Abstract
Objective:
Clinics are increasingly interested in identifying food insecurity (FI), but there is limited data on how to implement FI screening. Our objective was to determine the difference in FI disclosure rates by parents/guardians screened by a written questionnaire compared to verbally.
Methods:
The study occurred in one pediatric primary care clinic in which we screen for FI using the 2-item Hunger Vital Sign™. We used interrupted time series to evaluate the effect of changing from the clinician verbal screening to a written questionnaire. Screening results were extracted for all well-child visits from 4/2017-10/2018 for children age 0-18 years. The outcome was the proportion who screened positive for FI 9 months before and 9 months after the implementation of the written questionnaire. We estimated the difference in the level and trend of positive screens using ordinary least squares regression using Newey-West standard errors and adjusting for autocorrelation.
Results:
In 7,996 well-child visits, 1,141 (14.3%) patients screened positive. In bivariate analysis, there was a significant difference in the FI disclosure rates between patients screened by written questionnaire compared to verbally (16.3% vs 10.4%, p<0.001). In interrupted time series, changing to the written questionnaire was associated with a significant increase in FI disclosure rates (β=0.04, 95% CI: 0.01, 0.07; p=0.02). There was no significant change in the trend in disclosure rates.
Discussion:
Multiple barriers exist to effectively implementing FI screening in clinical care. Changing from a verbal to a written questionnaire resulted in an immediate and significant increase in the number of parents/guardians who reported FI.
Keywords: food insecurity, social determinants of health, public health
Introduction
Food insecurity (FI), or the lack of consistent access to enough food, is a major public health problem in the United States (US), and 13.9% of US households with children were food insecure in 2018.1 FI has also been associated with numerous negative outcomes in children.2–5 Because of the prevalence and the impact on health, national organizations, including the American Academy of Pediatrics (AAP) and the Academic Pediatric Association, have recommended that all clinicians routinely screen patients for household FI.6–10
Although there is a growing body of research developing strategies to address FI in healthcare settings, there is limited data on how to implement these strategies.11–15 One area that remains unclear is how to most effectively screen patients for FI and other social determinants of health (SDH). Screening patients verbally or face-to-face allows the opportunity to build trust and rapport with the family. Because of fear or social desirability, however, parents/guardians and patients may be less likely to disclose FI if asked face-to-face. Further, parents/guardians have reported that they would feel more comfortable responding to FI questions using a written questionnaire.16 Two randomized trials in pediatric emergency departments found that parents/guardians were more likely to disclose FI or other unmet social needs when screened on a tablet compared to parents/guardians who were asked face-to-face, but limited data in primary care exists.17,18 The objective of this study was to determine if parents/guardians were more likely to disclose FI if they had been screened by a written questionnaire or verbally by the clinician in one pediatric primary care clinic.
Methods
Study setting and design
We evaluated a natural experiment that occurred in one large pediatric academic primary care clinic. The clinic receives ~19,000 visits annually and serves a predominantly low-income, minority population. The clinic is the teaching site for the pediatric residency program and is staffed by 14 attending physicians who primarily supervise the residents, 5 of whom directly provide patient care. There are 41 residents who provide care; 13 are first year residents. Prior to starting at the clinic, all clinicians (attendings and residents) receive a detailed orientation discussing clinic procedures. This orientation includes a presentation about FI, including the clinic’s process for screening and providing resources. Clinicians also receive periodic lectures about FI and the clinic’s process for addressing FI throughout the year. The onboarding process for clinicians was the same for both the verbal and written screening.
In July 2014, the clinic began screening all parents/guardians of patients presenting for a well-child visit (WCV) using the AAP-recommended 2-item Hunger Vital Sign (HVS™).7,19 Response items to the 2 questions were ‘yes’ or ‘no’, and an affirmative response to either question was considered a positive screen.7 Parents who screened positive were able to receive a bag of non-perishable food items, a list of local food pantries, and meet with the clinic’s patient navigator or care coordinator to discuss additional community resources. Clinicians verbally asked all parents/guardians the HVS™ during the visit and were instructed to read the questions verbatim. For patients who did not speak English, the clinic has in-person Spanish interpreters available. If one of the in-person Spanish interpreters was not available or the patient spoke a language other than English or Spanish, the clinic has video interpreters available in a range of languages. In March 2017, the HVS™ was embedded in all WCV documentation templates in the electronic health record (EHR), in a section specific for FI screening, in order to standardized documentation, further prompt clinicians to screen, and allow the clinic to evaluate the frequency with which providers were documenting results.
Starting January 8, 2018, the entire clinic moved to screening all patients using a paper-based form rather than the clinician verbally asking. This was done because the clinic was expanding the FI screen to all visit types (including urgent and return visits) and to include other SDH (such as housing or lack of transportation). While the patient was being roomed, the nurse provided the parent/guardian with a written questionnaire (in English or Spanish) that included the same HVS™ clinicians were previously verbally asking (included the same questions and response items). The results of the questionnaire were then reviewed by the clinician at the time of the visit, discussed with the family, and entered into the well-child documentation template (in the section specific for FI screening). Parents/guardians who screened positive were still eligible to receive a food bag, list of food pantries, and meet with the care coordinator. Families were eligible to receive resources and meet with the care coordinator no matter how many times they had screened positive for FI in the past or received resources on prior visits.
We extracted data from the EHR (EpicCare Verona, WI) for all WCV that occurred between April 1, 2017 and October 31, 2018 for patients 0-18 years of age. All WCV during this time were eligible to be included.
Measures
The primary outcome was the FI disclosure rate per month, or the proportion of patients who screened positive. The predictor was the screening modality (written versus verbal screening). We also evaluated for differences in documentation of the FI screen in the EHR and extracted patient demographics to compare the study population screened verbally to those screened with the written questionnaire. All demographic data was extracted from the EHR and is based on parents/guardians’ self report. Demographics included age, gender, preferred language (English, Spanish, or other), and race/ethnicity (Hispanic, White, African American, or other). “Other” race/ethnicity includes Native Hawaiian/Pacific Islander, Asian, other, unknown, or patient refused. Because over 95% of the patients seen receive Medicaid, we did not include insurance type.
Statistical analysis
We performed bivariate analyses testing for differences in documentation rates and demographics using chi-square or t-test. We used interrupted times series to evaluate the difference in FI disclosure rates when changing from a verbal to a written screen.20 We estimated the change in the level and trend (or slope) in disclosure rates in the 9 months prior to and the 9 months after changing to a written questionnaire. The written questionnaire was implemented January 8, 2018. We excluded the screening results from January 2018 in the main analyses to provide time for the questionnaire to be fully implemented, i.e. the nurse remembering to provide the written questionnaire or the clinician entering the results in the EHR. Sensitivity analyses that included January and those limited to only the first time patients presented for a WCV found similar results (data not shown). We conducted interrupted time series ordinary least squares regression using Newey-West standard errors to assess the change in screening modality. We adjusted for autocorrelation in time series up to five lags. We used a two-sided hypothesis test, and considered an alpha <0.05 significant. All statistical analyses were conducted using Stata 15.0 (StataCorp, College Station, TX). The Wake Forest School of Medicine Institutional Review Board approved this study.
Results
Of the 10,571 WCV that occurred between April 2017-October 2018 (excluding January 2018), 7,996 visits (75.6%) included the results of the FI screen. There were no significant differences in gender, race/ethnicity, and preferred language between patients with a documented FI screen and patients without. WCV for younger patients were more likely to have a document FI screen (mean 8.0 vs 9.7 years, p<0.001). There was a significant difference in the documentation rates between patients screened via the written questionnaire (2018) compared to patients screened verbally (2017) (96.6% vs 53.5%, p<0.001).
Of the 7,996 WCV, 1,141 (14.3%) screened positive for FI. In bivariate analysis, there was a significant difference in the FI disclosure rates between patients screened via a written questionnaire compared to verbally (16.3% vs 10.4%, p<0.001). We did not find significant differences in gender, preferred language, or race/ethnicity (Table), but there was a small but significant difference in age between patients screened by written questionnaire and those screened verbally (Mean 70.1 months vs 67.0 months, p=0.03).
Table:
Demographics of the Patients Seen during Well-Child Visits
| Total population: N (%) | Verbal (2017) | Written (2018) | p-value | ||
|---|---|---|---|---|---|
| 7,996 | 2,750 (34.4) | 5,246 (65.6) | |||
| Food Insecurity | <0.0001 | ||||
| Yes | 1,141 (14.3) | 287 (10.4) | 854 (16.3) | ||
| No | 6,855 (85.7) | 2,463 (89.6) | 4,392 (83.7) | ||
| Age (months) | Mean (SD) | 69.1 (63.8) | 67.0 (64.0) | 70.1 (63.6) | 0.03 |
| Gender | 0.73 | ||||
| Female | 3,833 (47.9) | 1,311 (47.7) | 2,522 (48.1) | ||
| Male | 4,163 (52.1) | 1,439 (52.3) | 2,724 (51.9) | ||
| Preferred language | English | 3,851 (48.2) | 1,274 (46.3) | 2,577 (49.1) | 0.052 |
| Spanish | 3,999 (50.0) | 1,427 (51.9) | 2,572 (49.1) | ||
| Other | 143 (1.8) | 48 (1.8) | 95 (1.8) | ||
| Race/Ethnicity | 0.13 | ||||
| Hispanic | 4,703 (58.8) | 1,660 (60.4) | 3,043 (58.0) | ||
| AA* | 1,791 (22.4) | 590 (21.5) | 1,201 (22.9) | ||
| White | 471 (5.9) | 167 (6.1) | 304 (5.8) | ||
| Other | 1,031 (12.9) | 333 (12.1) | 698 (13.3) |
AA-African American
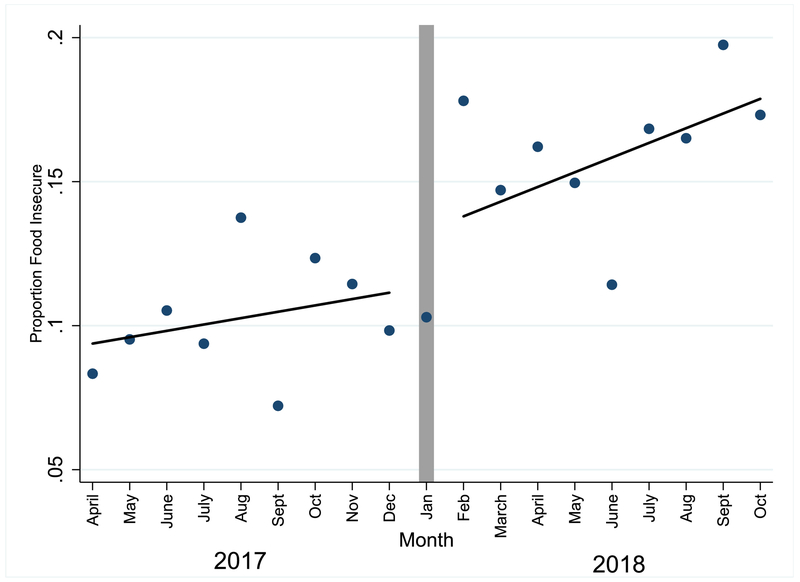
The figure shows the FI disclosure rates in the 9 months prior to the implementation of the written questionnaire and the 9 months after. The change from the verbal to the written FI questionnaire was associated with a significant increase in the FI disclosure rates (β=0.04, 95% CI: 0.01, 0.07; p=0.02). We did not find a significant change in the trend over time in FI disclosure rates in the 9 months prior (β=0.00, 95% CI: 0.000, 0.004; p=0.07) or the 9 months after (β=0.00, 95% CI: −0.004, 0.005; p=0.76) the implementation of the written questionnaire.
Figure:
Change in the Proportion who Screened Positive for Food Insecurity with Implementation of Written Questionnaire
The proportion of patients who screened positive for household food insecurity per month when changing from a verbal (2017) to a written food insecurity screen (2018). The change from the verbal to the written FI questionnaire was associated with a significant increase in the food insecurity disclosure rates (β=0.04, 95% CI: 0.01, 0.07; p=0.02). The trend over time in FI disclosure rates in the 9 months prior (β=0.00, 95% CI: 0.000, 0.004; p=0.07) and the 9 months after (β=0.00, 95% CI: −0.004, 0.005; p=0.76) the implementation of the written questionnaire were not significant.
Discussion
An increasing number of national healthcare organizations have recommended that clinicians screen patients for FI.6–10 This study provides new data about how primary care practices can most effectively implement FI screening. We found that changing from a verbal to a written screen resulted in an improvement in the documentation of the FI results and in a statistically significant increase in the proportion of parents/guardians who disclosed FI. The increase in the proportion of parents/guardians who disclosed FI remained elevated after the written questionnaire was implemented.
A number of studies have begun to test strategies to address FI in clinical settings.11–13,21 However, there is limited data on how to implement these strategies. We found that changing from a verbal to a written screen resulted in a significant increase in FI disclosure rates. There are several potential reasons why. The first is the difference in documentation rates. We found that clinicians were significantly more likely to document the results of the HVS™ when patients were screened by written questionnaire. Because clinicians were more likely to document the results with the written questionnaire, an increased number of positive screens could have been included. However, we evaluated the proportion of positive screens, and we would expect clinicians to document if a patient screened positive for FI even if they were screened verbally. Our results do suggest that a written questionnaire may be a more efficient method of documenting screening results in a busy clinic. Future studies should evaluate how these different SDH screening modalities impact clinic workflow (e.g. time, staffing, literacy rates).
The second possibility why we found an increase in disclosure rates is parents/guardians may feel less comfortable reporting FI when asked face-to-face. Parents/guardians have reported in prior qualitative work that they would be more likely to report FI if they were asked ‘anonymously’, such as on a written questionnaire, as opposed to being asked verbally.16 Prior studies in primary care have also found that patients and parents/guardians are more likely to report sensitive information, such as substance abuse or post-partum depression17,22,23, if they are screened using a written or electronic questionnaire as opposed to being verbally asked.
A third possibility is that parents may have become more comfortable with the clinic screening over time. One barrier to parents/guardians reporting FI is fear of being reported to child protective services.16 Over time, parents may have seen the screening as a routine part of clinical care, recognized that the clinic was screening to offer services, and felt more comfortable reporting FI. The change to a written FI screen also occurred concurrently with the expansion of the screening to all visits types and the inclusion of other SDH. This could have also made parents/guardians feel more comfortable that the screening was being done as a routine part of care for all families. The increase in FI disclosure rates, however, occurred immediately after the implementation of the written questionnaire, and we did not find a significant change in the trend in disclosure rates before or after the implementation of the written questionnaire.
A fourth possibility is that the patient population seen after the written questionnaire was implemented has a higher proportion of families who were food insecure. National and statewide FI rates have been slowly declining since 2011 though.1 It is still possible that there was an outside factor that we cannot account for that led to the patient population that was screened by the written questionnaire to be more food insecure than the patient population screened verbally. We are not aware of any major changes that occurred to the availability of local resources during this time, however.
There are several limitations to this study that should be acknowledged. First, this study was done in a single clinic that serves a predominantly low-income population. Also, 50% of the study population preferred Spanish, and the results may not be generalizable to other practice settings. Second, the FI disclosure rates were based on the results that were documented in the EHR. We cannot be sure that the clinicians were accurately documenting the results in the well-child documentation. Third, there was no control group available. It is possible that other factors may have influenced how screening was being conducted during this time; however, clinic and nursing administration did not report this. Fourth, for both the verbal and written screen the clinic used the dichotomous response items (yes or no) as opposed to the Likert scale (never, sometimes true, or often true). The HVS™ with the dichotomous response items has been found to be less sensitive than the Likert scale, and there may have been families with FI who were missed because the dichotomous screen used.24 Fifth, over time providers often modify or tailor verbal screening questions, which can result in the validity of a survey tool being weakened.25 New hires at the clinic, both attendings and residents, received training on asking the questions verbatim. However, we cannot confirm the accuracy of verbal screening which may limit our ability to compare screening modalities.
Conclusion
In this natural experiment, we found that changing from a verbal to a written questionnaire resulted in an improvement in the documentation rates and an immediate and significant increase in the number of parents/guardians who reported FI. Although further research is needed to confirm our results, parents and guardians may feel more comfortable disclosing FI by responding to a written questionnaire as opposed to being asked verbally. As an increasing number of health systems and clinics begin to address FI and other SDH, understanding how to most effectively and efficiently implement screening into clinical workflow will become increasingly important.
What’s New:
In this natural experiment, we evaluate the change in the proportion of parents and guardians who report household food insecurity in one large, academic primary care clinic that changed from screening verbally to a written food insecurity questionnaire.
Acknowledgements:
This study was supported by the Kate B. Reynolds Charitable Trust. We would like to acknowledge the Data Management services of the Wake Forest Clinical and Translational Science Institute (WF CTSI), which is supported by the National Center for Advancing Translational Sciences (NCATS), National Institutes of Health, through Grant Award Number UL1TR001420. The funding sources did not have any role in the study design; in the collection, analysis, and interpretation of data; in the writing of the report; and in the decision to submit the article for publication. Portions of this study were presented at the 2019 Pediatric Academic Societies Meeting in Baltimore, MD.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest: The authors have no conflicts of interest to disclose.
References
- 1.Coleman-Jensen A, Rabbitt MP, Gregory CA, Singh A. Household Food Security in the United States in 2019, ERR-270 U.S. Department of Agriculture, Economic Resarch Service. [Google Scholar]
- 2.Gundersen C, Kreider B. Bounding the effects of food insecurity on children’s health outcomes. J Health Econ. September 2009;28(5):971–983. [DOI] [PubMed] [Google Scholar]
- 3.Gundersen C Food insecurity is an ongoing national concern. Adv Nutr. January 2013;4(1):36–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cook JT, Frank DA. Food security, poverty, and human development in the United States. Ann N Y Acad Sci. 2008;1136:193–209. [DOI] [PubMed] [Google Scholar]
- 5.Rose-Jacobs R, Black MM, Casey PH, et al. Household food insecurity: associations with at-risk infant and toddler development. Pediatrics. January 2008;121(1):65–72. [DOI] [PubMed] [Google Scholar]
- 6.APA Task Force on Childhood Poverty: A strategic road-map: Committed to Bringing the Voice of Pediatricians to the Most Important Problem Facing Children in the US Today. 2013; https://http://www.academicpeds.org/taskforces/pdfs/StrategicRoadMap_ver3.pdf.
- 7.Council on Community Pediatrics; Committee on Nutrition. Promoting Food Security for All Children. Pediatrics. 2015. November;136(5):e1431–1438. [DOI] [PubMed] [Google Scholar]
- 8.Council on Community Pediatrics. Poverty and Child Health in the United States. Pediatrics. 2016. April; 137(4). [DOI] [PubMed] [Google Scholar]
- 9.Healthy People 2020: An Opportunity to Address Societal Determinants of Health in the United States Secretary’s Advisory Committee on National Health Promotion and Disease Prevention Objectives for 2020. U.S Department of Health & Human Services; Available at: https://www.healthvpeople.gov/2010/hp2020/advisory/societaldeterminantshealth.htm. Accessed Oct 7, 2019. [Google Scholar]
- 10.Daniel H, Bornstein SS, Kane GC. Addressing Social Determinants to Improve Patient Care and Promote Health Equity: An American College of Physicians Position Paper. Ann Intern Med. April 17 2018;168(8):577–578. [DOI] [PubMed] [Google Scholar]
- 11.Morgenlander MA, Tyrrell H, Garfunkel LC, Serwint JR, Steiner MJ, Schilling S. Screening for Social Determinants of Health in Pediatric Resident Continuity Clinic. Acad Pediatr. March 9 2019. [DOI] [PubMed] [Google Scholar]
- 12.Alderwick HAJ, Gottlieb LM, Fichtenberg CM, Adler NE. Social Prescribing in the U.S. and England: Emerging Interventions to Address Patients’ Social Needs. Am JPrev Med. May 2018;54(5):715–718. [DOI] [PubMed] [Google Scholar]
- 13.Gottlieb LM, Wing H, Adler NE. A Systematic Review of Interventions on Patients’ Social and Economic Needs. Am J Prev Me. November 2017;53(5):719–729. [DOI] [PubMed] [Google Scholar]
- 14.Gottlieb L, Cottrell EK, Park B, Clark KD, Gold R, Fichtenberg C. Advancing Social Prescribing with Implementation Science. J Am Board Fam Med. May-Jun 2018;31(3):315–321. [DOI] [PubMed] [Google Scholar]
- 15.DeVoe JE, Bazemore AW, Cottrell EK, et al. Perspectives in Primary Care: A Conceptual Framework and Path for Integrating Social Determinants of Health Into Primary Care Practice. Ann Fam Med. March 2016;14(2): 104–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Palakshappa D, Doupnik S, Vasan A, et al. Suburban Families’ Experience With Food Insecurity Screening in Primary Care Practices. Pediatrics. July 2017; 140(1). [DOI] [PubMed] [Google Scholar]
- 17.Gottlieb L, Hessler D, Long D, Amaya A, Adler N. A randomized trial on screening for social determinants of health: the iScreen study. Pediatrics. December 2014; 134(6):e1611–1618. [DOI] [PubMed] [Google Scholar]
- 18.Cullen D, Woodford A, Fein J. Food for Thought: A Randomized Trial of Food Insecurity Screening in the Emergency Department. Acad Pediatr. January 10 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hager ER, Quigg AM, Black MM, et al. Development and validity of a 2-item screen to identify families at risk for food insecurity. Pediatrics. July 2010; 126(1):e26–32. [DOI] [PubMed] [Google Scholar]
- 20.Hacker K, Penfold R, Zhang F, Soumerai SB. Impact of electronic health record transition on behavioral health screening in a large pediatric practice. Psychiatr Serv. March 2012;63(3):256–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.De Marchis EH, Torres JM, Fichtenberg C, Gottlieb LM. Identifying Food Insecurity in Health Care Settings: A Systematic Scoping Review of the Evidence. Fam Community Health. Jan-Mar 2019;42(1):20–29. [DOI] [PubMed] [Google Scholar]
- 22.Carroll AE, Biondich P, Anand V, Dugan TM, Downs SM. A randomized controlled trial of screening for maternal depression with a clinical decision support system. J Am Med Inform Assoc. Mar-Apr 2013;20(2):311–316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fleegler EW, Lieu TA, Wise PH, Muret-Wagstaff S. Families’ health-related social problems and missed referral opportunities. Pediatrics. June 2007;119(6):e1332–1341. [DOI] [PubMed] [Google Scholar]
- 24.Makelarski JA, Abramsohn E, Benjamin JH, Du S, Lindau ST. Diagnostic Accuracy of Two Food Insecurity Screeners Recommended for Use in Health Care Settings. Am J Public health. November 2017; 107(11): 1812–1817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Williams EC, Achtmeyer CE, Thomas RM, et al. Factors Underlying Quality Problems with Alcohol Screening Prompted by a Clinical Reminder in Primary Care: A Multi-site Qualitative Study. J Gen Intern Med. August 2015;30(8): 1125–1132. [DOI] [PMC free article] [PubMed] [Google Scholar]