Graphical abstract
The trochlear dysplasia achieved by femoral rotational osteotomy and increased FA was the more common hyperplastic variant with boss formation in the anterior proximal trochlea.
Keywords: Patellar dislocation, Trochlea dysplasia, Femoral anteversion, Boss, Femoral osteotomy
Abstract
Increased femoral anteversion (FA) has been recently demonstrated as one risk factor for recurrent patellar dislocation (RPD). However, it has been still unclear whether the increase of FA can result in patellar dislocation, and subsequent morphological and trabecular microarchitectural changes in the trochlea has not been investigated. Forty knees from 20 rabbits at 3 months of age were included. The right knees underwent surgery with internal rotation of distal femur to increase FA, with the left knees acting as internal controls. The surgical knees were called operated group, and non-operated knees were control group. Micro-CT scans for distal femur were acquired after 4 months of surgery. In the operated group, a boss located proximal to the entrance of the groove was formed. The central trochlear height was significantly greater, sulcus angle was significantly greater, both lateral and medial trochlear slope were significantly lower, and boss height was significantly greater in comparison to the control group. Regarding the microarchitectural changes, the trabecular thickness were increased by 67.5% at the groove, 33.0% and 29.5%, at the medial and lateral femoral condyle, and trabecular number were decreased by 37.8% and 26.5% at the groove and medial femoral condyle. This study provided a novel animal model of trochlea dysplasia by femoral rotational osteotomy and increased FA. These changes were associated with the load redistribution in the patellofemoral joint after the increase of FA.
Introduction
Recurrent patellar dislocation (RPD) is a multifactorial clinical problem with the incidence of approximately 7 in 100,000 of general population, and the rate is higher for younger and more active populations [1]. Different bony risk factors such as trochlear dysplasia, patella alta, lateralization of tibial tuberosity, and increased femoral anteversion (FA) have been reported [2], [3], [4], [5], and should be considered and potentially addressed in the treatment. Among these factors, increased FA has been demonstrated as one risk factor to assess for patellar instability [6], [7], [8], [9]. Increased FA is associated with inferior clinical outcomes of patients with RPD, treated with tibial tubercle osteotomy and medial patellofemoral ligament (MPFL) reconstruction [10].
In RPD with an insufficient MPFL, 100 of increased FA can be regarded as a significant risk factor for patellar instability [6], [7]. As a consequence, an increased FA may increase stress loading of lateral facet of the patellofemoral joint (PFJ) or raise strains to the medial patellar retinaculum [6], [7]. Any changes in the load distribution will affect the stress state of the cartilage, subchondral bone, and cancellous bone, ultimately influence the physiology and morphology of the PFJ [11], [12]. Therefore, increasing the FA by external rotation of the femur might induce changes in the microarchitecture of the trochlea.
It is still not confirmed whether increased FA can result in patellar dislocation. In previous studies, most animal models of RPD were achieved by surgical release of medial soft tissue restraints [13], and further suture with overlapping lateral retinaculum [14], [15]. Nevertheless, the bony risk factors, such as FA, were not involved in these soft tissue procedures. Therefore, these models have limitations with respect to their clinical applicability, because significantly increased FA in patients with RPD compared to normal controls have been reported in several studies [16], [17], [18].
Therefore, the purpose of present study was to provide a rabbit model of patellar dislocation by increasing FA, and observe the changes of external morphology and internal architecture of femoral trochlea using micro-computed tomography (CT). It was hypothesized that a rabbit model of patellar dislocation could be successfully achieved by increasing FA, and subsequent changes in the femoral trochlea could be found.
Material and methods
Study design
The experimental protocol was approved by the Institutional Animal Care and Use Committee, and conducted according to the Guide for the Care and Use of Laboratory Animals. Forty knees of 20 New Zealand white healthy rabbits (provided by the Laboratory Animal Center of our University) with 3 months of age and 1.8–2.3 kg in weight were included in the study. There was normal birth and life history for all rabbits. They have no patellar dislocation in extension and flexion activity and no limp in daily walk. The right knees underwent surgery, with the left knees acting as internal controls. The surgical knees were called operated group, and non-operated knees were control group. All rabbits were followed up for 4 months. As it’s known, the skeletal growth and maturation of the rabbits is completed at 28 weeks [19].
Surgical protocol
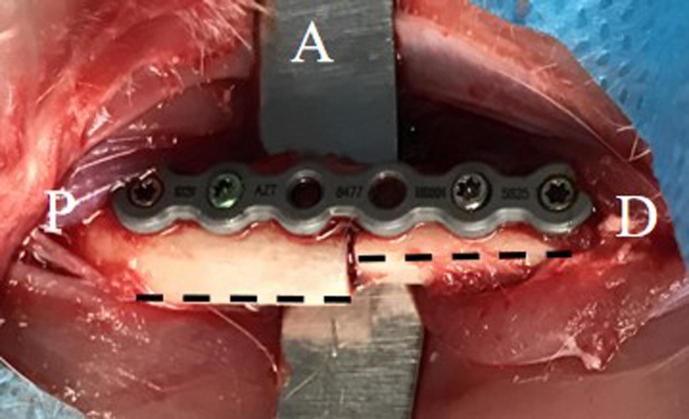
All surgeries were performed under intravenous anesthesia with ketamine (20 mg/kg) and xylazine (5 mg/kg). Before surgery, the right lower limb was shaved and sterilized following standard protocol. For the surgical procedure, the rabbit was placed in left lateral decubitus position. A 5-cm longitudinal incision was made in the middle of lateral thigh, and followed by the dissection in the inter-muscular space between vastus lateralis and biceps femoris muscle. The femoral shaft was exposed, and a transverse osteotomy perpendicular to the shaft was performed at the location where it’s slightly distal from the midpoint of shaft and progressed carefully with an electric saw. A 6-hole locking plate was used and placed along the posterior ridge of the femur. The distal femur was first fixed by two locking screws and then rotated internally. The goal was to increase the distance between the posterior ridge of distal and proximal femur by approximately 3–4 mm (about 200 of increase of FA) (Fig. 1). Fixation was then achieved by two locking screws in the proximal femur. The patellar kinematics was checked during passive knee extension and flexion. The aim was to get the patella to shift laterally at terminal knee extension, and engage into the groove with knee flexion. The incision was closed with suture of fascia, subcutaneous tissue and skin. At the end of the surgery, a dressing was applied.
Fig. 1.
The surgical image of femoral osteotomy, the plate was placed along the posterior ridge of the femur (black dashed line). The distal femur was rotated internally. The rotation angle was assessed by the distance between the posterior ridge of distal and proximal femur. A: anterior; P: proximal; D: distal.
All rabbits were housed under the same conditions. Each animal had an individual stainless steel cage and was allowed an unrestricted activity in the cage. Intramuscular buprenorphine (0.05 mg/kg) was administered twice daily for the first 3 days. Oral ciprofloxacin (10 mg/kg) was administered as antibiotic prophylaxis for the first 3 days after surgery.
Micro-CT scanning
All rabbits were euthanized by venous air embolism 4 months after surgery. All distal femurs without soft tissues were collected. After gross observation, the samples were scanned by micro-CT (PerkinElmer, Inc., Waltham, MA) with the parameters set as follows: resolution ratio, 45 mm; voltage, 90 kV; current, 88 uA.
Macroscopic measurement
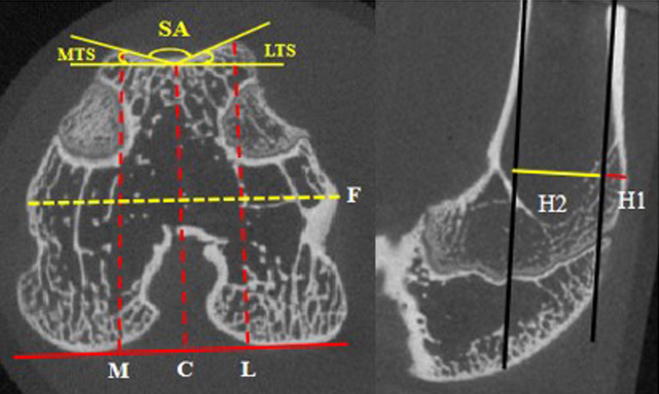
Micro-CT scan data were converted into 3-dimensional (3D) models using Mimics 19.0 software (Materialise, Leuven, Belgium). The axial slice of the proximal chondral entrance of the groove where the trochlea is initially completely covered with cartilage was defined, as described by Hingelbaum et al. [20]. The following well-established quantitative parameters were determined in the axial slice 5 mm further distal to this proximal slice [21]: medial, central, and lateral trochlear height (relative to the width of distal femur), sulcus angle, and lateral and medial trochlear slope. In the sagittal plane, the slice through the center of groove was selected, and the boss height (relative to the height of distal femur) was measured (Fig. 2). All measurements were performed on the Mimics 19.0 software using a mouse cursor with automated distance or angle calculation. All parameters were measured by two investigators, and the mean was used for further analysis.
Fig. 2.
The schematic diagram of the measurements. F indicates the total width of femoral condyle; M, C, and L indicate the distance from the highest point of the medial condyle, groove, lateral condyle to the posterior condyle line. Trochlear height (medial, central, and lateral) was measured as M/F, C/F, and L/F, respectively. H1 indicates the distance of the top point of boss to the anterior cortex line; H2 indicate the distance between the anterior cortex line and its parallel line through the posterior cortex. Boss height was measured as H1/H2. SA: sulcus angle; MTS: medial trochlear slope; LTS: lateral trochlear slope.
Microscopic analysis
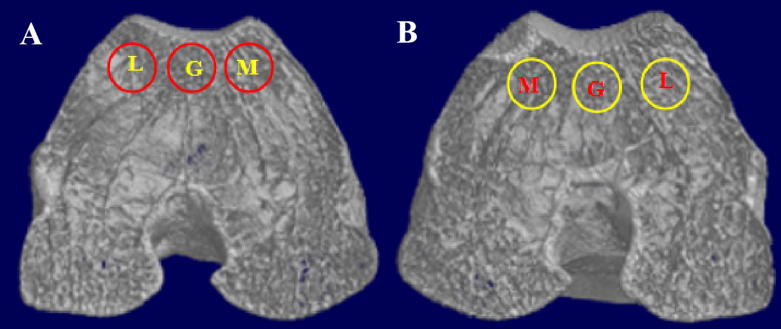
For microscopic analysis, three spatially distributed cylindrical bone biopsies with a diameter of 3 mm under the groove, medial and lateral femoral condyle in axial image were chosen as the region of interest (ROI). Scans were integrated into 3D voxel images (Fig. 3). After 3D reconstruction, the parameters such as bone volume fraction (BV/TV, %), trabecular thickness (Tb.Th, mm), trabecular number (Tb.N, 1/mm), trabecular spacing (Tb.Sp, mm), and bone mineral density (BMD, mg/cm3) were used to evaluate the trabecular microarchitectural structure.
Fig. 3.
The 3-dimensional images of trabecular bone from operated knee (A) and control knee (B) to show three regions of interest (ROI) from groove (G), medial (M) and lateral (L) femoral condyle.
Statistical analysis
Before the investigation, the sample size was estimated using sulcus angle as the primary variable. On the basis of previous study [22], the standard deviation was assumed at 80 in both experiment and control groups. and an estimated difference of 100 between the groups. A power calculation was performed with a confidence level of 95% (α = 0.05) and power (1-β) of 90%. This yielded an estimated sample size of 14 knees per group.
All continuous data were reported as mean and standard deviation for description. After the test normality and homogeneity of variances, the paired-sample T test or nonparametric Mann-Whitney U test was used to analyze the difference between groups. A X2 test or Fisher exact test were used to compare groups for the categorical variables. Data analysis was performed with SPSS 23.0 software (SPSS Inc, Chicago, Illinois). The statistical significance level was set at 0.05.
Results
There was no dislocation in the preoperative state in both groups. In the follow up of operated knees, one rabbit sustained a hip dislocation without patellar dislocation. Three knees developed complete patellar dislocation in daily flexion position, and the remaining 16 patellae were still in the groove without complete dislocation, but dislocated when the knee was passively placed in the maximal extension position. No dislocation was found in the follow up of the non-operated knees.
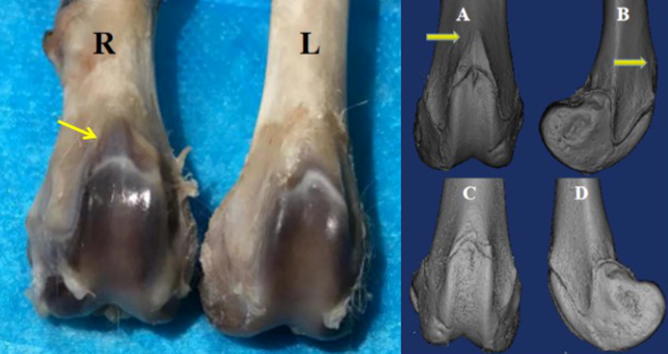
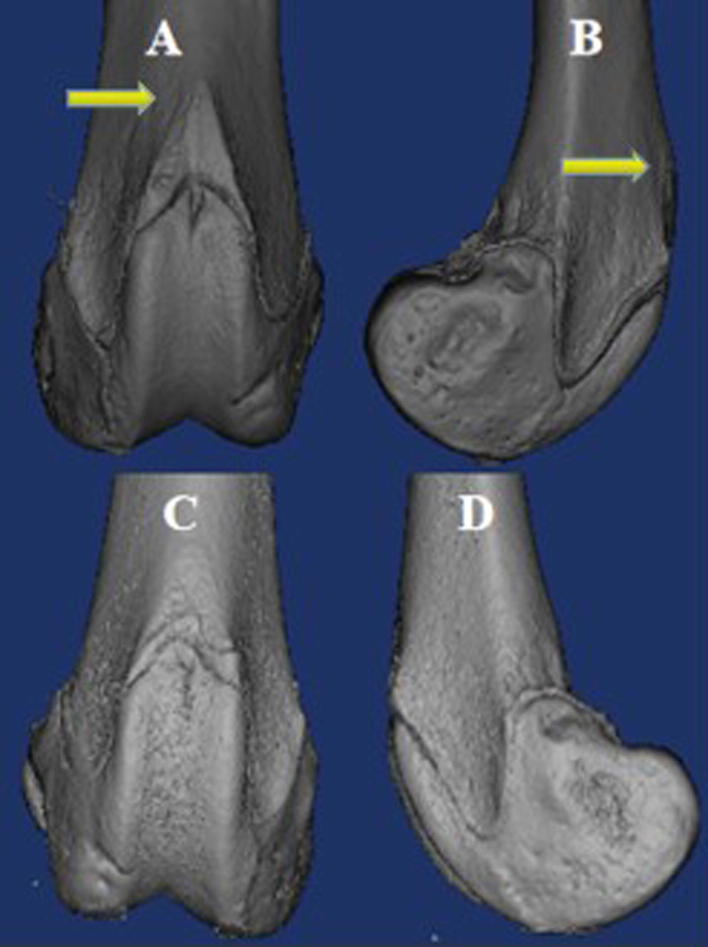
On inspection, the articular cartilage was smooth, and no obvious osteoarthritis was observed in the PFJ in both control and operated groups (Fig. 4). Compared to the control knees, a local boss was formed in all operated knees and located proximal to the entrance of the groove (Fig. 4, Fig. 5). The groove was observed a little wider and shallower in the operated group (sulcus angle: 142.90 ± 2.43 and 138.26 ± 1.57, P = 0.000).
Fig. 4.
The macroscopic observation of trochlea. A local boss was formed and located proximal to the entrance of the groove in the operated group (see the arrow). R: right knee; L: left knee.
Fig. 5.
Three-dimensional images of the femoral trochlea. The local boss can be seen on anterior view (A) and lateral view (B) (see the arrow) in the operated group. No boss was formed in the control group (C: anterior view; D: lateral view).
Macroscopic measurement
All parameters for the measurement of trochlear height showed that central troclear height in the operated group was significantly greater than that in the control group. No significant differences were found in the medial and lateral trochlear height between two groups (Table 1).
Table 1.
Results of macroscopic measurement for operated and control groups.
| Parameters | Operated group | Control group | P Value |
|---|---|---|---|
| Medial trochlear height, ratio | 0.97 ± 0.38 | 0.97 ± 0.43 | 0.520 |
| Central trochlear height, ratio | 0.94 ± 0.04 | 0.92 ± 0.04 | 0.006 |
| Lateral trochlear height, ratio | 0.97 ± 0.07 | 0.99 ± 0.04 | 0.090 |
| Sulcus angle, degree | 142.90 ± 2.43 | 138.26 ± 1.57 | 0.000 |
| Medial trochlea slope, degree | 20.49 ± 1.81 | 22.30 ± 1.33 | 0.000 |
| Lateral trochlea slope, degree | 17.40 ± 1.19 | 19.56 ± 1.54 | 0.000 |
| Boss height, ratio | 0.18 ± 0.07 | 0.09 ± 0.03 | 0.000 |
All parameters for the measurement of trochlear angle showed that sulcus angle in the operated group was significantly greater than that in the control group. Both the lateral and medial trochlear slope were significantly lower than that in the control group.
In the sagittal slice, boss height in the operated group was significantly greater than that in the control group.
Microscopic analysis
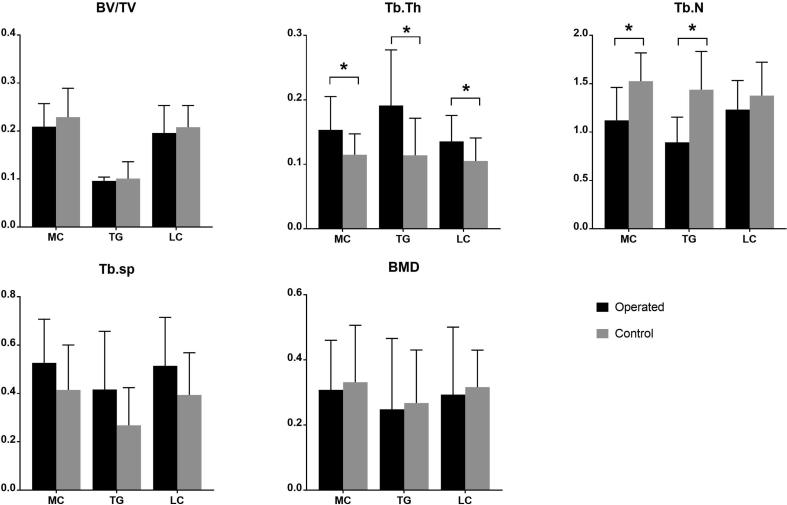
Regarding the trabecular bone microarchitecture, the results indicated significant differences in Tb.Th and Tb.N between the operated and control groups (Fig. 6). Tb.Th in the operated group were 67.5%, 33.0% and 29.5% higher than those in the control group at the groove, medial and lateral femoral condyle, respectively. Tb.N in the operated group were 37.8% and 26.5% lower than those in the control group at the groove and medial femoral condyle, but no significant difference was found in lateral femoral condyle (Table 2).
Fig. 6.
Microscopic analysis of trabecular bone through micro-CT. The significant differences for the operated knees were the increase of trabecular thickness and decrease of trabecular number in comparison with control knees.
Table 2.
Results of microscopic analysis for operated and control groups.
| Parameters | ROI | Operated group | Control group | P Value |
|---|---|---|---|---|
| BV/TV (%) | TG | 9.647 ± 0.825 | 10.062 ± 3.622 | 0.633 |
| MC | 20.886 ± 4.886 | 22.895 ± 6.187 | 0.298 | |
| LC | 19.551 ± 5.818 | 20.839 ± 4.573 | 0.409 | |
| Tb.Th (mm) | TG | 0.191 ± 0.089 | 0.114 ± 0.059 | 0.005 |
| MC | 0.153 ± 0.053 | 0.115 ± 0.033 | 0.003 | |
| LC | 0.136 ± 0.041 | 0.105 ± 0.037 | 0.008 | |
| Tb.N (1/mm) | TG | 0.894 ± 0.267 | 1.438 ± 0.407 | 0.000 |
| MC | 1.121 ± 0.349 | 1.526 ± 0.301 | 0.000 | |
| LC | 1.233 ± 0.308 | 1.377 ± 0.355 | 0.235 | |
| Tb.Sp (mm) | TG | 0.416 ± 0.247 | 0.268 ± 0.160 | 0.057 |
| MC | 0.527 ± 0.186 | 0.414 ± 0.191 | 0.045 | |
| LC | 0.514 ± 0.206 | 0.393 ± 0.179 | 0.082 | |
| BMD (g/mm3) | TG | 0.248 ± 0.224 | 0.268 ± 0.167 | 0.738 |
| MC | 0.308 ± 0.157 | 0.332 ± 0.180 | 0.639 | |
| LC | 0.294 ± 0.213 | 0.316 ± 0.117 | 0.698 |
ROI, region of interest; TG, trochlea groove; MC, medial condyle; LC, lateral condyle; BV/TV, bone volume fraction; Tb.Th, trabecular thickness; Tb.N, trabecular number; Tb.Sp, trabecular spacing; BMD, bone mineral density.
There was an increasing trend in Tb.Sp in the operated group, but the difference was not statistically significant between two groups. No significant differences were found in BV/TV and BMD between two groups.
Discussion
The most important finding of the present study was the creation of a novel animal model of trochlear dysplasia by femoral rotational osteotomy and increased FA in the normal immature rabbit. The trochlear dysplasia formed was the more common hyperplastic variant (in humans) with boss formation in the anterior proximal trochlea. Associated with this trochlear trabecular thickness was increased but decreased trabecular number. This reflects the change in loading across the PFJ as the displaced patella allows overgrowth of the anterior distal femoral physis.
In the present study, the model of patellar dislocation was achieved successfully by femoral rotational osteotomy and increased FA. This was quite different from previous animal models used to release of the medial soft tissues to create lateral patellar displacement. Huri et al. [13] performed the release of the medial soft tissue restraints to make the model of patellar dislocation. Li et al. [14] and Wang et al. [15] further sutured with overlapping lateral soft tissue in addition to the medial release. They all showed the development of patellar dislocation in association with a flattened femoral trochlea. They demonstrated the effect of the loss of medial soft tissue integrity that is seen in RPD, but not the important morphological changes in the trochlea.
Abnormal femoral anteversion is an uncommon and therefore under-recognised cause of patellar dislocation. Diederichs et al. [16] reported that patients with RPD had a 1.56 times higher mean FA (20.30 ± 10.40) compared with healthy controls (13.00 ± 8.40). Prakash et al. [17] measured Asian patients and found a similarly significant difference in FA between patellar dislocation patients and healthy controls (19.20 ± 10.40 and 12.00 ± 8.40) respectively. Takagi et al. [18] demonstrated that alignment in the transverse plane, especially, increased FA (30.90 ± 9.60 and 17.00 ± 8.40), but not the sagittal or coronal plane, affected the risk of RPD. Therefore increased FA is a risk factor for RPD and could be a focus for further basic research.
A novel model of trochlear dysplasia was created by femoral rotational osteotomy and increased FA. This finding was in accordance with the results of image analysis that trochlear morphology is significantly related to FA. Increased FA is associated with a flatter, and more dysplastic trochlea [9], [21]. Besides the finding of flattening of the femoral groove in previous studies [13], [14], [15], the most obvious change of trochlea dysplasia was the boss formation in the anterior proximal trochlea, which will damage the smooth engagement of patella into the groove when the knee flexes. The reason for the development of trochlea dysplasia has been poorly understood. In principle, it is possible that the trochlear morphology is (1) genetically predetermined, (2) a result of mechanical stimuli during intrauterine or childhood growth, or (3) combined influence by genetics and mechanical stimuli. Several reports of familial forms of the femoral trochlear dysplasia leading to bilateral RPD shown the possible genetic factor of trochlear dysplasia [23], [24]. Others supported the theory that, to a certain extent the development of trochlear morphology is susceptible to mechanical stimuli [13], [14], [15], [22]. The present study supports the view that, the trochlear dysplasia may be induced by mechanical stimuli since the pressure changes in the PFJ as a result of increased FA.
In the present study, the model was achieved by femoral rotational osteotomy and the increase of FA. The load between the PFJ could be altered with increased FA. Liska et al. [25] found that, in simulated increased FA and corresponding lateralization of the patella the mean and peak pressure is higher on the lateral facet compared to the medial facet. Liao et al. [26] reported that patella cartilage stress was significantly higher, mean hydrostatic pressure increased 26% and 36%, and mean octahedral shear stress increased 25% and 30% when the femur was rotated 50 and 100 from the natural position, respectively. Lee et al. [11] reported a nonlinear increase in the PFJ contact pressure, from 00 to 200 of fixed rotation, there was only a small increase in contact pressure. However, from 200 to 300 of femoral rotation, there was a significantly greater increase in pressure.
Along load redistribution in the PFJ after the increase of FA, trabecular bone microarchitecture was changed concomitantly. The most obvious change was the increase of Tb.Th in the distal femur, especially the increase of 67.5% at the groove. The Tb.N and Tb.Sp were constant in the lateral condyle, but the Tb.N was decreased and Tb. Sp was increased in the medial condyle. The increase of Tb.Th in the distal femur may reflect the increase of load in the PFJ due to femoral rotation, the incongruence of PFJ, the integrity of soft tissue envelope and muscle contraction [27]. The different changes in Tb.N and Tb.Sp between medial and lateral condyle indicated the different load distribution in PFJ after the increase of FA. Kaiser et al. [6], [7] demonstrated that there was a significant center of force shift towards the lateral side of PFJ with increased internal femoral torsion. All the changes follow the general concept of “bone functional adaptation” to mechanical loading. In the PFJ, mechanical stress is transmitted from articular cartilage to subchondral bone and then to cancellous bone. In this process of stress transmission, the formation of local boss, associated trabecular bone formation and migration were the response to the different local force after the change of femoral torsion.
The present study could reflect the effect of FA on the trochlear dysplasia with the creation of the model by femoral rotational osteotomy and increased FA. However, the accuracy of osteotomy could be better controlled in the osteotomy orientation and amount of rotation. In the present study, the transverse osteotomy was perpendicular to the shaft at the location where it’s slightly distal from the midpoint of shaft. Due to the different femoral mechanical and anatomical axes, derotational femoral osteotomy can cause malalignment in the frontal plane [28], [29], a valgus-producing effect has been stated when the cutting plane is perpendicular to the distal shaft axis, but osteotomy at mid-shaft level could reduce this effect [28]. Regarding to the amount of rotation, rotation was controlled by the distance in the present study, not the measurement of degree. This may result in the difference of model with three patellae of out of the groove and 16 patellae of riding along the lateral side of the groove. In clinical practice, Zhang et al. [10] reported clinical results of 66 patients of RPD (70 knees) at a median follow-up time of 28 months with a comparison of patients with different FA angles. Patients with an increased FA angle (>300) had inferior postoperative clinical outcomes, including greater patellar laxity, a higher rate of residual J-sign and lower patient-reported outcomes after MPFL reconstruction and combined tibial tubercle osteotomy.
Several limitations should be acknowledged for the present study. First, although rabbit was the common animal for model creation of patellar dislocation in literature, a rabbit limb with a flexed knee can not completely equate to a human knee with upright stance. Caution should be observed when interpreting small mammal data with human bipedalism. Second, since many factors as osteotomy position and orientation, amount of rotation have great effect on the results, preoperative limb alignment and precise design for the osteotomy should be considered in the set-up next time. Third, the record of load change between the PFJ and histologic evaluation of cartilage were not involved, these data would complement the mirco-CT data to fully understand the change of trochlea after the increase of FA. Fourth, for the available fixation tool, rabbits with age of 3-month were selected, and only four months to mature were left to observe the results. In the future, small surgical tools could be introduced and younger animals may be better to observe the trochlear development in a longer follow up.
Conclusions
A novel animal model of trochlear dysplasia was achieved by femoal rotational osteotomy and increased femoral anteversion in the normal immature rabbit. The trochlear dysplasia formation was the more common hyperplastic variant (in humans) with boss formation in the anterior proximal trochlea. Associated with this there were increased trochlear trabecular thickness but decreased trabecular number. These changes were associated with the load redistribution in the patellofemoral joint after the increase of FA.
Compliance with ethics requirements
All Institutional and National Guidelines for the care and use of animals (fisheries) were followed.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The authors gratefully acknowledge the Laboratory Animal Center of Hebei Medical University for their care of rabbits and Dr. Yi Wang from the Chinese PLA general hospital for assistance with micro-computed tomography data acquisition and analysis. This work was supported by the National Natural Science Foundation of China (81873983), Key Program of Natural Science Foundation of Hebei Province (H2019206694) and Hebei Province Key Project of Achievement Transformation (zh2018007).
Footnotes
Peer review under responsibility of Cairo University.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jare.2020.02.002.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- 1.Frosch S., Balcarek P., Walde T.A., Schuttrumpf J.P., Wachowski M.M., Ferleman K.G. The treatment of patellar dislocation: a systematic review. Z Orthop Unfall. 2011;149(6):630–645. doi: 10.1055/s-0030-1250691. [DOI] [PubMed] [Google Scholar]
- 2.Fu K., Duan G., Liu C., Niu J., Wang F. Changes in femoral trochlear morphology following surgical correction of recurrent patellar dislocation associated with trochlear dysplasia in children. Bone Joint J. 2018:811–821. doi: 10.1302/0301-620X.100B6.BJJ-2017-1295.R1. 100-B(6) [DOI] [PubMed] [Google Scholar]
- 3.Lee D.Y., Park Y.J., Song S.Y., Hwang S.C., Park J.S., Kang D.G. Which technique is better for treating patellar dislocation? A systematic review and meta-analysis. Arthroscopy. 2018;34(11):3082–3093. doi: 10.1016/j.arthro.2018.06.052. [DOI] [PubMed] [Google Scholar]
- 4.Tan S.H.S., Ibrahim M.M., Lee Z.J., Chee Y.K.M., Hui J.H. Patellar tracking should be taken into account when measuring radiographic parameters for recurrent patellar instability. Knee Surg Sports Traumatol Arthrosc. 2018;26(12):3593–3600. doi: 10.1007/s00167-017-4795-0. [DOI] [PubMed] [Google Scholar]
- 5.Ward S.R., Terk M.R., Powers C.M. Patella alta: association with patellofemoral alignment and changes in contact area during weight bearing. J Bone Joint Surg Am. 2007;89(8):1749–1755. doi: 10.2106/JBJS.F.00508. [DOI] [PubMed] [Google Scholar]
- 6.Kaiser P., Schmoelz W., Schottle P.B., Heinrichs C., Zwierzina M., Attal R. Isolated medial patellofemoral ligament reconstruction for patella instability is insufficient for higher degrees of internal femoral torsion. Knee Surg Sports Traumatol Arthrosc. 2019;27(3):758–765. doi: 10.1007/s00167-018-5065-5. [DOI] [PubMed] [Google Scholar]
- 7.Kaiser P., Schmoelz W., Schoettle P., Zwierzina M., Heinrichs C., Attal R. Increased internal femoral torsion can be regarded as a risk factor for patellar instability: a biomechanical study. Clin Biomech (Bristol, Avon) 2017;47:103–109. doi: 10.1016/j.clinbiomech.2017.06.007. [DOI] [PubMed] [Google Scholar]
- 8.Kaiser P., Konschake M., Loth F., Plaikner M., Attal R., Liebensteiner M. Derotational femoral osteotomy changes patella tilt, patella engagement and tibial tuberosity trochlear groove distance. Knee Surg Sports Traumatol Arthrosc. 2019 doi: 10.1007/s00167-019-05561-9. [DOI] [PubMed] [Google Scholar]
- 9.Imhoff F.B., Funke V., Muench L.N., Sauter A., Englmaier M., Woertler K. The complexity of bony malalignment in patellofemoral disorders: femoral and tibial torsion, trochlear dysplasia, TT-TG distance, and frontal mechanical axis correlate with each other. Knee Surg Sports Traumatol Arthrosc. 2019 doi: 10.1007/s00167-019-05542-y. [DOI] [PubMed] [Google Scholar]
- 10.Zhang Z., Zhang H., Song G., Zheng T., Ni Q., Feng H. Increased femoral anteversion is associated with inferior clinical outcomes after MPFL reconstruction and combined tibial tubercle osteotomy for the treatment of recurrent patellar instability. Knee Surg Sports Traumatol Arthrosc. 2019 doi: 10.1007/s00167-019-05818-3. [DOI] [PubMed] [Google Scholar]
- 11.Lee T.Q., Morris G., Csintalan R.P. The influence of tibial and femoral rotation on patellofemoral contact area and pressure. J Orthop Sports Phys Ther. 2003;33(11):686–693. doi: 10.2519/jospt.2003.33.11.686. [DOI] [PubMed] [Google Scholar]
- 12.Souza R.B., Draper C.E., Fredericson M., Powers C.M. Femur rotation and patellofemoral joint kinematics: a weightbearing magnetic resonance imaging analysis. J Orthop Sports Phys Ther. 2010;40(5):277–285. doi: 10.2519/jospt.2010.3215. [DOI] [PubMed] [Google Scholar]
- 13.Huri G., Atay O.A., Ergen B., Atesok K., Johnson D.L., Doral M.N. Development of femoral trochlear groove in growing rabbit after patellar instability. Knee Surg Sports Traumatol Arthrosc. 2012;20(2):232–238. doi: 10.1007/s00167-011-1603-0. [DOI] [PubMed] [Google Scholar]
- 14.Li W., Wang Q., Wang F., Zhang Y., Ma L., Dong J. Femoral trochlear dysplasia after patellar dislocation in rabbits. Knee. 2013;20(6):485–489. doi: 10.1016/j.knee.2013.05.016. [DOI] [PubMed] [Google Scholar]
- 15.Wang S., Ji G., Yang X., Wang X., Wang R., Li M. Femoral trochlear groove development after patellar subluxation and early reduction in growing rabbits. Knee Surg Sports Traumatol Arthrosc. 2016;24(1):247–253. doi: 10.1007/s00167-014-3372-z. [DOI] [PubMed] [Google Scholar]
- 16.Diederichs G., Kohliz T., Kornaropoulos E., Heller M.O., Vollnberg B., Scheffler S. Magnetic resonance imaging analysis of rotational alignment in patients with patellar dislocations. Am J Sports Med. 2013;41:51–57. doi: 10.1177/0363546512464691. [DOI] [PubMed] [Google Scholar]
- 17.Prakash J., Seon J.K., Woo S.H., Jin C., Song E.K. Comparison of radiological parameters between normal and patellar dislocation groups in korean population: a rotational profile CT-based study. Knee Surg Relat Res. 2016;28:302–311. doi: 10.5792/ksrr.16.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Takagi S., Sato T., Watanabe S., Tanifuji O., Mochizuki T., Omori G. Alignment in the transverse plane, but not sagittal or coronal plane, affects the risk of recurrent patella dislocation. Knee Surg Sports Traumatol Arthrosc. 2018;26(10):2891–2898. doi: 10.1007/s00167-017-4806-1. [DOI] [PubMed] [Google Scholar]
- 19.Masoud I., Shapiro F., Kent R., Moses A. A longitudinal study of the growth of the New Zealand white rabbit: cumulative and biweekly incremental growth rates for body length, body weight, femoral length, and tibial length. J Orthop Res. 1986;4:221–231. doi: 10.1002/jor.1100040211. [DOI] [PubMed] [Google Scholar]
- 20.Hingelbaum S., Best R., Huth J., Wagner D., Bauer G., Mauch F. The TT-TG index: a new knee size adjusted measure method to determine the TT-TG distance. Knee Surg Sports Traumatol Arthrosc. 2014;22:2388–2395. doi: 10.1007/s00167-014-3204-1. [DOI] [PubMed] [Google Scholar]
- 21.Liebensteiner M.C., Ressler J., Seitlinger G., Djurdjevic T., El Attal R., Ferlic P.W. High femoral anteversion is related to femoral trochlea dysplasia. Arthroscopy. 2016;32(11):2295–2299. doi: 10.1016/j.arthro.2016.03.023. [DOI] [PubMed] [Google Scholar]
- 22.Kaymaz B., Atay O.A., Ergen F.B., Mermerkaya M.U., Olgun Z.D., Atesok K. Development of the femoral trochlear groove in rabbits with patellar malposition. Knee Surg Sports Traumatol Arthrosc. 2013;21(8):1841–1848. doi: 10.1007/s00167-012-2163-7. [DOI] [PubMed] [Google Scholar]
- 23.Rebolledo B.J., Nam D., Cross M.B., Green D.W., Sculco T.P. Familial association of femoral trochlear dysplasia with recurrent bilateral patellar dislocation. Orthopedics. 2012;35(4):e574–e579. doi: 10.3928/01477447-20120327-30. [DOI] [PubMed] [Google Scholar]
- 24.Chan CJ, Chau YJ, Woo SB, Luk HM, Lo IF. Familial patellar dislocation associated with t(15;20) (q24;q13.1). J Orthop Surg (Hong Kong) 2018;26(2):2309499018777026. [DOI] [PubMed]
- 25.Liska F., von Deimling C., Otto A., Willinger L., Kellner R., Imhoff A.B. Distal femoral torsional osteotomy increases the contact pressure of the medial patellofemoral joint in biomechanical analysis. Knee Surg Sports Traumatol Arthrosc. 2019;27(7):2328–2333. doi: 10.1007/s00167-018-5165-2. [DOI] [PubMed] [Google Scholar]
- 26.Liao T.C., Yang N., Ho K.Y., Farrokhi S., Powers C.M. Femur rotation increases patella cartilage stress in females with patellofemoral pain. Med Sci Sports Exerc. 2015;47(9):1775–1780. doi: 10.1249/MSS.0000000000000617. [DOI] [PubMed] [Google Scholar]
- 27.Christoforakis J., Bull A.M., Strachan R.K., Shymkiw R., Senavongse W., Amis A.A. Effects of lateral retinacular release on the lateral stability of the patella. Knee Surg Sports Traumatol Arthrosc. 2006;14(3):273–277. doi: 10.1007/s00167-005-0699-5. [DOI] [PubMed] [Google Scholar]
- 28.Nelitz M., Wehner T., Steiner M., Dürselen L., Lippacher S. The effects of femoral external derotational osteotomy on frontal plane alignment. Knee Surg Sports Traumatol Arthrosc. 2014;22(11):2740–2746. doi: 10.1007/s00167-013-2618-5. [DOI] [PubMed] [Google Scholar]
- 29.Imhoff F.B., Beitzel K., Zakko P., Obopilwe E., Voss A., Scheiderer B. Derotational osteotomy of the distal femur for the treatment of patellofemoral instability simultaneously leads to the correction of frontal alignment: a laboratory cadaveric study. Orthop J Sports Med. 2018;6(6) doi: 10.1177/2325967118775664. 2325967118775664. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.