Abstract
Background:
The acute effects of aerobic exercise on improved mood and anxiety reduction have been demonstrated across clinical and nonclinical populations. Limited work has evaluated the acute effects of aerobic exercise on negative affect, obsessions, and compulsions in patients with Obsessive Compulsive Disorder (OCD).
Method:
Fifty-five patients (64% female) with treatment-resistant OCD were randomized to either 12 weeks of aerobic exercise (AE) or health education contact (HEC) control. Participants rated negative affect (i.e., mood and anxiety), obsessions and compulsions before and after each weekly AE or HEC session. Multilevel models were constructed to evaluate the effect of intervention condition, treatment week (time), and their interaction term in terms of acute change in affect, obsession, and compulsions.
Results:
Results reflected a main effect of condition, such that AE resulted in significantly larger increases in positive mood, and reductions in anxiety and compulsions, as compared to HEC. There was also a main effect of time in predicting acute anxiety reduction, such that linear reductions in anxiety over the course of treatment were observed. No significant effects were observed for acute changes in obsessions.
Limitations:
The sample was small and was limited in demographic heterogeneity. Bouts of aerobic exercise were not standardized in terms of duration and mode, which could impact affective response to exercise, and acute affective OCD effects were exclusively self-reported.
Discussion:
The current findings may help elucidate potential mechanisms of action of exercise on OCD outcomes. In addition, these results point toward the potential of designing exercise interventions that can teach patients to utilize individual bouts of physical activity, “in-the-moment” to improve mood and reduce anxiety and compulsions.
Keywords: OCD, physical inactivity, acute effects, BMI, exercise, anxiety
Introduction
Obsessive-compulsive disorder (OCD) is a chronic psychiatric illness characterized by intrusive thoughts, images or impulses that produce anxiety and distress (obsessions) and persistent mental or behavioral attempts to reduce distress (compulsions) (APA, 2013). OCD is associated with significant psychosocial and functional impairment (Macy et al., 2013; Vikas et al., 2011), leading to substantial societal burden (Eaton et al., 2008). Despite existing behavioral and pharmacological interventions for OCD, many patients continue to experience clinically significant levels of symptomatology (Atmaca, 2015; Fineberg et al., 2013; Olatunji et al., 2013). Therefore, novel augmentation treatments are of increased interest including brain stimulation (Narayanaswamy et al., 2015) and pharmacotherapy (Simpson et al., 2013). One promising approach in reducing OCD symptomatology is aerobic exercise (Abrantes et al., 2017b; Brown et al., 2007; Lancer et al., 2007; Rector et al., 2015). In a randomized clinical trial, we tested the efficacy of a 12-week aerobic exercise intervention versus a health education contact control for augmenting cognitive-behavioral therapy for OCD (Abrantes et al., 2017b). While both conditions were associated with lower OCD severity, patients in the exercise condition demonstrated a trend toward higher rates of treatment response, defined by 35% reduction in OCD symptoms.
A number of mechanisms have been proposed for why aerobic exercise may lead to reduced OCD symptoms (Abrantes et al., 2012), including affective processes and their impact on OCD severity. There is a large body of literature on the acute effects of exercise for improving positive affect and decreasing negative affect (Basso and Suzuki, 2017; Cheval et al., 2018; Ensari et al., 2015; Reed and Buck, 2009). Indeed, acute decreases in negative affect and increases in positive affect may help attenuate OCD symptom severity via increased approach behavior and decreased avoidance behavior (i.e., exposure) (McKay et al., 2015). Alternatively, bouts of exercise may also, more directly, decrease obsessive thoughts and/or the urge to engage in compulsive behaviors. Only one prior study examined the acute effects of exercise on OCD symptom severity in patients with OCD (Abrantes et al., 2009). In that open trial of 15 patients with OCD who despite adequate treatment were still experiencing high levels of OCD symptomatology, significant acute improvements in negative affect (i.e., mood and anxiety), obsessions, and compulsions were observed following each bout of moderate-intensity aerobic exercise over the course of an exercise intervention (Abrantes et al., 2009). Further, the magnitude of the effect of exercise on acute changes in negative affect remained stable over the course of a 12-week intervention. While these findings are promising in elucidating mechanistic factors related to exercise’s impact on OCD, this prior study was limited by the small sample size and lack of control group.
Indeed, it is possible that the acute effects of exercise may result in a cumulative effect over time on OCD outcomes. Though much of the acute effects of exercise literature have focused on single-session, experimental studies, several exercise intervention studies have examined acute effects at weekly sessions and show support (Brown et al., 2016) and lack of support (Williams et al., 2011) for the potential cumulative effect of acute changes on long-term benefits. However, to date, no study has examined the potential relationship between acute effects aggregating over time to result in improved outcomes in patients with OCD engaged in an exercise intervention.
The purpose of the current study was to extend this line of research by evaluating the acute effects of aerobic exercise compared to a control condition on negative affect, obsessions and compulsions. We conducted a secondary data analysis of our randomized controlled trial in which patients with OCD were assigned to aerobic exercise or health education. It was hypothesized that aerobic exercise, relative to a control condition, would result in acute improvements in negative affect (better mood, lower anxiety), and lower obsessions and compulsions before and after each session over the course of a 12-week intervention. These effects were expected after adjusting for relevant covarying factors, including baseline anxiety and depressive symptoms and body mass index. Further, we also examined whether there were cumulative effects of the intervention on pre-session scores of negative affect, obsessions, and compulsions.
Method
Participants
Participants (N = 56) were recruited for a randomized controlled trial testing the efficacy of a 12-week aerobic exercise (AE, n = 28) intervention relative to a health-education control (HEC, n = 28) group for the treatment of OCD. One participant randomized to HEC did not start treatment, thus a total of 55 cases were utilized in analyses. Design details, intervention descriptions, and participants characteristics have been published elsewhere (Abrantes et al., 2017b). In brief, participants currently receiving OCD treatment but with a Yale-Brown Obsessive Compulsive Scale (Goodman et al., 1989b) scores ≥ 16 who were physically inactive (less than 60 minutes of aerobic exercise per week in the last 3 months) were eligible to participate.
Procedures
All protocol procedures were approved by the Institutional Review Board where the study took place. Participants randomized to AE attended 12 weekly exercise sessions, supervised by an exercise physiologist. Exercise consisted of moderate-intensity aerobic exercise using standard exercise modalities (e.g., treadmills, ellipticals). Sessions started at 20 minutes in duration (including a 5 minute warm-up) in the early weeks of the program leading up to 35–40 minute sessions by 12 weeks. Participants were also instructed to exercise on their own between two and four days during the week (increasing from two days/week early in the intervention to four days/week later in the intervention period). By the last several weeks of the intervention, participants were given the goal of attaining a minimum of 150 minutes of moderate-intensity aerobic exercise per week. Prior to each exercise session, participants engaged in a 20-minute discussion session with a research staff member on topics related to increasing physical activity (e.g., time-management, motivation, goal-setting). Participants in the HEC condition received 12 weekly 45–60 minute long psychoeducation sessions. Sample topics included nutrition, sleep hygiene, caffeine, alcohol, cigarette smoking, and coordinating your medical treatment. Participants in the HEC and AE conditions were equated for time and incentives.
Measures
Baseline Assessment.
The Yale-Brown Obsessive Compulsive Scale (Y-BOCS), a clinician-administered 10-item scale, was used to assess severity of OCD symptoms (Goodman et al., 1989a, 1989b). Depression symptoms were assessed with the Beck Depression Inventory-II (BDI-II), a well-validated 21-item self-report assessment (Beck et al., 1996; Dozois et al., 1998; Steer et al., 1997). Anxiety symptoms were assessed with the Beck Anxiety Inventory (BAI), which is a well-validated 21-item self-report assessment of cognitive and somatic aspects of anxiety. Body mass index (BMI) was calculated based on measured weight and height during the baseline assessment ([weight(lbs)/[height (in)]2 × 703]) (World Health Organization, 2002)
Acute Symptoms Self-Rating Scale.
The National Institute of Mental Health Self-Rating Scale (NIMH-SR) has been used to capture acute changes in negative affect (mood and anxiety), obsessions, and compulsions as a function of aerobic exercise in previous studies (Abrantes et al., 2009; Brown et al., 2016). At every AE and HEC intervention visit, participants were asked to rate, on a 10-point Likert scale their current level for each of the following: mood (0 = Feel worst ever to 10 = Feel best ever), anxiety (0 = No anxiety to 10 = Extreme anxiety), and obsessions and compulsions (0 = None to 10 = Constant) just prior to and again immediately following either the AE or HEC session. Lower ratings on the mood item and higher ratings on the anxiety item reflect negative affect.
Statistical Analyses
Analytic Models.
Analyses were conducted using Stata Software (version 14). Two sets of multi-level models were constructed. Primary analyses including four multilevel models were constructed predicting post-session mood, anxiety, obsessions, and compulsions. In order to examine changes in negative affect, obsessions and compulsions before and after each weekly intervention session, pre-session ratings were entered in the corresponding model. Thus, the model coefficients can be interpreted as the degree of change from pre-post session. The second set tested the cumulative effects of treamtment over time on pre-session mood, anxiety, obsessions, and compulsions. Four multilevel models were constructed predicting pre-session mood, anxiety, obsessions, and compulsions. In all models, treatment condition (0=HEC, 1=AE), time, and the interaction term was entered. Time was mean-centered. We provide effect size estimates, based on Feingold (2013).
Model Assumptions.
Analyses utilize maximum likelihood approaches to produce estimates of the regression parameters, which uses all available data without requiring imputation of missing values. Missingness included 19.7% of pre-session ratings and 20.3% of post-session ratings were missing. The intraclass correlation (ICC) values for all outcomes in the first set of models (i.e., post-session ratings) were above the conservative recommended value of .10, and were as follows: Post-Mood (ICC = .53, 95%CI = .42–.63); Post-Anxiety (ICC = .64, 95%CI = .54–.73); Post-Obsessions (ICC = .67, 95%CI = .58–.76); Post-Compulsions (ICC = .70, 95%CI = .61–.78). The intraclass correlation (ICC) values for outcomes in the second set of models (i.e., pre-session ratings) were acceptable: Pre-Mood (ICC = .33, 95%CI = .23–.44); Pre-Anxiety (ICC = .59, 95%CI = .49–.69); Pre-Obsessions (ICC = .60, 95%CI = .50–.70); Pre-Compulsions (ICC = .66, 95%CI = .56–.75). Linear, quadratic, cubic and hyperbolic effects of time were modeled, and model fit was examined using Akaike information criterion (AIC) and the Bayesian information criterion (BIC); linear models were fit to the data. Random intercepts and slopes were included in all models. Huber/White/Sandwich robust standard errors were estimated in order to adjust for heteroskedasticity in the error terms, and an unstructured covariance matrix was specified to allow for each covariance to be uniquely estimated.
Model Covariates.
Based on documented baseline differences between groups on the Y-BOCS, BDI, and BAI (Abrantes et al., 2017b) these baseline scores were entered as covariates. As reported in parent trial, concurrent behavioral and pharmacological treatment for OCD did not differ between conditions and was not included as covariate in this study. Given the theoretical relevance of weight status on acute affective response to exercise, BMI was also entered as a covariate in all models (Ekkekakis and Lind, 2006). The variance inflation factor (VIF) was computed between model covariate (YBOCS, BDI, BAI, BMI) with average scores on each of the primary predictors (pre-session mood, anxiety, obsessions, and compulsions) as a test of multicollinearity. All VIFs were all below recommended values of 2.5, and were as follows: Mood (VIFs = 1.13–1.19); Anxiety (VIFs = 1.12–1.19); Obsessions (VIFs = 1.12–1.18); Compulsions (VIFs = 1.11–1.18).
Results
Descriptive Overview
Participants (n = 55, 64.6% female, Mage = 38.9, SD = 13.1) were primarily Caucasian (83.9%), employed (63.6%), and 60.7% had completed college. At baseline, participants had moderately severe symptoms based on average Y-BOCS scores (M = 24.9, SD = 5.26). Average BMI was in the obese range (M = 30.3, SD = 7.4). Of the 12-weekly AE or HEC group sessions, participants completed an average of 10.0 sessions (SD = 2.3).
Acute Changes in Negative Affect, Obsessions, and Compulsions
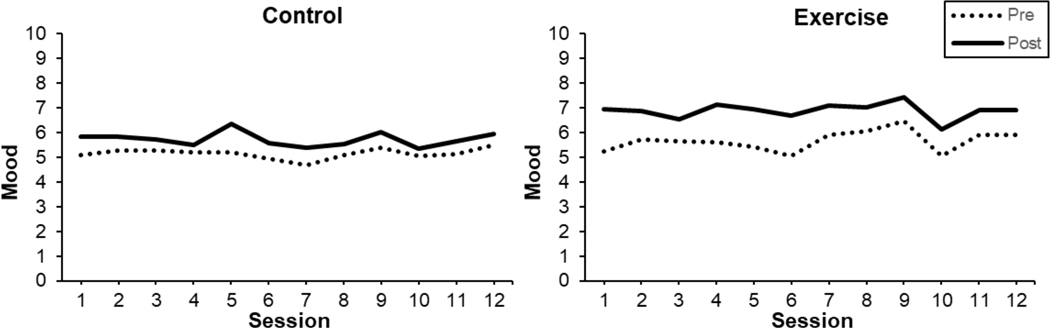
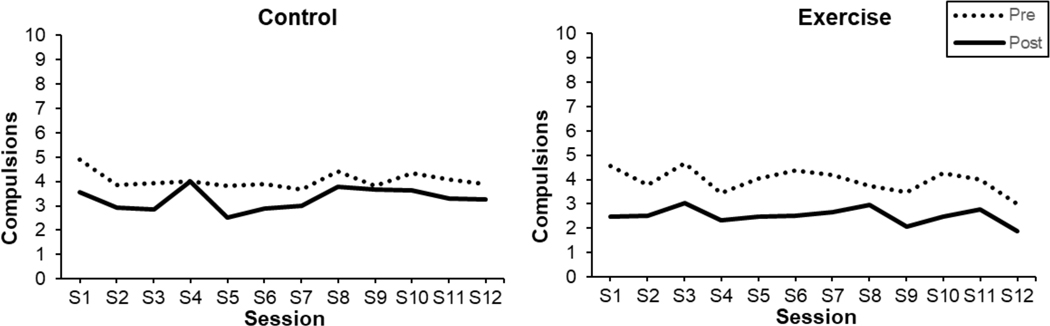
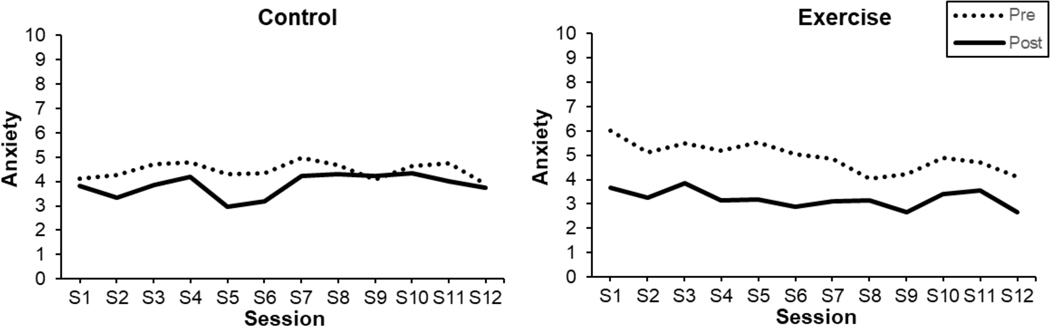
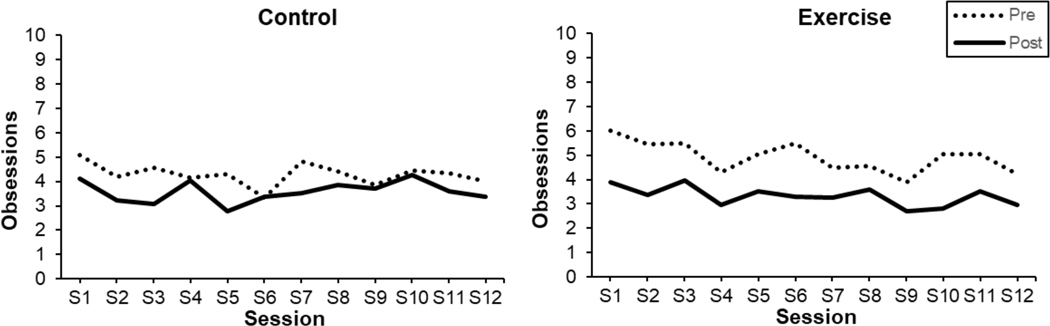
See Table 1 for summarized results of multilevel models, and Figures 1–4 for visualization of mean mood, anxiety, obsession and compulsions, by treatment condition, over the course of treatment. The covariate effects were non-significant in all models.
Table 1.
Effect of intervention on acute changes in affect, obsessions, and compulsions before to after treatment sessions
| b | se | z | CI | p | |
|---|---|---|---|---|---|
| Mood (after session) | |||||
| Mood before session | 0.543 | 0.030 | 18.18 | 0.484, 0.601 | < .0001 |
| Time | −0.015 | 0.018 | −0.81 | −0.050, 0.021 | .415 |
| Treatment Condition | 0.907 | 0.223 | 4.07 | 0.470, 1.344 | < .0001 |
| Time x Treatment | −0.007 | 0.025 | −0.29 | −0.066, 0.042 | .775 |
| Anxiety (after session) | |||||
| Anxiety before session | 0.420 | 0.031 | 13.29 | 0.358, 0.482 | < .0001 |
| Time | 0.040 | 0.020 | 1.96 | −0.001, 0.080 | .050 |
| Treatment Condition | −0.969 | 0.294 | −3.29 | −1.546, −0.392 | .001 |
| Time x Treatment | −0.046 | 0.029 | −1.60 | −0.102, 0.010 | .110 |
| Obsessions (after session) | |||||
| Obsessions before session | −0.490 | 0.035 | 14.08 | 0.421, 0.557 | < .0001 |
| Time | 0.025 | 0.024 | 1.05 | −0.022, 0.072 | .293 |
| Treatment Condition | −0.549 | 0.342 | −1.61 | −1.220, 0.121 | .108 |
| Time x Treatment | −0.029 | 0.033 | −0.86 | −0.094, 0.036 | .389 |
| Compulsions (after session) | |||||
| Compulsions before session | 0.487 | 0.032 | 15.17 | 0.424, 0.550 | < .0001 |
| Time | 0.019 | 0.022 | 0.86 | −0.025, 0.063 | .392 |
| Treatment Condition | −0.763 | 0.309 | −2.47 | −1.348, −0.158 | .014 |
| Time x Treatment | −0.008 | 0.031 | −0.27 | −0.069, 0.053 | .789 |
Note: Level-1 variables (mood, anxiety, and obsessions, compulsions, time [treatment week]); level-2 variables (condition [0=Control, 1=Exercise], pre-session rating, covariates, not displayed).
Figure 1.
Acute Changes in Pre- and Post-Session Mood
Figure 4.
Acute Changes in Pre- and Post-Session Compulsions
Mood.
There was a significant main effect of treatment condition (p < .001), such that improvement in mood was significantly larger following AE relative to HEC sessions. The main effect of time and interaction of condition x time were non-significant.
Anxiety.
There was a significant main effect of treatment condition (p = .001), indicating significantly larger reductions in anxiety after AE relative to HEC sessions. There was a main effect of time (p = .050), reflecting linear reductions in post-session anxiety over the course of treatment. The condition x time interaction was non-significant.
Obsessions.
No differences in acute changes in obsessions across treatment, time, or their interaction were observed.
Compulsions.
There was a significant main effect of treatment (p = .014), such that AE sessions, relative to HEC, resulted in significantly larger reductions in compulsions. The main effect of time and the interaction of condition x time were non-significant.
Longitudinal Changes in Pre-Session Negative Affect, Obsessions, and Compulsions
Results are presented in Table 2 and patterning of effects is illustrated in Figures 1–4.
Table 2.
Effect of intervention on changes in pre-session affect, obsessions, and compulsions over the course of the treatment
| b | se | z | CI | p | |
|---|---|---|---|---|---|
| Mood (before session) | |||||
| Time | 0.017 | 0.033 | 0.052 | −0.047, 0.081 | .605 |
| Treatment Condition | 0.852 | 0.269 | 3.17 | 0.326, 1.379 | .002 |
| Time x Treatment | 0.024 | 0.046 | 0.53 | −0.065, 0.114 | .594 |
| Anxiety (before session) | |||||
| Time | −0.011 | 0.034 | −0.33 | −0.077, 0.055 | .740 |
| Treatment Condition | 0.141 | 0.475 | 0.30 | −0.789, 1.072 | .766 |
| Time x Treatment | −0.116 | 0.047 | −2.47 | −0.207, −0.024 | .014 |
| Obsessions (before session) | |||||
| Time | −0.068 | 0.034 | −2.01 | −0.134, −0.002 | .044 |
| Treatment Condition | 0.306 | 0.481 | 0.64 | −0.637, 1.249 | .525 |
| Time x Treatment | −0.015 | 0.047 | −0.31 | −0.107, 0.078 | .756 |
| Compulsions (before session) | |||||
| Time | −0.053 | 0.033 | −1.60 | −0.119, 0.012 | .110 |
| Treatment Condition | −0.380 | 0.518 | −0.73 | −1.395, 0.635 | .463 |
| Time x Treatment | −0.005 | 0.047 | −0.11 | −0.096, 0.086 | .913 |
Note: Level-1 variables (mood, anxiety, and obsessions, compulsions, time [treatment week]); level-2 variables (condition [0=Control, 1=Exercise], covariates, not displayed).
Mood.
There were no significant changes in pre-session mood during the course of treatment. There was a significant main effect of treatment condition (p = .002), reflecting significantly greater positive pre-session mood in the AE condition relative to HEC. The interaction of condition x time was non-significant.
Anxiety.
There were no significant changes in pre-session anxiety during the course of treatment. There was also a non-significant main effect of treatment condition. However, there was a significant interaction of condition x time (p = .014), such that reductions in pre-session anxiety emerged throughout the course of treatment in the AE but not HEC condition.
Obsessions.
There was a significant reduction in pre-session obsessions during the course of treatment (p = .044). The main effect of treatment condition and the interaction term were non-significant.
Compulsions.
There were no significant changes in pre-session compulsions during the course of treatment. The main effect of treatment condition and the interaction term were non-significant.
Discussion
Findings provide novel evidence for the acute effects of aerobic exercise on reductions in negative affect (i.e., better mood, lower anxiety) and compulsions relative to an active control condition in patients with treatment resistant OCD. Findings indicate that aerobic exercise (but not control) uniquely produced cumulative anxiolytic effects over the course of the 12-week intervention. These results are the first to stem from a well-designed study that included a control condition and larger sample of patients with OCD than in prior work.
On average, patients in both treatment conditions reported lower levels of obsessions over the course of the 12-week intervention immediately before intervention sessions, suggesting a potential cumulative effect of any active intervention on decreased obsessions. Due to the active control condition, it is possible that the participants in this study found the health information in this condition and/or the social support received by attending weekly sessions with a research interventionist helpful such that obsessions decreased. Interestingly, pre-session compulsions did not decrease over time though an acute effect was observed with exercise. It is possible that the acute effects of exercise may have lasted longer for obsessions, relative to compulsions, such that a cumulative effect over time was observed. Future research that examines how long acute effects last post exercise sessions will aid in the understanding of these findings.
The findings of this study have several notable clinical implications. For example, vulnerabilities underlying OCD include the tendency to experience heightened negative affect (Bienvenu et al., 2004), and lower levels of positive affect (Spinella, 2005) and poor regulation of these affective states. These, in turn, influence the motivational processes of behavioral activation and behavioral inhibition (Carver and White, 1994), leading to more severe symptomatology (McGuire et al., 2012). Therefore, it may be possible to teach patients with OCD to use bouts of aerobic exercise to manage affective states “in-the-moment”. Interestingly, given that the urge to engage in compulsions also decreases acutely after a bout of exercise, patients with OCD may benefit from the strategic use of exercise to manage or override urges for compulsions. Such an approach has been utilized successfully with individuals with compulsive substance use behaviors who have been instructed to use bouts of aerobic exercise to manage negative affect as well as cravings (Abrantes et al., 2017a; Linke et al., 2012). As such, aerobic exercise may be a tangible, easily implementable strategy that patients can use to regulate affect and OCD symptoms. Future studies are needed to empirically test whether aerobic exercise, if efficacious and effectively implemented, can enhance patients’ ability to resist compulsions.
While the current findings are promising, a number of additional factors related to developing more effective exercise prescription for patients with OCD are worth considering. First, the bouts of exercise in this study were at least 20 minutes in duration. Yet, it is possible that shorter duration bouts may produce comparable effects based on evidence in other related literatures. For example, even a 5-minute bout of activity resulted in reduced depressive affect and improved mood on the Profile of Mood States (POMS) among a sample of young adults (Jaffery et al., 2017). Second, the aerobic intervention in this study was moderate-intensity exercise, thus the efficacy of light and vigorous intensity exercise on acute changes in affect and OCD symptoms is important to evaluate. For example, while moderate-intensity aerobic exercise produces larger acute effects on negative affect relative to light or vigorous intensity (Ensari et al., 2016), the acute affective benefits from exercise among patients with psychiatric symptoms (e.g., depression) appear to be consistent regardless of intensity level (Meyer et al., 2016). Third, the exercise intervention in this study was supervised by an exercise physiologist, who provided encouragement during sessions. In patients with OCD, who may be more reactive to environmental safety and reassurance cues, this type of supervision may have influenced the affective experience of exercise. Future studies should examine whether supervised versus unsupervised exercise influences acute effects in this population. Fourth, a patients’ baseline levels of physical activity can influence the acute affective response to aerobic exercise wherein those with lowest levels of physical activity (i.e., sedentary) experience the largest acute effects of aerobic exercise on anxiety reduction compared to those who with higher levels of physical activity (Ensari et al., 2015). Future studies should evaluate long-term changes in the acute effects among patients with OCD are able to sustain increase in exercise and whether these mediate changes in OCD symptomatology.
Limitations
Several limitations are worth noting. The sample, albeit comparable to many OCD trials, was small. The patients were primarily women who identified race as white. Greater heterogeneity in sex, age, and ethnicity will be necessary to generalize findings to the larger population of OCD patients. Bouts of aerobic exercise were not standardized in terms of duration and mode (e.g., some may have used treadmill, others the elliptical), which could have impacted affective responses. Additionally, because the sessions were supervised, this limits external validity and introduces testing bias due to being observed. Lastly, negative affect and OCD symptoms were all self-reported. Experimental studies that employ a standardized, sedentary control and behavioral challenges after exercise to evaluate whether patients do resist the urge to engage in compulsions, for example, would provide a more rigorous test of the hypotheses proposed in this study. Such studies would also provide an opportunity to examine plausible physiological mechanisms through which exercise might improve anxiety-related illnesses (Anderson and Shivakumar, 2013).
Conclusions
This is the first randomized controlled trial of the acute effects of exercise on negative affect, obsessions and compulsions in patients with OCD. The findings may help to inform future intervention efforts that can augment existing OCD treatments to improve outcomes in this population.
Figure 2.
Acute Changes in Pre- and Post-Session Anxiety
Figure 3.
Acute Changes in Pre- and Post-Session Obsessions
Highlights.
Aerobic Exercise (AE) produced greater acute mood improvements than Health Education Contact (HEC) control in patients with Obsessive Compulsive Disorder (OCD)
AE produced greater reductions in anxiety than HEC in patients with OCD
AE produced greater reductions in compulsions than HEC in patients with OCD
Neither AE nor HEC produced acute changes in obsessions
Linear reductions in anxiety occurred longitudinally over the course of treatment
Acknowledgments
Funding: This research was supported by a grant from National Institute of Mental Health (R01 MH086513). The second author is supported by a grant from the National Heart, Lung, and Blood Institute (T32-HL076134–11). If the funding sources had no involvement in the research other than financial support.
Footnotes
Declarations of Interest
Drs. Abrantes, Farris, Greenberg, and McLaughlin, Strong, and Riebe have no disclosures to report. Dr. Brown has equity ownership in Health Behavior Solutions, Inc., which is developing products for tobacco cessation although not products directly related to this publication. The terms of this arrangement have been reviewed and approved by the University of Texas at Austin in accordance with its policy on objectivity in research.
Submission Declaration
This manuscript has not been published previously, it is not under consideration for publication elsewhere, the publication was approved by all authors. The work is the responsibilities of Dr. Abrantes and Butler Hospital, where the study took place and where the protocol was approved by the Institutional Review Board. If the manuscript is accepted, it will not be published elsewhere in the same form, in English or in any other language, including electronically without the written consent of the copyright-holder.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Abrantes AM, Blevins CE, Battle CL, Read JP, Gordon AL, Stein MD, 2017a. Developing a Fitbit-supported lifestyle physical activity intervention for depressed alcohol dependent women. J. Subst. Abuse Treat 80, 88–97. 10.1016/j.jsat.2017.07.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abrantes AM, Brown RA, Strong DR, McLaughlin N, Garnaat SL, Mancebo M, Riebe D, Desaulniers J, Yip AG, Rasmussen S, Greenberg BD, 2017b. A pilot randomized controlled trial of aerobic exercise as an adjunct to OCD treatment. Gen. Hosp. Psychiatry 49, 51–55. 10.1016/j.genhosppsych.2017.06.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abrantes AM, Mclaughlin N, Greenberg BD, Strong DR, Riebe D, Mancebo M, Rasmussen S, Desaulniers J, Brown RA, 2012. Design and rationale for a randomized controlled trial testing the efficacy of aerobic exercise for patients with obsessive-compulsive disorder. Ment. Health Phys. Act 5, 155–165. 10.1016/j.mhpa.2012.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abrantes AM, Strong DR, Cohn A, Cameron AY, Greenberg BD, Mancebo MC, Brown RA, 2009. Acute changes in obsessions and compulsions following moderate-intensity aerobic exercise among patients with obsessive-compulsive disorder. J. Anxiety Disord 23, 923–927. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association, 2013. Diagnostic and statistical manual of mental disorders : DSM-5., Diagnostic and Statistical Manual of Mental disorders, Fifth edition. [Google Scholar]
- Anderson E, Shivakumar G, 2013. Effects of Exercise and Physical Activity on Anxiety. Front. Psychiatry 4, 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atmaca M, 2015. Treatment-refractory obsessive compulsive disorder. Prog. Neuro-Psychopharmacology Biol. Psychiatry 10.1016/j.pnpbp.2015.12.004 [DOI] [PubMed] [Google Scholar]
- Basso JC, Suzuki WA, 2017. The Effects of Acute Exercise on Mood, Cognition, Neurophysiology, and Neurochemical Pathways: A Review. Brain Plast 2, 127–152. 10.3233/BPL-160040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK, 1996. Manual for Beck Depression Inventory-II. Psychological Corporation, San Antonio, TX. [Google Scholar]
- Bienvenu OJ, Samuels JF, Costa PT, Reti IM, Eaton WW, Nestadt G, 2004. Anxiety and depressive disorders and the five-factor model of personality: A higher- and lower-order personality trait investigation in a community sample. Depress. Anxiety 20, 92–97. 10.1002/da.20026 [DOI] [PubMed] [Google Scholar]
- Bolger N, Stadler G, & Laurenceau J-P (2012). Power analysis for intensive longitudinal studies In Mehl MR & Conner TS (Eds.), Handbook of research methods for studying daily life (pp. 285–301). New York, NY, US: Guilford Press. [Google Scholar]
- Brown RA, Abrantes AM, Strong DR, Mancebo MC, Menard J, Rasmussen S. a, Greenberg BD, 2007. A pilot study of moderate-intensity aerobic exercise for obsessive compulsive disorder. J. Nerv. Ment. Dis 195, 514–20. 10.1097/01.nmd.0000253730.31610.6c [DOI] [PubMed] [Google Scholar]
- Brown RA, Prince MA, Minami H, Abrantes AM, 2016. An exploratory analysis of changes in mood, anxiety and craving from pre- to post-single sessions of exercise, over 12 weeks, among patients with alcohol dependence. Ment. Health Phys. Act 11, 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carver CS, White TL, 1994. Behavioral inhibition, behavioral activation, and affective responses to impending reward and punishment: The BIS/BAS Scales. J. Pers. Soc. Psychol 67, 319–333. 10.1037/0022-3514.67.2.319 [DOI] [Google Scholar]
- Cheval B, Radel R, Neva JL, Boyd LA, Swinnen SP, Sander D, Boisgontier MP, 2018. Behavioral and Neural Evidence of the Rewarding Value of Exercise Behaviors: A Systematic Review. Sport. Med. 10.1007/s40279-018-0898-0 [DOI] [PubMed] [Google Scholar]
- Dozois DJA, Dobson KS, Ahnberg JL, 1998. A psychometric evaluation of the Beck Depression Inventory-II. Psychol. Assess 10, 83–89. 10.1037/1040-3590.10.2.83 [DOI] [Google Scholar]
- Eaton WW, Martins SS, Nestadt G, Bienvenu OJ, Clarke D, Alexandre P, 2008. The burden of mental disorders. Epidemiol. Rev 30, 1–14. 10.1093/epirev/mxn011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ekkekakis P, Lind E, 2006. Exercise does not feel the same when you are overweight: the impact of self-selected and imposed intensity on affect and exertion. Int. J. Obes. (Lond) 30, 652–60. 10.1038/sj.ijo.0803052 [DOI] [PubMed] [Google Scholar]
- Ensari I, Greenlee TA, Motl RW, Petruzzello SJ, 2015. Meta-Analysis of Acute Exercise Effects on State Anxiety: an Update of Randomized Controlled Trials Over the Past 25 Years. Depress. Anxiety 32, 624–634. 10.1002/da.22370 [DOI] [PubMed] [Google Scholar]
- Ensari I, Sandroff BM, Motl RW, 2016. Intensity of treadmill walking exercise on acute mood symptoms in persons with multiple sclerosis. Anxiety. Stress. Coping 1–11. 10.1080/10615806.2016.1146710 [DOI] [PubMed] [Google Scholar]
- Feingold A (2013). A Regression Framework for Effect Size Assessments in Longitudinal Modeling of Group Differences. Review of General Psychology : Journal of Division 1, of the American Psychological Association, 17(1), 111–121. 10.1037/a0030048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fineberg N. a, Reghunandanan S, Brown A, Pampaloni I, 2013. Pharmacotherapy of obsessive-compulsive disorder: evidence-based treatment and beyond. Aust. N. Z. J. Psychiatry 47, 121–41. 10.1177/0004867412461958 [DOI] [PubMed] [Google Scholar]
- Goodman WK, Price LH, Rasmussen SA, Mazure C, Delgado P, Heninger GR, Charney DS, 1989a. The Yale-Brown Obsessive Compulsive Scale. II. Validity. Arch. Gen. Psychiatry 46, 1012–6. [DOI] [PubMed] [Google Scholar]
- Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischmann RL, Hill CL, Heninger GR, Charney DS, 1989b. The Yale-Brown Obsessive Compulsive Scale. I. Development, use, and reliability. Arch. Gen. Psychiatry 46, 1006–11. [DOI] [PubMed] [Google Scholar]
- Jaffery A, Edwards MK, Loprinzi PD, 2017. Randomized Control Intervention Evaluating the Effects of Acute Exercise on Depression and Mood Profile: Solomon Experimental Design. Mayo Clin. Proc 10.1016/j.mayocp.2016.12.017 [DOI] [PubMed] [Google Scholar]
- Lancer R, Motta R, Lancer D, 2007. The effect of aerobic exercise on obsessive-compulsive disorder, anxiety, and depression: A preliminary investigation. Behav. Ther 30, 53–62. [Google Scholar]
- Linke SE, Rutledge T, Myers MG, 2012. Intermittent exercise in response to cigarette cravings in the context of an Internet-based smoking cessation program. Ment. Health Phys. Act 5, 85–92. 10.1016/j.mhpa.2012.02.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macy AS, Theo JN, Kaufmann SCV, Ghazzaoui RB, Pawlowski P. a, Fakhry HI, Cassmassi BJ, IsHak WW, 2013. Quality of life in obsessive compulsive disorder. CNS Spectr. 18, 21–33. 10.1017/S1092852912000697 [DOI] [PubMed] [Google Scholar]
- McGuire JF, Storch EA, Lewin AB, Price LH, Rasmussen SA, Goodman WK, 2012. The role of avoidance in the phenomenology of obsessive-compulsive disorder. Compr. Psychiatry 53, 187–194. 10.1016/j.comppsych.2011.03.002 [DOI] [PubMed] [Google Scholar]
- McKay D, Sookman D, Neziroglu F, Wilhelm S, Stein DJ, Kyrios M, Matthews K, Veale D, 2015. Efficacy of cognitive-behavioral therapy for obsessive-compulsive disorder. Psychiatry Res. 10.1016/j.psychres.2015.02.004 [DOI] [PubMed] [Google Scholar]
- Meyer JD, Koltyn KF, Stegner AJ, Kim JS, Cook DB, 2016. Influence of Exercise Intensity for Improving Depressed Mood in Depression: A Dose-Response Study. Behav. Ther 47, 527–537. 10.1016/j.beth.2016.04.003 [DOI] [PubMed] [Google Scholar]
- Narayanaswamy JC, Jose D, Chhabra H, Agarwal SM, Shrinivasa B, Hegde A, Bose A, Kalmady SV, Venkatasubramanian G, Reddy YCJ, 2015. Successful application of add-on transcranial direct current stimulation (tDCS) for treatment of SSRI resistant OCD. Brain Stimul. 10.1016/j.brs.2014.12.003 [DOI] [PubMed] [Google Scholar]
- Olatunji BO, Davis ML, Powers MB, Smits JAJ, 2013. Cognitive-behavioral therapy for obsessive-compulsive disorder: A meta-analysis of treatment outcome and moderators. J. Psychiatr. Res 47, 33–41. 10.1016/j.jpsychires.2012.08.020 [DOI] [PubMed] [Google Scholar]
- Rector NA, Richter MA, Lerman B, Regev R, Rector NA, Richter MA, Lerman B, Regev R, Rector NA, Richter MA, Lerman B, 2015. A Pilot Test of the Additive Benefits of Physical Exercise to CBT for OCD A Pilot Test of the Additive Benefits of Physical Exercise to CBT for OCD 6073. 10.1080/16506073.2015.1016448 [DOI] [PubMed]
- Reed J, Buck S, 2009. The effect of regular aerobic exercise on positive-activated affect: A meta-analysis. Psychol. Sport Exerc. 10.1016/j.psychsport.2009.05.009 [DOI] [Google Scholar]
- Simpson HB, Foa EB, Liebowitz MR, Huppert JD, Cahill S, Maher MJ, McLean CP, Bender J, Marcus SM, Williams MT, Weaver J, Vermes D, Van Meter PE, Rodriguez CI, Powers M, Pinto A, Imms P, Hahn C-G, Campeas R, 2013. Cognitive-Behavioral Therapy vs Risperidone for Augmenting Serotonin Reuptake Inhibitors in Obsessive-Compulsive Disorder: A Randomized Clinical Trial. JAMA Psychiatry 70, 1190–9. 10.1001/jamapsychiatry.2013.1932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spinella M, 2005. Mood in relation to subclinical obsessive-compulsive symptoms. Int. J. Neurosci 115, 433–443. 10.1080/00207450590522838 [DOI] [PubMed] [Google Scholar]
- Steer RA, Ball R, Ranieri WF, Beck AT, 1997. Further evidence for the construct validity of the Beck depression Inventory-II with psychiatric outpatients. Psychol. Rep 80, 443–6. 10.2466/pr0.1997.80.2.443 [DOI] [PubMed] [Google Scholar]
- Vikas A, Avasthi A, Sharan P, 2011. Psychosocial impact of obsessive-compulsive disorder on patients and their caregivers: a comparative study with depressive disorder. Int. J. Soc. Psychiatry 57, 45–56. 10.1177/0020764009347333 [DOI] [PubMed] [Google Scholar]
- Williams DM, Dunsiger S, Whiteley JA, Ussher MH, Ciccolo JT, Jennings EG. Acute effects of moderate intensity aerobic exercise on affective withdrawal symptoms and cravings among women smokers. Addict Behav. 2011;36(8):894–897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization, 2002. Quantifying selected major risks to health, in: World Health Report 2002 - Reducing Risks, Promoting Healthy Life. pp. 47–97. [Google Scholar]