Type III IFNs, or IFN-λ, are the latest addition to the IFN family. Thanks to a restricted pattern of expression of their receptor and to unique immunomodulatory properties, IFN-λ stimulates pathogen clearance while, at the same time, curbing inflammation to maintain barrier integrity.
Abstract
Type III IFNs, or IFN-λ, are the newest members of the IFN family and were long believed to play roles that were redundant with those of type I IFNs. However, IFN-λ displays unique traits that delineate them as primary protectors of barrier integrity at mucosal sites. This unique role stems both from the restricted expression of IFN-λ receptor, confined to epithelial cells and to a limited pool of immune cells, and from unique immunomodulatory properties of IFN-λ. Here, we discuss recent findings that establish the unique capacity of IFN-λ to act at the barriers of the host to balance tissue tolerance and immune resistance against viral and bacterial challenges.
Introduction
Type III IFNs, also known as IFN-λ, are the latest addition to the IFN family. They were discovered by two independent groups in 2003 as new members of the broad class II cytokine family and are structurally related to cytokines of the IL-10 family, but they have functions that are similar to those of type I IFNs (Sheppard et al., 2003; Kotenko et al., 2003; Kotenko, 2011). The type III IFN family consists of four cytokines: IFN-λ1 (IL-29), IFN-λ2 and IFN-λ3 (IL-28A and IL28B, respectively), and IFN-λ4. IFN-λ1 is only expressed in humans (it is a pseudogene in mice), whereas IFN-λ2 and IFN-λ3 are expressed in both species and are the most related to each other, displaying 96% amino acid sequence identity (Kotenko, 2011; Sheppard et al., 2003). IFN-λ4 is absent in mice, and in humans its expression is suppressed either at the mRNA or protein level (Hong et al., 2016).
As with other IL-10 family cytokines, IFN-λ signals through a heterodimeric receptor that comprises the common IL-10 receptor-β (IL-10RB) chain plus the cytokine binding–specific chain IFN-λ receptor 1 (IFNLR1; Kotenko, 2011; Sheppard et al., 2003). However, the downstream signaling pathway and functional output of receptor binding share many characteristics with the responses that are elicited by type I IFNs via the IFN-α/β receptor (IFNAR). In fact, both cytokine receptor complexes activate the same JAK family kinases, except for JAK2, which is activated only downstream of IFN-λ (Odendall et al., 2014; Odendall and Kagan, 2015). Activated JAKs in turn recruit and phosphorylate STAT family members, which then migrate into the nucleus and, together with IFN-regulatory factor 9 (IRF9), mediate the transcription of overlapping sets of IFN-stimulated genes (ISGs; Kotenko, 2011; Lazear et al., 2015a, 2019; Andreakos et al., 2019; Pervolaraki et al., 2019). Finally, both classes of cytokines are induced in response to viral infection and contribute to antiviral immunity (Odendall and Kagan, 2015; Kotenko, 2011; Lazear et al., 2019).
Despite their many similarities to other IFNs, IFN-λ is now emerging as highly specialized group of cytokines, and different aspects of its biological activity have been recently reviewed (Andreakos et al., 2019; Lazear et al., 2019; Ye et al., 2019c). Our review focuses on the unique capacity of IFN-λ to counter pathogen invasion at mucosal sites, where they stimulate pathogen clearance while curbing inflammation to maintain barrier integrity. This specialization of IFN-λ stems partly from the restricted expression of their receptor, partly from the tropism of IFN-λ production, and partly from the unique immunomodulatory properties of this class of IFNs. The type I IFN receptor IFNAR consists of the two chains, IFNAR1 and IFNAR2, and is expressed in virtually every nucleated cell, albeit low levels of mRNA expression have been shown at certain barrier sites, such as the gut (Mahlakõiv et al., 2015; Lin et al., 2016). In contrast, expression of the IFN-λ–specific receptor IFNLR1 is tightly regulated (Ding et al., 2014; Mordstein et al., 2010; Sommereyns et al., 2008; Hermant et al., 2014). At homeostasis, IFNLR1 is expressed at high levels in cells of epithelial lineage (Sommereyns et al., 2008; Hernández et al., 2015; Mordstein et al., 2010; Pott et al., 2011) and in a selected pool of immune cells, with highest levels found in neutrophils (Blazek et al., 2015; Galani et al., 2017; Koltsida et al., 2011; Espinosa et al., 2017; Broggi et al., 2017). This distribution ensures that cells forming the barrier epithelia can rely on a specific IFN system for protection from viral infections. Moreover, the same epithelial cells preferentially express IFN-λ over type I IFNs in response to viral infections (Galani et al., 2015, 2017; Mahlakõiv et al., 2015). In this scenario, the IFN-λ system is triggered in response to mucosal infections that threaten barrier integrity and directly promotes maintenance of barrier function by protecting epithelial cells. Also, innate IFN-λ expression pathways are similar to those that govern expression of type I IFNs, but they involve their own sets of pattern recognition receptors (Odendall et al., 2017), distinct IRF transcription factors, and signaling adaptors (Odendall et al., 2014; Swider et al., 2014); and exhibit a different dependence on NF-κB (Iversen et al., 2010; Ank et al., 2008).
However, what really sets the two IFN systems apart is their differential capacity to modulate the immune response (Zanoni et al., 2017; Ye et al., 2019c). Type I IFNs promote a strong inflammatory response and induce cell-mediated immunity, thereby contributing to the activation of cytotoxic lymphocytes and natural killer cells (Stetson and Medzhitov, 2006; González-Navajas et al., 2012). While type I IFNs can efficiently prevent viral infections by promoting sterilizing immunity, sustained type I IFN signaling during an infection can severely compromise mucosal barrier functions by promoting inflammatory cytokine and chemokine secretion and massive recruitment of inflammatory cells (Trinchieri, 2010; Davidson et al., 2014).
While our understanding of IFN-λ’s capacity to modulate the immune system is in its infancy, some emerging patterns configure the IFN-λ as probarrier cytokines. For example, IFN-λ acts directly on neutrophils to downmodulate tissue-damaging responses such as the release of granules and the production of reactive oxygen species (ROS; Broggi et al., 2017). Also, IFN-λ dampens neutrophil migration to the inflamed tissues and the formation of neutrophil extracellular traps (Blazek et al., 2015; Chrysanthopoulou et al., 2017). Moreover, while IFN-λ and type I IFNs are both able to induce ISG expression in neutrophils, albeit with different magnitude and kinetics, only type I IFNs can trigger the expression of inflammatory cytokines (Galani et al., 2017).
In addition to directly influencing innate immune functions, IFN-λ also promotes humoral adaptive immunity indirectly by stimulating airway epithelial cells (Ye et al., 2019b) and influences lung DCs’ function to promote T-cell memory (Hemann et al., 2019), thereby favoring long-term protection and less damaging immune responses. Here, we describe in detail how IFN-λ helps to maintain mucosal homeostasis at different barrier sites and highlight the unique functions of IFN-λ that set it apart from type I IFNs and configure them as gatekeepers against mucosal infections.
The respiratory tract
The respiratory system is continuously in contact with the environment. We breathe approximately 25,000 times per day, and we constantly expose our nasal, bronchial, and lung mucosae to a variety of microbes. It is thus not surprising that respiratory tract infections, especially those of viral origin, are among the most common illnesses (van Woensel et al., 2003). However, despite this constant exposure of nasal and lung mucosae, we are relatively protected from such viral infections, which are often confined to the upper respiratory tract. In this context, the specific role of type III IFNs in mucosal protection is of particular relevance; however, even though IFN-λ is produced in the respiratory tract in response to a variety of viral pathogens (Crotta et al., 2013; Mahlakõiv et al., 2012; Okabayashi et al., 2011; Baños-Lara et al., 2015), most mechanistic insights into the function of IFN-λ in the airways have been gained in the context of influenza A virus (IAV) infection.
In response to IAV infection, epithelial cells in the respiratory tract express higher levels of type III IFN transcripts and proteins than the expression of type I IFNs, as described in vitro for epithelial cell lines and cultured primary tracheal epithelial cells (Davidson et al., 2016; Crotta et al., 2013) and in vivo for bronchial epithelial cells (Galani et al., 2017). Epithelial cells from the respiratory tract respond to type I as well as type III IFNs (Mordstein et al., 2010; Crotta et al., 2013), and, accordingly, control of IAV infection in Ifnar−/− as well as Ifnlr1−/− animals is impaired in most experimental mouse models (Mordstein et al., 2010; Crotta et al., 2013; Davidson et al., 2014, 2016; Wack et al., 2015; Galani et al., 2017; Wang et al., 2017b).
Of note, though, these animal models are generated by applying high doses of the virus directly to the lower airways, which bypasses the more physiological process of infection. Indeed, the spread of IAV in humans relies on contact between small doses of virus and the upper airways, where most viral infections are controlled and prevented from evolving into more serious lower respiratory tract infections. When mouse models are fine-tuned to reflect the dynamics of physiological infection, the specific role of IFN-λ emerges more clearly. One such approach to more closely mimic the dynamics of IAV transmission in humans was introduced by Galani et al. (2017), who systematically dissected the respective roles of IFN-λ and type I IFNs across a range of infectious doses. They found that at sublethal doses of infection, which more closely reflect the natural exposure to IAV in humans, only mice that were defective in Ifnlr1 exhibited higher viral titers and more severe lung inflammation. This correlates with production of high levels of IFN-λ, especially at the early stage of the infection. Conversely, when the mice are challenged with a lethal dose of IAV, both IFN systems are required for maximal protection, but even under these conditions, early production of IFN-λ is essential for controlling viral titers, as assessed early in IAV encounter.
Another shortcoming common to most experimental models of IAV infection is that the virus is either delivered directly intratracheally or delivered intranasally in large volumes, in essence bypassing the upper airways. Klinkhammer et al. (2018) used an elegant approach to more closely mimic the natural course of infection. They administered IAV intranasally in a very limited volume that prevented the direct delivery of the virus to the trachea and lung. They were thus able to study how the IAV spreads from the upper to the lower airways. They showed that under these conditions, IFN-λ efficiently decreases IAV infection in nasal epithelial cells and is required to limit IAV from spreading to the trachea and lung. As a consequence, Ifnlr1−/− mice showed higher viral titers in nasal secretions, and the IAV infection spread to cohoused sentinel mice more efficiently (Klinkhammer et al., 2018).
Thus, IFN-λ is more efficient in controlling sublethal infections at the site of exposure, whereas type I IFNs become essential once the infection spreads to the lower respiratory tract. Notably, although type I IFNs and IFN-λ are both able to stimulate similar levels of ISG transcription in cultured primary epithelial cells as well as in epithelial cell lines (Galani et al., 2017; Davidson et al., 2016; Crotta et al., 2013; Klinkhammer et al., 2018), when IFNs are administered in vivo, a fraction of nasal epithelial cells remains unresponsive to type I IFNs and is preferentially infected by IAV; this partially explains the higher efficiency of IFN-λ in protecting against IAV infection in the upper airways. The importance of IFN-λ in the upper airways is highlighted by the recent discovery that commensal bacteria that colonize the upper airways are able to induce a primed antiviral state in the lung by inducing IFN-λ (Kim et al., 2019); this IFN-λ–dependent antiviral state is sufficient to protect mice from subsequent IAV infections.
Besides inducing an antiviral state via ISG induction, at least two additional mechanisms must be considered with regard to how IAV infection is restricted by IFN-λ: (i) regulation of the inflammatory process and (ii) modulation of the adaptive immune response. IFN-λ directly protects the respiratory tract epithelia, as demonstrated in conditional mouse models that are deficient in IFN-λ signaling in respiratory epithelial cells (Galani et al., 2017) and in bone marrow chimeras (Crotta et al., 2013; Galani et al., 2017). However, in response to IAV infection, IFN-λ can directly as well as indirectly modulate the immune response in order to ensure long-term protection against IAV (Lazear et al., 2019; Ye et al., 2019b; Andreakos et al., 2019) and to protect the mucosae from collateral damage (Davidson et al., 2016; Galani et al., 2017).
Of the immune cells, neutrophils express the highest levels of Ifnlr1, and IFN-λ can modulate the activation status of purified neutrophils in vitro (Galani et al., 2017; Blazek et al., 2015; Chrysanthopoulou et al., 2017; Broggi et al., 2017). The importance of neutrophil regulation during IAV infection is highlighted in mouse models wherein both neutrophil-specific and respiratory epithelial cell–specific conditional Ifnlr1−/− have a higher viral burden, whereas mice that have a neutrophil-specific knockout of Ifnlr1 have a higher inflammatory signature (Galani et al., 2017). Indeed, during IAV infection, epithelial cells and neutrophils are both infected, and IFN-λ is able to protect both cell types from infection by inducing ISG production. However, while type I IFNs also induce the transcriptional regulation of proinflammatory cytokines in neutrophils, IFN-λ only induces ISGs; thus, IFN-λ contributes to antiviral defense but not to an increase in the inflammatory signature. These results nicely mirror the capacity of IFN-λ treatment to induce a lower inflammatory signature in IAV-infected mice compared to mice that are treated with IFN-α prior to IAV infection, even though both cytokines induce a similar reduction in IAV levels (Davidson et al., 2014, 2016).
An additional layer of protection against respiratory viral infection can be ascribed to the capacity of IFN-λ to indirectly stimulate protective adaptive immunity. In fact, while the majority of immune cells (including B cells) do not respond to IFN-λ in mice, Ifnlr1−/− mice that are infected with IAV have lower levels of hemagglutinin-specific IgG1 and IgA, whereas administration of IFN-λ concomitantly with the infection (or with vaccination) enhances the humoral adaptive response. Notably, bone marrow chimera experiments show that IFN-λ influences humoral adaptive immunity indirectly and stimulates the production of thymic stromal lymphopoietin (TSLP) from lung M cells, which in turn acts on CD103+ migratory lung dendritic cells (DCs) to promote germinal center reactions (Ye et al., 2019a). In contrast, exposure to type I IFNs under the same conditions favors the development of IgG2c independently of TSLP induction (Ye et al., 2019c). IFN-λ also modulates the function of lung DCs to promote skewing of the immune response toward a T helper type 1 cell response (Koltsida et al., 2011; Hemann et al., 2019). Following IAV infection, IFN-λ influences CD103+ DC functions to promote T-cell memory and protect mice from heterologous viral challenge (Hemann et al., 2019). Although mice that lack the IFNLR1 exclusively in DCs are less efficient in generating CD8+ memory T cells, DCs seem to respond ex vivo only to very high doses of recombinant IFN-λ3 (Hemann et al., 2019), suggesting that not only direct IFN-λ signaling in DCs but also indirect activities of IFN-λ on other cells might modulate the immune response elicited against IAV.
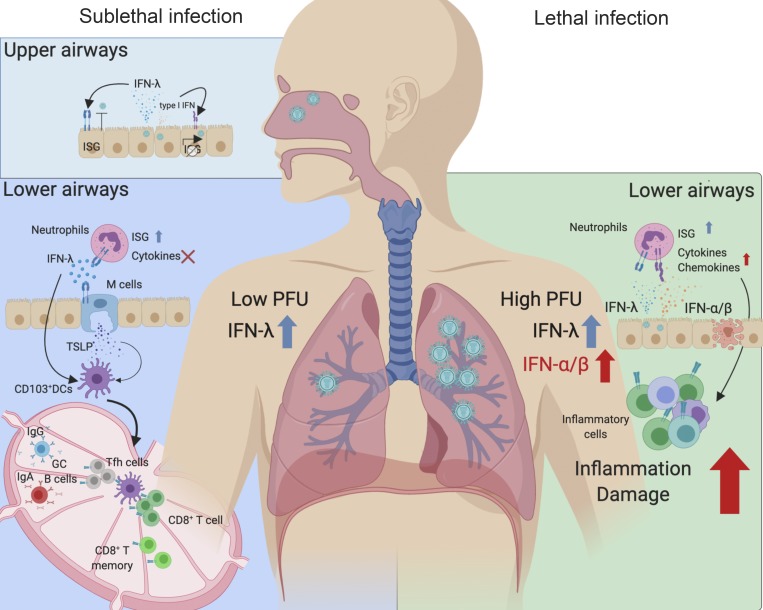
Overall, in response to viral pathogens, IFN-λ protects the airway mucosae by (i) restricting viral replication in epithelial cells at the point of entry, thereby limiting the spread of the virus to the lower airways; (ii) stimulating protective adaptive immunity; and (iii) limiting inflammation and damaging leukocyte responses to maintain barrier integrity (Fig. 1).
Figure 1.
IFN-λ protects the airways against IAV infection. IFN-λ is produced in the upper airways in response to IAV infection and protect the nasal epithelium early after IAV encounter. In the lower airways, at early time points and low infection IAV titers, IFN-λ is sufficient to protect the host from IAV infection. IFN-λ directly induces ISGs in epithelial cells and neutrophils and prevents viral infection but do not induce proinflammatory cytokine production. IFN-λ stimulates long-lasting adaptive immunity by inducing TSLP secretion by airway M cells, which in turn stimulates CD103+ DCs to promote germinal center response. CD103+ DCs also respond directly to IFN-λ stimulation to promote CD8+ T-cell memory. At high viral titers, type I and type III IFNs are both needed for host protection. The production of type I IFNs is associated with a stronger inflammatory response and with the secretion of proinflammatory cytokines. GC B cells, germinal center B cells; Tfh, T follicular helper cell. Images were created with BioRender.
While the majority of viral infections are self-limiting and do not spread to the lower airways, the most severe cases are often accompanied by secondary bacterial superinfections (Krammer et al., 2018). The mechanisms by which viral infections predispose the host to bacterial superinfections are still not completely understood; however, the IFN response appears to play an important role (Parker, 2017). Thus, while IFN-λ serves the function of promoting the mucosal barrier, its capacity to limit the inflammatory response could additionally contribute to the immunosuppressed status of IAV-infected hosts and to the pathogenesis of secondary bacterial superinfections. Accordingly, Ifnlr1−/− mice are partially protected from Staphylococcus aureus and Streptococcus pneumoniae superinfections (Pires and Parker, 2018; Planet et al., 2016), whereas mice that are administered an IFN-λ–overexpressing adenoviral vector have a higher bacterial burden in their lungs (Rich et al., 2019). The molecular and cellular mechanisms that underpin this action of IFN-λ are yet to be defined; however, Ifnlr1−/− mice reportedly clear bacteria more efficiently (Planet et al., 2016; Pires and Parker, 2018) and display higher levels of antimicrobial peptides in the lung than IFN-λ–competent mice (Planet et al., 2016). In contrast, overexpression of IFN-λ in vivo, concomitantly with IAV infection, reduces the number of neutrophils in the bronchoalveolar lavage and impairs the capacity of these cells to phagocytose and kill bacteria (Rich et al., 2019).
While the contribution of IFN-λ to barrier integrity is best investigated following IAV infections in mice, studies on human cell lines have highlighted a role for IFN-λ in the response against human-restricted viral pathogens such as respiratory syncytial virus (RSV; Chi et al., 2006; Okabayashi et al., 2011; Hillyer et al., 2018) and metapneumovirus (Baños-Lara et al., 2015). IFN-λ is preferentially secreted by primary epithelial cells in response to RSV (Okabayashi et al., 2011); however, both IFN systems seem to be necessary for controlling RSV in epithelial cell lines and primary T cells (Chi et al., 2006; Hillyer et al., 2018). Interestingly, in order to escape control by type III IFNs, RSV has evolved the ability to counteract IRF1-dependent IFN-λ secretion by inducing epidermal growth factor signaling (Kalinowski et al., 2018; Hillyer et al., 2012). In agreement with these data, the levels of expression of IFN-λ and Ifnlr1 measured in nasal lavages of RSV-infected pediatric patients correlate with disease severity (Selvaggi et al., 2014; Pierangeli et al., 2018).
Finally, IFN-λ can also be induced in the lung outside the context of viral infection. In a model of Aspergillus fumigatus–induced pneumonia, IFN-λ stimulates pathogen clearance by enhancing ROS production in neutrophils in a STAT1-dependent manner, in contrast to what is observed in vitro in response to bacterial or inflammatory stimuli and in vivo in a model of intestinal inflammation (Broggi et al., 2017), suggesting that IFN-λ can modulate inflammation differently in response to different classes of pathogens (Espinosa et al., 2017).
The gastrointestinal system
The delicate balance between pathogen resistance and maintenance of barrier function is of pivotal importance in the gastrointestinal tract, as it is home to the highest number and greatest diversity of commensal microbes in the body. IFN-λ is unique in protecting the intestine from enteric viral infections while maintaining an anti-inflammatory state that safeguards the barrier function. Here, too, the tropism of IFN-λ production and sensing is key to its function. In contrast to the airway epithelium, the gut intestinal epithelial cells (IECs) respond preferentially to IFN-λ in vivo (although epithelial cell lines and isolated primary IECs are able to respond to both IFNs ex vivo; Pott et al., 2011), whereas lamina propria lymphocytes mainly respond to type I IFNs. This creates a compartmentalized system in which IFN-λ protects the barrier epithelia, whereas type I IFNs intervene only when the barrier has been breached. This selective responsiveness is reflected in receptor expression: IECs express high transcript levels of Ifnlr1 and lower levels of Ifnar1 and Ifnar2 transcripts, whereas lamina propria lymphocytes only express the type I IFN receptor (Bhushal et al., 2017; Lin et al., 2016; Mordstein et al., 2010; Feng et al., 2008; Pott et al., 2011; Mahlakõiv et al., 2015). Responsiveness to IFN-λ is also influenced by the epigenetic and polarization status of IECs (Pott et al., 2011; Bhushal et al., 2017; Lin et al., 2016; Ding et al., 2014). Moreover, the two receptor systems have been recently shown to cross-regulate each other’s downstream signaling pathway. Epithelial cell lines where IFNLR signaling is blocked induce higher levels of ISGs when stimulated with type I IFNs, whereas depletion or blockade of IFNAR1 and IFNAR2 negatively regulates the sensitivity of IFN-λ (Pervolaraki et al., 2019). This effect is independent of regulation of receptor expression and acts at the level of STAT1 phosphorylation (Pervolaraki et al., 2019).
Another layer of compartmentalization is conferred by the differential induction of IFN types; in particular, IECs preferentially express IFN-λ in response to viral infection in vivo (Mahlakõiv et al., 2015; Hernández et al., 2015). In vitro evidence derived from human epithelial cell lines suggests that the subcellular localization of the signaling adaptor mitochondrial antiviral-signaling protein (MAVS) dictates the preferential induction of one class of IFNs over the other (Odendall et al., 2014; Odendall and Kagan, 2015): the association of MAVS with peroxisomes induces IFN-λ, whereas type I IFNs are induced in response to activation of mitochondrial MAVS. The particularly abundant pool of peroxisomes in epithelial cells explains the preferential induction of IFN-λ (Odendall et al., 2014).
The existence of such compartmentalization is supported by results of analyzing variations in the capacity of different families of IFNs to control viruses with dissimilar tropisms. Indeed, IFN-λ preferentially controls viruses that infect epithelial cells, whereas type I IFNs are fundamental to the control of viruses that bypass the epithelial layer and can spread systemically. A clear example of such tropism is seen during norovirus infection: human norovirus causes acute gastroenteritis that typically resolves within 1–2 d, with viral shedding persisting in the stools of asymptomatic patients for several days (Karst et al., 2014; Robilotti et al., 2015). The mouse relative norovirus (MNV-1) can induce either an acute illness that is typically controlled by the adaptive immune system (Chachu et al., 2008a; 2008b) or a persistent infection characterized by continuous fecal shedding (Thackray et al., 2007; Kernbauer et al., 2014). Over the years, a variety of MNV strains have been isolated that trigger either acute or persistent infection (Thackray et al., 2007) and have been thoroughly characterized (Nice et al., 2018). Acute norovirus bypasses epithelial barriers and infects immune cells in the intestinal lamina propria before spreading systemically (Nice et al., 2013; Strong et al., 2012). Consistent with the compartmentalized system that exists in the gut, the acute virus strain is completely dependent on type I IFNs for clearance, as Ifnar−/− mice and Stat1−/− mice succumb to the infection (Karst et al., 2003; Nice et al., 2016). In contrast, the persistent strain of norovirus, which only infects tuft cells of epithelial lineage (Wilen et al., 2018), is controlled specifically by IFN-λ (Baldridge et al., 2015; Nice et al., 2015): therapeutic administration of IFN-λ is sufficient to completely clear persistent norovirus, even in the absence of an adaptive immune system. Furthermore, if conditional epithelial cell–specific Ifnlr1−/− mice are infected with the persistent norovirus strain, they are insensitive to IFN-λ administration and present higher viral titers and viral shedding than WT mice (Baldridge et al., 2017). Another testament to the importance of IFN-λ in the control of the epithelial tropic form of MNV comes from microbiome studies in which bacterial depletion by antibiotic treatment favors norovirus clearance in WT mice. However, this effect is abrogated only in Ifnlr1−/− mice, whereas deletion of Ifnar1, Ifngr1, and sensors such as retinoic acid-inducible gene I (RIG-I), TLRs, and their signaling adaptors did not alter the phenotype (Baldridge et al., 2015). This effect of commensal bacteria only affects the persistence of norovirus, because neither antibiotic treatment nor IFNLR1 deficiency affects MNV strains that do not infect the epithelium, such as the acute strain CW3.
The importance of IFN-λ in controlling persistent norovirus is also evident from the viewpoint of the pathogen: the viral nonstructural protein NS1 that is required for IEC tropism of persistent norovirus is genetically different in strains that induce acute infections (Nice et al., 2013), and it has been recently implicated in conferring resistance to IFN-λ control (Lee et al., 2019).
Another pathogen that reveals the specialization of the two classes of IFNs in the gut is reovirus, which infects epithelial cells and also directly spreads in the underlying lamina propria. Type I IFNs are necessary to contain systemic spread, and, consequently, Ifnar1−/− mice develop lethal reovirus infections that cause encephalitis (Johansson et al., 2007). The infection of epithelial cells, however, is completely dependent on IFN-λ because reovirus is only detectable in epithelial cells of Ifnlr1−/− mice (Mahlakõiv et al., 2015), and conditional epithelial knockout mice have a higher viral burden in the intestine (Baldridge et al., 2017) and shed significantly more virus in the feces (Mahlakõiv et al., 2015).
Rotavirus, which prominently infects epithelial cells, is efficiently controlled by IFN-λ (Hernández et al., 2015; Pott et al., 2011), and only Ifnlr1−/−(and not Ifnar1−/−) mice shed more virus in the feces and display higher viral titers and stronger epithelial damage (Hernández et al., 2015; Pott et al., 2011). However, depending on the mouse strain, the use of homologous or heterologous viral strains, and the age of the mouse, type I IFNs and IFN-λ may have overlapping functions in the control of rotavirus infections (Lin et al., 2016; Ingle et al., 2018; Feng et al., 2008). In particular, although adult IECs do not respond to type I IFNs in vivo, the IECs from neonatal mice respond to both classes of IFNs, indicating that both IFN systems are required during development for optimal protection against rotavirus (Lin et al., 2016). Infection models in human enteroids confirm the central role of IFN-λ in the control of rotavirus infection because infected enteroids preferentially induce high levels of the IFN-λ transcript as opposed to that for type I IFNs, and transcriptional upregulation of antiviral ISGs is abolished by treatment with an antibody against IFNLR1 (Saxena et al., 2017). However, antibody blockade of IFNLR1 does not alter the outcome of rotavirus infection in human enteroids, suggesting that rotavirus has adapted to overcome autocrine IFN-λ control or that larger amounts of IFN-λ from hematopoietic sources are necessary.
Although IFN-λ is most studied for its direct antiviral action on IECs, recent studies also highlight the importance of these cytokines in curbing excessive inflammation in acute models of intestinal inflammation (Chiriac et al., 2017; Rauch et al., 2015; Broggi et al., 2017). Indeed, IFN-λ acts on neutrophils in vitro to downmodulate tissue-damaging functions such as ROS production and degranulation through a unique nontranslational mechanism that is also independent of STAT activation and ISG transcription (Broggi et al., 2017). This is reflected in mouse models of acute intestinal inflammation, where administering dextran sulfate sodium to Ifnlr1−/− mice leads to an aggravated pathological state characterized by a high level of oxidative stress response. Moreover, IFN-λ2 administration greatly ameliorates colitis in WT animals (Chiriac et al., 2017; Broggi et al., 2017). Chimera experiments and the use of mice with specific Ifnlr1 depletion only in neutrophils reveal that the protective effect of IFN-λ can be ascribed to the regulation of neutrophil responses (Broggi et al., 2017). IFN-λ also protects barrier integrity during acute intestinal inflammation in the absence of an active viral infection. Indeed, low mRNA levels of IFN-λ capable of inducing tonic ISG expression are detected in the gut in homeostatic conditions (Mahlakõiv et al., 2015; Lin et al., 2016; Ingle et al., 2019). Tonic production of IFN-λ has been linked to the intestinal virome (Broggi et al., 2017). In fact, when the mouse virome is perturbed following treatment with an antiviral drug cocktail, tonic IFN-λ and IFN-β levels are low (Yang et al., 2016; Broggi et al., 2017), and mice become more susceptible to dextran sulfate sodium–induced colitis. The absence of protective IFN-λ is the likely cause of this increased susceptibility because Ifnar−/− mice behave similarly to WT mice, whereas Ifnlr1−/− mice largely phenocopy mice that have been depleted of enteric viruses (Broggi et al., 2017). Treatment of mice with antiviral drugs induces changes in the composition of the intestinal virome, similar to the alterations observed in patients with inflammatory bowel disease (Norman et al., 2015) and in mouse models of chronic colitis (Duerkop et al., 2018).
Because most of the viruses identified in the mammalian gut are bacteriophages, it is difficult to discriminate between direct effects of the mammalian virome on the host immune system and secondary effects based on remodeling of the bacterial microbiome (Virgin, 2014). The serendipitous discovery that a previously unidentified strain of mouse astrovirus is sufficient to protect immunodeficient hosts from norovirus infections supports the hypothesis that commensal viruses induce IFN-λ (Ingle et al., 2019). Mice colonized with astrovirus display basal levels of IFN-λ produced by the gut epithelial cells that have been infected by the virus, and colonization of Ifnlr1−/− mice with this virus is ineffective in inducing protection. Therefore, basal levels of IFN-λ induced by commensals poise the gut epithelium to respond to viral infections. These levels of IFN-λ are sufficient to protect the intestinal epithelium even in the absence of an adaptive immune response (Ingle et al., 2019). This effect is specific for IFN-λ: astrovirus colonization has no effect on inducing type I or type II IFN.
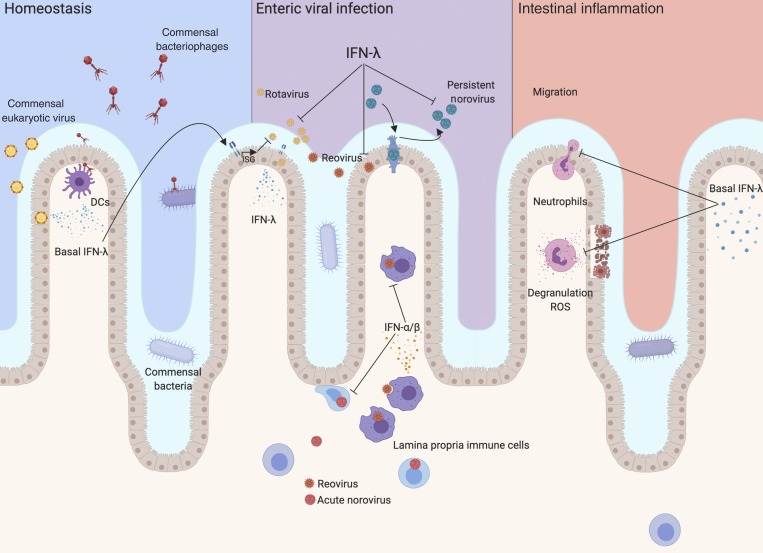
In summary, IFN-λ provides a vital defense mechanism in the gut. They protect the epithelium from viral infections, and the tonic expression of IFN-λ maintains an anti-inflammatory state that is fundamental in such a microbe-rich environment (Fig. 2).
Figure 2.
IFN-λ protects intestinal barrier functions. In homeostatic conditions, commensal viruses stimulate basal IFN-λ production that maintains both an antiviral state and an anti-inflammatory environment. Basal ISGs induced by IFN-λ in IECs protect them from enteric viral infections. During enteric viral infections, IFN-λ is preferentially induced and protects the mucosae from epithelial tropic viruses such as rotavirus, reovirus, and persistent strains of norovirus. Low transcript expression of IFNAR1/2 by IECs renders them largely dependent on IFN-λ for protection against viruses. In contrast, protection against viruses that can bypass the epithelium and infect lymphocytes residing in the lamina propria, such as reovirus and acute strains of norovirus, is dependent on type I IFNs. During acute intestinal inflammation, IFN-λ induced by commensals inhibits neutrophil-damaging functions and protects the mucosal barrier from excessive damage. Images were created with BioRender.
Other barrier sites
Although IFN-λ has been most intensely studied in the respiratory and gastrointestinal systems, additional barrier tissues also depend on IFN-λ to maintain their integrity.
Although mouse hepatocytes do not express IFNLR1 and are not responsive to IFN-λ, in humans, the IFNLR1 is expressed at very high levels in hepatocytes, and IFN-λ plays an important role in protection against liver viral infections. IFN-λ is expressed at high levels in the liver of patients with chronic hepatitis C (CHC; Thomas et al., 2012) and in chimpanzees experimentally infected with hepatitis C virus (HCV; Thomas et al., 2012; Park et al., 2012). Moreover IFN-λ is preferentially induced over type I IFNs in response to HCV or hepatitis B virus (HBV) infection of human hepatocytes (Thomas et al., 2012; Marukian et al., 2011; Park et al., 2012) and protect them from HBV or HCV infection (Doyle et al., 2006; Marcello et al., 2006; Robek et al., 2005). Accordingly, several genome-wide association studies identified polymorphisms in IFN-λ genes that are associated with the outcome of HBV or HCV infection and the responsiveness to therapy, as extensively reviewed elsewhere (Onabajo et al., 2019; Pagliaccetti and Robek, 2010; Hemann et al., 2017; Boisvert and Shoukry, 2016). Before the introduction of direct-acting antiviral (DAA) drugs that target HCV proteases and RNA polymerases, the main therapeutic option against CHC was the combination of ribavirin and type I IFNs, a treatment with many side effects prominently due to type I IFN administration (Bruening et al., 2017). The efficacy of IFN-λ in inducing HCV clearance in vitro and the limited pattern of expression of IFNLR1 raised interest in the use of IFN-λ to treat CHC. Indeed, patients treated with recombinant IFN-λ1 conjugated with polyethylene glycol (PEG–IFN-λ1) in combination with ribavirin and/or DAAs exhibited lesser side effects, whereas success rates in reducing detectable HCV RNA in the blood were similar to those seen in patients treated with the conventional PEG–IFN-α2a combination therapy (Muir et al., 2010; Muir et al., 2014; Flisiak et al., 2016a; Flisiak et al., 2016b). While the pursuit of IFN-λ as a therapeutic for CHC has been stalled by the discovery of DAA drugs, these studies highlighted the safety of PEG–IFN-λ therapies.
Other cells of epithelial lineage, such as those in the female reproductive tract mucosa, respond to IFN-λ, and administration of IFN-λ is protective against infection by HSV-2 (Ank et al., 2006) and Zika virus (Caine et al., 2019). Recent studies highlight a role for IFN-λ in protecting the placental barrier from viral infection. Human trophoblasts cultured from full-term placentas constitutively express IFN-λ1, and supernatant from cultured primary human trophoblasts protects nonplacental cells from infection with Zika virus or other teratogenic viruses. This protective effect depends on IFN-λ because treatment with human trophoblast supernatant is ineffective in cells that are naturally unresponsive to type III IFNs or in cells wherein the expression of Ifnlr1 is knocked down via RNA interference (Bayer et al., 2016; Corry et al., 2017). IFN-λ acts in a paracrine fashion, protecting nonplacental cells from viral infection, but they also contribute to the autocrine protection of the placental barrier. Indeed, cells of human chorionic villi express high basal levels of ISGs in the absence of a viral infection; these levels can be reduced when JAK signaling is blocked with use of chemical inhibitors (Corry et al., 2017). Further indication of the relevance of IFN-λ in protecting the fetus against transplacental transmission of virus comes from mouse studies. Infection of pregnant dams with Zika virus before placentation leads to embryonic lethality in both WT and Ifnlr1−/− animals, but following full placentation, only the placentas of fetuses that lack IFNLR1 permit efficient vertical transmission, which in turn leads to higher rates of fetal malformation. When only the pregnant dam is deficient in IFN-λ signaling, the heterozygous Ifnlr1-sufficient progeny do not display higher viral burden or fetal abnormalities, also supporting the relevance of IFN-λ signaling in the fetal placenta and not in maternal tissues (Jagger et al., 2017). Treatment of WT pregnant dams with IFN-λ further decreases vertical viral transmission, pointing to the therapeutic potential of IFN-λ.
Finally, IFN-λ also contributes to barrier integrity at the blood–brain barrier (BBB). When infected with the neurovirulent West Nile virus, higher viral burden in the central nervous system of Ifnlr1−/− mice than in that of WT mice correlates with increased permeability (Lazear et al., 2015b). Similarly, mice deficient in both type I IFN and IFN-λ signaling succumb after infection with the live attenuated strain of yellow fever virus YFV-17D. In contrast, Ifnar−/− mice, though unable to control viral titer as well as WT mice, survive the infection. The lethality of the double mutant correlated with the enhanced permeability of the BBB (Douam et al., 2017). The capacity of IFN-λ to preserve the integrity and function of the BBB was also recapitulated in vitro. Thus, treatment of brain microvascular endothelial cells with IFN-λ increases transepithelial resistance and decreased leakage of the West Nile virus across the barrier. Of note, IFN-λ acts in a transcription- and STAT1-independent manner in neutrophils as well as in endothelial cells, confirming the existence of an IFN-λ–specific nontranscriptional pathway.
Conclusions and perspectives
Since their discovery, IFN-λ has been compared with type I IFNs and has faced scrutiny in relation to its apparent redundancy, but in the last 15 yr, we gained significant insights into the uniqueness of this class of cytokines. Initially considered to be a second layer of defense to protect barrier epithelia against viral infections, new specialized functions of IFN-λ has continued to emerge. To date, the most specialized role of IFN-λ is ascribed to their specific immunoregulatory role, which (contrary to that of type I IFNs) promotes a gentler inflammatory response that better protects the integrity of barrier mucosae without compromising their capacity to fight pathogen invasion. Few immune cell types (namely, neutrophils and DCs) directly respond to IFN-λ signaling in mice, but the recent discovery of their indirect immunomodulatory effects with profound and long-lasting effects on adaptive immunity opens the gate for an exciting field of study. While our knowledge of how IFN-λ influences immune cells in mice is expanding, the translation of these findings to humans is confounded by the different pattern of expression of the IFNLR1 in human cells. For instance, neutrophils display the highest response to IFN-λ in mice, but mature human neutrophils express lower transcript levels of the receptor, which is upregulated in inflammatory conditions (Broggi et al., 2017; Espinosa et al., 2017). Also in humans, plasmacytoid DCs (Finotti et al., 2017, 2016a, 2016b; Kelly et al., 2016) and macrophages (Wang et al., 2017b; Hou et al., 2009) respond directly to IFN-λ. The existence of a soluble splice variant of human IFNLR1 that is incapable of signaling and is expressed mainly in immune cells further complicates the study of IFN-λ biology in humans (Witte et al., 2009).
Additional insights into IFN-λ signaling derive from the discovery of IFN-λ–specific functions that are not shared with those of type I IFNs: for example, nontranscriptional pathways that modulate neutrophil function or tightening of the BBB, or the unknown pathway that induces TSLP production in the airway epithelium downstream only of type III IFNs. Although the JAK–STAT signaling pathways have been extensively studied, it is still unclear how different receptors that use similar adaptors and result in similar patterns of STAT member phosphorylation give rise to different transcriptional responses (Subramaniam et al., 2001). IFN-λ induces an intracellular response that is remarkably similar to that triggered by type I IFNs, but they can also use different signaling adaptors such as JAK2 (Odendall et al., 2014; Odendall and Kagan, 2015) which participate in noncanonical JAK–STAT signaling pathways that rely on nuclear translocation of the cytokine–receptor complex and histone phosphorylation to regulate transcriptional specificity downstream of IFN-γ (Johnson et al., 2019; Dawson et al., 2009).
Moreover, both classes of IFNs can activate alternative pathways, such as the MAPK pathway, and differences in the capacity to activate these signaling cascades may contribute to the unique roles of IFN-λ (Pervolaraki et al., 2017). Specific roles of the two classes of IFNs can also stem from the differential dynamics of ISG induction (Bolen et al., 2014; Marcello et al., 2006; Jilg et al., 2014; Pervolaraki et al., 2018). Studies in human hepatocytes and human colonoids indicate that although type I IFNs induce transcription of ISG rapidly but transiently, IFN-λ has a slower response that is sustained over time (Bolen et al., 2014; Jilg et al., 2014; Pervolaraki et al., 2018; Forero et al., 2019). Moreover, IFN-λ induces lower levels of ISGs in cells stimulated with the same amount of type I IFN and IFN-λ (Zhou et al., 2007; Crotta et al., 2013). Ram Savan’s group recently elucidated some of the molecular basis of the different dynamics of these two groups of IFNs (Forero et al., 2019). The early induction of ISGs elicited by type I IFNs can be ascribed to their ability to induce STAT1-dependent transcription of IRF1. IRF1 is induced at much lower levels by IFN-λ than type I IFNs and is responsible not only for promoting early ISG induction but also for shutting off ISG transcription. Indeed, IRF1 uniquely promotes the transcription of the negative regulator USP18 (Forero et al., 2019), which selectively inhibits type I IFN signaling without affecting IFN-λ signaling (Blumer et al., 2017). The capacity of type I IFNs to efficiently induce the activation of IRF1 also explains their increased inflammatory capacity compared with IFN-λ, because IRF1 uniquely controls the transcription of proinflammatory chemokines, such as CXCL10 and CXCL9 (Forero et al., 2019). The differences between the two groups of IFNs are intrinsically regulated by the specific signaling capacity of each receptor complex and the respective ability to induce STAT1 dimer formation (Pervolaraki et al., 2019; Forero et al., 2019). Further exploration of the noncanonical intracellular pathways and the kinetic of IFN-λ signaling will uncover IFN-λ–specific functions that are not shared with other classes of IFNs.
In summary, what we know about IFN-λ biology positions these cytokines as frontline defenses that protect our mucosal barriers from viral threats and contribute to the maintenance of an efficient barrier by finely modulating the immune response. Further study of IFN-λ–specific signaling and of the nuances of IFN-λ's direct and indirect modulation of inflammation is warranted to comprehend the full potential of IFN-λ.
Acknowledgments
I. Zanoni is supported by the National Institutes of Health (grants R01AI121066, R01DK115217, and NIAID-DAIT-NIHAI201700100). A. Broggi is supported by a Crohn’s and Colitis Foundation of America research fellowship award (number 549868). F. Granucci is supported by the Associazione Italiana per la Ricerca sul Cancro (IG 2016Id.18842), the Cariplo Foundation (grant 2014-0655), and the Fondazione Regionale per la Ricerca Biomedica.
The authors declare no competing financial interests.
Author contributions: A. Broggi, F. Granucci, and I. Zanoni wrote the manuscript and designed the figures.
References
- Andreakos E., Zanoni I., and Galani I.E.. 2019. Lambda interferons come to light: dual function cytokines mediating antiviral immunity and damage control. Curr. Opin. Immunol. 56:67–75. 10.1016/j.coi.2018.10.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ank N., West H., Bartholdy C., Eriksson K., Thomsen A.R., and Paludan S.R.. 2006. Lambda interferon (IFN-lambda), a type III IFN, is induced by viruses and IFNs and displays potent antiviral activity against select virus infections in vivo. J. Virol. 80:4501–4509. 10.1128/JVI.80.9.4501-4509.2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ank N., Iversen M.B., Bartholdy C., Staeheli P., Hartmann R., Jensen U.B., Dagnaes-Hansen F., Thomsen A.R., Chen Z., Haugen H., et al. 2008. An important role for type III interferon (IFN-λ/IL-28) in TLR-induced antiviral activity. J. Immunol. 180:2474–2485. 10.4049/jimmunol.180.4.2474 [DOI] [PubMed] [Google Scholar]
- Baldridge M.T., Nice T.J., McCune B.T., Yokoyama C.C., Kambal A., Wheadon M., Diamond M.S., Ivanova Y., Artyomov M., and Virgin H.W.. 2015. Commensal microbes and interferon-λ determine persistence of enteric murine norovirus infection. Science. 347:266–269. 10.1126/science.1258025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baldridge M.T., Lee S., Brown J.J., McAllister N., Urbanek K., Dermody T.S., Nice T.J., and Virgin H.W.. 2017. Expression of Ifnlr1 on intestinal epithelial cells is critical to the antiviral effects of interferon lambda against norovirus and reovirus. J. Virol. 91:e02079-16 10.1128/JVI.02079-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baños-Lara M.R., Harvey L., Mendoza A., Simms D., Chouljenko V.N., Wakamatsu N., Kousoulas K.G., and Guerrero-Plata A.. 2015. Impact and regulation of lambda interferon response in human metapneumovirus infection. J. Virol. 89:730–742. 10.1128/JVI.02897-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bayer A., Lennemann N.J., Ouyang Y., Bramley J.C., Morosky S., Marques E.T. Jr., Cherry S., Sadovsky Y., and Coyne C.B.. 2016. Type III interferons produced by human placental trophoblasts confer protection against Zika virus infection. Cell Host Microbe. 19:705–712. 10.1016/j.chom.2016.03.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhushal S., Wolfsmüller M., Selvakumar T.A., Kemper L., Wirth D., Hornef M.W., Hauser H., and Köster M.. 2017. Cell polarization and epigenetic status shape the heterogeneous response to type III interferons in intestinal epithelial cells. Front. Immunol. 8:671 10.3389/fimmu.2017.00671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blazek K., Eames H.L., Weiss M., Byrne A.J., Perocheau D., Pease J.E., Doyle S., McCann F., Williams R.O., and Udalova I.A.. 2015. IFN-λ resolves inflammation via suppression of neutrophil infiltration and IL-1β production. J. Exp. Med. 212:845–853. 10.1084/jem.20140995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blumer T., Coto-Llerena M., Duong F.H.T., and Heim M.H.. 2017. SOCS1 is an inducible negative regulator of interferon λ (IFN-λ)-induced gene expression in vivo. J. Biol. Chem. 292:17928–17938. 10.1074/jbc.M117.788877 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boisvert M., and Shoukry N.H.. 2016. Type III interferons in hepatitis C virus infection. Front. Immunol. 7:628 10.3389/fimmu.2016.00628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolen C.R., Ding S., Robek M.D., and Kleinstein S.H.. 2014. Dynamic expression profiling of type I and type III interferon-stimulated hepatocytes reveals a stable hierarchy of gene expression. Hepatology. 59:1262–1272. 10.1002/hep.26657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broggi A., Tan Y., Granucci F., and Zanoni I.. 2017. IFN-λ suppresses intestinal inflammation by non-translational regulation of neutrophil function. Nat. Immunol. 18:1084–1093. 10.1038/ni.3821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruening J., Weigel B., and Gerold G.. 2017. The role of type III interferons in hepatitis C virus infection and therapy. J. Immunol. Res. 2017:7232361 10.1155/2017/7232361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caine E.A., Scheaffer S.M., Arora N., Zaitsev K., Artyomov M.N., Coyne C.B., Moley K.H., and Diamond M.S.. 2019. Interferon lambda protects the female reproductive tract against Zika virus infection. Nat. Commun. 10:280 10.1038/s41467-018-07993-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chachu K.A., LoBue A.D., Strong D.W., Baric R.S., and Virgin H.W.. 2008a Immune mechanisms responsible for vaccination against and clearance of mucosal and lymphatic norovirus infection. PLoS Pathog. 4:e1000236 10.1371/journal.ppat.1000236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chachu K.A., Strong D.W., LoBue A.D., Wobus C.E., Baric R.S., and Virgin H.W. IV. 2008b Antibody is critical for the clearance of murine norovirus infection. J. Virol. 82:6610–6617. 10.1128/JVI.00141-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chi B., Dickensheets H.L., Spann K.M., Alston M.A., Luongo C., Dumoutier L., Huang J., Renauld J.-C., Kotenko S.V., Roederer M., et al. 2006. Alpha and lambda interferon together mediate suppression of CD4 T cells induced by respiratory syncytial virus. J. Virol. 80:5032–5040. 10.1128/JVI.80.10.5032-5040.2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiriac M., Günther C., Becker C., Siebler J., and Neurath M.. 2017. IL-28-dependent activation of epithelial STAT1 drives epithelial wound healing in inflammatory bowel disease [abstract]. Gastroenterology. 152(5, 5 suppl_1):S90 10.1016/S0016-5085(17)30650-9 [DOI] [Google Scholar]
- Chrysanthopoulou A., Kambas K., Stakos D., Mitroulis I., Mitsios A., Vidali V., Angelidou I., Bochenek M., Arelaki S., Arampatzioglou A., et al. 2017. Interferon lambda1/IL-29 and inorganic polyphosphate are novel regulators of neutrophil-driven thromboinflammation. J. Pathol. 243:111–122. 10.1002/path.4935 [DOI] [PubMed] [Google Scholar]
- Corry J., Arora N., Good C.A., Sadovsky Y., and Coyne C.B.. 2017. Organotypic models of type III interferon-mediated protection from Zika virus infections at the maternal-fetal interface. Proc. Natl. Acad. Sci. USA. 114:9433–9438. 10.1073/pnas.1707513114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crotta S., Davidson S., Mahlakõiv T., Desmet C.J., Buckwalter M.R., Albert M.L., Staeheli P., and Wack A.. 2013. Type I and type III interferons drive redundant amplification loops to induce a transcriptional signature in influenza-infected airway epithelia. PLoS Pathog. 9:e1003773 10.1371/journal.ppat.1003773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson S., Crotta S., McCabe T.M., and Wack A.. 2014. Pathogenic potential of interferon αβ in acute influenza infection. Nat. Commun. 5:3864 10.1038/ncomms4864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson S., McCabe T.M., Crotta S., Gad H.H., Hessel E.M., Beinke S., Hartmann R., and Wack A.. 2016. IFNλ is a potent anti-influenza therapeutic without the inflammatory side effects of IFNα treatment. EMBO Mol. Med. 8:1099–1112. 10.15252/emmm.201606413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson M.A., Bannister A.J., Göttgens B., Foster S.D., Bartke T., Green A.R., and Kouzarides T.. 2009. JAK2 phosphorylates histone H3Y41 and excludes HP1α from chromatin. Nature. 461:819–822. 10.1038/nature08448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ding S., Khoury-Hanold W., Iwasaki A., and Robek M.D.. 2014. Epigenetic reprogramming of the type III interferon response potentiates antiviral activity and suppresses tumor growth. PLoS Biol. 12:e1001758 10.1371/journal.pbio.1001758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Douam F., Soto Albrecht Y.E., Hrebikova G., Sadimin E., Davidson C., Kotenko S.V., and Ploss A.. 2017. Type III interferon-mediated signaling is critical for controlling live attenuated yellow fever virus infection in vivo. MBio. 8:e00819-17 10.1128/mBio.00819-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doyle S.E., Schreckhise H., Khuu-Duong K., Henderson K., Rosler R., Storey H., Yao L., Liu H., Barahmand-pour F., Sivakumar P., et al. 2006. Interleukin-29 uses a type 1 interferon-like program to promote antiviral responses in human hepatocytes. Hepatology. 44:896–906. 10.1002/hep.21312 [DOI] [PubMed] [Google Scholar]
- Duerkop B.A., Kleiner M., Paez-Espino D., Zhu W., Bushnell B., Hassell B., Winter S.E., Kyrpides N.C., and Hooper L.V.. 2018. Murine colitis reveals a disease-associated bacteriophage community. Nat. Microbiol. 3:1023–1031. 10.1038/s41564-018-0210-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Espinosa V., Dutta O., McElrath C., Du P., Chang Y.-J., Cicciarelli B., Pitler A., Whitehead I., Obar J.J., Durbin J.E., et al. 2017. Type III interferon is a critical regulator of innate antifungal immunity. Sci. Immunol. 2:eaan5357 10.1126/sciimmunol.aan5357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng N., Kim B., Fenaux M., Nguyen H., Vo P., Omary M.B., and Greenberg H.B.. 2008. Role of interferon in homologous and heterologous rotavirus infection in the intestines and extraintestinal organs of suckling mice. J. Virol. 82:7578–7590. 10.1128/JVI.00391-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finotti G., Tamassia N., Calzetti F., Fattovich G., and Cassatella M.A.. 2016a Endogenously produced TNF-α contributes to the expression of CXCL10/IP-10 in IFN-λ3-activated plasmacytoid dendritic cells. J. Leukoc. Biol. 99:107–119. 10.1189/jlb.3VMA0415-144R [DOI] [PubMed] [Google Scholar]
- Finotti G., Tamassia N., and Cassatella M.A.. 2016b Synergistic production of TNFα and IFNα by human pDCs incubated with IFNλ3 and IL-3. Cytokine. 86:124–131. 10.1016/j.cyto.2016.08.005 [DOI] [PubMed] [Google Scholar]
- Finotti G., Tamassia N., and Cassatella M.A.. 2017. Interferon-λs and plasmacytoid dendritic cells: A close relationship. Front. Immunol. 8:1015 10.3389/fimmu.2017.01015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flisiak R., Kawazoe S., Znoyko O., Assy N., Gadano A., Kao J.-H., Lee K.-S., Zwirtes R., Portsmouth S., Dong Y., et al. 2016a Peginterferon lambda-1a/ribavirin with daclatasvir or peginterferon alfa-2a/ribavirin with telaprevir for chronic hepatitis C genotype 1b. J. Interferon Cytokine Res. 36:635–643. 10.1089/jir.2015.0173 [DOI] [PubMed] [Google Scholar]
- Flisiak R., Shiffman M., Arenas J., Cheinquer H., Nikitin I., Dong Y., Rana K., and Srinivasan S.. 2016b A randomized study of peginterferon lambda-1a compared to peginterferon alfa-2a in combination with ribavirin and telaprevir in patients with genotype-1 chronic hepatitis C. PLoS One. 11:e0164563 10.1371/journal.pone.0164563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forero A., Ozarkar S., Li H., Lee C.H., Hemann E.A., Nadjsombati M.S., Hendricks M.R., So L., Green R., Roy C.N., et al. 2019. Differential activation of the transcription factor IRF1 underlies the distinct immune responses elicited by type I and type III interferons. Immunity. 51:451–464.e6. 10.1016/j.immuni.2019.07.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galani I.E., Koltsida O., and Andreakos E.. 2015. Type III interferons (IFNs): Emerging master regulators of immunity. Adv. Exp. Med. Biol. 850:1–15. 10.1007/978-3-319-15774-0_1 [DOI] [PubMed] [Google Scholar]
- Galani I.E., Triantafyllia V., Eleminiadou E.-E., Koltsida O., Stavropoulos A., Manioudaki M., Thanos D., Doyle S.E., Kotenko S.V., Thanopoulou K., and Andreakos E.. 2017. Interferon-λ mediates non-redundant front-line antiviral protection against influenza virus infection without compromising host fitness. Immunity. 46:875–890.e6. 10.1016/j.immuni.2017.04.025 [DOI] [PubMed] [Google Scholar]
- González-Navajas J.M., Lee J., David M., and Raz E.. 2012. Immunomodulatory functions of type I interferons. Nat. Rev. Immunol. 12:125–135. 10.1038/nri3133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hemann E.A., Gale M. Jr., and Savan R.. 2017. Interferon lambda genetics and biology in regulation of viral control. Front. Immunol. 8:1707 10.3389/fimmu.2017.01707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hemann E.A., Green R., Turnbull J.B., Langlois R.A., Savan R., and Gale M. Jr. 2019. Interferon-λ modulates dendritic cells to facilitate T cell immunity during infection with influenza A virus. Nat. Immunol. 20:1035–1045. 10.1038/s41590-019-0408-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hermant P., Demarez C., Mahlakõiv T., Staeheli P., Meuleman P., and Michiels T.. 2014. Human but not mouse hepatocytes respond to interferon-lambda in vivo. PLoS One. 9:e87906 10.1371/journal.pone.0087906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernández P.P., Mahlakõiv T., Yang I., Schwierzeck V., Nguyen N., Guendel F., Gronke K., Ryffel B., Hoelscher C., Dumoutier L., et al. 2015. Interferon-λ and interleukin 22 act synergistically for the induction of interferon-stimulated genes and control of rotavirus infection. Nat. Immunol. 16:698–707. 10.1038/ni.3180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hillyer P., Mane V.P., Schramm L.M., Puig M., Verthelyi D., Chen A., Zhao Z., Navarro M.B., Kirschman K.D., Bykadi S., et al. 2012. Expression profiles of human interferon-alpha and interferon-lambda subtypes are ligand- and cell-dependent. Immunol. Cell Biol. 90:774–783. 10.1038/icb.2011.109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hillyer P., Shepard R., Uehling M., Krenz M., Sheikh F., Thayer K.R., Huang L., Yan L., Panda D., Luongo C., et al. 2018. Differential responses by human respiratory epithelial cell lines to respiratory syncytial virus reflect distinct patterns of infection control. J. Virol. 92:e02202-17 10.1128/JVI.02202-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hong M., Schwerk J., Lim C., Kell A., Jarret A., Pangallo J., Loo Y.-M., Liu S., Hagedorn C.H., Gale M. Jr., and Savan R.. 2016. Interferon lambda 4 expression is suppressed by the host during viral infection. J. Exp. Med. 213:2539–2552. 10.1084/jem.20160437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hou W., Wang X., Ye L., Zhou L., Yang Z.Q., Riedel E., and Ho W.Z.. 2009. Lambda interferon inhibits human immunodeficiency virus type 1 infection of macrophages. J. Virol. 83:3834–3842. 10.1128/JVI.01773-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ingle H., Peterson S.T., and Baldridge M.T.. 2018. Distinct effects of type I and III interferons on enteric viruses. Viruses. 10:46 10.3390/v10010046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ingle H., Lee S., Ai T., Orvedahl A., Rodgers R., Zhao G., Sullender M., Peterson S.T., Locke M., Liu T.-C., et al. 2019. Viral complementation of immunodeficiency confers protection against enteric pathogens via interferon-λ. Nat. Microbiol. 4:1120–1128. 10.1038/s41564-019-0416-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iversen M.B., Ank N., Melchjorsen J., and Paludan S.R.. 2010. Expression of type III interferon (IFN) in the vaginal mucosa is mediated primarily by dendritic cells and displays stronger dependence on NF-kappaB than type I IFNs. J. Virol. 84:4579–4586. 10.1128/JVI.02591-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jagger B.W., Miner J.J., Cao B., Arora N., Smith A.M., Kovacs A., Mysorekar I.U., Coyne C.B., and Diamond M.S.. 2017. Gestational stage and IFN-λ signaling regulate ZIKV infection in utero. Cell Host Microbe. 22:366–376.e3. 10.1016/j.chom.2017.08.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jilg N., Lin W., Hong J., Schaefer E.A., Wolski D., Meixong J., Goto K., Brisac C., Chusri P., Fusco D.N., et al. 2014. Kinetic differences in the induction of interferon stimulated genes by interferon-α and interleukin 28B are altered by infection with hepatitis C virus. Hepatology. 59:1250–1261. 10.1002/hep.26653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johansson C., Wetzel J.D., He J., Mikacenic C., Dermody T.S., and Kelsall B.L.. 2007. Type I interferons produced by hematopoietic cells protect mice against lethal infection by mammalian reovirus. J. Exp. Med. 204:1349–1358. 10.1084/jem.20061587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson H.M., Noon-Song E., and Ahmed C.M.. 2019. Noncanonical IFN signaling, steroids, and STATs: A probable role of V-ATPase. Mediators Inflamm. 2019:4143604 10.1155/2019/4143604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalinowski A., Galen B.T., Ueki I.F., Sun Y., Mulenos A., Osafo-Addo A., Clark B., Joerns J., Liu W., Nadel J.A., et al. 2018. Respiratory syncytial virus activates epidermal growth factor receptor to suppress interferon regulatory factor 1-dependent interferon-lambda and antiviral defense in airway epithelium. Mucosal Immunol. 11:958–967. 10.1038/mi.2017.120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karst S.M., Wobus C.E., Lay M., Davidson J., and Virgin H.W. IV. 2003. STAT1-dependent innate immunity to a Norwalk-like virus. Science. 299:1575–1578. 10.1126/science.1077905 [DOI] [PubMed] [Google Scholar]
- Karst S.M., Wobus C.E., Goodfellow I.G., Green K.Y., and Virgin H.W.. 2014. Advances in Norovirus Biology. Cell Host Microbe. 15(6):668–680. 10.1016/j.chom.2014.05.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly A., Robinson M.W., Roche G., Biron C.A., O’Farrelly C., and Ryan E.J.. 2016. Immune cell profiling of IFN-λ response shows pDCs express highest level of IFN-λR1 and are directly responsive via the JAK-STAT pathway. J. Interferon Cytokine Res. 36:671–680. 10.1089/jir.2015.0169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kernbauer E., Ding Y., and Cadwell K.. 2014. An enteric virus can replace the beneficial function of commensal bacteria. Nature. 516:94–98. 10.1038/nature13960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim H.J., Jo A., Jeon Y.J., An S., Lee K.-M., Yoon S.S., and Choi J.Y.. 2019. Nasal commensal Staphylococcus epidermidis enhances interferon-λ-dependent immunity against influenza virus. Microbiome. 7:80 10.1186/s40168-019-0691-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klinkhammer J., Schnepf D., Ye L., Schwaderlapp M., Gad H.H., Hartmann R., Garcin D., Mahlakõiv T., and Staeheli P.. 2018. IFN-λ prevents influenza virus spread from the upper airways to the lungs and limits virus transmission. eLife. 7:e33354 10.7554/eLife.33354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koltsida O., Hausding M., Stavropoulos A., Koch S., Tzelepis G., Übel C., Kotenko S.V., Sideras P., Lehr H.A., Tepe M., et al. 2011. IL-28A (IFN-λ2) modulates lung DC function to promote Th1 immune skewing and suppress allergic airway disease. EMBO Mol. Med. 3:348–361. 10.1002/emmm.201100142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotenko S.V. 2011. IFN-λs. Curr. Opin. Immunol. 23:583–590. 10.1016/j.coi.2011.07.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotenko S.V., Gallagher G., Baurin V.V., Lewis-Antes A., Shen M., Shah N.K., Langer J.A., Sheikh F., Dickensheets H., and Donnelly R.P.. 2003. IFN-lambdas mediate antiviral protection through a distinct class II cytokine receptor complex. Nat. Immunol. 4:69–77. 10.1038/ni875 [DOI] [PubMed] [Google Scholar]
- Krammer F., Smith G.J.D., Fouchier R.A.M., Peiris M., Kedzierska K., Doherty P.C., Palese P., Shaw M.L., Treanor J., Webster R.G., and García-Sastre A.. 2018. Influenza. Nat. Rev. Dis. Primers. 4:3 10.1038/s41572-018-0002-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazear H.M., Nice T.J., and Diamond M.S.. 2015a. Interferon-λ: Immune Functions at Barrier Surfaces and Beyond. Immunity. 43:15–28. 10.1016/j.immuni.2015.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazear H.M., Daniels B.P., Pinto A.K., Huang A.C., and Vick S.C.. 2015b. Interferon-λ restricts West Nile virus neuroinvasion by tightening the blood-brain barrier. Sci. Transl. Med. 7:284ra59 10.1126/scitranslmed.aaa4304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazear H.M., Schoggins J.W., and Diamond M.S.. 2019. Shared and distinct functions of type I and type III interferons. Immunity. 50:907–923. 10.1016/j.immuni.2019.03.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S., Liu H., Wilen C.B., Sychev Z.E., Desai C., Hykes B.L. Jr., Orchard R.C., McCune B.T., Kim K.-W., Nice T.J., et al. 2019. A secreted viral nonstructural protein determines intestinal norovirus pathogenesis. Cell Host Microbe. 25:845–857.e5. 10.1016/j.chom.2019.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin J.-D., Feng N., Sen A., Balan M., Tseng H.-C., McElrath C., Smirnov S.V., Peng J., Yasukawa L.L., Durbin R.K., et al. 2016. Distinct roles of type I and type III interferons in intestinal immunity to homologous and heterologous rotavirus infections. PLoS Pathog. 12:e1005600 10.1371/journal.ppat.1005600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahlakõiv T., Ritz D., Mordstein M., DeDiego M.L., Enjuanes L., Müller M.A., Drosten C., and Staeheli P.. 2012. Combined action of type I and type III interferon restricts initial replication of severe acute respiratory syndrome coronavirus in the lung but fails to inhibit systemic virus spread. J. Gen. Virol. 93:2601–2605. 10.1099/vir.0.046284-0 [DOI] [PubMed] [Google Scholar]
- Mahlakõiv T., Hernandez P., Gronke K., Diefenbach A., and Staeheli P.. 2015. Leukocyte-derived IFN-α/β and epithelial IFN-λ constitute a compartmentalized mucosal defense system that restricts enteric virus infections. PLoS Pathog. 11:e1004782 10.1371/journal.ppat.1004782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcello T., Grakoui A., Barba-Spaeth G., Machlin E.S., Kotenko S.V., MacDonald M.R., and Rice C.M.. 2006. Interferons α and λ inhibit hepatitis C virus replication with distinct signal transduction and gene regulation kinetics. Gastroenterology. 131:1887–1898. 10.1053/j.gastro.2006.09.052 [DOI] [PubMed] [Google Scholar]
- Marukian S., Andrus L., Sheahan T.P., Jones C.T., Charles E.D., Ploss A., Rice C.M., and Dustin L.B.. 2011. Hepatitis C virus induces interferon-λ and interferon-stimulated genes in primary liver cultures. Hepatology. 54:1913–1923. 10.1002/hep.24580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mordstein M., Neugebauer E., Ditt V., Jessen B., Rieger T., Falcone V., Sorgeloos F., Ehl S., Mayer D., Kochs G., et al. 2010. Lambda interferon renders epithelial cells of the respiratory and gastrointestinal tracts resistant to viral infections. J. Virol. 84:5670–5677. 10.1128/JVI.00272-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muir A.J., Shiffman M.L., Zaman A., Yoffe B., de la Torre A., Flamm S., Gordon S.C., Marotta P., Vierling J.M., Lopez-Talavera J.C., et al. 2010. Phase 1b study of pegylated interferon lambda 1 with or without ribavirin in patients with chronic genotype 1 hepatitis C virus infection. Hepatology. 52:822–832. 10.1002/hep.23743 [DOI] [PubMed] [Google Scholar]
- Muir A.J., Arora S., Everson G., Flisiak R., George J., Ghalib R., Gordon S.C., Gray T., Greenbloom S., Hassanein T., et al. EMERGE study group . 2014. A randomized phase 2b study of peginterferon lambda-1a for the treatment of chronic HCV infection. J. Hepatol. 61:1238–1246. 10.1016/j.jhep.2014.07.022 [DOI] [PubMed] [Google Scholar]
- Nice T.J., Strong D.W., McCune B.T., Pohl C.S., and Virgin H.W.. 2013. A single-amino-acid change in murine norovirus NS1/2 is sufficient for colonic tropism and persistence. J. Virol. 87:327–334. 10.1128/JVI.01864-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nice T.J., Baldridge M.T., McCune B.T., Norman J.M., Lazear H.M., Artyomov M., Diamond M.S., and Virgin H.W.. 2015. Interferon-λ cures persistent murine norovirus infection in the absence of adaptive immunity. Science. 347:269–273. 10.1126/science.1258100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nice T.J., Osborne L.C., Tomov V.T., Artis D., Wherry E.J., and Virgin H.W.. 2016. Type I interferon receptor deficiency in dendritic cells facilitates systemic murine norovirus persistence despite enhanced adaptive immunity. PLoS Pathog. 12:e1005684 10.1371/journal.ppat.1005684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nice T.J., Robinson B.A., and Van Winkle J.A.. 2018. The role of interferon in persistent viral infection: insights from murine norovirus. Trends Microbiol. 26:510–524. 10.1016/j.tim.2017.10.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norman J.M., Handley S.A., Baldridge M.T., Droit L., Liu C.Y., Keller B.C., Kambal A., Monaco C.L., Zhao G., Fleshner P., et al. 2015. Disease-specific alterations in the enteric virome in inflammatory bowel disease. Cell. 160:447–460. 10.1016/j.cell.2015.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Odendall C., and Kagan J.C.. 2015. The unique regulation and functions of type III interferons in antiviral immunity. Curr. Opin. Virol. 12:47–52. 10.1016/j.coviro.2015.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Odendall C., Dixit E., Stavru F., Bierne H., Franz K.M., Durbin A.F., Boulant S., Gehrke L., Cossart P., and Kagan J.C.. 2014. Diverse intracellular pathogens activate type III interferon expression from peroxisomes. Nat. Immunol. 15:717–726. 10.1038/ni.2915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Odendall C., Voak A.A., and Kagan J.C.. 2017. Type III IFNs are commonly induced by bacteria-sensing TLRs and reinforce epithelial barriers during infection. J. Immunol. 199:3270–3279. 10.4049/jimmunol.1700250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okabayashi T., Kojima T., Masaki T., Yokota S., Imaizumi T., Tsutsumi H., Himi T., Fujii N., and Sawada N.. 2011. Type-III interferon, not type-I, is the predominant interferon induced by respiratory viruses in nasal epithelial cells. Virus Res. 160:360–366. 10.1016/j.virusres.2011.07.011 [DOI] [PubMed] [Google Scholar]
- Onabajo O.O., Muchmore B., and Prokunina-Olsson L.. 2019. The IFN-λ4 conundrum: When a good interferon goes bad. J. Interferon Cytokine Res. 39:636–641. 10.1089/jir.2019.0044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pagliaccetti N.E., and Robek M.D.. 2010. Interferon-λ in the immune response to hepatitis B virus and hepatitis C virus. J. Interferon Cytokine Res. 30:585–590. 10.1089/jir.2010.0060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park H., Serti E., Eke O., Muchmore B., Prokunina-Olsson L., Capone S., Folgori A., and Rehermann B.. 2012. IL-29 is the dominant type III interferon produced by hepatocytes during acute hepatitis C virus infection. Hepatology. 56:2060–2070. 10.1002/hep.25897 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker D. 2017. Impact of type I and III interferons on respiratory superinfections due to multidrug-resistant pathogens. J. Infect. Dis. 215(suppl_1):S58–S63. 10.1093/infdis/jiw466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pervolaraki K., Stanifer M.L., Münchau S., Renn L.A., Albrecht D., Kurzhals S., Senís E., Grimm D., Schröder-Braunstein J., Rabin R.L., and Boulant S.. 2017. Type I and Type III interferons display different dependency on mitogen-activated protein kinases to mount an antiviral state in the human gut. Front. Immunol. 8:459 10.3389/fimmu.2017.00459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pervolaraki K., Rastgou Talemi S., Albrecht D., Bormann F., Bamford C., Mendoza J.L., Garcia K.C., McLauchlan J., Höfer T., Stanifer M.L., and Boulant S.. 2018. Differential induction of interferon stimulated genes between type I and type III interferons is independent of interferon receptor abundance. PLoS Pathog. 14:e1007420 10.1371/journal.ppat.1007420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pervolaraki K., Guo C., Albrecht D., Boulant S., and Stanifer M.L.. 2019. Type-specific crosstalk modulates interferon signaling in intestinal epithelial cells. J. Interferon Cytokine Res. 39:650–660. https://doi.org/ 10.1089/jir.2019.0040 [DOI] [PubMed] [Google Scholar]
- Pierangeli A., Statzu M., Nenna R., Santinelli L., Petrarca L., Frassanito A., Gentile M., Antonelli G., Midulla F., and Scagnolari C.. 2018. Interferon lambda receptor 1 (IFNL1R) transcript is highly expressed in rhinovirus bronchiolitis and correlates with disease severity. J. Clin. Virol. 102:101–109. 10.1016/j.jcv.2018.03.003 [DOI] [PubMed] [Google Scholar]
- Pires S., and Parker D.. 2018. IL-1β activation in response to Staphylococcus aureus lung infection requires inflammasome-dependent and independent mechanisms. Eur. J. Immunol. 48:1707–1716. 10.1002/eji.201847556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Planet P.J., Parker D., Cohen T.S., Smith H., Leon J.D., Ryan C., Hammer T.J., Fierer N., Chen E.I., and Prince A.S.. 2016. Lambda interferon restructures the nasal microbiome and increases susceptibility to Staphylococcus aureus superinfection. MBio. 7:e01939–e15. 10.1128/mBio.01939-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pott J., Mahlakõiv T., Mordstein M., Duerr C.U., Michiels T., Stockinger S., Staeheli P., and Hornef M.W.. 2011. IFN-lambda determines the intestinal epithelial antiviral host defense. Proc. Natl. Acad. Sci. USA. 108:7944–7949. 10.1073/pnas.1100552108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rauch I., Rosebrock F., Hainzl E., Heider S., Majoros A., Wienerroither S., Strobl B., Stockinger S., Kenner L., Müller M., and Decker T.. 2015. Noncanonical effects of IRF9 in intestinal inflammation: more than type I and type III interferons. Mol. Cell. Biol. 35:2332–2343. 10.1128/MCB.01498-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rich H.E., McCourt C.C., Zheng W.Q., McHugh K.J., Robinson K.M., Wang J., and Alcorn J.F.. 2019. Interferon lambda inhibits bacterial uptake during influenza superinfection. Infect. Immun. 87:e00114-19 10.1128/IAI.00114-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robek M.D., Boyd B.S., and Chisari F.V.. 2005. Lambda interferon inhibits hepatitis B and C virus replication. J. Virol. 79:3851–3854. 10.1128/JVI.79.6.3851-3854.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robilotti E., Deresinski S., and Pinsky B.A.. 2015. Norovirus. Clin. Microbiol. Rev. 28:134–164. 10.1128/cmr.00075-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saxena K., Simon L.M., Zeng X.-L., Blutt S.E., Crawford S.E., Sastri N.P., Karandikar U.C., Ajami N.J., Zachos N.C., Kovbasnjuk O., et al. 2017. A paradox of transcriptional and functional innate interferon responses of human intestinal enteroids to enteric virus infection. Proc. Natl. Acad. Sci. USA. 114:E570–E579. 10.1073/pnas.1615422114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selvaggi C., Pierangeli A., Fabiani M., Spano L., and Nicolai A.. 2014. Interferon lambda 1–3 expression in infants hospitalized for RSV or HRV associated bronchiolitis. J. Infect. 68:467–477. 10.1016/j.jinf.2013.12.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheppard P., Kindsvogel W., Xu W., Henderson K., Schlutsmeyer S., Whitmore T.E., Kuestner R., Garrigues U., Birks C., Roraback J., et al. 2003. IL-28, IL-29 and their class II cytokine receptor IL-28R. Nat. Immunol. 4:63–68. 10.1038/ni873 [DOI] [PubMed] [Google Scholar]
- Sommereyns C., Paul S., Staeheli P., and Michiels T.. 2008. IFN-lambda (IFN-lambda) is expressed in a tissue-dependent fashion and primarily acts on epithelial cells in vivo. PLoS Pathog. 4:e1000017 10.1371/journal.ppat.1000017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stetson D.B., and Medzhitov R.. 2006. Type I interferons in host defense. Immunity. 25:373–381. 10.1016/j.immuni.2006.08.007 [DOI] [PubMed] [Google Scholar]
- Strong D.W., Thackray L.B., Smith T.J., and Virgin H.W.. 2012. Protruding domain of capsid protein is necessary and sufficient to determine murine norovirus replication and pathogenesis in vivo. J. Virol. 86:2950–2958. 10.1128/JVI.07038-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subramaniam P.S., Torres B.A., and Johnson H.M.. 2001. So many ligands, so few transcription factors: a new paradigm for signaling through the STAT transcription factors. Cytokine. 15:175–187. 10.1006/cyto.2001.0905 [DOI] [PubMed] [Google Scholar]
- Swider A., Siegel R., Eskdale J., and Gallagher G.. 2014. Regulation of interferon lambda-1 (IFNL1/IFN-λ1/IL-29) expression in human colon epithelial cells. Cytokine. 65:17–23. 10.1016/j.cyto.2013.09.020 [DOI] [PubMed] [Google Scholar]
- Thackray L.B., Wobus C.E., Chachu K.A., Liu B., Alegre E.R., Henderson K.S., Kelley S.T., and Virgin H.W. IV. 2007. Murine noroviruses comprising a single genogroup exhibit biological diversity despite limited sequence divergence. J. Virol. 81:10460–10473. 10.1128/JVI.00783-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas E., Gonzalez V.D., Li Q., Modi A.A., Chen W., Noureddin M., Rotman Y., and Liang T.J.. 2012. HCV infection induces a unique hepatic innate immune response associated with robust production of type III interferons. Gastroenterology. 142:978–988. 10.1053/j.gastro.2011.12.055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trinchieri G. 2010. Type I interferon: friend or foe? J. Exp. Med. 207:2053–2063. 10.1084/jem.20101664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Woensel J.B., van Aalderen W.M., and Kimpen J.L.. 2003. Viral lower respiratory tract infection in infants and young children. BMJ. 327:36–40. 10.1136/bmj.327.7405.36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Virgin H.W. 2014. The virome in mammalian physiology and disease. Cell. 157:142–150. 10.1016/j.cell.2014.02.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wack A., Terczyńska-Dyla E., and Hartmann R.. 2015. Guarding the frontiers: the biology of type III interferons. Nat. Immunol. 16:802–809. 10.1038/ni.3212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y., Li T., Chen Y., Wei H., Sun R., and Tian Z.. 2017b Involvement of NK cells in IL-28B–mediated immunity against influenza virus infection. J. Immunol. 199:1012–1020. 10.4049/jimmunol.1601430 [DOI] [PubMed] [Google Scholar]
- Wilen C.B., Lee S., Hsieh L.L., Orchard R.C., Desai C., Hykes B.L. Jr., McAllaster M.R., Balce D.R., Feehley T., Brestoff J.R., et al. 2018. Tropism for tuft cells determines immune promotion of norovirus pathogenesis. Science. 360:204–208. 10.1126/science.aar3799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witte K., Gruetz G., Volk H.-D., Looman A.C., Asadullah K., Sterry W., Sabat R., and Wolk K.. 2009. Despite IFN-λ receptor expression, blood immune cells, but not keratinocytes or melanocytes, have an impaired response to type III interferons: implications for therapeutic applications of these cytokines. Genes Immun. 10:702–714. 10.1038/gene.2009.72 [DOI] [PubMed] [Google Scholar]
- Yang J.-Y., Kim M.-S., Kim E., Cheon J.H., Lee Y.-S., Kim Y., Lee S.-H., Seo S.-U., Shin S.-H., Choi S.S., et al. 2016. Enteric viruses ameliorate gut inflammation via Toll-like receptor 3 and Toll-like receptor 7-mediated interferon-β production. Immunity. 44:889–900. 10.1016/j.immuni.2016.03.009 [DOI] [PubMed] [Google Scholar]
- Ye L., Ohnemus A., Ong L.C., Gad H.H., Hartmann R., Lycke N., and Staeheli P.. 2019a Type I and type III interferons differ in their adjuvant activities for influenza vaccines. J. Virol. 93:e01262-19 10.1128/JVI.01262-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ye L., Schnepf D., Becker J., Ebert K., Tanriver Y., Bernasconi V., Gad H.H., Hartmann R., Lycke N., and Staeheli P.. 2019b Interferon-λ enhances adaptive mucosal immunity by boosting release of thymic stromal lymphopoietin. Nat. Immunol. 20:593–601. 10.1038/s41590-019-0345-x [DOI] [PubMed] [Google Scholar]
- Ye L., Schnepf D., and Staeheli P.. 2019c Interferon-λ orchestrates innate and adaptive mucosal immune responses. Nat. Rev. Immunol. 19:614–625. 10.1038/s41577-019-0182-z [DOI] [PubMed] [Google Scholar]
- Zanoni I., Granucci F., and Broggi A.. 2017. Interferon (IFN)-λ takes the helm: immunomodulatory roles of type III IFNs. Front. Immunol. 8:1661 10.3389/fimmu.2017.01661 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou Z., Hamming O.J., Ank N., and Nielsen A.L.. 2007. Type III Interferon (IFN) Induces a Type I IFN-Like Response in a Restricted Subset of Cells through Signaling Pathways Involving both the Jak-STAT Pathway and the Mitogen-Activated Protein Kinases. J. Virol. 81:7749–7758. 10.1128/jvi.02438-06 [DOI] [PMC free article] [PubMed] [Google Scholar]