Abstract
Background
Systemic lupus erythematous (SLE) disproportionately impacts patients of color and socioeconomically disadvantaged patients. Similar disparities in HIV were reduced through a World Health Organization-endorsed Care Continuum strategy targeting “retention in care,” defined as having at least two annual visits or viral load lab tests. Using similar definitions, this study aimed to examine predictors of lupus retention in care, to develop an SLE Care Continuum and inform interventions to reduce disparities. We hypothesized that Black patients and those residing in disadvantaged neighborhoods would have lower retention in care.
Methods
Abstractors manually validated 545 potential adult cases with SLE codes in 2013–2014 using 1997 American College of Rheumatology (ACR) or 2012 Systemic Lupus Erythematosus International Collaborating Clinics (SLICC) criteria. We identified 397 SLE patients who met ACR or SLICC criteria for definite lupus, had at least one baseline rheumatology visit, and were alive through 2015. Retention in care was defined as having two ambulatory rheumatology visits or SLE labs (e.g., complement tests) during the outcome year 2015, analogous to HIV retention definitions. Explanatory variables included age, sex, race, ethnicity, smoking status, neighborhood area deprivation index (ADI), number of SLE criteria, and nephritis. We used multivariable logistic regression to test our hypothesis and model predictors of SLE retention in care.
Results
Among 397 SLE patients, 91% were female, 56% White, 39% Black, and 5% Hispanic. Notably, 51% of Black versus 5% of White SLE patients resided in the most disadvantaged ADI neighborhood quartile. Overall, 60% met visit-defined retention and 27% met complement lab-defined retention in 2015. Retention was 59% lower for patients in the most disadvantaged neighborhood quartile (adjusted OR 0.41, CI 0.18, 0.93). No statistical difference was seen based on age, sex, race, or ethnicity. More SLE criteria and non-smoking predicted greater retention.
Conclusions
Disadvantaged neighborhood residence was the strongest factor predicting poor SLE retention in care. Future interventions could geo-target disadvantaged neighborhoods and design retention programs with vulnerable populations to improve retention in care and reduce SLE outcome disparities.
Keywords: Systemic lupus erythematosus, Health disparities, Social determinants of health, Retention in care, Health care quality
Background
Systemic lupus erythematosus (SLE) is an autoimmune disease that disproportionately impacts young women, patients of color, and the socioeconomically disadvantaged, making SLE an important target for health disparity measurement and research [1]. Despite many effective lupus monitoring strategies and treatments [2, 3], significant healthcare disparities and outcome gaps remain [4–6]. Compared to White women, the US Black women are up to seven times more likely to develop renal failure, and two to three times as likely to die prematurely [4, 7]. SLE is also a leading chronic disease cause of death in the US women ages 18–25 [8]. Arguing against a purely biological mechanism, higher SLE damage was noted in the US African descendants but not in other African descendants in ten other countries in the SLICC cohort [9]. High-quality clinical care can reduce risk for many poor lupus outcomes [10, 11]. Yet, some data suggest that Black or low SES patients with milder onset SLE are more likely to ultimately die of their disease, suggesting that differences in healthcare follow-up might be to blame [7, 12].
Human immunodeficiency virus (HIV), which also disproportionately impacts young, Black, and socioeconomically disadvantaged populations, is an analogous condition where healthcare gaps have been targeted as a means by which to reduce disparities. As a framework, experts at the World Health Organization (WHO) [13], US Institute of Medicine (IOM) [14], and Centers for Disease Control and Prevention (CDC) [15] have defined an “HIV Care Continuum” outlining five critical healthcare steps to achieve successful viral suppression. The Care Continuum offers standard definitions to measure gaps at each step from (1) diagnosis to (2) linkage with specialty HIV care, (3) retention in care, and (4) retention on antiretroviral therapy, and finally to (5) control with suppressed HIV viral loads [16]. Using this continuum, HIV researchers determined that gaps in retention in care account for most (61%) failures to control HIV [16]. Moreover, continuum research has led to a compendium of evidence-based interventions [15] to close gaps at each step including many interventions to improve retention in HIV care. A similar approach holds promise for improving disparities in SLE. As such, we proposed an SLE Care Continuum from (1) diagnosis to (2) linkage with specialty lupus care, (3) retention in care, (4) retention on immune therapy, and finally (5) low lupus disease activity (Fig. 1). In this study, we first focus on predictors of retention in care.
Fig. 1.
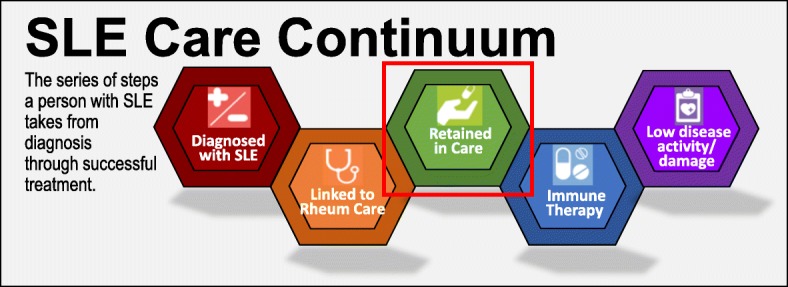
Proposed SLE Care Continuum adapted with permission from the HIV.gov Care Continuum
Rheumatologists often observe that keeping some lupus patients, particularly young, Black, or socioeconomically disadvantaged lupus patients [17], in follow-up care is a challenge, yet no metrics exist to identify who is or is not retained in lupus care. In HIV, retention in care is defined by WHO [13] and CDC [15] experts as having two annual HIV visits or one viral load every 6 months. Creating such metrics was pivotal for identifying gaps and testing strategies to reduce HIV health disparities [15]. Despite an urgent need to reduce SLE disparities and known concerns regarding retention, we have no established methods to measure gaps in retention in care or other disparities across an SLE Care Continuum.
We were particularly interested in investigating relationships between race, socioeconomic disadvantage, and retention in lupus care in this cohort [18]. Black patients and the socioeconomically disadvantaged are more likely to reside in disadvantaged US neighborhoods, which are linked to high disease rates and mortality offering geographic targets for policy, practice change, and research [19, 20].
We hypothesized that Black patients and those residing in highly disadvantaged neighborhoods would have lower retention in care because of the multitude of socioeconomic, access, and other adverse social determinants of health that such residents face [21–23]. The objectives of this study were to validate an urban lupus cohort, to create metrics for retention in care, and to examine how race and other social determinants of health predict lupus retention in care. Defining lupus retention in care and its predictors are key steps toward designing future interventions to improve retention and reduce lupus outcome disparities.
Methods
Inclusion and study population
For this cohort study, we first searched all Jan 2013–June 2014 electronic health records (EHR) at an urban US academic center for all inpatient or outpatient visits with the International Classification of Diseases ninth or tenth edition (ICD-9 or 10) codes representing possible SLE [ICD-9 710.0 or ICD-10 M32, M32.1, M32.8, M32.9]. Inclusion required being age 18 or over, living through 2015 to assure eligibility for retention in care, and having at least one ambulatory visit in rheumatology [physician (MD, DO), nurse practitioner (NP), physician assistant (PA), resident, or fellow] and one in primary care (family medicine, internal medicine, geriatrics, obstetrics and gynecology, or pediatrics) in 2013–2014 to assure equal capture of baseline comorbidity and healthcare utilization information and follow-up. Recognizing that not all patients with lupus diagnosis codes meet clinical criteria, trained health professionals manually validated all potential SLE cases using a standard REDCap abstraction tool to assess the 1997-modified 1982 American College of Rheumatology (ACR) classification criteria and 2012 Systemic Lupus Collaborating Clinics (SLICC) SLE classification criteria [24]. Laboratory, pathology, imaging, and clinical note data were reviewed for all patients with possible lupus. Those with drug-induced lupus or not meeting either definite classification of SLE were excluded. All patients meeting either the 1997 ACR or 2012 SLICC SLE classification criteria and other inclusion criteria were included in the study. Patients were followed from the study start date of their first lupus diagnosis code, through death, or the end of 2015 as a study end date. Data elements for each individual were linked via a unique pseudo identifier, and direct identifiers were removed for a final limited dataset for analysis.
The Institutional Review Board approved of this minimal risk medical record review study with a waiver of individual informed consent and use of a limited dataset.
Data sources
In addition to manually abstracted items, EHR data were electronically extracted for definite SLE cases including (1) patient-level sociodemographic variables (age, sex, race, ethnicity, rural-urban commuting area (RUCA) classification, date of death), (2) visit-level information (all rheumatology encounter dates and all encounter ICD codes), and (3) select laboratory data (e.g., C3/C4 complement and anti-double-stranded DNA antibody testing dates). In addition to SLE classification criteria, sociodemographic and behavioral factors also reviewed during manual abstraction were nine-digit ZIP postal code and smoking history. Disease severity was noted using the number of SLE criteria, and a history of lupus nephritis was also manually validated.
Outcome definitions for lupus retention in care
EHR dates of rheumatology visits attended and complete blood count (CBC), creatinine anti-double-stranded DNA (dsDNA), or C3 or C4 complement tests during the calendar year 2015 were used to test potential retention definitions. Thresholds of one, two, or four visits or complement or dsDNA lab tests were compared. We focused on two visit-defined and two lab-defined SLE retention in care in those without nephritis analogous to HIV definitions and consistent with guidelines for nephritis screening and quality measures [2, 11]. We also tested a four lab-defined threshold consistent with SLE guidelines for those with lupus nephritis [2, 3]. Non-specific tests such as complete blood counts and creatinine were tested but not used as final definitions as they may be ordered by other providers for other non-SLE reasons and may not indicate lupus retention in care. Tests such as urinalyses, while important to most lupus care, were avoided given that SLE patients on dialysis may forgo such testing or have results at external dialysis centers and thus not present in EHR data.
Predictors and covariates
Consistent with the National Institute of Minority Health and Health Disparities research framework [21], multilevel predictors of interest included individual-level age, sex, race, ethnicity, and smoking status, and ZIP code linked contextual-level rural urban (RUCA) classification, and neighborhood disadvantage quartile. We used the Area Deprivation Index (ADI), a neighborhood disadvantage metric encompassing 17 education, employment, housing quality, transportation, and poverty measures to match from 69 million nine-digit ZIP postal code census block groups, i.e., “neighborhoods” of approximately 1500 people [19, 20, 25]. Twenty-five patients were missing residential ADI data and were excluded from multivariable modeling. The number of ACR criteria and any history of nephritis were included as markers of lupus severity.
Statistical analysis
Baseline lupus cohort characteristics were presented as frequencies and proportions for the overall and the cohort stratified by race. Differences between proportions were examined by the chi-square test. Retention rates during the 2015 period were calculated as percent of eligible patients meeting visit or laboratory testing definitions. We also examined definitions specific to guideline-recommended lab frequencies for those with lupus nephritis [2, 12]. Next, to determine predictors of retention, univariate and multivariable logistic regression analyses were performed, and results are presented as odds ratios (ORs) along with 95% confidence intervals (CIs). Potential interactions between ADI neighborhood disadvantage and other covariates (e.g., race or ethnicity) were tested as sensitivity analyses. We a priori estimated 80% power to detect an odds ratio of 0.60 if retention in care is 65% in White compared to 53% in Black patients using a two-sided Z test, significance level 0.05, similar to a 15% reported race gap in medication adherence [26]. Analyses were completed using SAS version 9.4 (Cary, NC) and STATA version 13.1 (College Station, TX).
Results
Cohort description
Of 528 abstracted potential lupus cases, 397 patients met ACR or SLICC classification criteria for definite lupus and were included in our study (Fig. 2). Among definite lupus patients, 91% were female, 39% Black, 5% Other, and 4% Hispanic (see Table 1).
Fig. 2.
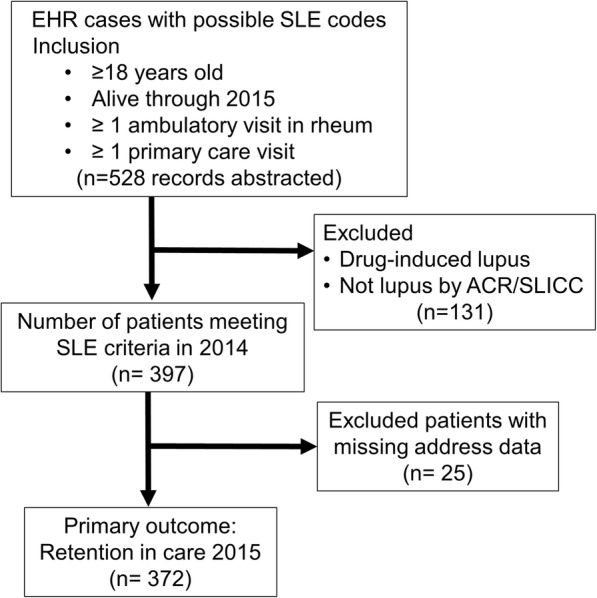
Flow diagram of project design and inclusion
Table 1.
Prevalent systemic lupus erythematosus cohort description (n = 397)
| Total cohort | White/other | Black | p | |
|---|---|---|---|---|
| n = 397 | n = 241 | n = 156 | ||
| Age category | ||||
| 18–29 | 54 (13.6%) | 30 (12.5%) | 24 (15.4%) | < 0.001 |
| 30–40 | 96 (24.2%) | 50 (20.8%) | 46 (29.5%) | |
| 40–60 | 175 (44.1%) | 102 (42.3%) | 73 (46.8%) | |
| 60–80 | 67 (16.9%) | 56 (23.2%) | 11 (7.1%) | |
| 80+ | 5 (1.3%) | 3 (1.2%) | 2 (1.3%) | |
| Female | 361 (90.9%) | 219 (90.9%) | 142 (91.0%) | 0.96 |
| Race | ||||
| White | 221 (55.7%) | 221 (91.7%) | NA | < 0.001 |
| Black | 156 (39.3%) | NA | 156 (100%) | |
| Other | 20 (5.0%) | 20 (8.3%) | NA | |
| Ethnicity | ||||
| Hispanic | 17 (4.3%) | 16 (6.6%) | 2 (1.3%) | 0.01 |
| RUCA | ||||
| Urban | 329 (82.9%) | 175 (72.6%) | 154 (98.7%) | < 0.001 |
| Suburban | 36 (9.1%) | 36 (14.9%) | 0 (0%) | |
| Large town | 15 (3.8%) | 14 (5.8%) | 1 (0.6%) | |
| Small town | 17 (4.3%) | 16 (6.6%) | 1 (0.6%) | |
| Smoking (ever) | 168 (42.3%) | 103 (43%) | 65 (42%) | 0.60 |
| Payer | ||||
| Commercial | 176 (44.3%) | 139 (57.7%) | 37 (23.7%) | < 0.001 |
| Medicaid | 71 (17.9%) | 24 (10.0%) | 47 (30.1%) | |
| Medicare | 142 (35.8%) | 72 (29.9%) | 70 (44.9%) | |
| Uninsured/unknown | 8 (2.0%) | 6 (2.5%) | 2 (0.06%) | |
| Neighborhood disadvantage by ADI quartile | ||||
| 1st (least disadvantage) | 93 (25.0%) | 83 (34.4%) | 10 (6.4%) | < 0.001 |
| 2nd | 93 (25.0%) | 78 (32.4%) | 15 (9.6%) | |
| 3rd | 93 (25.0%) | 54 (22.4%) | 39 (25.0%) | |
| 4th (most disadvantage) | 93 (25.0%) | 13 (5.4%) | 80 (51.3%) | |
| Positive ACR criteria | 365 (91.9%) | 210 (87.1%) | 148 (94.9%) | 0.02 |
Compared to White patients with lupus, Black patients were younger, more likely to reside in urban areas, and 10 times more likely to reside in a neighborhood within the most disadvantaged quartile (51% Blacks vs. 5% Whites). Black patients were also more likely to meet ACR SLE criteria (95% vs. 87%). Payer varied significantly by race (75% of Black versus 40% of White patients received public insurance), and only 2% of patients were uninsured or had unknown payer status.
Testing retention definitions
When examining definitions of lupus retention in care, we first examined visit-based definitions similar to those employed in HIV. Overall, as shown in Table 2, 83% (n = 331) of eligible lupus patients had at least one ambulatory rheumatology visit in 2015, and 60% (n = 238) had at least two visits. This was comparable to 74% with two or more visits in the baseline year 2014 (data not shown).
Table 2.
Examining visit- and lab-defined retention in care thresholds in SLE cases with and without nephritis (n = 397)
| All SLE | Lupus nephritis | p | ||||
|---|---|---|---|---|---|---|
| n = 397 | n = 145 | |||||
| Definition | Interval | n | % | n | % | |
| Visit definitions | ||||||
| Rh visits | ≥ 1/year | 331 | 83 | 120 | 83 | 0.802 |
| *Rh visits | ≥ 2/year | 238 | 60 | 96 | 66 | 0.054 |
| Rh visits | ≥ 4/year | 79 | 20 | 46 | 32 | < 0.001 |
| Lab definitions | ||||||
| C3/C4 | ≥ 1/year | 184 | 46 | 78 | 54 | 0.024 |
| *C3/C4 | ≥ 2/year | 106 | 27 | 49 | 34 | 0.015 |
| C3/C4 | ≥ 4/year | 30 | 8 | 20 | 14 | < 0.001 |
| CBC | ≥ 1/year | 213 | 54 | 90 | 62 | 0.011 |
| CBC | ≥ 2/year | 159 | 40 | 72 | 50 | 0.001 |
| CBC | ≥ 4/year | 93 | 23 | 52 | 36 | 0.003 |
| Creatinine | ≥ 1/year | 211 | 53 | 89 | 61 | 0.013 |
| Creatinine | ≥ 2/year | 163 | 41 | 74 | 51 | 0.002 |
| Creatinine | ≥ 4/year | 92 | 23 | 49 | 34 | < 0.001 |
| dsDNA | ≥ 1/year | 149 | 38 | 67 | 46 | 0.007 |
| dsDNA | ≥ 2/year | 77 | 19 | 39 | 27 | 0.004 |
| dsDNA | ≥ 4/year | 18 | 5 | 12 | 8 | 0.007 |
Abbreviations: Rh rheumatology MD, DO, NP, PA, or fellow; C3/C4 complement component 3 or 4 lab tests which were each independently assessed yielding identical results that are shown together; CBC complete blood counts; dsDNA double-stranded DNA antibody test
*Final models used two visits and at least two labs per year consistent with WHO/CDC HIV definitions and ACR SLE guidelines
When testing lab-defined retention in care, we sequentially examined C3 and C4 complement, CBC, creatinine, and anti-dsDNA testing (Table 2). In 2015 follow-up, 54% of patients had at least one CBC and 46% of patients had at least one complement result recorded in the EHR. Only 27% and 41% had two annual complement and creatinine tests, respectively, compared to 43% with at least two complement tests in the 2014 baseline year (data not shown). Any single anti-dsDNA result was available on only 29% of the cohort during 2015, with only 19% having two dsDNA tests, leading us to operationalize the equally specific two complement test definition for lab-defined lupus retention in care for multivariable modeling although other definitions could be assessed in future studies.
Predictors of lupus retention in care
In adjusted multivariable models, residing in the neighborhood quartile with worst disadvantage was the strongest predictor of lower retention in care, predicting nearly 60% lower odds (OR 0.41, CI 0.18, 0.93; Table 3). Smoking likewise significantly predicted lower visit-defined retention in care (OR 0.63, 0.40, 0.99). Neither Black race nor Hispanic ethnicity was predictive of lupus retention in care.
Table 3.
Predictors of two visit-defined lupus retention in care (n = 372, multivariable analysis included 372 of 397 SLE patients with complete data)
| Unadjusted OR (95% CI) | Adjusted OR (95% Cl) | |
|---|---|---|
| Age | ||
| 18–29 | Ref | Ref |
| 30–40 | 0.95 (0.47, 1.93) | 0.81 (0.36, 1.81) |
| 40–60 | 0.65 (0.34, 1.24) | 0.65 (0.31, 1.36) |
| 60–80 | 0.62 (0.29, 1.30) | 0.71 (0.30, 1.68) |
| 80+ | 0.75 (0.11, 4.90) | 1.15 (0.11, 12.38) |
| Female | 0.73 (0.35, 1.50) | 0.50 (0.22, 1.12) |
| Race | ||
| White | Ref | Ref |
| Black | 1.24 (0.81, 1.89) | 1.56 (0.81, 3.03) |
| Other | 0.71 (0.29, 1.78) | 0.98 (0.29, 3.33) |
| Ethnicity (Hispanic) | 0.52 (0.20, 1.34) | 0.63 (0.18, 2.28) |
| RUCA | ||
| Urban | Ref | Ref |
| Suburban | 1.03 (0.51, 2.08) | 1.19 (0.54, 2.65) |
| Large town | 1.31 (0.44, 3.91) | 1.12 (0.33, 3.88) |
| Small town | 0.46 (0.17, 1.23) | 0.41 (0.14, 1.23) |
| Ever Smoking | 0.63 (0.42, 0.95) | 0.63 (0.40, 0.99) |
| Payer | ||
| Commercial | Ref | |
| Medicaid | 0.72 (0.41, 1.25) | |
| Medicare | 1.25 (0.79, 1.98) | |
| Neighborhood disadvantage by ADI | ||
| 1st (least disadvantage) | Ref | Ref |
| 2nd quartile | 1.05 (0.58, 1.88) | 1.02 (0.55 (1.92) |
| 3rd quartile | 1.26 (0.69, 2.29) | 1.01 (0.52, 2.00) |
| 4th (most disadvantage) | 0.74 (0.41, 1.32) | 0.41 (0.18, 0.93) |
| Number of ACR criteria | 1.13 (1.01, 1.27) | 1.10 (0.95, 1.27) |
| Lupus nephritis | 1.52 (0.99, 2.32) | 1.35 (0.78, 2.36) |
Examining unadjusted odds using the two complement definitions of retention, nephritis predicted greater retention (OR 1.70, CI 1.12, 2.59; Table 4); small town residence predicted lower lab-defined retention. However, in multivariate models, nephritis patients did not have significantly different retention (OR 1.41, CI 0.82, 2.41) and only a higher number of SLE criteria predicted greater retention (OR 1.17, CI 1.01, 1.35).
Table 4.
Predictors of two complement lab-defined retention in care (n = 372, multivariable analysis included 372 of 397 SLE patients with complete data)
| Unadjusted OR (95% CI) | Adjusted OR (95% CI) | |
|---|---|---|
| Age | ||
| 18–29 | Ref | Ref |
| 30–40 | 0.93 (0.47, 1.86) | 1.10 (0.51, 2.39) |
| 40–60 | 1.28 (0.68, 2.39) | 1.68 (0.83, 3.41) |
| 60–80 | 0.89 (0.42, 1.88) | 1.40 (0.59, 3.30) |
| 80+ | 1.13 (0.17, 7.37) | 2.94 (0.36, 24.28) |
| Female | 0.77 (0.39, 1.54) | 0.77 (0.36, 1.64) |
| Race | ||
| White | Ref | Ref |
| Black | 1.29 (0.85, 1.97) | 0.82 (0.43, 1.55) |
| Other | 1.18 (0.46, 3.00) | 1.15 (0.34, 3.92) |
| Ethnicity (Hispanic) | 1.00 (0.38, 2.65) | 0.99 (0.28, 3.61) |
| RUCA | ||
| Urban | Ref | Ref |
| Suburban | 0.90 (0.44, 1.84) | 1.32 (0.59, 2.95) |
| Large town | 1.82 (0.64, 5.13) | 1.63 (0.49, 5.43) |
| Small town | 0.87 (0.50, 0.78) | 0.95 (0.32, 2.86) |
| Ever Smoking | 1.08 (0.72, 1.63) | 1.01 (0.64, 1.59) |
| Payer | ||
| Commercial | Ref | |
| Medicaid | 0.92 (0.52, 1.62) | |
| Medicare | 1.13 (0.72, 1.77) | |
| Neighborhood disadvantage by ADI | ||
| 1st (least disadvantage) | Ref | Ref |
| 2nd quartile | 0.87 (0.47, 1.59) | 0.80 (0.42, 1.51) |
| 3rd quartile | 1.20 (0.66, 2.18) | 1.10 (0.56, 2.15) |
| 4th (most disadvantage) | 1.56 (0.88, 2.82) | 1.39 (0.94, 3.04) |
| Number of ACR criteria | 1.19 (1.06, 1.33) | 1.17 (1.01, 1.35) |
| Lupus nephritis | 1.70 (1.12, 2.59) | 1.41 (0.82, 2.41) |
Among 145 patients with lupus nephritis, slightly more (66 vs. 60%) met the two visit-defined retention criteria. Likewise, 34% vs. 27% had at least two complement tests, but in such patients, only 14% had four tests per year as recommended per ACR guidelines for lupus nephritis [2].
Discussion
Using definitions analogous to those used by the WHO, IOM, and CDC [13–15] to define HIV retention in care, we were able to define and examine predictors of lupus retention in care. We examined both visit and lab-defined retention in care noting that 40% of patients lacked recommended visits and more than half of patients lacked recommended lupus labs. Notably, our visit-based models revealed that neighborhood disadvantage was the strongest predictor of gaps in lupus retention in care. Patients with lupus nephritis performed slightly better using basic measures, but only 14% met guideline recommended quarterly lab-defined retention.
More broadly, our data, and those of others [27, 28], support defining and investigating a Care Continuum across lupus care to inform the design of targeted interventions to eliminate disparities. Supporting the idea that the SLE Care Continuum would likewise correlate with outcomes, prior studies have shown retention on therapy for instance links to patient outcomes in SLE. Specifically, hydroxychloroquine improves outcomes [6], and nonadherence gaps correlate with worse outcomes, particularly, in disparities populations [27, 28]. A Canadian study correlated better hydroxychloroquine adherence with 5-year reductions in cumulative steroid use, disease activity, and lupus damage [28]. Conversely, a US Medicaid study reported that hydroxychloroquine therapy gaps (as defined by < 80% medication possession) were seen in 83% of patients and correlated with increased emergency visits and hospitalizations by 4 months [27]. We focused upstream in the Care Continuum noting that retention in care is critical to receive prescriptions for such treatments, to decrease treatment interruptions, and to signal treatment escalation when necessary.
Based on prior literature describing outcome disparities and follow-up gaps in Black patients or those from socioeconomic disadvantaged backgrounds [17], we predicted lower retention in care in those groups. We observed that neighborhood disadvantage was most strongly predictive, independent of race. Geographically, our site for this study, urban Milwaukee, WI, USA, may be more segregated than other cities [29] influencing the relative weights of predictors. We observed that 51% of Black patients with SLE resided in the most disadvantaged quartile neighborhoods compared to only 5% of White patients. Both race and neighborhood disadvantage in addition to other factors may be predictive of retention in care in other places, yet data suggest that neighborhood disadvantage predicts health independent of individual socioeconomic status as well [30]. Neighborhood context can directly affect access to healthcare as well as access to transportation, food, education, health behaviors, safety, discrimination, and chronic stress influencing many health outcomes [22, 23, 31]. Mechanistically, if transportation is less available or healthcare facilities are farther from disadvantaged populations, as shown in a US SLE Medicaid study [32], then getting routine visits and lab tests is more challenging. A strength of neighborhood disadvantage as a disparities predictor is that it can be calculated using already collected addresses within EHRs to identify patients who may need additional resources. It can also be used as a first step toward additional targeted research to disentangle the myriad of mechanisms that may underlie lupus disparities and to specifically target these actionable factors for interventions across policy, research, and clinical domains.
Retention in care is a well-developed metric in the HIV literature that has been central to the WHO and US National HIV/AIDS Strategy [15] and for measuring progress in reducing disparities [33]. Among those retained in care, 89% received treatment and 80% achieved viral suppression control, highlighting that retention in care is a key target. Encouragingly, a meta-analysis [34] and the compendium [15] highlight numerous evidence-based interventions proven to improve retention in HIV care and reduce disparities. Policy-driven programs have used such HIV Care Continuum strategies to increase viral suppression from 69 to 81% among Black participants between 2012 and 2016 [35]. Individual patients with HIV now also know that two viral load lab tests per year define a minimum standard to share accountability. Overall, success reducing disparities in HIV highlights the need to measure SLE retention in care as a necessary first step toward designing interventions, policies, and building patient partnerships to eliminate lupus outcome disparities.
Despite strengths of carefully validating lupus cases, applying a novel Care Continuum from HIV, and testing associations using multivariable regression, we also acknowledge limitations. First, our analysis included only one health system in one US city. Future projects will test retention definitions in other health systems or regions. Second, patients with nephritis or skin predominant SLE may be followed more closely in nephrology or dermatology which was not examined in this study. Future studies could examine retention in care including visits provided by nephrologists or dermatologists, who may share care for patients with SLE. A strength of our EHR-derived visit-based approach to define retention is the possibility of reproducing this metric across or between health systems. It is possible that compared to single-system EHR assessments, payer claims datasets might show higher retention in care given capture of visit or lab claims anywhere, including labs performed in other local health systems. For instance, we noted that small town residents had lower univariate odds of complement tests; some may have had lab testing in local clinics while others simply did not have tests. Likewise, only 2% of our cohort was uninsured and retention rates may vary in populations with more patients who are uninsured. We also acknowledge that some patients may have been lost to follow-up—migrating or intentionally changing insurance or providers, without true gaps in lupus retention in care. Residence may also change more frequently in patients with greatest disadvantage or adverse life experiences [36, 37]. Such time-varying factors could be examined in future multi-site studies.
Conclusions
Defining lupus retention in care and its predictors are key steps toward future evidence-based interventions to improve retention and reduce some disparities in lupus outcomes. Residence in a disadvantaged neighborhood was the strongest factor predicting poor SLE retention in care. Constructing future interventions could leverage geo-targeting disadvantaged neighborhoods, as well as designing programs specifically with and for vulnerable populations residing within these neighborhoods. Ultimately, we aim to use the SLE Care Continuum measures to design evidence-based care strategies and policies to reduce health disparities and advance outcome equity among patients with lupus.
Acknowledgements
Authors would like to thank Marit Johnson RN, for the chart review and data acquisition, Amanda Perez for the project management, Kristen Osinski for the electronic health record searches, Patrick Fergusson for the programming and analysis support, and Monica Messina for the manuscript support.
Abbreviations
- ACR
American College of Rheumatology
- ADI
Neighborhood area deprivation index
- CDC
Centers for Disease Control and Prevention
- DNA
Deoxyribonucleic acid
- dsDNA
Double stranded DNA antibody test
- EHR
Electronic health record
- HIV
Human immunodeficiency virus
- ICD
International Classification of Diseases
- IOM
US Institute of Medicine
- RUCA
Rural-urban commuting area
- SLE
Systemic lupus erythematosus
- SLICC
Systemic Lupus Erythematosus International Collaborating Clinics
- WHO
World Health Organization
Authors’ contributions
CMB, AKR, and XW had full access to the data in the study and take responsibility for the integrity of the data and statistical data analysis. CMB, AKR, and AJK conceptualized the study and interpreted the data. CMB and AKR obtained funding and oversaw data acquisition. UA and IC performed manual validation of the SLE cases and were contributors in writing the manuscript. CMB and XW performed and supervised the statistical analysis. CMB, AJK, XW, and AKR drafted the manuscript. UA, IC, NE, SG, and MS assisted result interpretation and substantively contributed to critical manuscript revisions for important intellectual content. The author(s) read and approved the final manuscript.
Funding
Primary funding for this project was provided by University of Wisconsin School of Medicine and Public Health through the Wisconsin Partnership Program New Investigator Program award. Support was also provided in part by the University of Wisconsin (UW) Clinical and Translational Science Award (CTSA), through the National Institutes of Health National Center for Advancing Translational Sciences (NIH NCATS grant UL1TR000427), and under National Institute on Minority Health and Health Disparities Research Award Number (NIH NIA R01MD010243 PI-Kind). Funders played no role in the design, conduct, analysis, or interpretation of results or writing of the manuscript. The manuscript content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Availability of data and materials
The datasets generated and analyzed during the current study are not publicly available due to limited patient health information but may be reviewed with the corresponding author on reasonable request.
Ethics approval and consent to participate
The Medical College of Wisconsin Institutional Review Board approved of this minimal risk medical record review study with waiver of individual informed consent and use of a limited dataset (PRO00029061).
Consent for publication
Not applicable
Competing interests
CMB receives peer-reviewed institutional grant funding from the Independent Grants for Learning and Change (Pfizer) for research unrelated to this study. All other authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.U.S. Department of Health and Human Services, National Institutes of Health, National Institute of Arthritis and Musculoskeletal and Skin Diseases. The future directions of lupus research. Bethesda; 2007. https://www.niams.nih.gov/about/future-directions-lupus-research. Accessed 30 Sept 2019
- 2.Hahn BH, Mcmahon MA, Wilkinson A, Wallace WD, Daikh DI, Fitzgerald JD, et al. American College of Rheumatology guidelines for screening, treatment, and management of lupus nephritis. Arthritis Care Res. 2012;64(6):797–808. doi: 10.1002/acr.21664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fanouriakis A, Kostopoulou M, Alunno A, Aringer M, Bajema I, Boletis JN, et al. 2019 update of the EULAR recommendations for the management of systemic lupus erythematosus. Ann Rheum Dis. 2019;78(6):736–745. doi: 10.1136/annrheumdis-2019-215089. [DOI] [PubMed] [Google Scholar]
- 4.Lim SS, Bayakly AR, Helmick CG, Gordon C, Easley KA, Drenkard C. The incidence and prevalence of systemic lupus erythematosus, 2002-2004: the Georgia lupus registry. Arthritis Rheumatol. 2014;66(2):357–368. doi: 10.1002/art.38239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Drenkard C, Rask KJ, Easley KA, Bao G, Lim SS. Primary preventive services in patients with systemic lupus erythematosus: study from a population-based sample in Southeast U.S. Semin Arthritis Rheum. 2013;43(2):209–216. doi: 10.1016/j.semarthrit.2013.04.003. [DOI] [PubMed] [Google Scholar]
- 6.Urowitz MB, Gladman DD, Anderson NM, Su J, Romero-Diaz J, Bae SC, et al. Cardiovascular events prior to or early after diagnosis of systemic lupus erythematosus in the systemic lupus international collaborating clinics cohort. Lupus Sci Med. 2016;3(1):e000143. doi: 10.1136/lupus-2015-000143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gonzalez LA, Toloza SM, Alarcon GS. Impact of race and ethnicity in the course and outcome of systemic lupus erythematosus. Rheum Dis Clin N Am. 2014;40(3):433–454. doi: 10.1016/j.rdc.2014.04.001. [DOI] [PubMed] [Google Scholar]
- 8.Yen EY, Singh RR. Brief report: lupus-an unrecognized leading cause of death in young females: a population-based study using nationwide death certificates, 2000-2015. Arthritis Rheumatol. 2018;70(8):1251–1255. doi: 10.1002/art.40512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bruce IN, O'Keeffe AG, Farewell V, Hanly JG, Manzi S, Su L, et al. Factors associated with damage accrual in patients with systemic lupus erythematosus: results from the Systemic Lupus International Collaborating Clinics (SLICC) Inception Cohort. Ann Rheum Dis. 2015;74(9):1706–1713. doi: 10.1136/annrheumdis-2013-205171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alarcon GS, McGwin G, Bertoli AM, Fessler BJ, Calvo-Alen J, Bastian HM, et al. Effect of hydroxychloroquine on the survival of patients with systemic lupus erythematosus: data from LUMINA, a multiethnic US cohort (LUMINA L) Ann Rheum Dis. 2007;66(9):1168–1172. doi: 10.1136/ard.2006.068676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yazdany J, Panopalis P, Gillis JZ, Schmajuk G, MacLean CH, Wofsy D, et al. A quality indicator set for systemic lupus erythematosus. Arthritis Rheum. 2009;61(3):370–377. doi: 10.1002/art.24356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Anderson E, Nietert PJ, Kamen DL, Gilkeson GS. Ethnic disparities among patients with systemic lupus erythematosus in South Carolina. J Rheumatol. 2008;35(5):819–825. [PMC free article] [PubMed] [Google Scholar]
- 13.Medland NA, McMahon JH, Chow EP, Elliott JH, Hoy JF, Fairley CK. The HIV care cascade: a systematic review of data sources, methodology and comparability. J Int AIDS Soc. 2015;18:20634. doi: 10.7448/IAS.18.1.20634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rebeiro PF, Horberg MA, Gange SJ, Gebo KA, Yehia BR, Brooks JT, et al. Strong agreement of nationally recommended retention measures from the Institute of Medicine and Department of Health and Human Services. PLoS One. 2014;9(11):e111772. doi: 10.1371/journal.pone.0111772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention: Recommendations for HIV prevention with adults and adolescents with HIV in the United States. 2014. https://stacks.cdc.gov/view/cdc/44064. Accessed 30 Sept 2019.
- 16.Skarbinski J, Rosenberg E, Paz-Bailey G, Hall HI, Rose CE, Viall AH, et al. Human immunodeficiency virus transmission at each step of the care continuum in the United States. JAMA Intern Med. 2015;175(4):588–596. doi: 10.1001/jamainternmed.2014.8180. [DOI] [PubMed] [Google Scholar]
- 17.Bertoli AM, Fernandez M, Calvo-Alen J, Vila LM, Sanchez ML, Reveille JD, et al. Systemic lupus erythematosus in a multiethnic U.S. cohort (LUMINA) XXXI: factors associated with patients being lost to follow-up. Lupus. 2006;15(1):19–25. doi: 10.1191/0961203306lu2257oa. [DOI] [PubMed] [Google Scholar]
- 18.Harper S, MacLehose RF, Kaufman JS. Trends in the black-white life expectancy gap among US states, 1990-2009. Health Aff (Millwood) 2014;33(8):1375–1382. doi: 10.1377/hlthaff.2013.1273. [DOI] [PubMed] [Google Scholar]
- 19.Kind AJ, Jencks S, Brock J, Yu M, Bartels C, Ehlenbach W, et al. Neighborhood socioeconomic disadvantage and 30-day rehospitalization: a retrospective cohort study. Ann Intern Med. 2014;161(11):765–774. doi: 10.7326/M13-2946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kind AJH, Buckingham WR. Making neighborhood-disadvantage metrics accessible - the neighborhood atlas. N Engl J Med. 2018;378(26):2456–2458. doi: 10.1056/NEJMp1802313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Alvidrez J, Castille D, Laude-Sharp M, Rosario A, Tabor D. The National Institute on Minority Health and Health Disparities research framework. Am J Public Health. 2019;109(S1):S16–S20. doi: 10.2105/AJPH.2018.304883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Badley EM, Canizares M, Gunz AC, Davis AM. Visits to rheumatologists for arthritis: the role of access to primary care physicians, geographic availability of rheumatologists, and socioeconomic status. Arthritis Care Res (Hoboken) 2015;67(2):230–239. doi: 10.1002/acr.22413. [DOI] [PubMed] [Google Scholar]
- 23.Feldman CH, Hiraki LT, Liu J, Fischer MA, Solomon DH, Alarcon GS, et al. Epidemiology and sociodemographics of systemic lupus erythematosus and lupus nephritis among US adults with Medicaid coverage, 2000-2004. Arthritis Rheum. 2013;65(3):753–763. doi: 10.1002/art.37795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Petri M, Orbai AM, Alarcon GS, Gordon C, Merrill JT, Fortin PR, et al. Derivation and validation of the systemic lupus international collaborating clinics classification criteria for systemic lupus erythematosus. Arthritis Rheum. 2012;64(8):2677–2686. doi: 10.1002/art.34473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bidaut-Russell M, Gabriel SE, Scott CG, Zinsmeister AR, Luthra HS, Yawn B. Determinants of patient satisfaction in chronic illness. Arthritis Rheum. 2002;47(5):494–500. doi: 10.1002/art.10667. [DOI] [PubMed] [Google Scholar]
- 26.Feldman CH, Yazdany J, Guan H, Solomon DH, Costenbader KH. Medication nonadherence is associated with increased subsequent acute care utilization among Medicaid beneficiaries with systemic lupus erythematosus. Arthritis Care Res (Hoboken) 2015;67(12):1712–1721. doi: 10.1002/acr.22636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Feldman CH, Collins J, Zhang Z, Subramanian SV, Solomon DH, Kawachi I, et al. Dynamic patterns and predictors of hydroxychloroquine nonadherence among Medicaid beneficiaries with systemic lupus erythematosus. Semin Arthritis Rheum. 2018;48(2):205–213. doi: 10.1016/j.semarthrit.2018.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pakchotanon R, Gladman DD, Su J, Urowitz MB. More consistent antimalarial intake in first 5 years of disease is associated with better prognosis in patients with systemic lupus erythematosus. J Rheumatol. 2018;45(1):90–94. doi: 10.3899/jrheum.170645. [DOI] [PubMed] [Google Scholar]
- 29.Massey DS, Tannen J. A research note on trends in black hypersegregation. Demography. 2015;52(3):1025–1034. doi: 10.1007/s13524-015-0381-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ludwig J, Duncan GJ, Gennetian LA, Katz LF, Kessler RC, Kling JR, et al. Neighborhood effects on the long-term well-being of low-income adults. Science. 2012;337(6101):1505–1510. doi: 10.1126/science.1224648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Arcaya MC, Tucker-Seeley RD, Kim R, Schnake-Mahl A, So M, Subramanian SV. Research on neighborhood effects on health in the United States: a systematic review of study characteristics. Soc Sci Med. 2016;168:16–29. doi: 10.1016/j.socscimed.2016.08.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gillis JZ, Yazdany J, Trupin L, Julian L, Panopalis P, Criswell LA, et al. Medicaid and access to care among persons with systemic lupus erythematosus. Arthritis Rheum. 2007;57(4):601–607. doi: 10.1002/art.22671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hall HI, Frazier EL, Rhodes P, Holtgrave DR, Furlow-Parmley C, Tang T, et al. Differences in human immunodeficiency virus care and treatment among subpopulations in the United States. JAMA Intern Med. 2013;173(14):1337–1344. doi: 10.1001/jamainternmed.2013.6841. [DOI] [PubMed] [Google Scholar]
- 34.Higa DH, Crepaz N, Mullins MM. Identifying best practices for increasing linkage to, retention, and re-engagement in HIV medical care: findings from a systematic review, 1996–2014. AIDS Behav. 2016;20(5):951–966. doi: 10.1007/s10461-015-1204-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.US Health Resources and Services Administration . Ryan White HIV/AIDS Program Annual Client-Level Data Report. 2016. [Google Scholar]
- 36.Dong M, Anda RF, Felitti VJ, Williamson DF, Dube SR, Brown DW, et al. Childhood residential mobility and multiple health risks during adolescence and adulthood: the hidden role of adverse childhood experiences. Arch Pediatr Adolesc Med. 2005;159(12):1104–1110. doi: 10.1001/archpedi.159.12.1104. [DOI] [PubMed] [Google Scholar]
- 37.Tseliou F, Maguire A, Donnelly M, O’Reilly D. The impact of childhood residential mobility on mental health outcomes in adolescence and early adulthood: a record linkage study. J Epidemiol Community Health. 2016;70(3):278–285. doi: 10.1136/jech-2015-206123. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and analyzed during the current study are not publicly available due to limited patient health information but may be reviewed with the corresponding author on reasonable request.


