Abstract
Background:
Good communication skills enhance the patient experience, clinical outcomes, and patient satisfaction.
Objective:
A course was developed by an interdisciplinary team (surgeon, nurse practitioner, and nurse MBA) for advanced practice providers (APPs) working for the department of surgery—a mix of practice and hospital-employed professionals—to enhance communications skills in an inpatient setting.
Methods:
Current concepts on provider–patient communication were discussed. Participants also asked to view and critique a video “provider–patient communication gone wrong” scenario. Lastly, participants were provided with techniques for improving provider–patient communication. The participants assessed the course. Provider communication scores were tracked from quarter 1, Fiscal Year 2014 to quarter 4 Fiscal Year 2017.
Results:
Of 110 eligible APPs, 95 (86%) attended the course. The anonymous survey response rate was 90% (86/95). Participants expressed satisfaction with the course content confirmed by Likert score weighted averages of >4.6/5 in all 8 domains. Communication scores increased with time.
Conclusion:
An interdisciplinary course aimed at enhancing provider–patient communication skills was well-received by the APP participants. The course was part of ongoing system-wide efforts to improve patient experiences, satisfaction, and outcomes. Continuing education in communication continues to play a key role in improving clinical outcomes and patient satisfaction.
Keywords: provider–patient communication, patient satisfaction, risk management, CAHPS scores, outcomes
Introduction
Better communication with patients and families is considered important enough to be an overarching health system team goal—improving nurse and doctor communication Consumer Assessment of Healthcare Providers and Services, Hospital (CAHPS-H) scores—alongside such clinical imperatives as decreasing rates of mortality, unplanned readmissions, and hospital acquired infections. In the Department of Surgery, our quality initiatives are intended to align with the team goals, and in particular, an improved patient experience through better communication. Historically, providers honed their own, immutable style for communication skills at the bedside. The current perspective views communication skills as a set of modifiable behaviors that can be objectively assessed (1).
All health professions include good communication skills as an important competency. The Association of American Medical Colleges lists as an Interprofessional Collaborative Practice Competency, “[I]nterprofessional communication with patients, families, communities, and other health professionals in a responsive and responsible manner that supports a team approach to the maintenance of health and the treatment of disease” (2). The National Organization of Nurse Practitioner Faculties notes that “[A]reas of increased knowledge, skills, and expertise include advanced communication skills, as well as collaboration, complex decision making, leadership, and the business of health care” (3). In the Physician Assistant profession, “[I]nterpersonal and communication skills encompass the verbal, nonverbal, written, and electronic exchange of information. Physician assistants must demonstrate interpersonal and communication skills that result in effective information exchange with patients, patients’ families, physicians, professional associates, and other individuals within the health-care system” (4).
When lines of communication are open, patients are more likely to acknowledge health problems, understand treatment options, and follow medication schedules (5). Where studied, good provider–patient communication is associated with better outcomes, including better adherence to preoperative preparation, better in-hospital care, and earlier detection of postdischarge complications (5). Lastly, good communication is associated with lower malpractice claims (6). The purpose of this article is to describe an academic Department of Surgery experience providing a course in inpatient communication skills for advanced practice providers (APPs)—nurse practitioners (NPs) and physician assistants (PAs)—who work directly with faculty and house staff based in the Department of Surgery.
Methods
Curriculum Development
Course content was developed in response to an enthusiastic request by surgery APPs for a course similar to that previously given for faculty and house staff (5). The course was organized in collaboration with our academic health system’s Advance Practice Provider Council. The rationale for communication skills as a core competency was linked to research showing that good communication enhances patient care. Incorporating patient-centered communication into the NPs’ practice is associated with improving patient outcomes including improved patient satisfaction, increased adherence to treatment plans, and improved patient health (7,8). To combat limited health literacy in a suburban urgent care setting, clear provider communication was documented as essential in optimizing outcomes (9).
The value of good communication was also emphasized by discussing the impact of CAHPS-H scores. Patient satisfaction with their experiences may assume a greater role in reimbursement of health-care dollars by the Centers for Medicare and Medicaid Services (CMS) and perhaps other third-party insurers (10). The CMS is responsible for the implementation of this survey and publicly reports results including doctor and nurse communication scores (11). Further, there is a positive correlation between CAHPS-H scores and nurse empowerment (12).
After the didactic portion of the course, APPs viewed a “Surgi-Drama,” or scripted video, with actors simulating a “provider–patient communication gone-wrong” scenario as initially developed for surgeons and house staff (5). Participating APPs were encouraged to critique the video segment representing poor communication skills and how one might better communicate. As they watched the interaction, participants were asked to think about ways in which the communication between the provider and the patient could be improved. The intent of the video was to document the many ways that communication can go awry. Many of the errors in communication written into the scenario were suggested by CAHPS-H comments as published previously (5).
Resources for best practices around communication skills comprised the last section of the course. Strategies that could be implemented immediately were emphasized. One simple mnemonic for a patient interaction at the bedside was the “2-3-4”: Knock 2 times on the door; wait 3 seconds, then ask for permission to enter quietly. Four refers to 4 “must-do” behaviors: introduce team members; ask for permission to examine the patient, and only then do so; discuss the plan of care; and ask the patient if there are questions, encouraging self-participation (5). The Press-Ganey organization has made available a number of suggestions for improving provider patient communication for the CAHPS-H questions (13).
Another strategy taught that when providers sit, patients report a more positive interaction and a better understanding of their condition (14). Few nonverbal cues mean more than looking someone straight in the eye; signaling a willingness to listen and acknowledge the patient’s worth (15). The practice of patient-centered communication was encouraged: allowing time to tell the story; give thorough explanations, practice interpersonal skills including emotional/empathic communication skills training, query psychosocial issues, and talk about the patient’s specific care not generalities (16). Providers should repeat and reinforce important information throughout a patient’s hospitalization (17). Kaiser Permanente’s Four Habits Model, invest in the beginning, elicit the patient’s perspective, demonstrate empathy, and invest in the end, is also a good way to connect with the patient (18).
Survey Development and Analysis
An anonymous survey of 8 questions and 2 free-text comment sections were provided to the attendees to share their experience about the course with the organizers (Table 1). These were adapted from similar questions asked of faculty and residents as previously published (5). There was no sampling; the entire group was surveyed. Survey results were analyzed and tabulated to assist designing future courses (number of responses, N = 86, survey response rate = 90.52%, see Table 2). Course organizers utilized a 5-point Likert scale to measure the audience experience during the APP Communication Course (5, 6). Each response in the survey was anchored as follows: strongly disagree (1), disagree (2), neither agree or nor disagree (3), agree (4), and strongly agree (5). The weighted average of each question was calculated by using the following formula (19):
Table 1.
Advance Practice Provider Communication Course Survey Questions.
| Q# | Question Description |
|---|---|
| 1. | What is your overall evaluation of the program? |
| 2. | This presentation addressed the gaps in knowledge and practice regarding provider–patient communication. The content was relevant to the stated overall purpose. |
| 3. | This presentation introduced the relevance of current concepts of provider–patient communication. |
| 4. | This presentation discussed the current data reflecting patient assessment of the communication skills of Penn providers. |
| 5. | This presentation provided a “toolkit” of techniques for improving provider–patient communication. |
| 6. | The program’s speaker was effective in delivering the program content. |
| 7. | This program’s content was relevant to my practice. |
| 8. | The learning materials utilized in this program were helpful. |
Table 2.
Likert Scores and Weighted Averages of Advance Practice Provider Communication Course.a
| Q # | Disagree [N (%)] | Neutral [N (%)] | Agree [N (%)] | Strongly Agree [N (%)] | Total Responses | Weighted Average |
|---|---|---|---|---|---|---|
| 1 | 0 | 6 (6.98%) | 20 (23.26%) | 60 (69.77%) | 86 | 4.63 |
| 2 | 0 | 1 (1.16%) | 3 (3.49%) | 82 (95.35%) | 86 | 4.70 |
| 3 | 0 | 4 (4.65%) | 15 (17.44%) | 67 (77.91%) | 86 | 4.73 |
| 4 | 0 | 4 (4.65%) | 18 (20.93%) | 64 (74.42%) | 86 | 4.70 |
| 5 | 0 | 5 (5.88%) | 16 (18.82%) | 64 (75.29%) | 85 | 4.69 |
| 6 | 0 | 5 (5.81%) | 13 (15.12%) | 68 (79.07%) | 86 | 4.73 |
| 7 | 1 (1.16) | 8 (9.30%) | 7 (8.14%) | 70 (81.14%) | 86 | 4.80 |
| 8 | 0 | 7 (8.24%) | 19 (22.35%) | 59 (69.41%) | 85 | 4.61 |
a There were no “Strongly Disagree” responses.
* = weighted average of the responses; Wi = weight of the answer choice; Xi = response count for answer choice.
Computation of a Linear Regression Trend Line
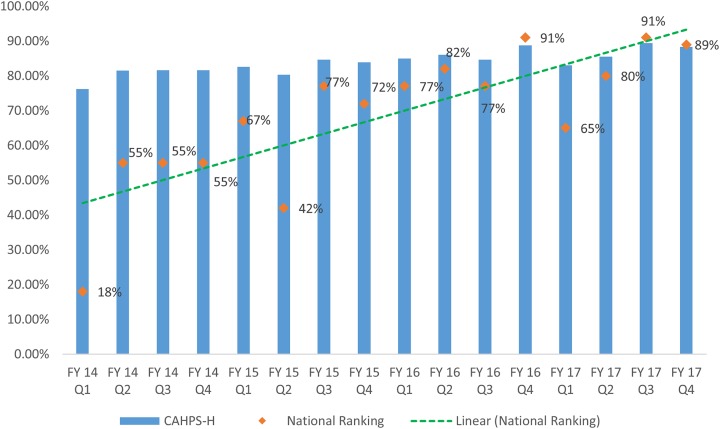
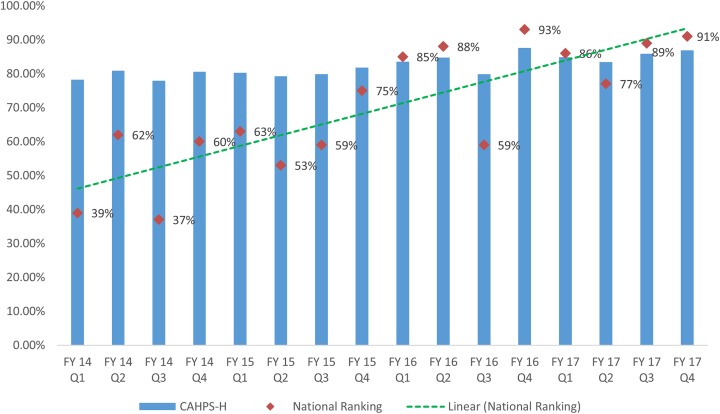
Department of Surgery CAHPS-H percent top box scores and national percentile rankings over a 4-year period were discussed. A trend line—linear regression equation—for the national percentile ranking was then plotted (Figures 1 and 2). Computation of the linear regression is based on the general equation: (20)
Figure 1.
Consumer Assessment of Healthcare Providers and Services, Hospital (CAHPS-H) doctor communication.
Figure 2.
Consumer Assessment of Healthcare Providers and Services, Hospital (CAHPS-H) nurse communication.
Yi = dependent variable, Xi = independent variable; a = intercept (value of Y when X = 0); bi = slope of the line. Data for both nurses and doctors were calculated, as the free-text comments suggested that APPs were identified as either. A process control chart was also created to show the position of the APP communication course relative to the percent top box scores (21).
Our institutional review board (IRB) considered the work exempt from IRB review; no individually identifiable information was collected, and the work was purely educational.
Results
One hundred ten APPs were eligible to participate in the course. The APPs attended either in person at 1 of 4 sessions (n = 73, 77%) or by reviewing a web-based version of the course (n = 22, 23%), bringing the total participation to 86% (n = 95). The ability to teach individual groups of APPs (for instance, those APPs based in cardiac surgery or trauma) allowed targeted questions regarding communication issues and the smaller group sizes made for more personal discussions. The course presentation lasted about 1 hour. The online version allowed certain individuals to participate who would otherwise have missed out on the information. Attendees completed an anonymous survey after the completion of the course (N = 86, response rate = 90%, see Table 2). Quantitatively, each of 8 questions had a weighted average of more than 4.6. Qualitatively, the remaining 2 questions asked individuals to comment on the most valuable learnings from the course and improvement opportunities for future sessions (Tables 3 and 4).
Table 3.
Identify Specifically What You Intend to Incorporate into Your Practice From What You Have Learned in This Program.a
| To Incorporate | N |
|---|---|
| Active listening | 9 |
| Four habits model | 3 |
| Understanding patient perspective | 3 |
| Not applicable to outpatient setting | 3 |
| Already utilizing communication strategies | 2 |
| Follow-up phone calls | 1 |
| Daily patient assessment to improve communication | 1 |
| Unable to differentiate between doctors and APPs | 1 |
Abbreviation: APP, advanced practice providers
a Answered 23/86—27%.
Table 4.
What Improvements Would You Suggest for Future Sessions?a
| Improvements | N |
|---|---|
| None | 8 |
| Increase audience interaction during course | 2 |
| Distribution of written material on communication strategies | 2 |
| Specific strategies for outpatient setting | 2 |
| More simulation of communication scenarios | 1 |
a Answered 15/86—17%.
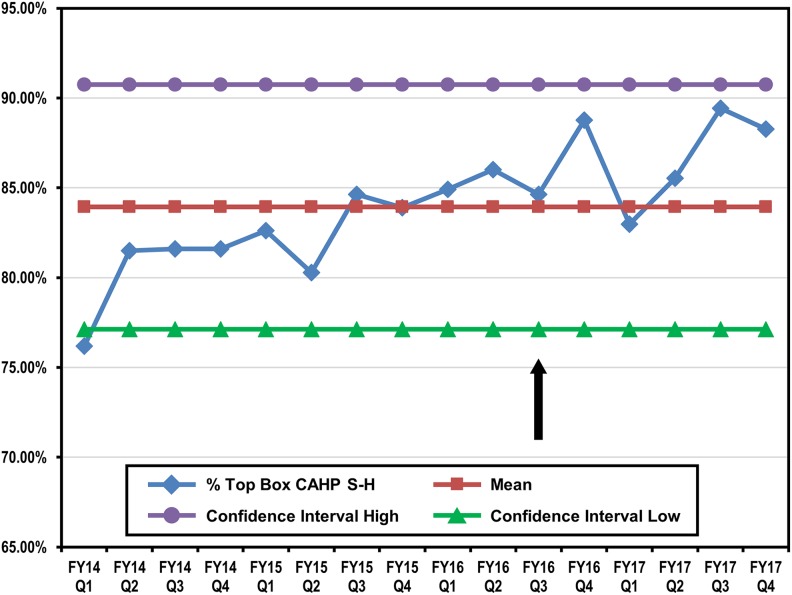
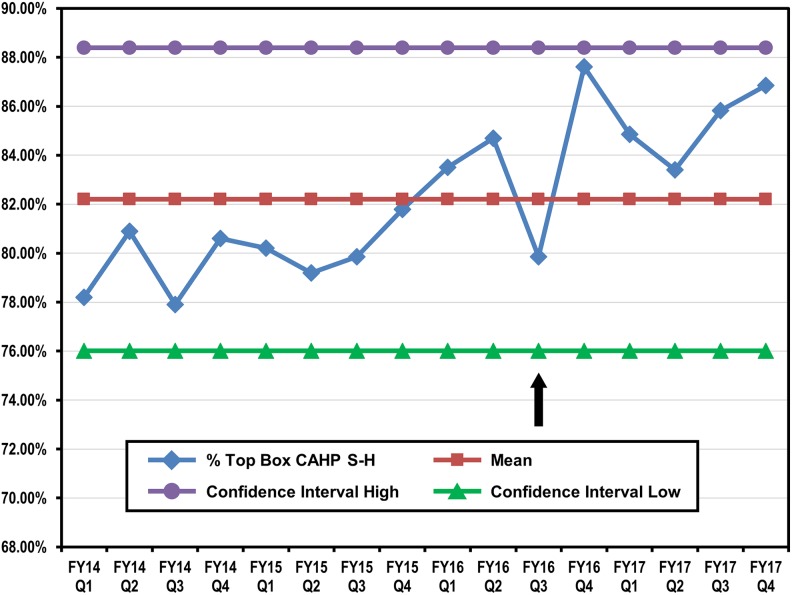
The CAHPS-H survey does not specifically ask about APPs; however, the free-text comments suggest that APPs may be perceived as either members of the nursing staff or as physicians (despite appropriate badging). Thus, a comparative analysis of quarterly CAHPS-H data on both nurse and doctor communication scores was performed, with a trend line plotted for from Q1 FY 2014 to Q4 FY 2017. The comparative analysis focused on how relatively small increases in the percent top box scores translate into proportionately larger increases in the national rankings linear regression score behaved between the data sets of doctor and nurse communication scores during implementation of the various communication courses (Figures 1 and 2). The linear regression score is indicative of a direct relationship between the communication courses and CAHPS-H communication scores. Comparative analysis shows a sustained increase in both doctor and nurse communication CAHPS-H scores year over year with the implementation of the APP and other communication courses (Figures 1 and 2). Process control charts for both nurse and doctor communications did show a modest bump in top box scores that persisted in subsequent quarters (Figures 3 and 4).
Figure 3.
Process control chart for doctor communication. The arrow denotes the time period of the advanced practice provider (APP) communication course. Note the increase in scores after the course.
Figure 4.
Process control chart for nurse communication. The arrow denotes the time period of the advanced practice provider (APP) communication course. Note the increase in scores after the course.
Limitations
This work was specifically designed for a group of surgical advanced practitioners in a single health system in a specific state jurisdiction; hence, certain aspects of the course would not be applicable in all settings. Further, the relatively small group (110 practitioners) eligible to participate might influence the results that could be different with a larger regional or national educational effort. It would be disingenuous to assert cause and effect between the APP course and CAHPS-H scores; only an association.
In the CAHPS-H survey methodology, advanced practitioners are not represented; the surveys are focused on physicians and registered nurses hence it was not possible to provide APP specific data in this setting. The provision of such data will be available for the Clinical Group CAHPS-H (22). Despite the lack of specific CAHPS-H data in the inpatient setting, advanced practitioners have a great deal of influence on the inpatient experience; hence, the communication principles as presented in this course are still important.
A further limitation is the lack of testing regarding recall of the information provided. For the amount of material condensed into such a short course, it is possible that certain of the topics were presented too quickly to assimilate. Cognitive overload is a concern when detailed information is discussed in a format such as ours (23). Future courses will include a pretest/posttest option to assess whether the materials presented were comprehended. It is not known whether or to what extent any of the communications skills materials referenced were subsequently reviewed by course participants.
Discussion
Perhaps the most notable part of the program is that it was tailored for the specific types of communications that surgery APPs have with inpatients every day. To accommodate the logistical needs of the APPs, live courses were offered at 4 different locations in 3 health system entities. In addition, an e-learning module was also published for 30 days on our institution’s education portal to reach out to eligible participants who were unable to attend the live sessions. Continuing nursing education and continuing medical education credits were offered to NPs and PAs, respectively, who attended the live courses.
Developing and implementing a course on improving inpatient communication skills for APPs was one approach to an overall increased emphasis on enhancing the patient experience in our health system. Our educational endeavor was not intended as a research project; as evidenced by the exempt status given by our IRB. Rather, we articulate one approach to teaching communication as a set of modifiable behaviors. Our course was very favorably rated, and given the robust attendance numbers, the data are likely reliable. However, the objective metric—improvement in CAHPS-H scores—was positive, but modest. Given the relative lack of approaches to teaching communication in the academic setting, there is value in describing in detail how to teach APPs about specific communication skills.
Communication skills assessed by the CAHPS-H is a standardized survey developed for measuring patients’ views on in-hospital care (24). A percentage of inpatients discharged to home receive an CAHPS-H survey in the mail. There are 9 domains: communication with nurses, communication with doctors, responsiveness of hospital staff, cleanliness of the environment, quietness of the environment, pain management, communication about medicines, discharge information, transition of care, overall hospital rating, and likelihood to recommend to friends and family (25).
Providers have great influence on 2 domains: doctor communication and nurse communication. In fact, doctor and nurse communication are the most important drivers of overall patient satisfaction (26). The greatest impact for improving patient satisfaction may be through focusing on nursing care; each 1-point increase in the nursing domain score increased the odds of achieving a CAHPS-H top-box score by 4.9% (27). Better nurse communication scores have a causative impact on other CAHPS-H domains, readmission rates, hospital acquired conditions, reduced mortality, and reimbursement to health-care organizations (28,29).
The continued rise in CAHPS-H scores as shown by the trend line in Figures 1 and 2 suggests no single initiative—or “one and done”—is effective, but that repeated efforts over time are necessary. In addition to the APP course, separate courses on communication had been previously taught to surgical faculty and house staff (5). No similar communication courses were provided to other nursing staff, or nonsurgical groups of APPs. However, other strategies—patient-centered nursing rounds, staff “trading cards,” and postdischarge nursing outreach—were being implemented in the same timeframe. The process control chart also shows an increase in CAHPS-H scores after the APP course but also that to sustain such increases over time requires ongoing communication efforts.
Implications
The articulation of one approach to educating advanced practitioners in basic communication skills as described here can be used to improve the patient experience and quality of care in a variety of settings. A study of NPs in Maryland who had taken a communication course beyond their initial education was a predictor for using additional communication techniques (30). This work adds to a meager literature regarding communication skills in APPs. A PubMed search (4/20/2018), resulted in only 23 articles looking specifically at advanced practitioner inpatient education in the past 5 years and none in CINAHL (31). Unlike the inpatient setting, APPs will be transparently identified in outpatient settings so similar courses can be tailored to the outpatient venue. Our findings could be used to develop policies in continuing education on communication that will improve the quality of care delivery. Future research is needed on the education of APPs in patient communication to further develop our understanding of APP needs and strategies for improvement.
Conclusions
Accreditation bodies have stated that advanced practice provider/patient communication skills are important. Our work articulates one approach to educating APPs on improving their communication skills. The course was well received as determined by the evaluation scores. The course also provided a number of strategies and resources available for improving communication skills. Continued emphasis on educating health-care providers is one important component of initiatives designed to help improve CAHPS-H scores as an outcome metric for communication skills currently transparent on an institutional (and likely individual) basis.
Author Biographies
Johncy Joseph, RN-BSN, MBA, is Quality & Risk Manager, Department of Surgery, University of Pennsylvania Health System, Philadelphia, PA.
Corinna Sicoutris, MSN, ACNP, FAANP, FCCM, is the director of Advanced Practice Providers at the Hospital of the University of Pennsylvania, in Philadelphia and a Clinical Instructor for the Acute Care Nurse Practitioner (ACNP) Program at the University of Pennsylvania School of Nursing.
Steven E Raper, MD, JD, is an associate professor of Surgery, Vice-chairman for Quality and Risk Management, Department of Surgery, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Steven E. Raper, MD, JD  https://orcid.org/0000-0001-9191-4681
https://orcid.org/0000-0001-9191-4681
References
- 1. Banerjee SC, Manna R, Coyle N, Penn S, Gallegos TE, Zaider T, et al. The implementation and evaluation of a communication skills training program for oncology nurses. Transl Behav Med. 2017;7:615–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Interprofessional Collaborative Practice Competencies (AAMC). 2016. http://www.ipecollaborative.org/resources.html. Accessed October 16, 2018.
- 3. Nurse Practitioner Core Competencies Content. 2012. https://cdn.ymaws.com/www.nonpf.org/resource/resmgr/competencies/2017_NPCoreComps_with_Curric.pdf. Accessed October 16, 2018.
- 4. Competencies for the Physician Assistant Profession. 2012. http://www.nccpa.net/Uploads/docs/PACompetencies.pdf. Accessed October 16, 2018. [DOI] [PubMed]
- 5. Raper SE, Gupta M, Okusanya O, Morris JB. Improving communication skills: a course for academic medical center surgery residents and faculty. J Surg Educ. 2015;72:e202–11. [DOI] [PubMed] [Google Scholar]
- 6. Raper SE, Joseph J, Seymour WG, Sullivan PG. Tipping the scales: educating surgeons about medical malpractice. J Surg Res. 2016;206:206–13. [DOI] [PubMed] [Google Scholar]
- 7. Charlton CR, Dearing KS, Berry JA, Johnson MJ. Nurse practitioners’ communication styles and their impact on patient outcomes: an integrated literature review. J Am Acad Nurse Pract. 2008;20:382–8. [DOI] [PubMed] [Google Scholar]
- 8. Alberti TL, Nannini A. Patient comprehension of discharge instructions from the emergency department: a literature review. J Am Assoc Nurse Pract. 2013;25:186–94. [DOI] [PubMed] [Google Scholar]
- 9. Alberti TL, Morris NJ. Health literacy in the urgent care setting: what factors impact consumer comprehension of health information? J Am Assoc Nurse Pract. 2017;29:242–7. [DOI] [PubMed] [Google Scholar]
- 10. Centers for Medicare and Medicaid Services. Patient- and caregiver centered experience of care/care coordination domain. 2018. Retrieved from: http://www.medicare.gov/HospitalCompare/Data/patient-and-caregiver-centered-experience-of-care-care-coordination-domain.html. Accessed October 16, 2018.
- 11. Consumer Assessment of Healthcare Providers and Systems Hospital Survey. Content last reviewed June 2017. Rockville: Agency for Healthcare Research and Quality; Retrieved from: http://www.ahrq.gov/cahps/surveys-guidance/hospital/index.html. Accessed October 16, 2018. [Google Scholar]
- 12. Donahue MO, Piazza IM, Griffin MQ, Dykes PC, Fitzpatrick JJ. The relationship between nurses’ perceptions of empowerment and patient satisfaction. Applied Nurs Res. 2008;21:2–7. [DOI] [PubMed] [Google Scholar]
- 13. Hospital Consumer Assessment of Healthcare Providers and Systems Solutions Starter. 2014. Retrieved from: https://paws.gru.edu/pub/patient-family-engagement/resources/Documents/Best%20Practices/solutions_starter_hcahps_2014.pdf. Accessed October 16, 2018.
- 14. Patel S, Fullam F, Behel JM. How we improved hospitalist-patient communication. 2017. http://catalyst.nejm.org/how-we-improved-hospitalist-patient-communication/. Accessed October 16, 2018.
- 15. Swayden KJ, Anderson KK, Connelly LM, Moran JS, McMahon JK, Arnold PM. Effect of sitting vs. standing on perception of provider time at bedside: a pilot study. Patient Educ Couns. 2012;86:166–71. [DOI] [PubMed] [Google Scholar]
- 16. Gorawara-Bhat R, Cook MA. Eye contact in patient-centered communication. Patient Educ Couns. 2011;82:442–47. [DOI] [PubMed] [Google Scholar]
- 17. Street RL. The many “disguises” of patient-centered communication: problems of conceptualization and measurement. Patient Educ Coun. 2017;100:2131–4. [DOI] [PubMed] [Google Scholar]
- 18. Frankel RM, Stein T. Getting the most out of the clinical encounter: the four habits model. Permanente J. 1999;3(3):79–88. [PubMed] [Google Scholar]
- 19. Gelman A. Struggles with survey weighting and regression modeling. Stat Sci. 2007;22:153–60. [Google Scholar]
- 20. Schneider A, Hommel G, Blettner M. Linear regression analysis: part 14 of a series on evaluation of scientific publications. Dtsch Arztebl Int. 2010;107:776–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Wheeler DJ, Chambers DS. Understanding Statistical Process Control. 3rd ed Knoxville: SPC PRESS (Statistical Process Control; ); 2010:43–47. [Google Scholar]
- 22. Clinician and Group CAHPS. 2018. Retrieved from: http://www.pressganey.com/resources/cahps-programs/cgcahps. Accessed October 16, 2018.
- 23. Kaylor SK. Preventing information overload: cognitive load theory as an instructional framework for teaching pharmacology. J Nursing Ed. 2014;53:108–11. [DOI] [PubMed] [Google Scholar]
- 24. Consumer Assessment of Healthcare Providers and Systems Hospital Survey. 2018. Baltimore: Centers for Medicare & Medicaid Services; Retrieved from: http://www.hcahpsonline.org/en/survey-instruments/. Accessed October 16, 2018. [Google Scholar]
- 25. Summary Analyses. 2018. Retrieved from: http://www.hcahpsonline.org/en/summary-analyses/. Accessed October 16, 2018.
- 26. Paddison CAM, Abel GA, Roland MO, Elliott MN, Lyratzopoulos G, Campbell JL. Drivers of overall satisfaction with primary care: evidence from the English General Practice Patient Survey. Health Expect. 2015;18:1081–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Wolosin R, Ayala L, Fulton BR. Nursing care, inpatient satisfaction, and value-based purchasing: vital connections. J Nurs Admin. 2012;42:321–5. [DOI] [PubMed] [Google Scholar]
- 28. Dempsey C, Reilly B, Buhlman N. Improving the patient experience: real-world strategies for engaging nurses. J Nurs Admin. 2014;44:142–5. [DOI] [PubMed] [Google Scholar]
- 29. Centers for Medicare and Medicaid Services, Baltimore, MD. 2018. Survey instruments English. Retrieved from: http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/HospitalHCAHPS.html. Accessed October 16, 2018.
- 30. Koo LW, Horowitz AM, Radice SD, Wang MQ, Kleinman DV. Nurse practitioners’ use of communication techniques: results of a Maryland oral health literacy survey. PLoS One. 2016;11:e0146545 doi:10.1371/journal.pone.0146545. eCollection 2016. Accessed August 23, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. PubMed search strategy: ((“nurse practitioners”[MeSH Terms] OR (“nurse”[All Fields] AND “practitioners”[All Fields]) OR “nurse practitioners”[All Fields] OR (“nurse”[All Fields] AND “practitioner”[All Fields]) OR “nurse practitioner”[All Fields]) AND (“inpatients”[MeSH Terms] OR “inpatients”[All Fields] OR “inpatient”[All Fields]) AND (“communication”[MeSH Terms] OR “communication”[All Fields])) AND (“2013/04/22”[PDat]: “2018/04/20”[PDat] AND “humans”[MeSH Terms] AND English[lang]) as well as ((“physician assistants”[MeSH Terms] OR (“physician”[All Fields] AND “assistants”[All Fields]) OR “physician assistants”[All Fields] OR (“physician”[All Fields] AND “assistant”[All Fields]) OR “physician assistant”[All Fields]) AND (“inpatients”[MeSH Terms] OR “inpatients”[All Fields] OR “inpatient”[All Fields]) AND (“communication”[MeSH Terms] OR “communication”[All Fields])) AND (“2013/04/22”[PDat]: “2018/04/20”[PDat] AND “humans”[MeSH Terms] AND English[lang]). CINAHL search strategy: (MH “Education, Nursing, Continuing/EV/PF”) (MH “Communication Skills Training/ED”)