Abstract
Pregnancy provides motivation for women to improve their diets and increase their physical activity. Opportunistic brief interventions delivered as part of routine primary care have produced improvements in patients' health behaviour. Consequently, there have been calls for midwives to use contacts during pregnancy in this way. This study explored the experiences of pregnant women and research midwives/nurses of a brief intervention called Healthy Conversation Skills (HCS) being delivered as part of a randomised control trial, assessing the acceptability and feasibility of including this intervention in routine maternity care. Three research questions were addressed using mixed methods to produce four datasets: face‐to‐face interviews with participants, a focus group with the HCS‐trained midwives/nurses, case reports of participants receiving HCS and audio‐recordings of mid‐pregnancy telephone calls to the women which produced midwife/nurse HCS competency scores. Midwives/nurses used their HCS to support women to make plans for change and set goals. Women welcomed the opportunity to address their own health and well‐being as distinct from that of their baby. Midwives/nurses were competent in using the skills and saw healthy conversations as an effective means of raising issues of diet and physical activity. Recent extension of maternity appointment times provides ideal opportunities to incorporate a brief intervention to support behaviour change. Incorporating HCS training into midwifery education and continuing professional development would facilitate this. HCS is a scalable, brief intervention with the potential to improve the diets and physical activity levels of women during pregnancy, and hence the health of themselves and their babies.
Keywords: brief intervention, diet, Healthy Conversation Skills, routine maternity care, physical activity, pregnancy
Key messages.
Pregnant women value a focus on their own health as well as that of their babies.
A brief intervention in the form of healthy conversations with midwives/nurses was appreciated and led to many women setting behaviour change goals.
Incorporating HCS in maternity care and midwifery education could more effectively support women to improve their diets and physical activity levels during and after pregnancy.
An HCS approach provides a scalable option for helping to tackle obesity in pregnancy.
1. INTRODUCTION
Globally, approximately half of women enter pregnancy overweight or obese (Godfrey et al., 2017; International Weight Management in Pregnancy Collaborative Group, 2017; Poston et al., 2016). This has long‐term metabolic consequences for both women and babies and raises the risk of pregnancy complications (Ma, Schmidt, Tam, McIntyre, & Catalano, 2017). Weight control and lifestyle interventions have been shown to limit weight gain in obese pregnant women and elicit small improvements on women's quality of diet and physical activity levels, but these interventions require substantial support and encouragement from healthcare practitioners (Hanson et al., 2017; International Weight Management in Pregnancy Collaborative Group, 2017; Thangaratinam et al., 2012). There is a clear need to find more efficient and scalable ways of supporting pregnant women to make positive health behaviour changes.
Pregnancy may provide a stimulus for women to improve their diets and increase their physical activity. Pregnancy is also an opportunity for midwives and other healthcare professionals to provide support for women to adopt healthier behaviour (Olander, Darwin, Atkinson, Smith, & Gardner, 2015; Phelan, 2010). Opportunistic brief interventions delivered as part of routine primary care appointments have been shown to achieve significant improvements in health behaviours, including weight loss and smoking reduction, particularly if delivered by respected and trusted authorities (Aveyard et al., 2016; Aveyard, Begh, Parsons, & West, 2011). Consequently, there have been calls for midwives to use the relationship of trust they have with pregnant women in their care to engage women in improving their diets and nutritional status (Arrish, Yeatman, & Williamson, 2017). In the United Kingdom, these calls come in the context of Public Health England's agenda for “making every contact count” (NHS Health Education England, 2018).
Publicly funded maternity services, however, currently operate in an environment that severely constrains capacity to spend time supporting pregnant women to improve their diets and increase their physical activity. In an effort to maximise efficiency and impact of maternity services in the United Kingdom, the National Maternity Review “Better Births” proposed the reorganisation of services into local centres, bringing care providers together in community hubs, where women can access all elements of their care. These hubs offer midwifery and obstetric care alongside smoking cessation and weight management services (National Maternity Review, 2016). An obstacle to the provision of these services is that midwives have expressed a lack of confidence in their skills to broach such topics (Arrish et al., 2017; Holton, East, & Fisher, 2017). Recent research suggests that practitioners working in similar centres can be successfully trained to deliver a brief, opportunistic intervention to support behaviour change in their patients and clients (Black et al., 2014; Lawrence et al., 2016). What is not known is how best to incorporate this type of brief, opportunistic support for behaviour change into routine maternity care, nor whether such strategies are effective in engaging pregnant women in improving their health behaviour.
This paper describes the experiences of pregnant women and research midwives/nurses taking part in a trial of a brief intervention using Healthy Conversation Skills (HCS). HCS takes an empowerment approach to interpersonal communications, supporting goal setting and subsequent changes to behaviour. Training in HCS aims to shift practitioners from using a telling and suggesting approach to asking open discovery questions (Barker et al., 2011; Lawrence et al., 2016). See Box 1 for details.
Box 1. Description of Healthy Conversation Skills (HCS) training.
“Healthy Conversation Skills” training
Based on the principle that higher self‐efficacy is related to the adoption of better health behaviours, use of these HCS by front‐line practitioners is intended to increase individuals’ self‐efficacy levels, thereby supporting them to make positive changes. Communication is enhanced through practitioners developing the skill of asking open discovery questions ‐ those that generally begin with “how” and “what”. Such healthy conversations allow a patient to explore an issue, identify barriers, and generate solutions that can be reviewed with the practitioner at their next meeting. Training aims to increase self‐efficacy and sense of control of both practitioners and their patients/clients.
The four core skills are:
To ask open discovery questions (those that specifically support exploring of issues, barriers and priorities; problem‐solving; and identifying first steps to change).
To reflect on practice.
To listen rather than provide information.
To support goal setting through SMARTER (Specific, Measurable, Action‐oriented, Realistic, Timed, Evaluated, Reviewed) planning.
HCS training typically consists of two 3‐4 hour group sessions over one to two weeks to allow time for practising and reflecting on skills. Training is delivered by an HCS trainer experienced in group work and behaviour change, generally to a group of between 6 and 16 trainees. This should be followed by a period of on‐going support, which may include a phone call or visit from one of the trainers to find out how skills are being implemented in practice. The phone call/visit allow trainees to reflect on the training, how they have implemented their new skills, any barriers to their implementation and plans for continued or increased use, including embedding self and peer reflection as part of normal practice. Any follow‐up activities are also opportunities to collect evaluation data to assess the effectiveness of the training. Undertaking these activities from one month post‐training is based on an assumption that staff will have had opportunities to practise their new skills, and if they were finding this challenging, it would be a good time to reflect on this and make plans for progress. Further follow‐ups can be undertaken at later stages to assess longer term use of the skills in practice.
This study addressed three research questions:
How acceptable do women and research midwives/nurses find healthy conversations in planning diet and physical activity improvements during pregnancy?
How do healthy conversations support women to set behaviour change goals?
What do women think about having healthy conversations as part of their routine maternity care, and how feasible do midwives/nurses think these are to include?
2. METHODS
2.1. Setting: Southampton PRegnancy Intervention for the Next Generation (SPRING) trial
The data reported in this paper are drawn from those being collected as part of the SPRING trial (ISRCTN07227232). SPRING is being conducted in a large teaching hospital located in Southampton, UK (from October 2013 to October 2022). In 2015, the city of Southampton ranked 67th on the overall index of multiple deprivation out of the 326 local authorities in England (1 = most deprived; Southampton City Council, 2015b). In 2014/2015, 47% of pregnant women in Southampton were classified as overweight or obese at their first midwifery appointment (Southampton City Council, 2015a).
SPRING is a randomised controlled trial of vitamin D supplementation alongside a brief intervention that aims to improve pregnant women's diets and physical activity levels (Baird et al., 2016). The brief intervention is delivered by HCS‐trained midwives and paediatric nurses, referred to as midwives/nurses in this paper. Participants are recruited opportunistically from the local maternity hospital and are randomly assigned to one of four arms of the trial (vitamin D supplement + HCS, vitamin D supplement only, placebo supplement + HCS, and placebo supplement only). Within the trial, participants are asked, among other things, to attend four research appointments at 14, 19, and 34 weeks of gestation at the maternity hospital and 1 month post‐birth at home (diet and lifestyle questionnaires are completed at these times). Women also receive a phone call at 26 weeks of gestation from a research midwife/nurse.
2.2. Ethics
SPRING has ethical approval from the NRES Committee South Central—Hampshire B (13/SC/0409) and is conducted according to the Declaration of Helsinki. All participants provided written consent to take part in the trial and the subsequent face‐to‐face interview.
2.3. Brief intervention/HCS arms
At 14, 19, 26, and 34 weeks of gestation and 1 month post‐birth, the intervention midwives/nurses engage the women in the HCS arms of the trial in discussions about health behaviour change; however, the women are unaware that these healthy conversations form part of an intervention. All midwives/nurses delivering the brief intervention attended HCS training led by WL (Box 1; Barker et al., 2011). Ongoing support to enhance midwife/nurse competence and confidence in using the skills is provided regularly by WL/CV; this includes meetings, observations, discussions, and feedback.
2.4. Control arms
At each of the same five time points, the control midwives/nurses follow the standard protocol including completing body composition measurements, scans, questionnaires, and 26‐week phone calls but do not engage women in any exploratory conversations about their health behaviour.
2.5. Data presented in this paper
Data were collected using four different methods from participants and midwives/nurses involved in SPRING. Qualitative datasets consisted of face‐to‐face interviews with women after the trial (a), a focus group with the HCS‐trained midwives/nurses (b), and case reports of participants in the HCS arms (c). The fourth dataset was quantitative, reporting intervention midwives/nurses' HCS competency levels assessed from audio recordings of midpregnancy telephone calls to the women (d). Table 1 provides an overview of the data collection processes and time points. In the sections below, each bulleted number indicates one of the four data methods/datasets.
Table 1.
Summary of data collection methods
| Data collection method | Timing of data collection | Design | Participants | Tools/measures | Analysis strategy |
|---|---|---|---|---|---|
| 1. Face‐to face interview | 3‐6 months post‐birth | Researcher conducted audio‐recorded interview with participant in her home |
20 women from HCS arms 10 women from control arms |
Semi‐structured discussion guide
Coding frame |
Thematic analysis of transcripts using NVivo to manage data. RQ1, RQ2, and RQ3 |
| 2. Focus group | October 2015 | Moderated/observed by researchers independent of the study team; audio‐recorded discussion | One focus group with four HCS midwives/nurses | Semi‐structured discussion guide | Thematic analysis approach used to identify over‐arching topics. RQ1, RQ2, and RQ3 |
| 3. Case report | 14, 19, 26, and 34 weeks of gestation and 1 month post‐birth | Midwife/nurse completed two‐page report focused on SMARTER goal setting based on the healthy conversation at each of the five time points | All 20 women interviewed from HCS arms |
Case report template
HCS competency coding rubric |
Content analysis of topics discussed and goals set at the five time points. RQ2 |
| 4. Telephone interview | 26 weeks of gestation | Research midwife/nurse conducted audio‐recorded telephone interview with participant | 17/20 women interviewed from HCS arms (three failed recordings) |
Brief introductory script
HCS competency coding rubric |
Quantitative analysis: Mean HCS competency scores from each midwife/nurse were calculated. RQ2 |
Abbreviations: HCS, Healthy Conversation Skills; RQ, research question.
2.6. Participants and procedure
Qualitative interviews: Data were collected from two samples of women recruited to SPRING between April and December 2014 who had completed the trial; one group who had received the HCS intervention and another that had not. Between February and September 2015, all participants who recently had their 1 month post‐birth visit were sent invitations to participate in an interview in their own homes. Following consent, interviews were audio recorded and observed by another researcher.
Focus group: Five midwives/nurses were trained to deliver the HCS intervention in SPRING. In October 2015, four were available to participate in a focus group. The discussion explored their experiences of using HCS and impression of the effect on women's health behaviour. The focus group was audio recorded, moderated, and observed by researchers independent of the study team in order to encourage a full and frank discussion.
Participant case reports: The midwives/nurses complete case reports for all participants in the HCS arms of the trial at each of the five time points. Content of case reports for those who attended face‐to‐face interviews described in point 1 above was analysed.
Telephone interviews: HCS midwives/nurses telephone all SPRING participants in the HCS arms at approximately 26 weeks of gestation to conduct a short audio‐recorded interview. The purpose of this call is to hold another healthy conversation to provide ongoing support for goals set. Data from calls with the HCS participants who provided face‐to‐face interviews described in point 1 above were analysed.
2.7. Materials (available from first author on request)
Qualitative interviews: A semi‐structured discussion guide was developed to explore participants' experiences of the trial, particularly their interactions with the research midwives/nurses. Ethically approved consent forms and patient information sheets were also provided.
Focus group: A semi‐structured discussion guide was developed to explore midwives/nurses' experiences of using HCS.
Participant case reports: A template was developed for the HCS midwives/nurses to capture details of healthy conversations at each of the five time points, and evidence of SMARTER goal setting (Box 1).
Telephone interviews: A short introductory script was provided for all midwives/nurses to guide the 26‐week calls. Conversations are structured around each participant's case report.
2.8. Analysis strategy
2.8.1. Qualitative data—Thematic analysis
All audio recordings and transcripts used participant and midwife/nurse ID numbers as sole identifiers.
Face‐to‐face interview recordings were transcribed verbatim and analysed thematically following established guidelines (Braun & Clarke, 2006), using NVivo software (QSR International, version 11). Initial codes were developed by creating “nodes” in NVivo as new topics arose. Where a section of text fitted into more than one code, it was categorised under all appropriate codes. After all transcripts had been coded this way, nodes were organised into themes and subthemes. An initial coding frame was developed based on themes arising inductively from analyses of the first three transcripts (TM, SS, and WL), using a constant comparative approach in line with a relativist ontological and subjective epistemic position (Boyatzis, 1998; Swift & Tischler, 2010). The coding frame was refined through double coding of 20 transcripts (TM, SS, and WL) until a final coding frame was agreed. To assess rigour, a subset of five transcripts were analysed for interrater reliability; minor discrepancies arose in 134 out of 2,216 lines, equating to a 94% level of agreement. Themes and subthemes were illustrated with verbatim quotations. Finally, codes and quotes were used to produce a theoretical framework that would best address the research questions. Comparison of the data for HCS and control arm participants allowed differences and similarities in women's experiences, opinions, and feelings to be identified. Sufficient participants from each arm were interviewed for data saturation to be reached (Fusch & Ness, 2015). This paper is based on the data from three of the five emergent themes from the interviews; these being the themes that relate to behaviour change and goal setting and how the HCS approach compares to routine care (coding frame detailing all themes available from the first author).
For the HCS midwife/nurse focus group, the processes and principles of conducting thematic analysis were followed, with two of the HCS developers (WL/CV) taking a similar approach to the analysis and interpretation described above.
HCS participant case reports were scanned into NVivo and content analysis undertaken to identify topics discussed and goals set over the course of the trial.
2.8.2. Quantitative data—Statistical analysis
Responses to the question asking for “highest level of education attainment” (EA) were collapsed from seven to three categories: high, medium, and low EA; no one reported having no qualifications. Responses to “Other” were all recoded into medium as being the most appropriate level for the qualifications reported.
Statistical analyses were completed using the Stata statistical software package version 13.0 (Statacorp, 2013). Descriptive analyses were conducted using data from the 26‐week phone calls to score HCS midwives/nurses' competence in use of three HCS (asking open discovery questions, listening, and supporting SMARTER goal setting, see Box 1 using a previously developed coding rubric (Black et al., 2014; Lawrence et al., 2016). Scores can range from 0 (no evidence of competence) to 4 (high level of competence) and were totalled for all three competencies to give an overall mean out of 12 for each HCS midwife/nurse. Data from the case reports and 26‐week phone calls were analysed to identify the frequency with which topics were discussed. Chi‐squared tests were performed to assess whether there were differences in educational attainment and number of children, between this study sample and all women recruited onto the SPRING trial during the same period.
3. RESULTS
Figure 1 shows the number of participants whose data contributed to the analysis presented in this paper at each time point.
Figure 1.
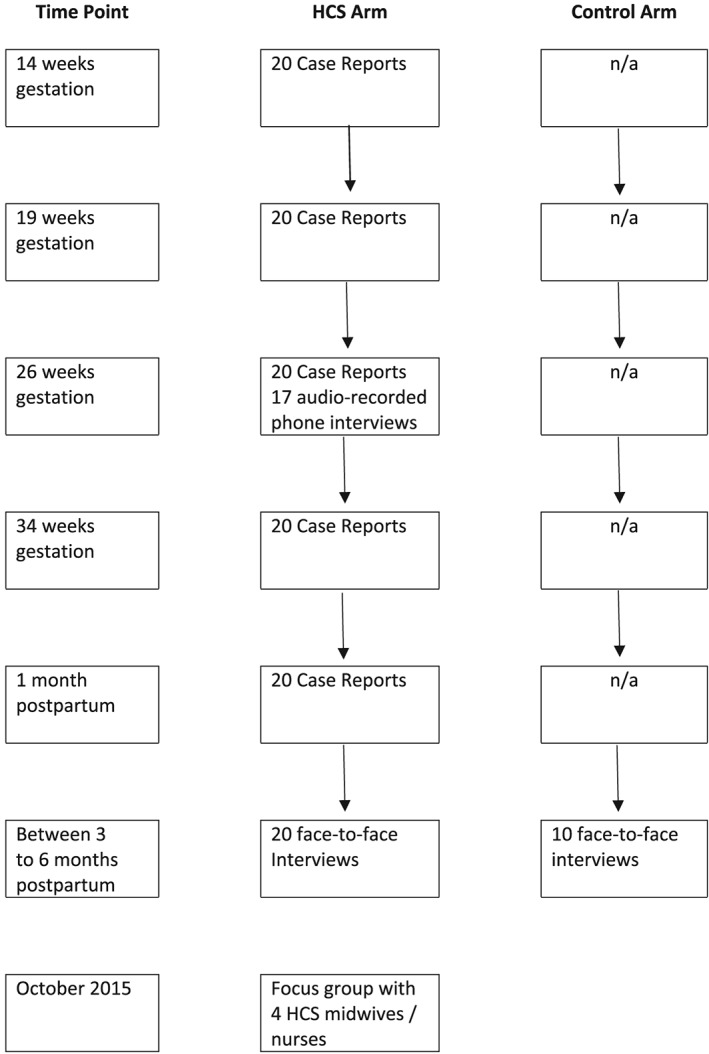
Number of participants whose data contributed to the analysis at each time point. HCS, Healthy Conversation Skills
3.1. Characteristics of participants
A total of 20 women from the HCS arms and 10 from the control arms (total n = 30) took part in the face‐to‐face interviews. Those interviewed did not differ significantly in demographic profile from all other women who were recruited to SPRING between the same dates (Table 2). The HCS midwives/nurses who took part in the focus group have a range of skills in nursing, midwifery, and research practice but are all experienced practitioners (Table 3).
Table 2.
Characteristics of the women recruited to SPRING between April and December 2014 (n = 145)
| Level of educational attainment (EA) N (%) | Total children, inc index child N (%) | ||||||
|---|---|---|---|---|---|---|---|
| Group | Mean age in years (SD) | Secondary education (CSE, O level/GCSE) Low EA | Further education (A level, HND, diploma) Medium EA | Higher education (degree) High EA | 1 | 2 | 3 |
| Intervention participants (n = 20) | 31 (6.24) | 7 (35%) | 8 (40%) | 5 (25%) | 10 (53%) | 5 (26%) | 4 (21%) |
| Control participants (n = 10) | 33 (3.83) | 1 (10%) | 3 (30%) | 6 (60%) | 3 (30%) | 5 (50%) | 2 (20%) |
| Remaining group of women recruited to SPRING between April and December 2014 (n = 115)a | 31 (5.13) | 17 (15%) | 47 (41%) | 50 (44%) | 42 (38%) | 43 (39%) | 25 (23%) |
| Chi‐square | χ2(4) = 6.80, P = .15 | χ2(4) = 2.24, P = .69 | |||||
Some missing data for number of children (n = 110) and level of education (n = 114).
Table 3.
Characteristics of four Healthy Conversation Skills midwives/nurses taking part in the focus group
| Research midwife/nurse | Age | Ethnicity | Years qualified as nurse | Years' experience as midwife | Years' experience of research |
|---|---|---|---|---|---|
| 1 | 56 | White British | 34 | 6 | 27 |
| 2 | 54 | White British | 32 | 4 | 21 |
| 3 | 57 | White British | 0 | 13 | 7 |
| 4 | 45 | White British | 23 | 0 | 7 |
Findings from analyses of data from the face‐to‐face interviews with participants and the midwife/nurse focus group are presented as they address each research question in turn. Each quote is identified by intervention or control, ID number, age, number of children (including the baby born during the trial), and level of educational attainment (see Table 2).
How acceptable do women and research midwives/nurses find healthy conversations in supporting diet and physical activity improvement in pregnancy?
3.2. Acceptability to women
Thematic analysis of the face‐to‐face interviews with 20 women in the HCS arms and 10 in the control arms identified differences in the way they perceived the support they received from the research midwives/nurses. Women in the HCS arms generally found the intervention acceptable, the experience empowering, and welcomed the midwives'/nurses' interest in their own, as well as their babies' health.
I think sometimes it's helpful for people to ask you things like that. It makes you reflect on, actually, how are you managing in pregnancy? Are you making the right choices? (Int12229, 36 years, one child, high EA)
I think it just takes you away from everything else going on, and gets you to think about just being a pregnant woman for once … make you focus on being healthy for you, and exercising for you. So that was good. (Int12309, 28 years, one child, low EA)
There were, however, a few instances where women felt judged or under pressure to make a change.
Maybe just that slightly judgemental, ‘last time you did say you were going to go to the gym and you've only done your induction’ and I came away thinking I'd sort of let myself or them down a little bit. (Int12243, 35 years, one child, high EA)
Every time they rang you … it was a little bit like the diet police. (Int12496, 39 years, two children, low EA)
In contrast with the experience of the women in the HCS arms, women in the control arms did not mention any specific benefits from their conversations with the research midwives/nurses.
Just work really … how the kids were, just chit‐chat, just making me relaxed. (Con12369, 32 years, three children, medium EA)
There was no indication of any exploratory conversations about women's health occurring in the control arms. Conversations tended to focus on other aspects of daily life.
I remember getting into a discussion with one of the midwives down to where we were buying our Christmas turkeys … it wasn't very much about the pregnancy! (Con12275, 39 years, two children, high EA)
These contrasting experiences demonstrate that the HCS intervention encouraged the majority of participants to think about improving their health behaviour.
3.3. Acceptability to midwives/nurses
The midwives/nurses enjoyed the HCS training, valuing the insights gained from training in a mixed group and the interactive, nondidactic approach.
It was very good, very creative and good that you're all involved … it made you question your own thoughts and views.
They felt that post‐training interactions with trainers and each other allowed them to learn from others' experiences and provided a model for embedding the skills in their practice.
I saw you do a “healthy conversation” and it was really helpful for me to see the natural conversation with mum, rather than it being—“right now we are going to talk about your goals.”
At the beginning, the midwives/nurses were concerned about how the participants might react to attempts to engage them in discussion about their diet and physical activity, as these are typically seen as difficult issues to raise. On reflection, they realised these concerns were unfounded.
I thought when I did the training that the mums might find it difficult. But nobody seems to have reflected back to me that that's the case.
Midwives/nurses felt that conversations that resulted from using the skills were productive. They saw the approach as having the potential to transform how they support women's health.
As a practitioner I find it reassuring that by having this conversation and asking a couple of opportune questions you can just get below the surface of what is on her mind, and what is important, and what she can change.
In summary, the evidence addressing RQ1 indicates that whilst participants were unaware that they were having “healthy conversations,” they described the interactions in positive terms and valued having conversations that focused on themselves as well as their baby. Focus group data revealed that the midwives/nurses found the HCS training to be acceptable in its format and delivery and valued the skills obtained.
How do healthy conversations support women to set behaviour change goals?
3.4. Interview and focus group data
Women in the HCS arms frequently described experiences of discussing plans for change with the research midwives/nurses.
I did make a change in terms of the amount of cake I was eating … we pinpointed that I worked in an office where people brought stuff in a lot. And I don't want to say no to it, because it's nice and someone's brought it in, and why shouldn't I have a bit of cake? But I think what changed is I stopped buying and taking stuff like that to work. (Int12243, 35 years, one child, high EA)
Women in the HCS arms described being prompted to identify barriers to change and strategies for overcoming these, like taking alternative forms of exercise.
If I can't go (to the gym), instead of using my car to take my son to school, I'll walk him to the school and obviously then walk back again … walking is the next best thing (Int12427, 40 years, three children, low EA)
I don't want to leave (baby), so I want to do some fitness classes where I can take her along and use her as a weight or something! (Int12378, 25 years, one child, medium EA)
In contrast, none of the participants in the control arms mentioned having made any plans to change as a result of talking to the midwife/nurse.
I: What plans did you make to change anything when you were pregnant?
P: None … not knowingly. (Con12508, 39 years, one child, high EA)
In the focus group, the midwives/nurses recalled many instances of supporting women to make a SMARTER plan for change and identify barriers to be overcome.
I had a lady that wanted to eat more fruit and one of her barriers was actually being able to physically carry it, because she went on a bike … which I never would have known! And it is interesting to see where they are coming from rather than if you are just giving advice.
… they have learnt that they might not be able to go swimming five times a week but they could walk three times a week or something and that's valuable for them I think. Because they have explored it and they have tried.
Using the HCS skills (asking open discovery questions, listening, and supporting SMARTER goal setting) provided a structured and empowering framework that enabled the midwives/nurses to support the participants to reflect on their current behaviour, often leading to plans for change.
She said to me “… it has made me think about snacking on chocolate and it has made a difference” … she is telling you about something she has done because of her involvement in the study.
Furthermore, whilst the HCS participants were blind to the intervention, they unknowingly provided confirmation that the midwives/nurses had been having healthy conversations with them, as they could recall specific open discovery questions they had been asked.
I: What kind of things did you talk about with them?
P: A lot about diet, healthy lifestyle, how I was living. How the pregnancy was developing. How I was feeling, who supported me, the types of food I was eating. (Int12229, 36 years, one child, high EA)
The participants' perceptions of these healthy conversations were supported by an assessment of the midwives/nurses' competence in using HCS against a standard competency framework based on data from the 26‐week phone call recordings (Table 4). These data confirm that the midwives/nurses demonstrated a high standard of competence in all three skills; total mean score was 3.8 out of 4.
Table 4.
Mean competency scores for three Healthy Conversation Skills (HCS) midwives/nurses from 26‐week phone call
| Research midwife/nurse | No. of calls made | Asking open discovery questions | Listening | Supporting SMARTER goal setting | Mean HCS score |
|---|---|---|---|---|---|
| 1 | 1 | 4 | 4 | 4 | 4 |
| 2 | 5 | 3.8 | 4 | 3.4 | 3.7 |
| 3 | 11 | 4 | 3.8 | 3.3 | 3.7 |
| Total | 17a | 3.9 | 3.9 | 3.6 | 3.8 |
Note. Scale 0–4: 0 = no competency; 4 = high competency.
Three audio recordings failed.
3.5. Case report data
Analysis of the case report data collected from women in the HCS arms indicated that all 20 women discussed their physical activity and 19 discussed their diets on at least one occasion (Figure 2). These data also indicate that all women set at least one goal at some point in the trial: 18 of the 20 women set a goal to increase physical activity, 18 to eat more healthily, and 13 focused on another health behaviour such as breastfeeding (n = 12), smoking cessation (n = 4), or mental health (n = 3). At the first visit, a total of 22 goals were set, with slightly more goals being set at the three later consultations in pregnancy (30, 36, and 29 goals, respectively) and at the 1 month post‐birth visit (n = 36; Figure 3). These numbers indicate that some set more than one goal during the course of the trial.
Figure 2.
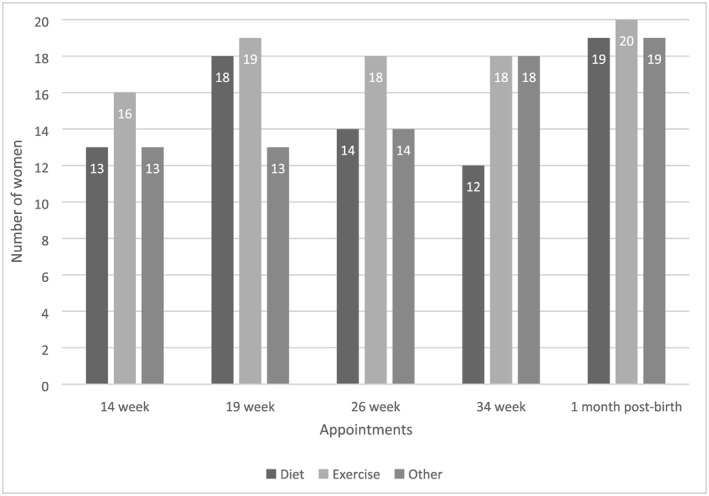
Case report data—topics discussed at each time point
Figure 3.
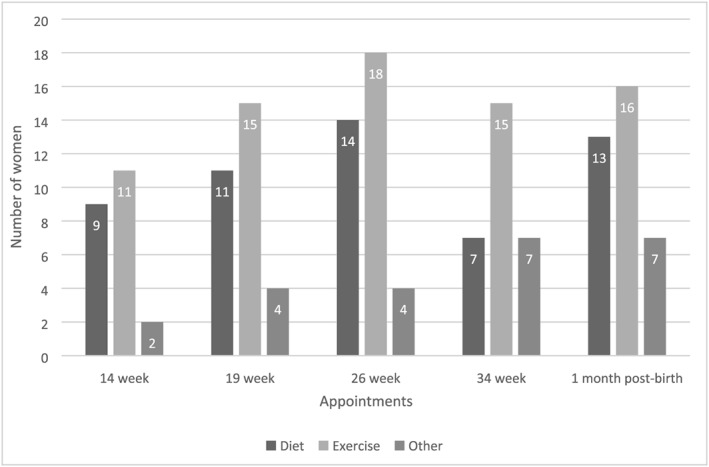
Case report data—types of goals set or ongoing at each time point
The factors that appear to be important for the effectiveness of HCS in supporting women to set behaviour change goals were the high level of competence midwives/nurses displayed in using HCS and women's acceptance of and engagement with this empowerment approach.
What do women think about having healthy conversations as part of their routine maternity care, and how feasible do midwives/nurses think these are to include?
3.6. Women's views on research midwife/nurse versus routine midwifery care
Participants from all arms of the study commented on the short NHS appointment times and mixed experiences of NHS care.
Once you have had more than one child you don't see midwives as much anyway … so it was nice to know that I could contact them (research midwife/nurse), but I never did really. Just got on with it … my (NHS) midwife was never there. (Con12369, 32 years, three children, medium EA)
Women in receipt of the HCS intervention appreciated the chance to reflect on their own health that was offered by the research midwives/nurses, feeling this was missing within routine NHS care.
It does make you more aware, if there was that support for general pregnancies … then maybe it would increase people's awareness of what they are eating. (Int12087, 40 years, three children, low EA)
They also would like to be asked questions by their NHS midwife to encourage them to explore their perspectives and health rather than be left to take responsibility for raising issues.
It probably would be beneficial to have some kind of well‐being discussion. It's always left to the women to ask the midwife, like “Can I do more exercise? Is that OK?” rather than the midwife instigating …. (Int14021, 32 years, two children, high EA)
Furthermore, they enjoyed the opportunity to think about themselves as distinct from the baby. They felt the current focus within NHS care on the health of the fetus could be broadened to include their own health, making the point that this does not have to take long, so would be feasible to accommodate within a standard appointment.
The big difference is the fact that … they have to do the forms and medical bits as well; it's just tagging that extra five minutes on the end … How are you feeling? … that's the bit that makes the difference I think. It doesn't have to be long. (Int12001, 44 years, two children, high EA)
3.7. Midwives/nurses' views
The midwives/nurses felt that adopting a HCS approach was feasible and that it became easier with practice, providing a model of what might be achieved in routine NHS midwife/nursing care.
So I wanted to have an extra session that said “So what you are going to do is A,B,C,X,Y,Z, and this is what you might come up against”. Looking back, actually what we did was went out and got on with it, and learnt a lot in the first few interviews … it was enough to do the training and then just go on and do it.
Midwives/nurses suggested that health behaviour change could be better supported in routine maternity care by including HCS in midwifery education.
They could use it for student midwives … an afternoon session or something like that.
If they said “Well we are going to give you this time, and you're going to have this training and we are going to set aside time for it and give you support afterwards,” then I think maybe we are alright with it!
They also expressed insights into the benefits and challenges of embedding healthy conversations into routine NHS midwifery appointments. Despite the limitations of time, the midwives/nurses advocated for the use of healthy conversations in providing the high quality care they wished to deliver.
It is very easy to say “oh you are overweight and … you have put on this much, and you should not be putting on anymore”. Helping (women) identify where they can actually make some positive changes has got to be good. We are all very passionate about our ladies, and getting them having
best outcomes possible.
There was some conversation about the impact of anticipated changes in policy on antenatal care and how these changes might include an increase in length of appointments. This was felt to be timely for facilitating the introduction of healthy conversations into routine care, with significant consequences for the interactions with women.
I think (healthy conversations) would be very useful … I have heard rumours that we may be increasing our standard antenatal appointment times, which would be great, and which would hopefully allow us to be asking more of these types of questions … (We would) definitely be able to explore more, improve our relationship with women, especially around obesity.
One suggestion to support the introduction of HCS into routine practice was to train other healthcare professionals in these skills.
Having someone, maybe not a midwife, who could actually spend the time with the women; because so many women want to talk … and there isn't always that time.
To answer RQ3, women welcomed the opportunity to discuss their own health and well‐being. Midwives/nurses found their confidence in using HCS built over time, and it was feasible to have healthy conversations with the women. They saw healthy conversations as having great potential to help address the effect of health issues such as obesity. They suggested that the anticipated policy review meant it was a good time to engage midwives and commissioners in thinking about incorporating skills to support behaviour change into routine antenatal appointments and into midwifery/nursing training and education.
4. DISCUSSION
This paper set out to address three questions, and findings in relation to these are summarised below.
RQ1. How acceptable do women and research midwives/nurses find healthy conversations in supporting diet and physical activity improvement in pregnancy?
Analysis of interview data suggests that women found it supportive to have exploratory conversations with the research midwife/nurse about their diet and physical activity. The general feeling was that the conversations were personalised and empowering; women appreciated the opportunity to discuss their own health and goals. A minority of women expressed a feeling of being judged at points during the conversations, one using the term “the diet police.” This clearly is not the aim of these exploratory conversations and practitioners need to be aware of the potential to come across in this way and strive to keep their tone and expression neutral but supportive. Midwives/nurses enjoyed the training and valued the ongoing support. They found it effective to use their newly acquired skills to engage the women in healthy conversations and were reassured that the women were not resistant to these.
RQ2. How do healthy conversations support women to set behaviour change goals?
The interview and focus group data indicate that women felt able, through discussions with research midwives/nurses, to identify barriers to change and strategies to overcome them, which led them to set a health behaviour goal. Audio recordings of midpregnancy phone calls demonstrated that the research midwives/nurses had high levels of competence in using open discovery questions, listening, and supporting SMARTER goal setting. Case report data confirmed that midwives/nurses engaged the women in discussing their diets, physical activity, and other health‐related topics and supported them to make plans for change. Though exploratory conversations were held at every time point, more goals were set in the later stages of pregnancy and post‐birth.
RQ3. What do women think about having healthy conversations as part of their routine maternity care, and how feasible do midwives/nurses think these are to include?
In the interviews, women described appreciating the opportunity to reflect on their health, prompted and empowered by the research midwives/nurses, and suggested that this was missing from routine maternity care. They felt that the current antenatal focus was all on their babies rather than themselves. Research midwives/nurses described how using HCS in their practice became more feasible over time as their skills and confidence increased. They felt that HCS could be incorporated into routine NHS practice through a combination of inclusion into midwifery training and education, revising the length of antenatal appointments and training staff other than midwives to have healthy conversations with pregnant women.
4.1. Implications for policy and practice
Pregnancy offers an opportunity to improve women's health and the lifelong health of their babies (Phelan, 2010; Poston et al., 2016). Effective interventions in pregnancy, however, tend to be those that require significant resource, a lot of input from healthcare professionals, and a major commitment from the women themselves (Hanson et al., 2017). This presents a conundrum because such interventions are difficult to take to scale and to incorporate into routine care.
Brief interventions such as HCS may offer a solution because they require minimal resource and are scalable for delivery within opportunities provided by current primary care (Lamming et al., 2017). The “making every contact count” agenda in the United Kingdom recognises the potential that health and social care practitioners have to support behaviour change in their patients. Public Health England reports examples where this approach has been used effectively to improve health and health behaviour in different population groups (Public Health England, 2016). They describe a brief intervention as being level two of four intervention types to change behaviour according to level of intensity. It is described as “discussion, negotiation or encouragement, with or without written or other support or follow‐up. It may also involve a referral for further interventions, directing people to other options, or more intensive support and usually takes less than thirty minutes” (Public Health England, 2016, p. 15). A systematic review of interventions using this approach in primary care shows significant increases in physical activity (Lamming et al., 2017), and one large‐scale application of a brief intervention delivered in a general practice setting resulted in population weight loss (Aveyard et al., 2016).
In the United Kingdom, satisfaction with pregnancy services is reportedly high (Henderson & Redshaw, 2017). In Australia, midwives were described as being in a position of trust with the women in their care, making them ideally placed to deliver a brief intervention (Arrish et al., 2017). These Australian midwives struggled however to find time within the existing care pathway to have effective conversations about nutrition. Time and resource constraints as well as a lack of confidence have all previously been reported as barriers to addressing diet and weight by U.K. midwives (Macleod et al., 2013; McCann et al., 2018). Current maternity care arrangements in the United Kingdom offer multiple opportunities for brief interventions; women will routinely be seen approximately 10 times during pregnancy and post‐birth. The routine time for an antenatal appointment in Southampton, UK, where this study is based recently increased from 20 to 30 min. Anecdotally, midwives report that this makes appointments less stressful for them and allows more time to talk to women about their health and well‐being. Training the maternity workforce in HCS could enable them to use this additional time more effectively to support women to improve their health behaviour. Our analysis (in Figures 2 and 3) shows that women may not respond to the first conversation by setting goals for change but are likely to do so in subsequent consultations, suggesting that having more than one opportunity to reflect and plan for change may increase the impact of such conversations.
Midwives already have skills and expertise in matters pertaining to a woman's experience of pregnancy. Evidence suggests, however, that they lack confidence in supporting behaviour change, finding it particularly difficult to raise the topic of weight (Holton et al., 2017; Lee, Haynes, & Garrod, 2012). Training midwives in skills to deliver brief interventions such as that described within this paper can support them to do this. Midwives/nurses who delivered the intervention in our study felt HCS would be useful as part of routine consultations. Others have identified the form of delivery to be crucial in determining intervention success (Dombrowski, O'Carroll, & Williams, 2016), but it is largely unexplored as a factor in determining effectiveness. It can obviously influence intervention engagement, adherence, and fidelity. Interventions are only effective if people engage with them. HCS offer a method of introducing behaviour change techniques such as goal setting, which most women in our study found to be acceptable and empowering. In a Canadian study, dietitians using HCS to support women manage pregnancy weight gain found the skills to be acceptable and possible to accommodate within a time‐constrained setting (Jarman, Adam, Lawrence, Barker, & Bell, 2018). Women in that study who were supported by a practitioner trained in HCS were more satisfied with their care than women who saw other practitioners. This experience is in marked contrast to midwives' concerns that if they broach topics such as weight, they will damage their relationship with the women in their care (Holton et al., 2017; Lee et al., 2012; Macleod et al., 2013).
There is a gap in support currently offered to midwives to help them fulfil their role in promoting diet and lifestyle improvements in pregnancy. One example of an initiative to fill this gap that is local to the study reported in this paper but as yet untested is a service called Southampton Healthy Living. This has just begun to provide local people including pregnant women with support for health behaviour change through contact with dedicated staff (SCA Group, Southampton Voluntary Services,, & Solent NHS Trust, 2018). This service provides both the time and focus that midwives require to engage pregnant women in making plans to improve their health.
NICE guidance and the associated quality standard makes recommendations in relation to maternal and child nutrition, based on “advise,” “encourage,” and “provide information” models of intervention (NICE, 2008, 2015). We know these methods are less likely to support change in women's health behaviour than the empowering, problem‐solving methods employed in healthy conversations (Kelly & Barker, 2016). Guidance also suggests training for healthcare professionals in nutrition, but there is no suggestion that they may need training in effective modes of delivery of nutrition advice and support. Both the women and midwives/nurses in the current study indicated that they would value the adoption of a HCS approach in routine midwifery consultations.
Lack of time in routine consultations was a barrier to implementing HCS that concerned the research midwives/nurses. As one solution, they suggested that other staff involved in women's care also be trained in HCS. The National Maternity Review “Better Births” suggests that bringing a range of healthcare practitioners under one roof provides an ideal opportunity to provide continuity of care, something that is widely called for (Henderson & Redshaw, 2017). HCS training for all staff involved in maternity care could improve continuity, providing a coherent and consistent approach to communication and support. It would enable doctors and other healthcare professionals to better support women in improving their health behaviour. Our previous research has demonstrated that a wide range of health and social care staff can be trained to use HCS (Lawrence et al., 2016).
4.1.1. Strengths and limitations
As with any qualitative research, no claim is made that the views expressed by the participants in this study are representative of all pregnant women in Southampton. However, they were a relatively heterogeneous group, with similar characteristics to the larger SPRING population of women. Recruitment to the SPRING trial is ongoing so little is currently known about the representativeness of the trial participants, but there is no reason to believe that the views expressed by women in this study would be very different if we had recruited a different sample. It seems reasonable to speculate that the findings reported here are relevant to maternity care outside the United Kingdom, but it would be useful to explore the views of midwives and pregnant women from other countries.
To minimise the likelihood of interpretation of the qualitative data being misrepresentative, members of the research team worked together to follow a rigorous and standard methodology and to develop the coding frames for both the interviews and focus group until the final versions were felt to represent the findings discussed above (Boyatzis, 1998; Braun & Clarke, 2013; Swift & Tischler, 2013).
The sample size for the interviews was reasonable for this type of study. Whilst there was only one focus group with four midwives/nurses, this was moderated and observed by researchers independent of the study team to minimise any bias. All but one of the midwives/nurses conducting the HCS arm of the trial at that time attended the focus group, so there were no others whose views could have been sought. Including these focus group data has provided some validation of what the women recalled about their appointments, and some insight into the midwives/nurses' experiences of delivering the HCS intervention. Drawing on their combined years of experience of midwifery and nursing practice also provides important insights into how HCS could be incorporated into routine NHS care.
5. CONCLUSION
The recent move to extend maternity appointment times provides an ideal opportunity to incorporate a brief intervention to support behaviour change such as HCS. One way to facilitate this would be to incorporate HCS training into midwifery education and continuing professional development. Using HCS in research appointments was found to be acceptable and feasible and led to women making plans for health behaviour change. It thus represents a basis for a scalable, brief intervention with the potential to improve the diets and physical activity levels of women during pregnancy, and therefore the long‐term health of their offspring.
CONFLICTS OF INTEREST
The authors declare that they have no competing interests
CONTRIBUTIONS
All authors took part in the design of the study. WTL and MB drafted the manuscript with input from all authors. The data were collected by WL, TM, DW, SS, KH, KM, and JH and analysed by SS, TM, BT, and CV led by WL. CC is Chief Investigator; MB, NCH, and JB are Principal Investigators and together they have overall responsibility for the SPRING trial. HI is the statistician on SPRING, and CV leads the trial process evaluation. JH, KH, and KM are research midwives/nurses on the trial. All authors approved the final manuscript for publication.
AVAILABILITY OF DATA AND MATERIAL
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request. All data generated or analysed during this study are included in this published article (and its supplementary information files).
ACKNOWLEDGMENTS
We thank the mothers who gave us their time, the SPRING team for their assistance with the study, and Carol Chapman and Ilse Bloom for running the focus group with the midwives/nurses.
JB, MB, NCH, and TM have received funding from Danone NutriciaEarly Life Nutrition. Members of HI's team have received funding fromNestec and Abbott Nutrition. CC reports personal fees, consultancy,lecture fees, and honoraria from Alliance for Better Bone Health,Amgen, Eli Lilly, GlaxoSmithKline, Medtronic, Merck, Novartis, Pfizer,Roche, Servier, and Takeda, outside the submitted work. NCH reportspersonal fees, consultancy, lecture fees, and honoraria from Alliancefor Better Bone Health, AMGen, MSD, Eli Lilly, Servier, Shire,Consilient Healthcare, and Internis Pharma, outside the submittedwork. WL reports consultancy and lecture fees from Danone Nutricia,outside the submitted work.
Lawrence W, Vogel C, Strömmer S, et al. How can we best use opportunities provided by routine maternity care to engage women in improving their diets and health?. Matern Child Nutr. 2020;16:e12900 10.1111/mcn.12900
REFERENCES
- Arrish, J. , Yeatman, H. , & Williamson, M. (2017). Midwives' role in providing nutrition advice during pregnancy: Meeting the challenges? A qualitative study. Nursing Research and Practice, 2017 10.1155/2017/7698510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aveyard, P. , Begh, R. , Parsons, A. , & West, R. (2011). Brief opportunistic smoking cessation interventions: A systematic review and meta‐analysis to compare advice to quit and offer of assistance. Addiction Review, Article first published online: 28 Feb 2012, 107(6), 1066–1073. [DOI] [PubMed] [Google Scholar]
- Aveyard, P. , Lewis, A. , Tearne, S. , Hood, K. , Christian‐Brown, A. , Adab, P. , … Jebb, S. A. (2016). Screening and brief intervention for obesity in primary care: A parallel, two‐arm, randomised trial. The Lancet, 388, 2492–2500. 10.1016/S0140-6736(16)31893-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baird, J. , Barker, M. , Harvey, N. C. , Lawrence, W. , Vogel, C. , Jarman, M. , … Cooper, C. (2016). Southampton PRegnancy Intervention for the Next Generation (SPRING): Protocol for a randomised controlled trial. Trials, 17(1), 493 10.1186/s13063-016-1603-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barker, M. , Baird, J. , Lawrence, W. , Jarman, M. , Black, C. , Barnard, K. , … Cooper, C. (2011). The Southampton initiative for health: A complex intervention to improve the diets and increase the physical activity levels of women from disadvantaged communities. Journal of Health Psychology, 16(1), 178–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Black, C. , Lawrence, W. , Cradock, S. , Ntani, G. , Tinati, T. , Jarman, M. , … Baird, J. (2014). Healthy Conversation Skills: Increasing competence and confidence in front‐line staff. Public Health Nutrition, 17(3), 700–707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyatzis, R. E. (1998). Transforming qualitative information: Thematic analysis and code development. Thousand Oaks, CA, US: Sage. [Google Scholar]
- Braun, V. , & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3, 77–101. [Google Scholar]
- Braun, V. , & Clarke, V. (2013). Successful qualitative research: A practical guide for beginners. London: SAGE Publications. [Google Scholar]
- Dombrowski, S. U. , O'Carroll, R. E. , & Williams, B. (2016). Form of delivery as a key ‘active ingredient’ in behaviour change interventions. British Journal of Health Psychology, 21(4), 733–740. 10.1111/bjhp.12203 [DOI] [PubMed] [Google Scholar]
- Fusch, P. I. , & Ness, L. R. (2015). Are we there yet? Data saturation in qualitative research. The Qualitative Report, 20(9), 1408–1416. [Google Scholar]
- Godfrey, K. M. , Reynolds, R. M. , Prescott, S. L. , Nyirenda, M. , Jaddoe, V. W. V. , Eriksson, J. G. , & Broekman, B. F. P. (2017). Influence of maternal obesity on the long‐term health of offspring. The Lancet Diabetes & Endocrinology, 5(1), 53–64. 10.1016/S2213-8587(16)30107-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanson, M. , Barker, M. , Dodd, J. M. , Kumanyika, S. , Norris, S. , Steegers, E. , … Yang, H. (2017). Interventions to prevent maternal obesity before conception, during pregnancy, and post partum. The Lancet Diabetes and Endocrinology, 5(1), 65–76. 10.1016/s2213-8587(16)30108-5 [DOI] [PubMed] [Google Scholar]
- Henderson, J. , & Redshaw, M. (2017). Change over time in women's views and experiences of maternity care in England, 1995–2014: A comparison using survey data. Midwifery, 44, 35–40. 10.1016/j.midw.2016.11.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holton, S. , East, C. , & Fisher, J. (2017). Weight management during pregnancy: A qualitative study of women's and care providers' experiences and perspectives. BMC Pregnancy and Childbirth, 17, 351 10.1186/s12884-017-1538-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- International Weight Management in Pregnancy Collaborative Group (2017). Effect of diet and physical activity based interventions in pregnancy on gestational weight gain and pregnancy outcomes: Meta‐analysis of individual participant data from randomised trials. BMJ, 358, j3119 10.1136/bmj.j3119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jarman, M. , Adam, L. , Lawrence, W. , Barker, M. , & Bell, R. (2018). Healthy Conversation Skills as an intervention to support healthy gestational weight gain: Experience and perceptions from intervention deliverers and participants. Patient Education and Counseling, 102(5), 924–931. (Dec 23. pii: S0738‐3991(18)31026‐7. 10.1016/j.pec.2018.12.024. [Epub ahead of print]). 10.1016/j.pec.2018.12.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly, M. P. , & Barker, M. (2016). Why is changing health‐related behaviour so difficult? Public Health, 136, 109–116. 10.1016/j.puhe.2016.03.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamming, L. , Pears, S. , Mason, D. , Morton, K. , Bijker, M. , Sutton, S. , & Hardeman, W. (2017). What do we know about brief interventions for physical activity that could be delivered in primary care consultations? A systematic review of reviews. Preventive Medicine, 99, 152–163. 10.1016/j.ypmed.2017.02.017 [DOI] [PubMed] [Google Scholar]
- Lawrence, W. , Black, C. , Tinati, T. , Cradock, S. , Begum, R. , Jarman, M. , … Barker, M. (2016). Making every contact count’: Longitudinal evaluation of the impact of training in behaviour change on the work of health and social care practitioners. Journal of Health Psychology, 21(2), 138–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee, D. J. , Haynes, C. L. , & Garrod, D. (2012). Exploring the midwife's role in health promotion practice. British Journal of Midwifery, 20(3), 178–186. 10.12968/bjom.2012.20.3.178 [DOI] [Google Scholar]
- Ma, R. C. W. , Schmidt, M. I. , Tam, W. H. , McIntyre, H. D. , & Catalano, P. M. (2017). Clinical management of pregnancy in the obese mother: Before conception, during pregnancy, and post partum. The Lancet Diabetes & Endocrinology, 4(12), 1037–1049. 10.1016/S2213-8587(16)30278-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macleod, M. , Gregor, A. , Barnett, C. , Magee, E. , Thompson, J. , & Anderson, A. S. (2013). Provision of weight management advice for obese women during pregnancy: A survey of current practice and midwives' views on future approaches. Maternal & Child Nutrition, 9(4), 467–472. 10.1111/j.1740-8709.2011.00396.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCann, M. T. , Newson, L. , Burden, C. , Rooney, J. S. , Charnley, M. S. , & Abayomi, J. C. (2018). A qualitative study exploring midwives' perceptions and knowledge of maternal obesity: Reflecting on their experiences of providing healthy eating and weight management advice to pregnant women. Maternal & Child Nutrition, 14(2), e12520 10.1111/mcn.12520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Maternity Review (2016). BETTER BIRTHS Improving outcomes of maternity services in England. Retrieved from https://www.england.nhs.uk/mat-transformation/mat-review/
- NHS Health Education England (2018). Making every contact count. Retrieved from http://www.makingeverycontactcount.co.uk/
- NICE (2008). Maternal and child nutrition (NICE public health guidance 11). Retrieved from London: https://www.nice.org.uk/guidance/ph11/resources/maternal-and-child-nutrition-pdf-1996171502533
- NICE (2015). Quality statement 1: Healthy eating in pregnancy. Retrieved from London: https://www.nice.org.uk/guidance/qs98/chapter/Quality-statement-1-Healthy-eating-in-pregnancy
- Olander, E. K. , Darwin, Z. J. , Atkinson, L. , Smith, D. M. , & Gardner, B. (2015). Beyond the ‘teachable moment’—A conceptual analysis of women's perinatal behaviour change. Women and Birth, 29, e67–e71. 10.1016/j.wombi.2015.11.005 [DOI] [PubMed] [Google Scholar]
- Phelan, S. (2010). Pregnancy: A teachable moment for weight control and obesity prevention. American Journal of Obstetrics and Gynecology, 202(2), 135.e131–135.e138. 10.1016/j.ajog.2009.06.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poston, L. , Caleyachetty, R. , Cnattingius, S. , Corvalan, C. , Uauy, R. , Herring, S. , & Gillman, M. W. (2016). Preconceptional and maternal obesity: Epidemiology and health consequences. The Lancet Diabetes and Endocrinology, 4(12), 1025–1036. 10.1016/s2213-8587(16)30217-0 [DOI] [PubMed] [Google Scholar]
- Public Health England (2016). Making every contact count (MECC): Consensus statement. Retrieved from https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/515949/Making_Every_Contact_Count_Consensus_Statement.pdf
- SCA Group, Southampton Voluntary Services, & Solent NHS Trust (2018). Southampton healthy living. Retrieved from https://www.southamptonhealthyliving.org.uk/services/
- Southampton City Council (2015a). Public health summary report: The first 1000 days. Retrieved from Southampton http://www.publichealth.southampton.gov.uk/images/southampton-phar-2015-final-summary-report.pdf
- Southampton City Council (2015b). Southampton statistics. Retrieved from https://www.southampton.gov.uk/council-democracy/council-data/statistics/imd2015.aspx
- Statacorp (2013). Stata statistical software: Release 13 (Version 11). Texas: College Station.
- Swift, J. , & Tischler, V. (2010). Qualitative research in nutrition and dietetics: Getting started. Journal of Human Nutrition and Dietetics, 23(6), 559–566. [DOI] [PubMed] [Google Scholar]
- Swift, J. A. , & Tischler, V. (2013). Qualitative research in nutrition and dietetics: Getting started. Journal of Human Nutrition and Dietetics, 2010 Dec;23(6), 559–566. https://doi:10.1111/j.1365-277X.2010.01116.x [DOI] [PubMed] [Google Scholar]
- Thangaratinam, S. , Rogozinska, E. , Jolly, K. , Glinkowski, S. , Duda, W. , Borowiack, E. , … Khan, K. S. (2012). Interventions to reduce or prevent obesity in pregnant women: A systematic review. Health Technology Assessment, 16(31), 1–191. 10.3310/hta16310 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request. All data generated or analysed during this study are included in this published article (and its supplementary information files).


