Abstract
Occlusion of both the limbs of accessory middle cerebral artery (AMCA) poses a unique challenge in management of acute ischaemic stroke by mechanical thrombectomy. The patient is a 30-year-old man, presenting with acute onset of left-sided hemiparesis for 4 hours. Non-contrast CT brain showed no bleed and three-dimensional CT angiogram of head and neck vessels showed dissection involving right carotid bulb and tandem occlusion of right MCA with presence of two MCA stumps. Aspiration thrombectomy was done using a reperfusion catheter, advanced separately into both the MCA stumps and complete recanalisation of both the limbs of MCAs was achieved, which was found to be AMCA. Balloon angioplasty for the internal carotid artery dissection was performed. Although occlusion of AMCA in acute ischaemic stroke is a chance occurrence, it is important to identify this variant as recanalisation of both the limbs by mechanical thrombectomy is required for favourable outcome after the procedure.
Keywords: stroke, interventional radiology
Background
Anterior circulation ischaemic stroke due to occlusion of M1 segment of middle cerebral artery (MCA) is very common. However, occlusion of both the limbs of accessory MCA (AMCA) in acute ischaemic stroke is extremely rare and only one case has been reported earlier in English literature.1 Additionally, the occlusion of duplicated MCA (DMCA) in acute ischaemic stroke has been reported in another case report earlier.2 Although this was a chance phenomenon, the presence of this anatomical variation can pose a significant challenge in management by mechanical thrombectomy. Here we report the management of one such challenging case and treatment options for such cases.
Case presentation
A 30-year-old man presented with complaints of acute onset of left hemiparesis for 4 hours. Patient was also having vague right-sided neck pain for 1 day after undergoing some chiropractic neck manipulations in local massage parlour. His previous medical history was otherwise unremarkable.
Investigations
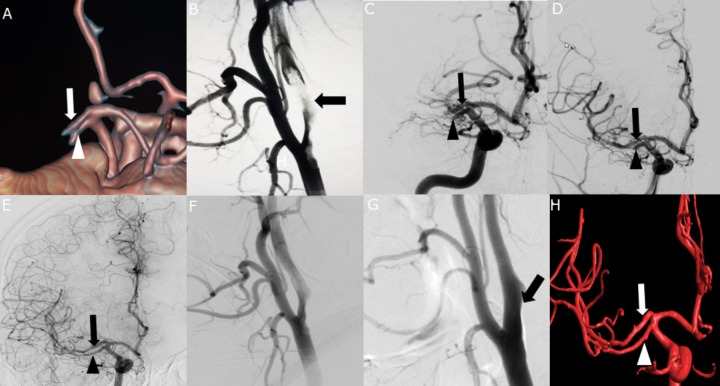
Non-contrast CT (NCCT) head showed few patchy hypodensities in right MCA territory with Alberta stroke programme early CT score (ASPECTS) of 7. CT angiogram (CTA) revealed dissection involving right carotid bulb and tandem occlusion of right AMCA with only the proximal stumps of the duplicated segments being visible (figure 1A).
Figure 1.
Coronal reformatted volume rendered CT angiogram image (A) showing occluded duplicated middle cerebral artery stump with arrow showing occluded superior limb and arrowhead showing occluded inferior limb. (B–G) Digital subtraction angiography images. (B) Right common carotid artery (CCA) injection, lateral projection showing dissection involving right carotid bulb (arrow). (C) Right internal carotid artery (ICA) injection showing occluded MCA stumps with arrow showing the occluded limb arising from anterior cerebral artery (ACA) (also giving rise to lenticulostriate vessels) and arrowhead showing other occluded limb arising from terminal ICA. (D) Right ICA injection after first pass showing recanalisation of the limb arising from proximal ACA (arrow) and occluded other limb (arrowhead) from terminal ICA. (E) Right ICA injection after two passes showing recanalisation of both the limbs of MCA. (F) Right CCA injection after balloon angioplasty showing significant opening up of right carotid bulb with residual thrombus. (G) Right CCA injection at 1 month showed near complete resolution of carotid bulb dissection with small residual contrast filled outpouching (arrow). (H) Reconstructed three-dimensional rotational angiogram at 1 month demonstrating completely recanalised MCA with presence of accessory MCA.
Treatment
Aspiration thrombectomy was planned with a triaxial approach after informed consent. Right femoral access was obtained and a 6F neuro-sheath, Neuron 088 Max (Penumbra, Oakland, California, USA), was placed into right common carotid artery (CCA), just proximal to the right carotid bulb dissection. The dissection flap was limited to right carotid bulb and proximal cervical internal carotid artery (ICA). A large bore aspiration catheter, ACE 60 reperfusion catheter (Penumbra), was advanced through the Neuron Max over a 035″, 150 cm Radifocus guidewire M (Terumo Medical Corporation, Tokyo, Japan) guidewire. The soft tip guidewire was used to cross the segment with carotid dissection (figure 1B) and the ACE 60 catheter was advanced into the true lumen in the distal cervical ICA over the wire. Diagnostic angiogram showed occluded right AMCA stump (figure 1C). Headway 27/Traxcess 14 (MicroVention, Tustin, California, USA) microcatheter/ microguidewire assembly was advanced through the ACE 60 catheter into the limb of AMCA arising from A1 segment of right anterior cerebral artery (ACA). and ACE 60 catheter was advanced over microcatheter/microguidewire assembly till the level of the clot. Thrombo-aspiration was performed with ACE 60 catheter using aspiration pump (Penumbra). After single pass, recanalisation of the AMCA limb arising from right A1 ACA was achieved (figure 1D). Similarly the procedure is repeated for limb of AMCA arising from ICA terminus. Check angiogram showed complete recanalisation of both the limbs of AMCA (figure 1E). Balloon angioplasty was performed for the dissected segment using a 6×20 mm Mustang percutaneous transluminal angioplasty (PTA) balloon dilation catheter (Boston Scientific, Natick, Massachusetts, USA) and significant opening of right carotid bulb was achieved with residual thrombus (figure 1F). Stenting was not done in acute phase because of excellent collaterals from posterior circulation and presence of insignificant right capsule-ganglionic haemorrhage on X-per CT. Patient was started on low molecular weight heparin and clopidogrel and was discharged after 4 days on aspirin and clopidogrel.
Outcome and follow-up
Patient was taken up for carotid stenting after 4 weeks. However, diagnostic angiogram performed during stenting showed near complete resolution of dissection with haemodynamically insignificant stenosis and no visible intimal flap (figure 1G). A small beak-like projection is seen at the level of right carotid bulb (figure 1G) which is likely to be sequel of previous dissection. Hence, stenting was not performed for the patient. Three-dimensional rotational angiography performed showed completely recanalised both the limbs of AMCA (figure 1H). At 3-month follow-up, patient had a Modified Rankin Score of 0.
Discussion
The MCA is phylogenetically youngest of all the cerebral vessels. In brief, phylogenetically far older ACA gives rise to MCA. Multiple perforating vessels arise from ACA to maintain supply to growing cerebrum in the initial stage of neocortical development.3 With the enlarging cortex, the perforator system also evolve from multiple competing channels into a single, dominant vessel—the MCA. MCA anomalies are relatively rare and are classified into various categories as accessory, duplicated, duplicated origin, fenestrated or twig-like.3 Crompton was the first to use the term AMCA, describing a vessel passing into the Sylvian fissure along with MCA.4 By this definition, it included both AMCA and DMCA. However, Teal et al proposed that the term AMCA should strictly be restricted to the anomalous artery arising from the ACA, while the branch arising from ICA to be termed DMCA.5 In angiographic and anatomical studies, AMCA and DMCA have been found to have an incidence of 0.3%–4.0% and 0.2%–2.9%, respectively.6 Several theories are in vogue regarding embryological origin of AMCA. Handa et al suggested AMCA represents hypertrophied recurrent artery of Heubner.7 Takahashi et al suggested that the AMCA may represent a persistent form of anastomotic channels between medial striate arteries from the ACA and lateral striate arteries from the MCA.8 Komiyama et al postulated that early ramification of early branches of MCA gives rise to AMCA or DMCA, because they have a consistent cortical supply through the AMCA and DMCA to the anterior frontal lobe and anterior temporal lobe, respectively.6 Although these MCA variations themselves bear no clinical significance, rare aneurysms have been reported at the origin of the AMCA or DMCA and are generally considered as chance occurrence.9 10
To the best of our knowledge, involvement of AMCA or DMCA in acute ischaemic stroke has been reported in one case each in English literature.1 2 Although this was a chance occurrence, it posed a significant challenge in management by mechanical thrombectomy. The presence of concomitant ICA dissection made the case more challenging. We decided to treat the case by direct aspiration first pass technique (ADAPT). For optimal results, it was necessary to remove clots from both the limbs of AMCA.
Although whether size of AMCA or DMCA is equal or less compared with size of single M1 MCA remains controversial,3 an aspiration catheter with lesser outer diameter was used to decrease the chance of vessel injury. The division of MCA arising from ACA measured ~2.2 mm while that arising from the ICA measured ~2.17 mm in our case. Of note, the left M1 MCA in the same patient measured 4.1 mm. The measurements are taken just after the origin of the respective vessels. Keeping in mind the relatively lesser size of the occluded vessel, ACE 60 catheter was used instead of ACE 68 catheter as the former has a distal outer diameter (OD) of 5.4 F (French) compared with distal OD of 6 F in the latter. Although the distal inner diameter (ID) was compromised (0.060″ vs 0.068″ in ACE 60 and ACE 68, respectively), this ensured optimum aspiration force and less chance of vascular injury during catheter navigation. Since the limb of MCA, arising from ACA, was giving rise to the lenticulostriate vessels (figure 1C), it was accessed first, followed by the other limb. This was done because recanalisation of the vessel giving rise to lenticulostriate branches is more crucial to achieve a good outcome. Complete recanalisation (mTICI score of 3) was achieved after single pass aspiration from each of the limbs.
Stent retriever thrombectomy could have been used also in the treatment of this case. However, aspiration was used as the first line of treatment because of potential endothelial injury by stent retriever. Koge et al described endothelial injury by stent retriever device in a case of DMCA occlusion with concomitant ICA occlusion and suggested aspiration thrombectomy in similar situation.2 The authors in that case however was not fortunate like us to know about the existence of potential anatomical variation as the vessels were entirely occluded in their case and retrospective diagnosis of variant anatomy was made by faint opacification of duplicated branch and lack of complete expansion of the stent retriever device in M1 MCA. In our case, as the stump of the both the limbs were visible, the existence of an anatomical variation was diagnosed prospectively and aspiration thrombectomy was chosen over stent retriever thrombectomy. Still we believe, stent retriever thrombectomy can be used as a bailout method in case aspiration thrombectomy fails to recanalise in similar situations. Koge et al have used a stent retriever of diameter 6 mm in their case.2 Hence, we recommend, if required, a stent retriever of smaller diameter (4 mm or less) should be used in similar situation to reduce the chances of vessel injury.
Learning points.
Accessory middle cerebral artery (MCA) occlusion poses a unique challenge in management of acute ischaemic stroke.
Although it is likely to be a chance association, neuro-interventionists should recognise this variation.
Complete recanalisation of both limbs of occluded MCA is essential for a favourable clinical outcome. It is important to recanalise the limb bearing lenticulostriate branches first as occlusion of the same likely to result in poorer prognosis.
Aspiration thrombectomy should be preferred over stent retriever to reduce chance of vessel injury.
A smaller diameter aspiration catheter or stent retriever is recommended in such situations to prevent potential vascular injuries.
Footnotes
Twitter: @DrNirmalyaRay
Contributors: NR and JD performed the case, designed the research and wrote the manuscript. SJ and LJ compiled the data and wrote the manuscript. All authors critically revised the manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Bayer-Karpinska A, Lutz J, Birnbaum T, et al. . Severe MCA stroke without MCA occlusion? Thrombectomy uncovers accessory middle cerebral artery. Neurology 2015;85:831–2. 10.1212/WNL.0000000000001894 [DOI] [PubMed] [Google Scholar]
- 2. Koge J, Kato S, Hashimoto T, et al. . Vessel wall injury after stent retriever thrombectomy for internal carotid artery occlusion with duplicated middle cerebral artery. World Neurosurg 2019;123:54–8. 10.1016/j.wneu.2018.11.223 [DOI] [PubMed] [Google Scholar]
- 3. Uchiyama N. Anomalies of the middle cerebral artery. Neurol Med Chir 2017;57:261–6. 10.2176/nmc.ra.2017-0043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Crompton MR. The pathology of ruptured middle-cerebral aneurysms with special reference to the differences between the sexes. Lancet 1962;2:421–5. 10.1016/S0140-6736(62)90281-7 [DOI] [PubMed] [Google Scholar]
- 5. Teal JS, Rumbaugh CL, Bergeron RT, et al. . Anomalies of the middle cerebral artery: accessory artery, duplication, and early bifurcation. Am J Roentgenol Radium Ther Nucl Med 1973;118:567–75. 10.2214/ajr.118.3.567 [DOI] [PubMed] [Google Scholar]
- 6. Komiyama M, Nakajima H, Nishikawa M, et al. . Middle cerebral artery variations: duplicated and accessory arteries. AJNR Am J Neuroradiol 1998;19:45–9. [PMC free article] [PubMed] [Google Scholar]
- 7. Handa J, Shimizu Y, Matsuda M, et al. . The accessory middle cerebral artery: report of further two cases. Clin Radiol 1970;21:415–6. 10.1016/S0009-9260(70)80084-8 [DOI] [PubMed] [Google Scholar]
- 8. Takahashi S, Hoshino F, Uemura K, et al. . Accessory middle cerebral artery: is it a variant form of the recurrent artery of Heubner? AJNR Am J Neuroradiol 1989;10:563–8. [PMC free article] [PubMed] [Google Scholar]
- 9. Nomura M, Tamase A, Kamide T, et al. . Accessory middle cerebral artery associated with an unruptured aneurysm at its origin. Surg Neurol Int 2015;6:421–3. 10.4103/2152-7806.166179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ren H, Ma L, Wei M, et al. . Duplicated middle cerebral artery origin with an aneurysm. Medicine 2018;97:e9947 10.1097/MD.0000000000009947 [DOI] [PMC free article] [PubMed] [Google Scholar]