins ER (2011). A heuristic for developing transdiagnostic models of psychopathology: Explaining multifinality and divergent trajectories. Perspectives on Psychological Science, 6, 589–609. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Wisco BE, & Lyubomirsky S (2008). Rethinking rumination. Perspectives on Psychological Science, 3, 400–424. [DOI] [PubMed] [Google Scholar]
- Olatunji BO, Ciesielski BG, & Tolin DF (2010). Fear and loathing: A meta-analytic review of the specificity of anger in PTSD. Behavior Therapy, 41, 93–105. [DOI] [PubMed] [Google Scholar]
- Orth U, Cahill SP, Foa EB, & Maercker A (2008). Anger and posttraumatic stress disorder symptoms in crime victims: A longitudinal analysis. Journal of Consulting and Clinical Psychology, 76, 208. [DOI] [PubMed] [Google Scholar]
- Patel S, Day TN, Jones N, & Mazefsky CA (2017). Association between anger rumination and autism symptom severity, depression symptoms, aggression, and general dysregulation in adolescents with autism spectrum disorder. Autism, 21, 181–189. 10.1177/1362361316633566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pouw LBC, Rieffe C, Stockmann L, & Gadow KD (2013). The link between emotion regulation, social functioning, and depression in boys with ASD. Research in Autism Spectrum Disorders, 7, 549–556. 10.1016/j.rasd.2013.01.002. [DOI] [Google Scholar]
- Pugliese CE, Fritz MS, & White SW (2015). The role of anger rumination and autism spectrum disorder-linked perseveration in the experience of aggression in the general population. Autism, 19, 704–712. 10.1177/1362361314548731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raine A, et al. (2006). The reactive–proactive aggression questionnaire: Differential correlates of reactive and proactive aggression in adolescent boys. Aggressive Behavior: Official Journal of the International Society for Research on Aggression, 32, 159–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rieffe C, Oosterveld P, Terwogt MM, Mootz S, van Leeuwen E, & Stockmann L (2011). Emotion regulation and internalizing symptoms in children with autism spectrum disorders. Autism, 15, 655–670. 10.1177/1362361310366571. [DOI] [PubMed] [Google Scholar]
- Samson AC, Hardan AY, Lee IA, Phillips JM, & Gross JJ (2015a). Maladaptive behavior in autism spectrum disorder: The role of emotion experience and emotion regulation. Journal of Autism and Developmental Disorders, 45, 3424–3432. 10.1007/s10803-015-2388-7. [DOI] [PubMed] [Google Scholar]
- Samson AC, Hardan AY, Podell RW, Phillips JM, & Gross JJ (2015b). Emotion regulation in children and adolescents with autism spectrum disorder. Autism Research, 8, 9–18. 10.1002/aur.1387. [DOI] [PubMed] [Google Scholar]
- Silverman WK, & Albano AM (1996). Anxiety disorders interview schedule for DSM-IV, Child Version. New York, NY: Oxford University Press. [Google Scholar]
- Simonoff E, Pickles A, Charman T, Chandler S, Loucas T, & Baird G (2008). Psychiatric disorders in children with autism spectrum disorders: Prevalence, comorbidity, and associated factors in a population-derived sample. Journal of the American Academy of Child and Adolescent Psychiatry, 47, 921–929. [DOI] [PubMed] [Google Scholar]
- Smith SD, Stephens HF, Repper K, & Kistner JA (2016). The relationship between anger rumination and aggression in typically developing children and high-risk adolescents. Journal of Psychopathology and Behavioral Assessment, 38, 515–527. [Google Scholar]
- Spinhoven P, Penninx BW, Krempeniou A, van Hemert AM, & Elzinga B (2015). Trait rumination predicts onset of post-traumatic stress disorder through trauma-related cognitive appraisals: A 4-year longitudinal study. Behaviour Research and Therapy, 71, 101–109. [DOI] [PubMed] [Google Scholar]
- Sukhodolsky DG, Golub A, & Cromwell EN (2001). Development and validation of the anger rumination scale. Personality and Individual Differences, 31, 689–700. [Google Scholar]
- Sukhodolsky DG, & Scahill L (2012). Cognitive-behavioral therapy for anger and aggression in children. New York: Guilford Press. [Google Scholar]
- Sukhodolsky DG, et al. (2008). Parent-rated anxiety symptoms in children with pervasive developmental disorders: Frequency and association with core autism symptoms and cognitive functioning. Journal of Abnormal Child Psychology, 36, 117–128. 10.1007/s10802-007-9165-9. [DOI] [PubMed] [Google Scholar]
- van Steensel FJ, Bogels SM, & de Bruin EI (2013). Psychiatric comorbidity in children with autism spectrum disorders: A comparison with children with ADHD. Journal of Child and Family Studies, 22, 368–376. 10.1007/s10826-012-9587-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler D (1997). WAIS-III administration and scoring manual. San Antonio, TX: The Psychological Corporation. [Google Scholar]
- Westerhof GJ, Bohlmeijer E, & Webster JD (2010). Reminiscence and mental health: A review of recent progress in theory, research and interventions. Ageing & Society, 30, 697–721. [Google Scholar]
- White BA, & Turner KA (2014). Anger rumination and effortful control: Mediation effects on reactive but not proactive aggression. Personality and Individual Differences, 56, 186–189. [Google Scholar]


