Abstract
Introduction
Overuse injury in youth overhead athletes remains a concern. The introduction of pitch count guidelines was designed to limit the number of pitches per game. South Carolina is considered a warm weather climate which has been proven to expose overhead athletes to higher risk for injury. The purpose of this study was to detect baseline rates of arm pain and sequelae (injury, surgery, impact on participation) among southern youth baseball/softball players to better counsel players, parents, coaches and league administration on the prevention of arm injury.
Methods
A survey was distributed to 14 pediatric practices within the South Carolina Pediatric Practice Research Network. The 2-page survey included 28 closed-ended and descriptive questions that investigated physical and psychosocial responses during and after play. Additional questions were conducted on adherence and understanding of USA Baseball guidelines and pitch counting behavior.
Results
Two hundred and seventy three surveys were completed by parents of baseball/softball players. The players’ average age was 11.6 years, who played on an average of 1.78 teams/leagues for 5.2 months each year. Only 26% of baseball players answered “Sometimes”, “Often” or “Always” to their arm hurting. Arm fatigue, older age, parent/coach frustration with play, and months played were statistically significantly associated with arm pain. The survey revealed 58.9% of families were familiar with pitch count guidelines.
Discussion
Arm pain is relatively prevalent among the South Carolina youth baseball community and worse in older players and experience fatigue. This survey found lower percentage of youth overhead athletes experiencing arm discomfort when compared to prior studies. It is important for warm weather climate athletes to abide by guidelines, as they are more susceptible to arm injury. Increased recognition, education and compliance with pitch count guidelines will help protect these youth athletes from overuse injury.
Level of evidence
IV, Descriptive Epidemiology Study;
Keywords: Youth baseball, Pitching, Pitch count, Arm pain, Survey study
1. Introduction
Shoulder and elbow pain are well documented within the youth baseball community with an in-season incidence of approximately 30%.1 The current understanding is that many of the injuries result from repetitive, cumulative microtrauma from years of competition beginning in youth leagues.2,3 Growing concern over the effects of overhead activity and increasing number of injuries led to the development of guidelines regarding pitch number and type in the mid 1990's.4 Despite increased awareness, there was a fourfold increase in the number of elbow surgeries performed on collegiate pitchers and a six fold increase for high school throwers between 2000 and 2004 compared to 1994 to 1999.5 Athletes in warmer climates have more opportunity to participate in outdoor sport and a prior study found that pitchers from warm weather climates perform “pitching activities” 3 months more per year compared to athletes from colder climates.6 Additionally, a study of MLB pitchers found that a higher proportion of pitchers who underwent UCL reconstruction played high school baseball in warm weather climates.7
The purpose of this study was to detect baseline frequency of arm pain and subsequent sequelae (injury, surgery, impact on participation) among southern youth baseball/softball players to better counsel players, parents, coaches and league administration on the prevention of shoulder and elbow injury. We hypothesized that reports of injury and arm pain would be higher in a southern state than previously documented arm pain in a northern state. We expected similar results to prior studies regarding risk factors for the development of arm pain. The survey also aims to capture awareness of players and families toward pitch count guidelines. We hypothesize that despite heightened public awareness, a majority of players and families remain unfamiliar with the most recent guidelines.
2. Materials and methods
2.1. Setting
A survey was distributed to 14 pediatric practices in the South Carolina Pediatric Practice Research Network, a practice-based research network with primary care physicians experienced in outcomes-based research. The Network includes most of coastal South Carolina and extends centrally to include parts of Columbia, South Carolina and rural practices. Each practice obtained anonymous surveys from parents and guardians on behalf of their children, who are youth athletes engaged in overhead throwing activities. Parents of pediatric patients who came into each clinic for any reason (not documented in this study) were asked if their children played baseball or softball; if so, they were encouraged to complete the survey during their time in the office. There was no recruitment or survey distribution beyond each pediatric practice. No input from coaches was included unless an athlete's parent happened to be the coach of his/her respective team.
2.2. Survey
The 2-page survey, modeled from a prior published survey (Makhni et al. (2015)) included 28 closed-ended and descriptive questions that investigated physical and psychosocial responses during and after play.8 Each question was designed to focus on frequency of the symptom. The survey collected demographic data such as age, sport, position, injuries, surgeries, general overhead motion questions, and questions specific to baseball/softball. Subject matter questions explored pain, fatigue, coach/parental frustration and the effect on sports performance for all athletes in overhead throwing sports. Lastly, additional questions were conducted on adherence and understanding of USA Baseball guidelines and pitch counting behavior. Non-binary questions were given using a Likert five point frequency scale.
2.3. Data analysis
The survey results for baseball and softball players were aggregated and entered into an electronic database, and subsequently analyzed with IBM SPSS Statistics-Version 24 (IBM SPSS Inc., Arnock, NY). During analysis, the frequency scaled responses were separated into dichotomous answers. Backward stepwise logistic regression to identify variables independently associated with increased rates of pain. Chi-squared analysis was performed to determine the association with the presence of pain and risk factors with subsequent odds ratios calculated for pitchers. Chi square tests of independence were used to compare the frequencies of never/rarely or sometimes, often, always survey responses between different groups of players. For all statistical comparisons p ≤ 0.05 was considered statistically significant. Institutional review board approval was obtained for this study.
3. Results
Two hundred and seventy three surveys were completed by parents of baseball/softball players and analyzed. The players’ average age was 11.6 ± 2.9 years, and they reported playing on an average of 1.8 teams/leagues for 5.2 months each year (Table 1a, Table 1b). Fifty nine (21.6%) were injured during play and four received surgery. Of the fifty nine players that reported injury, fourteen (23.7%) reported shoulder/elbow/arm injuries. In addition, four players (1.5%) needed surgery related to activity from sport. Out of the four surgeries, only one player had a surgery involving his/her arm. The other surgeries included an open reduction internal fixation of an ankle, closed reduction of nasal bone and a nasal septum repair. Thus, only one out of two hundred and seventy three (0.04%) players, required surgery on the throwing arm related to overhead activity.
Table 1a.
Descriptive statistics extracted from survey results.
| Total baseball/softball players: | 273 | ||
|---|---|---|---|
| Positions played* | |||
| Pitcher | 107 | 39.20% | |
| Catcher | 81 | 29.70% | |
| Infield | 175 | 64.10% | |
| Outfield | 145 | 53.10% | |
| Injuries | ' | 60 (21.6%) | |
| Surgeries | 4 (1.5%) | ||
| Familiar with USA Baseball guidelines | 58.80% | ||
| Interested in using a free phone app | 41% | ||
Table 1b.
Average age of participants; average number of months and teams the youth athlete participated in the last year.
| Minimum | Maximum | Mean | Standard Deviation | |
|---|---|---|---|---|
| Age | 7 | 17 | 11.59 | 2.93 |
| Teams played | 0 | 6 | 1.68 | 0.94 |
| Months played | 0 | 12 | 5.18 | 2.72 |
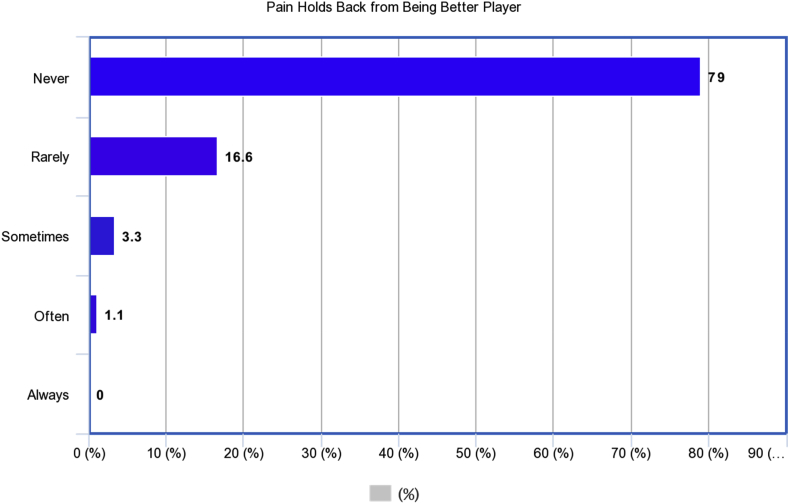
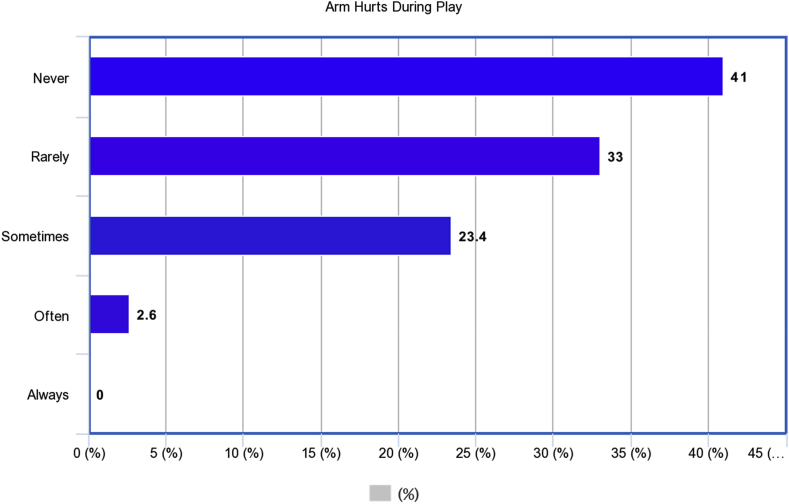
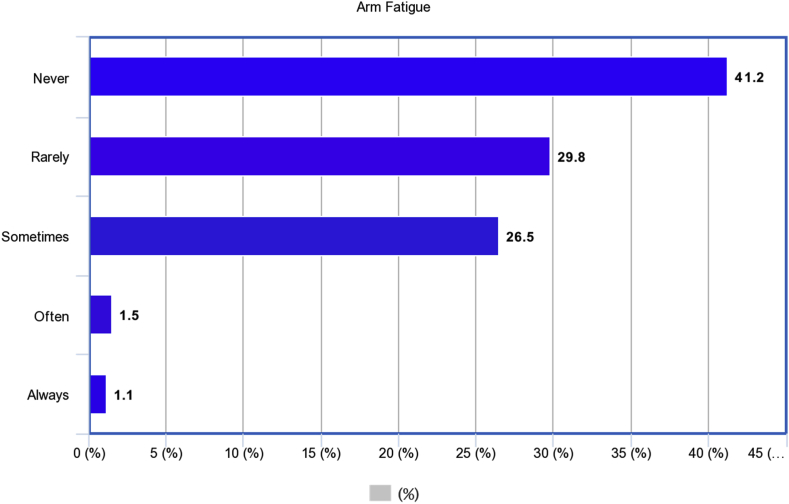
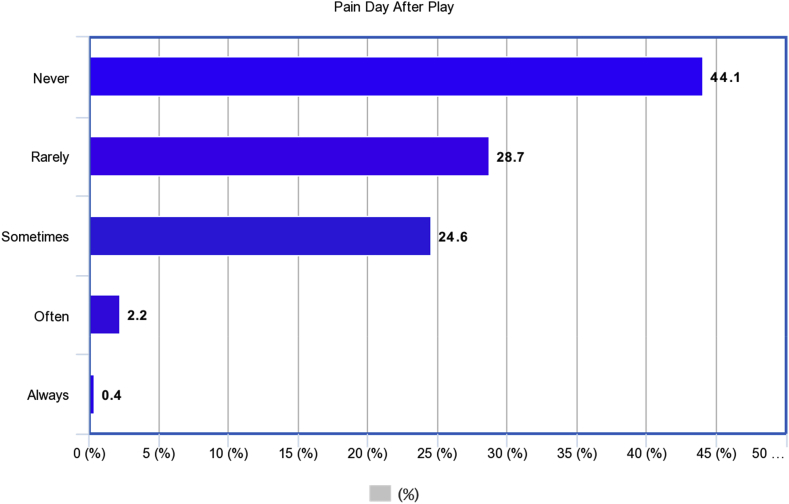
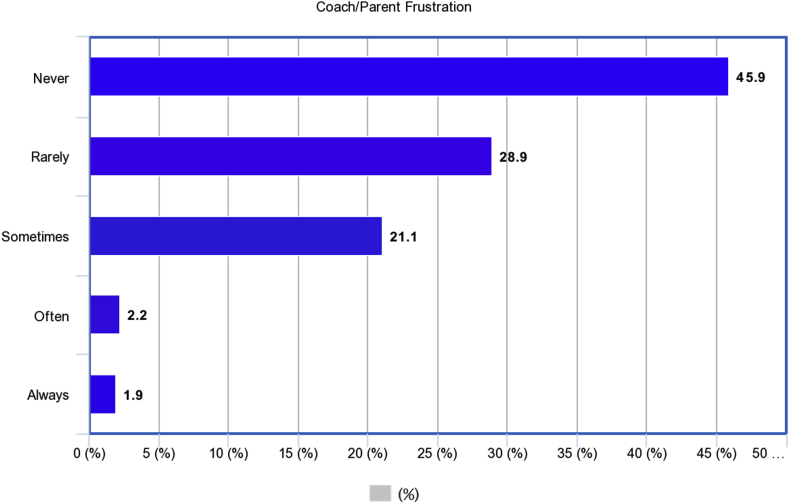
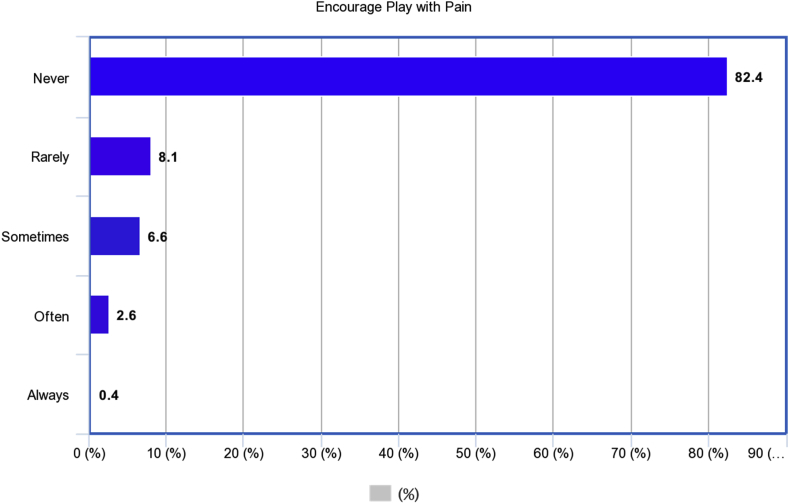
The survey revealed that 26% of baseball players answered “Sometimes”, “Often” or “Always” to their arm hurting. Of responders, 29% experienced arm fatigue at least “Sometimes” while playing and 27.2% of responders reported arm pain the day after play. Players reported that coaches/parents got frustrated at the player 25.2% of time regarding the competitors arm pain. A small percentage (9.6%) of young athletes reported that coaches encouraged players to continue play despite arm pain. Another small percentage of players reported that arm pain held them back from being a better player (4.4%) and arm pain prevented the player from playing in multiple leagues (3.3%). Chi-squared odds ratio analysis of whether pitching is correlated with incidence of pain found players were more likely to experience pain while playing that position (OR = 1.89; p = 0.02) and pain after throwing was more likely for pitchers (OR = 1.87; p = 0.02). (Fig. 1f, Fig. 1a, Fig. 1b, Fig. 1c, Fig. 1d, Fig. 1e).
Fig. 1f.
Distribution of players who feel pain limits their performance.
Fig. 1a.
Distribution of Players whose arms hurt during play.
Fig. 1b.
Distribution of players who experienced arm fatigue during play.
Fig. 1c.
Distribution of players who experience arm pain the day after play.
Fig. 1d.
Distribution of players whose coaches/parents get frustrated with performance.
Fig. 1e.
Distribution of players whose coaches/parents encourage play despite arm pain.
Whether the respondents tracked pitch counts or self-reported guideline adherence did not show an association with pain or fatigue. Backward stepwise logistic regression found that arm fatigue (p = 0.001), older age (p = 0.025), parent/coach frustration with play (p = 0.001) and months played (p = 0.023) were independently associated with arm pain in this investigation.
Another aspect of the survey analyzed familiarity of families with current pitch count guidelines. Families answered “Yes” to being familiar with the pitch count guidelines in 58.9% of surveys. According to the survey, pitch counts were largely tracked by coaches (66.3%), next by parents (25.3%), next by “other” (10.3%), and lastly, by the player (5.5%). Survey responders reported interest in using a free mobile app for tracking pitches if it were available in 41% of surveys.
4. Discussion
In this study, the primary factors that were predictive of arm pain were player age and arm fatigue. There was also found to be an association between arm pain and frustration from coaches and/or parents which alludes to a psychosocial effect on performance and participation in this population. There are multiple risk factors that have been associated with dominant arm injury; the strongest association being overuse.9,10 A retrospective study of 140 pitchers found averaging greater than 80 pitches per game, pitching competitively for 8 months or more per year, or pitching while fatigued, all independently increased the odds of surgery.11 In another study, 476 pitchers (Age 9–14) were followed for one full season, and demonstrated an increased risk of elbow and shoulder pain with a higher number of pitches per game and per season.8 Two studies have found pitcher and catcher player positions as risk factors associated with the development of arm pain.12,13
These results contrasted with those of Mahkni et al., who found that a majority of youth overhead throwing athletes in New York and New Jersey (cold climate) experienced some arm pain during competition and there was a definitive psychosocial impact on performance, enjoyment and frustration from their adult peers.8 In this study, 203 youth baseball players (average age of 15.2 years) were surveyed. Many responders (74%) said they had arm pain while throwing, with 80% of players describing pain the day after throwing and 82% of players responding that they had arm fatigue during a game or practice. The findings of our study were more consistent with Lyman et al., who reported shoulder pain by 32% of pitchers and elbow pain by 25.5% of pitchers (average age 10.8 years).1
Possible explanations for the major difference in percentage of players with arm pain in Mahkni's study may be the older population or the setting of data collection, since surveys were obtained during competitive summer league play. As older players mature, they accumulate increased microtrauma and apply higher stress across the joint which may lead to a higher propensity for injury. In addition, the Mahkni study patient population included highly competitive players participating in summer league while the present study was conducted at general pediatric offices throughout coastal South Carolina. These subjects may not have been as highly competitive in sport compared to the Mahkni subjects. The data from the present study was more characteristic to the general youth baseball population similar to the surveys conducted in Japan that revealed similar rates of arm pain.14,15 From a survey of 1563 youth Japanese players, the prevalence of shoulder pain and elbow pain in the throwing arm occurred in 15.9% and 29.2% of players respectively. Shoulder pain was associated with increasing age and elbow pain was associated with increased age, increased years of baseball experience and playing catcher.15 A retrospective cohort study among 8354 elementary school baseball players in Japan discovered 18% of males and 9% of females had shoulder and elbow pain over the past year.14
Our study found that arm fatigue was associated with arm pain, supporting prior findings in the literature. Many experienced sports medicine professionals believe that shoulder or elbow pain in young overhead athletes serve as a warning sign for the future development of overuse injury.10 Overuse is a significant risk factor for the development of throwing arm injury. Fleisig et al. followed 481 young pitchers for 10 years and determined that the most significant risk factor for undergoing surgery among adolescent overhead athletes was pitching more than 100 innings in a single season.5 12 Olsen et al. surveyed adolescent pitchers who underwent shoulder/elbow surgery and compared then with a control group of pitchers who never had surgery. Pitchers who underwent surgery pitched more months per year, games per year, innings per game, pitches per game and warm up pitches before games.11
The warm weather climate of South Carolina has an advantage for player development but also places these pitchers at higher risk of arm injury secondary to increase time spent in participation. Erickson et al. demonstrated a higher proportion of pitchers who underwent UCL reconstruction were from warm weather climates (2.2% [95% CI, 1.9%–2.6%] compared to cold weather areas 0.94% [95%CI, 0.78%–1.1%] (p < 0.0001).7 In addition the timing of surgery among pitchers from warm weather climates was at a younger age and earlier in their MLB careers, suggestive of possible increased microtrauma due to year round competition. We expected this cohort of survey responders to be participating in sport for greater than 6 months out of the year. However, our youth participants demonstrated a wide variability in amount of play. This again may be representative of the setting in which the surveys were obtained and therefore the youth athletes that were chosen may not be participating in more competitive leagues. The average age of players (11.6) may also be a reason why this cohort of players did not play baseball more months of the year. Generally, as players progress beyond little league, showcase tournaments and highly competitive travel teams begin to form.
Another important aspect of this survey was assessing awareness of the recommended guidelines that were established to maximize longevity and arm durability of youth baseball players. Despite significant efforts in education about the development of arm injuries and growing incidence of surgical intervention for young pitchers, knowledge of current recommendations remains poor. A majority of families (58.8%) indicated familiarity with USA Baseball Medical and Safety Advisory Committee Pitch Limit Guidelines. Our survey did not delve into specific detail regarding the degree of understanding of the guidelines but it is likely that significantly fewer could demonstrate accurate understanding of the guidelines.
Fazarale et al. found that among youth baseball coaches, only 43% of their questions regarding pitch count and rest periods were answered correctly.16 In our survey, 66.3% of families acknowledged coaches as the primary trackers of pitch count data. Our study also found an association with coach's frustration and arm pain. This demonstrates that continued education must be provided to the youth coaches regarding appropriate pitch counting which will ideally provide better arm care among these young athletes. Additionally, there seems to be a psychological association of arm pain and coach frustration which further places importance on coach education and emphasis on the player-coach relationship. Furthermore, parents were shown to be tracking their kids pitch counts 25% of the time. Therefore, the education of pitch count compliance must be delivered to all who are involved in youth baseball. Useful tools such as pitch count tracker mobile apps or other easily accessible methods may serve as helpful resources for monitoring overhead athletes for overuse injuries.
A limitation of this study was that data collection occurred during a pediatric clinic appointment rather than an on-site baseball setting, which may result in recall bias. Our study team believed that obtaining data from a network of primary care pediatric practices rather than a sports clinic/league will collect data from a wider population and will represent the general pediatric population. This data collection method explains why the frequency of arm pain reported may be less than the frequency reported in a survey from a competitive, in-season youth league. This is a commonly found phenomenon when comparing primary care population with referral/specialist population. This study may be prone to selection bias due to the method of recruiting players/parents to participate in the study as these families were likely to be more invested in the sport of interest. In addition, some families may have refused to participate for many reasons.
Parents' perception may result in over reporting or underreporting of injury history and psychosocial elements, since it is dependent on the youth to report pain to the parent. However, in the data collection process, the parent and child were together when the survey was completed which may have minimized this effect. There was no information obtained regarding the competitiveness of the leagues participating in or amount of participation as well. As a result, it is unclear whether our results will be generalizable to other regions or are representative of youth baseball.
There may be flaws in some questions in the survey as well. The original survey design required standardization of questions that may not be applicable to the wider general pediatric population. Survey questions can offer options that lead participants to interpret the answers differently. The discrepancy of “rare” versus “sometimes” or “sometimes” versus “often” can be translated differently among different responders. However, the survey that was used in this study was adapted from a prior published study as mentioned previously.
5. Conclusion
Arm pain remains prevalent among the South Carolina youth baseball/softball community, and worse in pitchers or players that experience frequent fatigue and are older. These factors corroborate the assumption that overuse is an underlying risk factor for shoulder and elbow injuries. Simple screening questionnaires or better communication between players, parents, and coaches may help identify players who are at risk for overuse injury. In addition, understanding and awareness of pitch count guidelines remains limited. A comprehensive and all-inclusive approach in education of the USA Baseball Medical and Safety Advisory Guidelines will be the best method in limiting the risk for upper extremity pain and injury. This survey provides preliminary data to assess the need for an intervention device such as a mobile app or easily accessible website to help disseminate knowledge on pitch count guidelines. More research is required to elucidate the enforcement and effectiveness of pitching limits, and more awareness on the subject can improve injury prevention and comfort on the field.
Declaration of competing interest
Josef K. Eichinger MD, J. Brett Goodloe MD, Jackie J. Lin BS, Alyssa Greenhouse BS, Meghana Rao BS, Richard J. Friedman MD, James J. Roberts MD declare that they have no conflict of interest related to this submission. None of the authors listed above received any payments or services from any third parties during the completion of this research. There are no financial relationships associated with this submission. There are no patents planned or pending in regards to this work.
References
- 1.Lyman S., Fleisig G.S., Waterbor J.W. Longitudinal study of elbow and shoulder pain in youth baseball pitchers. Med Sci Sports Exerc. 2001 Nov;33(11):1803–1810. doi: 10.1097/00005768-200111000-00002. Epub 2001/11/02. [DOI] [PubMed] [Google Scholar]
- 2.Danis R.P. Injuries in youth baseball. J Am Med Assoc. 2003 Jul 9;290(2):194. doi: 10.1001/jama.290.2.194-a. author reply -5. Epub 2003/07/10. [DOI] [PubMed] [Google Scholar]
- 3.Ray T.R. Youth baseball injuries: recognition, treatment, and prevention. Curr Sports Med Rep. 2010 Sep-Oct;9(5):294–298. doi: 10.1249/JSR.0b013e3181f27403. Epub 2010/09/10. [DOI] [PubMed] [Google Scholar]
- 4.Andrews J.R. How many pitches should I allow my child to throw? USA Baseb. News. 1996 1996. [Google Scholar]
- 5.Fleisig G.S., Kingsley D.S., Loftice J.W. Kinetic comparison among the fastball, curveball, change-up, and slider in collegiate baseball pitchers. Am J Sports Med. 2006 Mar;34(3):423–430. doi: 10.1177/0363546505280431. Epub 2005/11/02. [DOI] [PubMed] [Google Scholar]
- 6.Kaplan K.M., Elattrache N.S., Jobe F.W., Morrey B.F., Kaufman K.R., Hurd W.J. Comparison of shoulder range of motion, strength, and playing time in uninjured high school baseball pitchers who reside in warm- and cold-weather climates. Am J Sports Med. 2011 Feb;39(2):320–328. doi: 10.1177/0363546510382230. Epub 2010/11/06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Erickson B.J., Harris J.D., Tetreault M., Bush-Joseph C., Cohen M., Romeo A.A. Is tommy john surgery performed more frequently in major league baseball pitchers from warm weather areas? Orthop. J. Sports Med. 2014 Oct;2(10) doi: 10.1177/2325967114553916. 2325967114553916. Epub 2015/11/05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Makhni E.C., Morrow Z.S., Luchetti T.J. Arm pain in youth baseball players: a survey of healthy players. Am J Sports Med. 2015 Jan;43(1):41–46. doi: 10.1177/0363546514555506. Epub 2014/11/05. [DOI] [PubMed] [Google Scholar]
- 9.Fleisig G.S., Andrews J.R. Prevention of elbow injuries in youth baseball pitchers. Sport Health. 2012 Sep;4(5):419–424. doi: 10.1177/1941738112454828. Epub 2012/09/28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lyman S., Fleisig G.S., Andrews J.R., Osinski E.D. Effect of pitch type, pitch count, and pitching mechanics on risk of elbow and shoulder pain in youth baseball pitchers. Am J Sports Med. 2002 Jul-Aug;30(4):463–468. doi: 10.1177/03635465020300040201. Epub 2002/07/20. [DOI] [PubMed] [Google Scholar]
- 11.Olsen S.J., 2nd, Fleisig G.S., Dun S., Loftice J., Andrews J.R. Risk factors for shoulder and elbow injuries in adolescent baseball pitchers. Am J Sports Med. 2006 Jun;34(6):905–912. doi: 10.1177/0363546505284188. Epub 2006/02/03. [DOI] [PubMed] [Google Scholar]
- 12.Fleisig G.S., Andrews J.R., Cutter G.R. Risk of serious injury for young baseball pitchers: a 10-year prospective study. Am J Sports Med. 2011 Feb;39(2):253–257. doi: 10.1177/0363546510384224. Epub 2010/11/26. [DOI] [PubMed] [Google Scholar]
- 13.Matsuura T., Suzue N., Kashiwaguchi S., Arisawa K., Yasui N. Elbow injuries in youth baseball players without prior elbow pain: a 1-year prospective study. Orthop. J. Sports Med. 2013 Oct;1(5) doi: 10.1177/2325967113509948. 2325967113509948. Epub 2013/10/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Takagishi K., Matsuura T., Masatomi T. Shoulder and elbow pain in elementary school baseball players: the results from a nation-wide survey in Japan. J Orthop Sci. 2017 Jul;22(4):682–686. doi: 10.1016/j.jos.2017.03.016. Epub 2017/05/10. [DOI] [PubMed] [Google Scholar]
- 15.Matsuura T., Suzue N., Iwame T., Arisawa K., Fukuta S., Sairyo K. Epidemiology of shoulder and elbow pain in youth baseball players. Phys. Sportsmed. 2016;44(2):97–100. doi: 10.1080/00913847.2016.1149422. Epub 2016/02/03. [DOI] [PubMed] [Google Scholar]
- 16.Fazarale J.J., Magnussen R.A., Pedroza A.D., Kaeding C.C., Best T.M., Classie J. Knowledge of and compliance with pitch count recommendations: a survey of youth baseball coaches. Sport Health. 2012 May;4(3):202–204. doi: 10.1177/1941738111435632. Epub 2012/09/28. [DOI] [PMC free article] [PubMed] [Google Scholar]