Abstract
Smoke Sense is a citizen science project with investigative, educational, and action‐oriented objectives at the intersection of wildland fire smoke and public health. Participants engage with a smartphone application to explore current and forecast visualizations of air quality, learn about how to protect health from wildfire smoke, and record their smoke experiences, health symptoms, and behaviors taken to reduce their exposures to smoke. Through participation in the project, individuals engage in observing changes in their environment and recording changes in their health, thus facilitating progression on awareness of health effects of air pollution and adoption of desired health‐promoting behaviors. Participants can also view what others are reporting. Data from the pilot season (1 August 2017 to 7 January 2018; 5,598 downloads) suggest that there is a clear demand for personally relevant data during wildfire episodes motivated by recognition of environmental hazard and the personal concern for health. However, while participants shared clear perceptions of the environmental hazard and health risks in general, they did not consistently recognize their own personal health risk. The engagement in health protective behavior was driven in response to symptoms rather than as preventive courses of action. We also observed clear differences in the adoption likelihood of various health protective behaviors attributed to barriers and perceived benefits of these actions. As users experience a greater number and severity of symptoms, the perceived benefits of taking health protective actions exceeded the costs associated with the barriers and thus increased adoption of those actions. Based on pilot season data, we summarize key insights which may improve current health risk communications in nudging individuals toward health protective behavior; there is a need to increase personal awareness of risk and compelling evidence that health protective behaviors are beneficial.
Keywords: Citizen Science, Health Behavior, Wildfire Smoke, Smartphone App
Key Points
With Smoke Sense, citizen scientists become human sensors of their own behavior in relation to their environment
Smoke Sense reaches participants when and where they experience wildfire smoke
Increasing personal awareness of risk and providing compelling evidence of health benefit is needed
1. Introduction
Wildfire smoke, as one of the largest sources of unhealthy air quality, is an emerging health issue, associated with an estimated 340,000 excess deaths each year globally (Larsen et al., 2018; National Interagency Coordination Center, 2018). Exposures to particles and gasses found in wildfire smoke are linked to a range of health outcomes, including lower birth weight, increased rates of cardiorespiratory emergency visits, hospitalizations, and death (Dennekamp & Abramson, 2011; Dennekamp et al., 2015; Haikerwal et al., 2015; Haikerwal et al., 2015; Morgan et al., 2010; Reid et al., 2016; Wettstein et al., 2018). Some individuals are more susceptible to these clinical outcomes due to underlying health conditions, age, socioeconomic status, and other factors (Rappold et al., 2012; Reid et al., 2016). Even healthy individuals experience respiratory, ear‐nose‐throat symptoms, difficulty sleeping, viral infections, and other subclinical or precursor events that reduce productivity and can result in delayed but serious health outcomes (Integrated Science Assessment (ISA) for Particulate Matter, 2009; Krewski et al., 2005). Reducing the amount, duration, and intensity of smoke exposure by using an air filter and limiting outdoor activities is widely recommended as a health preventive action (Cascio, 2018; Wildfire Smoke: A Guide for Public Health Officials, 2016). To achieve better public health outcomes, we need to apply what we know about health risks and protective health behavior effectively.
Despite the increased attention on wildfires and smoke exposure, there remains significant uncertainty in how to reduce the public health burden of these events. Existing knowledge about health risk, preventative measures, and risk communication has not reduced the uncertainty in our understanding and practice of how to best respond to this emerging issue (Fisk & Chan, 2017; Laumbach, 2019; Sandoval & Krapfl, 2014). A public health perspective provides theoretical models that can inform strategies to address this knowledge gap. Health belief models and the theory of planned behavior suggest that understanding perceptions, motivations, and barriers to behavioral change (physical, social, or financial) among impacted individuals may shed light on the disconnect between observed health outcomes and what we know about ways to reduce risks (Ajzen, 1991; K. Glanz et al., 2015; Rosenstock et al., 1988). Understanding an individual's perception of who is at risk, the role of previous experiences with poor air quality; informational needs; feelings of efficacy for changing personal exposures given prevailing environmental conditions; and perceptions of benefit when an action is taken can help us characterize when, why, and how individuals change their routine behaviors to adopt health protective measures. This knowledge helps public health experts construct strategies that motivate behavioral change and result in improved outcomes. However, today, as we witness growth of large wildfires, there is virtually no research documenting how individuals respond to the smoke as a health risk or even how effectively recommended actions improve public health and productivity.
The estimated health burdens (Fann et al., 2018; Fay H. Johnston et al., 2012) indicate that there is a pressing need to achieve better public health outcomes related to smoke exposure. However, reducing the health burden is a complex problem with a multitude of possible solutions. Because of the clear demand for solutions, in the fall of 2017, U.S. Environmental Protection Agency (EPA) researchers devised a novel citizen science approach called the Smoke Sense initiative, which encourages participants to report changes in their health and changes in the environment, resulting in the participant finding personal relevance in the adoption of health protective behaviors. Drawing on elements from the theory of planned behavior and the health belief model (Driver, 1991; Karen Glanz et al., 2002; Rosenstock et al., 1988; Theory at a Glance ‐ A Guide For Health Promotion Practice, 2005), participation in the study encourages preventive health behaviors and invites users to record their smoke observations and health symptoms, play educational trivia games, and explore what other participants are reporting through a smartphone app. Various components of the app are intended to facilitate participants' progression in air quality awareness and adoption of desired health‐promoting behaviors by tapping into the desire to gain and display expertise via learning. Within the app, participants can explore current and forecasted daily air quality, maps of fire locations, and satellite images of smoke plumes and learn about health consequences of wildfire smoke.
The overarching objective of the Smoke Sense initiative is to develop and maintain an interactive platform for building knowledge in individuals through engagement with the issue and systematic knowledge through research about wildfire smoke, health, and protective actions to bridge existing gaps and improve public health outcomes. The platform envisions the creation of multiple points of entry to engage with the issue: individuals, the wider research community, and partner organizations. At the organizational level, the platform has the potential to supplement and complement partner organizations' efforts in addressing this issue by serving as a tool for engagement and discussion (e.g., state health agencies use the app as an entry point for conversations with stakeholders). Key benefits to the wider research community include access to individual‐level responses during smoke events and overcoming potential limitations of conventional research design methods (e.g., the possibility of recall bias or ecologic fallacy, difficulties in reaching affected populations and collecting of responses over time, etc.). In this paper we examine Smoke Sense pilot data for the feasibility to reach target audiences, engage participants on the topic of health impacts of smoke, and gain insights into factors that affect health protective behaviors. Specifically, we investigate the role of personal health, perceptions of risk, and experiencing symptoms in relation to adopting preventive health behaviors. In addressing these objectives, we develop a causal diagram tracing how health and exposure factors interrelate with protective actions; these relationships are then used to define future steps for exploring the impact of engagement and effectiveness of health protective behaviors.
2. Data and Methods
Citizen scientists could opt‐in to participate by downloading the EPA Smoke Sense app available on Android and iOS platforms. The app provided users with three key features designed to facilitate connections between wildfire smoke, health impacts, and ways to protect health: (1) record observations of smoke, symptoms, and actions, (2) view responses of other participants, and (3) receive information about air quality, current fires, existing and forecasted smoke plumes, and the health consequences of smoke exposure. The home screen displayed the current and next day's forecasted air quality with associated health messages, a brief tutorial about the Air Quality Index (Figure 1), and tabs leading to four major features of the app (“My Profile,” “Symptoms and Smoke Observations,” “Fire and Smoke Near me,” and “Air Quality 101”).
Figure 1.

Smoke Sense mobile app user interface.
During the pilot season, the Smoke Sense app was available on the Android platform from 1 August to 20 November 2017 and on the iOS platform from 5 October 2017 through 7 January 2018. During this time, the app was downloaded 5,598 times (40% Android) and launched over 50,000 times.
2.1. My Profile
Smoke Sense participants were prompted to establish a profile to begin using the app. They were asked to provide a zip code, demographic information (sex, age, race, and education level), baseline health information (preexisting conditions, physical activity level, and time spent outdoors), and current beliefs about smoke and air pollution (e.g., does smoke impact health?); however, only the zip code was required to continue using the app (see Table 1 in the Supplemental Material for the full list of questions).
2.2. Symptoms and Smoke Observations
In the “Symptoms and Smoke Observations” tab of the app, participants reported observations of smoke, health symptoms, and behaviors adopted to reduce smoke exposures and symptoms. Each week, considering Monday as the start of a week, the app captured responses in four symptom categories—eyes and ears, respiratory, cardiovascular, and/or other—as well as additional information indicating the severity of adverse health effects (i.e., duration of the symptoms, whether medication was used to treat their symptoms and whether an unplanned trip to a physician was made as a result). A list of all specific questions asked in the Smoke Sense app is provided in the Supplemental Materials, titled “Smoke Sense Reporting Pilot Instrument—2017” (Table S1).
2.3. Fire and Smoke Near Me
A “Fire and Smoke Near Me” tab provided the most recent air quality data measured at monitoring sites across the country using the data from the AirNow program (http://www.airnow.gov) and satellite‐detected fire smoke plumes from the National Oceanic and Atmospheric Administration (NOAA) Hazard Mapping System (HMS) Fire and Smoke product (Ruminski et al., 2007). The HMS provided the geospatial extent of smoke plumes as seen by visible bands of satellite imagery from seven NOAA and National Aeronautics and Space Administration environmental satellites each day.
2.4. Air Quality 101
An “Air Quality 101” module led to trivia games which tested knowledge of air quality facts and provided correct answers for each lesson. These trivia games were created by the EPA research team based on sections of the Wildfire Guide for Public Health Officials (2016). The purpose of the lessons was to summarize the Guide and prompt participants to engage with learning to identify health risks and ways to protect their health.
2.5. Additional Engagement and Education
To encourage continued engagement with the app, Smoke Sense included in‐app badges awarded for accomplishments within the app. These badges were intended to promote certain desired behaviors: completing a user profile, launching the app weekly to check local air quality, reporting smoke and symptom observations, expanding air quality knowledge with air quality lessons, and exploring the map. Participants could also view cumulative statistics of symptoms reported by all participants.
To support the user group and troubleshoot issues, the Smoke Sense team established a project‐level website and project‐level email (smokesense@epa.gov) during the pilot season. Activities related to communications and engagement also included giving a webinar, posting to Twitter and Facebook using the hashtag #SmokeSense, writing up print materials to give out at meetings and conferences, keeping the website updated with new information and FAQs about the app, and working with select communities that wanted to participate in promoting the app.
2.6. Analysis
In the analysis, we defined “users” as individuals who completed only the profile questionnaire (n = 3,061) and “participants” as individuals who also reported at least one instance in “Symptoms and Smoke Observations” (n = 1,897). Apart from providing a designated home area zip code, no survey questions required responses. This led to a dataset where the number of responses to each question varies. Users who did not participate were still able to access all functions of the app such as the Air Quality Index, Fire Near Me maps, and Air Quality 101 module. The return rate to the app among both users and participants exceeded 92%.
We examined Smoke Sense pilot data for the feasibility to reach individuals affected by smoke and to characterize motivations for participation. We examined basic demographics of users and participants based on their profile report, their perceptions of smoke as an environmental risk, their perceptions of smoke as a health risk, and the role of preexisting self‐reported health conditions on those perceptions. The unit of observation was the participant week in which participants reported their observations. The full reporting format and number of participants answering each question are given in the Supplemental Material Tables S1 and S2, respectively. We examined the likelihood of adopting exposure reduction behaviors (ERBs) and mitigating behavior in relation to the severity of symptoms using logistic regression models. Each ERB was examined individually. ERBs included wearing a dust mask, wearing a respirator, avoiding daily activities such as school, work, or church, using an air cleaner in the house, avoiding outdoor recreational activities, staying indoors, doing other activities, or not changing behavior. Symptom‐mitigating behaviors included using over‐the‐counter medication, prescription medication, unscheduled outpatient visits to a physician, and unscheduled inpatient visits. However, for analysis, we collapsed self‐reported healthcare usage, including medication and doctor visits, into two levels: “No Meds/No Doctor” and “Meds/Doctor.” Analysis was conducted using simple linear regression and logistic regression in the R statistical software package (R Core Team, 2014).
We used HMS smoke plumes for validation of participant‐reported observations of smoke. We compared participant‐reported smoke observations to NOAA HMS detections of smoke plumes at each ZIP code per participant week and the number of smoke days to participants' perceptions of how long they smelled smoke inside and outside the home. We did not use air quality values measured at the monitoring sites because they were not available for all participant‐reported ZIP codes.
To explore the representativeness of the participant sample to the underlying population, we compared participants' demographic information to the American Community Survey (ACS) 2012–2016 5‐yr estimates at the zip code level. ACS estimates were used to calculate the population‐weighted mean for the four demographic variables—age, gender, race, and education—across zip codes reported by any Smoke Sense user.
This study was reviewed by the Office of Human Research Ethics Institutional Review Board at the University of North Carolina, Chapel Hill. The study was exempted from further review under 45 CFR 46.101(b) Exemption Category 2. Participation in Smoke Sense was voluntary on an opt‐in basis. Participant's locations were not recorded using GPS, and phone identifiers were not collected. Each participant was given a unique identifier based on the app download instance.
3. Results
3.1. Smoke Sense Population Demographics
Smoke Sense participants and users were more representative of the mobile app user population than their community demographics. Participants of Smoke Sense during the pilot study were younger (30.2% age 18–29; 25% age 30–39; 19.3% age 40–49; 18.9% age 50–64; and 6.5% age 65+), more educated (71.6% had at least a college degree), and a higher proportion white (80.1%) and female (64.2%) than the reference population based on ACS (Supplemental Material Table 3).
3.2. Participants' Perceptions of Smoke Events
Smoke Sense participation was motivated by the experience of a significant smoke event, with 80% of downloads occurring during smoke events. Most participants and users were from Washington and California, states with particularly severe wildfire smoke events in the late 2017 fire season (Figure 2). Their perception of smoke exposure was consistent with occurrences of smoke plumes as measured by NOAA's HMS smoke plume product. Among participants, 80% of the reported smoke observations matched NOAA HMS smoke observations in the same zip code as a smoke event (2,180 out of 2,708 responses). Further, 51% (n = 2,680) of the reported smoke observations during which the user smelled smoke inside or outside the home also matched the duration/length of time of NOAA HMS smoke observations in the same zip code.
Figure 2.
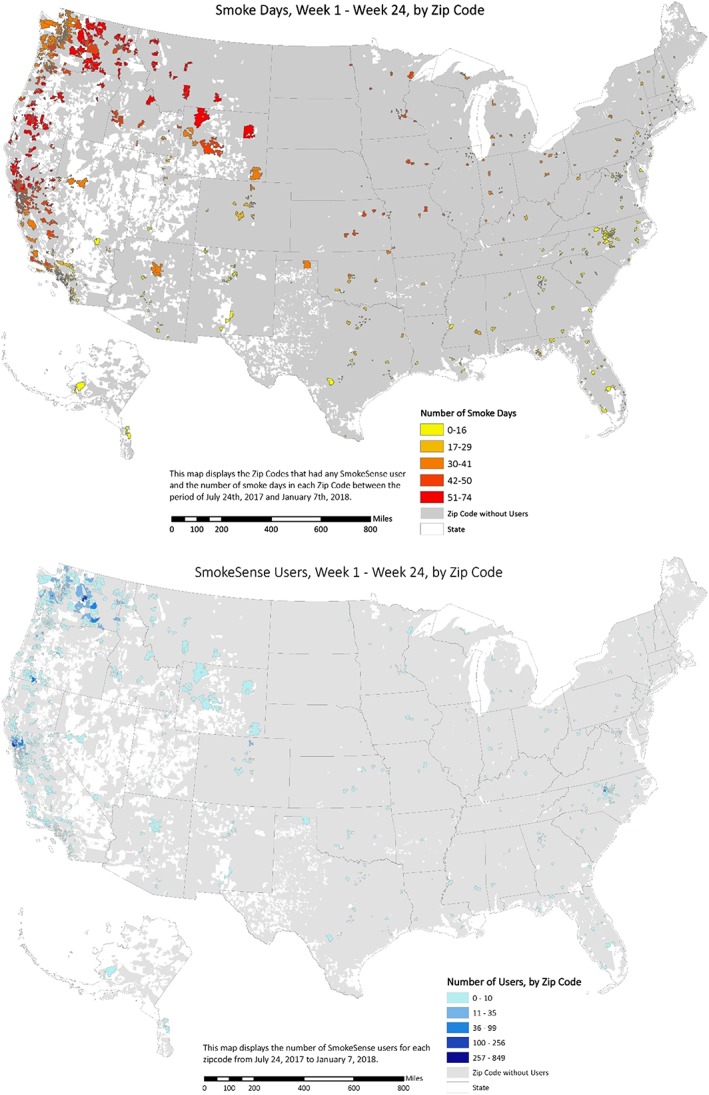
Spatial distribution of Smoke Sense users and participants and the number of days with satellite‐detected smoke plumes.
3.3. Personal Health, Risk Perception, and Engagement
Participation in Smoke Sense was motivated not only by the presence of smoke but also out of concern for personal health. Individuals with a previous or current health concern also had a higher interest in participation; 57% of users and 71% of participants had a previous diagnosis of a chronic health condition. Participants with current health concerns also stayed engaged longer; the longest participation was observed for those with self‐reported “respiratory” conditions and history of “allergies,” with an average of 2.74 and 2.41 weeks, respectively. By comparison, participants with no self‐reported health concerns engaged for the shortest average duration, 1.6 weeks. Except for chronic obstructive pulmonary disease (COPD) with low numbers, differences in the number of participation weeks between those with preexisting health concerns and those without were significantly different (Supplemental Material Table S4).
While participants reported a clear perception of smoke as a health risk and the participation was driven by health concern, on average, participants did not consistently recognize the risk to themselves. More specifically, while 91% (n = 1,482) recognized that smoke and air pollution affect the health of some individuals, only 72% thought that smoke and air pollution affect health in general. The percentage‐point difference was larger in participants who did not regularly experience symptoms (27%) and smaller in those who did (13 %).
3.4. Symptom Reporting Patterns
Participants were more likely to self‐report symptoms on days when they recorded smoke observations (Figure 3). When experiencing a smoke event, they reported, on average, 2.5 different symptoms per week. In contrast, when smoke was not reported, participants reported an average of 0.8 symptoms per week. The most commonly reported symptoms were “respiratory”‐related (smoke days 87%, nonsmoke days 38%) followed by “eyes and ears”‐related (smoke days 79%, nonsmoke days 26%) (Supplemental Material Table 5). Cardiovascular symptoms were the least common (smoke days 25%, nonsmoke days 8%), although the proportional magnitude of the increase was consistent with other conditions. However, because motivations for participation influenced the act of reporting, we do not generalize proportional increases in reported symptoms to population‐level risk measures of smoke exposures.
Figure 3.

Odds ratio of reporting symptoms between participants with and without previous history of health conditions on smoke days only. Likelihood of each symptom was examined individually. Point estimates and 95% confidence intervals are reported in Supplemental Material Table 6.
On days when participants reported smoke observations, those who reported having a previous history of chronic health conditions in the profile section of the app were more likely to report symptoms in comparison to those without a reported history of chronic conditions (Figure 3). Participants with diagnoses of COPD and respiratory illnesses reported particularly high rates of “cardiovascular” and “respiratory”‐related symptoms in comparison to those without any history of chronic conditions (respiratory diagnosis vs. none: “eyes and ears” symptoms OR 1.80(1.01,3.2); “respiratory” symptoms 5.60(2,15.65); “cardiovascular” symptoms 4.27(2.56,7.13); and “other” symptoms 4.92(2.64, 9.18)), which is consistent with known biological responses in this population. Surprisingly, participants with previous diagnoses of allergies, asthma, diabetes, or heart conditions were also more likely to report symptoms which were not specific to the previous diagnoses. Namely, those with asthma, in comparison to those without, were equally more likely to report “cardiovascular” (OR: 2.58(1.87, 3.57), “respiratory” (OR: 2.73(1.87, 3.98)), “eyes and ears” (OR: 1.59(1.19, 2.13)), or “other” conditions (OR: 2.12(1.62, 2.77)). Odds ratios for all outcomes are reported in Supplemental Table S6.
3.5. Exposure Reduction Behaviors (ERBs)
A clear majority of Smoke Sense participants (89%) responded to smoke by changing behavior. Most people reported taking multiple actions, while few people (<1%, −11 individuals) reported taking all eight ERBs (62% selected two or more ERBs, 31% selected a single ERB). When experiencing smoke, the likelihood of adopting ERBs increased with the number of symptoms but did not depend strongly on previously reported health history (Figure 4). The probability of “no exposure reduction” actions went down from 52% among participants without symptoms to 1% among the participants all with four symptoms. The actions most likely to be taken were “stayed indoors” and “avoided outdoor recreation,” while “dust mask” and “leaving the area” were the least likely.
Figure 4.
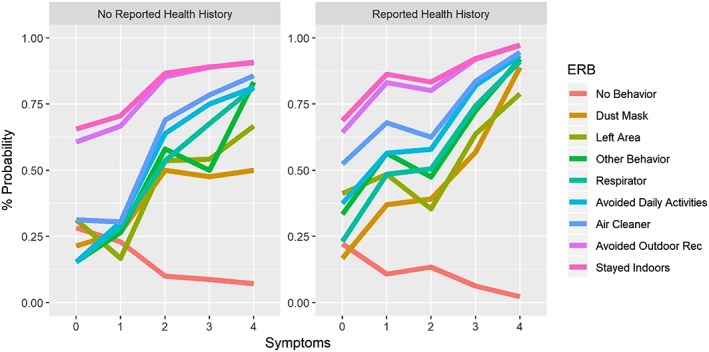
Probability of taking exposure reduction behavior (ERB) by number of symptoms per week among participants who have experienced smoke. The left panel references participants without preexisting health conditions, and the right panel references participants with preexisting conditions. Probabilities were estimated using logistic regression; odds ratios and 95% confidence intervals are reported in Supplemental Material 7.
3.6. Mitigating Actions: Medication and Doctor Visits
Participants who experienced symptoms also reported using medication, visiting a doctor for unscheduled visits, or both (56%), while only 2% of participants who did not experience symptoms took similar actions. Healthcare usage was also reported more often as the number of symptoms per week increased: 32% for one symptom, 52% for two, 67% for three, and 72% for four symptoms. As such, we refer to the usage of medication and unplanned doctor visits as an action to mitigate symptom severity, taken in response to symptoms with the purpose of reducing the severity of health burden.
3.7. Those Who Took Mitigating Action Were More Likely to Adopt ERBs Than Those Who Did Not
Among participants with a single symptom and who mitigated the severity of their symptoms, the likelihood of adopting any of ERBs exceeded 45%. In this group, the likelihood of adopting any ERB when experiencing all four symptoms was over 90%. For both groups, “avoided outdoor recreation” and “staying indoors” are the ERBs most likely to be adopted, regardless of the number of symptoms, indicating either low costs or high perceived benefits, or both. In the “Meds/Doctor” group, for most of the other ERB, the probability of adoption did not increase until three symptoms were experienced, suggesting relatively steep costs or larger uncertainties about the benefits of the ERB. For the “No Meds/No Doctor” group, there was a relatively sharp increase in the adoption of “air cleaner” and “avoided daily activities” with respect to the number of symptoms (severity), suggesting relatively lower costs or higher perceived benefits. As expected, as people experienced symptoms, the probability of doing nothing falls, with a greater decline for those mitigating symptoms. This suggests that those choosing to both mitigate symptoms and adopt ERB may be experiencing more severe symptoms and therefore see a greater perceived benefit from avoiding additional symptoms (Figure 5).
Figure 5.
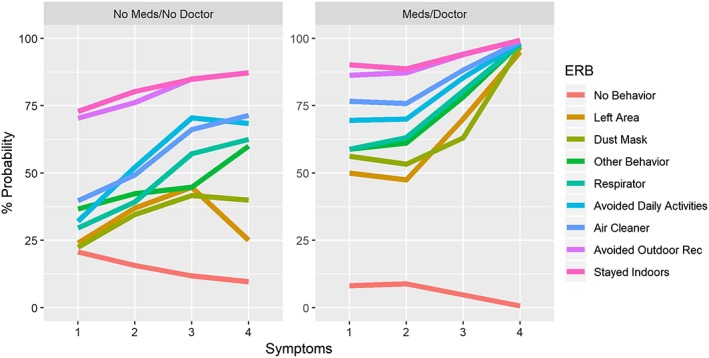
Probability of taking exposure reduction behavior (ERB) by number of symptoms per week and mitigating actions among the participants who have experienced smoke and at least one symptom. The left panel references participants who did not take medications or visit a doctor, and the right panel refers to participants who had at least one symptom and did take medication or visit a doctor. Probabilities were estimated using logistic regression.
4. Discussion
4.1. Pilot Season Findings on the Relationships Between Smoke Exposure, Health Protective Behaviors, and Personal Factors That Influence Them
We examined Smoke Sense citizen scientist reports for feasibility of reaching target audiences and ability to engage participants in protecting their health and and to learn how exposure‐reducing behaviors are adopted in response to wildfire smoke exposure. Participation and return rates indicated a clear demand for learning more about smoke impacts and health protective behaviors. Whereas most participants consistently identified smoke as an environmental hazard and a health risk in general, participants with preexisting health history were more likely to perceive their own health to be at risk; they engaged and reported symptoms more often. However, the range of symptoms reported by health‐motivated participants was not consistent with biological responses specific to personal health history. For example, participants with asthma were equally likely to report symptoms of eyes and ears as respiratory symptoms, indicating that the range of symptoms experienced by individuals goes beyond existing health concerns.
Simultaneously, the engagement in health protective behavior was not driven by the health factors that motivated participation. More specifically, 71% of participants and 57% of users had reported existing health concerns; participants with respiratory symptoms engaged for, on average, 2.74 weeks, while those without health conditions engaged for 1.62 weeks, and participants with self‐reported allergies were 3.23 times more likely to report symptoms. Additionally, participants who did not take exposure‐reducing actions had a lower number of symptom days (Figure S1), while those with more symptom days were more likely to take any of the actions (Figure 4), which suggested that the engagement in health protective behavior was driven in response to symptoms as reactive rather than preventive courses of action. We also observed variations in the likelihood of adopting ERBs reflecting social, physical, or financial burden or the amount of perceived benefit. Higher probabilities suggested that “staying indoors” and “avoiding outdoor recreation” are, on average, the easiest ways to modify daily routines or have the most certain perceived benefit in reducing smoke exposure. Conversely, “avoiding daily activities,” such as going to work or school, was the most difficult way to modify daily routine, but the perceived benefit increased rapidly with the increase in number of symptoms. A higher average number of symptoms among participants who actively mitigated their symptoms provided suggestive evidence that as symptoms increased, participants tried to treat those symptoms with medication and doctor visits. Finally, when examining engagement in exposure‐reducing behavior, we observed a higher likelihood among those who also mitigated the severity of their symptoms by seeking healthcare. While we were unable to directly identify the impact of specific barriers to adoption or perceived benefits of adoption, there are clear differences in the likelihood of adoption between ERB, which suggests that there are differences in barriers and benefits. However, these differences become less relevant as more symptoms are experienced, especially for those reporting use of medications or doctors, which is likely an indication of the greater severity of their symptoms. Pilot year observations about exposure‐reducing behavior motivated a subsequent change in the reporting survey where we can explore and identify barriers to each of the actions.
We summarize our findings in a causal diagram describing the relationship between smoke exposure, health history, health symptoms, exposure‐reduction behaviors, and outcome‐mitigating behaviors (Supplemental Material Figure S2a). The diagram defines current behavior as being reactive to symptoms (S ‐‐ > ERB) and mediated through mitigating actions taken to reduce exposure (S ‐‐ > MB ‐‐ > ERB). The diagram also describes the lack of relationship between personal health history and adoption of exposure reduction behavior. The desired causal diagram is depicted in panel b with a directed link between ERBs and symptoms, where ERBs are taken preventatively to reduce symptoms and possibly eliminate the severity of outcomes (Supplemental Material Figure S2b). The diagram summarizes relationships between smoke exposure, health protective behaviors, and personal factors that influence these relationships and enable us to identify future directions.
4.2. Insights on Health Risk Messaging in the Context of Protective Health Behavior During Smoke Episodes
Participant reports during the pilot season led us to form two main insights about approaches that may improve health risk communications designed to nudge individuals toward health protective behavior. These two insights emphasize that health risk messaging should be personally relevant and health risk messages should reinforce the benefit of protective health behavior. Health and risk messages that recognize informational needs, beliefs, motivations, and health behaviors of users have been shown to increase perceived relevance and increase the likelihood of behavioral change in other health domains (Lustria, 2017). These previous experiences support the hypothesis that realizing the key insights may increase the individual level of responsiveness in the context of changing behavior during wildfire smoke exposure.
The first insight refers to increasing personal awareness of health risk as a way of increasing health protective behaviors in comparison to the current focus of delivering information on air quality. Furthermore, our hypothesis suggests that the effectiveness of health risk messages is likely to increase if the messages can reduce the gap between “self” and “others” in assessment of personal risks, thus reducing the “better than average affect” (e.g., people thinking that they are generally healthy and therefore at a lower risk from smoke exposure compared to the average person) (Brown, 2011). Highlighting a broader range of potential risks, such as irritation of eyes or loss of good sleep, which may be easier to identify as a personal risk and may act as a cue to action for a wider population, could thus reduce the chance of more severe outcomes across the board. Of course, this suggestion does not negate the need to communicate the risk of severe outcomes such as asthma attack, pneumonia, or myocardial infarction. While these are very serious and valid health concerns, they are poor cues to actions at the population level. Most individuals do not realistically expect to be personally affected by a severe outcome, but a great many do perceive the risk of lower level symptoms that impact our wellness, such as the immediate value in reducing the risk of a poor night of sleep.
The second key insight is that lack of awareness of health benefits related to behavioral changes and high perceived barriers can be significant deterrents to adoption of ERB. The pilot season data provided important insights into motivations (perceived benefits) and barriers to adopting exposure‐reducing behaviors. The likelihood of adopting ERBs increased with the severity of health impacts. The differences in the rates of adoption of ERB and the response to the number of symptoms experienced suggest that there are differences in perceived costs (barriers), perceived benefits, or both. The combination of low awareness of personal risk or perceived benefits coupled with perceived barriers resulted in participants acting in response to experienced symptoms, rather than preventively. Therefore, to overcome those barriers, individuals need to perceive that the benefits of the action exceed these costs. Because these perceptions may be determined at least partially by potentially modifiable factors such as costs, convenience, and perception of efficacy, clear evidence and compelling messaging that behavioral changes are effective and provide benefit are needed.
Behavioral changes in individuals have been the key to achieving many public health objectives, particularly in the cases where new behaviors can be introduced as habitual and backed up by social evidence (smoking cessation, washing hands, and flu shots). The challenge in moving the needle with respect to individual‐level behavior during wildfire periods is at least partially explained by the transient and episodic nature of these events. Under urgent response circumstances, messaging related to health risks and protective behaviors challenges individual and organizational bandwidth in delivering, receiving, processing, or acting upon new information, even when the consequences are real and substantial. In the absence of clear message content, behavioral tendencies and prescriptions lead us to ignore or downplay common risks while fearing highly unlikely events (Tversky & Kahneman, 1973).
Cognitive biases and behavioral tendencies are important to keep in mind in the public health domain of this emerging issue. Numerous examples in the literature related to decisions about health‐related behavior involving diet, exercise, and finances have demonstrated the allure of inaction in the short term. Several factors are potentially at play: (1) the perceived impact of actions; a single instance of behavior change may be considered a “drop in the bucket” compared to estimates of the magnitude of change needed, (2) the perceived costs of actions; these may be financial, time‐based, or psychological, including loss of enjoyment or the perceived effort involved in implementing a change, and (3) the temporal disconnect between behavior and outcomes; a “good” behavior might provide benefits days, weeks, months, or years in the future, in contrast to the immediate costs and perceived immediate benefits of “bad” behavior. Behaviors that are not part of a routine will have perceived and real costs that must be weighed against potential benefits. When benefits of behavior change are uncertain or unknown, a common human tendency is to continue default behavioral patterns (status quo bias; Kahneman et al. (1991); Samuelson and Zeckhauser (1988). Even when benefits are clear, changing a behavior may be perceived as a loss or removal of the familiar. Our human tendency to discount future gains compared to more immediate gains likely also works against the motivation to action as opposed to inaction (delay discounting, intertemporal choice; Loewenstein and Prelec (1992)).
4.3. Smoke Sense as an Innovative Study
The issue of wildfire smoke and health is a complex problem that challenges us to expand our approaches to understanding and identifying effective strategies that can improve public health outcomes. Environmental epidemiology has delivered evidence of health impacts when individuals are exposed to wildfire smoke. This evidence is important for scientific consensus and knowledge advancement, which over time becomes formulated in public health communications strategies. Citizen science research designs complement the current landscape by providing more avenues through which research can be carried out, tapping into the potential for collecting data using a distributed network of observers.
To our knowledge, Smoke Sense represents the first set of large‐scale observational data sets on individual behavioral responses to smoke exposure. The study also represents a leap forward in when, where, and how information about health impacts from environmental changes can be collected and understood. Here, we highlight two innovative concepts this study brings:
4.3.1. Citizen Scientists Become Human Sensors of Their Own Behavior in Relation to Their Environment
The first key innovation in Smoke Sense is that citizen scientists become human sensors of their own behavior in relation to their environment. They do this by recording health symptoms and smoke observations and reporting their behavioral responses and perceptions of smoke as an environmental hazard and health risk. Earlier efforts have focused on citizen‐collected environmental data, such as through electronic air quality sensors, but have not linked changes in environmental conditions to changes in personal health and behavior. Smoke Sense provides a unique ability to measure a participant's initial understanding of health risks and behaviors and how these evolve as they learn about smoke, air quality, and health. These knowledge gains not only benefit individual citizen scientists but also expand collective knowledge that can inform community health protection strategies during wildfires. Over time, this research effort can elucidate behavioral mechanisms, such as implementation intentions (Milkman et al., 2011), that provide opportunities for interventions which help individuals link goal intentions directly to behaviors.
4.3.2. Enabling Rapid Data Collection in Emerging Disasters With Continuous User Interaction Over Time
The second key innovation is the ability to gain and share systematic knowledge acquired when and where participants are afflicted by smoke. Designing and executing epidemiological or health and behavior survey studies in the context of emerging disasters is costly and highly challenging. Various institutional and structural barriers surrounding such research efforts can limit when and where data is collected, subsequently affecting its applicability and usage (e.g., research planning, approval processes, funding acquisition, data collection logistics, etc.). These barriers are especially challenging when data needs to be collected during an unplanned event, which can occur in any location and population. Smoke Sense embraces principles of citizen science and crowd sourcing where users can opt‐in to engage. As such, this research effort is less constrained by factors common to sample driven research such as prior sample identification, gathering contact information, sending invitations, etc. Further, participants can respond immediately and over multiple fire seasons indefinitely, likely minimizing recall bias and allowing the research team to track perspectives and behaviors across smoke events over time without having to redeploy an entire survey, as in traditional methods. As a smartphone app, Smoke Sense is also a platform to continuously reconnect with users, sharing results that may influence attitudes, normative beliefs, and perceived control over smoke exposures.
4.4. Advances Using Citizen Science and Smartphone Approaches
Like community‐engaged research projects, citizen science studies can be formulated to address community needs which can enable communities to solve problems over time. These studies bring together individuals in communities with environmental public health issues to make observations and clarify regional perspectives. With the gathered information, health authorities, working with “Culture Brokers” ((U.S. FEMA), 2019), can give risk and health promotion messages best suited for the structure of social and political dynamics in existing regional networks (Smell Pittsburgh, 2018; The University of Texas Medical Branch at Galveston, 2018). In epidemiology, citizen science approaches have been used to enable the public to actively participate in health surveillance (Deepwater Horizon spill, Sullivan et al. (2018)) or in observing environmental changes. In Tasmania, researchers developed an AirRater app that integrates symptom surveillance, environmental monitoring, and notifications of environmental conditions such as wildfire smoke and pollen (F. H. Johnston et al., 2018). While similar to Smoke Sense in its common aim of reducing health impacts, AirRater does not focus on behavioral responses and education but has also been widely used in response to environmental conditions.
Smartphones have changed the way we consume and respond to information. Mobile devices offer multiple ways to communicate (call, text, messaging, social media, etc.) and enable a continuous stream of information (from online news, interoperable schedules, etc.), thus changing the way we think and behave. New citizen scientists and crowdsourcing research efforts have successfully capitalized on the power of smartphones to engage users when the information is most relevant. Katapally et al. (2018) reported on a recent study using a mobile app to collect information on physical activity, physical and social context, and motivation and tested information interventions to increase active living behaviors. Chrisinger and King (2018) engaged citizen scientists to report objective and perceived elements of the built environment that contribute to chronic stress. Rosas et al. (2016) engaged citizen scientists in Mexico to collect and gather data about barriers and facilitators of physical activity in participants' neighborhoods and facilitate the use of data to collectively advocate for local environmental‐ and policy‐level changes to support active living. Another surveillance tool facilitated through crowdsourcing is Flu Near You, which enables prediction of the onset of flu season (Smolinski et al., 2015).
As a smartphone app, Smoke Sense provides several advantages over traditional research. The smartphone platform provides an avenue to enhance social normative learning and to evaluate the impact of risk and behavior messages to those who are affected by smoke. The application provides a platform for testing different behavioral mechanisms such as implementation intentions, which help people translate goal intentions into behaviors. Participants may benefit from just‐in‐time, scheduled, and self‐triggered reminders to consider relevant ERB that they can take to reduce health risks from smoke episodes (Pirolli, 2016; Pirolli et al., 2017). Smartphone applications have been shown to influence human behavior. With the BreezoMeter app (Polak, 2019) which provides information on the air quality and sends notifications when the pollution level rises above a certain level, researchers have examined factors that influence decisions to change behavior. In AIR Louisville projects, researchers showed that the use of electronic inhaler sensors on the smartphone to monitor where and when they used medication had positive clinical outcomes and influenced environmental policy in the community (Barrett et al., 2018). Tools that promptly communicate the health risks from and promote education and engagement with smoke exposure may help people make informed decisions to protect their health. Most importantly, the app is available for reporting observations when participants are affected by smoke episodes. In most places in the United States, threats from wildfire smoke bear more similarity to natural disasters or disease outbreaks that are transient or seasonal events. The precise geographic location and spatial extent of wildfires are emergent threats, meaning unique groups of people and different communities or regions are affected in any given year. The ability to understand how individuals respond in different geographic areas and over time can provide meaningful insights and value to public health officials.
Notwithstanding the novelty, Smoke Sense and app‐based participation is not without its limits. To make participation feasible at the national level, Smoke Sense is dependent on several external resources (air quality monitors, AirNow, fire incidence reporting, satellite data, health messaging, etc.) which all must work in tandem to have an effective user interface. By far, the most commonly reported issue that we received was related to the lack of air quality monitors. This is because permanent stationary air quality monitors are established for regulatory purposes and are positioned around large population centers. However, individual‐level needs for information, especially during wildfire smoke events, exceed the capacity of the regulatory network. As reflected by demographics of Smoke Sense participants, smartphone applications may be more attractive and accessible to some segments of the population and less to others. To increase the overall participation and in response to our community's needs, Smoke Sense is now available in Spanish, and a K–12 curriculum and a public facing data visualization site are being developed. The Smoke Sense research and communications team is also actively reaching out to state and organizational leaders in developing strategies to reach wider audiences; however, even with this effort, not all segments of the population will find a smartphone app appealing or feasible.
Another limitation of the study is that Smoke Sense participation is completely anonymous, and individual's personal exposure levels at more granular spatial scales are not known. For this purpose, we are exploring ways for delivering new metrics of exposure based on personal sensors, special purpose sensors, and satellite data. In the pilot season, Smoke Sense was conceived to facilitate within person changes in behavior, where enrollment in the study would occur randomly in time. However, after the massive fire season in 2017, participation was largely driven by smoke episodes which limited the ability to characterize health and behavior effects only due to smoke episodes. Namely, voluntary opt‐in participation gives rise to selection bias which will require development of new statistical methods to compare effects between smoke and nonsmoke periods.
5. Conclusions
Smoke Sense is an innovative citizen science effort that makes a personal connection between changes in environmental conditions and changes in personal health to promote protective health behavior. Smoke Sense uses educational tools, real‐time information, and gamification to promote issue engagement among participants. To our knowledge, the study represents the first set of large‐scale observational data on individual behavioral responses to smoke exposure largely unavailable from other sources.
Based on participant reports during the pilot season, we concluded that there is a clear demand for personally relevant data during wildfire episodes. Participation and symptom‐reporting actions were clearly related to personal characteristics such as health history; however, health protective behavior and reported symptom types were not consistent with personal risk factors. This observation leads us to two recommendations that may make health risk messages more effective: they should be personally relevant and provide compelling evidence that behavioral change is effective. These observations are being further explored in the current version of Smoke Sense which is being implemented during the 2019 wildfire season. The long‐term goal for Smoke Sense as a citizen science platform is to allow continuous engagement with participants which over time has the potential to shape their attitudes and sense of efficacy regarding control over smoke exposures.
Conflict of Interest
The authors declare no conflicts of interest relevant to this study.
Supporting information
Supporting Information S1
Acknowledgments
The authors declare no conflicts of interest. The authors would like to thank many valuable colleagues who believed in the project and helped make it happen. Special thanks to EPA's Office of Research and Development communications team including Ann Brown, Monica Linnenbrink, Melissa Anley‐Mills, and Haley Trapp; EPA Office of Mission Support Scott Philbrick, Andrew Yuen, and Michelle Ibarra; app and database developers Kevin Ting, Angela L. Ekstrand, Anthony Cavallaro, Tim Blakey, Alan Healy, Tom Transue, and Matt Freeman; EPA's Office of Air and Radiation Susan Stone, Phil Dickerson, and John E. White; and NOAA National Weather Service. The authors also thank the American Lung Association for their interest in wildfire smoke research and especially for providing support to Sequoia Foundation for an intern, Xing Gao. The authors would like to thank Dr. Dan Ariely and Dr. Jamie Foehl at the Center for Advanced Hindsight at Duke University for the opportunity to engage and discuss principles of behavioral science research in the context of air quality. Data Availability Statement Data and meta data for this study can be accessed at the website of Environmental Protection Agency (https://edg.epa.gov/metadata/catalog/search/resource/details.page?uuid=https://doi.org/10.23719/1503824). Disclaimer Although this work has been reviewed for publication by the U.S. Environmental Protection Agency and California Department of Public Health, it does not necessarily reflect the views and policies of these agencies.
Rappold, A. G. , Hano, M. C. , Prince, S. , Wei, L. , Huang, S. M. , Baghdikian, C. , et al. (2019). Smoke Sense Initiative Leverages Citizen Science to Address the Growing Wildfire‐Related Public Health Problem. GeoHealth, 3, 443–457. 10.1029/2019GH000199
References
- U. S. FEMA (2019). Building cultures of preparedness: A report for the emergency management higher education community. Retrieved from Washington, DC:
- Ajzen, I. (1991). The theory of planned behavior. Organizational Behavior and Human Decision Processes, 50(2), 179–211. 10.1016/0749-5978(91)90020-T [DOI] [Google Scholar]
- Barrett, M. , Combs, V. , Su, J. G. , Henderson, K. , Tuffli, M. , Collaborative, A. I. R. L. , & Collaborative, A. I. R. L. (2018). AIR Louisville: Addressing asthma with technology, crowdsourcing, cross‐sector collaboration, and policy. Health Aff (Millwood), 37(4), 525–534. 10.1377/hlthaff.2017.1315 [DOI] [PubMed] [Google Scholar]
- Brown, J. D. (2011). Understanding the better than average effect: Motives (still) matter. Personality and Social Psychology Bulletin, 38(2), 209–219. 10.1177/0146167211432763 [DOI] [PubMed] [Google Scholar]
- Cascio, W. E. (2018). Wildland fire smoke and human health. Sci Total Environ, 624, 586–595. 10.1016/j.scitotenv.2017.12.086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chrisinger, B. W. , & King, A. C. (2018). Stress experiences in neighborhood and social environments (SENSE): A pilot study to integrate the quantified self with citizen science to improve the built environment and health. International Journal of Health Geographics, 17(1), 17 10.1186/s12942-018-0140-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennekamp, M. , & Abramson, M. J. (2011). The effects of bushfire smoke on respiratory health. Respirology, 16(2), 198–209. 10.1111/j.1440-1843.2010.01868.x [DOI] [PubMed] [Google Scholar]
- Dennekamp, M. , Straney, L. D. , Erbas, B. , Abramson, M. J. , Keywood, M. , Smith, K. , et al. (2015). Forest fire smoke exposures and out‐of‐hospital cardiac arrests in Melbourne, Australia: A case‐crossover study. Environmental Health Perspectives, 123(10), 959–964. 10.1289/ehp.1408436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Driver, B. L. (1991). Prediction of leisure participation from behavioral, normative, and control beliefs: An application of the theory of planned behavior AU ‐ Ajzen, Icek. Leisure Sciences, 13(3), 185–204. 10.1080/01490409109513137 [DOI] [Google Scholar]
- Fann, N. , Alman, B. , Broome, R. A. , Morgan, G. G. , Johnston, F. H. , Pouliot, G. , & Rappold, A. G. (2018). The health impacts and economic value of wildland fire episodes in the U.S.: 2008–2012. Sci Total Environ, 610‐611, 802–809. 10.1016/j.scitotenv.2017.08.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisk, W. J. , & Chan, W. R. (2017). Health benefits and costs of filtration interventions that reduce indoor exposure to PM2.5 during wildfires. Indoor Air, 27(1), 191–204. 10.1111/ina.12285 [DOI] [PubMed] [Google Scholar]
- Glanz, K. , Rimer, B. K. , & Lewis, F. M. (2002). Health behavior and health education: Theory, research, and practice (3rd Edition ed.). Jossey‐Bass.
- Glanz, K. , Rimer, B. K. , & Viswanath, K. (2015). Health behavior: Theory, research, and practice. Wiley.
- Haikerwal, A. , Akram, M. , Del Monaco, A. , Smith, K. , Sim, M. R. , Meyer, M. , Tonkin, A. M. , Abramson, M. J. , & Dennekamp, M. (2015). Impact of fine particulate matter (PM2.5) exposure during wildfires on cardiovascular health outcomes. Journal of the American Heart Association, 4(7). 10.1161/jaha.114.001653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haikerwal, A. , Reisen, F. , Sim, M. R. , Abramson, M. J. , Meyer, C. P. , Johnston, F. H. , & Dennekamp, M. (2015). Impact of smoke from prescribed burning: Is it a public health concern? Journal of the Air & Waste Management Association (1995), 65(5), 592–598. 10.1080/10962247.2015.1032445 [DOI] [PubMed] [Google Scholar]
- Integrated Science Assessment (ISA) for Particulate Matter . (2009). Washington, DC.
- Johnston, F. H. , Henderson, S. B. , Chen, Y. , Randerson, J. T. , Marlier, M. , Defries, R. S. , Kinney, P. , Bowman, D. M. , & Brauer, M. (2012). Estimated global mortality attributable to smoke from landscape fires. Environmental Health Perspectives, 120(5), 695–701. 10.1289/ehp.1104422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston, F. H. , Wheeler, A. J. , Williamson, G. J. , Campbell, S. L. , Jones, P. J. , Koolhof, I. S. , Lucani, C. , Cooling, N. B. , & Bowman, D. M. J. S. (2018). Using smartphone technology to reduce health impacts from atmospheric environmental hazards. Environmental Research Letters, 13(4), 044019 10.1088/1748-9326/aab1e6 [DOI] [Google Scholar]
- Kahneman, D. , Knetsch, J. L. , & Thaler, R. H. (1991). Anomalies: The endowment effect, loss aversion, and status quo bias. Journal of Economic Perspectives, 5(1), 193–206. 10.1257/jep.5.1.193 [DOI] [Google Scholar]
- Katapally, T. R. , Bhawra, J. , Leatherdale, S. T. , Ferguson, L. , Longo, J. , Rainham, D. , Larouche, R. , & Osgood, N. (2018). The SMART study, a mobile health and citizen science methodological platform for active living surveillance, integrated knowledge translation, and policy interventions: Longitudinal study. JMIR Public Health and Surveillance, 4(1), e31 10.2196/publichealth.8953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krewski, D. , Burnett, R. , Jerrett, M. , Pope, C. A. , Rainham, D. , Calle, E. , Thurston, G. , & Thun, M. (2005). Mortality and long‐term exposure to ambient air pollution: Ongoing analyses based on the American Cancer Society cohort. Journal of Toxicology and Environmental Health. Part A, 68(13‐14), 1093–1109. 10.1080/15287390590935941 [DOI] [PubMed] [Google Scholar]
- Larsen, A. E. , Reich, B. J. , Ruminski, M. , & Rappold, A. G. (2018). Impacts of fire smoke plumes on regional air quality, 2006–2013. Journal of Exposure Science & Environmental Epidemiology, 28(4), 319–327. 10.1038/s41370-017-0013-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laumbach, R. J. (2019). Clearing the air on personal interventions to reduce exposure to wildfire smoke. Annals of the American Thoracic Society, 16(7), 815–818. 10.1513/AnnalsATS.201812-894PS [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loewenstein, G. , & Prelec, D. (1992). Anomalies in intertemporal choice: Evidence and an interpretation. The Quarterly Journal of Economics, 107(2), 573–597. 10.2307/2118482 [DOI] [Google Scholar]
- Lustria, M. (2017, July 27). Message tailoring in health and risk messaging. Oxford Research Encyclopedia of Communication. Retrieved 4 Oct. 2019, from https://oxfordre.com/communication/view/10.1093/acrefore/9780190228613.001.0001/acrefore-9780190228613-e-323
- Milkman, K. L. , Beshears, J. , Choi, J. J. , Laibson, D. , & Madrian, B. C. (2011). Using implementation intentions prompts to enhance influenza vaccination rates. Proceedings of the National Academy of Sciences, 108(26), 10415 10.1073/pnas.1103170108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan, G. , Sheppeard, V. , Khalaj, B. , Ayyar, A. , Lincoln, D. , Jalaludin, B. , Beard, J. , Corbett, S. , & Lumley, T. (2010). Effects of bushfire smoke on daily mortality and hospital admissions in Sydney, Australia. Epidemiology, 21(1), 47–55. 10.1097/EDE.0b013e3181c15d5a [DOI] [PubMed] [Google Scholar]
- National Interagency Coordination Center . (2018). Total wildland fires and acres (1926–2017). Retrieved from https://www.nifc.gov/fireInfo/fireInfo_stats_totalFires.html
- Pirolli, P. (2016). A computational cognitive model of self‐efficacy and daily adherence in mHealth. Translational Behavioral Medicine, 6(4), 496–508. 10.1007/s13142-016-0391-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pirolli, P. , Mohan, S. , Venkatakrishnan, A. , Nelson, L. , Silva, M. , & Springer, A. (2017). Implementation intention and reminder effects on behavior change in a mobile health system: A predictive cognitive model. Journal of Medical Internet Research, 19(11), e397 10.2196/jmir.8217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polak, S. (2019). According to a new study, BreezoMeter's data can change people's behavior.
- R Core Team . (2014). R: A language and environment for statistical computing. Retrieved from http://www.R-project.org/
- Rappold, A. G. , Cascio, W. E. , Kilaru, V. J. , Stone, S. L. , Neas, L. M. , Devlin, R. B. , & Diaz‐Sanchez, D. (2012). Cardio‐respiratory outcomes associated with exposure to wildfire smoke are modified by measures of community health. Environmental Health, 11, 71 10.1186/1476-069X-11-71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reid, C. E. , Jerrett, M. , Tager, I. B. , Petersen, M. L. , Mann, J. K. , & Balmes, J. R. (2016). Differential respiratory health effects from the 2008 northern California wildfires: A spatiotemporal approach. Environmental Research, 150, 227–235. 10.1016/j.envres.2016.06.012 [DOI] [PubMed] [Google Scholar]
- Rosas, L. G. , Salvo, D. , Winter, S. J. , Cortes, D. , Rivera, J. , Rodriguez, N. M. , & King, A. C. (2016). Harnessing technology and citizen science to support neighborhoods that promote active living in Mexico. Journal of Urban Health, 93(6), 953–973. 10.1007/s11524-016-0081-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenstock, I. M. , Strecher, V. J. , & Becker, M. H. (1988). Social learning theory and the health belief model. Health Education Quarterly, 15(2), 175–183. [DOI] [PubMed] [Google Scholar]
- Ruminski, M. , Kondragunta, S. , Draxler, R. , & Rolph, G. (2007). Use of environmental satellite imagery for smoke depiction and transport model initialization.
- Samuelson, W. , & Zeckhauser, R. (1988). Status quo bias in decision making. Journal of Risk and Uncertainty, 1(1), 7–59. 10.1007/BF00055564 [DOI] [Google Scholar]
- Sandoval, D. , & Krapfl, H. (2014). Using Evaluation to Improve a Risk Communication Campaign about the Health Impacts from Wildfire Smoke (87504642).
- Smell Pittsburgh . (2018). Smell Pittsburgh. Retrieved from https://smellpgh.org
- Smolinski, M. S. , Crawley, A. W. , Baltrusaitis, K. , Chunara, R. , Olsen, J. M. , Wójcik, O. , Santillana, M. , Nguyen, A. , & Brownstein, J. S. (2015). Flu Near You: Crowdsourced symptom reporting spanning 2 influenza seasons. American Journal of Public Health, 105(10), 2124–2130. 10.2105/AJPH.2015.302696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan, J. , Croisant, S. , Howarth, M. , Rowe, G. T. , Fernando, H. , Phillips‐Savoy, A. , Jackson, D. , Prochaska, J. , Ansari, G. A. , Penning, T. M. , & Elferink, C. (2018). Building and maintaining a citizen science network with fishermen and fishing communities post deepwater horizon oil disaster using a CBPR approach. New Solutions, 28(3), 416–447. 10.1177/1048291118795156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- The University of Texas Medical Branch at Galveston . (2018). Gulf coast health alliance: Health risks related to the Macondo spill (GC‐HARMS). Retrieved from https://www.utmb.edu/GCHARMS
- Theory at a Glance ‐ A Guide For Health Promotion Practice . (2005).
- Tversky, A. , & Kahneman, D. (1973). Availability: A heuristic for judging frequency and probability. Cognitive Psychology, 5(2), 207–232. 10.1016/0010-0285(73)90033-9 [DOI] [Google Scholar]
- Wettstein, Z. S. , Hoshiko, S. , Fahimi, J. , Harrison, R. J. , Cascio, W. E. , & Rappold, A. G. (2018). Cardiovascular and cerebrovascular emergency department visits associated with wildfire smoke exposure in California in 2015. Journal of the American Heart Association, 7(8). 10.1161/jaha.117.007492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wildfire Smoke: A Guide for Public Health Officials . (2016).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting Information S1


