The emergence of Neisseria gonorrhoeae strains that are resistant to azithromycin and extended-spectrum cephalosporins represents a public health threat, that of untreatable gonorrhea infections. Multivariate regression modeling was used to determine the contributions of molecular antimicrobial resistance determinants to the overall antimicrobial MICs for ceftriaxone, cefixime, azithromycin, tetracycline, ciprofloxacin, and penicillin.
KEYWORDS: MIC, Neisseria gonorrhoeae, antimicrobial resistance, molecular analysis, whole-genome sequencing
ABSTRACT
The emergence of Neisseria gonorrhoeae strains that are resistant to azithromycin and extended-spectrum cephalosporins represents a public health threat, that of untreatable gonorrhea infections. Multivariate regression modeling was used to determine the contributions of molecular antimicrobial resistance determinants to the overall antimicrobial MICs for ceftriaxone, cefixime, azithromycin, tetracycline, ciprofloxacin, and penicillin. A training data set consisting of 1,280 N. gonorrhoeae strains was used to generate regression equations which were then applied to validation data sets of Canadian (n = 1,095) and international (n = 431) strains. The predicted MICs for extended-spectrum cephalosporins (ceftriaxone and cefixime) were fully explained by 5 amino acid substitutions in PenA, A311V, A501P/T/V, N513Y, A517G, and G543S; the presence of a disrupted mtrR promoter; and the PorB G120 and PonA L421P mutations. The correlation of predicted MICs within one doubling dilution to phenotypically determined MICs of the Canadian validation data set was 95.0% for ceftriaxone, 95.6% for cefixime, 91.4% for azithromycin, 98.2% for tetracycline, 90.4% for ciprofloxacin, and 92.3% for penicillin, with an overall sensitivity of 99.9% and specificity of 97.1%. The correlations of predicted MIC values to the phenotypically determined MICs were similar to those from phenotype MIC-only comparison studies. The ability to acquire detailed antimicrobial resistance information directly from molecular data will facilitate the transition to whole-genome sequencing analysis from phenotypic testing and can fill the surveillance gap in an era of increased reliance on nucleic acid assay testing (NAAT) diagnostics to better monitor the dynamics of N. gonorrhoeae.
INTRODUCTION
Neisseria gonorrhoeae is a Gram-negative organism causing gonorrhea, the second most prevalent sexually transmitted bacterial infection in Canada after Chlamydia trachomatis (https://www.canada.ca/en/public-health/services/publications/drugs-health-products/national-surveillance-antimicrobial-susceptibilities-neisseria-gonorrhoeae-annual-summary-2017.html). Increasing in vitro antimicrobial resistance (AMR) in N. gonorrhoeae threatens the long-term sustainability of current dual-antimicrobial therapeutic regimens (ceftriaxone and azithromycin) and raises concerns for future treatment of gonorrhea (1–6).
The antimicrobial resistance mechanisms for N. gonorrhoeae have been extensively documented (7, 8) and with few exceptions can fully explain the observed antimicrobial phenotypes. Azithromycin resistance in N. gonorrhoeae has been attributed primarily to 23S rRNA point mutations (9, 10), the overexpression of the MtrCDE efflux pump mostly caused by disruptions in the promoter region of an mtrR repressor such as the −35A deletion, mosaic N. meningitidis-like and WHO-P-like disrupted sequences (11, 12), and smaller contributions from the MtrR A39T and G45D mutations (13, 14). Other less common macrolide resistance mechanisms include the mef and MacAB efflux pumps, the presence of ermA, ermB, ermC, and ermF genes encoding 23S rRNA methylases, and mutations in the ribosomal genes rplD and rplV (7). Penicillin and extended-spectrum cephalosporin resistance has been associated with mutations and recombination within penA, porB, ponA, and the presence of bla (8, 15–17). Fluoroquinolone resistance has been well described by variations in GyrA at amino acid positions S91 and D95 and in ParC at positions D86, S87, S88, and E91 (18–20), while tetracycline resistance has been attributed to the presence of tetM (21) and point mutations in rpsJ, mtrR, and porB (22).
Monitoring the dissemination and dynamics of antimicrobial-resistant N. gonorrhoeae has traditionally relied upon in vitro phenotypic susceptibility testing of bacterial cultures; however, the increase in nucleic acid assay testing (NAAT) to diagnose gonorrhea has resulted in fewer bacterial cultures being available for testing. Over 80% of gonococcal infections in Canada are now detected using NAAT, and some jurisdictions no longer maintain the capacity to culture the bacteria (https://www.canada.ca/en/public-health/services/publications/drugs-health-products/national-surveillance-antimicrobial-susceptibilities-neisseria-gonorrhoeae-annual-summary-2017.html) (23). This gap in antimicrobial susceptibility surveillance data may be addressed by the development of novel molecular-based techniques to determine antimicrobial resistance (24–26) by detecting the presence/absence of specific genes or single nucleotide variations (SNVs).
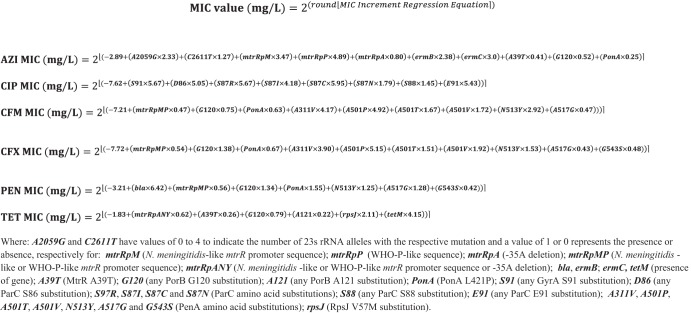
Multivariate regression modeling as a method to predict MICs was first introduced in 2016 to determine azithromycin MICs in N. gonorrhoeae (27) and later expanded in 2017 to include other antimicrobials (28). In this study, we employ a statistical approach not only to determine the categorical antimicrobial resistance or susceptibility, but also to determine the contribution of each molecular determinant to antimicrobial MIC values and provide simple mathematical equations that can be applied to determine the MICs for ceftriaxone, cefixime, azithromycin, penicillin, tetracycline, and ciprofloxacin.
RESULTS
Regression analysis indicated that the predicted MIC (MICpred) for cephalosporins depended upon 5 amino acid substitutions in PenA (A311V, A501P/T/V, N513Y, A517G, and G543S), the presence of a disrupted mtrR promoter (N. meningitidis-like or WHO-P-like), an amino acid change in PorB at G120, and the L41P substitution in PonA. The molecular determinants having the largest effect on ceftriaxone MICs were the A501P/T/V, A311V, N513Y, and the PorB G120 amino acid substitutions, producing an adjusted R2 of 0.721 (see the supplemental material). All ceftriaxone MICpred values calculated from the regression equation (Fig. 1) agreed within one doubling dilution with the published MIC (MICpub) (29) and phenotypically determined MIC (MICpheno) values for the panel of 14 WHO reference strains (Table 1). There was 95.0% (1,040/1,095) concordance within one doubling dilution of the MICpheno of the Canadian validation strains (Table 2). There was only a single Canadian isolate with a ceftriaxone MICpheno of 0.5 mg/liter (corresponding to the resistant interpretative breakpoint) in the Canadian data set. Therefore, meaningful sensitivity and specificity values could not be calculated; however, there were no major (MA) or very major (VMA) interpretative errors.
FIG 1.
Multivariate regression equations to determine the MIC values of azithromycin (AZI), ceftriaxone (CFX), cefixime (CFM), penicillin (PEN), ciprofloxacin (CIP), and tetracycline (TET) based on molecular resistance determinants of Neisseria gonorrhoeae.
TABLE 1.
Correlation of antimicrobial MICs of WHO reference strains determined by logistic regression of molecular antimicrobial resistance determinants and phenotypically determined MICs
| Strain IDa | MIC (mg/liter) data for drugb: |
|||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ciprofloxacin |
Tetracycline |
Cefixime |
Ceftriaxone |
Penicillin |
Azithromycin |
|||||||||||||
| MICpred | MICpub | MICpheno | MICpred | MICpub | MICpheno | MICpred | MICpub | MICpheno | MICpred | MICpub | MICpheno | MICpred | MICpub | MICpheno | MICpred | MICpub | MICpheno | |
| WHO-F | ≤0.004 | 0.004 | 0.004 | ≤0.25 | 0.25 | 0.5 | ≤0.008 | <0.016 | 0.002 | ≤0.004 | 0.001 | 0.001 | ≤0.125 | 0.032 | 0.032 | ≤0.125 | 0.125 | 0.125 |
| WHO-G | 0.25 | 0.125 | 0.125 | 32 | 32 | 16 | 0.016 | <0.016 | 0.016 | 0.008 | 0.008 | 0.008 | 1 | 0.5 | 0.5 | 0.25 | 0.25 | 0.25 |
| WHO-K | ≥32 | >32 | 64 | 4 | 2 | 2 | 0.125 | 0.25 | 0.25 | 0.063 | 0.063 | 0.063 | 2 | 2 | 2 | 0.5 | 0.25 | 0.5 |
| WHO-L | ≥32 | >32 | 32 | 2 | 2 | 2 | 0.063 | 0.125 | 0.063 | 0.125 | 0.125 | 0.125 | 2 | 2 | 2 | 0.25 | 0.5 | 0.25 |
| WHO-M | 0.25 | 2 | 1 | 4 | 2 | 2 | 0.031 | <0.016 | 0.016 | 0.031 | 0.016 | 0.016 | 128 | ≥32 | 32 | 0.5 | 0.25 | 0.5 |
| WHO-N | 4 | 4 | 4 | ≥32 | 16 | 16 | 0.016 | <0.016 | 0.008 | 0.008 | 0.008 | 0.008 | 64 | >32 | 64 | 0.25 | 0.25 | 0.25 |
| WHO-O | ≤0.004 | 0.008 | 0.016 | 4 | 2 | 4 | 0.031 | 0.016 | 0.032 | 0.031 | 0.032 | 0.032 | 128 | >32 | ≥256 | 0.5 | 0.25 | 0.5 |
| WHO-P | ≤0.004 | 0.004 | 0.004 | 2 | 1 | 1 | 0.016 | <0.016 | 0.016 | 0.008 | 0.008 | 0.008 | 0.5 | 0.25 | 0.5 | 4 | 4 | 4 |
| WHO-U | ≤0.004 | 0.004 | 0.004 | 1 | 1 | 2 | 0.016 | <0.016 | 0.004 | 0.008 | 0.004 | 0.004 | 1 | 0.125 | 0.5 | 4 | 4 | 4 |
| WHO-V | 16 | >32 | 32 | 4 | 4 | 8 | 0.031 | <0.016 | 0.032 | 0.031 | 0.063 | 0.063 | ≥256 | >32 | ≥256 | ≥256 | >256 | ≥64 |
| WHO-W | ≥32 | >32 | 64 | 4 | 4 | 4 | 0.125 | 0.25 | 0.25 | 0.063 | 0.125 | 0.125 | 2 | 4 | 8 | 0.5 | 0.5 | 0.25 |
| WHO-X | ≥32 | >32 | 64 | 4 | 2 | 8 | 2 | 4 | ≥4 | 1 | 2 | 2 | 2 | 4 | 8 | 0.5 | 0.5 | 0.25 |
| WHO-Y | 16 | >32 | 16 | 4 | 4 | 8 | ≥4 | 2 | ≥4 | 2 | 2 | 2 | 2 | 1 | 2 | 0.5 | 1 | 0.5 |
| WHO-Z | ≥32 | >32 | 32 | 2 | 4 | 4 | 2 | 2 | 2 | 1 | 0.5 | 0.5 | 2 | 2 | 4 | 0.25 | 1 | 0.5 |
| Agreement (%) | 92.9 | 85.7 | 100 | 100 | 100 | 92.9 | 100 | 100 | 92.9 | 85.7 | 92.9 | 100 | ||||||
ID, identifier.
MICpred, MICpub, and MICpheno represent predicted MIC, published MIC by Unemo et al. (18), and phenotypically determined MICs in this study, respectively. Values in bold identify MIC value differences greater than 2 doubling dilutions for each antimicrobial.
TABLE 2.
Correlation between MICs determined by logistic regression of molecular antimicrobial resistance determinants and phenotypically determined MICs
| Antimicrobial | Data seta | No. of isolates matching MIC dilutions ofb: |
% ±1 doubling dilution | Sensitivity (%)d | Specificity (%)d | % MIC interpretive errorsc |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| >−2 | −2 | −1 | 0 | +1 | +2 | >2 | MI | MA | VMA | |||||
| Ceftriaxone | Canada | 0 | 48 | 612 | 363 | 65 | 7 | 0 | 95.0 | NA | 100 | NB | 0 | 0 |
| UK/USA | 18 | 61 | 157 | 133 | 51 | 9 | 2 | 79.1 | NA | 100 | NB | 0 | 0 | |
| Cefixime | Canada | 0 | 23 | 204 | 615 | 228 | 22 | 3 | 95.6 | NA | 100 | NB | 0 | 0 |
| UK/USA | 10 | 20 | 119 | 126 | 117 | 36 | 3 | 84.0 | NA | 100 | NB | 0 | 0 | |
| Azithromycin | Canada | 16 | 73 | 187 | 754 | 60 | 2 | 3 | 91.4 | 99.7 | 81.2 | NB | 7.7 | 0.2 |
| UK/USA | 12 | 14 | 73 | 114 | 134 | 77 | 7 | 74.5 | 77.3 | 99.8 | NB | 0.2 | 1.2 | |
| Ciprofloxacin | Canada | 13 | 70 | 297 | 512 | 181 | 19 | 3 | 90.4 | 100 | 100 | 0.5 | 0 | 0 |
| UK/USA | 7 | 14 | 31 | 258 | 106 | 5 | 10 | 91.7 | 100 | 98.8 | 1.9 | 0.5 | 0 | |
| Tetracycline | Canada | 0 | 20 | 386 | 631 | 58 | 0 | 0 | 98.2 | 100 | 100 | 13.3 | 0 | 0 |
| UK/USA | 8 | 15 | 101 | 152 | 127 | 22 | 6 | 88.2 | 99.7 | 88.0 | 19.0 | 0.7 | 0.2 | |
| Penicillin | Canada | 13 | 67 | 423 | 487 | 101 | 4 | 0 | 92.3 | 100 | NA | 13.9 | 0 | 0 |
| UK/USA | 60 | 53 | 125 | 106 | 72 | 15 | 0 | 70.3 | 100 | NA | 34.1 | 0.2 | 0 | |
| Overall | Canada | 42 | 301 | 2,109 | 3,362 | 693 | 54 | 9 | 93.8 | 99.9 | 97.1 | 4.6 | 1.3 | 0.03 |
| UK/USA | 115 | 117 | 606 | 889 | 607 | 164 | 28 | 81.3 | 99.2 | 99.5 | 9.2 | 0.3 | 0.2 | |
Canadian validation data set, n = 1,095, and UK/U.S. international data set from Eyre et al. (28), n = 431.
The number of isolates with MICpred and MICpheno values that differ by the number of 2-fold dilutions.
The percentage of isolates with minor (MI), major (ME), and very major (VME) interpretative errors for susceptibilities. NB, no CLSI intermediate resistance interpretative breakpoints for these antimicrobials.
NA, too few isolates available with resistant or susceptible interpretative breakpoints were available to provide meaningful specificity or sensitivity values, respectively.
The MICpred values for cefixime were similarly dependent upon the PenA mutations associated with those influencing ceftriaxone MICs, except for PenA G543S, which had an insignificant P value of 0.514 (see the supplemental material) and was removed from the regression model for cefixime MIC calculation. PenA A501P and A311V had the greatest influence, followed by the N513Y and A501T/V substitutions. Smaller contributions to the cefixime MICpred were from the PonA L421P, PorB G120, and PenA A517G mutations and a disrupted mtrR promoter (meningitidis-like or WHO-P-like), resulting in an adjusted R2 of 0.783. MICpred values for the WHO reference strains corresponded to all of the MICpub and MICpheno values (Table 1), except for those of WHO-F (MICpred, 0.008 mg/liter; MICpheno, 0.002 mg/liter) and WHO-U (MICpred, 0.016 mg/liter; MICpheno, 0.004 mg/liter). There was 95.6% (1,047/1,095) concordance between the cefixime MICpred and MICpheno values to within 1 doubling dilution in the Canadian validation data set and 84.0% (362/431) in the UK/U.S. validation data set. There were no Canadian or UK/U.S. validation isolates with a cefixime MICpheno of ≥1.0 mg/liter (resistant interpretative breakpoint); therefore, a meaningful sensitivity value could not be calculated. There were no major or very major interpretative errors.
The MICpred for azithromycin was strongly influenced by the number of 23S rRNA alleles with the A2059G or C2611T mutation, the presence of mtrR meningitidis-like and WHO-P-like promoter mutations, and the presence of ermB or ermC, while lesser contributions were attributed to the mtrR −35A deletion, MtrR A39T, and PonA L421P, producing an adjusted R2 of 0.831. The azithromycin MICpred values for the panel of 14 WHO reference strains agreed within one doubling dilution to the MICpub and MICpheno values, except for strain WHO-Z (MICpred, 0.25 mg/liter; MICpub, 1 mg/liter). Agreement within one doubling dilution of the MICpred and MICpheno was 91.4% (1,001/1,095) and 74.5% (321/431) for the Canadian and UK/U.S. validation data sets, respectively (Table 2). There was a high degree of sensitivity for resistant predictions (99.7%) but a lower specificity for susceptible predictions (81.2%) due to the relatively large number of susceptible isolates (n = 69) that were one MICpheno dilution below the CLSI resistance breakpoint of 2 mg/liter.
Ciprofloxacin MICs were most influenced by GyrA S91, ParC S87R/I/C, ParC E91, and ParC S86 mutations, with smaller regression coefficients attributed to ParC S87N and ParC S88. The GyrA D95 was found to be an insignificant contributor to increased ciprofloxacin resistance (P = 0.778) and was removed from the regression model, resulting in an adjusted R2 of 0.979. The MICpred values matched the MICpub and MICpheno values for most of the WHO reference strains within one dilution. WHO-M had the GyrA S91F ciprofloxacin resistance determinant, producing a ciprofloxacin MICpred of 0.25 mg/liter but an MICpub of 2 mg/liter and MICpheno of 1 mg/liter; WHO-O had an MICpred of 0.004 mg/liter, two dilutions away from the MICpheno of 0.016 mg/liter. There was 90.4% (990/1,095) agreement of the ciprofloxacin MICpred and MICpheno values within one dilution with the Canadian validation data, with sensitivity and specificity both at 100%, 6 minor errors, and no major or very major errors. Agreement with the international UK/U.S. data was 91.7% (395/431), with 100% sensitivity, 98.8% specificity, and 8 minor, 2 major, and no very major interpretative errors.
The best regression model for tetracycline MICpred had an adjusted R2 value of 0.812, with tetM and the V57M RpsJ amino acid substitution providing the greatest contributions, followed by PorB G120 and A121 mutations, mtrR promoter disruptions (N. meningitidis-like or WHO-P-like or −35A deletion), and the MtrR A39T substitution. All tetracycline MICpred values for the WHO reference strain panel were within one dilution of the MICpub and MICpheno values. There was a 98.2% (1075/1,095) correlation between the MICpred and MICpheno values within one dilution for the Canadian data set, with 100% sensitivity and specificity, 142 minor errors, and no major or very major interpretative errors. There was also a high degree of agreement with the UK/U.S. validation isolates, at 88.2% (380/431), as well as 99.7% sensitivity, 88.0% specificity, 82 minor interpretative errors, 3 major errors, and 1 very major error.
The greatest contributor to penicillin resistance in the regression model was the presence of bla, distantly followed by the presence of a disrupted mtrR promoter (N. meningitidis-like or WHO-P-like), PorB G120, PonA L421P, and PenA N513Y, A517G, and G543S amino acid substitutions for an adjusted R2 value of 0.720. Among the WHO reference strain penicillin MICs, the MICpred for WHO-F was 0.125 mg/liter, two dilutions higher than the MICpub and MICpheno values (0.032 mg/liter for each); similarly, for WHO-U, the MICpred was 1 mg/liter, but the MICpub was 0.125 mg/liter. WHO-W and WHO-X had an MICpred of 2 mg/liter, within a single dilution of the MICpub of 4 mg/liter; however, it was two dilutions lower than the MICpheno of 8 mg/liter. The penicillin MICpred agreed within one dilution to 92.3% (1,011/1,095) of the Canadian MICpheno, with 100% sensitivity, 152 minor errors, and no major or very major interpretative errors. The penicillin MICpred agreement for the UK/U.S. data set was 70.3% (303/431), with 100% sensitivity and specificity and 147 minor errors, 1 major error, and no very major interpretative errors. The relatively large number of minor errors in both validation data sets was due to the very broad CLSI intermediate resistance interpretative breakpoint range for penicillin covering 4 doubling dilutions from 0.125 to 1 mg/liter.
DISCUSSION
Multivariate linear regression modeling successfully estimated the contributions of the commonly recognized molecular antimicrobial resistance determinants in N. gonorrhoeae to the MIC values for each antimicrobial investigated. Numerous mutations in penA and the presence of recombinant mosaic sequences from other commensal Neisseria spp., as well as other contributing factors, including changes to mtrR, porB, and ponA, have been associated with decreased susceptibility of extended-spectrum cephalosporins; however, it was thought that these factors do not fully account for the phenotypes observed and that other factors may be involved (7, 16, 30–40). The optimized regression model indicated that extended-spectrum cephalosporin susceptibility within the data sets of this study can be fully described by the combination of a relatively small number of factors, including five key amino acid changes in PenA, and the presence or absence of the disrupted mtrR promoter, a PorB G120 mutation, and/or the PonA L421P mutation.
The PenA A501P had the largest regression coefficient value of approximately 5 for both cefixime and ceftriaxone, corresponding to 5 MIC doubling dilution increments, whereas the A501V and A501T substitutions had coefficients of approximately 1.5 to 2.0, representing 2-fold increases in MICs. Transformation experiments investigating the contributions of various PenA amino acid substitutions to increasing cephalosporin MIC values (41–45) have reported a similar 5-fold MIC increase attributed to the A501P mutation and a 2-fold increase due to the A501T/V mutations. The A311V mutation also was found to contribute significantly to the overall cephalosporin MIC, with regression coefficients representing 4 doubling dilutions; this is higher than in transformation experiments, where only a 2-fold increase was reported (43). The regression coefficients for the N513Y mutation of 3 and 1.5 for cefixime and ceftriaxone, respectively, corresponded to transformation studies reporting 2-fold increases in cephalosporin MICs (42). It has also been reported that the PenA G453S substitution is more important for ceftriaxone resistance than for cefixime (42), which is reflected in the increased regression coefficient of 0.5 for ceftriaxone compared to an insignificant regression P value for cefixime. The regression model predicted ceftriaxone and cefixime MICs matching those expected for the WHO reference strain panel (Table 1) and over 95% of the phenotypically determined MICs among the Canadian validation data set within one doubling dilution.
Azithromycin MICpred values were most influenced by the A2059G and C2611T 23S rRNA mutations, where each allele with an A2059G mutation contributed 2.6 dilution increments, and each allele with a C2611T mutation contributed 1.3 dilution increments to the predicted MIC. Disruption of the mtrR promoter region was also identified as an important contributor to overall azithromycin MIC levels, with the WHO-P-like promoter contributing more to azithromycin resistance than does the N. meningitidis-like promoter, with regression coefficients of 4.9 and 3.5, respectively. Although rare, the presence of ermB or ermC also contributed to MIC values with high regression coefficient values of 2.4 and 3.0, respectively. Smaller contributions to overall azithromycin MIC values were the mtrR −35A deletion and the MtrR A39T and PorB G120 amino acid substitutions. The regression results agree with previous reports that describe major macrolide resistance mechanisms in N. gonorrhoeae, including 23S rRNA mutations, inhibited regulation of the MtrCDE efflux pump, and smaller contributions from MtrR amino acid substitutions (10, 11, 13, 14). Macrolide resistance has not been previously associated with porB; however, the regression analysis generated significant P values for the PorB G120 amino acid substitution, and including it in the regression model improved the azithromycin MIC correlations with the WHO reference strains. It is unclear if this may be due to a coincidental statistical association caused by the content of the training data set which is enriched with antimicrobial-resistant isolates, or speculatively, that the altered porin protein may decrease the influx of azithromycin into the cell, as has been described for increased resistance to other hydrophobic antimicrobials and tetracycline (8, 22, 46).
Fluoroquinolone resistance has been strongly associated with GyrA and ParC amino acid substitutions (18–20); however, regression analysis of these reported mutations was able to predict the contribution of each mutation to the overall MIC. While the GyrA D95 mutation seemed to have no influence on ciprofloxacin MICs, they were highly dependent upon the GyrA S91 and the ParC S86, S87, and E91 amino acid substitutions each having regression coefficients greater than 5, and the ParC S88P mutation contributed less, with a coefficient of 1.4. Furthermore, the magnitude of the MIC contribution associated with the ParC S87 mutation was found to be dependent upon the particular amino acid substituted, with S87I, S87IR, and S87C having the greatest influence (coefficient, >4), whereas the S87N mutation contributed less (coefficient, <2).
The presence of bla was largest contributor to penicillin MIC values, with a regression coefficient of over 6, and its presence typically resulted in MICpred values of at least 32 mg/liter. Other more moderate increases to MIC were due to the PonA L421P, PorB G120, and PenA N513Y and A517G mutations, followed by weaker contributions by an N. meningitidis-like or WHO-P-like mtrR promoter and the PenA G543S substitution. The contributions of molecular determinants to tetracycline resistance generally coincide with those previously described (22, 28), with the presence of tetM having the greatest effect, followed by the presence of the RpsJ V57M mutation, a disrupted mtrR promoter (N. meningitidis-like or WHO-P-like), and smaller contributions from MtrR A39T, PorB G120, and PorB G121.
Predicted MIC values for the six antimicrobials matched 96% of those published for the panel of 14 WHO reference strains (18) within one doubling dilution (Table 1). Phenotypic MIC values for the WHO reference strains were determined as the modal MIC value from routine quality assurance testing, and the overall MICpred concordance was 93%. WHO-M possessed the GyrA S91F substitution as the sole fluoroquinolone resistance determinant, which resulted in a ciprofloxacin MICpred of 0.25 mg/liter. Although this MICpred was two dilutions lower than the modal MICpheno of 1 mg/liter during routine testing using WHO-M as a control strain in 10 quality assurance panels, it fell within the range of MICs from 0.5 to 4 mg/liter. Similarly, the PonA L421P and PenA A517G penicillin resistance determinants present in WHO-U produce an MICpred of 1 mg/liter, two dilutions higher than the phenotypic modal value of 0.25 mg/liter but within the range of MICs of 0.125 to 0.5 mg/liter. WHO-Z possessed only the PorB G120K azithromycin resistance determinant producing a low MICpred of 0.25 mg/liter, which was two dilutions below the modal phenotypic value of 1 mg/liter (range, 0.5 to 1 mg/liter). These wide ranges of phenotypically derived MIC values reveal the high degree of variability and subjectivity in the nature of phenotypic MIC testing which may explain these discrepancies; however, the presence of additional undescribed factors present in these control strains influencing MIC values cannot be discounted. The regression modeling in this study selected only those factors contributing to increased MIC values by having positive regression coefficients. In the case of the higher-than-expected penicillin MICpred for WHO-U, it may be possible that there are other factors that interfere with the full expression of resistance factors to decrease MIC values.
There was an overall correlation of 93.8% for MICpred to MICpheno within one dilution in the Canadian validation data set, lower than the 81.3% agreement for the UK/U.S. validation data set (Table 2) but higher than the 92.4% correlation of MICpred comparisons reported by Eyre et al. (28) for the 431 isolates of the UK/U.S. data set (Table S13). In particular, greater MICpred correlations were attained for cefixime, penicillin, and tetracycline in this study, whereas higher agreement of azithromycin and ciprofloxacin MICpred was seen in the data set presented by Eyre et al. (28). Correlation rates also varied geographically, with higher agreement with U.S. strains for ceftriaxone and penicillin, whereas for cefixime and azithromycin, agreement was higher with the UK validation data. Lower MIC correlations using the Canadian-based training data set to generate the regression equations with the international data set could be due to different sampling, culturing methods, laboratory testing procedures, interpretation of results, geographical clonal variation, and the inability to confirm phenotypic or sequencing results.
Despite these discrepancies, the comparison of MICpred to MICpheno compares favorably to comparison studies of purely phenotypic results. A study in 2015 compared the results of 25 quality assurance proficiency panels for the Canadian National Gonococcal Antimicrobial Susceptibility Comparison Program (47), where the average MIC agreement ranged from 85.6% to 98.9% and interpretation agreed from 85.7% to 98.1% between 9 reference laboratories over a 10-year period. The results from a 2018 comparison of international antimicrobial proficiency panel results from various Caribbean and South American countries (48) reported an overall agreement of >90% for MIC results and modal MICs for 5 of the 11 participants, with agreement among the other laboratories ranging from 60.0% to 82.4%. MIC agreement among the participating laboratories for cefixime and azithromycin was >90%, whereas for tetracycline, ceftriaxone, and ciprofloxacin, agreement ranged from 84.5% to 89.1%, and for penicillin, overall agreement was 78.8%.
The limitations of the study include that the accuracy and precision of the MIC prediction based on molecular determinants are largely limited by the training data used to generate the regression equations. The training data may include variability due to the subjective nature of phenotypic testing, where the same phenotypes may not always be observed on repeat testing; molecular resistance profile errors and the possible presence of as-yet-unidentified resistance factors affect the formation of the regression model. While using a large training data set to develop the regression model can resolve some discrepancies, some rare resistance patterns, such as very high ceftriaxone and cefixime resistance, are reliant on the availability of a relatively small number isolates with this phenotype. Furthermore, there may also be some rare resistance determinants that were not present or were present in insufficient numbers to significantly influence the regression model. These limitations can be reduced by increasing the size of the training data with strains from more varied regions of the world and regularly updating the regression model with newly discovered factors and updated coefficient values for currently identified factors. Furthermore, the MIC prediction models described here can be easily generated using the molecular markers discussed in this study with local training phenotypic data sets which may be more applicable to different laboratory testing environments.
The spread of antimicrobial-resistant N. gonorrhoeae emphasizes the need for surveillance systems that not only closely track the dissemination of known resistant strains but also promptly detect the novel expansion of resistant clones as they emerge to limit the expansion through sexual networks. As molecular-based genomic techniques become more broadly available not only to identify lineages but also provide additional information regarding molecular antibiotic resistance, virulence, and fitness determinants (27, 49, 50), the MIC-predicting strategy described here can provide a powerful tool to replace traditional phenotypic MIC determination. The ability to acquire detailed antimicrobial resistance information directly from molecular data for use in molecular assays will enhance the monitoring of the dynamics of N. gonorrhoeae strains and effectively inform public health interventions to reduce the burden of disease.
MATERIALS AND METHODS
Isolates and antimicrobial susceptibility testing.
Multivariate linear regression analysis was performed using Excel 2010 (version 14.0.7151.5001; Microsoft Corp.) on a training data set of 1,264 N. gonorrhoeae isolates collected from 1989 to 2018 for which whole-genome sequencing data were available from previous projects (27, 49, 51, 52). Isolates from these projects provided a broad range of ciprofloxacin, azithromycin, cefixime, ceftriaxone, penicillin, and tetracycline MICs and consisted of 510 Canadian isolates enriched with isolates having decreased cephalosporin susceptibility (49), a set of 429 Canadian and 47 Dutch isolates enriched for azithromycin resistance (27, 51), 117 Canadian isolates with diverse antimicrobial resistance used for the development of a real-time PCR antimicrobial resistance assay (52), and a convenience sample of 161 other diverse Canadian isolates selected from a national enhanced gonococcal antimicrobial resistance surveillance project (https://www.canada.ca/en/public-health/services/publications/drugs-health-products/national-surveillance-antimicrobial-susceptibilities-neisseria-gonorrhoeae-annual-summary-2017.html). Fourteen WHO reference strains (18) were included to enrich the training data with high-level cephalosporin phenotypic MICs, and 2 strains from Eyre et al. (28) (SRA accession numbers ERR191763 and ERR191769) with the relatively rare ParC S87I substitution were also added to enhance ciprofloxacin MIC regression training. The validation data included a data set of 1,095 Canadian isolates collected from 2013 to 2019 and an international validation data set described by Eyre et al. (28), with 431 N. gonorrhoeae isolates with complete antimicrobial resistance data from the United Kingdom (n = 245) and United States (n = 186) obtained from the Sequence Read Archive of the NCBI.
Antimicrobial susceptibilities to ciprofloxacin, azithromycin, cefixime, ceftriaxone, penicillin, and tetracycline for the Canadian and U.S. data sets were determined using the agar dilution method, according to Clinical and Laboratory Standards Institute (CLSI) guidelines (53), and those for the UK were determined by the GRASP method (28). MIC resistance interpretations were based on the CLSI criteria for penicillin (MIC, ≥2.0 mg/liter), tetracycline (MIC, ≥2.0 mg/liter), and ciprofloxacin (MIC, ≥1.0 mg/liter) (53). WHO guidelines were used to define cefixime and ceftriaxone resistance at MICs of ≥0.25 mg/liter and ≥0.5 mg/liter, respectively (54), and the resistance breakpoint for azithromycin was an MIC of ≥2.0 mg/liter (55).
Molecular analysis.
Molecular antimicrobial resistance determinants were identified in silico from whole-genome sequencing data, as previously described (27, 28, 49). The mtrR promoter disruptions (−35A deletion, mosaic N. meningitidis-like and WHO-P disrupted sequences), presence of the ermB and ermC genes, MtrR A39T and G45D mutations, and 23S rRNA A2059G and C2611T mutations (23S rRNA mutations are Escherichia coli numbering corresponding to A2045G and C2597T in N. gonorrhoeae NCCP11945, respectively) were included as azithromycin susceptibility determinants. Tetracycline resistance markers included the presence of tetM, mtrR promoter disruptions, and the RpsJ V57M, MtrR A39T and G45D, PorB G120 and A121, and PonA L421P substitutions. GyrA amino acid substitutions S91 and D95 and ParC D86, S87, S88, and E91 substitutions were analyzed as ciprofloxacin resistance determinants. Penicillin and cephalosporin resistance factors analyzed included the presence of bla, penA mutations, mtrR promoter disruptions, and MtrR A39T and G45D, PorB G120 and A121, and PonA L421P substitutions.
Multivariate regression analysis.
Multivariate regression analyses (56) were performed using Excel 2010 (version 14.0.7151.5001; Microsoft Corp.) to determine the relationship of the molecular antimicrobial resistance determinants contained in an isolate to the phenotypically determined MIC values for azithromycin, penicillin, ceftriaxone, cefixime, ciprofloxacin, and tetracycline (27, 28). The doubling phenotypic MIC values were standardized to exact doubling dilutions (512, 256, 128, 64, 32, 16, 8, 4, 2, 1, 0.5, 0.25, 0.125, 0.0625, 0.03125, 0.015625, 0.0078125, 0.00390625, 0.001953125, and 0.000976563 mg/liter), converted to a linear increment scale using a formula, phenotypic MIC increment = log2(standardized MIC), and used as the dependent variable in the regression analysis. Molecular markers were used as independent variables and represented by a presence or absence with a value of 1 or 0, respectively, except the variable for the 23S rRNA A2059G and C2611T mutations, which corresponded to the number of alleles with a respective mutation. A regression model for each antimicrobial was built from a preliminary analysis that included all independent variables, followed by stepwise removal of variables with relatively high individual P values and those causing little change in the adjusted coefficient of determination (R2) value (see the supplemental material for metadata and MS Excel regression outputs). An adjusted R2 value (95% confidence interval) of 0.0 to 0.1 was considered no correlation to a very weak correlation, 0.2 to 0.4 was a weak correlation, 0.5 to 0.7 was a moderate correlation, 0.8 to 0.9 was a strong correlation, and >0.9 was a very strong correlation. Predicted MIC (MICpred) values for each antimicrobial were calculated by first calculating the predicted MIC increment by summing the regression intercept and independent variable coefficients for each isolate, rounding fractional values up or down to the nearest whole integer, and then converting this value back to a doubling MIC value using the following formula: predicted MIC value = 2predicted MIC increment. Individual P values of <0.05 for the independent variables at a confidence interval of 95% were considered significant.
Sensitivity and specificity for the MICpred were based on agreement of the antimicrobial susceptibilities as predicted by the molecular markers to that confirmed by traditional phenotypic testing, with true positive (TP) defined as resistant predicted and phenotypic MICs, false negative (FN) defined as resistant predicted MICs and susceptible phenotypic MICs, true negative (TN) defined as susceptible predicted and phenotypic MICs, and false positive (FP) defined as a susceptible predicted MICs and resistant phenotypic MICs. Calculations were performed as follows: sensitivity (SENS) = TP/(FN + TP) × 100, and specificity (SPEC) = TN/(FP + TN) × 100 (57). Antimicrobial resistance interpretative errors were defined as follows: a minor error (MI) was when the MICpred corresponded to intermediate resistance and phenotypically derived MICs (MICpheno) corresponded to either susceptible or resistance interpretations and vice versa, a major error (ME) was when the MICpred corresponded to a resistant interpretation and the MICpheno was susceptible, and a very major error (VME) was when the MICpred was susceptible and the MICpheno was resistant.
Supplementary Material
ACKNOWLEDGMENTS
We thank Gary Liu, Angela Yuen, and Shelley Peterson from the Streptococcus and Sexually Transmitted Diseases Unit at NML for their laboratory technical assistance; the NML Science Technology Cores and Services Division for their genomics infrastructure, software tools, technical support, and guidance; the NML Genomics Core Facility for their next-generation sequencing and analytical expertise; and the New Brunswick Department of Health (Rita Gad, Sophie Wertz, and Louis-Alexandre Jalbert) and staff in New Brunswick regional labs for participating in the surveillance program.
Footnotes
Supplemental material is available online only.
REFERENCES
- 1.Unemo M, Golparian D, Shafer WM. 2014. Challenges with gonorrhea in the era of multi-drug and extensively drug resistance–are we on the right track? Expert Rev Anti Infect Ther 12:653–656. doi: 10.1586/14787210.2014.906902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Allen VG, Mitterni L, Seah C, Rebbapragada A, Martin IE, Lee C, Siebert H, Towns L, Melano RG, Low DE. 2013. Neisseria gonorrhoeae treatment failure and susceptibility to cefixime in Toronto, Canada. JAMA 309:163–170. doi: 10.1001/jama.2012.176575. [DOI] [PubMed] [Google Scholar]
- 3.Unemo M, Nicholas RA. 2012. Emergence of multidrug-resistant, extensively drug-resistant and untreatable gonorrhea. Future Microbiol 7:1401–1422. doi: 10.2217/fmb.12.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gratrix J, Bergman J, Egan C, Drews SJ, Read R, Singh AE. 2013. Retrospective review of pharyngeal gonorrhea treatment failures in Alberta, Canada. Sex Transm Dis 40:877–879. doi: 10.1097/OLQ.0000000000000033. [DOI] [PubMed] [Google Scholar]
- 5.Ison CA, Town K, Obi C, Chisholm S, Hughes G, Livermore DM, Lowndes CM, GRASP Collaborative Group. 2013. Decreased susceptibility to cephalosporins among gonococci: data from the Gonococcal Resistance to Antimicrobials Surveillance Programme (GRASP) in England and Wales, 2007–2011. Lancet Infect Dis 13:762–768. doi: 10.1016/S1473-3099(13)70143-9. [DOI] [PubMed] [Google Scholar]
- 6.Unemo M, Ison CA, Cole M, Spiteri G, van de Laar M, Khotenashvili L. 2013. Gonorrhoea and gonococcal antimicrobial resistance surveillance networks in the WHO European Region, including the independent countries of the former Soviet Union. Sex Transm Infect 89:iv42–iv46. doi: 10.1136/sextrans-2012-050909. [DOI] [PubMed] [Google Scholar]
- 7.Unemo M, Shafer WM. 2014. Antimicrobial resistance in Neisseria gonorrhoeae in the 21st century: past, evolution, and future. Clin Microbiol Rev 27:587–613. doi: 10.1128/CMR.00010-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Balashov S, Mordechai E, Adelson ME, Gygax SE. 2013. Multiplex bead suspension array for screening Neisseria gonorrhoeae antibiotic resistance genetic determinants in noncultured clinical samples. J Mol Diagn 15:116–129. doi: 10.1016/j.jmoldx.2012.08.005. [DOI] [PubMed] [Google Scholar]
- 9.Chisholm SA, Dave J, Ison CA. 2010. High-level azithromycin resistance occurs in Neisseria gonorrhoeae as a result of a single point mutation in the 23S rRNA genes. Antimicrob Agents Chemother 54:3812–3816. doi: 10.1128/AAC.00309-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ng LK, Martin I, Liu G, Bryden L. 2002. Mutation in 23S rRNA associated with macrolide resistance in Neisseria gonorrhoeae. Antimicrob Agents Chemother 46:3020–3025. doi: 10.1128/aac.46.9.3020-3025.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cousin SL, Whittington WLH, Roberts MC. 2003. Acquired macrolide resistance genes and the 1 bp deletion in the mtrR promoter in Neisseria gonorrhoeae. J Antimicrob Chemother 51:131–133. doi: 10.1093/jac/dkg040. [DOI] [PubMed] [Google Scholar]
- 12.Rouquette-Loughlin CE, Reimche JL, Balthazar JT, Dhulipala V, Gernert KM, Kersh EN, Pham CD, Pettus K, Abrams AJ, Trees DL, St. Cyr S, Shafer WM. 2018. Mechanistic basis for decreased antimicrobial susceptibility in a clinical isolate of Neisseria gonorrhoeae possessing a mosaic-like mtr efflux pump locus. mBio 9:e02281-18. doi: 10.1128/mBio.02281-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Warner DM, Shafer WM, Jerse AE. 2008. Clinically relevant mutations that cause derepression of the Neisseria gonorrhoeae MtrC-MtrD-MtrE efflux pump system confer different levels of antimicrobial resistance and in vivo fitness. Mol Microbiol 70:462–478. doi: 10.1111/j.1365-2958.2008.06424.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zarantonelli L, Borthagaray G, Lee EH, Shafer WM. 1999. Decreased azithromycin susceptibility of Neisseria gonorrhoeae due to mtrR mutations. Antimicrob Agents Chemother 43:2468–2472. doi: 10.1128/AAC.43.10.2468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lewis DA. 2010. The gonococcus fights back: is this time a knock out? Sex Transm Infect 86:415–421. doi: 10.1136/sti.2010.042648. [DOI] [PubMed] [Google Scholar]
- 16.Ohnishi M, Golparian D, Shimuta K, Saika T, Hoshina S, Iwasaku K, Nakayama S, Kitawaki J, Unemo M. 2011. Is Neisseria gonorrhoeae initiating a future era of untreatable gonorrhea? Detailed characterization of the first strain with high-level resistance to ceftriaxone. Antimicrob Agents Chemother 55:3538–3545. doi: 10.1128/AAC.00325-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ito M, Deguchi T, Mizutani KS, Yasuda M, Yokoi S, Ito SI, Takahashi Y, Ishihara S, Kawamura Y, Ezaki T. 2005. Emergence and spread of Neisseria gonorrhoeae clinical isolates harboring mosaic-like structure of penicillin-binding protein 2 in central Japan. Antimicrob Agents Chemother 49:137–143. doi: 10.1128/AAC.49.1.137-143.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Unemo M, Golparian D, Sánchez-Busó L, Grad Y, Jacobsson S, Ohnishi M, Lahra MM, Limnios A, Sikora AE, Wi T, Harris SR. 2016. The novel 2016 WHO Neisseria gonorrhoeae reference strains for global quality assurance of laboratory investigations: phenotypic, genetic and reference genome characterization. J Antimicrob Chemother 71:3096–3108. doi: 10.1093/jac/dkw288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Trees DL, Sandul AL, Peto-Mesola V, Aplasca MR, Leng HB, Whittington WL, Knapp JS. 1999. Alterations within the quinolone resistance-determining regions of GyrA and ParC of Neisseria gonorrhoeae isolated in the Far East and the United States. Int J Antimicrob Agents 12:325–332. doi: 10.1016/S0924-8579(99)00081-3. [DOI] [PubMed] [Google Scholar]
- 20.Belland RJ, Morrison SG, Ison C, Huang WM. 1994. Neisseria gonorrhoeae acquires mutations in analogous regions of gyrA and parC in fluoroquinolone-resistant isolates. Mol Microbiol 14:371–380. doi: 10.1111/j.1365-2958.1994.tb01297.x. [DOI] [PubMed] [Google Scholar]
- 21.Turner A, Gough KR, Leeming JP. 1999. Molecular epidemiology of tetM genes in Neisseria gonorrhoeae. Sex Transm Infect 75:60–66. doi: 10.1136/sti.75.1.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hu M, Nandi S, Davies C, Nicholas RA. 2005. High-level chromosomally mediated tetracycline resistance in Neisseria gonorrhoeae results from a point mutation in the rpsJ gene encoding ribosomal protein S10 in combination with the mtrR and penB resistance determinants. Antimicrob Agents Chemother 49:4327–4334. doi: 10.1128/AAC.49.10.4327-4334.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Centers for Disease Control and Prevention (CDC). 2012. Cephalosporin-resistant Neisseria gonorrhoeae public health response plan. Centers for Disease Control and Prevention, Atlanta, GA: https://www.cdc.gov/std/treatment/ceph-r-responseplanjuly30-2012.pdf. [Google Scholar]
- 24.Graham RMA, Doyle CJ, Jennison AV. 2017. Epidemiological typing of Neisseria gonorrhoeae and detection of markers associated with antimicrobial resistance directly from urine samples using next generation sequencing. Sex Transm Infect 93:65–67. doi: 10.1136/sextrans-2015-052422. [DOI] [PubMed] [Google Scholar]
- 25.Peterson SW, Martin I, Demczuk W, Bharat A, Hoang L, Wylie J, Allen V, Lefebvre B, Tyrrell G, Horsman G, Haldane D, Garceau R, Wong T, Mulvey MR. 2015. Molecular assay for detection of ciprofloxacin resistance in Neisseria gonorrhoeae isolates from cultures and clinical nucleic acid amplification test specimens. J Clin Microbiol 53:3606–3608. doi: 10.1128/JCM.01632-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Peterson SW, Martin I, Demczuk W, Bharat A, Hoang L, Wylie J, Allen V, Lefebvre B, Tyrrell G, Horsman G, Haldane D, Garceau R, Wong T, Mulvey MR. 2015. Molecular assay for detection of genetic markers associated with decreased susceptibility to cephalosporins in Neisseria gonorrhoeae. J Clin Microbiol 53:2042–2048. doi: 10.1128/JCM.00493-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Demczuk W, Martin I, Peterson S, Bharat A, Van Domselaar G, Graham M, Lefebvre B, Allen V, Hoang L, Tyrrell G, Horsman G, Wylie J, Haldane D, Archibald C, Wong T, Unemo M, Mulvey MR. 2016. Genomic epidemiology and molecular resistance mechanisms of azithromycin-resistant Neisseria gonorrhoeae in Canada from 1997 to 2014. J Clin Microbiol 54:1304–1313. doi: 10.1128/JCM.03195-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Eyre DW, De Silva D, Cole K, Peters J, Cole MJ, Grad YH, Demczuk W, Martin I, Mulvey MR, Crook DW, Walker AS, Peto TEA, Paul J. 2017. WGS to predict antibiotic MICs for Neisseria gonorrhoeae. J Antimicrob Chemother 72:1937–1947. doi: 10.1093/jac/dkx067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Low N, Unemo M. 2016. Molecular tests for the detection of antimicrobial resistant Neisseria gonorrhoeae: when, where, and how to use? Curr Opin Infect Dis 29:45–51. doi: 10.1097/QCO.0000000000000230. [DOI] [PubMed] [Google Scholar]
- 30.Golparian D, Hellmark B, Fredlund H, Unemo M. 2010. Emergence, spread and characteristics of Neisseria gonorrhoeae isolates with in vitro decreased susceptibility and resistance to extended-spectrum cephalosporins in Sweden. Sex Transm Infect 86:454–460. doi: 10.1136/sti.2010.045377. [DOI] [PubMed] [Google Scholar]
- 31.Ropp PA, Hu M, Olesky M, Nicholas RA, Hill C, Carolina N. 2002. Mutations in ponA, the gene encoding penicillin-binding protein 1, and a novel locus, penC, are required for high-level chromosomally mediated penicillin resistance in Neisseria gonorrhoeae. Antimicrob Agents Chemother 46:769–777. doi: 10.1128/AAC.46.3.769-777.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Whiley DM, Jacobsson S, Tapsall JW, Nissen MD, Sloots TP, Unemo M. 2010. Alterations of the pilQ gene in Neisseria gonorrhoeae are unlikely contributors to decreased susceptibility to ceftriaxone and cefixime in clinical gonococcal strains. J Antimicrob Chemother 65:2543–2547. doi: 10.1093/jac/dkq377. [DOI] [PubMed] [Google Scholar]
- 33.Stoltey JE, Barry PM. 2012. The use of cephalosporins for gonorrhea: an update on the rising problem of resistance. Expert Opin Pharmacother 13:1411–1420. doi: 10.1517/14656566.2012.690396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lindberg R, Fredlund H, Nicholas R, Unemo M. 2007. Neisseria gonorrhoeae isolates with reduced susceptibility to cefixime and ceftriaxone: association with genetic polymorphisms in penA, mtrR, porB1b, and ponA. Antimicrob Agents Chemother 51:2117–2122. doi: 10.1128/AAC.01604-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lee SG, Lee H, Jeong SH, Yong D, Chung GT, Lee YS, Chong Y, Lee K. 2010. Various penA mutations together with mtrR, porB and ponA mutations in Neisseria gonorrhoeae isolates with reduced susceptibility to cefixime or ceftriaxone. J Antimicrob Chemother 65:669–675. doi: 10.1093/jac/dkp505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Osaka K, Takakura T, Narukawa K, Takahata M, Endo K, Kiyota H, Onodera S. 2008. Analysis of amino acid sequences of penicillin-binding protein 2 in clinical isolates of Neisseria gonorrhoeae with reduced susceptibility to cefixime and ceftriaxone. J Infect Chemother 14:195–203. doi: 10.1007/s10156-008-0610-7. [DOI] [PubMed] [Google Scholar]
- 37.Whiley DM, Limnios EA, Ray S, Sloots TP, Tapsall JW. 2007. Diversity of penA alterations and subtypes in Neisseria gonorrhoeae strains from Sydney, Australia, that are less susceptible to ceftriaxone. Antimicrob Agents Chemother 51:3111–3116. doi: 10.1128/AAC.00306-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zhao S, Duncan M, Tomberg J, Davies C, Unemo M, Nicholas RA. 2009. Genetics of chromosomally mediated intermediate resistance to ceftriaxone and cefixime in Neisseria gonorrhoeae. Antimicrob Agents Chemother 53:3744–3751. doi: 10.1128/AAC.00304-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Olesky M, Zhao S, Rosenberg RL, Nicholas RA. 2006. Porin-mediated antibiotic resistance in Neisseria gonorrhoeae: ion, solute, and antibiotic permeation through PIB proteins with penB mutations. J Bacteriol 188:2300–2308. doi: 10.1128/JB.188.7.2300-2308.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Unemo M, Golparian D, Nicholas R, Ohnishi M, Gallay A, Sednaoui P. 2012. High-level cefixime- and ceftriaxone-resistant Neisseria gonorrhoeae in France: novel penA mosaic allele in a successful international clone causes treatment failure. Antimicrob Agents Chemother 56:1273–1280. doi: 10.1128/AAC.05760-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tomberg J, Fedarovich A, Vincent LR, Jerse AE, Unemo M, Davies C, Nicholas RA. 2017. Alanine 501 mutations in penicillin-binding protein 2 from Neisseria gonorrhoeae: structure, mechanism, and effects on cephalosporin resistance and biological fitness. Biochemistry 56:1140–1150. doi: 10.1021/acs.biochem.6b01030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tomberg J, Unemo M, Davies C, Nicholas RA. 2010. Molecular and structural analysis of mosaic variants of penicillin-binding protein 2 conferring decreased susceptibility to expanded-spectrum cephalosporins in Neisseria gonorrhoeae: role of epistatic mutations. Biochemistry 49:8062–8070. doi: 10.1021/bi101167x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tomberg J, Unemo M, Ohnishi M, Davies C, Nicholas RA. 2013. Identification of amino acids conferring high-level resistance to expanded-spectrum cephalosporins in the penA gene from Neisseria gonorrhoeae strain H041. Antimicrob Agents Chemother 57:3029–3036. doi: 10.1128/AAC.00093-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kubanova AA, Kubanov AA, Koshushnaya OS, Vorobev DV, Solomka VS, Frigo NV. 2014. The role of some individual amino acid substitutions in penicillin-binding protein (PBP2) of Neisseria gonorrhoeae in the emergence of resistance to ceftriaxone. Mol Biol 48:858–863. doi: 10.1134/S0026893314060119. [DOI] [PubMed] [Google Scholar]
- 45.Takahata S, Senju N, Osaki Y, Yoshida T, Ida T. 2006. Amino acid substitutions in mosaic penicillin-binding protein 2 associated with reduced susceptibility to cefixime in clinical isolates of Neisseria gonorrhoeae. Antimicrob Agents Chemother 50:3638–3645. doi: 10.1128/AAC.00626-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Barry PM, Klausner JD. 2009. The use of cephalosporins for gonorrhea: the impending problem of resistance. Expert Opin Pharmacother 10:555–577. doi: 10.1517/14656560902731993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sawatzky P, Liu G, Dillon JAR, Allen V, Lefebvre B, Hoang L, Tyrrell G, Van Caeseele P, Levett P, Martin I. 2015. Quality assurance for antimicrobial susceptibility testing of Neisseria gonorrhoeae in Canada, 2003 to 2012. J Clin Microbiol 53:3646–3649. doi: 10.1128/JCM.02303-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sawatzky P, Martin I, Galarza P, Carvallo MET, Araya Rodriguez P, Cruz OMS, Hernandez AL, Martinez MF, Borthagaray G, Payares D, Moreno JE, Chiappe M, Corredor AH, Thakur SD, Dillon J. 2018. Quality assurance for antimicrobial susceptibility testing of Neisseria gonorrhoeae in Latin American and Caribbean countries, 2013–2015. Sex Transm Infect 94:479–482. doi: 10.1136/sextrans-2017-053502. [DOI] [PubMed] [Google Scholar]
- 49.Demczuk W, Lynch T, Martin I, Van Domselaar G, Graham M, Bharat A, Allen V, Hoang L, Lefebvre B, Tyrrell G, Horsman G, Haldane D, Garceau R, Wylie J, Wong T, Mulvey MR. 2015. Whole-genome phylogenomic heterogeneity of Neisseria gonorrhoeae isolates with decreased cephalosporin susceptibility collected in Canada between 1989 and 2013. J Clin Microbiol 53:191–200. doi: 10.1128/JCM.02589-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Grad YH, Harris SR, Kirkcaldy RD, Green AG, Marks DS, Bentley SD, Trees D, Lipsitch M. 2016. Genomic epidemiology of gonococcal resistance to extended-spectrum cephalosporins, macrolides, and fluoroquinolones in the United States, 2000–2013. J Infect Dis 214:1579–1587. doi: 10.1093/infdis/jiw420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wind CM, de Vries E, Schim van der Loeff MF, van Rooijen MS, van Dam AP, Demczuk WHB, Martin I, de Vries HJC. 2017. Decreased azithromycin susceptibility of Neisseria gonorrhoeae isolates in patients recently treated with azithromycin. Clin Infect Dis 65:37–45. doi: 10.1093/cid/cix249. [DOI] [PubMed] [Google Scholar]
- 52.Peterson SW, Martin I, Demczuk W, Hoang L, Wylie J, Lefebvre B, Labbé AC, Naidu P, Haldane D, Mulvey MR. 2018. A Comparison of real-time polymerase chain reaction assays for the detection of antimicrobial resistance markers and sequence typing from clinical nucleic acid amplification test samples and matched Neisseria gonorrhoeae culture. Sex Transm Dis 45:92–95. doi: 10.1097/OLQ.0000000000000707. [DOI] [PubMed] [Google Scholar]
- 53.Clinical and Laboratory Standards Institute. 2017. Performance standards for antimicrobial susceptibility testing: 27th informational supplement. CLSI document M100-S27. Clinical and Laboratory Standards Institute, Wayne, PA. [Google Scholar]
- 54.World Health Organization. 2012. Global action plan to control the spread and impact of antimicrobial resistance in Neisseria gonorrhoeae. World Health Organization, Geneva, Switzerland. [Google Scholar]
- 55.Centers for Disease Control and Prevention (CDC). 2018. Sexually transmitted disease surveillance 2017. Centers for Disease Control and Prevention, Atlanta, GA. [Google Scholar]
- 56.Triola MF, Goodman WM, Law R. 2002. Elementary statistics (2nd Canadian ed). Pearson Education Canada, Inc, Toronto, Ontario, Canada. [Google Scholar]
- 57.Parikh R, Mathai A, Parikh S, Chandra Sekhar G, Thomas R. 2008. Understanding and using sensitivity, specificity and predictive values. Indian J Ophthalmol 56:45–50. doi: 10.4103/0301-4738.37595. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.