Abstract
To evaluate the mechanism underlying the communication between myeloid malignant and bone marrow (BM) microenvironment cells in disease progression, the current study established BM mesenchymal stromal cells (MSCs) and assessed extracellular vesicle (EV) microRNA (miR) expression in 22 patients with myelodysplastic syndrome (MDS) and 7 patients with acute myeloid leukemia and myelodysplasia-related changes (AML/MRC). Patients with MDS were separated into two categories based on the revised International Prognostic Scoring System (IPSS-R), and EV-miR expression in BM-MSCs was evaluated using a TaqMan low-density array. The selected miRs were evaluated using reverse transcription-quantitative PCR. The current study demonstrated that the expression of BM-MSC-derived EV-miR was heterogenous and based on MDS severity, the expression of EV-miR-101 was lower in high-risk group and patients with AML/MRC compared with the control and low-risk groups. This reversibly correlated with BM blast percentage, with which the cellular miR-101 from BM-MSCs or serum EV-miR-101 expression exhibited no association. Database analyses indicated that miR-101 negatively regulated cell proliferation and epigenetic gene expression. The downregulation of BM-MSC-derived EV-miR-101 may be associated with cell-to-cell communication and may accelerate the malignant process in MDS cells.
Keywords: myelodysplastic syndrome, bone marrow mesenchymal stroma cells, extracellular vesicle, microRNA-101, disease progression
Introduction
The hematopoietic microenvironment comprises a mixture of bone marrow mesenchymal stromal cells (BM-MSCs), fibroblasts, vascular endothelial cells, etc. BM-MSCs support the proliferation and differentiation of hematopoietic stem cells, and themselves undergo differentiation into various functional cells, including adipocytes, osteocytes, and cells from the chondrogenic lineage (1,2). Studies on hematologic malignancies have demonstrated genetic abnormalities in neoplastic cells; however, the role of the hematopoietic microenvironment in the pathogenesis of human myeloid neoplasia is still unclear, therefore we attempted to assess BM-MSCs. Considering the anatomical architecture, BM-MSCs are components of the hematopoietic niche, and hematopoietic cells lie in close proximity to the bone endosteal surface, which is in direct contact with endothelial cells (1) and hence linked to drug sensitivity (3). BM-MSCs also act as immunosuppressive agents by inhibiting the proliferation of immune cells (4,5). Therefore, BM-MSCs may have an important effect on adjacent hematopoietic cells and immune control system in hematologic neoplasia.
Recent studies have demonstrated that neoplastic cells shed extracellular vesicles (EVs), including exosomes, and endow BM-MSCs to facilitate progression of neoplastic cells (6,7). Exosomes are EVs, about 50–150 nm in size, and contain genetic elements such as messenger RNA, microRNA (miR), and DNA (8–10). EVs act as cargos involved in cell-to-cell communication and are associated with the transformation of adjacent fibroblasts into cancer-associated fibroblasts (CAFs), which are involved in cancer progression (11,12). Tumor cell-derived EVs, including exosomes, also act as angiogenesis agents in the cancer microenvironment (10). Thus, certain types of tumors have the ability to reconstruct the surrounding environment to facilitate the progression of neoplastic cells. On the contrary, BM-MSCs affect functions of neoplastic cells associated with therapy resistance and disease progression (4). Therefore, cell-to-cell communication may exist between tumor cells and the surrounding environment, including fibroblasts, microvessels, and other adjacent tissues.
miRs are very short non-coding RNAs around 20 bp in length and are detected in various cell types and body fluids, including serum, urine, and saliva (9,10). miRs are considered as the candidates of liquid biopsy. In the body fluids, miRs are usually encapsulated in EVs in the stable forms and are transported to other cells, wherein they control cellular functions. As BM-MSCs are major players in the hematopoietic tissue and their genetic alterations in myelodysplastic syndrome (MDS) is plausible, we attempted to search EV-miRs in the BM-MSCs obtained from patients with MDS and acute myeloid leukemia with myelodysplasia-related changes (AML/MRC). We found that the expression of EV-miR-101 in BM-MSCs was downregulated and related to MDS progression.
Materials and methods
Patients
Twenty-nine consecutive patients with myeloid malignancies (22 with MDS and 7 with AML/MRC) were enrolled in this study (Table I). The diagnoses were established as per the World Health Organization criteria, and included three patients with MDS with single lineage dysplasia (SLD), seven with multilineage dysplasia (MLD), two with unclassifiable MDS, one with 5q-syndrome, five with excess blast (EB)-1, and four with EB-2. Risk analysis was carried out based on the revised International Prognostic Scoring System (IPSS-R) (13) and risk categorization was performed as per the NCCN guideline (14). Four patients with MDS with intermediate risk were tentatively included in the low-risk MDS group. Written informed consents were obtained from all patients before the collection of specimens according to the Declaration of Helsinki. The present study was validated by the internal review boards of Tokyo Medical University (no. 2648, approved 22 April, 2014). As controls, human BM-MSCs from healthy donors (normal BM-MSCs) were purchased from Lonza Inc. Control serum was obtained from age-matched healthy individuals.
Table I.
Hematologic features of myelodysplastic syndrome patients of whom bone marrow mesenchymal stroma cells were obtained.
| UPN | Age (Year) | M/F | Dx (WHO) | Date of material obtained | Transition to acute leukemia | Outcome | IPSS | IPSS-R | WBC | Neutrophils | Hb | Plt | PB-blasts (%) | BM-blasts (%) | Karyotype |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 33 | 51 | M | MDS-SLD | 2014/10/10 | No | Alive | Int-1 | Int | 5200 | 4030 | 7.6 | 135 | 0 | 0.8 | complex |
| 54 | 58 | F | MDS-EB1 | 2014/12/16 | No | Alive | Int-1 | Int | 2400 | 1080 | 9.3 | 74 | 0 | 5.6 | 46,XX |
| 59 | 55 | M | MDS-MLD | 2015/1/27 | No | Alive | Low | Very low | 4700 | 2961 | 13.7 | 56 | 0 | 0 | 46,XY |
| 82 | 78 | M | MDS-MLD | 2015/4/30 | No | Unknown | Int-1 | Very low | 1900 | 1267 | 10.6 | 57 | 0 | 2 | 45,X,-Y |
| 95 | 68 | M | MDS-SLD | 2015/8/20 | No | Unknown | Low | Low | 10200 | 7905 | 12.1 | 18 | 0 | 1.2 | 46,XY |
| 93 | 82 | M | MDS-SLD | 2015/8/11 | No | Dead | Low | Very low | 2200 | 1606 | 10.4 | 105 | 0 | 0 | 46,XY,del (20)(q11) |
| 101 | 77 | M | MDS-U based on defining cytogenetic abnormality | 2015/9/17 | No | Alive | Low | Very low | 4600 | 2852 | 10 | 30 | 0 | 0 | 45,X,-Y |
| 102 | 47 | F | MDS-MLD | 2015/9/30 | No | Alive | Int-1 | Low | 2800 | 1274 | 8.3 | 15 | 0 | 0 | 46,XX |
| 103 | 22 | M | MDS-MLD | 2015/10/9 | No | Unknown | Low | Int | 2600 | 845 | 6.3 | 21 | 0 | 0 | 46,XY |
| 107 | 82 | F | MDS-MLD | 2015/10/22 | No | Alive | Low | Low | 6100 | 4148 | 11.2 | 187 | 0.5 | 0.4 | 47,XX,+8 |
| 64_2 | 46 | F | MDS-MLD | 2016/3/8 | No | Alive | Low | Very low | 4500 | 2835 | 13.1 | 299 | 0 | 2 | 46,XX |
| 141 | 84 | M | MDS with isolated del(5q) | 2016/5/19 | No | Alive | Int-1 | Int | 3500 | 1295 | 9.5 | 344 | 0 | 0.5 | 46,XY,del(5q) |
| 115 | 50 | M | MDS-MLD | 2016/10/11 | No | Unknown | Int-1 | Low | 6600 | 5214 | 4.3 | 42 | 0.5 | 2 | 46,XY, del(11)(q14) |
| 8 | 72 | M | MDS-EB1 | 2014/8/8 | No | Unknown | Int-1 | High | 1700 | 408 | 9 | 78 | 0 | 5.2 | 46,XY |
| 12 | 38 | M | MDS-EB2 | 2014/8/26 | No | Unknown | Int-2 | High | 3000 | 1410 | 10.3 | 95 | 0.5 | 10 | 45,XY,-7 |
| 58 | 71 | M | MDS-EB1 | 2015/1/22 | No | Unknown | Int-2 | Very high | 2900 | 2233 | 8.3 | 31 | 0 | 9.2 | complex |
| 22 | 66 | M | MDS-EB1 | 2014/11/27 | Yes | Unknown | Int-1 | High | 2000 | 910 | 7.6 | 16 | 0 | 7.6 | 46,XY |
| 44 | 72 | M | MDS-EB2 | 2015/1/22 | Yes | Dead | High | Very high | 16300 | 2853 | 9.1 | 97 | 5 | 16.8 | 46,XY,-7,+m/46, XY,idem,del(12) (p13) |
| 38 | 56 | M | MDS-EB2 | 2014/10/14 | No | Dead | Int-2 | High | 5500 | 4895 | 8.3 | 164 | 0 | 12.4 | 46,XY |
| 120 | 68 | F | MDS-EB2 | 2016/3/10 | Yes | Dead | High | Very high | 1100 | 374 | 7.8 | 19 | 0 | 17.2 | complex |
| 108 | 87 | M | MDS-U with > 1% PB blasts | 2015/10/26 | No | Dead | in-2 | High | 11400 | 10864 | 8.1 | 65 | 1.5 | 4.8 | 46,XY,del(20) (q11)/46,XY, idem,-7,+8 |
| 175 | 68 | M | MDS-EB1 | 2016/2/3 | Yes | Dead | Int-2 | High | 2000 | 1110 | 8.8 | 30 | 2 | 4.4 | complex |
| 4 | 77 | M | AML with MRC | 2014/4/2 | Dead | 4500 | 393 | 8.9 | 23 | 17 | 49.5 | complex | |||
| 30 | 72 | M | AML with MRC | 2014/10/8 | Unknown | 800 | 248 | 7.7 | 50 | 2 | 21 | 45,X,-Y | |||
| 13 | 61 | M | AML (M6A) with MRC | 2014/9/10 | Dead | 1300 | 338 | 7.6 | 17 | 12 | 12.8 | complex | |||
| 18 | 67 | F | AML with MRC | 2014/9/16 | Dead | 2000 | 520 | 7.9 | 7 | 2.5 | 66 | 45,XX,-7 | |||
| 127 | 64 | M | AML with MRC | 2016/4/11 | Alive | 1300 | 240 | 9.3 | 78 | 0 | 23.2 | 46,XY | |||
| 133 | 67 | F | AML with MRC | 2016/4/26 | Dead | 1400 | 400 | 7.3 | 25 | 8 | 34 | 45,XX,-18 | |||
| 98 | 42 | F | AML with MRC | 2015/9/9 | Dead | 2000 | 270 | 11.3 | 175 | 1.5 | 21 | 46,XX,inv(16) (p13;q22)/47, XX,idem+22 |
UPN, unique patient number; M/F, male/female; Dx, diagnosis; IPSS, International Prognostic Scoring System; IPSS-R, revised IPSS; WBC, while blood cell count (×109/l); Hb, hemoglobin g/dl; Plt, platelets (×1012/l); PB, peripheral blood; BM, bone marrow; MDS, myelodysplastic syndrome; AML with MRC, acute myeloid leukemia with myelodysplasia-related changes; Unknown, due to transfer to another hospital.
Culture of BM-MSCs
BM-MSCs from patients with MDS and AML/MRC were isolated using the conventional plastic adhesion method with a minor modification (15). Briefly, 0.5 to 1 ml of freshy obtained heparinized BM aspirates were cultured in equivalent volumes of Roswell Park Memorial Institute (RPMI)-1640 medium (Thermo Fisher Scientific, Inc.) supplemented with 10% fetal bovine serum (FBS; HyClone) and 1% penicillin-streptomycin (P/S; Thermo Fisher Scientific, Inc.) and Dulbecco's modified Eagle's medium (DMEM) (Thermo Fisher Scientific) containing 10% FBS (GE Healthcare), 1% of P/S, and 1% non-essential amino acids (NEAAs; Thermo Fisher Scientific, Inc.). Cells were cultured for 3 to 5 days, and the medium was changed to DMEM (with 10% of FBS, 1% of P/S and 1% of NEAAs) for non-hematopoietic expansion after the removal of non-adherent cells. Cultured BM-MSC population was identified as CD34−/CD45−/CD73+/CD90+/CD105+ with flow cytometry with <5% CD34+ and CD45+ (15).
Isolation and miR profiling of BM-MSCs
BM-MSCs (4×104 cells/cm2) were cultured in 5 ml of DMEM and the culture supernatants were harvested after 48 h of incubation. EV fraction was purified with Exoquick-TC regent (System Biosciences) according to the manufacturer's instructions. EVs were quantitated with a nanoparticle tracking analysis (NanoSight LM10; Malven) (16–18). Isolation of BM-MSC-derived EV-miRs or cellular-miR and serum EV-miR was performed using the miRNeasy kit (Qiagen). Two-hundred microliters of EV were diluted with 700 µl of QIAzol (Qiagen). After 5 min incubation, 1 nM ath-miR-159 (Hokkaido System Science) was added [18]; the mixture was vortexed for 30 sec and incubated on ice for 10 min. Phenol extraction and cartridge filtration were subsequently performed according to the manufacture's instruction.
Screening of candidate miRNA
miRNA profiling was carried out using a TaqMan low-density miRNA array (TLDA; Thermo Fisher Scientific, Inc.), as previously reported (16,17). PCR was done on a Applied Biosystem 7900 HT thermocycler (Carlsberg) according to the manufacturer's recommended program (the reaction was first incubated at 95°C for 2 min, followed by 50 cycles of 95°C for 15 sec and 60°C for 1 min) using SDS2.2 software and Data Assist (Thermo Fisher Sciences, Inc.). The expression of miRNAs was calculated based on cycle threshold (Ct) values using the 2−ΔΔCq method (19) normalized to those of ath-miR-159, which was spiked in each sample. Data analysis was carried out using GeneSpring software (Agilent Technologies). The Benjamin-Hochberg algorithm was used for the estimation of false discovery rates, as previously reported (16,17).
Validation of candidate miRNA expression by qRT-PCR
To compare selected miRNA expression in various fractions (EV-miRNA, cellular miRNA, and serum EV-miRNA), quantitative real-time PCR was performed by TaqMan® MicorRNA Assays (ThermoFisher Scientific, Inc.) using an ABI Prism 7900 sequence detection system (Applied Biosystem) according to the manufacturer's instruction.
The microRNA specific stem-loop primers (has-miR-101, cat. no. 000438; ath-miR-159, cat. no. 000338) were purchased from ThermoFisher Scientific, Inc. The reaction was first incubated at 95°C for 2 min, followed by 50 cycles of 95°C for 15 sec and 60°C for 1 min, as we have reported previously (18).
Statistical analysis and evaluation of miR-101 targets
Data were expressed as means ± standard deviation (SD). Mann-Whitney U and chi-square tests were used to determine statistical significance for comparisons between the control and test groups. Multiple groups were compared with one-way analysis of variance (ANOVA). Statistical analysis was carried out using R and GraphPad Prism software (v. 5c for Macintosh; GraphPad Software Inc.).
miRs with a ΔCt value >1.0 or <-1.0, and P-values <0.05 were considered to exhibit differential expression. Following identification of differentially expressed miRs, the predicted target genes for these altered miRs were subjected to experimental validation using miR-target interaction database MiRTarBase (http://mirtarbase.mbc.nctu.edu.tw/). In addition, functional annotation of target genes was carried out with Database for Annotation, Visualization, and Integrated Discovery (DAVID Bioinformatics tools v6.7) (http://david.abcc.ncifcrf.gov).
Results
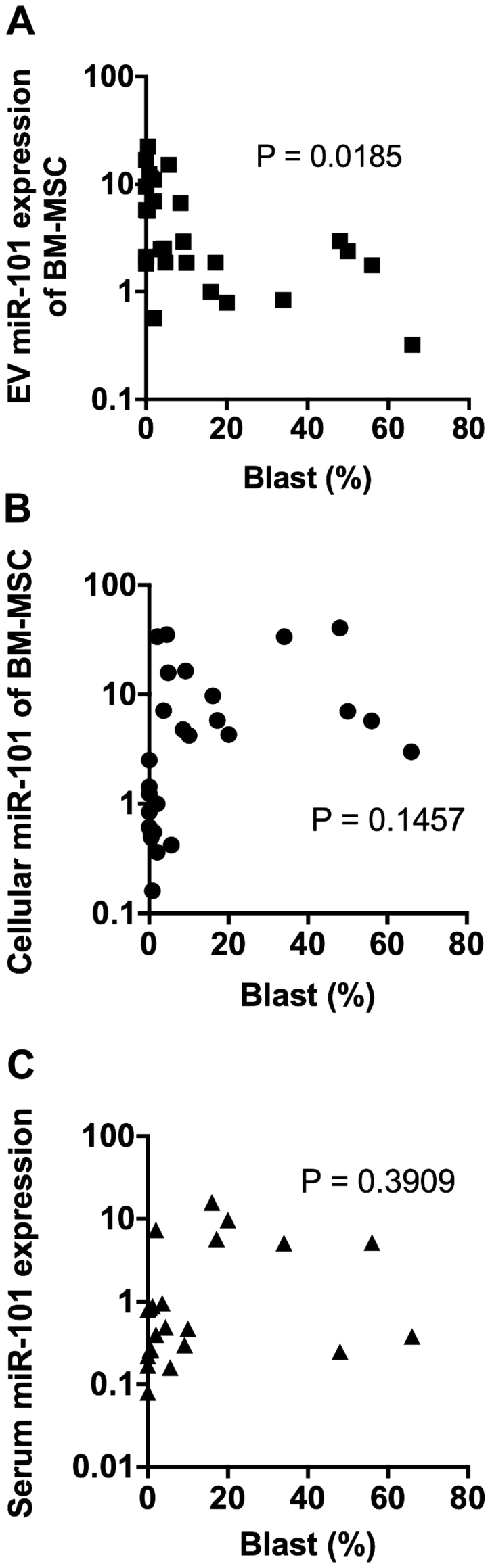
Downregulation of BM-MSC-derived EV miR-101 in patients with high-risk MDS
To identify the association between EV-miRs from BM-MSCs and risk in patients with MDS, we used TLDA to screen the miR expression profile between low-risk group (n=13: Very low, low, and intermediate risk; 9 males/4 females, mean age 61.5 years (range 22 to 84 years old)) and high-risk group (n=9: High and very high risk; 8 males/1 females, mean age 66.4 years (range 38 to 87 years old)) separated by the IPSS-R. Seven patients with AML-MRC included 4 males and 3 females, mean age 64.3 years with ranging 42 to 77 years old). We extracted nine miRs (has-miR-375, has-miR-101, has-miR-424, has-miR-548c-3p, has-miR-15b, has-miR-485-3p, has-miR-579, has-miR-195, and has-miR-369-3p) that were differentially expressed between low-risk and high-risk groups using R software-T test (Figs. 1 and S1) (GSE133276). We then compared the expression patterns of BM-MSC-derived EV-miRs detected with TLDA between normal controls (Lonza) and low-risk group or high-risk group. Of the nine EV-miRs, EV-miR-101 showed no significant difference between normal control and low-risk groups (P=0.5824), while its expression was downregulated in the high-risk group (P=0.0012). We separated 13 MDS patients as low-risk group, including 5 with very low MDS by IPSS-R with marrow blasts <2%, therefore, we considered the character of BM-MSC may overlap of those from normal control. On the other hand, EV-miR-15b expression was downregulated in both the low-risk (P=0.0004) and high-risk (P=0.0001) groups as compared with that in the control BM-MSCs, suggesting that EV-miR-15b could serve as a biomarker for MDS rather than that for disease progression (Fig. 1).
Figure 1.
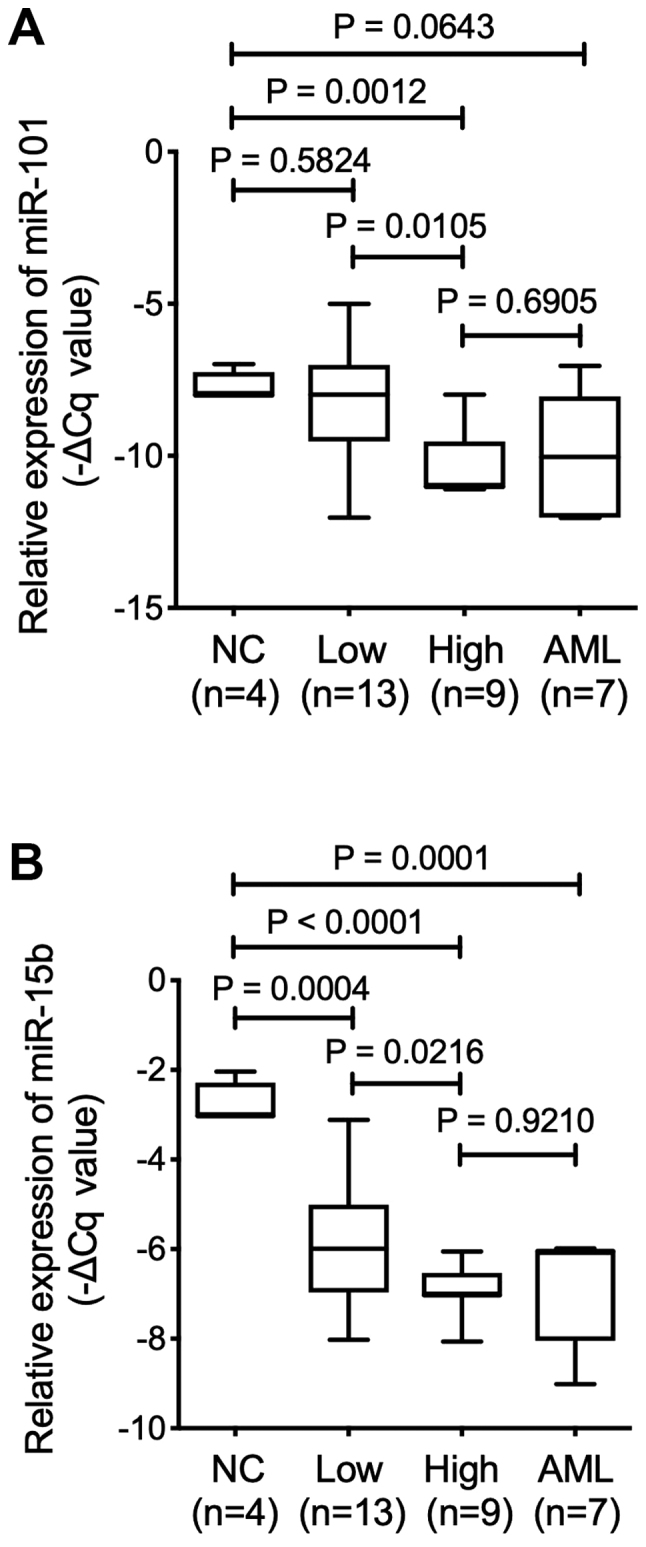
Expression of extracellular vesicle miR derived from BM-MSCs using TaqMan low-density Array (Thermo Fisher Scientific, Inc.). miR expression according to normal control (NC) vs. low-risk MDS group (Low), high-risk MDS group (High) and AML/MRC group (AML). Box plots depict the 75th percentile, median and 25th percentile values; and whisker plots represent minimum to maximum expression. P values were calculated using the independent two-sample t-test. (A) The expression of EV-miR-101 was significantly higher in the low-risk group compared with the high-risk group. The expression of miR-101 in the low-risk group indicated no significant difference compared with the normal controls. (B) Significant differences in the expression of miR-15b were observed between low-risk and normal control groups. miR, microRNA; BM-MSCs, bone marrow mesenchymal stromal cells; NC, negative control; MDS, myelodysplastic syndrome; AML/MRC, acute myeloid leukemia with myelodysplasia-related changes.
To confirm the observation of low expression level of BM-MSC-derived EV-miR-101 in high-risk group and patients with AML/MRC, we quantified the expression of EV-miR-101 with qRT-PCR. As a result, we found no significant difference in EV-miR-101 expression level in BM-MSCs from normal control and low-risk groups (P=0.2579). In contrast, EV-miR-101 expression significantly decreased in the high-risk group (P<0.0001) and patients with AML/MRC (P<0.0001) (Fig. 2A), indicating that BM-MSC-derived EV-miR-101 expression level was associated with disease severity in patients with MDS.
Figure 2.
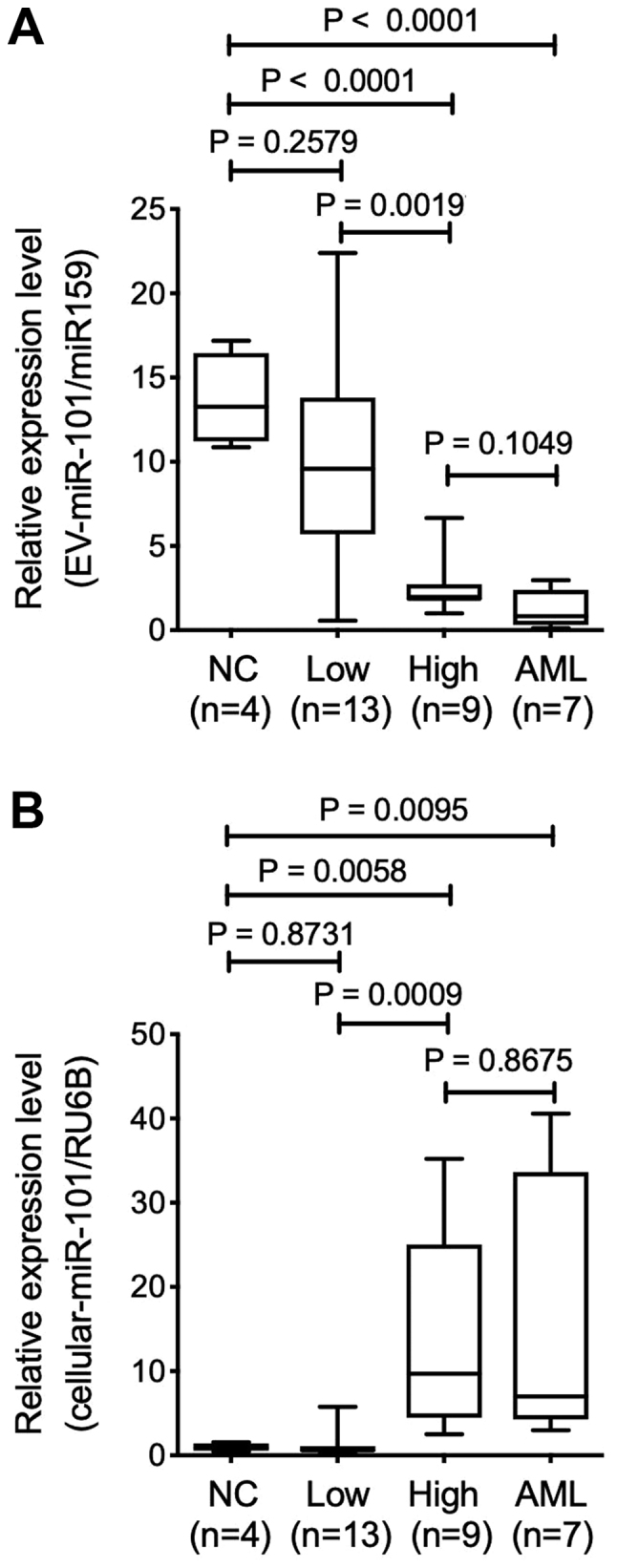
EV miR101 obtained from BM-MSCs. (A) Expression of miR-101 derived from BM-MSCs (B) or serum EV-miR-101 expression (C) as assessed using reverse transcription-quantitative PCR. The expression of EV-miR-101 in the BM-MSCs was significantly higher in the low-risk MDS group compared with the high-risk MDS group, while cellular miR-101 expression was significantly increased in the high-risk group compared with the low-risk group or normal controls. EV, extracellular vesicle; miR, microRNA; BM-MSCs, bone marrow mesenchymal stromal cells; MDS, myelodysplastic syndrome.
Expression pattern of miR-101 in BM-MSCs and serum EV-miR-101
We assessed miR-101 level in BM-MSCs using qRT-PCR, as the pattern of BM-MSC-derived EV-miR-101 was related to MDS disease progression. The relative expression level of miR-101 in control BM-MSCs (Lonza) was lower than that reported in the BM-MSCs from the high-risk group (P=0.0058) and patients with AML/MRC (P=0.0095). No significant difference was reported between normal control and low-risk groups (P=0.8713). Therefore, the expression profile of cellular miR-101 seemed to be a mirror image of the EV-miR-101 obtained from BM-MSCs (Fig. 2B).
We next assessed EV-miR-101 level obtained from the serum using qRT-PCR. Serum was obtained from identical patients with MDS assessed by TLDA, and normal control serum was obtained from age-matched healthy individuals (n=4). The expression level of serum EV-miR-101 was significantly downregulated in low-risk group (n=10) as compared with that in healthy control (P=0.0070), while no significant difference was observed in high-risk group (n=7) (P=0.3232) or patients with AML/MRC (n=6) (P=0.2731) as compared with healthy subjects (Fig. 2C). Serum EV-miR-101 expression pattern correlated with neither BM-MSC-derived EV-miR-101 nor BM-MSC-derived cellular-miR-101 level (data not shown).
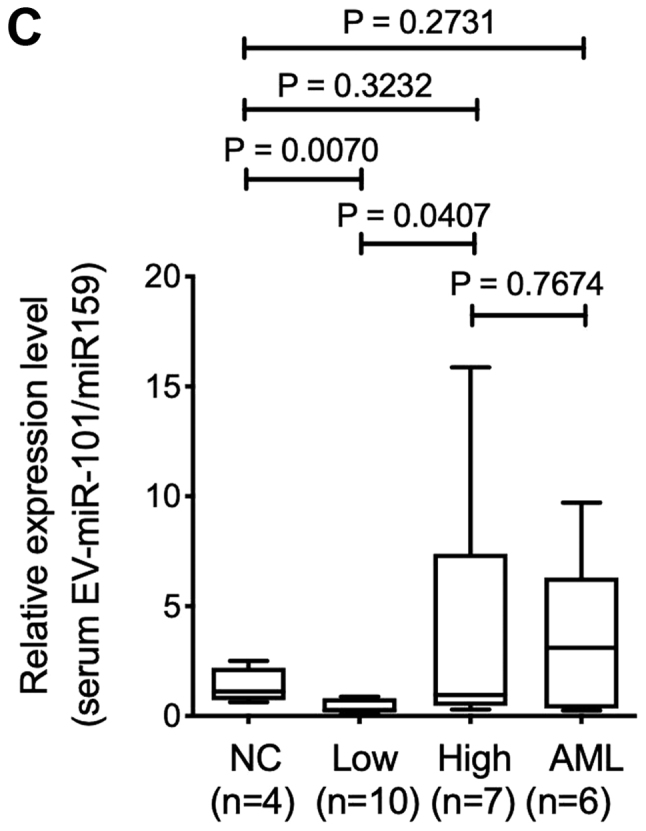
MiR-101 expression level and BM blast percentage
We assessed the association between miR-101 expression levels and percentage of blasts in the BM. The BM-MSC-derived EV-miR-101 level negatively correlated with the occupancy of blasts in the BM (P=0.0185) (Fig. 3A). No significant correlations were observed between BM blast percentage and BM-MSC-derived cellular miR-101 level (P=0.1457) (Fig. 3B) or serum EV-miR-101 level (P=0.3909) (Fig. 3C).
Figure 3.
Correlation between ΒΜ blast percentage and (A) BM-MSC-derived EV-miR-101, (B) cellular miR-101 from BM-MSCs or serum (C) EV-miR-101. ΒΜ, bone marrow; BM-MSCs, bone marrow mesenchymal stromal cells; miR, microRNA.
Target for miR-101
MiRTarBase was used to identify the predicted target genes of miR-101 to determine its biological significance. More than 50 target genes were extracted by MiRTarBase, and the target genes that showed a strong evidence are summarized in Supplementary Table I. The epigenetic regulator genes, including enhancer of zester homolog 2 (EZH2), part of polycomb repressive complex subunit (SUZ12), ten-eleven translocation oncogene family member 2 (TET2), and proto-oncogenes (c-FOS and c-MYC), were experimentally validated with a luciferase reporter assay in the literature. Functional annotation analysis with DAVID revealed the most affected biological pathways of these genes downregulated in the high-risk group, including cell-cycle related pathway and epigenetic regulation pathway (Table II).
Table II.
The gene ontology terms enriched in targets of miR-101. The terms with P-value <0.05 and false discovery rate <0.05 were listed.
| Term | P-value | Benjamini |
|---|---|---|
| Positive regulation of transcription from RNA polymerase II promoter | 9.90×1010 | 1.30×106 |
| Negative regulation of transcription from RNA polymerase II promoter | 4.10×107 | 2.60×104 |
| Positive regulation of gene expression | 2.00×106 | 8.70×104 |
| Negative regulation of cell proliferation | 5.00×106 | 1.60×103 |
| Positive regulation of transcription, DNA-templated | 5.70×106 | 1.50×103 |
| Response to estradiol | 1.20×105 | 2.50×103 |
| Positive regulation of neuroblast proliferation | 3.60×105 | 6.60×103 |
| Cochlea morphogenesis | 4.90 ×105 | 7.80 ×103 |
| Branching morphogenesis of an epithelial tube | 5.60 ×105 | 8.00 ×103 |
| Positive regulation of mesenchymal cell proliferation | 8.20×105 | 1.00×102 |
| Protein phosphorylation | 1.10×104 | 1.30×102 |
| Positive regulation of epithelial to mesenchymal transition | 1.70×104 | 1.80×102 |
| Epithelial to mesenchymal transition | 1.90×104 | 1.80×102 |
| Response to lipopolysaccharide | 2.00×104 | 1.80×102 |
| Coronary artery morphogenesis | 2.20×104 | 1.80×102 |
| Cellular response to hypoxia | 2.70×104 | 2.20×102 |
| Heart development | 3.30×104 | 2.40×102 |
| Thymus development | 3.70×104 | 2.60×102 |
| Positive regulation of apoptotic process | 4.30×104 | 2.90×102 |
| Response to drug | 4.60×104 | 2.90×102 |
| Positive regulation of cellular component movement | 4.70×104 | 2.80×102 |
| Negative regulation of epithelial cell differentiation | 5.70×104 | 3.30×102 |
| Negative regulation of gene expression, epigenetic | 5.80×104 | 3.20×102 |
| Regulation of apoptotic process | 6.50×104 | 3.40×102 |
| Positive regulation of protein phosphorylation | 7.90×104 | 4.00×102 |
| Positive regulation of epithelial cell proliferation | 1.00×103 | 4.80×102 |
miR, microRNA.
Discussion
The present study demonstrates that EV-miR-101 expression level in BM-MSCs was different depending on MDS severity. High-risk group and patients with AML/MRC showed significantly lower expression of BM-MSC-derived EV-miR-101 than the low-risk group or normal controls. In contrast, the expression of miR-101 derived from BM-MSCs was upregulated in patients from the high-risk group, indicative of the dissociation between miR-101 expression level and EV from BM-MSCs in patients with MDS. Although no relationship was observed between BM blast percentage and BM-MSC-derived cellular-miR-101 or serum EV-miR-101 expression level, EV-miR-101 level from BM-MSCs exhibited reverse correlation with BM blast percentage. These findings suggest the possibility that some specific miRs from BM-MSCs may be interrupted from translocation into EVs (or intra-cellular accumulation) and this phenomenon may be linked with the increase in the number of blasts in patients with MDS. The dissociation between cellular miR and EV-miR (or exosomal miR) has been observed in neoplastic cells (9), including leukemia cells (18). However, the current findings deny the possible utility of serum miR measurement as liquid biopsy for various diseases. The importance of BM-MSC-derived EV-miR may indicate the nature of EV-miR, which may participate in the communication between adjacent cells, especially between BM-MSCs and hematologic malignant cells.
Hematologic neoplasia-derived exosomes affect the microenvironment in the BM. For instance, chronic lymphocytic leukemia (CLL) cell-derived exosomes induce the transition of BM stroma cells into CAFs (20). These present enriched miR-150 and miR-146a in CLL-derived exosomes and an elevated miR-150 and miR-146a in BM-MSCs after co-culture with primary CLL cells. CLL exosomes induced the proliferation and migration of BM-MSCs with angiogenesis (20). We also reported that EV-miR-135b from multiple myeloma cells transfers and induces angiogenesis (18). In solid tumors, the phenomenon of transfiguration of the surrounding fibroblasts into CAF has been reported, and this change is known to affect cancer, leading to tumor progression and drug resistance (21). In hematologic neoplasia, the similar situation (CAF induction of BM-MSCs) could be plausible; however, such phenomenon is only limited in lymphoid neoplasia, i.e., CLL and multiple myeloma (20,22).
Ozdogan et al demonstrated the low expression level of DICER1 gene and miR dysregulation in the BM-MSCs obtained from patients with MDS and AML along with the downregulated expression of miRs (miR-30d-5p, miR-222-3p and miR-30a-3p) and overexpression of miR-4426 in MDS-derived BM-MSCs (23). Downregulation of DICER1 expression in the BM-MSCs from patients with MDS promoted cellular senescence and decreased the supportive capability of hematopoietic stem cells along with the downregulation of the expression of miR-17 family (miR-17-5p, miR-20a/b, miR-106a/b, and miR-93) (24). Studies on BM-MSC-derived EV (including exosomes) have focused on limited fields of hematologic neoplasia. Wang et al demonstrated that mouse BM-MSC (5T33)-derived exosomes increased the viability and proliferation and decreased the apoptosis of mouse myeloma cells (5T33 MM model) in response to bortezomib resistance (3). Moreover, these authors showed that human myeloma BM-MSC-derived exosomes increased the viability of human myeloma cells (RPMI-8226) in a dose-dependent manner (3). Umezu et al also reported that the BM-MSC-derived EV-miR-340 from normal young donor (Lonza), rather than old donor, inhibited myeloma-induced angiogenesis via hepatocyte growth factor/c-MET signaling (25). In this study, no particular correlation was observed in the expression level between BM-MSC-derived EV-miR-101 and serum EV-miR-101, suggesting that the BM-MSC-derived EV-miR-101 may affect adjacent cells, including MDS cells.
miR-101 is known to exert anti-neoplastic effects and facilitate apoptosis (26). For instance, miR-101 exhibited suppressive effects on bladder cancer via c-FOS (27), colorectal cancer via EZH2 (28), and breast cancer via EYA1 (29). miR-101 is also known to exert suppressive effects on vascular endothelial growth factor-C (30,31). Recent reports found that miR-101 regulates the development and progression of myeloid- and T-lymphoid lineage leukemia (32,33) and suppresses the proliferation of neoplastic cells by targeting genes related to epigenetic regulation (Tables II and SI). Thus, we speculate the possibility that EV-miR-101 from BM-MSCs transfer to MDS cells and control their proliferation via epigenetic regulation. In patients with high-risk MDS, the decrease in the expression level of EV-miR-101 may result in the release of the anti-proliferative effect on MDS cells. Another plausible possibility is that the more malignant clone during MDS progression may induce BM-MSCs to suppress EV-miR-101 expression. miR-101 antisense transfection assay showed enhanced proliferation of human myeloid leukemia (HL-60) cells with an increase in c-FOS expression (unpublished observation), thus suggesting that the downregulation of EV-miR-101 expression in patients with high-risk MDS may affect the proliferation of MDS cells.
Development of MDS is known to be associated with the accumulation of genetic abnormalities by aging, so-called ‘Clonal Hematopoiesis of Indeterminate Potential (CHIP)’, and additional mutations in critical genes, including epigenetic regulator genes, accelerate AML (34). In addition to genetic abnormalities in MDS cells, BM-MSCs are also shown to have synonymous or non-synonymous mutations (15,35,36) such as ‘genetic injury.’ The unresolved issue is whether demethylating agents available for patients with MDS could exert any effect on BM-MSCs, especially BM-MSC-derived EV, as miR-101 targets many epigenetic regulator genes. Poon et al demonstrated that a hypomethylating agent (azacytidine) could also target BM-MSCs in dysplastic MDS and contribute to the restoration of active hematopoiesis, whereas patients with MDS that failed to respond to hypomethylating treatment had disease progression (37). We could not reproduce the peculiarity of BM-MSC-derived miR concerning the anatomical architecture of MDS.
In conclusion, the current study demonstrates that the BM-MSCs obtained from patients with MDS were heterogenous with respect to the expression of EV-miR. Patients with high-risk MDS and AML/MRC had lower expression of BM-MSC-derived EV-miR-101 than those with low-risk MDS. This tendency was reversible as compared with the miR-101 level from BM-MSCs; the serum EV-miR-101 expression showed no association. Although we failed to clarify the exact mechanism underlying the downregulation of EV-miR-101 expression from BM-MSCs in patients with high-risk MDS, targeting miR-101 may regulate neoplastic proliferation. Thus, the downregulation of EV-miR-101 expression may affect adjacent cell-to-cell communication and accelerate the malignant process in MDS cells.
Supplementary Material
Acknowledgements
Not applicable.
Glossary
Abbreviations
- BM
bone marrow
- BM-MSC
bone marrow mesenchymal stromal cell
- miR
microRNA
- MDS
myelodysplastic syndrome
- AML
acute myeloid leukemia
- AML/MRC
acute myeloid leukemia with myelodysplasia-related changes
- TLDA
TaqMan-low density array
- CAF
cancer-associated fibroblast
- IPSS-R
revised International Prognostic Scoring System
Funding
The present study was supported by the Platform Project for Practical Research for Innovative Cancer Control from the Japan Agency for Medical Research and Development (grant no. 15Ack0106073h0002), the Private University Strategic Research-Based Support Project (grant no. S1311016) from the Ministry of Education, Culture, Sports, Science and Technology and JSPS KAKENHI (grant no. 19K16811).
Availability of data and materials
The datasets generated and/or analyzed during the present study are available from the Gene Expression Omnibus repository, https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE133276.
Authors' contributions
YS, MA, SY, SK, TS, HF, DA and KO treated the patients; TU and CKK performed TLDA, PCR and data analysis; SI established BM-MSCs; TU contributed essential reagents or tools; YS and KO wrote the manuscript; KO and JHO designed the research and supervised the project. All authors contributed to data analysis and drafting of the manuscript.
Ethics approval and consent to participate
Patient data was used in the present study according to the ethical principles for medical research involving human subjects of The Declaration of Helsinki (38). The study protocols were approved by The Regional Ethics Review Board of Tokyo Medical University (Tokyo, Japan), and all patients provided written informed consent prior to participation.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Morrison SJ, Scadden DT. The bone marrow niche for haematopoietic stem cells. Nature. 2014;505:327–334. doi: 10.1038/nature12984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anthony BA, Link DC. Regulation of hematopoietic stem cells by bone marrow stromal cells. Trends Immunol. 2014;35:32–37. doi: 10.1016/j.it.2013.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang J, Hendrix A, Hernot S, Lemaire M, De Bruyne E, Van Valckenborgh E, Lahoutte T, De Wever O, Vandenrkerken K, Menu E. Bone marrow stroma cell-derived exosomes as communications in drug resistance in multiple myeloma cells. Blood. 2014;124:555–566. doi: 10.1182/blood-2014-03-562439. [DOI] [PubMed] [Google Scholar]
- 4.Bernardo ME, Fibbe WE. Mesenchymal stromal cells: Sensors and switches of inflammation. Cell Stem Cell. 2013;13:392–402. doi: 10.1016/j.stem.2013.09.006. [DOI] [PubMed] [Google Scholar]
- 5.Nauta AJ, Fibbe WE. Immunomodulatory properties of mesenchymal stromal cells. Blood. 2007;110:3499–3506. doi: 10.1182/blood-2007-02-069716. [DOI] [PubMed] [Google Scholar]
- 6.Whiteside TL. Exosome and mesenchymal stem cell cross-talk in the tumor microenvironment. Semin Immunol. 2018;35:69–79. doi: 10.1016/j.smim.2017.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lin LY, Du LM, Cao K, Huang Y, Yu PF, Zhang LY, Li FY, Wang Y, Shi YF. Tumor cell-derived exosomes endow mesenchymal stromal cells with tumour-promotion capabilities. Oncogene. 2016;35:6038–6042. doi: 10.1038/onc.2016.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gebert LFR, MacRae IJ. Regulation of microRNA function in animals. Nat Rev Mol Cell Biol. 2019;20:21–37. doi: 10.1038/s41580-018-0045-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Makarova JA, Shkumikov MU, Wicklein D, Lange T, Samatov TR, Turchinovich AA, Tonevitsky AG. Intracellular and extracellular microRNA: An update on localization and biological role. Prog Histochem Cytochem. 2016;51:33–49. doi: 10.1016/j.proghi.2016.06.001. [DOI] [PubMed] [Google Scholar]
- 10.Ohyashiki JH, Umezu T, Ohyashiki K. Extracellular vesicle-mediated cell-cell communication in haematological neoplasms. Philos Trans R Soc Lond B Biol Sci. 2018;373(pii):20160484. doi: 10.1098/rstb.2016.0484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Azmi AS, Bao B, Sarkar FH. Exosomes in cancer development, metastasis and drug resistance: A comprehensive review. Cancer Metastasis Rev. 2013;32:623–642. doi: 10.1007/s10555-013-9441-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yang X, Li Y, Zou L, Zhu Z. Role of exosomes in crosstalk between cancer-associated fibroblasts and cancer cells. Front Oncol. 2019;9:356. doi: 10.3389/fonc.2019.00356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Greenberg PL, Tuechler H, Schanz J, Sanz G, Garcia-Manero G, Solé F, Bennett JM, Bowen D, Fenaux P, Dreyfus F, et al. Revised international prognostic scoring system for myelodysplastic syndromes. Blood. 2012;120:2454–2465. doi: 10.1182/blood-2012-03-420489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Greenberg PL, Stone RM, Al-Kli A, Barta SK, Bejar R, Bennett JM, Carraway H, De Castro CM, Deeg HJ, DeZern AE, et al. Myelodysplastic syndrome, version 2. 2017, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2017;15:60–87. doi: 10.6004/jnccn.2017.0007. [DOI] [PubMed] [Google Scholar]
- 15.Azuma K, Umezu T, Imanishi S, Asano M, Yoshizawa S, Katagiri S, Ohyashiki K, Ohyashiki JH. Genetic variations of bone marrow mesenchymal stromal cells derive from acute leukemia and myelodysplastic syndrome by targeted deep sequencing. Leuk Res. 2017;62:23–28. doi: 10.1016/j.leukres.2017.09.008. [DOI] [PubMed] [Google Scholar]
- 16.Umezu T, Ohyashiki K, Kuroda M, Ohyashiki JH. Leukemia cell to endothelial cell communication via exosomal miRNAs. Oncogene. 2013;32:2747–2755. doi: 10.1038/onc.2012.295. [DOI] [PubMed] [Google Scholar]
- 17.Yoshizawa S, Umezu T, Saitoh Y, Gotoh M, Akahane D, Kobayashi C, Ohyashiki JH, Ohyashiki K. Exosomal miRNA signatures for late-onset acute graft-versus host disease in allogeneic hematopoietic stem cell transplantation. Int J Mol Sci. 2018;19(pii):E2493. doi: 10.3390/ijms19092493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Umezu T, Tadokoro H, Azuma K, Yoshizawa S, Ohyashiki K, Ohyashiki JH. Exosomal miR-135b shed from hypoxic multiple myeloma cells enhances angiogenesis by targeting factor-inhibiting HIF-1. Blood. 2014;124:3748–3757. doi: 10.1182/blood-2014-05-576116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 20.Paggetti J, Haderk F, Seiffert M, Janji B, Distler U, Ammerlaan W, Kim YJ, Adam J, Lichter P, Solary E, et al. Exosomes released by chronic lymphocytic leukemia cells induce the transition of stromal cells into cancer-associated fibroblasts. Blood. 2015;126:1106–1117. doi: 10.1182/blood-2014-12-618025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Orimo A, Weinberg RA. Stromal fibroblasts in cancer: A novel tumor-promoting cell type. Cell Cycle. 2006;5:1597–1601. doi: 10.4161/cc.5.15.3112. [DOI] [PubMed] [Google Scholar]
- 22.De Veirman K, Rao L, De Bruyne E, Menu E, Van Valckenborgh E, Van Riet I, Frassanito MA, Di Marzo L, Vacca A, Vanderkerken K. Cancer associated fibroblasts and tumor growth: Focus on multiple myeloma. Cancers (Basel) 2014;6:1363–1381. doi: 10.3390/cancers6031363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ozdogan H, Gur Dedeoglu B, Oztemur Islakoglu Y, Aydos A, Kose S, Ataly A, Yegin ZA, Avcu F, Uckan Cetinkaya D, Ihan O. DICER1 gene and miRNA dysregulation in mesenchymal stem cells of patients with myelodysplastic syndrome and acute myeloblastic leukemia. Leuk Res. 2017;63:62–71. doi: 10.1016/j.leukres.2017.10.006. [DOI] [PubMed] [Google Scholar]
- 24.Zhao Y, Wu D, Fei C, Guo J, Gu S, Xu F, Zhang Z, Wu L, Li X, Chang C. Down-regulation of Dicer1 promotes cellular senescence and decreases the differentiation and stem cell-supporting capacities of mesenchymal stromal cells in patient with myelodysplastic syndrome. Haematologica. 2015;100:194–204. doi: 10.3324/haematol.2014.109769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Umezu T, Imanishi S, Azuma K, Kobayashi C, Yoshizawa S, Ohyashiki K, Ohyashiki JH. Replenishing exosomes from older bone marrow stromal cells with miR-340 inhibits myeloma-related angiogenesis. Blood Adv. 2017;1:812–823. doi: 10.1182/bloodadvances.2016003251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Su H, Yang JR, Xu T, Huang J, Xu L, Yuan Y, Zhuang SM. MicroRNA-101, down-regulated in hepatocellular carcinoma, promotes apoptosis and suppresses tumorigenicity. Cancer Res. 2009;69:1135–1142. doi: 10.1158/0008-5472.CAN-08-2886. [DOI] [PubMed] [Google Scholar]
- 27.Long Y, Wu Z, Yang X, Chen L, Han Z, Zhang Y, Liu L, Liu W, Liu X. MicroRNA-101 inhibits the proliferation and invasion of bladder cancer cells via targeting c-FOS. Mol Med Rep. 2016;14:2651–2656. doi: 10.3892/mmr.2016.5534. [DOI] [PubMed] [Google Scholar]
- 28.Peng Z, Zhang Y. Methyl jasmonate induces the apoptosis of human colorectal cancer cells via down regulation of EZH2 expression by microRNA-101. Mol Med Rep. 2017;15:957–962. doi: 10.3892/mmr.2016.6061. [DOI] [PubMed] [Google Scholar]
- 29.Guan H, Dai Z, Ma Y, Wang Z, Liu X, Whang X. MicroRNA-101 inhibits cell proliferation and induces apoptosis by targeting EYA1 in breast cancer. Int J Mol Med. 2016;37:1643–1651. doi: 10.3892/ijmm.2016.2557. [DOI] [PubMed] [Google Scholar]
- 30.Deng G, Teng Y, Huang F, Nie W, Zhu I, Huang W, Xu H. MicroRNA-101 inhibits the migration and invasion of intrahepatic cholangiocarcinoma cells via direct suppression of vascular endothelial growth factor-C. Mol Med Rep. 2015;12:7079–7085. doi: 10.3892/mmr.2015.4239. [DOI] [PubMed] [Google Scholar]
- 31.Li G, Yang F, Gu S, Li Z, Xue M. MicroRNA-101 induces apoptosis in cisplatin-resistant gastric cancer cells by targeting VEGF-C. Mol Med Rep. 2016;13:572–578. doi: 10.3892/mmr.2015.4560. [DOI] [PubMed] [Google Scholar]
- 32.Gonzales-Aloy E, Connerty P, Salik B, Liu B, Woo AW, Haber M, Norris MD, Wand J, Wand JY. MiR-101 suppresses the development of MLL-rearranged acute myeloid leukemia. Haematologica. 2019;104:e296–e300. doi: 10.3324/haematol.2018.209437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Qian L, Zhang W, Lei B, He A, Ye L, Li X, Don X. MicroRNA-101 regulates T-cell acute lymphoblastic leukemia progression and chemotherapeutic sensitivity by targeting Notch1. Oncol Rep. 2015;36:2511–2526. doi: 10.3892/or.2016.5117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ghobrial IM, Detappe A, Anderson KC, Steensma SP. The bone-marrow niche in MDS and MGUS: Implications for AML and MM. Nat Rev Clin Oncol. 2018;15:219–233. doi: 10.1038/nrclinonc.2017.197. [DOI] [PubMed] [Google Scholar]
- 35.Flores-Figueroa E, Arana-Trejo RM, Gutierrez-Espindola G, Perez-Cabrera A, Mayani H. Mesenchymal stem cells in myelodysplastic syndromes: Phenotypic and cytogenetic characterization. Leuk Res. 2005;29:215–224. doi: 10.1016/j.leukres.2004.06.011. [DOI] [PubMed] [Google Scholar]
- 36.Blau O, Hofmann WK, Baldus CD, Thiel G, Serbent GV, Schumann E, Thiel E, Blau IW. Chromosomal aberrations in bone marrow mesenchymal stroma cells from patients with myelodysplastic syndrome and acute myeloblastic leukemia. Exp Hematol. 2007;35:221–229. doi: 10.1016/j.exphem.2006.10.012. [DOI] [PubMed] [Google Scholar]
- 37.Poon Z, Dighe N, Venkatesan SS, Cheung AMS, Fan X, Bari S, Hota M, Ghosh S, Hwang WYK. Bone marrow MSCs in MDS: Contribution towards dysfunctional hematopoiesis and potential targets for disease response to hypomethylating therapy. Leukemia. 2019;33:1487–1500. doi: 10.1038/s41375-019-0406-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.World Medical Association; 2013. WMA declaration of Helsinki: Ethical principles for medical research involving human subjects. Retrieved from. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated and/or analyzed during the present study are available from the Gene Expression Omnibus repository, https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE133276.


