Abstract
Background:
Preventable hospital readmissions are costly and erode the quality of care delivery. Few efforts to incorporate the patient perspectives and social factors associated with readmission preventability exist.
Objective:
To identify patient perceptions and social barriers to care related to readmission.
Methods:
Prospective cohort study of 202 respondents readmitted within 30 days of hospital discharge from 2 inpatient adult medicine units at Massachusetts General Hospital, Boston, Massachusetts between January 2012 and January 2016.
Results:
Few participants indicated that their readmission was due to unattainable health care after discharge. Almost half indicated that they needed more general assistance to stay well outside the hospital. Those reporting a barrier related to at least 2 measures of social determinants of health were more likely to have preventable readmissions (34% vs 17%, P = .006). Participants with a history of homelessness or substance use disorder were more likely to have preventable readmissions (44% vs 20%, P = .04 and 32% vs 18%, P = .03, respectively).
Conclusion:
Strengthening nonmedical support systems and general social policy may be required to reduce preventable readmissions.
Keywords: patient perspectives, readmissions, hospital medicine, social determinants of health, readmission preventability
Introduction
The rising cost of hospital readmissions has garnered increasing attention from clinical, health policy, and process experts alike. Despite ongoing efforts, hospital readmissions contribute to disruptive and fractured care delivery (1) and continue to be associated with a significant proportion of health-care costs. In 2014, 18% of US hospital admissions covered by Medicare resulted in a 30-day readmission (2). This was associated with over US $15 billion in health-care costs (2). Up to 27% of these readmissions are classified as preventable. As the Centers for Medicare and Medicaid services defined quality indicator, health systems are accountable for rates of 30-day readmission as well as the financial penalties incurred for elevated rates of readmissions (3). Health-care systems have made significant investments in programming and services such as case management and home nursing to prevent readmission.
Ongoing efforts to understand key drivers of readmission, readmission preventability, and effective readmission reduction strategies continue (4 –7), yet unifying reasons for persistent elevation in 30-day readmission remain elusive. Relatively few studies have incorporated the patient perspective by asking patients to identify reasons for their own readmissions (8 –11) or examined patient perspectives on reasons for readmission within the context of clinical, demographic, and social characteristics (1,12,13).
To better understand patient perceptions of reasons for hospital readmission, we interviewed general medical patients readmitted within 30 days of discharge over a 4-year period. We hypothesized that having a better understanding of the challenges patients face after leaving the hospital may help identify the postdischarge factors that contribute to preventable readmissions. We queried a wide range of potential factors including inability to carry out or understand clinical discharge plans, challenges with access to health care, perceived challenges to staying healthy, availability of additional help to stay healthy outside the hospital, and social determinants of health (SDoH) including safe housing, food access, and economic stability.
Methods
Study Population and Setting
The population consisted of individuals readmitted to Massachusetts General Hospital (MGH), a near 1000-bed academic medical center in Boston, within 30 days of being admitted to one of 2 inpatient general medical units at the MGH between January 2012 and January 2016. Participants eligible for the study were >18 years of age, had capacity to complete the questionnaire, and spoke English (Table 1). Methods and results from the index admission survey have been reported previously (14). Patients were excluded if they had not been interviewed at the time of index admission or their readmission was planned. The 2 inpatient units included medical patients with similar distributions of insurance coverage and medical conditions. Readmissions among study participants were identified by daily surveillance of the census on both units. Efforts to interview all eligible readmitted participants were made, but for practical reasons (including research coordinator staffing limitations and patient transfer/discharge timing), not all readmitted participants were able to be interviewed prior to discharge. The institutional review board at the Partners HealthCare approved the study.
Table 1.
Patient Characteristics.a
| Patient Characteristics, n (%) or mean (SD) | Preventable Readmission Status | P Value | ||
|---|---|---|---|---|
| Total (N = 202) | Preventable (n = 46; % = 23) | Not Preventable (n = 156; % = 77) | ||
| Gender | ||||
| Male | 124 (61.4) | 27 (21.8) | 97 (78.2) | .67 |
| Female | 78 (38.6) | 19 (24.4) | 59 (75.6) | |
| Age, mean (SD) | 62.0 (15.7) | 60.0 (11.5) | 62.6 (16.8) | .31 |
| Race | ||||
| White | 174 (86.1) | 37 (21.2) | 137 (78.8) | .21 |
| Non-white | 28 (13.9) | 9 (32.1) | 19 (67.9) | |
| Hispanic | ||||
| Yes | 11 (5.4) | 2 (18.2) | 9 (81.8) | .71 |
| No | 191 (94.6) | 44 (23.0) | 147 (77.0) | |
| Education | ||||
| More than high school/GED | 89 (44.1) | 20 (22.5) | 69 (77.5) | .93 |
| Less or equal to high school/GED | 113 (55.9) | 26 (23.0) | 87 (77.0) | |
| Insurance | ||||
| Commercial | 61 (30.2) | 11 (18.0) | 50 (82.0) | .29 |
| Public/self/uninsured | 141 (69.8) | 35 (24.8) | 106 (75.2) | |
| English is primary language | ||||
| Yes | 6 (3.0) | 2 (33.3) | 4 (66.7) | .53 |
| No | 196 (97.0) | 44 (22.4) | 152 (77.6) | |
| Homeless in the last year | ||||
| Yes | 16 (7.9) | 7 (43.8) | 9 (56.2) | .04 |
| No | 186 (92.1) | 39 (21.0) | 147 (79.0) | |
| Substance use disorder | ||||
| Yes | 58 (28.7) | 19 (32.8) | 39 (67.2) | .03 |
| No | 144 (71.3) | 27 (18.8) | 117 (81.2) | |
| Marital status | ||||
| Married | 68 (33.7) | 13 (19.1) | 55 (80.9) | .38 |
| Not married | 134 (66.3) | 33 (24.6) | 101 (75.4) | |
| Need assistance or cannot do 2 or more ADLs | ||||
| Yes | 94 (46.5) | 18 (19.1) | 76 (80.9) | .25 |
| No | 108 (53.5) | 28 (26.0) | 80 (74.0) | |
| Problem with at least 2 SDOH | ||||
| Yes | 67 (33.2) | 23 (34.4) | 44 (65.7) | .006 |
| No | 135 (66.8) | 23 (17.0) | 112 (83.0) | |
Abbreviations: ADLs, activities of daily livings; GED, General Education Development; SDoH, social determinants of health.
a Presented as n (%) unless otherwise stated.
Sources of Data
Survey Development
Patient response data were drawn from interviewer-administered questionnaires conducted after obtaining informed consent from eligible patients during readmission. The patient questionnaire was developed by study investigators for interviewer-assisted administration with hospitalized patients. A qualitative process was used to identify core domains through key informant interviews with patients, community-based primary care providers, and post-acute care providers. This was supplemented by review of the literature on hospital patient experience and consultations with experts in survey and health services research. For benchmarking, we included some standard established patient experience measures from the Hospital Consumer Assessment of Healthcare Providers and Systems (15). Draft questionnaires were pretested with 5 patients and revised prior to study administration. The final readmission questionnaire included 30 items which are listed in Table 2. Trained research coordinators interviewed patients and verbally administered questionnaires as close as possible to hospital day 1 to 2 of readmission. Readmission questionnaires took at least 10 minutes to complete. Patient responses were recorded and stored in a secure online database (REDCap version 8.1.20 copyright 2018 Vanderbilt University) (16).
Table 2.
Readmission Questionnaire Results.a
| Patient Perceptions of Factors Related to Readmission | n (%) |
|---|---|
| Since you left the hospital, was there health care or medical help that you needed and could not get? | |
| No | 174 (86.1) |
| Unsure | 6 (3.0) |
| Yes | 22 (10.9) |
| Old symptoms getting worse | |
| Not important | 37 (18.3) |
| Somewhat important | 24 (11.9) |
| Unsure | 5 (2.5) |
| Very important | 131 (64.9) |
| New symptoms | |
| Not important | 80 (39.6) |
| Somewhat important | 20 (9.9) |
| Unsure | 4 (2.0) |
| Very important | 92 (45.5) |
| Trouble understanding how to take medications | |
| Not important | 179 (88.6) |
| Somewhat important | 10 (4.5) |
| Unsure | 0 (0) |
| Very important | 9 (4.5) |
| Trouble getting medications | |
| Not important | 167 (82.7) |
| Somewhat important | 16 (7.9) |
| Unsure | 0 (0) |
| Very important | 15 (7.4) |
| Trouble understanding what you were supposed to do to take care of yourself | |
| Not important | 177 (87.6) |
| Somewhat important | 7 (3.5) |
| Unsure | 1 (0.5) |
| Very important | 15 (7.4) |
| Trouble getting a primary care provider appointment | |
| Not important | 171 (84.7) |
| Somewhat important | 13 (6.4) |
| Unsure | 1 (0.5) |
| Very important | 14 (6.9) |
| Trouble getting a specialist appointment (kidney, heart, neurology doctor) | |
| Not important | 169 (83.7) |
| Somewhat important | 12 (5.9) |
| Unsure | 1 (0.5) |
| Very important | 15 (7.4) |
| Trouble with transportation to a clinic appointment or pharmacy | |
| Not important | 158 (78.2) |
| Somewhat important | 21 (10.4) |
| Unsure | 2 (1.0) |
| Very important | 18 (8.9) |
| During your previous hospitalization, how often did staff take your wishes into account in deciding what you would need when you left the hospital? | |
| Never | 7 (3.5) |
| Sometimes | 22 (10.9) |
| Usually | 36 (17.8) |
| Always | 130 (64.4) |
| NA | 6 (3.0) |
| During your previous hospitalization, how often did staff take the wishes of your caregivers into account in deciding what you would need when you left the hospital? | |
| Never | 10 (5.0) |
| Sometimes | 13 (6.4) |
| Usually | 30 (14.9) |
| Always | 112 (55.5) |
| NA | 35 (17.3) |
| After I left the hospital, I had a good understanding how to manage my health after I left the hospital. | |
| Strongly disagree | 1 (0.5) |
| Disagree | 11 (5.5) |
| Agree | 50 (24.8) |
| Strongly agree | 135 (66.8) |
| NA | 2 (1.0) |
| After I left the hospital, I clearly understood how to take my medications. | |
| Strongly disagree | 2 (1.0) |
| Disagree | 6 (3.0) |
| Agree | 40 (19.8) |
| Strongly agree | 152 (75.3) |
| NA | 0 (0) |
| Do you live: | |
| Alone in your own house, apartment | 56 (27.7) |
| With family or friends in your own home | 83 (41.1) |
| With family or friend in their home | 29 (14.4) |
| In an elderly housing or retirement community | 2 (1.0) |
| In a group home or boarding home with some assistance from professionals | 5 (2.5) |
| In an assisted living facility | 8 (4.0) |
| In a nursing home | 5 (2.5) |
| Do you have any of the following problems? | |
| Had to move because of health or medical problems | 29 (14.4) |
| Had trouble finding or keeping your job because of health or medical problems | 49 (24.3) |
| Had problems in your family | 31 (15.4) |
| Accident, injury, or fall | 48 (23.8) |
| Worried about being alone | 32 (15.8) |
| Problems knowing who to call if I need help | 14 (6.9) |
| SDOH: In the past year, have you had any problem having enough money to | |
| Buy food | 48 (23.8) |
| Buy clothing | 48 (23.8) |
| Pay rent, mortgage, or housing costs | 57 (28.2) |
| Pay medical bills (doctors, hospitals) | 39 (19.3) |
| Pay for prescription drugs | 40 (19.8) |
| Pay for medical equipment or supplies | 28 (13.9) |
| Pay for health-care services you need at home | 19 (9.4) |
| Do doctors or nurses ever ask you whether you need help to do these things? | |
| No | 117 (57.9) |
| Unsure | 16 (7.9) |
| Yes | 69 (34.2) |
| Prepare meals | |
| I can do this without assistance | 128 (63.4) |
| I can do this with assistance | 41 (20.3) |
| I cannot do this | 21 (10.4) |
| Does not apply | 11 (5.5) |
| Bathe or shower | |
| I can do this without assistance | 146 (72.3) |
| I can do this with assistance | 48 (23.8) |
| I cannot do this | 7 (3.5) |
| Does not apply | 1 (0.5) |
| Use the toilet | |
| I can do this without assistance | 162 (80.2) |
| I can do this with assistance | 32 (15.8) |
| I cannot do this | 6 (3.0) |
| Does not apply | 1 (0.5) |
| Get dressed | |
| I can do this without assistance | 163 (80.7) |
| I can do this with assistance | 34 (16.8) |
| I cannot do this | 4 (2.0) |
| Does not apply | 1 (0.5) |
| Eat | |
| I can do this without assistance | 180 (89.1) |
| I can do this with assistance | 13 (6.4) |
| I cannot do this | 5 (2.5) |
| Does not apply | 2 (1.0) |
| Get in and out of bed and chairs | |
| I can do this without assistance | 151 (74.8) |
| I can do this with assistance | 43 (21.3) |
| I cannot do this | 6 (3.0) |
| Does not apply | 1 (0.5) |
| Shopping and errands | |
| I can do this without assistance | 109 (54.0) |
| I can do this with assistance | 54 (26.7) |
| I cannot do this | 27 (13.4) |
| Does not apply | 11 (5.5) |
| Scheduling appointments | |
| I can do this without assistance | 157 (77.7) |
| I can do this with assistance | 23 (11.4) |
| I cannot do this | 10 (5.0) |
| Does not apply | 12 (5.9) |
| Paying bills | |
| I can do this without assistance | 148 (73.3) |
| I can do this with assistance | 32 (15.8) |
| I cannot do this | 9 (4.5) |
| Does not apply | 13 (6.4) |
| Manage medications and take them on schedule | |
| I can do this without assistance | 152 (75.3) |
| I can do this with assistance | 34 (16.8) |
| I cannot do this | 9 (4.5) |
| Does not apply | 6 (3.0) |
| Arranging transportation to appointments | |
| I can do this without assistance | 139 (68.8) |
| I can do this with assistance | 44 (21.8) |
| I cannot do this | 9 (4.5) |
| Does not apply | 4 (2.0) |
| Is there one person who is a family member or friend who does the most to help you manage your health care, medications, and other needs? | |
| No | 44 (21.7) |
| Unsure | 3 (1.5) |
| Yes | 154 (76.2) |
| Do you feel you need more assistance stay to well without needing to come to the hospital? | |
| No | 109 (54.0) |
| Unsure | 10 (5.0) |
| Yes | 79 (39.1) |
Abbreviation: SDoH, social determinants of health.
a Percent missing data ranged from 0% to 3%.
Questionnaire response domains queried the ability to carry out or understand discharge details, challenges with access to care, perceived challenges to staying healthy, and whether or not additional help to stay healthy outside the hospital was needed. We also asked respondents about whether they were having a problem paying for or buying any of the following: (a) food, (b) clothing, (c) rent, mortgage, or housing costs, (d) medical bills, (e) prescription drugs, (f) medical equipment, and (g) at-home health-care services. Demographic covariates included gender, age, race, ethnicity, marital status, education, primary language spoken, needing assistance with at least 2 activities of daily living (ADLs), and history of homelessness or a substance use disorder. We examined the proportion of individuals that fell into each response category. Readmission responses are detailed in the Table 2. The full questionnaire is available in an online appendix.
Clinical Data Repository/Case Review and Estimation of Cause and Preventability
In addition to patient-reported data, research coordinators completed a structured medical record review to obtain clinical history using the electronic medical record with data captured in the same REDCap database. Abstracted data included insurance status, education, primary diagnosis associated with readmission, and major medical and psychiatric comorbidities.
Both chart review and patient interview responses were used by our team to determine and classify underlying or precipitating causes of readmission as “preventable” or “not preventable.” We relied on a number of chart review and patient interview responses (including barriers to care related to medications, worsening of a known previous medical problem, onset of a new previous medical problem, access to their clinical team, understanding how best to take care of themselves, knowing who to call for questions, need for discharge to a different care setting, etc). We also used chart review for several types of clinical indicators (eg, symptoms, problem list, laboratory, and imaging reports). Responses to survey questions related to ADLs, home environment, or fulfillment of basic needs were not used. No other patient characteristic or demographic data were included as a part of the preventability determination.
Research coordinators were trained to recognize clinical and health-care system-related causes for readmission. “Health system–related” causes included barriers to getting/affording medications, access to clinic appointments, or transportation to appointments. If clinical reasons for readmission were paired with a preventable reason for admission reported by the patient, such as being unable to afford or fill a medication or access timely outpatient evaluation, the admission was considered “preventable.” If clinical reasons for readmission were not associated with self-reported health system–related reasons for readmission, the admission was considered “not preventable.” In cases where a health-care system-related cause for readmission was suspected but unclear (eg, cases where scheduling a simple postdischarge lab check or postdischarge primary care provider/specialist visit would have likely identified the need for adjustment of the clinical care plan), the admission was identified as probably preventable and categorized as preventable. All cases and preventability determinations were reviewed as a part of a bimonthly research team meeting that included the principle investigator and lead research coordinators prior to making a final assessment.
Statistical Analysis Plan
The primary outcome was preventable hospital readmission. Patient characteristics that were considered covariates included gender, age, race, ethnicity, marital status, education, insurance status, primary language spoken, needing assistance with at least 2 ADLs, and history of homelessness or a substance use disorder.
Bivariable analyses, using Pearson χ2 test for categorical variables and the Student t test for continuous variables, were performed to assess differences between preventable and nonpreventable readmission groups on all covariates. Associations between preventable readmission status and covariates of interest were assessed using a multivariable logistic regression model where race, SDoH, homelessness, and drug/alcohol abuse were included as independent variables, which all had bivariable P values <.25. A P value of <.05 was considered statistically significant. The proportion of missing data was assessed for random missingness at values <5%; the rate of missing data for all variables was 0%. All analyses were performed using SAS software version 9.4 (SAS Institute, Cary, North Carolina).
Results
Participant Characteristics
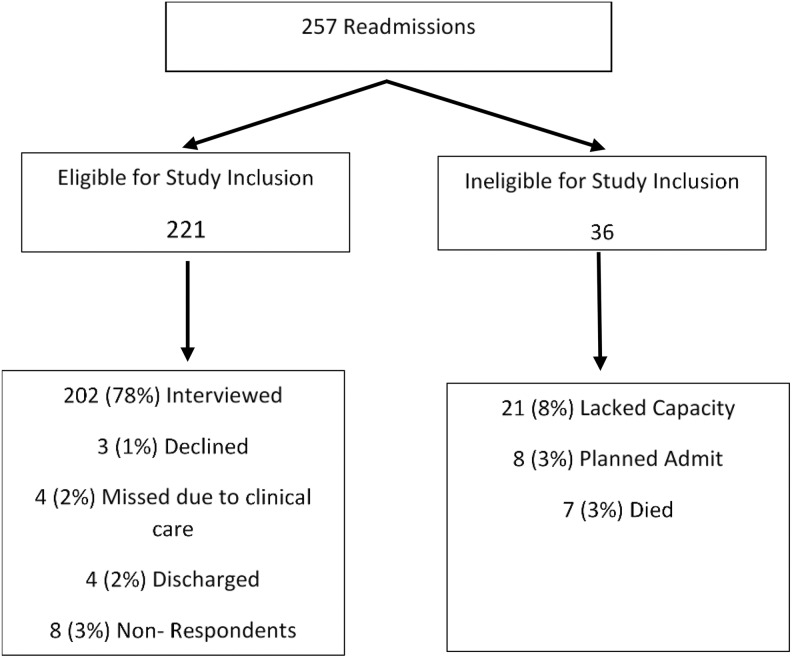
Two hundred two unique respondents readmitted within 30 days of a prior MGH admission to one of 2 preidentified internal medicine study units were interviewed during readmission, with a response rate of 79% of all enrolled patients readmitted within 30 days of index admission (Figure 1). Respondent characteristics are reported in Table 1 (16). Male respondents were 62% of the cohort. The majority of respondents were 55 years of age or older (67.3%) and identified themselves as white (86.1%). Of the respondents, 44% graduated from high school or higher level of education.
Figure 1.
Enrollment strategy.
Readmission Survey Results
Patient perceptions of reasons for hospital readmission are described in Table 2. Of the 202 respondents, 86.1% indicated that there was no specific medical care that they needed but could not obtain after being discharged (Table 2). A minority of participants (14%) cited the lack of an isolated health-care service-related reason for readmission as “very important.” Medical barriers included not being able to get an appointment with their primary care provider (6.9%), not being able to see a specialty doctor (7.4%), trouble with transportation (8.9%), trouble getting medications (7.4%), trouble understanding how to take medications (4.5%), or trouble understanding what to do to take care of themselves (7.4%). A need for more general (nonmedical) assistance to stay well outside the hospital was reported by 39.1% of respondents who cited reasons for readmission like being unable to obtain prescription medications due to financial costs or needing more help with ADLs.
Preventable Hospital Readmission Analysis
Out of 202 participants readmitted within 30 days of discharge, 46 (22.8%) had a preventable readmission (Table 1). There were a number of patterns of preventability associated with specific patient perspectives or demographics. Those with a history of homelessness within 12 months of enrollment were more likely to have a preventable 30-day readmission as compared to those respondents with no history of homelessness in the last year (44% vs 20%, P = .04). Also, respondents with a history of substance use disorder were more likely to have a preventable 30-day readmission than those respondents without a history of substance use disorder (32% vs 18%, P = .03). In addition, respondents identifying at least 2 unmet needs related to SDoH were more likely to have a preventable 30-day readmission as compared to all other survey respondents without at least 2 unmet SDoH-related needs (34% vs 17%, P = .006).
Crude and adjusted odds ratios (ORs) of preventable readmissions were also generated with the use of multivariable logistic regression (Table 3). In the unadjusted analyses, we found that those who reported being homeless in the last year (OR = 2.93, 95% confidence interval [CI]: 1.03-8.37), had a history of substance use disorder (OR = 2.11; 95% CI: 1.06-4.21), or had barriers due to at least 2 measures of SDoH (OR = 2.55; 95% CI: 1.30-5.00) had a higher odds of having a preventable readmission. In the analysis adjusted for race, SDoH, homelessness, and substance use disorder history, we found that those with at least 2 unmet SDoH needs had 2.09 times higher odds of having a preventable readmission (95% CI: 1.03-4.25) as compared to those without at least 2 unmet SDoH needs.
Table 3.
Crude and Adjusted Odds Ratios (95% Confidence Intervals) of Preventable Readmissions.
| Covariate | Crude OR (95% CI) | Adjusted OR (95% CI)a |
|---|---|---|
| Race | ||
| White | Ref | Ref |
| Non-white | 1.75 (0.73-4.19) | 1.70 (0.68-4.23) |
| Homeless in the last year | ||
| No | Ref | Ref |
| Yes | 2.93 (1.03-8.37)a | 1.76 (0.54-5.70) |
| Substance use disorder history | ||
| No | Ref | Ref |
| Yes | 2.11 (1.06-4.21)a | 1.58 (0.72-3.49) |
| Problem with at least 2 SDOHs | ||
| No | Ref | Ref |
| Yes | 2.55 (1.30-5.00)a | 2.09 (1.03-4.25)b |
Abbreviation: SDoH, social determinants of health.
a Adjusted logistic regression models included race, social determinants of heath, homelessness, and substance use disorder history as predictors.
b P < .05.
Discussion
This study identified novel factors associated with readmission risk and preventability by querying patient perspectives on barriers to care after index admission. Only 14% of patients reported being unable to access a medical service in association with preventable readmission. Rather, our findings demonstrated higher proportions of participants citing reasons for readmission related to nonmedical factors. We also noted increased risk of preventable readmissions associated with a history of homelessness, substance use disorder, or at least 2 unmet SDoH-related needs (Table 1). In the unadjusted analysis of a model generated by multivariate logistic regression, we found that substance use disorder, homelessness, or having 2 or more unmet needs related to SDoH (such as difficulty paying for food, clothing, or housing) conferred more than twice the odds of having a preventable readmission compared to a nonpreventable readmission (Table 3). Furthermore, in the adjusted analysis, those with at least 2 unmet SDoH needs were almost 3 times more likely to have a preventable readmission rather than a nonpreventable readmission.
These data underline important vulnerabilities and reflect the growing complexity and evolving scope of current medical practice. At least 2 of the 3 categories identified as associated with preventable readmissions could potentially be targeted for intervention. For example, for those respondents affected by homelessness, having sustainable, safe housing would remove vulnerabilities driven by marginal housing that contribute to hospital readmission risk. Similarly, for those respondents affected by 2 or more factors related to SDoH, improved general social assistance rather than medical assistance may impact readmission rates.
While these solutions may lie outside what is considered to be strict medical care, emerging studies have demonstrated a strong relationship between social support investment and health-care outcomes. Works published by Bradley et al and Thorpe et al clearly demonstrate a relationship between countries with higher levels of social support investment (including education, housing, mental health, etc) and lower health-care costs (17 –19). This is in contrast to US spending patterns which have proportionately less social service investment and substantially higher health-care costs, in both absolute and relative terms. These data support the hypothesis that the preemptive, year-to-year investment in social services not only serves to improve medical issues related to SDoH but also ensures that whatever health-care resources are administered have a greater impact. Seen through this lens, the mandate to generate higher health-care quality at lower cost may not be achievable without addressing social needs more fully.
There are many studies emphasizing the association between health-care utilization and factors associated with substance use, housing stability, and SDoH (20 –26). We found increased risk of preventable readmission in respondents with substance use disorder, homelessness, and 2 or more unmet needs related to SDoH compared to all respondents. However, limited studies have been performed focused on these characteristics as they relate to readmission preventability (2,27). We did identify a single study published by Goldfield et al with increased rates of preventable readmission in patients with substance use disorder (26). There is significant variation in documented contribution of clinical versus system-related barriers to care seen in other readmission studies (2,14).
Patient surveys about barriers to staying well after admission have not been widely documented in readmission literature. Outside of work performed by Misky et al and Kangovi et al in studies focused on the association of socioeconomic status or Medicaid insurance with patient perspectives on readmission (14,15), we are unaware of any previous studies that include patient perspectives on specific challenges to staying well after discharge.
There are several limitations to this study. It was not possible to track readmissions to other health systems, which may have resulted in an underestimation of readmission rate. The fact that this study was conducted on a single medical service among English-speaking patients also limits the generalizability of our findings. Our analysis included a small number of readmissions (202), with only 23% being identified as being preventable, which limited our power to detect weaker correlates of readmission. Our methods for classifying preventability relied on an approach used by Auerbach et al (1). While there is no “gold standard” for preventability assessment, a tested, reliable, and reproducible measure should be a goal of future research in this domain. Given the trends noted in differences between preventable and nonpreventable readmissions in a number of the covariate categories (including race, education, insurance coverage, marital status, and ADL deficits), we believe that if repeated with larger numbers of participants, this study would have been adequately powered to detect additional statistically significant correlates of preventable readmissions.
We believe that these limitations are outweighed by the quality of the open-ended patient response data describing barriers to maintaining health after discharge. Additional studies are needed to consider both preadmission/ postadmission application of a more robust network of linked interventions and services. This network of interventions will likely require the coordination of local/state departments of public health, health commissions, and social policy more broadly.
Conclusion
While most patients stated that there was no clinical or medical service that they needed and could not obtain after discharge, almost half said that they needed more general assistance to stay well outside the hospital. Among those readmitted, characteristics including homelessness, substance use disorder, or factors related to SDoH conferred increased risk of preventable readmission. Prioritizing interventions for patient populations with higher risk of preventable readmission may improve outcomes. Nonmedical support systems and policy changes are required to improve preventable readmissions for patients with nonclinical or social determinants of health-related needs.
Supplemental Material
Supplemental Material, Readmission_CTDAPatientQuestionnaire for Social Factors and Patient Perceptions Associated With Preventable Hospital Readmissions by Jocelyn Carter, Charlotte Ward, Anne Thorndike, Karen Donelan and Deborah J Wexler in Journal of Patient Experience
Author Biographies
Jocelyn Carter, MD, MPH, an instructor in medicine at Harvard Medical School, is an internal medicine hospitalist at Massachusetts General Hospital. Her research interests include readmissions and care transitions research with a focus on cost-effective, evidence-based interventions that improve outcomes.
Charlotte Ward, MPH is a PhD candidate in Health Services Research at Northwestern University. Her primary research interests include patterns of high-cost health care use among vulnerable patient populations, latent variable modeling and longitudinal data analysis.
Karen Donelan, ScD, MEd, an associate professor of Medicine at Harvard Medical School, is a health services survey researcher with experience leading institutional, local, regional, national and international surveys on a range of health and health policy topics. Sr. Scientist Donelan collaborates widely within the Dana Farber/Harvard Cancer Center, MGH Cancer Center, Mongan Institute Health Policy Center and MGH Institute for Technology Assessment.
Deborah J Wexler, MD, MSc, is associate professor of Medicine at Harvard Medical School, Boston, Massachusetts, the Associate Clinical Chief of the MGH Diabetes Unit, and Co-Clinical Director of the MGH Diabetes Center. Dr. Wexler’s research focuses on clinical effectiveness in type 2 diabetes. She has served on the American Diabetes Association’s Professional Practice Committee and is on the Editorial Board of Diabetes Care.
Footnotes
Authors’ Note: Contributors: Massachusetts General Physicians’ Organization, The Massachusetts General Hospital Center for Diversity and Inclusion and the MGH Department of General Internal Medicine, and the Tufts University Community Health Department. Poster version of related data presented at SGIM, Toronto, Canada, 2015. With regard to ethical approval, this study obtained Partners Healthcare Institutional Review Board approval. Verbal consent was obtained prior to patient enrollment per IRB protocol. Anonymized full data set and statistical codes are available upon request. J.C., D.W., and K.D. designed the study and outcomes of interest. J.C. wrote the original manuscript. D.W., K.D., A.T., and C.W. edited the manuscript. C.W. performed all statistical analysis. All authors listed have contributed sufficiently to the project to be included as authors, and all those who are qualified to be authors are listed in the author byline.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The Massachusetts General Physicians’ Organization in partnership with the Massachusetts General Hospital Center for Diversity and Inclusion.
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Auerbach AD, Kripalani S, Vasilevskis EE, Sehgal N, Lindenauer PK, Metlay JP, et al. Preventability and causes of readmissions in a national cohort of general medicine patients. JAMA Intern Med. 2016;176(4):484–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Academy Health. Reducing Hospital Readmissions. Washington, DC: Academy Health; 2008. http://www.academyhealth.org/files/publications/ReducingHospitalReadmissions.pdf. Accessed June 12, 2017. [Google Scholar]
- 3. McIlvennan C, Eapen Z, Allen L. Hospital readmissions reduction program. Circulation. 2015;131(20):1796–803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Boutwell A, Hwu S. Effective Interventions to Reduce Rehospitalizations: A Survey of the Published Evidence. Cambridge, MA: Institute for Healthcare Improvement; 2009. http://www.breecollaborative.org/wp-content/uploads/bree_readmissions_background_reading.pdf [Google Scholar]
- 5. Coleman EA, Parry C, Chalmers S, Min SJ. The care transitions intervention: results of a randomized controlled trial. Arch Intern Med. 2006;166(17):1822–28. [DOI] [PubMed] [Google Scholar]
- 6. Jack BW, Chetty VK, Anthony D, Greenwald JL, Sanchez GM, Johnson AE, et al. A reengineered hospital discharge program to decrease rehospitalization: a randomized trial. Ann Intern Med. 2009;150(3):178–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Carter JA, Carr LS, Collins J, Doyle Petrongolo J, Hall K, Murray J, et al. STAAR: improving the reliability of care coordination and reducing hospital readmissions in an academic medical centre. BMJ Innov. 2015;1(3):75–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Felix HC, Seaberg B, Bursac Z, Thostenson J, Stewart MK. Why do patients keep coming back? results of a readmitted patient survey. Soc Work Health Care. 2015;54(1):1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Stein J, Ossman P, Viera A, Moore C, Brubaker BA, French J, et al. Was this readmission preventable? Qualitative study of patient and provider perceptions of readmissions. South Med J. 2016;109(6):383–89. [DOI] [PubMed] [Google Scholar]
- 10. Strunin L, Stone M, Jack B. Understanding rehospitalization risk: can hospital discharge be modified to reduce recurrent hospitalization? J Hosp Med. 2007;2(6):297–304. [DOI] [PubMed] [Google Scholar]
- 11. Jeffs L, Dhalla I, Cardoso R, Bell CM. The perspectives of patients, family members and healthcare professionals on readmissions: preventable or inevitable? J Interprof Care. 2014;28(6):507–12. [DOI] [PubMed] [Google Scholar]
- 12. Kangovi S, Grande D, Meehan P, Mitra N, Shannon R, Long J. Perceptions of readmitted patients on the transition from hospital to home. J Hosp Med. 2012;7(9):709–12. [DOI] [PubMed] [Google Scholar]
- 13. Misky GJ, Burke RE, Johnson T, Del Pino Jones A, Hanson JL, Reid MB. Hospital readmission from the perspective of Medicaid and uninsured patients. J Healthc Qual. 2018;40(1):44–50. [DOI] [PubMed] [Google Scholar]
- 14. Carter J, Ward C, Wexler D. The association between patient experience factors and likelihood of 30-day readmission: a prospective cohort study [published online]. BMJ Qual Saf. doi:10.1136/bmjqs-2017-007184. [DOI] [PubMed] [Google Scholar]
- 15. Centers for Medicare & Medicaid Services. Baltimore, MD: HCAHPS Online. http://www.hcahpsonline.org. Accessed June 20, 2017.
- 16. Harris PA, Taylor R, Thielke Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bradley EH, Elkins BR, Herrin J, Elbel B. Health and social services expenditures: associations with health outcomes. BMJ Qual Saf. 2011;20(10):826–31. [DOI] [PubMed] [Google Scholar]
- 18. Thorpe KE, Joski P. The association of social service spending, environmental quality and health behaviors on health outcomes. Popul Health Manag. 2018;21(4):291–5. [DOI] [PubMed] [Google Scholar]
- 19. Bradley EH, Canavan M, Rogan E, Talbert-Slagle K, Ndumele C, Taylor L, et al. Variation in health outcomes: the role of spending on social services, public health and health care 2000-2009. Health Aff (Millwood). 2016;35(5):760–68. [DOI] [PubMed] [Google Scholar]
- 20. Arbaje AI, Wolff JL, Yu Q, Powe NR, Anderson GF, Boult C. Postdischarge environmental and socioeconomic factors and the likelihood of early hospital readmission among community-dwelling medicare beneficiaries. Gerontologist. 2008;48(4):495–504. [DOI] [PubMed] [Google Scholar]
- 21. Calvillo-King L, Arnold D, Eubank KJ, Lo M, Yunyongying P, Stieglitz H, et al. Impact of social factors on risk of readmission or mortality in pneumonia and heart failure: systematic review. J Gen Intern Med. 2013;28(2):269–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Bernheim SM, Spertus JA, Reid KJ, Bradley EH, Desai RA, Peterson ED, et al. Socioeconomic disparities in outcomes after acute myocardial infarction. Am Heart J. 2007;153(2):313–19. [DOI] [PubMed] [Google Scholar]
- 23. Tsuchihashi M, Tsutsui H, Kodama K, Kasagi F, Setoguchi S, Mohr M, et al. Medical and socioenvironmental predictors of hospital readmission in patients with congestive heart failure. Am Heart J. 2001;142(4):E7. [DOI] [PubMed] [Google Scholar]
- 24. Joynt KE, Jha AK. A path forward on Medicare readmissions. N Engl J Med. 2013;368(13):1175–77. [DOI] [PubMed] [Google Scholar]
- 25. Hu J, Gonsahn MD, Nerenz DR. Socioeconomic status and readmissions: evidence from an urban teaching hospital. Health Aff. 2014;33(5):778–85. [DOI] [PubMed] [Google Scholar]
- 26. Meddings J, Reichert H, Smith SN, Iwashyna TJ, Langa KM, Hofer T, et al. The impact of disability and social determinants of health on condition-specific readmissions beyond Medicare risk adjustments: a cohort study. J Gen Intern Med. 2017;32(1):71–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Goldfield NI, McCullough EC, Hughes JS, Tang AM, Eastman B, Rawlins LK, et al. Identifying potentially preventable readmissions. Health Care Financ Rev. 2008;30(1):75–91. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, Readmission_CTDAPatientQuestionnaire for Social Factors and Patient Perceptions Associated With Preventable Hospital Readmissions by Jocelyn Carter, Charlotte Ward, Anne Thorndike, Karen Donelan and Deborah J Wexler in Journal of Patient Experience