Abstract
Osteomas are bone tumours arising from the cortical or medullary bones of craniofacial skeleton. Involvement of frontal bone and paranasal sinuses is more frequent than jaw bones. Jaw osteomas are slow growing benign lesions, which are usually asymptomatic or present as painless swelling. Those involving mandibular condyle are relatively rare and result in significant functional and aesthetic disturbances. This paper reports a case of solitary central compact osteoma of mandibular condyle in an adult Indian female patient. A comprehensive review of previously published reports is also presented.
Keywords: dentistry and oral medicine, surgery, oral and maxillofacial surgery
Background
Osteomas are rare benign bone neoplasm characterised by abnormal proliferation of mature bone, which can be compact or cancellous in nature. They may arise from the cortical bone and are called peripheral osteoma. While those developing from the endosteal bone are termed as central osteoma.1 Multiple osteomas are present as a part of Gardner’s syndrome. Non-syndromic cases are usually isolated and are called solitary osteomas.
Osteomas are invariably restricted to craniofacial bones, and commonly involve the paranasal sinuses and jaw bone. Mandible is more frequently involved than maxilla. In mandible, the most common sites are the angle and lower border.1 Osteoma of mandibular condyle is relatively rare and was first reported by Ivy.2 Although jaw osteomas are slow growing benign lesions, those involving the condyle often produce significant functional and aesthetic disturbances. The purpose of this paper is to report a case of solitary central compact osteoma involving the mandibular condyle in an elderly Indian woman. The lesion presented as bony hard painless swelling in preauricular area, causing reduced mouth opening. The paper also presents a comprehensive review of English literature to identify 28 previously reported cases of osteoma of condyle and discuss them in relation to our experience.
Case presentation
A 65-year-old Indian woman presented to maxillofacial surgery clinic with chief complaint of progressive inability to open mouth since past 4 years. No history of trauma to face, ear infection or other systemic disease was reported. On extraoral examination, a localised swelling over the right preauricular region measuring about 2.5 cm was noticed (figure 1A). The swelling was non-tender and bony hard in consistency. The overlying skin was normal and pinchable over the lesion. There was no temporomandibular joint movement bilaterally on palpation. Mouth opening was significantly restricted with maximum interincisal opening of 3 mm (figure 1B). Intraoral examination showed poor oral hygiene with multiple periodontally involved teeth. Orthopantomogram revealed a well-defined round homogeneous radiopaque mass involving right condyle (figure 2A). Sectional CT of the right condyle showed complete replacement of the condyle anatomy with a hyperdense oval mass measuring 3×2.5 cm (figure 2B). The normal trabecular pattern was replaced with sclerotic bone.
Figure 1.

Photograph showing localised preauricular swelling (A) and restricted mouth opening (B).
Figure 2.
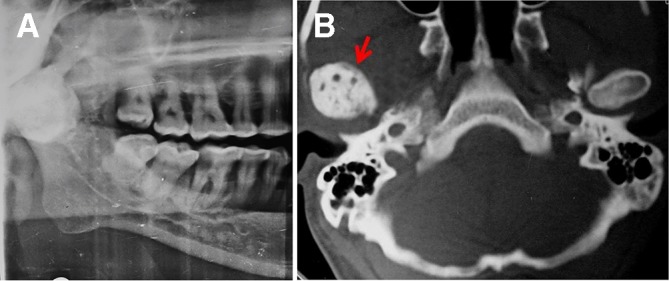
Orthopantomogram showing radiopaque lesion involving right condyle (A); CT revealing the hyperdense lesion replacing the condylar head (arrow head) (B).
Differential diagnosis
Based on the history, clinical features and radiological finding, a working diagnosis of central osteoma of condyle was made.
Treatment
Condylectomy for removal of the pathology was carried out under general anaesthesia, using preauricular approach. The excised lesion was submitted for histological evaluation. Microscopic study of the specimen showed mature lamellar compact bone with scanty marrow spaces (figure 3). Based on the clinical presentation, imaging characteristics and histological findings, a final diagnosis of solitary central compact osteoma of mandibular condyle was established.
Figure 3.
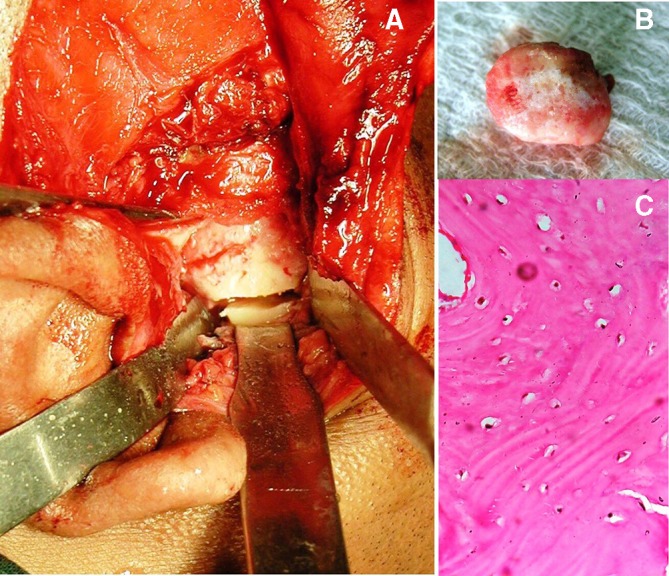
Intraoperative image showing exposure of lesion with preauricular incision and osteotomy cut placed for condylectomy (A), excised mass (B). Photomicrograph showing dense compact bone with osteocytes (×40 magnification) (C).
Outcome and follow-up
Due to the financial constraint, prosthetic joint was not chosen for reconstruction. Postoperatively, the patient was put on arch bar with guiding elastics to correct the deviation on mouth opening and stabilise the occlusion. Period of active physiotherapy and traction guided occlusion was followed for 3 months following with the patient showed stable occlusion and mouth opening. Presently the patient is kept on routine long-term follow-up protocol.
Discussion
Osteomas are benign osteogenic lesion characterised by formation of mature bone. It almost exclusively involves craniofacial skeleton, with frontal bone and paranasal sinus being the preferred sites. Other bones involved include the temporal bone, orbit, external auditory canal pterygoid bone and jaw.3 Osteoma of the mandibular condyle has been infrequently reported. Search of English literature from PubMed database, using terms osteoma, solitary, mandible and condyle, revealed 11 titles. References of these papers were comprehensively evaluated and a total of 28 papers (31 cases) of osteoma of mandibular condyle were identified. These papers were reviewed for demographic details, aetiology, clinical presentation, location, type, histological characteristic and treatment provided (table 1).2 4–30
Table 1.
Review of solitary osteoma involving condyle
| No | Author; year | Country | Age/sex | Trauma history | Clinical presentation | Side | Location | Type | Size (mm) | Pathological variant | Treatment |
| 1 | Ivy; 19272 | ||||||||||
| Case 1 | USA | 35/F | _ | Swelling, deviation of the chin, malocclusion. | Right | Condyle head | NA | 30 | NA | Condylectomy | |
| Case 2 | USA | 27/F | Facial asymmetry, malocclusion | Left | Condyle head | NA | NA | NA | Condylectomy | ||
| 2 | Worman; 19464 | NA | 24/F | Inability to open mouth, malocclusion | Left | Condyle head | C | 30 | Ca | Condylectomy | |
| 3 | Miles; 19515 | NA | 40/F | NA | Swelling | Left | Condyle head | NA | NA | Co | NA |
| 4 | Thoma; 19546 | USA | 37/M | NA | Swelling, facial asymmetry, pain, difficulty in opening mouth | Left | Condyle head | C | 40 | Ca | Condylectomy |
| 5 | Nelson; 19727 | NA | 49/M | + | Swelling | Right | Anteriomedial aspect of condyle | P | 30 | Co | Excision |
| 6 | MacLennan; 19748 | UK | 31/F | _ | Pain, swelling, facial asymmetry, deviation of jaw, malocclusion. | Left | Subcondyle and vertical ramus | P | 50 | Co | Subcondylectomy |
| 7 | Nwoku; 19749 | Germany | 34/F | NA | Facial asymmetry, malocclusion | Right | Condyle head | NA | NA | NA | Subcondylectomy |
| 8 | Wang-Norderud; 197610 | Egypt | 35/M | _ | Facial asymmetry, mandibular prognathism | Left | Anteriomedial aspect of condyle | P | 40 | Ca | Condylectomy |
| 9 | Weinberg; 197711 | NA | 31/M | _ | Malocclusion | Left | Condyle head | NA | 30 | Ca | Condylectomy |
| 10 | Seymour; 198112 | UK | 70/M | NA | Difficulty in eating, facial asymmetry, deviation of chin | Right | Condyle head | NA | NA | NA | Excision |
| 11 | Papavasiliou; 198313 | UK | 74/F | _ | Severe pain, trismus, preauricular swelling | Left | Condyle head and neck | P | 18 | Co | Condylectomy |
| 12 | Bessho; 198714 | Japan | 26/M | + | Painless swelling | Right | Mandibular notch | P | 34 | Co | Excision |
| 13 | Kondoh; 199815 | Japan | 40/M | NA | Malocclusion, facial asymmetry, difficulty in opening mouth | Left | Medial pole of condyle | P | 40 | Co | Excision |
| 14 | Sayan; 200216 | Turkey | NA/F | NA | NA | Left | Condyle head | P | Na | NA | NA |
| 15 | Siar; 200417 | Malaysia | 32/F | NA | Progressive painless restriction of mouth opening | Left | Neck of condyle | P | 48 | Ca | Condylectomy |
| 16 | Mancini; 200518 | Brazil | 19/M | NA | Facial asymmetry, chin deviation, malocclusion | Right | Condyle head | NA | 28 | Co | Condylectomy |
| 17 | Ortakoğlu; 200519 | Turkey | 22/M | NA | Mandibular deviation, malocclusion | NA | NA | NA | NA | NA | Condylectomy |
| 18 | Woldenberg; 200520 | Israel | 46/F | NA | Pain | Left | Condyle, coronoid notch, ascending ramus | P | 25 | NA | NA |
| 19 | Yonezu; 200721 | Japan | 50/M | NA | Diffuse swelling, pain, limited mouth opening | Left | Lateral surface of condyle head | P | NA | Ca | Excision |
| 20 | Cogburn; 200822 | USA | 22/M | _ | Malocclusion, truisms, inability to chew | Left | Anterior surface of condyle | P | NA | NA | Endoscopic excision and recontouring |
| 21 | Nah; 201123 | ||||||||||
| Case 1 | Korea | 29/F | NA | NA | NA | Anterior surface of condyle head | P | NA | NA | NA | |
| Case 2 | Korea | 44/F | NA | Difficulty in chewing | Left | Anterior surface of condyle head | p | NA | NA | NA | |
| Case 3 | Korea | 56/F | NA | Difficulty in chewing | Left | Anterior surface of condyle head | p | NA | NA | NA | |
| 22 | Chaurasia; 201224 | India | 45/F | NA | Swelling, facial asymmetry | Left | Condyle neck | P | 22 | NA | Conservative |
| 23 | Misra; 201325 | India | 22/M | _ | Difficulty in mouth opening | Left | Condyle, sigmoid noctch, glenoid fossa | C | 32 | Co | Condylectomy |
| 24 | Kashid; 201326 | India | 48/M | NA | Deviation of jaw, inability to chew, altered occlusion, facial asymmetry, swelling | Left | Anteromedial aspect of condyle | P | NA | Ca | Condylectomy |
| 25 | Rajshekar et al; 201527 | India | 35/M | + | Reduced mouth opening, | Right | Condyle head | C | 30 | NA | Condylectomy |
| 26 | Zafar; 201628 | Pakistan | 60/M | _ | Pain on mastication, deviation of lower jaw, facial asymmetry, maloclusion | Right | Condyle head | C | 30 | Co | Condylectomy |
| 27 | de Souza; 201729 | Brazil | 67/F | _ | Pain. Limited mouth opening, aesthetic disturbance | Right | Condyle head | C | 20 | Co | Condylectomy with TMJ reconstruction |
| 28 | Ostrofsky 201930 | South Africa | 60/M | + | Deviated opening, facial asymmetry | Left | Medial condyle pole | C | 30 | Ca | Condyletomy with TMJ reconstruction |
-, negative history of trauma; +, positive history of trauma; C, central; Ca, cancellous; Co, cortical; F, female; M, male; NA, data not available; P, peripheral; TMJ, temporomandibular joint.
Three theories have been proposed to explain the pathogenesis of osteoma, developmental, neoplastic and reactive.31 The developmental theory suggests osteoma to be a developmental anomaly or an end stage of a hamartomatous process like fibrous dysplasia. However, it is unlikely that osteomas are developmental disorder as it is rarely seen in young age group. In the review of cases of condylar osteoma, the mean age was 38.67, with youngest individual being 19 years of age.18 Males were more frequently affected than females in ratio of 2:1. Although osteomas are largely considered to be benign neoplasm, some authors believe it to be a reactive response to trauma or infection. Trauma as a precursor to the pathology is supported by the fact that in mandible, the most common sites are the angle and lower border which are susceptible to injury. Condyle is another region, which is exposed to trauma from direct injury or an indirect blow at chin or body of mandible. Positive history of trauma was reported in 4 out of 29 cases of osteoma of condyle (13.78%). No history of trauma could be elicited in the present case. Although the association of trauma with osteoma of condyle appears to be low, it can be due to the fact that it was ignored during history recording or the event may not be significant to be remembered by the patient, giving a false negative result. The location of mandibular osteomas in proximity to areas of muscle attachment, that is, masseter and medial pterygoid (lower border and angle of mandible) suggests that muscle traction along with trauma may play a role in its development. Condyle is susceptible to injury and is under traction of lateral pterygoid muscle, which may be the underlying factor for development of osteoma in this region. Some of the reported cases suggest that middle ear infection may stimulate an inflammatory hyperplasia and overgrowth of the condyle.13
Osteomas are slow growing lesion. It may be an incidental finding on radiograph or present as asymptomatic swelling. Symptoms depend on the site involved. Osteomas of paranasal sinus cause sinusitis, headache and ophthalmological manifestations.23 Unlike mandibular osteoma which is asymptomatic or causes painless swelling, those involving condyle cause noticeable functional and aesthetic disturbances. The clinical features include preauricular swelling, restriction or inability of mouth opening, malocclusion and mandibular prognathism with deviation of chin to the contralateral side. Reduced mouth opening with localised bony swelling in preauricular area was the presenting features of the current case. However, no occlusal discrepancy was noted.
Osteoma may arise from the medullary bone (central type). As the lesion grows the proliferating mass almost entirely replaces the normal anatomy of condyle. Whereas peripheral osteoma presents as localised pedunculated or mushroom like projections for the cortex. Peripheral osteomas of condyle (76%) are almost three times more common than the central variant (24%). Condyle head is by far most commonly involved site, followed by neck, sigmoid notch and ascending ramus. Left condyle was more frequently affected (70% cases). The size of lesion ranged from 18 to 50 mm. In the present case, the right condyle was entirely replaced by central lesion forming an oval radiodense mass measuring 30 mm. Although bone scan is not indicated in every case, when preformed it helps to study the physiologic activity of osteoma. It determines whether it is a long-standing lesion with no further growth potential or actively growing mass. Bone scintigraphy performed to evaluate condylar osteoma by Sayan et al and Siar et al showed increased uptake of technetium (99mTc) radioisotope at the involved site.16 17 Histologically osteoma is composed of mature lamellar bone with minimal marrow space (compact osteoma) or with fibrofatty marrow tissue (cancellous osteoma). Microscopic study of the present case showed compact bone having mature lamellae with scanty marrow. Nine of the previously reported case of condylar osteoma was compact while seven were cancellous in nature.
Management of craniofacial osteoma is indicated only for large symptomatic lesions. Osteoma involving condyle produces functional and morphological changes in temporomandibular joint early in its development, leading to progressive shift of occlusion with deviation of mandible to unaffected side. Large lesion leads to mechanical restriction of normal joint movements, resulting in trismus and pain. Surgical intervention is commonly indicated for condylar osteoma to relieve the symptoms and prevent its progression. Condylectomy and surgical excision of the bony mass are the two most commonly reported procedures. Use of costochondral graft for reconstruction after resection of osteoma was reported in young patient by Mancini et al.18 Preauricular incision with its modifications is the approach of choice to surgically access the pathology. Cogburn et al performed excision of osteoma with recontouring of condyle using endoscopy assisted intraoral approach, thus avoiding preauricular scar.22
Osteoma of mandibular condyle is rare bony pathology commonly seen in adults. Unlike craniofacial osteoma, these lesions frequently cause functional and aesthetic disturbance. As the mass grows, it results in progressive restriction of mouth opening and should be considered as possible cause of trismus. Condyle head is most preferred site, with peripheral variant arising from the cortical bone being more common. Condylectomy or surgical excision of the mass in the most commonly reported treatment.
Learning points.
Osteomas are benign bone tumours, which arise either from the cortex or medulla. In head and neck region, it frequently involves frontal bone and paranasal sinuses.
Those involving mandibular condyle are relatively rare and result in significant functional and aesthetic disturbances.
This paper describes a case of solitary central compact osteoma of mandible condyle with its management.
A comprehensive review of English literature for osteoma of mandible condyle in terms of demographic details, aetiology, clinical presentation, location, type, histological characteristic and treatment provided is discussed.
Footnotes
Contributors: KN was involved in the concept, design, literature search, data acquisition, manuscript preparation, review and editing. AV was involved in literature search and manuscript preparation. SR was involved in final drafting of manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Nilesh K, Bhujbal RB, Nayak AG. Solitary central osteoma of mandible in a geriatric patient: report and review. J Clin Exp Dent 2016;8:e219–22. 10.4317/jced.52792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ivy RH. Benign bony enlargement of the condyloid process of the mandible. Ann Surg 1927;85:27–30. 10.1097/00000658-192701000-00002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Nilesh K, V Vande A, K Veerabhadrappa S. Solitary peripheral ivory osteoma of the mandible presenting with difficulty in deglutition: a case report. J Dent Res Dent Clin Dent Prospects 2017;11:56–60. 10.15171/joddd.2017.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Worman HG, Waldron CW, Radusch DF. Osteoma of the mandibular condyle with deviation prognathic deformity. J Oral Surg 1946;4:27. [PubMed] [Google Scholar]
- 5. Miles AEW. The use of the biopsy drill and punch in the diagnosis of oral lesions. Br Dent J 1951;91:7–10. [PubMed] [Google Scholar]
- 6. Thoma KH. Tumors of the condyle and temporomandibular joint. Oral Surg Oral Med Oral Pathol 1954;7:1091–107. 10.1016/0030-4220(54)90220-0 [DOI] [PubMed] [Google Scholar]
- 7. Nelson DF, Gross BD, Miller FE. Osteoma of the mandibular condyle: report of case. J Oral Surg 1972;30:761. [PubMed] [Google Scholar]
- 8. MacLennan WD, Brown RD. Osteoma of the mandible. Br J Oral Surg 1974;12:219–24. 10.1016/0007-117X(74)90128-0 [DOI] [PubMed] [Google Scholar]
- 9. Nwoku AL, Koch H. The temporomandibular joint: a rare localisation for bone tumours. J Maxillofac Surg 1974;2:113–9. 10.1016/S0301-0503(74)80025-1 [DOI] [PubMed] [Google Scholar]
- 10. Wang-Norderud R, Ragab RR. Osteoma of the mandibular Condyloid process. Scand J Plast Reconstr Surg 1976;10:77–81. 10.3109/02844317609169750 [DOI] [PubMed] [Google Scholar]
- 11. Weinberg S. Osteoma of the mandibular condyle: report of case. J Oral Surg 1977;35:929–32. [PubMed] [Google Scholar]
- 12. Seymour RA. Osteoma of the condyle. Oral Surg Oral Med Oral Pathol 1981;52:223 10.1016/0030-4220(81)90325-X [DOI] [PubMed] [Google Scholar]
- 13. Papavasiliou A, Sawyer R, Lund V, et al. Benign conditions of the temporomandibular joint: a diagnostic dilemma. Br J Oral Surg 1983;21:222–8. 10.1016/0007-117X(83)90046-X [DOI] [PubMed] [Google Scholar]
- 14. Bessho K, Murakami K, Iizuka T, et al. Osteoma in mandibular condyle. Int J Oral Maxillofac Surg 1987;16:372–5. 10.1016/S0901-5027(87)80162-5 [DOI] [PubMed] [Google Scholar]
- 15. Kondoh T, Seto K, Kobayashi K. Osteoma of the mandibular condyle: report of a case with a review of the literature. J Oral Maxillofac Surg 1998;56:972–9. 10.1016/S0278-2391(98)90661-9 [DOI] [PubMed] [Google Scholar]
- 16. Sayan NB, Uçok C, Karasu HA, et al. Peripheral osteoma of the oral and maxillofacial region: a study of 35 new cases. J Oral Maxillofac Surg 2002;60:1299–301. 10.1053/joms.2002.35727 [DOI] [PubMed] [Google Scholar]
- 17. Siar C-H, Jalil AA, Ram S, et al. Osteoma of the condyle as the cause of limited-mouth opening: a case report. J Oral Sci 2004;46:51–3. 10.2334/josnusd.46.51 [DOI] [PubMed] [Google Scholar]
- 18. Mancini JCMA, Woltmann M, Felix VB, et al. Peripheral osteoma of the mandibular condyle. Int J Oral Maxillofac Surg 2005;34:92–3. 10.1016/j.ijom.2004.01.028 [DOI] [PubMed] [Google Scholar]
- 19. Ortakoğlu K, Gunaydin Y, Aydintug YS, et al. Osteoma of the mandibular condyle: report of a case with 5-year follow-up. Mil Med 2005;170:117–20. [PubMed] [Google Scholar]
- 20. Woldenberg Y, Nash M, Bodner L. Peripheral osteoma of the maxillofacial region. diagnosis and management: a study of 14 cases. Med Oral Patol Oral Cir Bucal 2005;10(Suppl 2):E139–42. [PubMed] [Google Scholar]
- 21. Yonezu H, Wakoh M, Otonari T, et al. Osteoma of mandibular condyle as cause of acute pain and limited-mouth-opening: case report. Bull Tokyo Dent Coll 2007;48:193–7. 10.2209/tdcpublication.48.193 [DOI] [PubMed] [Google Scholar]
- 22. Cogburn AC, Hales N, Krempl GA. Endoscopic resection of a mandibular condyle osteoma: report of a case. Laryngoscope 2008;118:1214–6. 10.1097/MLG.0b013e318171514d [DOI] [PubMed] [Google Scholar]
- 23. Nah K-S. Osteomas of the craniofacial region. Imaging Sci Dent 2011;41:107–13. 10.5624/isd.2011.41.3.107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Chaurasia A. An unusual osseous lesion of mandibular condyle. J Orofac Res 2012;2:174–7. 10.5005/jp-journals-10026-1036 [DOI] [Google Scholar]
- 25. Misra N, Srivastava S, Bodade PR, et al. Osteoma of temporomandibular joint: a rarity. BMJ Case Rep 2013;2013:bcr2013200268 10.1136/bcr-2013-200268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. L. Kashid A, S.P. K, KumbharE SP. Osteoma of mandibular condyle - a rare entity. J Evol Med Dent Sci 2013;2:5286–92. 10.14260/jemds/982 [DOI] [Google Scholar]
- 27. Rajshekar V, Basetty N, Govindaraju R, et al. "Out of the ordinary": A case report of osteoma of mandibular condyle. J Indian Acad Oral Med Radiol 2015;27:441–4. 10.4103/0972-1363.170490 [DOI] [Google Scholar]
- 28. Zafar E, Akbar Z, Niazi K, et al. Osteoma of mandibular condyle-a case report. Pakistan Oral Dent J 2016;36:383–6. [Google Scholar]
- 29. de Souza NT, Cavalcante RCL, de Albuquerque Cavalcante MA, et al. An unusual osteoma in the mandibular condyle and the successful replacement of the temporomandibular joint with a custom-made prosthesis: a case report. BMC Res Notes 2017;10:727 10.1186/s13104-017-3060-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Ostrofsky M, Morkel JA, Titinchi F. Osteoma of the mandibular condyle: a rare case report and review of the literature. J Stomatol Oral Maxillofac Surg 2019;120:584–7. 10.1016/j.jormas.2019.01.013 [DOI] [PubMed] [Google Scholar]
- 31. Regezi JA, Sciubba J, Oral Pathology. Vol. 407 edn 2 Philadelphia: Saunders, 1993. [Google Scholar]


