Oral fosfomycin trometamol is licensed as a single oral dose for the treatment of uncomplicated urinary tract infections, with activity against multidrug-resistant uropathogens. The impact of interindividual variability in urinary concentrations on antimicrobial efficacy, and any benefit of giving multiple doses, is uncertain.
KEYWORDS: PK/PD, antimicrobial resistance, fosfomycin, in vitro model, urinary tract infection
ABSTRACT
Oral fosfomycin trometamol is licensed as a single oral dose for the treatment of uncomplicated urinary tract infections, with activity against multidrug-resistant uropathogens. The impact of interindividual variability in urinary concentrations on antimicrobial efficacy, and any benefit of giving multiple doses, is uncertain. We therefore performed pharmacodynamic profiling of oral fosfomycin, using a dynamic bladder infection in vitro model, to assess high and low urinary exposures following a single oral dose and three repeat doses given every 72 h, 48 h, and 24 h against 16 clinical isolates with various MICs of fosfomycin (8 Escherichia coli, 4 Enterobacter cloacae, and 4 Klebsiella pneumoniae isolates). Baseline fosfomycin high-level-resistant (HLR) subpopulations were detected prior to drug exposure in half of the isolates (2 E. coli, 2 E. cloacae, and 4 K. pneumoniae isolates; proportion, 1 × 10−5 to 5 × 10−4% of the total population). Fosfomycin exposures were accurately reproduced compared to mathematical modeling (linear regression slope, 1.1; R2, 0.99), with a bias of 3.8% ± 5.7%. All 5/5 isolates with MICs of ≤1 μg/ml had no HLR and were killed, whereas 8/11 isolates with higher MICs regrew regardless of exposure to high or low urinary concentrations. A disk diffusion zone of <24 mm was a better predictor for baseline HLR and regrowth. Administering 3 doses with average exposures provided very limited additional kill. These results suggest that baseline heteroresistance is important for treatment response, while increased drug exposure and administering multiple doses may not be better than standard single-dose fosfomycin therapy.
INTRODUCTION
Fosfomycin trometamol is an old, off-patent oral antibiotic, recommended as a single 3-g dose as a first-line treatment in international guidelines for the treatment of uncomplicated urinary tract infections (uUTIs) (1–3). Surveillance reports demonstrate high rates of fosfomycin susceptibility, even among emergent multidrug-resistant (MDR) uropathogens (4–8). In the era of rising antimicrobial resistance seen globally, there is renewed interest in fosfomycin as an attractive therapeutic option (9–14).
High rates of fosfomycin susceptibility have been reported in many countries, with a 2016 systematic review demonstrating fosfomycin susceptibilities among extended-spectrum-β-lactamase (ESBL)-producing isolates of 95.1% for Escherichia coli and 83.8% for Klebsiella pneumoniae (15). Clinical efficacy, however, has been more variable. Although earlier clinical trials reported a treatment efficacy for uUTIs ranging from 77.2% to 95% (16), more recently, a retrospective study (17) found a microbiological cure rate of only 59% in the treatment of MDR uropathogens. Moreover, in a prospective randomized clinical trial (18), clinical resolution was achieved in 58% of patients receiving fosfomycin, compared to 70% receiving nitrofurantoin. This latest study raised doubts about whether a single 3-g dose reached adequately durable urine concentrations and the role of alternative fosfomycin prescribing practices, such as multiple doses given every 3 days (19, 20).
The original dosing studies for oral fosfomycin lacked the modern methods used today for the licensing of new antimicrobial agents. Supporting evidence for the efficacy of single-dose therapy was largely based upon pharmacokinetic (PK) reports of urinary concentrations of fosfomycin remaining greater than 128 mg/liter for 24 to 48 h (21). Several off-label dosing practices have since emerged, with some publications recommending giving 3 doses every 2 to 3 days and other studies recommending daily dosing, with emphasis on infections caused by MDR uropathogens and a longer duration of therapy following renal transplantation (17, 22–29). The efficacy of multidose oral fosfomycin has also been examined by population PK modeling (30). Repeat daily dosing of oral fosfomycin, however, has been associated with higher rates of diarrhea (31) and lacks detailed microbiological or clinical evidence for superiority over single-dose therapy.
Many studies evaluating the urine concentrations of fosfomycin after oral dosing have demonstrated significant variability between subjects (21, 31–37). Fosfomycin is primarily eliminated by the kidneys, with clearance approximating glomerular filtration. However, the resulting urinary concentrations in healthy populations have a wide range of values. As such, key urinary PK parameters, such as the peak urinary concentration (Cmax), the time of Cmax (tmax), and the duration of time that urinary concentrations remain above the MIC of the uropathogen, can be dramatically different. This ultimately creates uncertainty regarding what PK/pharmacodynamic (PD) index can best predict treatment efficacy.
To help address the uncertainty around fosfomycin efficacy in the context of varying urinary concentrations and multiple doses, we performed PD profiling of fosfomycin using a dynamic bladder infection in vitro model against common uropathogens.
RESULTS
Fosfomycin susceptibility of bacterial strains.
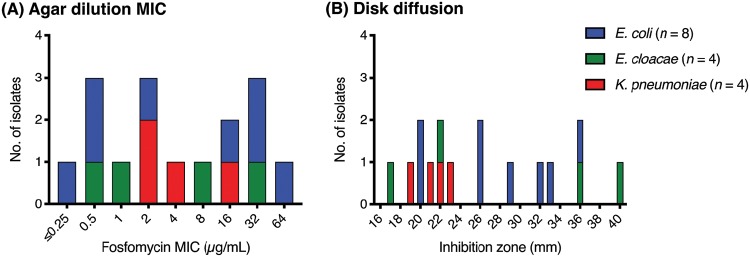
A total of 16 contemporary, Gram-negative uropathogens with varying MICs for fosfomycin were included in this study. Using agar dilution, the MIC values for eight E. coli isolates ranged from ≤0.25 to 64 μg/ml, those for four Enterobacter cloacae isolates ranged from 0.5 to 32 μg/ml, and those for four K. pneumoniae isolates ranged from 2 to 16 μg/ml (Fig. 1A). Using the disk diffusion susceptibility method, inhibition zone diameters ranged from 20 to 36 mm for E. coli, 17 to 40 mm for E. cloacae, and 19 to 23 mm for K. pneumoniae (Fig. 1B). All E. coli isolates were classified as susceptible by applying Clinical and Laboratory Standards Institute (CLSI) breakpoints (38), with no interpretations provided for E. cloacae and K. pneumoniae. Applying the European Committee on Antimicrobial Susceptibility Testing (EUCAST) Enterobacterales breakpoints (39), only one E. coli isolate was classified as resistant by MIC testing. The EUCAST provides disk diffusion susceptibility breakpoints for E. coli only (susceptible [S] at ≥24 mm), by which two isolates were classified as resistant. For the other species, all K. pneumoniae isolates and 2 of 4 E. cloacae isolates had inhibition diameters of less than 24 mm, without provided interpretation. We also assessed for baseline fosfomycin heteroresistance and found that two E. coli, two E. cloacae, and all K. pneumoniae isolates had evidence of high-level-resistant (HLR) subpopulations at a percentage of the total population from 1 × 10−5 to 5 × 10−4% (Table 1). None of the isolates with an agar dilution MIC of ≤1 μg/ml or a disk diffusion inhibition zone of >24 mm had a detectable HLR subpopulation at baseline. Of the isolates with inhibition zones of <24 mm, 8/8 had an HLR subpopulation, whereas of isolates with MICs of >1 μg/ml, 8/11 had an HLR subpopulation (2 E. coli, 2 E. cloacae, and 4 K. pneumoniae isolates). The 3 isolates with MICs of >1 μg/ml without HLR (MICs of 2, 32, and 64 μg/ml) were all E. coli isolates. Note that 4/4 K. pneumoniae isolates had MICs of ≥2 μg/ml, and all had detectable HLR.
FIG 1.
Baseline fosfomycin susceptibility of test isolates. (A) MIC testing was performed in triplicate by agar dilution. (B) Disk diffusion was performed using a FOT200 disk (Oxoid Ltd./Thermo Fisher Scientific, UK). E. coli ATCC 25922 was used as a quality control organism.
TABLE 1.
Isolate characteristics and response to urinary fosfomycin exposuresb
| Strain | Fosfomycin susceptibility |
Growth control (baseline HLR [%]) | Postexposure outcomea (bacterial count [log10 CFU/ml]/MIC [μg/ml]; HLR proportion) |
||||||
|---|---|---|---|---|---|---|---|---|---|
| MIC (μg/ml) | Disk diffusion (mm) | Single dose |
3 doses |
||||||
| Avg Cmax | Low Cmax | High Cmax | Every 72 h | Every 48 h | Every 24 h | ||||
| E. coli | |||||||||
| 41 | ≤0.25 | 33 | − | − | − | − | − | − | − |
| 11 | 0.5 | 36 | − | − | − | − | − | − | − |
| 39 | 0.5 | 32 | − | − | − | − | − | − | − |
| 12620 | 2 | 26 | − | − | − | − | − | − | − |
| 1016 | 16 | 20 | 2E−04 | 9.5/256; HLR +++ | 9.0/>1,024; HLR +++ | 9.0/>1,024; HLR +++ | 9.6/>1,024; HLR +++ | 9.5/>1,024; HLR +++ | 9.6/>1,024; HLR +++ |
| 1231 | 32 | 20 | 2E−04 | 9.5/>1,024; HLR +++ | 9.1/>1,024; HLR +++ | 9.3/>1,024; HLR +++ | 9.5/>1,024; HLR +++ | 9.3/>1,024; HLR +++ | 9.3/>1,024; HLR +++ |
| 4807 | 32 | 29 | − | − | − | − | − | − | − |
| 4757 | 64 | 26 | − | − | − | 6.3/64; no HLR | − | 7.5/64; HLR + | − |
| E. cloacae | |||||||||
| 35166 | 0.5 | 36 | − | − | − | − | − | − | − |
| 94 | 1 | 40 | − | − | − | − | − | − | − |
| 21 | 8 | 22 | 2E−05 | 9.5/>1,024; HLR +++ | 8.4/8; HLR +++ | 9.5/32; HLR ++ | 8.9/16; HLR +++ | 8.6/>1,024; HLR +++ | 6.6/16; no HLR |
| 32 | 32 | 17 | 5E−04 | 9.5/>1,024; HLR +++ | 9.4/>1,024; HLR +++ | 9.9/>1,024; HLR +++ | 9.7/>1,024; HLR +++ | 9.5/>1,024; HLR +++ | 9.4/>1,024; HLR +++ |
| K. pneumoniae | |||||||||
| 34672 | 2 | 23 | 1E−05 | 9.3/>1,024; HLR +++ | 7.3/4; HLR +++ | 9.6/1,024; HLR + | 9.5/>1,024; HLR +++ | 8.8/512; HLR ++ | − |
| 31865 | 2 | 22 | 2E−04 | 9.4/256; HLR ++ | 3.9/2; no HLR | 7.5/32; no HLR | − | 6.8/2; no HLR | 5.9/2; no HLR |
| 55 | 4 | 19 | 1E−04 | 6.9/4; no HLR | 4.6/8; no HLR | 9.6/>1,024; HLR + | 9.4/>1,024; HLR +++ | 9.5/512; HLR +++ | 9.5/512; HLR + |
| 52 | 16 | 21 | 5E−04 | 9.2/>1,024; HLR +++ | 6.8/16; no HLR | 2.8/256; no HLR | 9.6/16; HLR ++ | 5.2/16; no HLR | 9.2/1,024; HLR ++ |
Postexposure outcome was determined as no growth or the bacterial count measured at the final time point (72 h after the last administered fosfomycin dose). The fosfomycin MIC was reassessed on the total population regrowth (values presented in boldface type); dark gray shading highlights a >2-log2 rise in the MIC, and light gray shading highlights growth without a significant rise in MIC. The HLR proportion of the total population is presented as greater than 1% (+++), between 0.01 and 1% (++), or less than 0.01% (+). MIC testing of all HLR subpopulations confirmed MICs of ≥1,024 μg/ml after subculturing on TSB.
− indicates not detected or no growth.
Fosfomycin exposure in the bladder infection in vitro model.
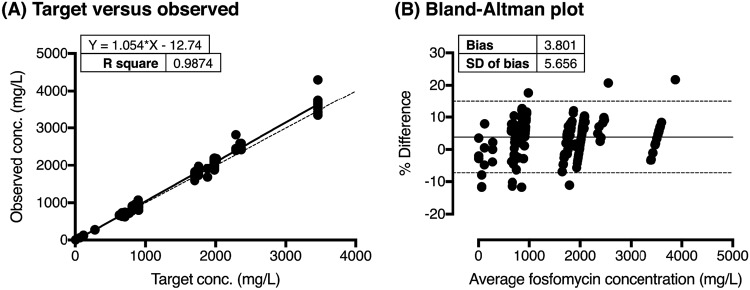
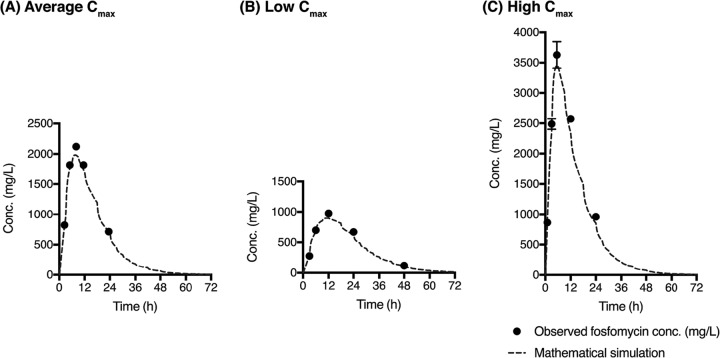
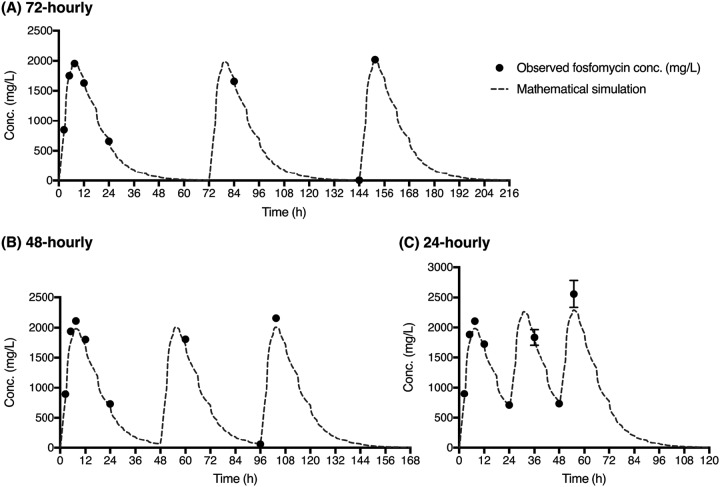
We used an adaptation of a previously described in vitro model (40). Observed in vitro concentrations closely matched the target concentration of each of the single and multidose fosfomycin exposure simulations. The slope of the linear regression line was equal to 1.1 (R2, 0.99), with a bias of 3.8% ± 5.7% (Fig. 2). There was minimal intercompartment variation, with an average relative standard deviation of 3.1% ± 1.9%. Following a single fosfomycin dose, targeting an average urinary exposure, the measured Cmax was 2,122.2 ± 46.0 mg/liter, whereas for the low-Cmax exposure, it was 975.7 ± 34.8 mg/liter, and for the high-Cmax exposure, it was 3,628.2 ± 218.4 mg/liter (Fig. 3). Following the multidose experiments, fosfomycin concentrations were accurately reproduced following dosing schedules every 72, 48, and 24 h (Fig. 4).
FIG 2.
Relationship between the observed and target fosfomycin concentrations. (A) Accuracy of observed fosfomycin concentrations compared with the target with linear regression (solid line) and y equal to x (dashed line). (B) Bland-Altman plot of the percent differences of the observed and target measurements (y axis) and the averages of the two measurements (x axis), presented with the bias (solid line) and 95% limits of agreement (dotted lines).
FIG 3.
Single-dose fosfomycin urinary concentrations. Fosfomycin was administered as a single dose, simulating an oral 3-g dose with average exposure (A), low urinary Cmax (B), and high urinary Cmax (C). The average measured fosfomycin concentrations are overlaid on the target concentration-time curves (dashed line). Note that the mathematically simulated urinary concentration curves do not demonstrate a smooth drug elimination phase due to the dynamic fluid shifts that occur after each voiding cycle of the bladder compartment.
FIG 4.
Multidose fosfomycin urinary concentrations. Shown are data for simulations of three 3-g oral doses of fosfomycin administered every 72 h (A), 48 h (B), and 24 h (C). The average measured fosfomycin concentrations are overlaid on the target concentration-time curve (dashed lines). Note that the mathematically simulated urinary concentration curves do not demonstrate a smooth drug elimination phase due to the dynamic fluid shifts that occur after each voiding cycle of the bladder compartment.
Impact of variable urinary fosfomycin concentrations on treatment response.
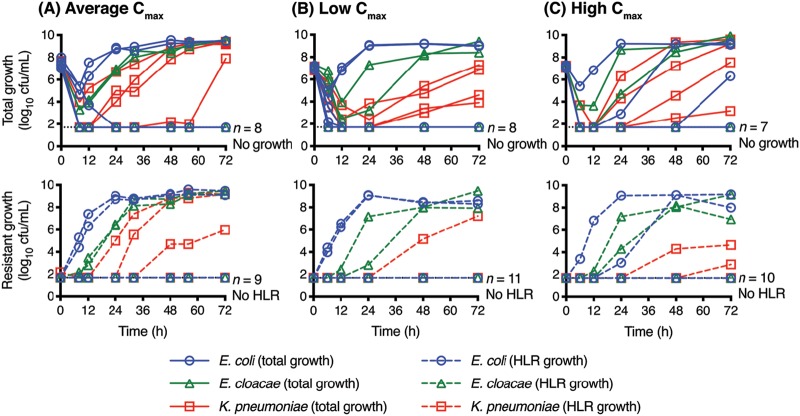
Given the variability observed in urinary fosfomycin concentrations in patients after a single oral dose, we tested the treatment efficacy of average, low, and high urinary fosfomycin Cmax values using our established dynamic bladder infection model (Fig. 5 and Table 1). Irrespective of the urinary fosfomycin concentration, the same bacterial isolates regrew over a 72-h period (two E. coli, two E. cloacae, and all K. pneumoniae isolates). For the majority of clinical isolates, following exposure to different urinary concentrations, regrowth was associated with baseline heteroresistance identified within the starting bacterial population (Table 1). Low-level-resistant (LLR) regrowth (growth on Mueller-Hinton II agar [MHA] with 64 mg/liter) coincided with the detection of high-level-resistant (HLR) growth (growth on MHA with 512 mg/liter). All 5/5 isolates with MICs of ≤1 μg/ml were killed, whereas isolates with higher MICs had mixed behavior depending on the presence of baseline HLR. Only one isolate with an inhibition zone of >24 mm (E. coli 4757) regrew, and this occurred only following high-Cmax exposure, without the emergence of HLR. All K. pneumoniae isolates regrew after all exposures, although the emergence of resistance during regrowth was lowest following exposure to a low Cmax.
FIG 5.
Growth outcome following a single fosfomycin dose. Shown are data for simulated 3-g oral doses of fosfomycin with average exposure (A), low Cmax (B), and high Cmax (C). Total growth and high-level-resistant (HLR) growth are presented for all 16 isolates: 8 E. coli isolates, 4 E. cloacae isolates, and 4 K. pneumoniae isolates. The limit of detection was 50 CFU/ml. The number of isolates at the final time point without growth or emergence of HLR is indicated. See Table 1 for isolate-specific details.
Impact of multiple doses of fosfomycin on treatment response.
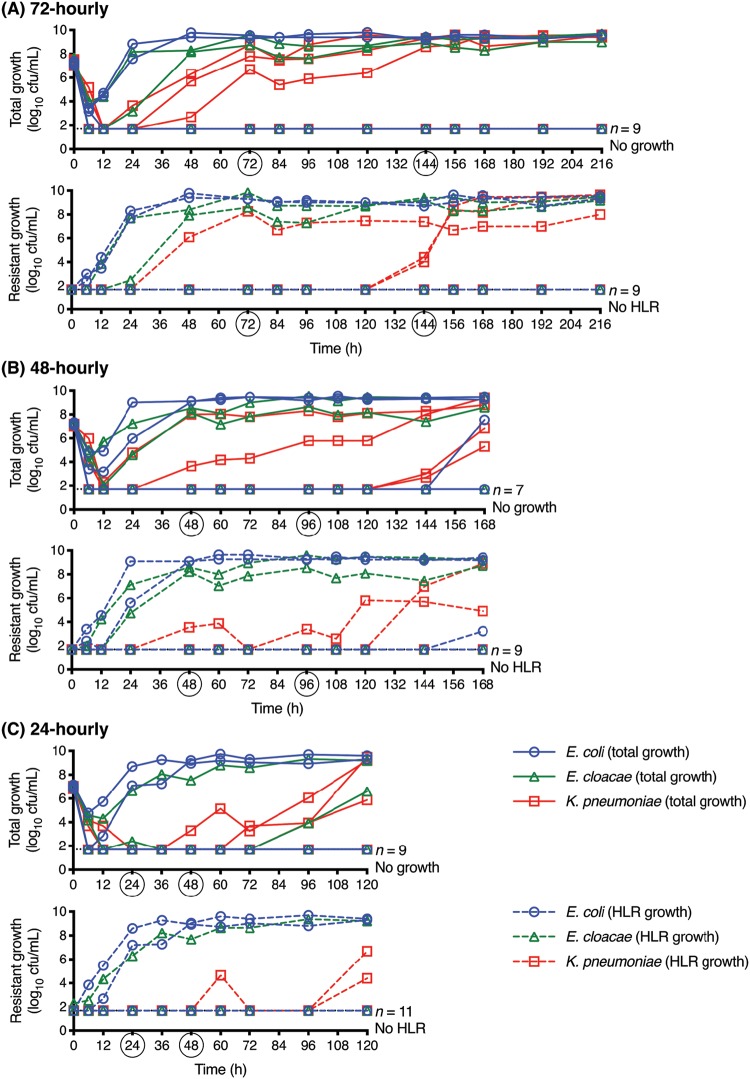
When 3 doses of fosfomycin were administered at different frequencies (every 72 h [q72], q48, and q24), pathogen kill was not uniformly enhanced (Table 1 and Fig. 6). Across all exposure experiments, the same five E. coli and two E. cloacae isolates were killed. E. coli 4757 (baseline MIC of 64 μg/ml) had regrowth detected at the final sampling time point, after 3 doses given q48, without any rise in the postexposure total population MIC. E. coli strains 1016 and 1231 and E. cloacae strain 32 regrew with emergence of HLR in all exposure experiments. Similarly, E. cloacae 21 also regrew following all exposures but had a variable emergence of HLR, with and without rises in the postexposure fosfomycin MIC. All 4 K. pneumoniae isolates tended to regrow following all exposure experiments (except K. pneumoniae 31865 after 3 doses q72 and K. pneumoniae 34672 after 3 doses q24). LLR regrowth coincided with HLR. Similar to that observed following varying urinary concentrations after a single dose, isolates with a preexposure MIC of >1 μg/ml had variable regrowth, whereas a disk diffusion inhibition zone of <24 mm and the presence of an HLR subpopulation at baseline better predicted regrowth.
FIG 6.
Growth outcome following multiple fosfomycin doses. Shown are data for three simulated 3-g oral doses of fosfomycin given every 72 h (A), 48 h (B), and 24 h (C). Total growth and high-level-resistant (HLR) growth are presented for all 16 isolates: 8 E. coli isolates, 4 E. cloacae isolates, and 4 K. pneumoniae isolates. The limit of detection was 50 CFU/ml. The number of isolates at the final time point without growth or emergence of HLR is indicated. The timing of the second and third doses of fosfomycin is indicated by circles on the x axis. See Table 1 for isolate-specific details.
DISCUSSION
Understanding how to optimize oral fosfomycin therapy, especially when other antimicrobial options are limited due to resistance or unfavorable safety profiles, is paramount for improving clinical efficacy. However, the impact on treatment efficacy of interpersonal variability in fosfomycin urinary concentrations and the benefit of off-label, multidose prescribing are uncertain. Here, we showed that variability in urinary exposures following a single 3-g oral dose did not correlate with any clear change in efficacy. Furthermore, increasing the total drug exposure by administering multiple doses failed to provide any additional suppression of regrowth in the majority of isolates compared to standard single-dose therapy. In our study, the efficacy of fosfomycin appeared to be influenced more by the baseline characteristics of the infecting pathogen than by variations in urinary drug exposure or dosing frequency. Baseline high-level heteroresistance and bacterial species were found to be more predictive of regrowth. Although isolates with an agar dilution MIC of ≤1 μg/ml were reliably killed, isolates with higher MICs demonstrated mixed behavior depending on the presence of HLR, in particular for E. coli isolates that were killed despite high MICs of up to 64 μg/ml. A disk diffusion zone of <24 mm, however, better predicted the presence of baseline HLR and regrowth after fosfomycin exposure. In addition, emergence of resistance was often detected early, within the first 24 h, such that repeat doses of fosfomycin given after that time had very little impact on the overall bacterial density. This rapid emergence of resistance negated the benefit of giving multiple doses and particularly questions the role of delaying repeat doses by 48 or 72 h. Overall, the efficacy of fosfomycin against our K. pneumoniae isolates appeared limited, regardless of the baseline MIC or drug exposure, a finding supported by other studies (40–42).
Treating physicians may look to increase urinary fosfomycin exposure for a number of reasons: in anticipation of the variability in urinary drug concentrations, limited alternative antimicrobial options, vulnerable patient groups (such as after kidney transplantation) (43, 44), urinary tract infections (UTIs) in male patients, E. coli isolates with elevated fosfomycin MIC values, and for the treatment of other species of Gram-negative uropathogens. Concerningly, discrepancies have been reported between different fosfomycin susceptibility methods (45–48), and the gold-standard MIC method by agar dilution may not be the best predictor of clinical efficacy (49). Furthermore, in one study, patients with UTIs with carbapenem-resistant K. pneumoniae had a microbiological cure rate of only 46% when treated with fosfomycin, despite an in vitro susceptibility of 92% (17). Our data suggest that baseline fosfomycin heteroresistance was more predictive of the treatment response in our bladder infection model, and if present, regrowth with resistant populations was almost universal irrespective of the modeled urinary concentrations or 3-dose frequency. This finding was supported by a clinical review of fosfomycin treatment in MDR UTIs, which found no association of treatment outcomes with the MIC of fosfomycin or the number of doses received (14).
Following a single-fosfomycin-dose exposure, there was no progressive improvement in efficacy from low to high urinary fosfomycin concentrations. Given that baseline resistant subpopulations had MICs of fosfomycin of >1,024 μg/ml, even with high urinary Cmax exposures, there would likely be a minimal time that concentrations were maintained above the mutant prevention concentration (MPC) in order to suppress growth. Similarly, the reduced emergence of resistance seen among the Klebsiella strains following low urinary concentrations may highlight the left side of the inverted U-shaped pattern that, in general, describes the relationship between exposure and emergence of resistance. In clinical practice, the inoculum size, duration of therapy, and activity of the immune system would impact the shape of this curve (50). In this setting, a prolonged treatment duration can make it increasingly difficult to suppress the amplification of the resistant subpopulation.
Compared to serum antimicrobial concentration measurements, the assessment of urinary concentrations has greater complexity. Although cumulative urinary measurements of an antimicrobial provide an assessment of the urinary recovery of the administered dose, the actual concentration measured in a voided urine sample at any one time is greatly impacted by individual behaviors, such as fluid intake, urine output, and voiding pattern. Because of these variabilities in observations, there can be uncertainty regarding which urinary PK/PD targets are important for clinical efficacy. Oral fosfomycin achieves urinary concentrations that are 100 to 1,000 times higher than the serum concentrations (21, 31–33). Such high urinary antimicrobial concentrations are essential for efficacy. In a mouse model, systemically administered therapy reaching only the bladder tissue (and not the bladder lumen) was found to be insufficient for bacterial eradication (51). However, optimizing clinical cure of UTIs by targeting only high antimicrobial urinary concentrations negates the other important nonantimicrobial factors that can also assist in bacterial clearance, such as increased fluid intake to promote increased urine output and dilution of bacteria in the bladder and high-volume and frequent urination to assist in bacterial clearance. However, such urokinetic strategies would concurrently reduce antimicrobial concentrations in the bladder.
An advantage of the bladder infection in vitro model used in this study is the application of a dynamic UTI simulation, which applies normal urodynamics and accurate urinary fosfomycin exposures, in which experiments with multiple different pathogens can be run for prolonged periods of time to reflect clinical dosing regimens. Although this study applied PK data from a single healthy-volunteer study (32), which reported relatively high urinary concentrations compared to those in other recent studies (31, 33), our single-dose experiments examined 1 standard deviation above and below the reported average to account for the observed interpersonal variability. The main limitation of the in vitro model, as with all in vitro models, is whether the pathogen response demonstrated can be translated to, and be predictive of, the real in vivo situation. Importantly, the in vitro model lacks bladder tissue architecture and host immune responses. The use of standard laboratory medium, Mueller-Hinton II broth (MHB) supplemented with glucose-6-phosphate (G6P), may also not reflect fosfomycin activity and pathogen growth in urine. Furthermore, bacterial density measurements collected at the time of the peak in vitro fosfomycin concentration may underestimate growth due to antibiotic carryover being addressed by serial dilutions only, although previous reports have demonstrated no difference between dilution and washing (52).
Fosfomycin is a very useful antimicrobial for uUTIs. Reassuringly, variabilities in individual urinary fosfomycin exposures seem to have a minimal impact. Given the current limitations of fosfomycin susceptibility methods and clinical breakpoints, more work is required to accurately identify isolates with a high likelihood of clinical success. Our in vitro data, however, provide caution for the off-label practice of administering multiple oral doses of fosfomycin. It is uncertain, however, whether repeat doses of fosfomycin could be beneficial in more complex infection syndromes, such as an ascending infection leading to pyelonephritis (53), or infections in difficult sites, such as the prostate and in biofilms (54, 55). We also await the results of the FORECAST study (56), which will examine the treatment of complicated UTIs with an intravenous (i.v.)-to-oral switch, comparing ciprofloxacin with fosfomycin administered daily to complete a total of 10 days of therapy. Furthermore, to build upon the clinical study by Huttner et al. (18), a randomized controlled trial examining the treatment of uUTI comparing nitrofurantoin at 100 mg twice daily for 5 days (macrocrystal-monohydrate formulation) versus 3 to 5 daily doses of 3 g fosfomycin would be a valuable clinical study to guide treatment recommendations. An assessment of baseline fosfomycin heteroresistance in the identified uropathogens would also be an important adjunct to standard susceptibility testing.
MATERIALS AND METHODS
Antibiotic and media.
Fosfomycin (Fomicyt; InfectoPharm, Germany) was reconstituted to a concentration of 50,000 mg/liter and used in the bladder infection in vitro model and for medium production. Cation-adjusted MHB (Becton, Dickinson [BD], USA) supplemented with G6P (catalog number G7879-5G; Sigma-Aldrich, USA) at a concentration of 25 mg/liter was used as the liquid medium in the in vitro model. Trypticase soy agar (TSA) containing 5% sheep blood (BD) was used for subculturing isolates from a freezer stock. Mueller-Hinton II agar (MHA) (BD) was used for the quantification of bacterial density. Emergence of resistance was assessed by plating on MHA with 64 mg/liter (low-level resistance [LLR]) and 512 mg/liter (high-level resistance [HLR]) of fosfomycin. Fosfomycin was also added to MHA (0.25 to 1,024 mg/liter) for agar dilution susceptibility testing. All media to which fosfomycin was added also contained 25 mg/liter G6P.
Bacterial strains and in vitro susceptibility testing.
Sixteen clinical isolates were selected to reflect a range of baseline fosfomycin MIC values, originating from The Netherlands (57). Isolates included 8 E. coli, 4 E. cloacae, and 4 K. pneumoniae isolates. Species identification was confirmed by matrix-assisted laser desorption ionization–time of flight mass spectrometry (MALDI-TOF MS) (Bruker Daltonik GmbH, Germany). Fosfomycin susceptibility was determined by agar dilution (in triplicate, presented as the median value) according to the reference methodology (58) and disk diffusion using a FOT200 disk (Oxoid Ltd./Thermo Fisher Scientific, UK). E. coli ATCC 25922 was used as the quality control organism. The baseline proportion of an HLR subpopulation was assessed from a culture grown overnight in drug-free MHB with G6P and plated onto MHA containing 512 mg/liter of fosfomycin, with the HLR bacterial density divided by the total-growth density on drug-free MHA.
Dynamic bladder infection in vitro model.
In short, the dynamic bladder infection in vitro model simulates dynamic urinary fosfomycin exposure, on a 1:16 scale to in vivo, to 16 independent bladder compartments (see Fig. S1 in the supplemental material). Fosfomycin is administered into the intestinal compartment, absorbed into the circulatory compartment, and eliminated into each bladder compartment in parallel. By applying drug distribution PK equations (Fig. S2) (59), the variables of the initial fosfomycin dose, compartment volumes, and flow rates were modified in order to simulate different urinary exposures following a single oral dose and the dynamic cumulative exposure following multiple doses. Test isolates were added to each bladder compartment, at an inoculum of 107 CFU, to provide a total number of bacteria equivalent to that expected in human infections (i.e., >105 CFU/ml in an average 250-ml void). The remainder of the starting inoculum was incubated overnight as a drug-free growth control from which an assessment of baseline HLR was performed, as described previously. Following exposure to fosfomycin within the in vitro model, pathogen kill and emergence of resistance were assessed by quantitative cultures on drug-free and fosfomycin-containing MHA (64 mg/liter and 512 mg/liter). Single-dose experiments were run for 72 h. Multidose experiments were run for an additional 72 h after the third dose of fosfomycin.
Fosfomycin dosing schedules and simulated urinary exposures.
Given the large recognized inter- and intrasubject variability in urinary fosfomycin concentrations following a single 3-g oral dose, average-, low-, and high-exposure situations were simulated, applying data from a healthy-volunteer PK study, which reported an average urinary fosfomycin Cmax of 1,982.0 ± 1,257.4 mg/liter (32). When targeting this average urinary exposure, the model was designed to deliver a blood elimination half-life of 6.9 h, urinary Cmax at 7.5 h, and urinary concentrations maintained at >128 mg/liter for at least 40 h. In order to simulate low urinary exposure, which could occur in vivo in the setting of increased fluid intake and increased urine output, a Cmax of 898 mg/liter was targeted, representing 1 standard deviation below the mean reported value. The same blood elimination half-life was targeted, with the in vitro flow rate and volumes of the gastrointestinal and circulatory compartments increased. For a high-urinary-exposure simulation, which could occur in the setting of reduced fluid intake and a decreased urine output volume, a urinary Cmax of 3,454 mg/liter at 5.5 h was targeted, representing 1 standard deviation above the mean. The same blood elimination half-life was again targeted, with the in vitro flow rate and volumes of the gastrointestinal and circulatory compartments reduced. The targeted total urinary fosfomycin exposure for the single-dose experiments were as follows: an average-exposure area under the concentration-time curve from 0 to 72 h (AUC0–72) of 36,941 mg · h/liter, reduced by 65.7% for the low-exposure experiment (24,284 mg · h/liter) and increased by 150.1% for the high-exposure experiment (55,457 mg · h/liter). To reflect different off-label oral dosing schedules commonly employed, 3 doses were administered either every 72, 48, or 24 h. All multidose experiments applied an average urinary exposure.
In vitro sample processing.
Samples for PK and PD assessments were taken directly from each bladder compartment at predetermined time points. Samples for fosfomycin concentration quantification, initially diluted 1:10 with saline when expected to fall outside the validated concentration range of the assay, were immediately frozen at −80°C until testing. Quantitative cultures for PD assessments were processed immediately, with bacterial density (CFU per milliliter) calculated at each time point. Specifically, medium from within each bladder compartment was sampled via a 3-way stopcock (BD) connected to the outflow tract and underwent serial 10-fold dilutions, of which 20 μl from each dilution was plated onto drug-free MHA and MHA containing 64 and 512 mg/liter of fosfomycin. The lower limit of detection was considered to be 50 CFU/ml, discounting nonviable growth such as pinpoint colonies or haze. All plates were incubated aerobically at 37°C for 16 to 20 h. Plates supplemented with fosfomycin were reincubated for a further 24 h.
Measurement of fosfomycin concentrations.
An ultraperformance liquid chromatography-tandem mass spectrometry (UPLC-MS/MS) method was used for the quantification of fosfomycin from PK samples collected from bladder compartments during each experiment. All bladder compartments were sampled during each experiment at the initial Cmax time point, providing an assessment of intercompartment variation. On all other occasions, three bladder compartments were sampled to provide representative concentration changes over time. For the single-dose experiments, samples were collected twice before and twice after the Cmax time point. Additionally, for the multidose experiments, samples were also collected 12 h after the second dose, and trough and peak samples were collected at around the 3rd dose. Observed concentrations were compared to target concentrations determined by the drug distribution equations (Fig. S2). Linear regression and Bland-Altman analysis were used to determine the accuracy of the observed concentrations compared to the target in terms of bias and precision. The UPLC-MS/MS method was validated for urine and plasma samples of fosfomycin (60), but additional tests confirmed its applicability for fosfomycin in MHB samples. The method was validated according to FDA guidelines (61) over a range of 0.75 to 375 mg/liter (R2, 0.9998). The lower limit of quantification was 0.75 mg/liter, and the lower limit of detection was 0.70 mg/liter. The method was found to be accurate and precise, with a maximum deviation of 5.0%. The stability of fosfomycin in MHB at 37°C for 72 h and stored at −80°C for at least 6 months was confirmed.
Supplementary Material
ACKNOWLEDGMENTS
We acknowledge the laboratory assistance of Carla Roodbol de Goeij (Department of Medical Microbiology and Infectious Diseases, Research and Development Unit, Erasmus Medical Centre) and of Alex Brouwer and Geert Springeling (Department of Experimental Medical Instrumentation, Erasmus Medical Centre) for their assistance in the in vitro equipment design and production.
This work was supported in part by the AIDA project LifeSciHealth Priority of the European Commission Seventh Framework Programme, FP7 (Preserving Old Antibiotics for the Future, grant number F3-2011-278348). I.J.A. was funded by an Australian Government Research Training Program scholarship (APP1114690) from the National Health and Medical Research Council of Australia. A.Y.P. and J.A.R. are in part funded through Australian National Health and Medical Research Council practitioner fellowships (APP1117940 and APP1117065, respectively).
J.W.M. has received research funding from Adenium, AstraZeneca, Basilea, Cubist, Polyphor, Roche, Eumedica, Basilea, VenatorX, AiCuris, Gilead, and Wockhardt. A.Y.P. has received research funding from MSD through an investigator-initiated research project. All other authors have no conflicts of interest to declare.
Footnotes
Supplemental material is available online only.
REFERENCES
- 1.Gupta K, Hooton TM, Naber KG, Wullt B, Colgan R, Miller LG, Moran GJ, Nicolle LE, Raz R, Schaeffer AJ, Soper DE, Infectious Diseases Society of America, European Society for Microbiology and Infectious Diseases. 2011. International clinical practice guidelines for the treatment of acute uncomplicated cystitis and pyelonephritis in women: a 2010 update by the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases. Clin Infect Dis 52:e103–e120. doi: 10.1093/cid/ciq257. [DOI] [PubMed] [Google Scholar]
- 2.Bonkat G, Bartoletti RR, Bruyère F, Cai T, Geerlings SE, Köves B, Schubert S, Wagenlehner F, Mezei T, Pilatz A, Pradere B, Veeratterapillay R. 2019. EAU guidelines on urological infections. European Association of Urology, Arnhem, The Netherlands: https://uroweb.org/guideline/urological-infections/#1. [Google Scholar]
- 3.Therapeutic Guidelines Limited. 2019. Acute cystitis in adults In eTG complete. Therapeutic Guidelines Limited, Melbourne, Australia: https://tgldcdp.tg.org.au/etgcomplete. [Google Scholar]
- 4.Mueller L, Cimen C, Poirel L, Descombes MC, Nordmann P. 2019. Prevalence of fosfomycin resistance among ESBL-producing Escherichia coli isolates in the community, Switzerland. Eur J Clin Microbiol Infect Dis 38:945–949. doi: 10.1007/s10096-019-03531-0. [DOI] [PubMed] [Google Scholar]
- 5.de Greeff SC, Mouton JW, Schoffelen AF, Verduin CM. 2019. NethMap 2019: consumption of antimicrobial agents and antimicrobial resistance among medically important bacteria in the Netherlands. RIVM report 2019-0038. National Institute for Public Health and the Environment, Bilthoven, The Netherlands: https://www.rivm.nl/bibliotheek/rapporten/2019-0038.pdf. [Google Scholar]
- 6.Quaegebeur A, Brunard L, Javaudin F, Vibet MA, Bemer P, Le Bastard Q, Batard E, Montassier E, EuroUTI 2010-2016 Study Group. 2019. Trends and prediction of antimicrobial susceptibility in urinary bacteria isolated in European emergency departments: the EuroUTI 2010-2016 study. J Antimicrob Chemother 74:3069–3076. doi: 10.1093/jac/dkz274. [DOI] [PubMed] [Google Scholar]
- 7.Karlowsky JA, Lagace-Wiens PRS, Adam HJ, Baxter MR, Laing NM, Walkty AJ, Zhanel GG. 2019. In vitro susceptibility of urinary Escherichia coli isolates to first- and second-line empirically prescribed oral antimicrobials: CANWARD surveillance study results for Canadian outpatients, 2007-2016. Int J Antimicrob Agents 54:62–68. doi: 10.1016/j.ijantimicag.2019.04.012. [DOI] [PubMed] [Google Scholar]
- 8.Falagas ME, Athanasaki F, Voulgaris GL, Triarides NA, Vardakas KZ. 2019. Resistance to fosfomycin: mechanisms, frequency and clinical consequences. Int J Antimicrob Agents 53:22–28. doi: 10.1016/j.ijantimicag.2018.09.013. [DOI] [PubMed] [Google Scholar]
- 9.Zowawi HM, Harris PN, Roberts MJ, Tambyah PA, Schembri MA, Pezzani MD, Williamson DA, Paterson DL. 2015. The emerging threat of multidrug-resistant Gram-negative bacteria in urology. Nat Rev Urol 12:570–584. doi: 10.1038/nrurol.2015.199. [DOI] [PubMed] [Google Scholar]
- 10.Flores-Mireles AL, Walker JN, Caparon M, Hultgren SJ. 2015. Urinary tract infections: epidemiology, mechanisms of infection and treatment options. Nat Rev Microbiol 13:269–284. doi: 10.1038/nrmicro3432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hawkey PM, Warren RE, Livermore DM, McNulty CAM, Enoch DA, Otter JA, Wilson APR. 2018. Treatment of infections caused by multidrug-resistant Gram-negative bacteria: report of the British Society for Antimicrobial Chemotherapy/Healthcare Infection Society/British Infection Association Joint Working Party. J Antimicrob Chemother 73:iii2–iii78. doi: 10.1093/jac/dky027. [DOI] [PubMed] [Google Scholar]
- 12.Falagas ME, Kastoris AC, Kapaskelis AM, Karageorgopoulos DE. 2010. Fosfomycin for the treatment of multidrug-resistant, including extended-spectrum beta-lactamase producing, Enterobacteriaceae infections: a systematic review. Lancet Infect Dis 10:43–50. doi: 10.1016/S1473-3099(09)70325-1. [DOI] [PubMed] [Google Scholar]
- 13.Sastry S, Clarke LG, Alrowais H, Querry AM, Shutt KA, Doi Y. 2015. Clinical appraisal of fosfomycin in the era of antimicrobial resistance. Antimicrob Agents Chemother 59:7355–7361. doi: 10.1128/AAC.01071-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Seroy JT, Grim SA, Reid GE, Wellington T, Clark NM. 2016. Treatment of MDR urinary tract infections with oral fosfomycin: a retrospective analysis. J Antimicrob Chemother 71:2563–2568. doi: 10.1093/jac/dkw178. [DOI] [PubMed] [Google Scholar]
- 15.Vardakas KZ, Legakis NJ, Triarides N, Falagas ME. 2016. Susceptibility of contemporary isolates to fosfomycin: a systematic review of the literature. Int J Antimicrob Agents 47:269–285. doi: 10.1016/j.ijantimicag.2016.02.001. [DOI] [PubMed] [Google Scholar]
- 16.Falagas ME, Vouloumanou EK, Samonis G, Vardakas KZ. 2016. Fosfomycin. Clin Microbiol Rev 29:321–347. doi: 10.1128/CMR.00068-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Neuner EA, Sekeres J, Hall GS, van Duin D. 2012. Experience with fosfomycin for treatment of urinary tract infections due to multidrug-resistant organisms. Antimicrob Agents Chemother 56:5744–5748. doi: 10.1128/AAC.00402-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Huttner A, Kowalczyk A, Turjeman A, Babich T, Brossier C, Eliakim-Raz N, Kosiek K, Martinez de Tejada B, Roux X, Shiber S, Theuretzbacher U, von Dach E, Yahav D, Leibovici L, Godycki-Cwirko M, Mouton JW, Harbarth S. 2018. Effect of 5-day nitrofurantoin vs single-dose fosfomycin on clinical resolution of uncomplicated lower urinary tract infection in women: a randomized clinical trial. JAMA 319:1781–1789. doi: 10.1001/jama.2018.3627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Datta R, Juthani-Mehta M. 2018. Nitrofurantoin vs fosfomycin: rendering a verdict in a trial of acute uncomplicated cystitis. JAMA 319:1771–1772. doi: 10.1001/jama.2018.4654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Trevino SE, Babcock HM, Henderson JP, Lane MA, Beekmann SE, Polgreen PM, Marschall J. 2015. Perceptions and behaviours of infectious diseases physicians when managing urinary tract infections due to MDR organisms. J Antimicrob Chemother 70:3397–3400. doi: 10.1093/jac/dkv271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Patel SS, Balfour JA, Bryson HM. 1997. Fosfomycin tromethamine. A review of its antibacterial activity, pharmacokinetic properties and therapeutic efficacy as a single-dose oral treatment for acute uncomplicated lower urinary tract infections. Drugs 53:637–656. doi: 10.2165/00003495-199753040-00007. [DOI] [PubMed] [Google Scholar]
- 22.Sastry S, Doi Y. 2016. Fosfomycin: resurgence of an old companion. J Infect Chemother 22:273–280. doi: 10.1016/j.jiac.2016.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bielen L, Likic R. 2019. Experience with fosfomycin in the treatment of complicated urinary tract infections caused by extended-spectrum beta-lactamase-producing Enterobacteriaceae. Ther Adv Infect Dis 6:2049936119858883. doi: 10.1177/2049936119858883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Qiao LD, Zheng B, Chen S, Yang Y, Zhang K, Guo HF, Yang B, Niu YJ, Wang Y, Shi BK, Yang WM, Zhao XK, Gao XF, Chen M. 2013. Evaluation of three-dose fosfomycin tromethamine in the treatment of patients with urinary tract infections: an uncontrolled, open-label, multicentre study. BMJ Open 3:e004157. doi: 10.1136/bmjopen-2013-004157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pullukcu H, Tasbakan M, Sipahi OR, Yamazhan T, Aydemir S, Ulusoy S. 2007. Fosfomycin in the treatment of extended spectrum beta-lactamase-producing Escherichia coli-related lower urinary tract infections. Int J Antimicrob Agents 29:62–65. doi: 10.1016/j.ijantimicag.2006.08.039. [DOI] [PubMed] [Google Scholar]
- 26.Wilson DT, May DB. 2013. Potential role of fosfomycin in the treatment of community-acquired lower urinary tract infections caused by extended-spectrum beta-lactamase-producing Escherichia coli. Am J Ther 20:685–690. doi: 10.1097/MJT.0b013e3182204d60. [DOI] [PubMed] [Google Scholar]
- 27.Michalopoulos AS, Livaditis IG, Gougoutas V. 2011. The revival of fosfomycin. Int J Infect Dis 15:e732–e739. doi: 10.1016/j.ijid.2011.07.007. [DOI] [PubMed] [Google Scholar]
- 28.Jacobson S, Junco Noa L, Ahmed S, Wallace MR. 2016. Efficacy and safety of oral fosfomycin for urinary tract infections in hospitalized patients. Antimicrob Agents Chemother 60:1952. doi: 10.1128/AAC.02971-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.López-Medrano F, Silva JT, Fernández-Ruiz M, Vidal E, Origüen J, Calvo-Cano A, Luna-Huerta E, Merino E, Hernández D, Jironda-Gallegos C, Escudero R, Gioia F, Moreno A, Roca C, Cordero E, Janeiro D, Sánchez-Sobrino B, Montero MM, Redondo D, Candel FJ, Pérez-Flores I, Armiñanzas C, González-Rico C, Del Carmen Fariñas M, Rodrigo E, Loeches B, López-Oliva MO, Montejo M, Lauzurica R, Horcajada JP, Pascual J, Andrés A, Aguado JM, REIPI, REDinREN, GESITRA-IC/SEIMC. 24 September 2019. Oral fosfomycin for the treatment of lower urinary tract infections among kidney transplant recipients—results of a Spanish multicenter cohort. Am J Transplant doi: 10.1111/ajt.15614. [DOI] [PubMed] [Google Scholar]
- 30.Ortiz Zacarias NV, Dijkmans AC, Burggraaf J, Mouton JW, Wilms EB, van Nieuwkoop C, Touw DJ, Kamerling IMC, Stevens J. 2018. Fosfomycin as a potential therapy for the treatment of systemic infections: a population pharmacokinetic model to simulate multiple dosing regimens. Pharmacol Res Perspect 6:e00378. doi: 10.1002/prp2.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wenzler E, Bleasdale SC, Sikka M, Bunnell KL, Finnemeyer M, Rosenkranz SL, Danziger LH, Rodvold KA, Antibacterial Resistance Leadership Group. 2018. Phase I study to evaluate the pharmacokinetics, safety, and tolerability of two dosing regimens of oral fosfomycin tromethamine in healthy adult participants. Antimicrob Agents Chemother 62:e00464-18. doi: 10.1128/AAC.00464-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wijma RA, Koch BCP, van Gelder T, Mouton JW. 2018. High interindividual variability in urinary fosfomycin concentrations in healthy female volunteers. Clin Microbiol Infect 24:528–532. doi: 10.1016/j.cmi.2017.08.023. [DOI] [PubMed] [Google Scholar]
- 33.Wenzler E, Ellis-Grosse EJ, Rodvold KA. 2017. Pharmacokinetics, safety, and tolerability of single-dose intravenous (ZTI-01) and oral fosfomycin in healthy volunteers. Antimicrob Agents Chemother 61:e00775-17. doi: 10.1128/AAC.00775-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Segre G, Bianchi E, Cataldi A, Zannini G. 1987. Pharmacokinetic profile of fosfomycin trometamol (Monuril). Eur Urol 13(Suppl 1):56–63. doi: 10.1159/000472864. [DOI] [PubMed] [Google Scholar]
- 35.Bergan T, Thorsteinsson SB, Albini E. 1993. Pharmacokinetic profile of fosfomycin trometamol. Chemotherapy 39:297–301. doi: 10.1159/000239140. [DOI] [PubMed] [Google Scholar]
- 36.Scaglione F, Cicchetti F, Demartini G, Arcidiacono M. 1994. Fosfomycin distribution in the lower urinary tract after administration of fosfomycin trometamol salt. Int J Clin Pharmacol Res 14:107–109. [PubMed] [Google Scholar]
- 37.Forest Pharmaceuticals, Inc. 2011. Monurol (fosfomycin tromethamine) package insert. Forest Pharmaceuticals, Inc, St Louis, MO: https://www.accessdata.fda.gov/drugsatfda_docs/label/2011/050717s007lbl.pdf. Accessed 18 Jul 2019. [Google Scholar]
- 38.CLSI. 2019. Performance standards for antimicrobial susceptibility testing, 29th ed M100-S29 CLSI, Wayne, PA. [Google Scholar]
- 39.European Committee on Antimicrobial Susceptibility Testing. 2019. Breakpoint tables for interpretation of MICs and zone diameters. Version 9.0. http://www.eucast.org.
- 40.Abbott IJ, Meletiadis J, Belghanch I, Wijma RA, Kanioura L, Roberts JA, Peleg AY, Mouton JW. 2018. Fosfomycin efficacy and emergence of resistance among Enterobacteriaceae in an in vitro dynamic bladder infection model. J Antimicrob Chemother 73:709–719. doi: 10.1093/jac/dkx441. [DOI] [PubMed] [Google Scholar]
- 41.VanScoy B, McCauley J, Bhavnani SM, Ellis-Grosse EJ, Ambrose PG. 2016. Relationship between fosfomycin exposure and amplification of Escherichia coli subpopulations with reduced susceptibility in a hollow-fiber infection model. Antimicrob Agents Chemother 60:5141–5145. doi: 10.1128/AAC.00355-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zhao M, Bulman ZP, Lenhard JR, Satlin MJ, Kreiswirth BN, Walsh TJ, Marrocco A, Bergen PJ, Nation RL, Li J, Zhang J, Tsuji BT. 2017. Pharmacodynamics of colistin and fosfomycin: a ‘treasure trove’ combination combats KPC-producing Klebsiella pneumoniae. J Antimicrob Chemother 72:1985–1990. doi: 10.1093/jac/dkx070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ten Doesschate T, van Werkhoven H, Meijvis S, Stalenhoef J, van Zuilen A, de Vries A, Bonten M. 2019. Fosfomycin-trometamol for urinary tract infections in kidney transplant recipients. Transplantation 103:1272–1276. doi: 10.1097/TP.0000000000002427. [DOI] [PubMed] [Google Scholar]
- 44.Reid GE, Grim SA, Layden JE, Akkina S, Tang I, Campara M, Clark NM. 2013. The use of fosfomycin to treat urinary tract infections in kidney transplant recipients. Transplantation 96:e12–e14. doi: 10.1097/TP.0b013e318298dd26. [DOI] [PubMed] [Google Scholar]
- 45.Ballestero-Téllez M, Docobo-Pérez F, Rodríguez-Martínez JM, Conejo MC, Ramos-Guelfo MS, Blázquez J, Rodríguez-Baño J, Pascual A. 2017. Role of inoculum and mutant frequency on fosfomycin MIC discrepancies by agar dilution and broth microdilution methods in Enterobacteriaceae. Clin Microbiol Infect 23:325–331. doi: 10.1016/j.cmi.2016.12.022. [DOI] [PubMed] [Google Scholar]
- 46.Kaase M, Szabados F, Anders A, Gatermann SG. 2014. Fosfomycin susceptibility in carbapenem-resistant Enterobacteriaceae from Germany. J Clin Microbiol 52:1893–1897. doi: 10.1128/JCM.03484-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.van den Bijllaardt W, Schijffelen MJ, Bosboom RW, Cohen Stuart J, Diederen B, Kampinga G, Le T-N, Overdevest I, Stals F, Voorn P, Waar K, Mouton JW, Muller AE. 2018. Susceptibility of ESBL Escherichia coli and Klebsiella pneumoniae to fosfomycin in the Netherlands and comparison of several testing methods including Etest, MIC test strip, Vitek2, Phoenix and disc diffusion. J Antimicrob Chemother 73:2380–2387. doi: 10.1093/jac/dky214. [DOI] [PubMed] [Google Scholar]
- 48.de Cueto M, Lopez L, Hernandez JR, Morillo C, Pascual A. 2006. In vitro activity of fosfomycin against extended-spectrum-beta-lactamase-producing Escherichia coli and Klebsiella pneumoniae: comparison of susceptibility testing procedures. Antimicrob Agents Chemother 50:368–370. doi: 10.1128/AAC.50.1.368-370.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.van Mens SP, Ten Doesschate T, Kluytmans-van den Bergh MFQ, Mouton JW, Rossen JWA, Verhulst C, Bonten MJM, Kluytmans J. 2018. Fosfomycin Etest for Enterobacteriaceae: interobserver and interlaboratory agreement. Int J Antimicrob Agents 52:678–681. doi: 10.1016/j.ijantimicag.2018.06.014. [DOI] [PubMed] [Google Scholar]
- 50.Mouton JW, Ambrose PG, Canton R, Drusano GL, Harbarth S, MacGowan A, Theuretzbacher U, Turnidge J. 2011. Conserving antibiotics for the future: new ways to use old and new drugs from a pharmacokinetic and pharmacodynamic perspective. Drug Resist Updat 14:107–117. doi: 10.1016/j.drup.2011.02.005. [DOI] [PubMed] [Google Scholar]
- 51.Frimodt-Moller N, Maigaard S, Madsen PO. 1981. Effect of urine concentration versus tissue concentration of ampicillin and mecillinam on bacterial adherence in the rat bladder. Invest Urol 18:322–325. [PubMed] [Google Scholar]
- 52.Zhanel GG, Parkinson K, Higgins S, Denisuik A, Adam H, Pitout J, Noreddin A, Karlowsky JA. 2017. Pharmacodynamic activity of fosfomycin simulating urinary concentrations achieved after a single 3-g oral dose versus Escherichia coli using an in vitro model. Diagn Microbiol Infect Dis 88:271–275. doi: 10.1016/j.diagmicrobio.2017.04.007. [DOI] [PubMed] [Google Scholar]
- 53.Lopez-Montesinos I, Horcajada JP. 2019. Oral and intravenous fosfomycin in complicated urinary tract infections. Rev Esp Quimioter 32(Suppl 1):37–44. [PMC free article] [PubMed] [Google Scholar]
- 54.Karaiskos I, Galani L, Sakka V, Gkoufa A, Sopilidis O, Chalikopoulos D, Alivizatos G, Giamarellou E. 2019. Oral fosfomycin for the treatment of chronic bacterial prostatitis. J Antimicrob Chemother 74:1430–1437. doi: 10.1093/jac/dkz015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zhanel GG, Zhanel MA, Karlowsky JA. 2018. Oral fosfomycin for the treatment of acute and chronic bacterial prostatitis caused by multidrug-resistant Escherichia coli. Can J Infect Dis Med Microbiol 2018:1404813. doi: 10.1155/2018/1404813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ten Doesschate T, van Mens SP, van Nieuwkoop C, Geerlings SE, Hoepelman AIM, Bonten MJM. 2018. Oral fosfomycin versus ciprofloxacin in women with E. coli febrile urinary tract infection, a double-blind placebo-controlled randomized controlled non-inferiority trial (FORECAST). BMC Infect Dis 18:626. doi: 10.1186/s12879-018-3562-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mouton J, Voss A, Arends J, Bernards S. 2007. O435 prevalence of ESBL in the Netherlands: the ONE study. Int J Antimicrob Agents 29:S91–S92. doi: 10.1016/S0924-8579(07)70289-3. [DOI] [Google Scholar]
- 58.CLSI. 2012. Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically, 9th ed M07-A9 CLSI, Wayne, PA. [Google Scholar]
- 59.Rowe EL, Morozowich W. 1969. A simple dilution analog computer for simulation of drug distribution processes. J Pharm Sci 58:1375–1378. doi: 10.1002/jps.2600581117. [DOI] [PubMed] [Google Scholar]
- 60.Wijma RA, Bahmany S, Wilms EB, van Gelder T, Mouton JW, Koch BCP. 2017. A fast and sensitive LC-MS/MS method for the quantification of fosfomycin in human urine and plasma using one sample preparation method and HILIC chromatography. J Chromatogr B Analyt Technol Biomed Life Sci 1061–1062:263–269. doi: 10.1016/j.jchromb.2017.07.036. [DOI] [PubMed] [Google Scholar]
- 61.FDA. 2013. Guidance for industry: bioanalytical method validation. FDA, Rockville, MD. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.