Abstract
Objective:
Flu vaccinations are recommended for almost everyone, but uptake may vary due to perceived social norms. We aimed to examine the relationship between perceived social circle vaccine coverage (including family, friends, and acquaintances) and own vaccination behavior, as well as potential mediators.
Methods:
In 2011, 357 participants from RAND’s American Life Panel reported perceived social circle vaccine coverage for the 2010–11 flu season, own vaccination behavior for the 2009–10 and 2010–11 flu seasons, perceived flu risk without and with vaccination, and perceived vaccine safety. In 2012 and 2016, respectively, participants returned to report their own vaccination behavior for the 2011–12 flu season (N=338) and 2015–16 flu season (N=216).
Results:
Perceiving greater percent of 2010–11 social circle vaccine coverage was associated with greater likelihood of getting vaccinated in the 2010–11 flu season (OR=1.03, 95% CI=1.01–1.04), and the subsequent 2011–12 flu season (OR=1.02, 95% CI=1.01–1.03), but not the 2015–16 flu season (OR=1.00, 95% CI=.99–1.01), as seen in logistic regressions that controlled for demographics and 2009–10 vaccination behavior. All significant relationships between social circle vaccine coverage and own vaccination behavior were mediated by perceived flu risk without vaccination.
Conclusions:
Perceived social circle vaccine coverage is associated with own vaccination behavior in the current and subsequent flu season, establishing behavior patterns that may persist into the future. People’s vaccination decisions may be informed by their perceptions of their peers’ beliefs and behaviors. We discuss intervention strategies for promoting vaccine uptake by counteracting negative and increasing positive perceived social norms.
Keywords: influenza vaccination, risk perception, social sampling, social influences
INTRODUCTION
The CDC recommends routine annual influenza vaccination for almost everyone (Grohskopf et al., 2018). Influenza vaccine uptake has shown medium-sized correlations (in the .25-.36 range) to past vaccination behavior, and to perceptions of vaccine safety (Chapman & Coups, 1999). Health beliefs and behaviors may also be shared through social circles, including friends, family, and acquaintances (Brewer, Chapman, Rothman, Leask, & Kempe, 2016; Galesic, Olsson, & Rieskamp, 2018; Christakis & Fowler, 2013; McPherson, Smith-Lovin, & Cook, 2001). People’s perceptions of their social contacts’ behaviors have been found to be relatively accurate, and to influence their own behavior (Christiakis & Fowler, 2013; Galesic, Olsson, & Rieskamp, 2012; Galesic, Bruine de Bruin, et al., 2018).
In a 2010 flu survey, respondents who reported that ‘most’ (vs. ‘very few’) of their friends/family had gotten the H1N1 vaccine had 8.31 times the odds of vaccine acceptance (Kumar et al., 2011). In a 2012 flu survey, of the 39% respondents who said that the vaccination rates in their social circle influenced their vaccination decisions, 76% indicated that observing an increase in their social circle’s influenza vaccine coverage would encourage them to follow the perceived social norm to vaccinate rather than to ‘free ride’ on herd immunity (Parker, Vardavas, Marcum, & Gidengil, 2013).
However, none of these studies reported on validated methodologies for assessing perceptions of social network characteristics (e.g., Galesic et al., 2012; McCarty, 2012; Sudman, 1985). In a study on childhood vaccinations that did use such a methodology, parents who conformed to recommendations for their children’s complete and on-time vaccinations reported having more social contacts who recommended such conformity than those who did not (72% vs. 13%), perhaps in part as a result of discussions of perceived risks and vaccine safety (Brunson, 2013). Although cross-sectional data suggest that people’s vaccination decisions may be influenced by their perceptions of their social contacts’ beliefs and behaviors, the reverse is also possible: Individuals’ own vaccination decisions may influence their perceptions of their social contacts’ stance on vaccinations.
Here, we therefore analyzed data from a survey that used a validated procedure for assessing social network characteristics, and asked participants to report their vaccination behavior over subsequent flu seasons. Specifically, we examined whether (1) perceived social circle vaccine coverage was associated with flu vaccination behavior in cross-sectional and longitudinal analyses, and (2) perceptions of flu risk (with and without vaccination) and vaccine safety mediated these relationships, suggesting that beliefs shared through social circles play a role in flu vaccination behavior.
METHOD
Sample
We conducted secondary analyses of a longitudinal online survey with RAND’s American Life Panel, which was recruited through multiple probability-based approaches (www.rand.org/labor/alp.html). Interested individuals received equipment and internet access, if needed. Panel members are invited to answer online surveys for about $20 per 30 minutes. In this case, participants were invited to complete a study “about your thoughts and experiences with the flu and flu vaccination, as well as the experiences of people close to you.” The survey was originally designed to provide empirical evidence for informing an agent-based model of vaccination behavior (Vardavas & Markum, 2013). Informed consent was obtained from all participants. RAND’s Human Subjects Protection Committee approved the survey. Table 1 shows the timing of the three survey waves and the associated measures. The three surveys (numbered 216, 257, and 460) are available from https://alpdata.rand.org/.
Table 1:
Survey waves and associated measures.
| Measures | Survey Wave 1 (Sep 2011; N=357) | Survey Wave 2 (May-July 2012; N=338) | Survey Wave 3 (Sep-Oct 2016; N=216) |
|---|---|---|---|
| Dependent variables | |||
| Vaccination behavior in 2010–11 flu season | X | ||
| Vaccination behavior in 2011–12 flu season | X | ||
| Vaccination behavior in 2015–16 flu season | X | ||
| Predictor variable | |||
| Perceived social circle vaccine coverage in 2010–11 flu season | X | ||
| Control variables | |||
| Vaccination behavior in 2009–10 flu season | X | ||
| Perceived flu risk without vaccination | X | ||
| Perceived flu risk with vaccination | X | ||
| Perceived vaccine safety | X | ||
| Age | X | ||
| Female | X | ||
| College Education | X | ||
| White | X | ||
Note: All analyses were limited to participants who completed Survey Wave 1 in September 2011, before vaccine uptake among US adults took off for the 2011–12 flu season (Centers for Disease Control and Prevention, 2013).
We obtained data from 534 of 598 (89%) invited American Life Panel members who completed all relevant measures in Survey Wave 1 between September 2011 and February 2013. We limited our analyses to those 357 of the 598 invitees (60%) who completed Survey Wave 1 in September 2011, before vaccine uptake among US adults for the 2011–12 flu season took off in October 2011 and ultimately reached approximately 38% by the end of Spring 2012 (Centers for Disease Control and Prevention, 2013). The 2011–12 flu season started relatively late, with reports of outpatient visits for influenza-like illness remaining low through February 2012, and not peaking until mid-March 2012 (Centers for Disease Control and Prevention, 2012). Thus, participants who completed Survey Wave 1 in September 2011 reported their perceptions of their social circle’s 2010–11 vaccine coverage before they or their social contacts would likely have started getting vaccinated for the 2011–12 flu season, or getting the flu. Limiting our analyses to those participants who completed Survey Wave 1 in September 2011 did not affect the main conclusions of this paper.
Average age among the 357 Survey Wave 1 participants who were included in our analyses was 49.45 (SD=15.41), with 51% identifying as women and 89% as white, and 46% reporting having a college degree. By comparison, US Census Bureau statistics (2012) suggest that the American adult population at that time had a median age of 45–49 years old, while including 51% women, 81% whites, and 30% holding a college degree. Participants’ own reported vaccine coverage in the 2010–11 flu season (43%) and the 2009–10 flu season (43%) and their mean perceived social circle vaccine coverage (37%) for the 2010–11 flu season were each only 2–4 percentage points off from the US population’s national vaccine coverage for 2010–11 (41%) and 2009–10 (40%) (Centers for Disease Control and Prevention, 2017).
Of the 357 Survey Wave 1 participants who were included in our analyses, 338 (95%) completed Survey Wave 2 (May-July 2012), and 216 (61%) completed Survey Wave 3 (September-October 2016). Table S1 displays descriptive statistics, flagging significant differences in demographics and other Survey Wave 1 measures in comparisons (1) between invited panel members who completed Survey Wave 1 in September 2011 vs. later or not at all, (2) between Survey Wave 1 participants who completed Survey Wave 2 vs. not, and (3) between Survey Wave 1 participants who completed Survey Wave 3 vs. not. First, invited panel members who completed Survey Wave 1 in September 2011 did not significantly differ from those who did not complete it by then or at all, except that they were somewhat older (M=49.45, SD=15.41 vs. M=43.87, SD=15.44), t(579)=4.25, p<.001, significantly more likely to be white (89% vs. 80%), χ2(1)=8.86, p<.01, to have a college degree (46% vs. 36%), χ2(1)=5.59, p=.02, and to report that they got vaccinated in the 2009–10 flu season (43% vs. 30%), χ2(1)=7.63, p<.01, while also being marginally more likely to report that they got vaccinated in the 2010–11 flu season (43% vs. 35%), χ2(1)=2.84, p=.09, and giving marginally higher ratings for vaccine safety (M=4.22, SD=2.39 vs. M=3.78, SD=2.44), t(525)=1.97, p=.05. Second, included Survey Wave 1 participants who completed Survey Wave 2 (vs. not) were marginally older age (M=49.79, SD=15.27 vs. M=43.42, SD=17.04) t(355)=−1.76, p=.08. Third, included Survey Wave 1 participants who completed Survey Wave 3 (vs. not) were significantly older (M=53.27, SD=13.26 vs. M=43.60, SD=16.64), t(355)=−6.08, p<.001, and significantly more likely to have a college education (50% vs. 38%), χ2(1)=5.09, p=.02.
Survey Wave 1
Concurrent and past vaccination behavior.
Participants first answered “During the last flu season (Fall 2010 to Spring 2011), did you get a seasonal flu vaccine (either a shot or nasal spray?” The subsequent question used the same wording, but asked about “during the flu season before that (Fall 2009 to Spring 2010).” Thus, the first question reflected vaccination behavior that was concurrent to reported perceptions of social circle vaccine coverage, which also focused on the 2010–11 flu season.
Perceived social circle vaccine coverage.
Following validated numerical estimation procedures for sizes of social networks and their subgroups (Galesic et al., 2012; McCarty et al., 2001; Sudman, 1985),1 participants estimated the number of people from different social groups they had “regular contact with in the past six months” including “face-to-face, by phone or mail, or on the internet.” The social groups included family, close friends, coworkers, school or childhood relations, people who provide a service, neighbors, and others. Participants then judged how many out of the total number of these social contacts they knew and thought got vaccinated in the past year (Fall 2010 to Spring 2011). We computed the overall perceived percent of the social circle getting vaccinated in the 2010–11 flu season, on a scale from 0–100%.
Perceived flu risk and vaccine safety.
Participants judged their risk of getting the flu without vaccination, by answering “If you do not get the flu vaccine this year, what do you think are the chances that you will get the flu this flu season (between Fall 2011 and Spring 2012).” They also judged their risk of getting the flu with vaccination, by answering the same question “if you do get the flu vaccine this year.” Both questions were presented with a 0–100% visual linear scale, following Bruine de Bruin & Carman (2018). Participants also rated “concerns about safety, side effects, or getting sick from the vaccine” (1=not at all important, 7=extremely important). Perceptions of flu risk without and with vaccination and perceptions of vaccine safety have been validated in terms of correlations with vaccination behavior (Bruine de Bruin & Carman, 2018; Chapman & Coups, 1999; Brewer, Chapman, Gibbons, Gerard, McCaul, & Weinstein, 2007), with 0–100% scales and 7-point Likert scales tending to show similar validity (Weinstein & Diefenbach, 1997).
Demographic variables.
Participants reported their age, gender, race/ethnicity, and whether or not they had completed a college education.
Follow-up survey waves.
Vaccination behavior.
Survey Wave 2 asked “During the last flu season (Fall 2011 to Spring 2012), did you get a seasonal flu vaccine (either a shot or nasal spray)?” (yes=1, no=0). SurveyWave 3 asked how long ago participants last got vaccinated, including the recent Fall 2015-Spring 2016 flu season (yes=1, no=0).
Analysis plan.
To answer our first research question, we conducted three sets of analogous logistic regressions assessing relationships between reports of social circle vaccine coverage and of own vaccination behavior for three flu seasons. All analyses treated perceived social circle vaccine coverage as a continuous variable, but we categorized the variable for presentation purposes (Figure 1A–C). In the three analogous sets of logistic regressions, we predicted own vaccination behavior for (1) the 2010–11 flu season as reported in Survey Wave 1 (Table 2), (2) the 2011–12 flu season as reported in Survey Wave 2 (Table 3), and (3) the 2015–16 flu season as reported in Survey Wave 3 (Table 4), from perceived social circle vaccine coverage for the 2010–11 flu season reported in Survey Wave 1, after sequentially controlling for demographics (Model 1A), vaccination behavior reported for the 2009–10 flu season prior to the flu season of the social circle reports (Model 2A), and vaccination behavior in any subsequent flu seasons in the past (Models 3A-4A).
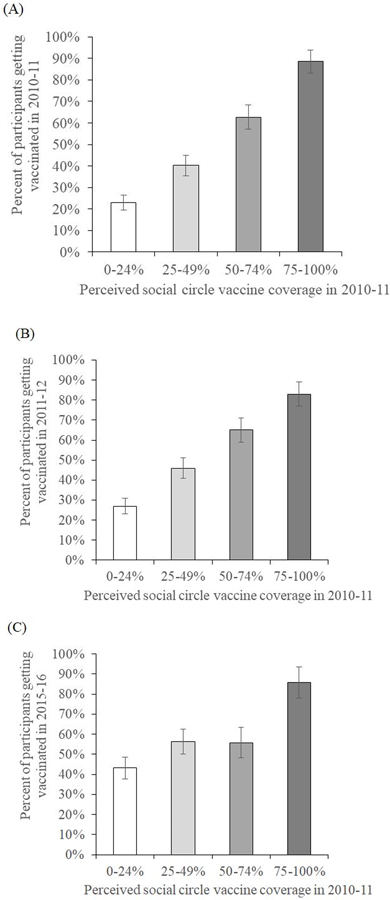
Figure 1:
Percent of participants reporting getting vaccinated in (A) the 2010–11 flu season as reported in Survey Wave 1 (B) the 2011–12 flu season as reported in Survey Wave 2 and (C) the 2015–16 flu season as reported in Survey Wave 3, by social circle vaccine coverage in 2010–11, as reported in Survey Wave 1.
Note: Error bars reflect standard errors. Perceived social circle vaccine coverage is displayed in categories for presentation purposes, but treated as a continuous variable in all analyses. N=357 for Figure 1A, N=338 for Figure 1B, N=216 for Figure 1C.
Table 2:
Logistic regressions predicting reported vaccination behavior for the 2010–11 flu season (Odds Ratio; 95% confidence interval)
| Predictor and control variables | Model 1A | Model 1B | Model 2A | Model 2B |
|---|---|---|---|---|
| Perceived social circle vaccine coverage in 2010–11 flu season (0–100%) | 1.04*** (1.03, 1.05) | 1.03*** (1.02, 1.05) | 1.03*** (1.01, 1.04) | 1.03*** (1.01, 1.04) |
| Perceived flu risk without vaccination (0–100%) | 1.04***a (1.02, 1.05) | - | 1.03**a (1.01, 1.04) | |
| Perceived flu risk with vaccination (0–100%) | .97*** (.96, .99) | - | .97** (.95, .99) | |
| Perceived vaccine safety (1–7) | 1.21**a (1.08,1.35) | - | 1.12 (.96, 1.31) | |
| Age | 1.05*** (1.03, 1.07) | 1.05*** (1.03, 1.07) | 1.05*** (1.03, 1.08) | 1.05*** (1.03, 1.08) |
| Female | 1.08 (.66, 1.76) | .94 (.54, 1.63) | 1.06 (.53, 2.11) | .96 (.46, 2.00) |
| College Education | 1.10 (.67, 1.80) | .96 (.55, 1.68) | .55 (.26, 1.14) | .42* (.19, .94) |
| White | .86 (.38, 1.93) | .79 (.31, 1.99) | 1.53 (.48, 4.89) | 1.42 (.40, 5.02) |
| Past vaccination behavior in 2009–10 flu season | - | - | 50.50*** (23.76, 107.33) | 41.36*** (18.74, 91.25) |
| Nagelkerke R2 | .33 | .47 | .70 | .73 |
p<.10;
p<.05;
p<.01;
p<.001
Mediated the relationship between perceived 2010–11 social circle vaccine coverage and predicted vaccination behavior (p<.05)
Mediated the relationship between perceived 2010–11 social circle vaccine coverage and predicted vaccination behavior (p<.10)
Note: Models were computed for participants who completed Survey Wave 1 in September 2011 (N=357). All variables were reported in Survey Wave 1 in September 2011 (Table 1).
Table 3:
Logistic regressions predicting reported vaccination behavior for the 2011–12 flu season (Odds Ratio; 95% confidence interval)
| Predictor and control variables | Model 1A | Model 1B | Model 2A | Model 2B | Model 3A | Model 3B |
|---|---|---|---|---|---|---|
| Perceived social circle vaccine coverage in 2010–11 flu season (0–100%) | 1.04*** (1.02,1.05) | 1.03*** (1.02, 1.04) | 1.02*** (1.01, 1.03) | 1.02** (1.01, 1.03) | 1.02* (1.00, 1.03) | 1.01+ (.99, 1.03) |
| Perceived flu risk without vaccination (0–100%) | 1.04***a (1.03, 1.06) | - | 1.03***a (1.02, 1.05) | - | 1.03**b (1.01, 1.04) | |
| Perceived flu risk with vaccination (0–100%) | .98* (.96, .99) | - | .98+ (.97, 1.00) | - | .99 (.97, 1.01) | |
| Perceived vaccine safety (1–7) | 1.13*b (1.01, 1.27) | - | 1.04 (.91, 1.19) | - | 1.01 (.88, 1.17) | |
| Age | 1.07*** (1.05, 1.09) | 1.08*** (1.05, 1.10) | 1.07*** (1.05, 1.10) | 1.08*** (1.05, 1.10) | 1.07*** (1.04, 1.09) | 1.07*** (1.05, 1.10) |
| Female | 1.04 (.63, 1.73) | .90 (.51, 1.59) | .95 (.53, 1.73) | .83 (.44, 1.57) | .97 (.50, 1.85) | .85 (.43, 1.68) |
| College Education | 1.19 (.72, 1.98) | 1.16 (.66, 2.05) | .81 (.44, 1.48) | .83 (.43, 1.58) | 1.00 (.51, 1.95) | 1.07 (.53, 2.14) |
| White | .44* (.20, 1.00) | .38 (.16, .94) | .47 (.18, 1.22) | .43+ (.16, 1.17) | .37 (.14, 1.01) | .34 (.12, .97) |
| Past vaccination behavior in 2009–10 flu season | 14.02*** (7.42, 26.50) | 10.24*** (5.23, 20.04) | 3.41** (1.48, 7.85) | 2.88* (1.20, 6.92) | ||
| Past vaccination behaviour in 2010–11 flu season | - | - | 10.44*** (4.63, 23.52) | 8.81*** (3.78, 20.52) | ||
| Nagelkerke R2 | .35 | .48 | .56 | .60 | .63 | .66 |
p<.10;
p<.05;
p<.01;
p<.001
Mediated the relationship between perceived 2010–11 social circle vaccine coverage and predicted vaccination behavior (Sobel test, p<.05)
Mediated the relationship between perceived 2010–11 social circle vaccine coverage and predicted vaccination behavior (Sobel test, p<.10)
Note: Models were computed for the 338 participants who returned for Survey Wave 2, while also having completed Survey Wave 1 in September 2011. The dependent variable was reported in Survey Wave 2 in May-July 2012. All predictor and control variables were reported in Survey Wave 1 in September 2011 (Table 1).
Table 4:
Logistic regressions predicting reported vaccination behavior for the 2015–16 flu season (Odds Ratio; 95% confidence interval)
| Predictor and control variables | Model 1A | Model 1B | Model 2A | Model 2B | Model 3A | Model 3B | Model 4A | Model4B |
|---|---|---|---|---|---|---|---|---|
| Perceived social circle vaccine coverage in 2010–11 flu season (0–100%) | 1.02** (1.01, 1.03) | 1.01+ (1.00, 1.03) | 1.00 (.99, 1.01) | 1.00 (.99,1.02) | 1.00 (.98, 1.01) | 1.00 (.98, 1.01) | 1.00 (.98, 1.01) | 1.00 (.98, 1.01) |
| Perceived flu risk without vaccination (0–100%) | 1.02**a (1.01, 1.04) | - | 1.02*b (1.00, 1.03) | - | 1.01 (1.00, 1.03) | - | 1.01 (.99, 1.03) | |
| Perceived flu risk with vaccination (0–100%) | .98+ (.97, 1.00) | - | .99 (.97, 1.01) | - | .99 (.98, 1.01) | - | .99 (.98, 1.01) | |
| Perceived vaccine safety (1–7) | 1.14+ (1.00, 1.30) | - | 1.06 (.91, 1.22) | - | 1.04 (.90, 1.21) | - | 1.04 (.90, 1.21) | |
| Age | 1.06*** (1.03, 1.08) | 1.05*** (1.03, 1.08) | 1.05** (1.02, 1.08) | 1.05** (1.02, 1.08) | 1.04** (1.01, 1.07) | 1.04** (1.01, 1.07) | 1.03* (1.00, 1.07) | 1.03* (1.00, 1.07) |
| Female | 1.41 (.76, 2.58) | 1.18 (.62,2.25) | 1.27 (.65,2.48) | 1.13 (.56, 2.25) | 1.20 (.60, 2.38) | 1.12 (.55, 2.27) | 1.16 (.57,2.34) | 1.10 (.53, 2.26) |
| College Education | 1.92* (1.04,3.53) | 1.83+ (.95,3.54) | 1.28 (.65, 2.52) | 1.31 (.64, 2.65) | 1.32 (.66, 2.65) | 1.32 (.65,2.72) | 1.27 (.62, 2.59) | 1.25 (.60, 2.61) |
| White | 1.61 (.57,4.54) | 1.35 (.46, 3.96) | 2.41 (.77, 7.55) | 2.21 (.68, 7.20) | 2.49 (.78, 8.00) | 2.27 (.69, 7.45) | 2.89+ (.86, 9.68) | 2.65 (.78, 9.03) |
| Past vaccination behavior in 2009–10 flu season | 8.46*** (3.93, 18.23) | 6.71*** (2.98, 15.07) | 3.54** (1.40,8.95) | 3.26* (1.25, 8.52) | 2.80* (1.06, 7.42) | 2.65+ (.97, 7.23) | ||
| Past vaccination behaviour in 2010–11 flu season | - | - | 4.71** (1.86,11.93) | 3.97** (1.49, 10.54) | 2.93* (1.04, 8.30) | 2.63+ (.90, 7.67) | ||
| Past vaccination behavior in 2011–12 flu season (Survey Wave 2) | - | - | - | - | 2.93* (1.21, 7.10) | 2.76* (1.12, 6.79) | ||
| Nagelkerke R2 | .24 | .32 | .40 | .43 | .45 | .46 | .47 | .48 |
p<.10;
p<.05;
p<.01;
p<.001
Mediated the relationship between perceived 2010–11 social circle vaccine coverage and predicted vaccination behavior (Sobel test, p<.05)
Mediated the relationship between perceived 2010–11 social circle vaccine coverage and predicted vaccination behavior (Sobel test, p<.10)
Note: Models were computed for the 216 participants who completed Survey Wave 3, with N=215 for Model 4 due to some participants having returned for Survey Wave 3 but not Survey Wave 2. The dependent variable was reported in Survey Wave 3 in September-October 2016. Except where noted otherwise, predictor and control variables were reported in Survey Wave 1 in September 2011.
To answer our second research question, we added the measures of perceived flu risk (without and with vaccination) and perceived vaccine safety to each logistic regression model (Tables 2–4; Model 1B-4B). We then computed parallel mediation models to assess whether measures of perceived flu risk (with and without vaccination) and perceived vaccine safety mediated any relationships between social circle reports and vaccination behaviors (Table S3; Figures S1–S3).2
RESULTS
To answer our first research question, we examined relationships between reports of social circle vaccine coverage and of own vaccination behavior concurrently and over time (Figure 1A–C). A first set of logistic regressions showed that greater 2010–11 social circle vaccine coverage was significantly associated with concurrent reports of vaccination behavior in the 2010–11 flu season in Survey Wave 1 (Table 2), while accounting for demographics (Model 1A), as well as past vaccination behavior reported for the 2009–10 flu season (Model 2A).3 A second set of logistic regressions showed that greater 2010–11 social circle vaccine coverage was significantly associated with vaccination behavior in the 2011–12 flu season as reported in Survey Wave 2 (Table 3), while accounting for demographics (Model 1A), as well as past vaccination behavior reported for the 2009–10 flu season (Model 2A) and the 2010–11 flu season (Model 3A). A third set of logistic regressions showed that greater 2010–11 social circle vaccine coverage was only significantly associated with vaccination behavior in the 2015–16 flu season as reported in Survey Wave 3 (Table 4), when accounting for demographics (Model 1A). That relationship was no longer significant after additionally controlling for past vaccination behavior reported for the 2009–10 flu season (Model 2A), as well as the 2010–11 flu season (Model 3A) and the 2011–12 flu season (Model 4A).4
To answer our second research question, we added measures of perceived flu risk (without and with vaccination) and perceived vaccine safety to each logistic regression (Tables 2–4), and conducted tests for mediation (Table S3; Figures S1–S3). Only perceived flu risk without vaccination significantly predicted vaccination behavior in all three flu seasons, when in addition to perceived 2010–11 social circle vaccine coverage, demographics (Tables 2–4; Model 1B) and 2009–10 vaccination behavior (Tables 2–4; Model 2B) were controlled for. In the models that controlled for demographics and 2009–10 vaccination behavior, perceived flu risk with vaccination added significantly to the prediction of 2010–11 vaccination behavior (Table 2; Model 2B), but only marginally to the prediction of 2011–12 vaccination behavior (Table 3; Model 2B), and not to the prediction of 2015–16 vaccination behavior (Table 4; Model 2B). In these models, perceived vaccine safety did not significantly add to the prediction of vaccination behavior in any of the flu seasons (Table 2–4; Model 2B). After additionally taking into account 2010–11 vaccination behavior in models predicting later vaccination behavior, perceived flu risk without vaccination still significantly predicted 2011–12 vaccination behavior (Table 3; Model 3B) but not 2015–16 vaccination behavior (Table 4; Model 3B).
Mediation analyses (Table S3) found that only perceived flu risk without vaccination systematically mediated relationships between perceived social circle vaccine coverage after taking into account demographics and past vaccination behavior, when predicting 2010–11 vaccination behavior (Figure S1A–B), and 2011–12 vaccination behavior (Figure S2A–C). In models predicting 2015–16 vaccination behavior (Table S3), this mediation was significant when taking into account demographics (Figure S3A), marginal when additionally considering 2009–10 vaccination behavior (Figure S3B), and not significant when additionally taking into account 2009–10, 2010–11, and 2011–12 vaccination behavior (Figure S3C–D).
DISCUSSION
Our longitudinal analyses suggest that participants’ perceived social circle vaccine coverage was associated with their vaccination behavior as reported for the concurrent and subsequent flu seasons. Relationships with vaccination behavior as reported five years later were accounted for by vaccination behaviors in intermediate flu seasons. Thus, effects of perceived social circle vaccine coverage may persist into the future due to the formation of consistent behavioral patterns. Indeed, vaccination behavior tends to be consistent across flu seasons (Chapman & Coups, 1999).
Our findings suggest that participants who perceived greater social circle vaccine coverage followed the perceived social norm. These conclusions are in line with previous survey research, in which participants stated that they would be more likely to get vaccinated if they perceived increases in their peers’ vaccine coverage, rather than free ride (Parker et al., 2013).
The significant relationships between social circle vaccine coverage and vaccination behavior were, at least in part, mediated by perceptions of flu risk without vaccination. Thus, people’s vaccination behavior may be informed by the social norms they perceive when observing their social contacts, as well as through explicit discussions with their social contacts about flu risks.
Our analyses had several main limitations. First, the invitation to the study we analyzed referred to flu and flu vaccinations, which may have increased participation by individuals who were interested in the topic. Although our sample was similar to the US Census (2012) at the time in terms of median age (45–49 year old) and percent of women (51%) and to estimates from the Centers for Disease Control and Prevention (2017) in terms of vaccination coverage (about 40%), our sample did include more individuals who self-reported being white (89% vs. 81%), and having a college degree (46% vs. 30%). Second, social circle vaccine coverage was only assessed for the 2010–11 flu season (Survey Wave 1), so we do not know whether changes in perceived social circle vaccine coverage may have occurred over subsequent flu seasons to inform vaccination behavior in 2015–2016 (Survey Wave 3). Third, concurrent reports of participants’ own vaccination behavior and that of their social contacts may have been affected by social projection, or a tendency to overestimate the like-mindedness of social contacts (Ross, Greene, & House, 1977). However, correlations between reported 2010–11 social circle vaccine coverage and vaccination behavior in later flu seasons controlled for those concurrent reports of behavior. Fourth, our findings examined correlations over time, which warrants conclusions about temporal relationships but not about causation. Fifth, we analyzed self-reports of vaccination behavior, which may not necessarily reflect actual vaccination behavior. However, self-reported vaccination behavior has been shown to have at least 90% sensitivity (i.e., percent of actual vaccinators who self-reported getting vaccinated) though specificity (i.e., percent of actual non-vaccinators who self-reported not getting vaccinated) has varied across adult samples from 65% to more than 90% (Irving, Donahue, Shay, Ellis-Coyle, & Belongia, 2009; Rolnick et al., 2013).
Our findings have implications for interventions. When people search for information about vaccination online, they are likely to come across negative views (Downs, Bruine de Bruin, & Fischhoff, 2008). Exposure to more online posts from people with adverse vaccination experiences undermines intentions to vaccinate, even in the presence of statistical information about the actual likelihood of adverse events in the population (Betsch, Renkewitz, Ulshöfer, & Betsch 2011). Especially individuals with lower numeracy skills may be persuaded by such personal narratives (Bruine de Bruin, Wallin, Parker, & Hanmer, 2017). Intervention strategies for counteracting the negative effects of anti-vaccine narratives on vaccination intentions may include warnings that narratives are not representative of the population (Betsch, Renkewitz, & Haase, 2013), and visual displays that make population statistics easier to understand (Fagerlin, Wang, & Ubel, 2005).
To further promote flu vaccination, interventions could aim to draw attention to the behaviors and risk perceptions of peers who vaccinate. Potentially, such interventions could broaden social perceptions beyond immediate social circles, which tend to consist of mostly like-minded individuals (McPherson et al., 2001). Health communications have incorporated narratives from peers who have experienced specific medical treatments, so as to share information, increase engagement, and model behavior, among other things (Shaffer & Zikmund-Fisher, 2012). Being randomly assigned to seeing friends declare on social media that they have voted (vs. to not seeing such declarations) increases the likelihood that people themselves will go out to vote (Bond et al., 2012). Social norms interventions that highlight information about the behavior of examplary peers inside and outside of one’s personal social network have also already been used for promoting pro-environmental behaviors such as reducing household energy use and increasing curbside recycling (Schultz, Nolan, Cialdini, Goldstein, & Griskevicius, 2007; Schultz, 1999).
Supplementary Material
Acknowledgments
Data collection was funded by the U.S. National Cancer Institute (R21CA157571), and the U.S. National Institute of Allergies and Infectious Diseases (R01AI118705). WBB was additionally supported by the Swedish Foundation for the Humanities and Social Sciences (Riksbanken Jubileumsfond) Program on Science and Proven Experience. MG was additionally supported by NIFA, USDA (2018–67023-27677). These funders had no role in study design, data collection, data analysis and interpretation, writing the report, or the decision to submit the report for publication.
Footnotes
No financial disclosures were reported by the authors of this paper.
Three studies have validated our numerical estimation procedure for the size of social networks and subgroups. The first showed that the numerical estimation procedure was better than name recall procedures for assessing social network sizes in groups with known networks (Sudman, 1985). The second showed that the numerical estimation procedure (also referred to as the summation method) produced similar estimates as an alternative procedure in which network size was assessed on the basis of the number of social contacts a participant reported from a known subpopulation, such as those named ‘Michael’ (McCarty et al., 2001). The third showed that, in a national survey in the Netherlands, participants’ assessments of their social network characteristics (e.g., health problems, work stress, relationship problems) were relatively in line with their overall population statistics (Galesic et al., 2012).
We computed Sobel tests to assess the significance of mediation patterns, because Sobel tests can handle the inclusion of linear regressions on the continuous mediator variables and logistic regressions on the dichotomous outcome variable (Herr, 2006). Sobel test results were replicated in bootstrapping mediation models with 5,000 bootstrap samples, which relied on linear regression estimates for both the continuous mediator variables and the dichotomous outcome variables (Hayes, 2018).
Our main findings for Survey Wave 1 were similar for the 215 Survey Wave 1 participants who were included in the analyses for each of the three survey waves, as compared to the 142 Survey Wave 1 participants who did not return for either of the subsequent survey waves. Specifically, the relationship between perceived social circle vaccine coverage in the 2010–11 flu season and vaccination behavior in the 2010–11 flu season (Table 2) was unaffected by whether or not participants were included in analyses for each survey wave. This is seen in the lack of significant interaction effects of perceived social circle vaccine coverage in the 2010–11 flu season with inclusion in analyses for each wave, when adding that interaction term to each model in Table 2 (p>.05 for each). Table S2 replicates the findings reported in Table 2, after limiting analyses of Survey Wave 1 to those 215 participants who were included in analyses for each survey wave (α=.05), with the exception that, for Model 1B, the perceptions of vaccine safety only marginally mediated the relationship between perceived 2010–11 social circle vaccine coverage and 2010–11 vaccination behavior.
In each model, we tested whether the relationship of perceived social circle vaccine coverage in the 2010–11 flu season with predicted vaccination behavior depended on whether or not participants vaccinated in the flu season prior to that (2009–10), the number of social groups reflected in the social circle, the size of the social circle, or the percent of social circle members for whom participants were sure (vs. thought) about vaccination behavior. With two exceptions, interaction terms of perceived social circle vaccine coverage in the 2010–11 flu season with each of these variables were not significant when each was separately added to any of the models (while taking into account associated main effects) in Tables 2–4 (p>.05 for each). The two exceptions were only observed for vaccination behavior in the 2010–11 flu season and not consistent across its models. First, we found that participants who were more confident about their social contacts’ 2010–11 vaccination status showed stronger associations between perceived 2010–11 social circle vaccine coverage and vaccination behavior in 2010–11 but only when 2009–10 vaccination behavior was not controlled for (Table 2, Model 1A, 1B). Second, we found a similar pattern for participants with larger social networks but only when 2009–10 vaccination behavior was controlled for (Table 2, Model 2A, 2B).
Contributor Information
Wändi Bruine de Bruin, University of Leeds and Carnegie Mellon University.
Andrew M. Parker, RAND Corporation
Mirta Galesic, Santa Fe Institute.
Raffaele Vardavas, RAND Corporation.
REFERENCES
- Betsch C, Renkewitz F, & Haase N (2012). Effect of narrative reports about vaccine adverse events and bias-awareness disclaimers on vaccine decisions. Medical Decision Making, 33, 14–25. [DOI] [PubMed] [Google Scholar]
- Betsch C, Ulshöfer C, Renkewitz F, & Betsch T (2011). The influence of narrative v. statistical information on perceiving vaccination risks. Medical Decision Making, 31, 742–53. [DOI] [PubMed] [Google Scholar]
- Bond RM, Farriss CJ, Jones JJ, Kramer ADI, Marlow C, Settle JE, & Fowler JH (2012). A 61-million person experiment in social influence and political mobilization. Nature, 489, 295–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer NT, Chapman GB, Gibbons FR, Gerard M, McCaul K & Weinstein ND (2007). A meta-analysis of the relationship between risk perception and vaccination behavior. Health Psychology, 26(2), 136–145. [DOI] [PubMed] [Google Scholar]
- Brewer NT, Chapman GB, Rothman AJ, Leask J, & Kempe A (2017). Increasing vaccination: Putting psychological science into action. Psychological Science in the Public Interest, 18,149–207. [DOI] [PubMed] [Google Scholar]
- Bruine de Bruin W, & Carman KG (2018). Measuring subjective probabilities: The effect of response mode on the use of focal responses, validity, and respondents’ evaluations. Risk Analysis, 38, 2128–2143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruine de Bruin W, Wallin A, Parker AM, Strough J & Hanmer J (2017). Effects of anti- vs. pro-vaccine narratives on responses by recipients varying in numeracy: A cross-sectional survey-based experiment. Medical Decision Making, 37, 860–870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brunson EK (2013). The impact of social networks on parents’ vaccination decisions. Pediatrics, 131, 1397–1407. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (2017). Final state-level influenza vaccination coverage estimates for the 2010–11 season–United States, National Immunization Survey and Behavioral Risk Factor Surveillance System, August 2010 through May 2011. Retrived April 2, 2019, from https://www.cdc.gov/flu/fluvaxview/coverage_1011estimates.htm
- Centers for Disease Control and Prevention (2013). Flu Vaccination Coverage, United States, 2011–12 Influenza Season. Retrieved April 2, 2019, from https://www.cdc.gov/flu/fluvaxview/coverage_1112estimates.htm
- Centers for Disease Control and Prevention (2012). 2011–2012 Influenza Season. Questions and Answers. Retrieved April 2, 2019, from https://www.cdc.gov/flu/pastseasons/1112season.htm
- Chapman G, & Coups EJ (1999). Predictors of influenza vaccine acceptance among healthy adults. Preventive Medicine, 29, 249–262. [DOI] [PubMed] [Google Scholar]
- Christakis NA, & Fowler JH (2013). Social contagion theory: examining dynamic social networks and human behavior. Stat Med, 20, 32, 556–577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Downs JS, Bruine de Bruin W & Fischhoff B (2008). Parents’ vaccination comprehension and decisions. Vaccine, 26, 1595–1607. [DOI] [PubMed] [Google Scholar]
- Fagerlin A, Wang C, & Ubel PA (2005). Reducing the influence of anecdotal reasoning on people’s health care decisions: Is a picture worth a thousand statistics? Medical Decision Making, 25, 398–405 [DOI] [PubMed] [Google Scholar]
- Galesic M, Bruine de Bruin W, Dumas M, Kapteyn A, Darling JE, & Meyer E (2018). Asking about social circles improves election predictions. Nature Human Behaviour, 2, 187–193. [Google Scholar]
- Galesic M, Olsson H, & Rieskamp J (2012). Social sampling explains apparent biases in judgments of social environments. Psychological Science, 23, 1515–1523. [DOI] [PubMed] [Google Scholar]
- Galesic M, Olsson H, & Rieskamp J (2018). A social sampling model of judgment. Psychological Review. [DOI] [PubMed]
- Goldstein NJ, Cialdini RB, & Griskeviscius V (2008). A room with a viewpoint: Using social norms to motivate environmental conservation in hotels. Journal of Consumer Research, 35, 472–482. [Google Scholar]
- Grohskopf LA, Sokolow LZ, Broder KR, Walter EB, Fry AM, & Jernigan DB (2018). Prevention and Control of Seasonal Influenza with Vaccines: Recommendations of the Advisory Committee on Immunization Practices—United States, 2018–19 Influenza Season. Morbidity and Mortality Weekly Report, 67, 1–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF (2018). Introduction to Mediation, Moderation, and Conditional Process Analyses: A Regression-based Approach. New York, NY: Guilford Press. [Google Scholar]
- Herr N (2006). Mediation with dichotomous variables. Retrieved January 30, 2019, from http://www.nrhpsych.com/mediation/logmed.html.
- Irving SA, Donahue JG, Shay DK, Ellis-Coyle TL, Belongia EA (2009). Evaluation of self-reported and registry-based influenza vaccination status in a Wisconsin cohort. Vaccine, 27, 6546–6549. [DOI] [PubMed] [Google Scholar]
- Kumar S, Quinn SC, Kim KH, Musa D, Hillyard KM, & Freimuth VS (2011). The social ecological model as a framework for determinants of 2009 H1N1 influenza vaccine uptake in the United States. Health Education and Behavior, 39, 229–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarty C, Killworth PD, Bernard HR, Johnsen EC, & Shelley GA (2001). Comparing two methods for estimating network size. Human Organization, 60, 28–39. [Google Scholar]
- McPherson M, Smith-Lovin L, & Cook JM (2001). Birds of a feather: Homophily in social networks. Annual review of sociology, 27, 415–444. [Google Scholar]
- Parker AM, Vardavas R, Marcum CS, & Gidengil CA (2013). Conscious consideration of herd immunity in influenza vaccination decisions. American Journal of Preventive Medicine, 45, 118–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rolnick SJ, Parker ED, Nordin JD, Hedblom BD, Wei F, Kerby T, Jackson JM, Crain AL, & Euler G (2013). Self-report compared to electronic medical records across eight adult vaccines: Do results vary by demographic factors? Vaccine, 31, 3928–3935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross L, Greene D, & House P (1977). The “false consensus effect”: An egocentric bias in social perception and attribution processes. Journal of Experimental Social Psychology, 13, 279–301. [Google Scholar]
- Schultz PW (1999). Changing behavior with normative feedback interventions: A field experiment on curbside recycling. Basic and Applied Social Psychology, 21, 25–36. [Google Scholar]
- Schultz PW, Nolan JM, Cialdini RB, Goldstein NJ, & Griskevicius V (2007). The constructive, destructive, and reconstructive power of social norms. Psychological Science, 18, 429–434. [DOI] [PubMed] [Google Scholar]
- Shaffer VA, & Zikmund-Fisher B (2013). All stories are not alike: Purpose-, content-, and valence-based taxonomy of patient narratives in decision aids. Medical Decision Making, 33, 4–13. [DOI] [PubMed] [Google Scholar]
- Sudman S (1985). Experiments in the measurement of the size of social networks. Social Networks, 7, 127–151. [Google Scholar]
- US Census Bureau (2012). Statistical abstract of the United States. Washington DC: US Department of Commerce. [Google Scholar]
- Vardavas R, & Marcum CS (2013). Modeling influenza vaccination behavior via inductive reasoning games In Manfredi P & d’Onofrio A (Eds). Modeling the interplay between human behavior and the spread of infectious diseases. New York, NY: Springer; (pp. 203–227). [Google Scholar]
- Weinstein ND, & Diefenbach MA (1997). Percentage and verbal category measures of risk likelihood. Health Education Research, 12, 139–141. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.