Abstract
Patient: Female, 6-year-old
Final Diagnosis: Burkitt’s leukemia
Symptoms: Right iliac fossa pain
Medication: —
Clinical Procedure: Laparoscopic cecectomy
Specialty: Surgery
Objective:
Rare disease
Background:
Appendicitis is the most common cause of an acute abdomen. Approximately 1% of appendicectomies will have an incidental finding of an appendiceal neoplasm. A primary appendiceal lymphoma is extremely rare, and is found in 0.015% of all appendiceal specimens. Burkitt lymphoma is an aggressive B cell lymphoma characterized by translocation and dysregulation of the c-Myc gene. Burkitt leukemia is considered to be an alternative manifestation of the same pathology, and is defined by the presence of >25% Burkitt blasts within the bone marrow. The treatment approaches for Burkitt leukemia/lymphoma are similar.
Case Report:
A 6-year old girl presented with a history, examination, and radiological imaging consistent with acute appendicitis. An inflamed, edematous appendix was identified intraoperatively, and a cecectomy was performed. Histopathological investigations demonstrated Burkitt leukemia with isolated extra-nodal involvement of the appendix. The patient was subsequently started on a multi-agent steroid and chemotherapy regimen. A literature review was performed, identifying cases of Burkitt leukemia/lymphoma presenting as appendicitis.
Conclusions:
This case highlights the importance of clinical vigilance and routine specimen histopathology review, and explores key management considerations associated with the incidental diagnosis of Burkitt leukemia/lymphoma.
MeSH Keywords: Appendiceal Neoplasms, Appendicitis, Burkitt Lymphoma
Background
Appendicitis is the most common cause of acute abdomen, and has a lifetime risk of approximately 7% [1]. The diagnosis of this pathology is traditionally made on a clinical basis, but may be supported by laboratory and imaging investigations. Subsequent management is dependent on the clinical context, but typically involves surgical intervention with an appendicectomy.
Approximately 1% of appendicectomies have an incidental finding of an appendiceal neoplasm [2]. A primary appendiceal lymphoma (PAL) is extremely rare, and is found in 0.015% of all appendiceal specimens [3]. A case series of 116 patients with PAL found that the predominant histological subtype was diffuse large B cell lymphoma (34.5%), followed by Burkitt lymphoma (25.9%) [4].
Burkitt lymphoma is an aggressive B cell lymphoma characterized by the translocation and dysregulation of the c-Myc gene. There are 3 main types of Burkitt lymphoma: endemic, sporadic, and immunodeficiency-associated [5]. The sporadic form typically manifests as an abdominal presentation [6], with the particular symptoms experienced by the patient dependent on the anatomical region affected. Burkitt leukemia is considered to be an alternative manifestation of the same pathology, and can present with or without lymphomatous involvement. This terminology is used when there are >25% Burkitt blasts within the bone marrow.
A case of a Burkitt leukemia with isolated extra-nodal involvement of the appendix masquerading as acute appendicitis in a 6-year-old girl is presented. We performed a literature review on this topic and highlight several key clinical considerations associated with this rare presentation.
Case Report
A 6-year-old girl was referred to the Emergency Department (ED) by her family physician (FP) with a 1-day history of right iliac fossa pain, with associated subjective fevers and anorexia. She did not have any comorbidities, prior surgical history, or developmental issues. On examination, there was marked right iliac fossa tenderness with focal peritonism. The remainder of the abdomen was soft, with no features of generalized peritonitis. Vital signs were within normal limits during the examination period. An ultrasound performed earlier by the FP demonstrated a severely inflamed appendix surrounded by multiple enlarged reactive lymph nodes (Figure 1). The patient was kept fasted, and she was started on intravenous fluids and antibiotics. Laboratory investigations were unavailable at the time of admission, as the patient presented in the evening and there are no after-hours pathology services available on site. A decision was made by the attending surgeon to proceed with a laparoscopic appendicectomy given the convincing clinical and sonographic findings of acute appendicitis. Intraoperatively, a significantly inflamed, edematous appendix without obvious perforation was identified in the subcecal position. There was concern of a synchronous pathological process of unclear etiology given the abnormally thickened intraoperative appearance of the entire appendix (Figure 2). A decision was made to proceed to a cecectomy using a laparoscopic stapling device to ensure complete resection of the pathological process by taking a sliver of the cecum along with the appendix. Generalized turbid free fluid and features of small-bowel ileus were noted within the abdomen. The remainder of the intra-abdominal and gynecological organs appeared unremarkable. The specimen was sent for histopathological analysis.
Figure 1.
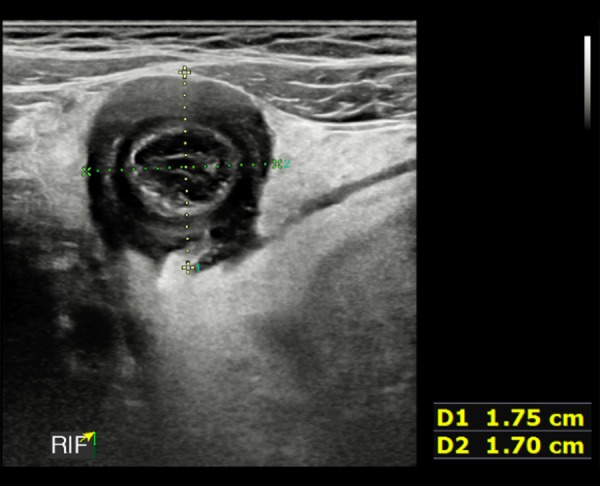
An ultrasound (US) view of the appendix, demonstrating significant inflammation. The AP dimension of the edematous bowel wall measures approximately 17 mm.
Figure 2.

The resected inflamed edematous appendix measuring 125 mm in length and up to 20 mm in diameter.
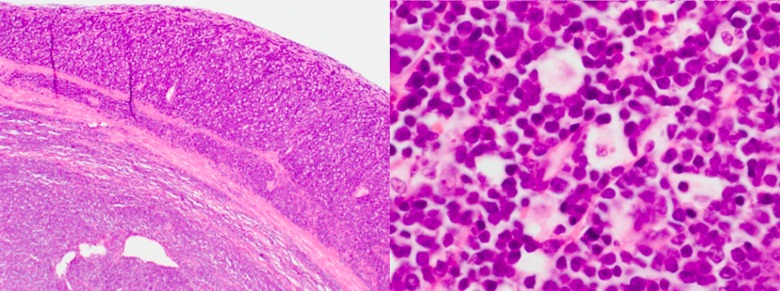
Postoperatively, the patient was sent to the pediatric ward and was continued on intravenous antibiotics due to the generalized purulent peritonitis. The patient subsequently recovered well without complications. She had returned to her usual baseline by postoperative day 2 and was flagged for discharge with oral antibiotics. However, prior to her departure, the surgical team received an urgent phone call from the Pathology Department regarding the incidental finding of a high-grade lymphoma within the surgical specimen. The hematoxylin and eosin slide demonstrated a monotonous sheet of lymphoid cells with scattered macrophages, resulting in a “starry sky” appearance diffusely infiltrating the entire specimen (Figure 3). There was no evidence of any appendiceal inflammation. Complete blood count (CBC) demonstrated a white cell count of 44.6×103, with a predominance of large immature lymphoid cells. Further immunohistochemistry testing demonstrated the cells were positive for CD20, CD10, and Bcl6. The Ki67 showed a proliferative index >95%. Fluorescence in-situ hybridization (FISH) studies confirmed a t(8;14) c-Myc translocation. These findings are consistent with Burkitt lymphoma.
Figure 3.
A hematoxylin and eosin slide demonstrating a sea of medium-to-large lymphoid cells and scattered tingible body macrophages. This “starry sky” appearance is suggestive of a high-grade malignant lymphoma, likely Burkitt lymphoma.
The patient was transferred to a tertiary pediatric hospital to facilitate further workup and management. Adequate IV hydration and close monitoring of electrolytes were warranted given the risk of tumor lysis syndrome. A positron emission tomography/computed tomography (PET/CT) scan did not demonstrate evidence of residual disease at the cecum, or any other nodal or distant disease above or below the diaphragm. Bone marrow biopsy demonstrated heavy (>90%) marrow infiltration by Burkitt blasts. The patient was started on a multi-agent steroid and chemotherapy (ANHL1131) regimen by the pediatric oncology team. The patient responded well to treatment and had a prolonged hospital stay secondary to chemo-therapy-related complications. Her long-term prognosis is considered to be favourable.
Discussion
Acute appendicitis (AA) is traditionally a clinical diagnosis [7], but the workup can be supported by laboratory and radiological investigations. The patient in this case presented with symptoms classical for AA, with supporting ultrasound imaging suggestive of this pathology.
The earliest sign of an atypical pathological process was identified intraoperatively with the significantly thickened appearance of the appendix. This triggered a heightened clinical vigilance, resulting in the use of a staple cecectomy to ensure complete resection of the unknown pathological process. The lack of preoperative laboratory investigations also contributed to the diagnostic difficulties encountered in this case – a white cell count of 44.6 x103 with a predominance of large immature lymphoid cells is strongly suggestive of a hematological pathology.
A diagnosis of Burkitt lymphoma is dependent on a combination of histologic (diffuse lymphoid infiltration with scattered macrophages), immunophenotypic (CD20, CD10, Bcl6 positive, and Ki-67 near 100%), and genetic features (c-Myc translocation) [5]. All of these features were identified in the present case. The heavy infiltration of Burkitt blasts within the marrow meets the criteria for the disease to be considered a Burkitt leukemia (>25% Burkitt blasts within the bone marrow) [8]. Therefore, this case was a Burkitt leukemia with isolated extra-nodal involvement of the appendix. Burkitt lymphoma/leukemia is generally considered to be different manifestations of the same pathology, and have similar treatment strategies. Our patient was started on a multi-agent chemotherapy regimen concordant with guideline recommendations.
A literature review of Burkitt leukemia/lymphoma mimicking appendicitis was performed, finding 30 cases involving Burkitt lymphoma (Table 1). None of these cases were documented to have met the marrow involvement threshold to be considered Burkitt leukemia. The demographics of this cohort were predominantly male (n=20/30, 66.7%), with the average age at presentation being 20.4 years old. The majority of cases clinically presented as classical acute appendicitis (n=22/29, 89.7%). The remainder of cases (n=7) presented atypically, but had subsequent radiological investigations demonstrating appendicitis. A palpable right iliac fossa (RIF) mass was identified in 21.4% of cases (n=6/28) and was usually assumed to be an appendicitis-related abscess. The overall preoperative imaging rate using at least 1 modality was 64.3% (18/28). Plain-film radiology (XR) was used in 4 cases, ultrasound (US) in 13 cases, and CT in 11 cases. An appendectomy (either open or laparoscopic) was the most commonly performed index procedure (n=19/29, 65.5%). An index right hemicolectomy was performed in 6 cases (20.7%), while a cecectomy/ileocecal re-section was performed in 2 cases (6.9%). Twenty-three cases demonstrated evidence of appendiceal involvement.
Table 1.
A list of case reports published in the medical literature of Burkitt lymphoma mimicking appendicitis.
| Author/Year | Age/Sex | Ethnicity | Clinical Presentation | RIF mass | Preop imaging | Index procedure | Burkitt location |
|---|---|---|---|---|---|---|---|
| Sin/1980 [10] | 8/M | Caucasian | Acute appendicitis (AA) | Yes | No | Appendectomy | Appendix |
| Sin/1980 [10] | 10/M | Caucasian | AA | No | No | Appendectomy | Appendix |
| Nanji/1983 [11] | 22/M | Not available (NA) | AA | No | No | Appendectomy | Appendix |
| Ghani/1984 [12] | 22/M | Malay | AA | No | No | Appendectomy | Appendix |
| Caine/1990 [13] | 3/F | Caucasian | AA | No | XR (chest+abdo) | Appendectomy | Appendix |
| Carstensen/1993 [14] | 17/M | NA | AA | Yes | No | Cecectomy | Appendix |
| Krepel/1996 [15] | 22/M | NA | NA | NA | NA | NA | NA |
| Bissen/2002 [16] | 12/M | European | AA | No | US CT |
Right hemicolectomy | NA |
| Jaganmohan/2006 [17] | 60/M | Caucasian | AA | No | CT | Appendectomy | Appendix |
| Biswas/2006 [18] | 14/M | NA | AA | No | No | Right hemicolectomy | Terminal ileum |
| Abdalla/2010 [19] | 49/M | NA | RIF pain+ right back pain + hematuria | No | XR (IVP+KUB) CT | Right hemicolectomy | Appendix, invading cecum |
| Bhardwaj/2010 [20] | 14/M | Caucasian | AA | Yes | No | Right hemicolectomy | Terminal ileum |
| Wang/2010 [21] | 10/M | NA | AA | No | XR (Abdo) US CT |
Appendectomy | Ileocecal |
| Goncalves/2012 [22] | 14/M | Caucasian | AA | No | US | Appendectomy | Appendix |
| Ryan/2013 [23] | 4/M | NA | AA | Yes | XR (Abdo) US CT |
Incision + drainage of purulent fluid | Appendix, sigmoid colon + mesentery, proximal rectum |
| Weledjil/2014 [24] | 13/F | NA | RIF pain years | No | US | Appendectomy | Appendix |
| Weledjil/2014 [24] | 18/F | NA | Vague RIF pain, subsequent cecal fistula | No | No | Appendectomy | Ileocecal |
| Ziari/2014 [25] | 10/M | NA | Fatigue 3 months RIF pain 2 weeks | No | US | Appendectomy | Appendix |
| Ziari/2014 [25] | 23/M | NA | AA | No | US CT |
Appendectomy | Appendix |
| Ziari/2014 [25] | 24/F | NA | AA | No | US | Appendectomy | Appendix |
| Vahhac/2015 [26] | 16/F | NA | AA | No | US CT |
Right hemicolectomy | Appendix, invading cecum |
| Vrancx/2015 [27] | 17/M | NA | Atypical RIF pain | No | US | Excisional biopsy | Terminal ileum |
| Sangma/2016 [28] | 27/F | NA | RIF pain 2 months | Yes | US CT |
Right hemicolectomy | Appendix, ileum, caecum |
| Chamarthy/2016 [29] | 53/M | NA | Generalized abdominal pain + left flank pain | No | CT | Appendectomy | Appendix, duodenum |
| Loh/2017 [30] | 20/M | Middle eastern | AA | NA | NA | Appendectomy | Appendix |
| Mastumara/2017 [31] | 16/M | NA | AA | No | CT | Appendectomy | Appendix |
| de Morais/2018 [32] | 36/M | NA | AA | No | No | Appendectomy | Appendix |
| Hui/2018 [33] | 13/F | NA | AA | No | US CT |
Appendectomy + left salpingo-oophorectomy | Appendix left ovary + oviduct |
| García-Norzagaraya/2019 [34] | 40/F | NA | AA | Yes | No | Appendectomy | Appendix |
| Mimery/2019 | 6/F | Sri Lankan | AA | No | US | Cecectomy | Appendix |
Several management learning points may be explored within this case. We recommend the use of imaging for patients who have an atypical presentation of AA, or a palpable RIF mass, to exclude an alternative pathology. Moreover, there are diagnostic benefits of imaging young females to exclude gynecological mimics of appendicitis. There is evidence that an increased appendiceal diameter (>3 cm) on imaging is suggestive of an underlying neoplastic process [9].
It is important to monitor for tumor lysis syndrome (TLS), an oncological emergency that arises due to the rapid release of intracellular tumor contents. Although this phenomenon typically occurs after chemotherapy commencement, spontaneous Burkitt lymphoma-associated TLS has been described in the literature, and is likely related to its highly aggressive nature and short tumor doubling time (24–48 h) [5]. Active monitoring of serum electrolytes and adequate fluid resuscitation are essential to prevent the development of arrhythmogenesis, acute renal failure, and seizures.
Conclusions
We present the case of a rare pathology mimicking a common general surgical presentation. This case highlights the importance of clinical vigilance and routine specimen histopathology review, and explores key management considerations associated with the incidental diagnosis of Burkitt leukemia/lymphoma.
Footnotes
Department and Institution where work was done
Department of Surgery, Gladstone Hospital, Gladstone, Australia
Conflicts of interest
None.
References:
- 1.Ergul E, Ucar A, Ozgun Y, et al. Importance of family history and genetics for the prediction of acute appendicitis. Internet J Surg. 2007;10(1):635–37. [Google Scholar]
- 2.Connor S, Hanna GB, Frizelle FA. Appendiceal tumors: Retrospective clinicopathologic analysis of appendiceal tumors from 7,970 appendectomies. Dis Colon Rectum. 1998;41(1):75–80. doi: 10.1007/BF02236899. [DOI] [PubMed] [Google Scholar]
- 3.Collins D. 71,000 Human appendix specimens. A final report, summarizing forty years’ study. Am J Proctol. 1963;14:265–81. [PubMed] [Google Scholar]
- 4.Ayub A, Santana-Rodríguez N, Raad W, Bhora FY. Primary appendiceal lymphoma: Clinical characteristics and outcomes of 116 patients. J Surg Res. 2017;207:174–80. doi: 10.1016/j.jss.2016.08.079. [DOI] [PubMed] [Google Scholar]
- 5.Ferry J. Burkitt’s lymphoma: Clinicopathologic features and differential diagnosis. Oncologist. 2006;11(4):375–83. doi: 10.1634/theoncologist.11-4-375. [DOI] [PubMed] [Google Scholar]
- 6.Blum K, Lozanski G, Byrd J. Adult Burkitt leukemia and lymphoma. Blood. 2004;104(10):3009–20. doi: 10.1182/blood-2004-02-0405. [DOI] [PubMed] [Google Scholar]
- 7.Humes D, Simpon J. Acute appendicitis. BMJ. 2006;333(7567):530–34. doi: 10.1136/bmj.38940.664363.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hecht J, Aster J. Molecular biology of Burkitt’s lymphoma. J Clin Oncol. 2000;18(21):3707–21. doi: 10.1200/JCO.2000.18.21.3707. [DOI] [PubMed] [Google Scholar]
- 9.Pickhardt P, Levy A, Rohrmann C, et al. Non-Hodgkin lymphoma of the appendix: Clinical and CT findings with pathologic correlation. Am J Roentgenol. 2002;187:1123–27. doi: 10.2214/ajr.178.5.1781123. [DOI] [PubMed] [Google Scholar]
- 10.Sin I, Ling E, Prentice R. Burkitt’s lymphoma of the appendix: Report of two cases. Hum Pathol. 1980;11(5):465–70. doi: 10.1016/s0046-8177(80)80055-4. [DOI] [PubMed] [Google Scholar]
- 11.Nanji A, Anderson F. Burkitt’s lymphoma with acute appendicitis. Arch Surg. 1983;118(11):1352. doi: 10.1001/archsurg.1983.01390110094023. [DOI] [PubMed] [Google Scholar]
- 12.Ghani S, Syed N, Tan P. A rare cause of acute appendicitis: Burkitt’s lymphoma of the appendix. Med J Malaysia. 1984;39(4):311–13. [PubMed] [Google Scholar]
- 13.Caine Y, Peylan-Ramu N, Livoff A, Schiller M. Primary Burkitt’s lymphoma of the appendix. Z Kinderchir. 1990;45(4):251–52. doi: 10.1055/s-2008-1042594. [DOI] [PubMed] [Google Scholar]
- 14.Carstensen K, Hoffmann E. [Primary malignant lymphoma in the appendix vermiformis] Ugeskr Laeger. 1993;155(32):2477–78. [in Danish] [PubMed] [Google Scholar]
- 15.Krepel V, van Erp W, Vlasveld L. Lymphoma of the appendix: Sonographic findings. Am J Roentgenol. 1996;167(1):286. doi: 10.2214/ajr.167.1.8659414. [DOI] [PubMed] [Google Scholar]
- 16.Bissen L, Brasseur R, Azagra J, Deirée P. Burkitt’s lymphoma of the appendix. JBR-BTR. 2002;85(5):257–59. [PubMed] [Google Scholar]
- 17.Jaganmohan S, Chauvin R, Burton G. Primary Burkitt’s lymphoma of the appendix presenting as acute appendicitis. Am J Gastroenterol. 2006;101:s146–47. [Google Scholar]
- 18.Biswas S. Report of a case of abdominal Burkitt’s lymphoma presenting as localised right iliac fossa pain mimicking acute appendicitis. Internet Journal of Surgery. 2006;9(1) [Google Scholar]
- 19.Abdalla M, El-Hennawy H. Unusual presentation for primary appendiceal lymphoma: A case report. Indian J Surg. 2010;72(Suppl. 1):289–92. doi: 10.1007/s12262-010-0093-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bhardwaj N, Bains S, Ortonowski G, Murphy P. A case of Burkitt’s lymphoma presenting as suspected acute appendicitis. Afr J Paediatr Surg. 2010;7(3):214–15. doi: 10.4103/0189-6725.70433. [DOI] [PubMed] [Google Scholar]
- 21.Wang S, Huang F, Wu C, et al. Ileocecal Burkitt’s lymphoma presenting as ileocolic intussusception with appendiceal invagination and acute appendicitis. J Formos Med Assoc. 2010;109(6):476–79. doi: 10.1016/S0929-6646(10)60080-0. [DOI] [PubMed] [Google Scholar]
- 22.Gonçalves JP, Cerqueira A, Antunes H, et al. Ileocecal Burkitt’s lymphoma presenting as acute appendicitis: A case report. Int J Case Rep Imag. 2012;3(11):32–34. [Google Scholar]
- 23.Ryan D, Friedmann A, Schmitz M, Ryan R. Case 11-2013 – a 4-year-old boy with fever and abdominal pain. N Engl J Med. 2013;368:1435–44. doi: 10.1056/NEJMcpc1209304. [DOI] [PubMed] [Google Scholar]
- 24.Weledji E, Ngowe M, Abba J. Burkitt’s lymphoma masquerading as appendicitis – two case reports and review of the literature. World J Surg Oncol. 2014;12:187. doi: 10.1186/1477-7819-12-187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ziari K, Alizadeh K, Rahmani O, Kazemi M. Primary lymphoma of appendix: Report of three cases and review of literature. Iran J Pathol. 2014;9(2):160–68. [Google Scholar]
- 26.Vahhac A, Nurettin A, Nilgün S, et al. Burkitt lymphoma of appendix not presenting with acute abdomen: Case report. Turkiye Klinikleri Journal of Case Report. 2015;23(4):461–64. [Google Scholar]
- 27.Vrancx S, Van de Sande J, Vanclooster P, et al. Burkitt lymphoma mimicking an acute appendicitis in a 17 years old boy: A case report. Acta Chir Belg. 2015;115(4):306–9. doi: 10.1080/00015458.2015.11681117. [DOI] [PubMed] [Google Scholar]
- 28.Sangma M, Dasiah S, Ashok A. Ileo-colic Burkitt lymphoma in a young adult female – a case report. J Clin Diagn Res. 2016;10(4):11–12. doi: 10.7860/JCDR/2016/19105.7582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chamarthy P, Moradi D, Bhandari B. Gastrointestinal Burkitt’s lymphoma initially presenting as nephrolithiasis and appendicitis. Am J Gastroenterol. 2016;111:S1120–21. [Google Scholar]
- 30.Loh J, Santos L. Burkitt’s lymphoma presenting as acute appendicitis – a case report and review of the literature. Pathology. 2017;49:S77. [Google Scholar]
- 31.Matsumura R, Osugi Y, Noma H, et al. [A case of primary Burkitt lymphoma of the appendix] Nihon ShMni Ketsueki Gan Gakkai Zasshi. 2017;54(2):133–37. [in Japanese] [Google Scholar]
- 32.de Morais S, Mikhael B, Németh S, et al. Burkitt’s lymphoma presenting as acute appendicitis: A case report. J Surg Case Rep. 2018;2018(6):ryj131. doi: 10.1093/jscr/rjy131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hui D, Rewerska J, Slater B. Appendiceal and ovarian Burkitt’s lymphoma presenting as acute appendicitis. J Pediatr Surg Case Rep. 2018;32:17–20. [Google Scholar]
- 34.García-Norzagaray J, Villalobos-López J, Flores-Nájera H, et al. Primary lymphoma of the appendix: A case report and review of the literature. Rev Gastroenterol Mex. 2019;84(2):254–57. doi: 10.1016/j.rgmx.2018.04.001. [DOI] [PubMed] [Google Scholar]