Abstract
Background
Psychosocial and emotional factors are important in childhood asthma. Nevertheless, drug therapy alone continues to be the main treatment. Treatment programmes that include behavioural or psychological interventions have been developed to improve disturbed family relations in the families of children with severe asthma. These approaches have been extended to examine the efficacy of family therapy to treat childhood asthma in a wider group of patients. This review systematically examines these studies.
Objectives
Recognition that asthma can be associated with emotional disturbances has led to the investigation of the role of family therapy in reducing the symptoms and impact of asthma in children. The objective of this review was to assess the effects of family therapy as an adjunct to medication for the treatment of asthma in children.
Search methods
We searched the Cochrane Airways Group Specialised Register of trials, and checked the reference lists in trial reports and review articles. The most recent search was carried out in January 2007.
Selection criteria
Randomised trials comparing children undergoing systematic therapy focusing on the family in conjunction with asthma medication, with children taking asthma medication only.
Data collection and analysis
Two reviwers (JY and CS) applied the study inclusion criteria.
Main results
Two trials with a total of 55 children were included. It was not possible to combine the findings of these two studies because of differences in outcome measures used. In one study, gas volume, peak expiratory flow rate and daytime wheeze showed improvement in family therapy patients compared to controls. In the other study, there was an improvement in overall clinical assessment and number of functionally impaired days in the patients receiving family therapy. There was no difference in forced expiratory volume or medication use in both studies.
Authors' conclusions
There is some indication that family therapy may be a useful adjunct to medication for children with asthma. This conclusion is limited by small study sizes and lack of standardisation in the choice of outcome measures.
Plain language summary
Family therapy for asthma in children
Psychological factors may have an effect on asthma in children, or its severity. As some children with families who are having problems have severe asthma, family therapy has been tried. The aim is to resolve any problems there might be in a family, in case they are causing the child stress and then making asthma worse. The review found some evidence from two trials that family therapy (in addition to standard asthma treatments) might help reduce a child's asthma symptoms, but more research is needed to be certain.
Background
The incidence of childhood asthma has increased annually at a rapid rate over the last 20 years. A variety of factors have been implicated in the pathogenesis of bronchial asthma including allergies, infections, endocrinological disorders, genetic predisposition and, more recently, psychological elements. Although psychological factors are widely acknowledged to play a part both in precipitating episodes of asthma, and in the control of symptoms, pharmacological treatment alone continues to be the main treatment, and therefore the focus of most research. Recently, however, traditional medical models upholding a split between the "psyche" and the "soma" are being replaced by those which recognise the powerful influences of the mind on the body. Similarly, the need for integrated treatment models which consider behavioural or psychological interventions in addition to pharmacotherapy are well documented (Cluss 1986; Lehrer 1992; Onnis 1984; Molinari 1994; Towns 1994)
Studies which do acknowledge psychosocial aspects to the disease range from cognitive behavioural approaches, to education programmes, relaxation techniques, autogenic therapy, and rational emotive behaviour modification as an adjunct to medication. However, such studies, although recognising that asthma has strong associations with emotional disturbances, have been conducted mainly with adults.
Of the few studies which examine psychological influences in childhood asthma, psychosocial and emotional factors are regarded as important in the most severely ill of asthmatic children (Gustafsson 1986; Lask 1979). A child's chronic illness can place psychological burdens on both child and family (Newacheck 1991; Pless 1991; Steinhauer 1974). In addition, Weil (Weil 1999) concluded that two psychological variables, child and carer mental health, were important predictors of subsequent asthma morbidity. The earliest research conducted in the 1970s indicated the presence of disturbed family relations in the families of children with severe asthma (Liebman 1974; Liebman 1976). This prompted a limited number of trials to be conducted in the area of family therapy.
The theoretical basis which underpins the systemic view of family therapy presupposes that "symptoms" can be the product of a dysfunctional family system. Therapeutic intervention is used to alert the family system to its dysfunctional behaviours and to empower it to adaptively overcome the difficulties which give rise to the symptoms. The body of research undertaken so far has been based on a structural family therapy perspective which assumes that relationships between family members adhere to certain patterns, which are often maladaptive to the current life situation. Systemic theories regard phenomena in terms of circularity, rather than in the linear terms of cause and effect inherent to the medical model of illness. Therefore asthma is assumed to be both a symptom of the family dysfunction, and a contributor to it (Lask 1979). Family therapy has been used to decrease the symptoms and impact of asthma.
Objectives
The objective of this review is to test whether family therapy as an adjunct to traditional medication can be shown to have a significant effect in reducing the symptoms and impact of asthma in children.
Methods
Criteria for considering studies for this review
Types of studies
Clinical trials included were randomised and controlled. Authors have been contacted to ascertain randomisation techniques. Trials included in this review compared family therapy + pharmacological intervention vs pharmacological intervention alone.
Types of participants
Chronically asthmatic children receiving medication who were treated at hospital outpatient departments or clinics, and their families.
Types of interventions
Any family therapy based on systemic theories which focus on the whole family and which aim to arrive at an understanding of the role of the symptoms of asthma within this system, in an attempt to understand dysfunctional family interaction and precipitate change. Only trials which included family therapists trained in and working within this framework were considered. Children undergoing this therapy were also taking prescribed medication. Control group children were taking prescribed medication only, and received no family therapy intervention .
Types of outcome measures
1. Health care utilisation 2. Lung function 2. Medication use 4. Asthma symptoms 5. Child absenteeism from school 6. Psychological indicators from questionnaires (e.g. coping skills, anxiety, depression, locus of control, self‐esteem, self efficacy, quality of life and psychological status) 7. Change of behavior as measured by behavior scales
Search methods for identification of studies
Electronic searches
Trials were identified using the Cochrane Airways Group Specialised Register of trials, which is derived from systematic searches of bibliographic databases, including the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, EMBASE and CINAHL, and handsearching of respiratory journals and meeting abstracts. All records in the Specialised Register coded as 'asthma' were searched using the following terms:
psychotherap* or (psych* or famil* or complian* or anxiet* or comply and (therap*))
The latest search was run in January 2007 and will be updated annually.
Searching other resources
Reference lists of primary studies and review articles were checked for additional references.
Data collection and analysis
Selection of studies
The literature search identified thirty four relevant studies. Two independent reviewers (JY and CS) established whether each study met the inclusion criteria.
Data extraction and management
During data extraction and through personal communication with the authors, it was noted that for the analysis of some outcomes, had employed a cross‐over design. Since it had previously been decided to enter onto 'Review Manager' only analyses which maintained the study groups according to the original randomization procedure, the analyses performed after cross‐over were not included and readers are referred to the original paper for this information.
Assessment of risk of bias in included studies
The methodological quality of the studies (allocation concealment) was independently assessed by two reviewers (JY and CS) using the following criteria for allocation concealment: Grade A: Adequate concealment Grade B: Uncertain Grade C: Clearly inadequate concealment Grade D: Not used
There were no disagreements on ratings given to the studies.
Each study was also assessed using the modified 0 to 5 scale developed by Jadad 1996 and summarised as follows: 1. Was the study described as randomised (1=yes; 0=no) 2. Was the outcome assessment blinded (1=yes; 0=no) 3. Was there a description of withdrawals and dropouts (1=yes; 0=no) 4. Was the method of randomisation well described and appropriate (1=yes; 0=no) 5. Was the method of blinding well described and appropriate (1=yes; 0=no) 6. Deduct on point if methods for randomisation or blinding were inappropriate.
Modification of this scale was essential as, due to the nature of the psychological interventions, it would be difficult to conduct double‐blind trials. Therefore step 2 and 5 'double‐blind' was changed to 'blind'.
Data synthesis
We planned to combined data with Review Manager software.
Results
Description of studies
Two RCTs were included. Between them, a maximum of 55 children with asthma and their families were studied, although not all participants were included in each comparison.
Lask 1979 was a controlled,randomised, unblinded study. Reported outcomes were objective measures of lung function.
Gustafsson 1986 was a controlled, randomised, single blinded study. Reported outcomes were objective measures of lung function and measures of asthma impact: General paediatric assessment; participant reported number of impaired days; participant reported number of nights where a beta2‐agonist was used. Cross‐over data were also reported, but were excluded from this review.
Results of the search
None of the studies reviewed for this update (n = 4) were included. Only the two originally included trials were appropriate for this review (Lask 1979 and Gustafsson 1986).
Included studies
The children from both studies were attending hospital outpatient departments for their asthma symptoms. Children eligible for selection in the trials were required to have asthma symptoms graded as C or D (as defined by where Grade C = children with a continuing history of episodic asthma over a number of years and D = children with a current history of very frequent or chronic unremitting asthma). The children were aged between 4 and 15 years. The duration of illness was only reported in the study by Gustafsson 1986, (mean = 7 years). Three families had more than one asthmatic child and all were included in the assessments. All children used bronchodilators, and some children were also using inhaled steroids. Children fitting these criteria and their families were selected for the trials.
Cultural setting
One study was conducted at a London postgraduate teaching hospital (Lask 1979) and the other at a University Hospital in Sweden (Gustafsson 1986).
Description of interventions
Neither trial reports on the training or background of the clinicians who gave the family therapy. Both trials assume the importance of therapists meeting the whole or part of the family for effective therapeutic intervention. The role of the asthma symptoms within the family system was explored in both trials. Focus was on specific themes such as the varying attitudes to the illness, the doctor and the medication, the fear of death and the experiencing of painful and frightening emotions (Lask 1979) in an attempt at enhancing communication between family members about the emotional impact of the disease (Gustafsson 1986).
The authors drew upon different theories in their explanations of the aims of family therapy for this group. The paper by Gustafsson 1986 draws on theories from the structural family therapy model which conceptualises families in terms of boundaries, hierarchies, and sub‐systems. The strengthening of boundaries between individuals and hierarchical sub‐systems, and the revelation of hidden conflicts is thereby assumed to alter dysfunctional patterns of interaction between family members. In this way the source of family tension is reduced or re‐routed away from the asthmatic child. The paper by Lask 1979 suggests that stresses in the family are alleviated by focusing on themes and attitudes towards the illness. In turn the attitudes of the family may be altered from the extreme to the more realistic, thus helping to promote an improvement in the psychological well‐being of the family.
Description of Study Design
In both studies parallel groups were randomly allocated to either an experimental group which received family therapy in addition to their usual pharmacological treatment, or a control group which received pharmacological treatment alone.
OUTCOMES
Data from Gustafsson 1986 is presented in terms of the numbers of patients who have 'improved', 'deteriorated' or remained 'unchanged' for each outcome measure. In the present overview, the 'deteriorated' and 'unchanged' groups were combined and compared with the 'improved' group. In contrast, Lask 1979 present mean scores for their measures. The outcome measures selected for examination by the reviewers are presented below, along with the original authors' descriptions.
LUNG FUNCTION
[in all cases, measures are expressed as a percentage of the predicted value for the child's height (% predicted)]:
• Peak expiratory flow rate (PEFR) (Gustafsson 1986) ‐ when and where this was measured and whether it is pre or post medication is not stated.
• Peak expiratory flow rate ‐ morning (PEFR‐am) (Lask 1979) ‐ patients recorded their pre‐medication PEFR for six weeks, the mean value was used in analysis.
• Peak expiratory flow rate ‐ evening (PEFR‐pm) (Lask 1979) ‐ this is the child's mean pre‐medication evening PEFR over six weeks.
• Forced expiratory volume in 0.75 seconds (FEV0.75) (Lask 1979) ‐ this was recorded in clinic. Whether it is pre or post medication is not stated.
• Thoracic gas volume (TGV) (Lask 1979) ‐ this is described as an index of lung overinflation.
MEDICATION USE
• Nights when beta2‐agonists were used (Gustafsson 1986) ‐ how this was calculated is not explicitly described. It is presumed that data comes from the parents' diary cards and an 'improved' patient is one who used beta2‐agonists fewer nights at follow up compared to baseline.
ASTHMA SYMPTOMS
• Functionally impaired days (Gustafsson 1986) ‐ a score of 0‐3, where 2 or more was considered equivalent to reduction of function, was given according to parents' diaries, the capacity of the child to function in daily activities at home and school, and night symptoms.
• Activity Limitation (Lask 1979) ‐ patients' activity limitation on a 0‐3 point scale of ascending severity was recorded during a six week baseline period and for a similar period at one year follow up.
• Day Wheeze (Lask 1979) ‐ as above, patients' day wheeze on a 0‐3 point scale was recorded for two six week periods.
• General paediatric assessment (Gustafsson 1986) ‐ this is a measure of change in the child's condition since the last visit. A score of +1 for improvement, ‐1 for deterioration and 0 for no change was given by a paediatric allergist who was blinded to the randomisation procedure. The score was based on clinical evaluation of: 'severity and frequency of asthma symptoms; amount of medication needed; school attendance; physical activity and the degree of general impairment'.
Risk of bias in included studies
Both studies (Gustafsson 1986; Lask 1979) were allocated a Jadad score of 2 and a concealment score of B. There were no disagreements between the two independent authors.
The method of randomisation was not reported in either study. Both authors were therefore contacted and provided the following information. In the Lask 1979 study, patients were allocated numbers which were placed in a hat. As they were drawn, the numbers were allocated alternately to treatment and control groups. In the Gustafsson 1986 study, participants were divided into pairs matched for age at onset, gender, age and number of siblings. One of each pair was then randomised to either the experimental or control group. The exact method of randomisation was not described.
Effects of interventions
Note: Lask 1979 do not report the number of observations or subjects used for each analysis. They do state, however, that, by the final follow up, there were 18 children in the experimental group and 11 controls, 3 of whom have one outcome measure missing. Where data is missing from Gustafsson 1986 analyses, details are provided with the findings described below.
HEALTH CARE UTILISATION
Gustafsson 1986 reported that emergency hospitalisation days/year decreased in the group receiving family therapy (from 2.67 to 0.17 days/yr, p=0.06).
LUNG FUNCTION
PEFR
No significant difference was found between the PEFR's of the control group and the experimental group in either paper, how ever it was measured. However, Lask 1979 found a significant improvement between baseline and follow‐up in the experimental group, but not in the controls (p<0.005, paired t test). Whether this applied to morning, evening or both measures is not stated. It is reported, however, that the experimental group's mean morning PEFR increased from 53%pred (SD 21) at baseline to 66% pred (SD 20) at follow up. Similarly, their mean evening PEFR increased from 61% pred (SD 20) at baseline to 72 %pred (SD 15) at follow up.
FEV 0.75
No significant change in FEV0.75 was found (Lask 1979).
TGV
A significant decrease in TGV (improvement) was found in the experimental group compared with the control group (p<0.02, rank sum test) (Lask 1979). The median values and inter‐quartile ranges (IQR) used in this test are not reported, however, means and standard deviations are provided. The experimental group's mean TGV was 155%pred (SD 45) at baseline and 146%pred (SD 38) at follow up. The control group's mean TGV was 158%pred (SD 31) at baseline and 176%pred (SD 33) at follow up.
MEDICATION USE
Nights when beta2‐agonists were used ‐ The number of improved compared with unchanged or deteriorated patients was not found to differ between the groups (Gustafsson 1986). Note: this analysis includes data from only 4 of the 9 experimental group patients and 7 of the 8 controls.
ASTHMA SYMPTOMS
Functionally impaired days
There were significantly more improved than unchanged or deteriorated patients in the experimental group compared with the control group (p<0.01, Fisher exact probability test) (Gustafsson 1986). Note: much data was missing from this analysis, of the 9 subjects in the experimental group data from only 3 was included, 7 out of a total of 8 control group subjects provided data for this analysis.
Activity Limitation
There was no significant difference in the change of activity limitation score between the groups (Lask 1979).
Day Wheeze
The day wheeze score was found to have improved in favour of the experimental group (p<0.01, rank sum test) (Lask 1979). Again median values and IQR's are not reported. For the experimental group mean symptom score at baseline is reported as 14 (SD 15) and 7 (SD 8) at follow up. For the control group mean symptom score was 20 (SD 12) at baseline and 21 (SD 11) at follow up.
General paediatric assessment ‐ When improved patients were compared to unchanged and deteriorated patients, improvement in the general paediatric assessment was significantly greater in the experimental group as compared to the control group (p<0.05, Fisher exact probability test) (Gustafsson 1986).
ABSENTEEISM FROM SCHOOL
This outcome was not measured.
PSYCHOLOGICAL AND BEHAVIORAL INDICATORS
These outcomes were not measured.
Discussion
It must be noted that this review concerns itself only with studies which have used family therapy in addition to traditional pharmacological treatments and not as an alternative. Of the only two randomised controlled trials conducted in this area, both demonstrated that children given family therapy in addition to their normal asthma medication show more improvements in their asthma symptoms than those treated with medication alone. Theories suggest that conflicts and relationships between family members are improved, and morbid fears and anxieties alleviated through family therapy interventions. Although the two trials do not show improvements in the same outcomes, a variety of improvements are demonstrated.
A number of our outcomes (health care utilisation (apart from emergency hospitalisations by Gustafsson 1986), school absenteeism, and psychological and behavioral indicators) were not evaluated in the included studies. These outcomes are considered to be important indicators of overall well‐being and therefore, we recommend their inclusion in trials evaluating psychologically orientated interventions as found in a related review of psychological interventions for children with asthma (Yorke 2005)
Lung Function
Compared with controls, an improvement in Thoracic Gas Volume (TGV) was found in those who had family therapy. Peak expiratory flow rate (PEFR) was also found to have improved post family therapy, but within the experimental group and not compared with the control group.
Symptoms
There are also indications that children receiving family therapy suffered fewer functionally impaired days than those who were on prescribed medication alone. Day wheezing also decreased in the experimental group of one study. One of the studies demonstrated improvements in a variety of subjective and objective measures of general health.
Despite the generally positive nature of these findings in favour of family therapy, it must be remembered that they have been derived from the only two randomised controlled trials published in this area. These two studies employed different outcome measures, which were often un‐standardised, ascertained these measures at different baseline and post‐treatment time periods, and used small samples. Missing data from one of the studies undermines the validity of some of the findings. These methodological limitations and restrictions make it difficult to draw conclusions which are generalisable to a wider population.
The assumptions behind family therapy treatment may have different epistemological bases, according to the model used, thus affecting the types of therapeutic interventions that would occur. For instance family therapy given by therapists who believe asthma to have a function in re‐routing conflicts within the family, may use an entirely different approach to those whose aim is to explore the impact of the disease on different family members and their relationships with one another. It is also important to note that the theories and practice of family therapy have changed to include a broader range of perspectives since the two studies included in this review were published. Future studies need to be more specific about the interventions and the models from which they derive in order to help distinguish which psychological phenomena have the most impact on the alleviation of asthma symptoms.
Finally, in only one RCT (Lask 1979) was any attempt made to control for the effects of increased attention alone on the patient and their families. The author told us that each control group patient was seen for 30 minutes longer than normal and was seen more often than normal. This makes it difficult to conclude whether it is the family therapy treatment itself or merely the extra attention on the patients and families, which has generated the improvement in asthma symptoms. Future studies are clearly warranted to compare trials conducted with alternative psychological interventions or 'placebo' + medication with trials using family therapy + medication, in order for these effects to be controlled.
Authors' conclusions
Implications for practice.
Family therapy does appear to produce benefits for children with asthma, but the mechanism by which this occurs is not clear. It should be noted that, since this these trials were performed, the theories and practice of family therapy have changed.
Implications for research.
This appears to be a field of treatment for asthma that warrants further research. This would require larger randomised trials, standardised rating scales and outcome measures, at similar time periods. We aslo recommend the inclusion of outcome measures that represent a child's overall well‐being and enable an analysis as to the economic value of such interventions, such as health care utilisation, school absenteeism, and psychological and behavioral indicators. Such studies are important in the light of the growing body of evidence supporting theories that the impact of asthma is not based upon molecular or organic processes alone, but involves a complex interrelationship between these and psychological phenomena.
What's new
| Date | Event | Description |
|---|---|---|
| 24 July 2008 | Amended | Converted to new review format. |
History
Protocol first published: Issue 1, 1996 Review first published: Issue 2, 1997
| Date | Event | Description |
|---|---|---|
| 20 September 1999 | New citation required and conclusions have changed | Substantive amendment |
Acknowledgements
We would like to thank the staff of the editorial base of the Cochrane Airways Group for assisting us with locating and retrieving relevant literature.
Data and analyses
Comparison 1. FAMILY THERAPY & DRUG THERAPY vs DRUG THERAPY ALONE.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 General paediatric assessment ‐ no improvement | 1 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Totals not selected | |
| 2 General paediatric assessment ‐ deterioration | 1 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Totals not selected | |
| 3 Functionally impaired days ‐ no improvement | 1 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Totals not selected | |
| 4 Functionally impaired days ‐ deterioration | 1 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Totals not selected | |
| 5 Nights B2 inhalers used ‐ no improvement | 1 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Totals not selected | |
| 6 Nights B2 inhalers used ‐ deterioration | 1 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Totals not selected | |
| 7 Peak expiratory flow rate ‐ no improvement | 1 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Totals not selected | |
| 8 Peak expiratory flow rate ‐ deterioration | 1 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Totals not selected | |
| 9 Peak expiratory flow rate ‐ pre‐medication, morning | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 10 Peak expiratory flow rate ‐ pre‐medication, evening | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 11 Forced expiratory volume ‐ (in 0.75 seconds) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 12 Thoracic gas volume | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 13 Day wheeze | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 14 Activity | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
1.1. Analysis.

Comparison 1 FAMILY THERAPY & DRUG THERAPY vs DRUG THERAPY ALONE, Outcome 1 General paediatric assessment ‐ no improvement.
1.2. Analysis.
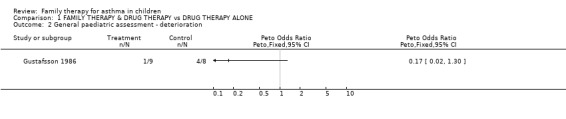
Comparison 1 FAMILY THERAPY & DRUG THERAPY vs DRUG THERAPY ALONE, Outcome 2 General paediatric assessment ‐ deterioration.
1.3. Analysis.
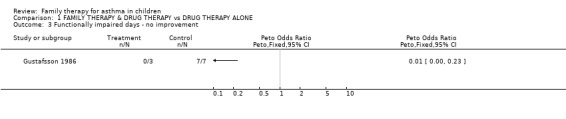
Comparison 1 FAMILY THERAPY & DRUG THERAPY vs DRUG THERAPY ALONE, Outcome 3 Functionally impaired days ‐ no improvement.
1.4. Analysis.
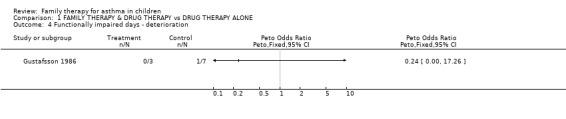
Comparison 1 FAMILY THERAPY & DRUG THERAPY vs DRUG THERAPY ALONE, Outcome 4 Functionally impaired days ‐ deterioration.
1.5. Analysis.
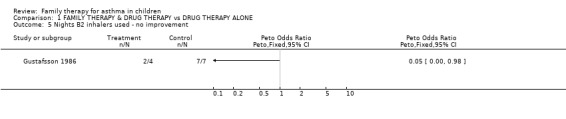
Comparison 1 FAMILY THERAPY & DRUG THERAPY vs DRUG THERAPY ALONE, Outcome 5 Nights B2 inhalers used ‐ no improvement.
1.6. Analysis.
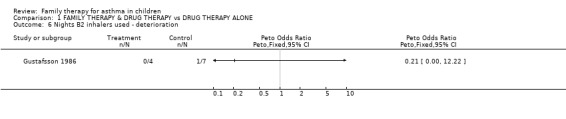
Comparison 1 FAMILY THERAPY & DRUG THERAPY vs DRUG THERAPY ALONE, Outcome 6 Nights B2 inhalers used ‐ deterioration.
1.7. Analysis.
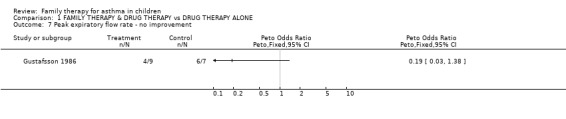
Comparison 1 FAMILY THERAPY & DRUG THERAPY vs DRUG THERAPY ALONE, Outcome 7 Peak expiratory flow rate ‐ no improvement.
1.8. Analysis.
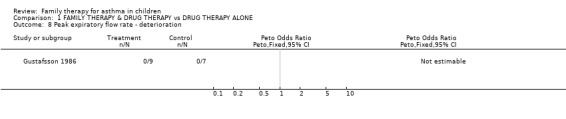
Comparison 1 FAMILY THERAPY & DRUG THERAPY vs DRUG THERAPY ALONE, Outcome 8 Peak expiratory flow rate ‐ deterioration.
1.9. Analysis.
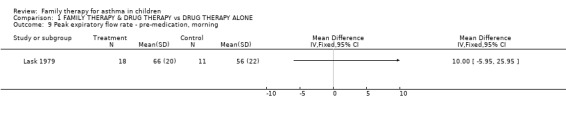
Comparison 1 FAMILY THERAPY & DRUG THERAPY vs DRUG THERAPY ALONE, Outcome 9 Peak expiratory flow rate ‐ pre‐medication, morning.
1.10. Analysis.
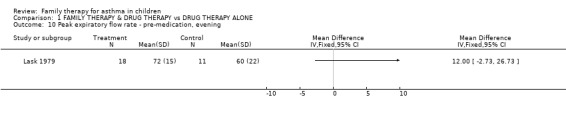
Comparison 1 FAMILY THERAPY & DRUG THERAPY vs DRUG THERAPY ALONE, Outcome 10 Peak expiratory flow rate ‐ pre‐medication, evening.
1.11. Analysis.
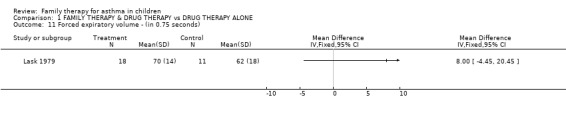
Comparison 1 FAMILY THERAPY & DRUG THERAPY vs DRUG THERAPY ALONE, Outcome 11 Forced expiratory volume ‐ (in 0.75 seconds).
1.12. Analysis.
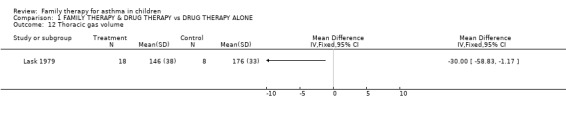
Comparison 1 FAMILY THERAPY & DRUG THERAPY vs DRUG THERAPY ALONE, Outcome 12 Thoracic gas volume.
1.13. Analysis.
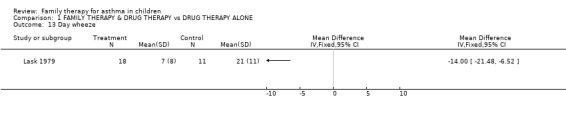
Comparison 1 FAMILY THERAPY & DRUG THERAPY vs DRUG THERAPY ALONE, Outcome 13 Day wheeze.
1.14. Analysis.
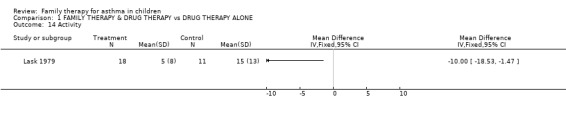
Comparison 1 FAMILY THERAPY & DRUG THERAPY vs DRUG THERAPY ALONE, Outcome 14 Activity.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Gustafsson 1986.
| Methods | Controlled, single‐blinded, randomised trial (method of randomisation not stated). A cross‐over design was employed for additional analyses. | |
| Participants | Chronic asthmatic children and their families | |
| Interventions | Family therapy and drug therapy vs drug therapy alone | |
| Outcomes | General paediatric assessment; functionally impaired days; nights that beta 2 agonists were used; PEFR. | |
| Notes | Only pre‐cross‐over data was examined in the present overview. | |
Lask 1979.
| Methods | controlled, unblinded, randomised trial (impossible to blind). Method of randomisation ‐ sample numbers placed in a hat ‐ first number drawn = treatment group, second number = control group etc. | |
| Participants | chronically asthmatic children and their families | |
| Interventions | family therapy and drug therapy vs drug therapy alone | |
| Outcomes | PEFR ‐ morning; PEFR ‐ evening; Forced expiratory volume (in 0.75 seconds); Thoracic gas volume. | |
| Notes | ||
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Ago 1979 | Not randomised family therapy trial ‐ psychosomatic allergies |
| Brown 2005 | Not randomised family therapy trial ‐ education program for families of young children with asthma |
| Campbell 1993 | Not randomised family therapy trial ‐ impact of family factors on childhood illness |
| Chiang 2004 | Not randomised family therapy trial ‐ CCT of an educational program for parents |
| Cluss 1986 | Not randomised family therapy trial ‐ behavioural interventions |
| Colland 2004 | Not randomised family therapy trial ‐ self‐treatment program for parents of children with asthma (educational intervention) |
| Donnelly 1987 | Not randomised family therapy trial ‐ pharmacological intervention vs pharmacological intervention alone. |
| Evans 1999 | Not randomised family therapy trial ‐ RCT of family educational and environmental interventions |
| Georgiou 2003 | Not randomised family therapy trial ‐ disease management program with education |
| Gustafsson 1988 | Evaluative paper |
| Gustafsson 2002 | Not randomised family therapy trial ‐ assessment of psycho‐social effects on families with an asthmatic child |
| Guttman 1981 | Book chapter |
| Haggerty 1983 | Literature review |
| Horner 2003 | Not randomised family therapy trial ‐ RCT of educational program for children and parents |
| La Roche 2005 | RCT of cultural minority groups ‐ no family therapy |
| Lehrer 1992 | Not randomised family therapy trial ‐ psychological approaches to treatment of asthma |
| Liebman 1974 | Book chapter |
| Liebman 1976 | Book chapter |
| Masterson 1985 | Not randomised family therapy trial ‐ family assessment of asthmatic child |
| McCarthy 2002 | Not randomised family therapy trial ‐ assessment of a family educational program |
| McNicol 1973a | Literature review |
| McNicol 1973b | Literature review |
| Mitchell 2005 | Not randomised family therapy trial ‐ RCT evaluating the effect of an asthma clinical pathway for children in general practice |
| Molinari 1994 | Not randomised family therapy trial ‐ application of family therapy theories in case studies of 4 asthmatic children and families |
| Morgan 2004 | Not randomised family therapy trial ‐RCT of family educational and environmental interventions |
| Onnis 1984 | Not randomised family therapy trial ‐ pharmacological intervention vs pharmacological intervention alone. |
| Onnis 1986 | Not randomised family therapy trial ‐ pharmacological intervention vs pharmacological intervention alone. |
| Onnis 1989 | Preliminary data on randomised control family therapy trial. |
| Onnis 1992 | Not randomised family therapy trial ‐ pharmacological intervention vs pharmacological intervention alone. |
| Onnis 1993 | Not randomised family therapy trial ‐ pharmacological intervention vs pharmacological intervention alone. |
| Onnis 1994 | Not randomised family therapy trial ‐ pharmacological intervention vs pharmacological intervention alone. |
| Smith 2004 | Not randomised family therapy trial ‐ RCT evaluating the effects of telephone asthma coaching and monetary incentive to improve follow‐up of children with asthma |
| Stevens 2002 | Not randomised family therapy trial ‐ RCT of family education and written self‐management plan |
| Towns 1994 | Not randomised family therapy trial ‐ uses family therapy theories to examine empowerment over asthma symptoms in children and families. |
| Walders 2006 | RCT of patient education with some problem solving therapy but not family orientated |
| Wirsching 1985 | Not randomised family therapy trial ‐ a description psychosocial characteristics of asthma patients and their families |
Contributions of authors
For the update: JY and CS assessed the search results and completed the update.
Initial version of the review. Jenny Panton initiated the study with help from Elizabeth Barley. Data were extracted, entered and verified by both reviewers. Both reviewers participated in the discussion and interpretation of the results and collaborated in writing the text. The passages of text describing family therapy theory were written by JP.
Sources of support
Internal sources
NHS Research and Development, UK.
External sources
Nuffield Provincial Hospitals Trust, Not specified.
Declarations of interest
Nil
Edited (no change to conclusions)
References
References to studies included in this review
Gustafsson 1986 {published data only}
- Gustafsson PA, Kjellman N‐I. Family therapy in the treatment of severe childhood asthma. Journal of Psychosomatic Research 1986;30(3):369‐74. [DOI] [PubMed] [Google Scholar]
Lask 1979 {published data only}
- Lask B, Matthew D. Childhood asthma. A controlled trial of family psychotherapy. Archives of Disease in Childhood 1979;54(2):116‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Ago 1979 {published data only}
- Ago Y, Teshima H, Nagata S, Inoue S, Ikemi Y. Psychosomatic studies of allergic disorders. Psychotherapy & Psychosomatics 1979;31(1‐4):197‐204. [DOI] [PubMed] [Google Scholar]
Brown 2005 {published data only}
- Brown JV, Demi AS, Celano MP, Bakeman R, Kobrynski L, Wilson SR. A home visiting asthma education program: challenges to program implementation. Health Education and Behaviour 2005;32(1):42‐56. [DOI] [PubMed] [Google Scholar]
Campbell 1993 {published data only}
- Campbell TL. Impact of family factors on childhood illness. Family Systems Medicine 1993;11(4):433‐40. [Google Scholar]
Chiang 2004 {published data only}
- Chiang LC, Huang JL, Yeh KW, Lu CM. Effects of a self‐management educational program in Taiwan based on PRECEDE‐PROCEED model for parents with asthmatic children. Journal of Asthma 2004;412(2):205‐15. [DOI] [PubMed] [Google Scholar]
Cluss 1986 {published data only}
- Cluss PA. Behavioral interventions as adjunctive treatments for chronic asthma. Progress in Behavior Modification 1986;20:123‐60. [DOI] [PubMed] [Google Scholar]
Colland 2004 {published data only}
- Colland VT, Essen‐Zandvliet LEMV, Lans C, Denteneer A, Westers P, Brackel HJL. Poor adherence to self‐medication instructions in children with asthma and their parents. Patient Education & Counseling 2004;55(3):416‐21. [DOI] [PubMed] [Google Scholar]
Donnelly 1987 {published data only}
- Donnelly JE, Donnelly WJ, Thong YH. Parental perceptions and attitudes toward asthma and its treatment: a controlled study. Social Science & Medicine 1987;24(5):431‐7. [DOI] [PubMed] [Google Scholar]
Evans 1999 {published data only}
- Evans R, Gergen PJ, Mitchell H, Kattan M, Kersmar C, Crain E, et al. A randomised clinical trial to reduce asthma morbidity among inner‐city children: results of the national cooperative inner‐city asthma study. Journal of Pediatrics 1999;135(3):332‐8. [DOI] [PubMed] [Google Scholar]
Georgiou 2003 {published data only}
- Georgiou A, Buchner DA, Ershoff DH, Blasko KM, Goodman LV, Feign J. The impact of a large scale population based asthma management program on pediatric asthma patients and their caregivers. Annals of Allergy, Asthma and Immunology 2003;90(3):308‐15. [DOI] [PubMed] [Google Scholar]
Gustafsson 1988 {published data only}
- Gustafsson PA. [Familjeinteraktion och familjeterapi vid psykosomatisk sjukdom hos barn: En familje‐ och systemorienterad syn pa sjukdom]. Nordisk Psykiatrisk Tidsskrift 1988;42(1):9‐15. [Google Scholar]
Gustafsson 2002 {published data only}
- Gustafsson D, Olofsson N, Anderson F, Lindberg B, Schollin J. Effect of asthma in childhood on psycho‐social problems in the family. Journal of Psychosomatic Research 2002;53(6):1071‐5. [DOI] [PubMed] [Google Scholar]
Guttman 1981 {published data only}
- Guttman HA. Systems Theory, Cybernetics and Epistemology. In: A.S. Gurman, D.P Kniskern editor(s). Handbook of Family Therapy. New York: Brunner Mazel, 1981. [Google Scholar]
Haggerty 1983 {published data only}
- Haggerty JJ. The psychosomatic family: an overview. Psychosomatics 1983;24(7):615‐23. [DOI] [PubMed] [Google Scholar]
Horner 2003 {published data only}
- Horner SD. Enhancing childrens and parents asthma management. Computer Retrieval of Information on Scientific Projects (CRISP) 2003.
La Roche 2005 {published data only}
- Roache MJ, Koinis‐Mitchell D, Gualdron L. A culturally competent asthma management intervention: a randomised controlled pilot study. Annals of Allergy, Asthma & Immunology 2005. [DOI] [PubMed] [Google Scholar]
Lehrer 1992 {published data only}
- Lehrer PM, Sargunaraj D, Hochron SM. Psychological approaches to the treatment of asthma. Special issue: behavioral medicine: an update for the 1990s. Journal of Consulting & Clinical Psychology 1992;60(4):639‐43. [DOI] [PubMed] [Google Scholar]
Liebman 1974 {published data only}
- Liebeman R, Minuchin S, Baker L. The use of structural family therapy in the treatment of intractable asthma. American Journal of Psychiatry 1974;131:535‐40. [PubMed] [Google Scholar]
Liebman 1976 {published data only}
- Liebman R, Minuchin S, Rosman B. The role of the family in the treatment of childhood asthma. In: Geurin TJ editor(s). Family Therapy Theory and Practice. New York: Gardner, 1976:309‐22. [Google Scholar]
Masterson 1985 {published data only}
- Masterson J. Family assessment of the child with intractable asthma. Journal of Developmental & Behavioral Pediatrics 1985;Vol 6(5):244‐51. [PubMed] [Google Scholar]
McCarthy 2002 {published data only}
- McCarthy MJ, Herbert R, Brimacombe M, Hansen J. Empowering parents through asthma education. Pediatric Nursing 2002;28(5):465‐77. [PubMed] [Google Scholar]
McNicol 1973a {published data only}
- McNico lK, Williams HB. Spectrum of asthma in children ‐ 1, clinical and physiological components. British Medical Journal 1973;4:7‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
McNicol 1973b {published data only}
- McNicol KN, Williams HB. Spectrum of asthma in children ‐ 111, psychological and social components. British Medical Journal 1973;4:16‐20. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mitchell 2005 {published data only}
- Mitchell EA, Didsbury PB, Kruithof N, Robinson E, Milmine M, Barry M, et al. A randomised controlled trial of an asthma clinical pathway for children in general practice. Acta Paediatrica 2005;94(2):226‐33. [DOI] [PubMed] [Google Scholar]
Molinari 1994 {published data only}
- Molinari E, Taverna A, Gasca G, Constantino AL. Collaborative team approach to asthma: a clinical study. Family Systems Medicine 1994;12(1):47‐59. [Google Scholar]
Morgan 2004 {published data only}
- Morgan WJ, Crain EF, Gruchalla RS, O'Connor GT, Kattan M, Evans R, et al. Results of a home‐based environmental intervention among urban children with asthma. The New England Journal of Medicine 2004;351(11):1068‐80. [DOI] [PubMed] [Google Scholar]
Onnis 1984 {published data only}
- Onnis L, et al. [Sistema familiare e asma infantile. Dati preliminari di una ricerca sull'influenza della famiglia nelle forme croniche d'asma]. Medicina Psicosomatica 1984;29(3):263‐78. [Google Scholar]
Onnis 1986 {published data only}
- Onnis L, Tortolani D, Cancrini L. Systemic research on chronicity factors in infantile asthma. Family Process 1986;25(1):107‐22. [DOI] [PubMed] [Google Scholar]
Onnis 1989 {published data only}
- Onnis L, Gennaro A, Cespa G, Agostini B, et al. [Utilita della psicoterapia familiare nelle malattie psicosomatiche croniche: dati preliminari di una ricerca sull'asma infantile]. Medicina Psicosomatica 1989;34(3):189‐203. [Google Scholar]
Onnis 1992 {published data only}
- Onnis L. [Langage du corps et langage de la therapie: la "sculpture du futur" comme methode d'intervention systemique dans les situations psychosomatiques]. Therapie Familiale 1992;13(1):3‐19. [Google Scholar]
Onnis 1993 {published data only}
- Onnis L, Gennaro A, Cespa G, Agostini B, et al. [Approche systemique et prevention de la chronicite. Resultats preliminaires d'une recherche sur les troubles psychosomatiques chroniques]. Therapie Familiale 1993;14(2):201‐16. [Google Scholar]
Onnis 1994 {published data only}
- Onnis L, Gennaro A, Cespa G, Agostini B, et al. Sculpting present and future: A systemic intervention model applied to psychosomatic families. Family Process 1994;33(3):341‐55. [DOI] [PubMed] [Google Scholar]
Smith 2004 {published data only}
- Smith SR, Jaffe DM, Fisher EB, Trinkaus KM, Highstein G, Strunk RC. Improving follow‐up for children with asthma after an acute emergency department visit. Journal of Pediatrics 2004;145(6):772‐7. [DOI] [PubMed] [Google Scholar]
Stevens 2002 {published data only}
- Stevens CS, Wesseldine LJ, Couriel JM, Dyer AJ, Osman LM, Silverman M. Parental education and guided self‐management of asthma and whezzing in the pre‐school child: a randomised controlled trial. Thorax 2002;57(1):39‐44. [DOI] [PMC free article] [PubMed] [Google Scholar]
Towns 1994 {published data only}
- Towns A. Asthma, power, and the therapeutic conversation. Family Process 1994;33(5):161‐72. [DOI] [PubMed] [Google Scholar]
Walders 2006 {published data only}
- Walders N, Kercsmar C, Schluchter M, Redline S, Kirchner L, Drotar D. An interdisciplinary Intervention for Untreated Pediatric Asthma. Chest 2006. [DOI] [PubMed] [Google Scholar]
Wirsching 1985 {published data only}
- Wirsching M, Stierlin H. Psychosomatics: I. Psychosocial characteristics of psychosomatic patients and their families (Trans H. Winawer). Family Systems Medicine 1985;3(1):6‐16. [Google Scholar]
Additional references
Newacheck 1991
- Newacheck PW, McManus MA, Fox HB. Prevalence and impact of chronic illness among adolescents. American Journal of Diseases of Children 1991;145(12):1367‐73. [DOI] [PubMed] [Google Scholar]
Pless 1991
- Pless IB, Nolan T. Revision, replication, and neglect: research on maladjustment in chronic illness. Journal of Child Psychology and Psychiatry, and allied disciplines 1991;32(2):347‐65. [DOI] [PubMed] [Google Scholar]
Steinhauer 1974
- Steinhauer P, Mushin D, Rae‐Grant Q. Psychological aspects of chronic illness. Pediatric Clinics of North America 1974;21(4):825. [DOI] [PubMed] [Google Scholar]
Weil 1999
- Weil CM, Wade SL, Bauman LJ, Lynn H, Michell H, Lavigne J. The relationship between psychological factors and asthma morbidity in inner‐city children with asthma. Pediatrics 1999;104(6):1274‐80. [DOI] [PubMed] [Google Scholar]
Yorke 2005
- Yorke J, Fleming S, Shuldham S. Psychological interventions for children with asthma (Cochrane review). Cochrane Database of Systematic Reviews 2005, Issue 4. [DOI] [PMC free article] [PubMed] [Google Scholar]


