Abstract
The lack of hormone receptors in triple negative breast cancer (TNBC) is associated with the inefficacy of anti-estrogen chemotherapies, leaving fewer options for patient treatment and higher mortality rates. Additionally, as with numerous types of inflammatory breast cancer, infiltration of tumor associated macrophages and other leukocyte sub-populations within the tumor inevitably lead to aggressive, chemo-resistant, metastatic and invasive types of cancer which escape immune surveillance. These processes are orchestrated by the release of potent cytokines, including TNFα, IL-6 and CCL2 from the stroma, tumor and immune cells within the tumor microenvironment. The present study evaluated apigenin modulating effects on the pro-inflammatory activating action of TNFα in TNBC MDA-MB-468 cells, derived from an African American woman. Initially, cell viability was determined to establish an optimal sub-lethal dose of TNFα and apigenin in MDA-MB-468 cells. Subsequently, various treatments effects were evaluated using whole transcriptomic analysis of mRNA and long intergenic non-coding RNA with Affymetrix HuGene-2.1-st human microarrays. Gene level differential expression analysis was conducted on 48,226 genes where TNFα caused significant upregulation of 53 transcripts and downregulation of 11 transcripts. The largest upward differential shift was for CCL2 [+61.86 fold change (FC); false discovery rate (FDR), P<0.0001]; which was down regulated by apigenin (to +10.71 FC vs. Control; FDR P-value <0.001), equivalent to an 83% reduction. Several TNFα deferentially upregulated transcripts were reduced by apigenin, including CXCL10, C3, PGLYRP4, IL22RA2, KMO, IL7R, ROS1, CFB, IKBKe, SLITRK6 (a checkpoint target) and MMP13. Confirmation of CCL2 experimentally induced transcript alterations was corroborated at the protein level by ELISA assays. The high level of CCL2 transcript in the cell line was comparable to that in our previous studies in MDA-MB-231 cells. The differential effects of TNFα were corroborated by ELISA, where the data revealed a >10-fold higher releasing rate of CCL2 in MDA-MB-468 cells compared with in MDA-MB-231 cells, both of which were attenuated by apigenin. The data obtained in the present study demonstrated a high level of CCL2 in MDA-MB-468 cells and a possible therapeutic role for apigenin in downregulating TNFα-mediated processes in these TNBC cells.
Keywords: whole transcriptome, triple negative breast cancer, apigenin, MDA-MB-468
Introduction
Within the past several decades, we have seen an increase in research on the infiltration of leukocyte sub-populations (LSPs), being drawn, sequestered and embedded within solid tumor tissue corresponding to elevated concentrations of chemokines such as CCL2 (1). Both animal and in vitro studies have shown CCL2 can sequester macrophages and other immune components such as myeloid-derived suppressor cells or regulatory T cells all of which promote immune evasion, epithelial-to-mesenchymal transition, tumor growth, metastasis, and immune evasion. High concentrations of pro-inflammatory proteins such as CCL2, TNFα, matrix metalloproteinase 9, interleukin-6 (IL-6), chemokine (C-X-C motif) ligands (e.g., CXCL) (1–4), granulocyte-macrophage colony-stimulating factor and other chemokine ligands (e.g., CCLs) (5–9) are commonly reported as tumor promoting proteins in diverse cancers such as thyroid, brain, gastric, lung, glioblastoma multiforme and breast (2–7,10–15).
What is evidently a critical situation is that these inflammatory proteins, in particular, the CCL2 and IL-6 are brought about by the actual cancer treatments themselves (e.g., radiotherapy (16) chemotherapy (8), which in turn are then associated with tumor recurrence (17) and chemo-resistance (18,19), Inflammatory events in general, whether it be from other parts of the body such as the liver (9,20) adipose tissue in obesity or arising from viral origin tend to elevate TNF-a, IL −6 and CCL2 then becoming risk factors for the development of diverse cancers (21) aggressive tumors with advanced stage tumor grade and greater rates of mortality (22,23). Meanwhile, it is believed that drugs or natural compounds that can attenuate CCL2 and IL-6 would slow the aggressive nature of advanced cancers (24–26) to the inclusion of triple negative breast cancer (TNBC) and hormone positive breast cancers (27,28). It is believed that utilizing synthetic or natural small molecules as CCR2 inhibitors (CCR2i) can increase overall survival odds (29,30).
In our previous work, we found that apigenin, a pigment naturally found in parsley, can modulate TNFα triggered release of chemokines in a TNBC model using MDA-MB-231 cells (31). In the present study, we carried out a similar experiment using a TNBC cell line derived from an African American woman (MDA-MB-468, MDA-MB-468 cells), which express enormously high levels of CCL2 upon impact by TNFα as demonstrated by the current work.
Materials and methods
Triple-negative human breast tumor (MDA-MB-468) cells were obtained from the American Type Culture Collection (Rockville, MD, USA). Dulbecco's modified Eagle's medium (DMEM), fetal bovine serum (FBS), and penicillin/streptomycin were all obtained from Invitrogen. Recombinant human TNFα and CCL2 ELISA kits were purchased from RayBiotech (RayBiotech Inc.).
Cell culture
MDA-MB-468 cells were grown in high-glucose DMEM (w/phenol red and glutamine) supplemented with 10% FBS and 1% [10,000 U/ml] penicillin G sodium + [10,000 µg/ml] streptomycin sulfate. Cells were grown at 37°C with humidified 95% air and 5% CO2 and sub-cultured every 3–5 days.
Cell viability assay
Viable cell count was determined by Alamar blue. Briefly, 96-well plates were seeded with MDA-MB-468 cells at a density of 5×104 cells/100 µl/well with various treatments. After 24 h, Alamar blue (0.1 mg/ml in HBSS) was added at 15% v/v to each well and incubated for 6–8 h. Quantitative analysis of dye conversion was measured using a Biotek Synergy multi-mode detection reader equipped with Gen5 software 550/580 (excitation/emission). Data were expressed as a percentage of the untreated control groups.
CCL2 detection by ELISA
Supernatants from experimental treatments were collected, centrifuged at 1,000 × g for 5 min at 4°C and evaluated for MCP-1/CCL2 using Human MCP1 ELISA from RaybioRayBiotech Life, following the manufacturer's instructions. Briefly, a dilution from 10–50% of supernatants was made with assay buffer (final working volume = 100 µl), and standards was added to 96-well plates pre-coated with the capture antibody. Samples were washed 4× between steps, and after adding the HRP-conjugate, the substrate/stopping solutions were added, and plates were read at 450 nm using a Biotek Synergy multi-mode detection reader equipped with Gen5 software. All data were expressed as concentration derived from a standard curve in pg/ml.
Microarray WT 2.1 human datasets
Cells were collected by a 3X wash in ice-cold HBSS, then a rapid freeze with storage at −80°C. Total RNA was isolated and purified using the TRIzol/chloroform method, the quality was assessed, and concentration was equalized to 82 ng/µl in nuclease-free water. Whole transcriptome analysis was conducted according to the GeneChipTM WT PLUS Reagent Manual for Whole Transcript (WT) Expression Arrays for human 2.1 Array Strips (32). Briefly, RNA was synthesized to first strand cDNA, second-strand cDNA and followed by transcription to cRNA. cRNA was purified and assessed for yield, before 2nd cycle single-stranded cDNA synthesis, hydrolysis of RNA and purification of 2nd cycle single-stranded cDNA. cDNA was then quantified for yield and equalized to 176 ng/ml. Subsequently, cDNA was fragmented, labeled and hybridized on to the arrays before being subject to fluidics and imaging using the Gene Atlas (Affymetrix- Thermo Fisher Scientific, Inc.).
Statistical analysis
A Kruskal-Wallis test, followed by a Dunn's multiple comparison test was used to evaluate statistical differences from controls and a one-way ANOVA followed by a Tukey's multiple comparisons test to evaluate statistical differences between two cell lines both using GraphPad prism software (GraphPad Software). The array data quality control and initial processing from CEL to CHP files were conducted using expression console, followed by data analysis using the Affymetrix transcriptome analysis console (Affymetrix-Thermo Fisher Scientific, Inc.). The data have been deposited into the Gene Expression Omnibus for public analysis at https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE133968.
Results
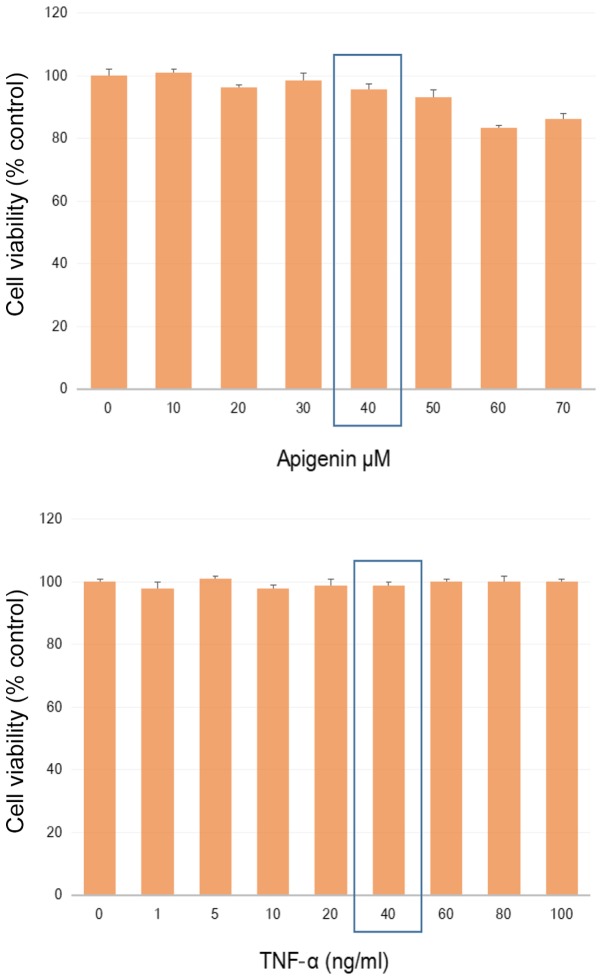
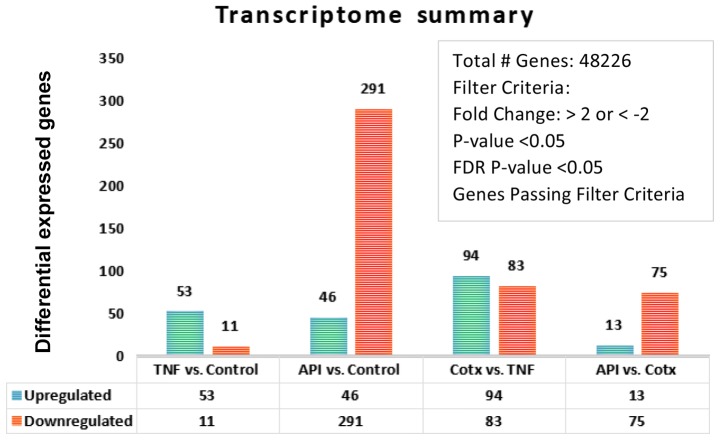
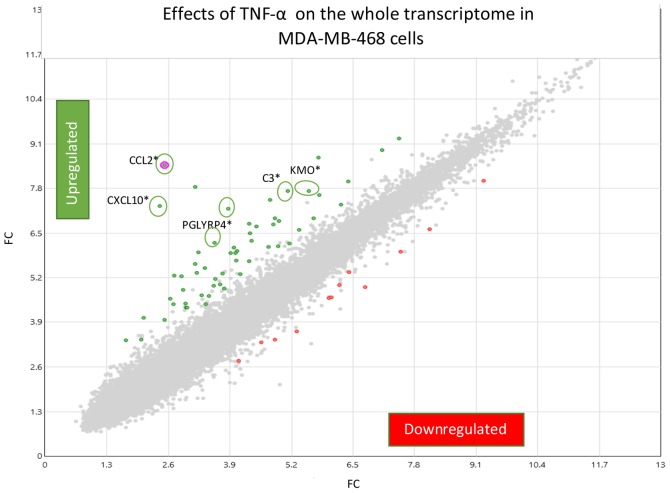
A non-lethal working concentration was established in MDA-MB-468 cells for TNFα and apigenin (Fig. 1) to where sub-lethal values were determined by a dose response using apigenin [40 uM], and TNFα [40 ng/ml]. Whole transcriptomic differential changes between untreated controls, TNFα (40 ng/ml), apigenin (40 uM) and co-treatment (CoTx) [TNFα (40 ng/ml) + apigenin (40 uM)] were acquired and the summary by a number of deferentially expressed genes shown in Fig. 2. Comparing the Control vs. TNFα only, we provide a fold change (FC) scatter plot (Fig. 3) corresponding to signal and processed data presented in Table I. Gene level differential expression analysis was conducted on 48,226 genes where TNFα caused significant up-regulation of 53 transcripts and down-regulation of 11 transcripts.
Figure 1.
Preliminary determination of sub-lethal working concentrations. The effect of TNFα and apigenin on cell viability of MDA-MB-468 cells at 5% CO2/Atm for 24 h. The data are presented as viability (% Ctrl), mean ± SEM (n=4). The significance of differences from the Ctrl were determined by a Kruskal-Wallis test, followed by a Dunn's multiple comparison test. N.S. TNF-, tumor necrosis factor α; Ctrl, control.
Figure 2.
Transcriptome summary. Whole transcriptomic differential changes between untreated controls, TNFα (40 ng/ml), apigenin (40 µM) and CoTx [TNFα (40 ng/ml) + apigenin (40 µM)] after 24 h treatment in MDA-MB-468 cells. A total of 48,226 gene transcripts were analyzed for each group. Diferentially expressed genes (upregulated and downregulated) that passed the filter criteria (FDR P-value and P-values <0.05) are presented by number. FDR, false discovery rate; TNF, tumor necrosis factor; Cotx, co-treatment; API, apigenin.
Figure 3.
TNF-α (40 ng/ml) induces alterations in MDA-MB-468 cells. The data are presented by a scatterplot showing differentially expressed genes meeting the filter criteria (FDR P-value and P-values <0.05) and FC <-2 and >2 are presented (full description in Table I). Green represents upregulated transcripts, gray represents genes omitted as significant falling below a 2-fold change in either direction, red represents downregulated transcripts and pink is the highest upregulated transcript. Genes relevant to the findings of the present study are circled and presented along with their corresponding official gene symbol. *attenuated by apigenin. FC, fold change; TNF-α, tumor necrosis factor-α; FDR, false discovery rate; CCL2, C-C motif chemokine ligand 2; CXCL10, C-X-C motif chemokine ligand 10; PGLYRP4, peptidoglycan recognition protein 4; C3, complement C3; KMO, kynurenine 3-monooxygenase.
Table I.
Differential whole transcriptome pattern induced by TNFα (40 ng/ml) relative to untreated controls in MM-468 cells.
| Control (Avg log2) | TNFα (Avg log2) | Fold change | P-value | FDR P-value | Gene symbol | Description |
|---|---|---|---|---|---|---|
| 2.52 | 8.47 | 61.86 | 2.37×10−10 | 3.82×10−6 | CCL2 | Chemokine (C-C motif) ligand 2 |
| 2.41 | 7.29 | 29.40 | 1.80×10−12 | 8.70×10−8 | C xCL10 | Chemokine (C- x-C motif) ligand 10 |
| 3.17 | 7.84 | 25.63 | 2.28×10−10 | 3.82×10−6 | C xCL8 | Chemokine (C- x-C motif) ligand 8 |
| 3.86 | 7.20 | 10.13 | 3.89×10−10 | 4.69×10−6 | TNFAIP3 | Tumor necrosis factor, alpha-induced protein 3 |
| 5.78 | 8.69 | 7.56 | 6.07×10−9 | 4.18×10−5 | BIRC3 | Baculoviral IAP repeat containing 3 |
| 3.23 | 5.94 | 6.55 | 2.62×10−7 | 6.00×10−4 | IGFL1 | IGF like family member 1 |
| 4.75 | 7.45 | 6.50 | 4.83×10−9 | 4.18×10−5 | C3 | Complement component 3 |
| 3.57 | 6.20 | 6.18 | 1.10×10−7 | 4.00×10−4 | PGLYRP4 | Peptidoglycan recognition protein 4 |
| 5.12 | 7.71 | 6.02 | 7.79×10−7 | 1.10×10−3 | KMO | Kynurenine 3-monoo xygenase |
| 2.72 | 5.27 | 5.86 | 2.80×10−7 | 6.00×10−4 | AMY1B | Amylase, alpha 1B |
| 4.3 | 6.78 | 5.57 | 7.89×10−7 | 1.10×10−3 | IL22RA2 | Interleukin 22 receptor, alpha 2 |
| 3.16 | 5.60 | 5.42 | 8.11×10−9 | 4.89×10−5 | SAA24 | Serum amyloid A2 |
| 2.87 | 5.23 | 5.13 | 1.85×10−5 | 1.44×10−2 | CCL20 | Chemokine (C-C motif) ligand 20 |
| 4.46 | 6.69 | 4.69 | 1.09×10−7 | 4.00×10−4 | CFB | Complement factor B |
| 4.32 | 6.48 | 4.48 | 5.63×10−9 | 4.18×10−5 | ABCC4 | ATP binding cassette subfamily C member 4 |
| 5.56 | 7.71 | 4.43 | 2.25×10−7 | 6.00×10−4 | TNFAIP2 | Tumor necrosis factor, alpha-induced protein 2 |
| 3.37 | 5.49 | 4.33 | 3.71×10−7 | 8.00×10−4 | IL7R | Interleukin 7 receptor |
| 3.98 | 6.07 | 4.27 | 8.37×10−7 | 1.20×10−3 | ROS1 | ROS proto-oncogene 1, receptor tyrosine kinase |
| 4.85 | 6.92 | 4.19 | 1.85×10−7 | 6.00×10−4 | OLR1 | Oxidized low density lipoprotein receptor 1 |
| 3.91 | 5.90 | 3.99 | 6.35×10−7 | 1.00×10−3 | TNF | Tumor necrosis factor |
| 2.07 | 4.04 | 3.91 | 4.86×10−6 | 4.60×10−3 | INHBA | Inhibin beta A |
| 2.64 | 4.58 | 3.84 | 6.31×10−6 | 5.80×10−3 | AMY1B | Amylase, alpha 1B |
| 4.81 | 6.74 | 3.81 | 1.27×10−7 | 5.00×10−4 | AKR1B1 | Aldo-keto reductase family 1, B1 |
| 2.91 | 4.83 | 3.79 | 4.31×10−6 | 4.30×10−3 | AMY1B | Amylase, alpha 1B |
| 4.93 | 6.85 | 3.79 | 2.41×10−6 | 2.80×10−3 | SAA1 | Serum amyloid A1 |
| 4.05 | 5.97 | 3.78 | 2.71×10−7 | 6.00×10−4 | IKBKE | Inhibitor of kappa LPGEK B-cells epsilon |
| 4.36 | 6.27 | 3.77 | 1.01×10−6 | 1.30×10−3 | TNC | Tenascin C |
| 4.02 | 5.92 | 3.72 | 4.15×10−7 | 9.00×10−4 | C1QTNF1 | C1q and TNF related protein 1 |
| 5.78 | 7.61 | 3.54 | 1.04×10−7 | 4.00×10−4 | MMP7 | Matri × metallopeptidase 7 |
| 7.11 | 8.91 | 3.48 | 2.62×10−6 | 2.90×10−3 | EDN1 | Endothelin 1 |
| 7.47 | 9.24 | 3.41 | 2.37×10−6 | 2.80×10−3 | ICAM1 | Intercellular adhesion molecule 1 |
| 1.71 | 3.38 | 3.17 | 1.86×10−7 | 6.00×10−4 | MMP13 | Matri × metallopeptidase 13 |
| 4.04 | 5.69 | 3.15 | 1.00×10−6 | 1.30×10−3 | SGPP2 | Sphingosin × 10-1-phosphate phosphatase 2 |
| 6.40 | 7.99 | 3.01 | 7.30×10−7 | 1.10×10−3 | SEMA3C | Semaphorin 3C |
| 3.75 | 5.33 | 2.98 | 2.03×10−5 | 1.51×10−2 | CHI3L2 | Chitinase 3-like 2; DENN/MADD domain containing 2D |
| 3.6 | 5.17 | 2.97 | 1.45×10−5 | 1.18×10−2 | SOD2 | Supero xide dismutase 2, mitochondrial |
| 2.96 | 4.44 | 2.80 | 5.71×10−8 | 3.00×10−4 | KCCAT211 | Renal clear cell carcinoma-associated transcript 211 |
| 2.52 | 3.98 | 2.74 | 2.52×10−6 | 2.90×10−3 | LRRC55 | Leucine rich repeat containing 55 |
| 4.71 | 6.10 | 2.62 | 3.87×10−5 | 2.59×10−2 | SLITRK6 | SLIT and NTRK-like family, member 6 |
| 2.03 | 3.40 | 2.59 | 1.52×10−5 | 1.21×10−2 | KLHL38 | Kelch-like family member 38 |
| 4.30 | 5.68 | 2.59 | 5.30×10−7 | 1.00×10−3 | SLC2A12 | Solute carrier family 2 M, 12 |
| 2.97 | 4.32 | 2.54 | 2.82×10−5 | 1.97×10−2 | BBO ×1 | Gamma-butyrobetaine hydro xylase |
| 2.99 | 4.32 | 2.51 | 1.41×10−5 | 1.17×10−2 | TNFSF15 | Tumor necrosis factor (ligand) superfamily, member 15 |
| 3.70 | 5.00 | 2.46 | 3.69×10−5 | 2.51×10−2 | GBP1 | Guanylate binding protein 1, interferon-inducible |
| 5.67 | 6.92 | 2.37 | 1.26×10−5 | 1.11×10−2 | NFKBIA | NFK light polypeptide GE in B-cells inhibitor, alpha |
| 5.37 | 6.60 | 2.35 | 4.67×10−6 | 4.50×10−3 | CTSS | Cathepsin S |
| 3.45 | 4.66 | 2.31 | 1.40×10−5 | 1.17×10−2 | FIBIN | Fin bud initiation factor homolog (zebrafish) |
| 4.92 | 6.10 | 2.27 | 7.08×10−5 | 4.27×10−2 | NFE2L3 | Nuclear factor, erythroid 2-like 3 |
| 4.12 | 5.29 | 2.25 | 2.48×10−5 | 1.76×10−2 | KRT6B | Keratin 6B, type II |
| 3.78 | 4.89 | 2.17 | 6.63×10−5 | 4.05×10−2 | ATP6V1C2 | ATPase, H+ transporting, lysosomal 42kDa V1 sub C2 |
| 6.24 | 7.32 | 2.12 | 2.89×10−6 | 3.20×10−3 | IFNGR1 | Interferon gamma receptor 1 |
| 3.38 | 4.42 | 2.05 | 3.43×10−5 | 2.36×10−2 | CYP7B1 | Cytochrome P450, family 7, sub B, polypeptide 1 |
| 5.16 | 6.19 | 2.04 | 1.99×10−5 | 1.51×10−2 | LACC1 | Laccase domain containing 1 |
| 6.41 | 5.35 | −2.08 | 4.62×10−5 | 2.97×10−2 | CD14 | CD14 molecule |
| 6.21 | 4.98 | −2.35 | 7.93×10−5 | 4.56×10−2 | P2RY2 | Purinergic receptor P2Y, G-protein coupled, 2 |
| 9.25 | 8.01 | −2.36 | 1.22×10−5 | 1.09×10−2 | GLYATL2 | Glycin × 10-N-acyltransferas × 10-like 2 |
| 4.08 | 2.78 | −2.46 | 1.98×10−7 | 6.00×10−4 | STAC2 | SH3 and cysteine rich domain 2 |
| 5.98 | 4.61 | −2.59 | 1.48×10−5 | 1.19×10−2 | SLC15A2 | Solute carrier family 15, member 2 |
| 6.04 | 4.62 | −2.69 | 3.30×10−6 | 3.50×10−3 | TF | Transferrin |
| 4.85 | 3.4 | −2.74 | 4.86×10−5 | 3.08×10−2 | KRT4 | Keratin 4, type II |
| 8.11 | 6.61 | −2.83 | 2.08×10−5 | 1.52×10−2 | CRISP3 | Cystein × 10-rich secretory protein 3 |
| 7.51 | 5.96 | −2.93 | 2.20×10−6 | 2.70×10−3 | SPDEF | SAM pointed DC ETS transcription factor |
| 5.31 | 3.63 | −3.20 | 6.33×10−6 | 5.80×10−3 | SCGB2A2 | Secretoglobin, family 2A, member 2 |
| 6.76 | 4.92 | −3.59 | 1.48×10−7 | 5.00×10−4 | CLCA2 | Chloride channel accessory 2 |
The data are presented as official gene symbol, gene description, bi-weighted averages (n=3), fold change P-value and FDR P-value. Avg, average; FDR, false discovery rate.
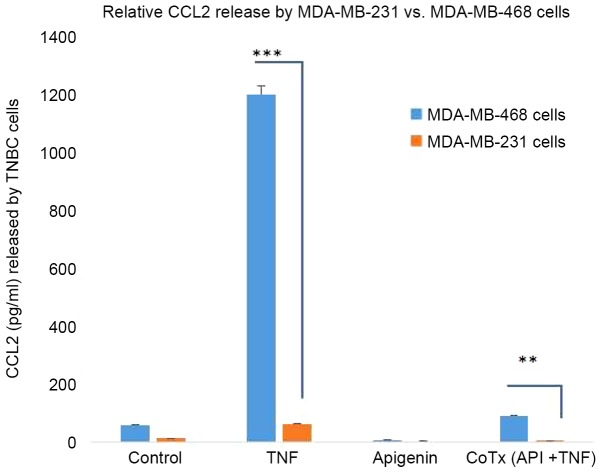
The effects of apigenin on modifying TNFα induced genes are presented in Table II. The table provides data on averaged signals, processed data, and percent reduction of TNFα treated cells. The largest upward differential shift was for CCL2 (+61.86-FC, false discovery rate (FDR) P-value <0.0001); which was down regulated by apigenin (to +10.71 FC vs. Control, FDR P-value <0.001), equivalent to an 83% reduction. The TNFα deferentially up-regulated transcripts were reduced by apigenin included; CXCL10, C3, PGLYRP4, IL22RA2, KMO, IL7R, ROS1,CFB, IKBKe, SLITRK6 (a checkpoint target) and MMP13 Our previous studies in MDA-MB-231 cells according to both mRNA and protein levels for CCL2 was meager in comparison. In order to confirm a heightened level in this particular cell line, and ELISA was conducted on both cell lines for all four groups (Fig. 4). These findings match the current microarray data, where CCL2 release in MDA-MB-468 cells was extremely high in concentration in comparison to MDA-MB-231 cells.
Table II.
Differential whole transcriptome changes upregulated by TNF-α (40 ng/ml) and downregulated by apigenin (40 µM) in MM-468 cells.
| Ctrl vs. TNF (differential) | TNF vs. Apig +TNF (differential) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| TNF vs. Apig+TNF (% reduction) | Symbol | Control signal Avg (log2) | TNF signal Avg (log2) | Apigenin+TNF signal Avg (log2) | Dir | FC | P-value | FDR P-value | Dir | FC | P-value | FDR P-value |
| −83 | CCL2 | 2.52 | 8.47 | 5.94 | ↑ | 61.86 | 2.37×10−10 | 3.82×10−6 | ↓ | −5.78 | 3.33×10−6 | 5.70×10−3 |
| −74 | CXCL10 | 2.41 | 7.29 | 5.32 | ↑ | 29.40 | 1.80×10−12 | 8.70×10−8 | ↓ | −3.90 | 5.29×10−8 | 5.00×10−4 |
| −76 | C3 | 4.75 | 7.45 | 5.40 | ↑ | 6.50 | 4.83×10−9 | 4.18×10−5 | ↓ | −4.16 | 6.13×10−8 | 5.00×10−4 |
| −67 | PGLYRP4 | 3.57 | 6.20 | 4.60 | ↑ | 6.18 | 1.10×10−7 | 4.00×10−4 | ↓ | −3.04 | 6.08×10−5 | 2.50×10−2 |
| −82 | KMO | 5.12 | 7.71 | 5.28 | ↑ | 6.02 | 7.79×10−7 | 1.10×10−3 | ↓ | −5.40 | 6.09×10−6 | 8.60×10−3 |
| −69 | AMY1B | 2.72 | 5.27 | 3.56 | ↑ | 5.86 | 2.80×10−7 | 6.00×10−4 | ↓ | −3.26 | 2.74×10−5 | 1.57×10−2 |
| −76 | IL22RA2 | 4.30 | 6.78 | 4.70 | ↑ | 5.57 | 7.89×10−7 | 1.1.0×10−3 | ↓ | −4.23 | 8.92×10−6 | 1.02×10−2 |
| −68 | CFB | 4.46 | 6.69 | 5.06 | ↑ | 4.69 | 1.09×10−7 | 4.00×10−4 | ↓ | −3.09 | 1.96×10−6 | 4.30×10−3 |
| −56 | ABCC4 | 4.32 | 6.48 | 5.29 | ↑ | 4.48 | 5.63×10−9 | 4.18 ×10−5 | ↓ | −2.29 | 1.70×10−5 | 1.25×10−2 |
| −76 | IL7R | 3.37 | 5.49 | 3.45 | ↑ | 4.33 | 3.71×10−7 | 8.00×10−4 | ↓ | −4.10 | 9.06×10−7 | 2.90×10−3 |
| −74 | ROS1 | 3.98 | 6.07 | 4.15 | ↑ | 4.27 | 8.37×10−7 | 1.20×10−3 | ↓ | −3.79 | 1.00×10−5 | 1.02×10−2 |
| −69 | AMY1B | 2.64 | 4.58 | 2.93 | ↑ | 3.84 | 6.31×10−6 | 5.80×10−3 | ↓ | −3.13 | 4.55×10−5 | 2.07×10−2 |
| −50 | AKR1B1 | 4.81 | 6.74 | 5.74 | ↑ | 3.81 | 1.27×10−7 | 5.00×10−4 | ↓ | −2.00 | 1.00×10−4 | 3.46×10−2 |
| −68 | AMY1B | 2.91 | 4.83 | 3.14 | ↑ | 3.79 | 4.31×10−6 | 4.30×10−3 | ↓ | −3.23 | 9.18×10−5 | 3.05×10−2 |
| −59 | SAA1 | 4.93 | 6.85 | 5.56 | ↑ | 3.79 | 2.41×10−6 | 2.80×10−3 | ↓ | −2.45 | 7.36×10−5 | 2.75×10−2 |
| −51 | IKBKE | 4.05 | 5.97 | 4.94 | ↑ | 3.78 | 2.71×10−7 | 6.00×10−4 | ↓ | −2.05 | 2.00×10−4 | 4.09×10−2 |
| −64 | TNC | 4.36 | 6.27 | 4.82 | ↑ | 3.77 | 1.01×10−6 | 1.30×10−3 | ↓ | −2.74 | 6.37×10−6 | 8.60×10−3 |
| −133 | MMP13 | 1.71 | 3.38 | 1.64 | ↑ | 3.17 | 1.86×10−7 | 6.00×10−4 | ↓ | −3.32 | 1.54×10−7 | 9.00×10−4 |
| −64 | SEMA3C | 6.40 | 7.99 | 6.51 | ↑ | 3.01 | 7.30×10−7 | 1.10×10−3 | ↓ | −2.79 | 2.38×10−6 | 4.90×10−3 |
| −135 | CHI3L2 | 3.75 | 5.33 | 3.71 | ↑ | 2.98 | 2.03×10−5 | 1.51×10−2 | ↓ | −3.07 | 1.32×10−5 | 1.16×10−2 |
| −50 | KCCAT211 | 2.96 | 4.44 | 3.44 | ↑ | 2.80 | 5.71×10−8 | 3.00×10−4 | ↓ | −2.01 | 1.56×10−6 | 4.00×10−3 |
| −188 | SLITRK6 | 4.71 | 6.10 | 3.51 | ↑ | 2.62 | 3.87×10−5 | 2.59×10−2 | ↓ | −6.01 | 2.24×10−8 | 5.00×10−4 |
| −142 | BBOX1 | 2.97 | 4.32 | 2.88 | ↑ | 2.54 | 2.82×10−5 | 1.97×10−2 | ↓ | −2.71 | 1.04×10−5 | 1.02×10−2 |
| −147 | CTSS | 5.37 | 6.60 | 5.21 | ↑ | 2.35 | 4.67×10−6 | 4.50×10−2 | ↓ | −2.62 | 1.41×10−5 | 1.17×10−2 |
Differential whole transcriptome changes upregulated by TNF α (40 ng/ml) and downregulated by apigenin (40 µM) in MM-468 cells. Up and down arrows represent upregulation and downregulation, respectively. The data are presented as official gene symbol, bi-weighted averages (n=3), fold change, ANOVA P-value and FDR P-value. % Reduction in column 1 is derived from % FC Control vs. TNFα and Control vs. co-treatment. AMY1B, AMY1A amylase, alpha 1B (salivary); amylase, alpha 1C (salivary); amylase, alpha 1A (salivary); ABCC4, ATP binding cassette subfamily C member 4; BBOX1, butyrobetaine (gamma), 2-oxoglutarate dioxygenase (gamma-butyrobetaine hydroxylase) 1; CTSS, cathepsin S; CCL2, chemokine (C-C motif) ligand 2; CXCL10, chemokine (C-X-C motif) ligand 10; CHI3L2, DENND2D chitinase 3-like 2; DENN/MADD, domain containing 2D; C3, complement component 3; CFB, complement factor B; IKBKE, inhibitor of kappa light polypeptide gene enhancer in B-cells, kinase epsilon; IL22RA2, interleukin 22 receptor, alpha 2; IL7R, interleukin 7 receptor; KMO, kynurenine 3-monooxygenase (kynurenine 3-hydroxylase); MMP13, matrix metallopeptidase 13; PGLYRP4, peptidoglycan recognition protein 4; ROS1, ROS proto-oncogene 1, receptor tyrosine kinase; SEMA3C, sema domain, immunoglobulin domain (Ig), short basic domain, secreted, (semaphorin) 3C; SAA1, serum amyloid A1; SLITRK6, SLIT and NTRK-like family, member 6; TNC, tenascin C; FDR, false discovery rate; FC, fold change; Ctrl, control; Dir, direction.
Figure 4.
CCL2 released by untreated controls, TNFα (40 ng/ml), apigenin (40 µM) and CoTx [TNFα (40 ng/ml) + apigenin (40 µM)] after 24 h treatment in MDA-MB-231 and MDA-MB-468 cells at equal plating density. The data are expressed as CCL2 (pg/ml), and statistical differences between the same treatments on different cell lines were determined by one-way ANOVA followed by a Tukey's multiple comparisons test. A significant difference was found in the TNF treatment group and the CoTx (API+TNF) treatment group. **P<0.01; ***P<0.0001. TNF, tumor necrosis factor; CCL2, C-C motif chemokine ligand 2; API, apigenin; CoTx, co-treatment.
Discussion
Limited therapeutic options are available for TNBC patients and consequently can result in aggressive metastatic disease, with greater mortality rates in African American (AA) women, relative to Caucasian-American (33,34). This health disparity may arise due to diagnosis at later stages of the disease (35) or a predisposed racially distinct genetic or epigenetic profile (36,37) with a propensity toward an overactive oncogenic p38 MAPK, Wnt/β-catenin, IGF2/ERbeta signaling axis (38–40). Additional factors to a health disparity arising in AA women regarding TNBC include vitamin D deficiencies (41) socioeconomic factors, later stage diagnosis, obesity, or even breast feeding patterns (42–44).
As with all human cancers, late stage diagnosis is associated with greater mortality rates to which the immune system can play a critical role. In the case with solid tumors such as breast cancer, inflammatory like secretion of cytokines to the tumor microenvironment can drive infiltration of tumor-associated macrophages (TAMs) and neutrophils (TANs) which promote tumor survival, metastasis, invasion, angiogenesis, resistance and turn off host immune surveillance, all equating to poor survival rates (2,45–47). It is believed that use of drugs or natural compounds that can suppress oncogenic cytokines (e.g., CXCL1, CCL18, CCL8, CCL2, IL-4, IL-8, IL-6, etc.) (17,48–53) such as apigenin, EGCG or butein can curtail these biochemical driven events and provide therapeutic advantages against aggressive inflammatory breast cancers (54,55).
In the present study, an inflammatory profile was evoked by TNFα, where the highest induced transcript in MDA-MB-468 cells was CCL2, confirmed at both the mRNA and protein level. The rise in CCL2 is reported throughout the literature, where it serves to drive tumor invasion, metastasis, and recurrence (2,17). CCl2 expression is also fairly consistent among breast cancer subcategories: (luminal: ER+ and/or PR+) (56), HER2+ (27) or basal like TNBC cell lines (6,57,58). Given that our studies suggest a possible disparity with higher levels of CCL2 in the African American cell line MDA-MB-468 vs. MM-231, we reviewed oncomine.org Oncomine™ for CCL2 difference among races, finding no obvious difference between African American vs. Caucasian in this aspect. Similarly, in our work-we find no difference in baseline CCL2 levels in the two cell lines, with the disparity arising only with the treatment of TNFα which is an experimental model of inflammatory breast cancer. Future studies will be required to evaluate the inflammatory response across racially divergent breast cancer cell lines or tissues.
What we do know, however, is that compounds like apigenin that attenuate the CCL2/CCR2 axis would slow the aggressive nature of TNBC and hormone positive breast cancers (27,28) by attenuating invasion, metastasis, EMT and the development of drug resistance (59–62). CCL2 inhibitors have been tested in various tumors, tumor cells and xenograft models with CCL2 lowering effects brought about by losartan (63) anlotinib (64) imatinib (65) zoledronic acid (66) oroxylin A (67) aspirin (68) natural compounds in coffee (kahweol acetate, cafestol) (69) or conophylline from Ervatamia microphylla (70) which can reduce invasive inflammatory tumor infiltration. The mechanism of action for CCL2 reducing agents may center around the modification of upstream or downstream targets such as PLEK2/EGRF (71) HER2-EGF/HRG, PI3K-NF-kB axis (27) SRC, PKC (58) the neddylation pathway (72) or the well-known mitogen-activated protein kinases and phosphatidylinositol 3-kinase/Akt cell signaling pathways (73). While others have reported apigenin to have an effect on NF-kappaB/Snail pathway (74), pSTAT3, pERK or PI3K/pAkt (75), our previous studies suggest the effects of TNFα in TNBC cell lines, as it relates to CCL2 are driven through the higher expression of IKBK epsilon (31).
It is important to note that when studying the effects of natural compounds such as apigenin on the entire transcriptome of cancer cells, there will most always likely be changes in both directions for oncogenes and tumor suppressors, some of these changes would not be advantageous. In this work, for example, we show that apigenin suppressed the TNFα mediated rise in a potent tumor suppressor: CXCL10. While previous studies consistently that CXCL10 is up-regulated in normal vs. tumor tissue (76,77) this particular protein acts as the major tumor suppressor, evoked by IFN-γ treatment and somehow plays a role in the re-expression of MHC-1, PD-L1, the infiltration of anti-tumoral CD4(+) and CD8(+) T cells (78,79), NK cells, cytotoxic lymphocytes (CTLs) to the tumor to turn on immune surveillance and heighted survival odds in diverse human cancers (80–82). While the beneficial effects of apigenin in cancer are consistently reported, any compound that would turn off the CXCL9, −10, −11/CXCR3 axis could harm the host immunes system to destroy self-malignant tumor tissue (83).
In contrast, the current study shows that apigenin turns on host immune surveillance by its effect on reducing-TNFα induced SLITRK6. SKITRK 6 is a membrane receptor, which is elevated in many cancers [e.g., epithelial tumors, bladder, lung, breast, and glioblastoma (84,85)] and has been deemed an immune checkpoint for target amongst a relatively new class of drugs approved by the FDA (86). SLITRK6 is the target of an antibody drug conjugate AGS15E currently in phase I clinical trials, believed to reactivate the hosts immune surveillance against self-malignant cells (87). While it is outside the scope of discussion to elaborate on every transcript change, this work serves as a general framework for public genomic data evaluation. Re: Gene Expression Omnibus for public analysis at https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE133968.
Previously reported data clearly indicate the existence of disparity in the mortality rates associated with TNBC in African Americans, and there a need for initiatives to establish novel and effective therapies to target aggressive tumors marked by a propelling inflammatory component. Overall, we believe there is enough support to warrant clinical trials for the use of apigenin, as there is a growing body of researching showing its antitumor effects from multiple stand points from blocking mutagenic induced cancers [e.g., methyl-nitrosourea, methyl-n-nitro-N-nitrosoguanidine, benzo(a)pyrene or 2-aminoanthracene] (88) to inhibition of ornithine decarboxylase (89) and its overall antioxidant, anti-inflammatory effects (90,91). Data on the clinical efficacy of substances like apigenin for human use to reduce CLL2 will also need to be confirmed, as well as establishing its bioavailability, absorption, therapeutic concentration and application (prevention, treatment or for chemotherapy drug augmentation) (55,91–94).
Acknowledgements
Not applicable.
Funding
The present study was supported by the National Institute of Minority Health and Health Disparities of the National Institutes of Health (grant nos. U54 MD007582 and P20 MD006738).
Availability of data and materials
The datasets generated and/or analyzed during the current study are available in the Gene Expression Omnibus repository (https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE133968).
Authors' contributions
DB was involved in the conceptualization of the manuscript, conducted the primary research, methodology and data analysis. EM carried out the transcriptomic microarray study, data analysis, and wrote and critically edited the manuscript. KFAS was involved in the conceptualization, experimental design and data analysis, and manuscript preparation and critical revision of the manuscript. In addition, KFAS provided oversight management of the project, including consultation, research direction and was responsible for funds acquisition, and the provision of the resources. AH was involved in the conceptualization of the manuscript, the methodology, and involved in writing and critically editing the manuscript. ETO was involved in the conceptualization of the manuscript, involved in the methodology, data analysis, and was involved in writing and critically editing the manuscript.
Ethics approval and consent to participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Yoshimura T. The production of monocyte chemoattractant protein-1 (MCP-1)/CCL2 in tumor microenvironments. Cytokine. 2017;98:71–78. doi: 10.1016/j.cyto.2017.02.001. [DOI] [PubMed] [Google Scholar]
- 2.Lee S, Lee E, Ko E, Ham M, Lee HM, Kim ES, Koh M, Lim HK, Jung J, Park SY, Moon A. Tumor-associated macrophages secrete CCL2 and induce the invasive phenotype of human breast epithelial cells through upregulation of ERO1-α and MMP-9. Cancer Lett. 2018;437:25–34. doi: 10.1016/j.canlet.2018.08.025. [DOI] [PubMed] [Google Scholar]
- 3.Porrello A, Leslie PL, Harrison EB, Gorentla BK, Kattula S, Ghosh SK, Azam SH, Holtzhausen A, Chao YL, Hayward MC, et al. Factor XIIIA-expressing inflammatory monocytes promote lung squamous cancer through fibrin cross-linking. Nat Commun. 2018;9:1988. doi: 10.1038/s41467-018-04355-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mandal PK, Biswas S, Mandal G, Purohit S, Gupta A, Majumdar Giri A, Roy Chowdhury S, Bhattacharyya A. CCL2 conditionally determines CCL22-dependent Th2-accumulation during TGF-beta-induced breast cancer progression. Immunobiology. 2018;223:151–161. doi: 10.1016/j.imbio.2017.10.031. [DOI] [PubMed] [Google Scholar]
- 5.Yoshimura T. The chemokine MCP-1 (CCL2) in the host interaction with cancer: A foe or ally? Cell Mol Immunol. 2018;15:335–345. doi: 10.1038/cmi.2017.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liubomirski Y, Lerrer S, Meshel T, Rubinstein-Achiasaf L, Morein D, Wiemann S, Körner C, Ben-Baruch A. Tumor-stroma-inflammation networks promote pro-metastatic chemokines and aggressiveness characteristics in triple-negative breast cancer. Front Immunol. 2019;10:757. doi: 10.3389/fimmu.2019.00757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rotondi M, Coperchini F, Latrofa F, Chiovato L. Role of Chemokines in Thyroid Cancer Microenvironment: Is CXCL8 the Main Player? Front Endocrinol (Lausanne) 2018;9:314. doi: 10.3389/fendo.2018.00314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Al-Mazidi S, Alotaibi M, Nedjadi T, Chaudhary A, Alzoghaibi M, Djouhri L. Blocking of cytokines signalling attenuates evoked and spontaneous neuropathic pain behaviours in the paclitaxel rat model of chemotherapy-induced neuropathy. Eur J Pain. 2018;22:810–821. doi: 10.1002/ejp.1169. [DOI] [PubMed] [Google Scholar]
- 9.Khazali AS, Clark AM, Wells A. Inflammatory cytokine IL-8/CXCL8 promotes tumour escape from hepatocyte-induced dormancy. Br J Cancer. 2018;118:566–576. doi: 10.1038/bjc.2017.414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang J, Wang X, Wang Y, Li S, Wang X. Krüppel like factor 6 splice variant 1 (KLF6-SV1) overexpression recruits macrophages to participate in lung cancer metastasis by up-regulating TWIST1. Cancer Biol Ther. 2019;20:680–691. doi: 10.1080/15384047.2018.1550570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li F, Kitajima S, Kohno S, Yoshida A, Tange S, Sasaki S, Okada N, Nishimoto Y, Muranaka H, Nagatani N, et al. Retinoblastoma inactivation induces a protumoral microenvironment via enhanced CCL2 secretion. Cancer Res. 2019;79:3903–3915. doi: 10.1158/0008-5472.CAN-18-3604. [DOI] [PubMed] [Google Scholar]
- 12.Cheng Y, Li H, Deng Y, Tai Y, Zeng K, Zhang Y, Liu W, Zhang Q, Yang Y. Cancer-associated fibroblasts induce PDL1+ neutrophils through the IL6-STAT3 pathway that foster immune suppression in hepatocellular carcinoma. Cell Death Dis. 2018;9:422. doi: 10.1038/s41419-018-0458-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhang H, Yu Y, Zhou L, Ma J, Tang K, Xu P, Ji T, Liang X, Lv J, Dong W, et al. Circulating tumor microparticles promote lung metastasis by reprogramming inflammatory and mechanical niches via a macrophage-dependent pathway. Cancer Immunol Res. 2018;6:1046–1056. doi: 10.1158/2326-6066.CIR-17-0574. [DOI] [PubMed] [Google Scholar]
- 14.Liu X, Jin G, Qian J, Yang H, Tang H, Meng X, Li Y. Digital gene expression profiling analysis and its application in the identification of genes associated with improved response to neoadjuvant chemotherapy in breast cancer. World J Surg Oncol. 2018;16:82. doi: 10.1186/s12957-018-1380-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mano Y, Yoshio S, Shoji H, Tomonari S, Aoki Y, Aoyanagi N, Okamoto T, Matsuura Y, Osawa Y, Kimura K, et al. Bone morphogenetic protein 4 provides cancer-supportive phenotypes to liver fibroblasts in patients with hepatocellular carcinoma. J Gastroenterol. 2019;54:1007–1018. doi: 10.1007/s00535-019-01579-5. [DOI] [PubMed] [Google Scholar]
- 16.Bedini N, Cicchetti A, Palorini F, Magnani T, Zuco V, Pennati M, Campi E, Allavena P, Pesce S, Villa S, et al. Evaluation of mediators associated with the inflammatory response in prostate cancer patients undergoing radiotherapy. Dis Markers. 2018;2018:9128128. doi: 10.1155/2018/9128128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Heiskala M, Leidenius M, Joensuu K, Heikkila P. High expression of CCL2 in tumor cells and abundant infiltration with CD14 positive macrophages predict early relapse in breast cancer. Virchows Arch. 2019;474:3–12. doi: 10.1007/s00428-018-2461-7. [DOI] [PubMed] [Google Scholar]
- 18.Izumi K, Mizokami A. Suppressive role of androgen/androgen receptor signaling via chemokines on prostate cancer cells. J Clin Med. 2019;8:E354. doi: 10.3390/jcm8030354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Natsagdorj A, Izumi K, Hiratsuka K, Machioka K, Iwamoto H, Naito R, Makino T, Kadomoto S, Shigehara K, Kadono Y, et al. CCL2 induces resistance to the antiproliferative effect of cabazitaxel in prostate cancer cells. Cancer Sci. 2019;110:279–288. doi: 10.1111/cas.13876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang X, Yang X, Tsai Y, Yang L, Chuang KH, Keng PC, Lee SO, Chen Y. IL-6 mediates macrophage infiltration after irradiation via up-regulation of CCL2/CCL5 in non-small cell lung cancer. Radiat Res. 2017;187:50–59. doi: 10.1667/RR14503.1. [DOI] [PubMed] [Google Scholar]
- 21.He S, Zhang X. The rs1024611 in the CCL2 gene and risk of gynecological cancer in Asians: A meta-analysis. World J Surg Oncol. 2018;16:34. doi: 10.1186/s12957-018-1335-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Guan X, Liu Z, Zhang J, Jin X. Myeloid-derived suppressor cell accumulation in renal cell carcinoma is correlated with CCL2, IL-17 and IL-18 expression in blood and tumors. Adv Clin Exp Med. 2018;27:947–953. doi: 10.17219/acem/70065. [DOI] [PubMed] [Google Scholar]
- 23.Amann B, Perabo FG, Wirger A, Hugenschmidt H, Schultze-Seemann W. Urinary levels of monocyte chemo-attractant protein-1 correlate with tumour stage and grade in patients with bladder cancer. Br J Urol. 1998;82:118–121. doi: 10.1046/j.1464-410x.1998.00675.x. [DOI] [PubMed] [Google Scholar]
- 24.Saik OV, Nimaev VV, Usmonov DB, Demenkov PS, Ivanisenko TV, Lavrik IN, Ivanisenko VA. Prioritization of genes involved in endothelial cell apoptosis by their implication in lymphedema using an analysis of associative gene networks with ANDSystem. BMC Med Genomics. 2019;12(Suppl 2):S47. doi: 10.1186/s12920-019-0492-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Roblek M, Protsyuk D, Becker PF, Stefanescu C, Gorzelanny C, Glaus Garzon JF, Knopfova L, Heikenwalder M, Luckow B, Schneider SW, Borsig L. CCL2 is a vascular permeability factor inducing CCR2-dependent endothelial retraction during lung metastasis. Mol Cancer Res. 2019;17:783–793. doi: 10.1158/1541-7786.MCR-18-0530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yumimoto K, Sugiyama S, Mimori K, Nakayama KI. Potentials of C-C motif chemokine 2-C-C chemokine receptor type 2 blockers including propagermanium as anticancer agents. Cancer Sci. 2019;110:2090–2099. doi: 10.1111/cas.14075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Triulzi T, Forte L, Regondi V, Di Modica M, Ghirelli C, Carcangiu ML, Sfondrini L, Balsari A, Tagliabue E. HER2 signaling regulates the tumor immune microenvironment and trastuzumab efficacy. Oncoimmunology. 2019;8:e1512942. doi: 10.1080/2162402X.2018.1512942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Song M, Sasazuki S, Camargo MC, Shimazu T, Charvat H, Yamaji T, Sawada N, Kemp TJ, Pfeiffer RM, Hildesheim A, et al. Circulating inflammatory markers and colorectal cancer risk: A prospective case-cohort study in Japan. Int J Cancer. 2018;143:2767–2776. doi: 10.1002/ijc.31821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Grossman JG, Nywening TM, Belt BA, Panni RZ, Krasnick BA, DeNardo DG, Hawkins WG, Goedegebuure SP, Linehan DC, Fields RC. Recruitment of CCR2+ tumor associated macrophage to sites of liver metastasis confers a poor prognosis in human colorectal cancer. Oncoimmunology. 2018;7:e1470729. doi: 10.1080/2162402X.2018.1470729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Coniglio SJ. Role of tumor-derived chemokines in osteolytic bone metastasis. Front Endocrinol (Lausanne) 2018;9:313. doi: 10.3389/fendo.2018.00313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bauer D, Redmon N, Mazzio E, Soliman KF. Apigenin inhibits TNFalpha/IL-1alpha-induced CCL2 release through IKBK-epsilon signaling in MDA-MB-231 human breast cancer cells. PLoS One. 2017;12:e0175558. doi: 10.1371/journal.pone.0175558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mazzio EA, Lewis CA, Soliman KFA. Transcriptomic profiling of MDA-MB-231 cells exposed to boswellia serrata and 3-O-acetyl-B-boswellic acid; ER/UPR mediated programmed cell death. cancer genomics proteomics. 2017;14:409–425. doi: 10.21873/cgp.20051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Garlapati C, Joshi S, Sahoo B, Kapoor S, Aneja R. The persisting puzzle of racial disparity in triple negative breast cancer: Looking through a new lens. Front Biosci (Schol Ed) 2019;11:75–88. doi: 10.2741/s527. [DOI] [PubMed] [Google Scholar]
- 34.Newman LA, Jenkins B, Chen Y, Oppong JK, Adjei E, Jibril AS, Hoda S, Cheng E, Chitale D, Bensenhaver JM, et al. Hereditary susceptibility for triple negative breast cancer associated with western sub-saharan african ancestry: Results from an international surgical breast cancer collaborative. Ann Surg. 2019;270:484–492. doi: 10.1097/SLA.0000000000003459. [DOI] [PubMed] [Google Scholar]
- 35.Hossain F, Danos D, Prakash O, Gilliland A, Ferguson TF, Simonsen N, Leonardi C, Yu Q, Wu XC, Miele L, Scribner R. Neighborhood social determinants of triple negative breast cancer. Front Public Health. 2019;7:18. doi: 10.3389/fpubh.2019.00018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jiagge E, Jibril AS, Davis M, Murga-Zamalloa C, Kleer CG, Gyan K, Divine G, Hoenerhoff M, Bensenhave J, Awuah B, et al. Androgen receptor and ALDH1 expression among internationally diverse patient populations. J Glob Oncol. 2018;4:1–8. doi: 10.1200/JGO.18.00056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bassey-Archibong BI, Hercules SM, Rayner LGA, Skeete DHA, Smith Connell SP, Brain I, Daramola A, Banjo AAF, Byun JS, Gardner K, et al. Kaiso is highly expressed in TNBC tissues of women of African ancestry compared to Caucasian women. Cancer Causes Control. 2017;28:1295–1304. doi: 10.1007/s10552-017-0955-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Telonis AG, Rigoutsos I. Race disparities in the contribution of miRNA isoforms and tRNA-derived fragments to triple-negative breast cancer. Cancer Res. 2018;78:1140–1154. doi: 10.1158/0008-5472.CAN-17-1947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Torres-Luquis O, Madden K, N'Dri N M, Berg R, Olopade OF, Ngwa W, Abuidris D, Mittal S, Lyn-Cook B, Mohammed SI. LXR/RXR pathway signaling associated with triple-negative breast cancer in African American women. Breast Cancer (Dove Med Press) 2018;11:1–12. doi: 10.2147/BCTT.S185960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Austin D, Hamilton N, Elshimali Y, Pietras R, Wu Y, Vadgama J. Estrogen receptor-beta is a potential target for triple negative breast cancer treatment. Oncotarget. 2018;9:33912–33930. doi: 10.18632/oncotarget.26089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wu Y, Sarkissyan M, Clayton S, Chlebowski R, Vadgama JV. Association of vitamin D3 Level with breast cancer risk and prognosis in African-American and hispanic women. Cancers (Basel) 2017;9:E144. doi: 10.3390/cancers9100144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ma H, Ursin G, Xu X, Lee E, Togawa K, Duan L, Lu Y, Malone KE, Marchbanks PA, McDonald JA, et al. Reproductive factors and the risk of triple-negative breast cancer in white women and African-American women: A pooled analysis. Breast Cancer Res. 2017;19:6. doi: 10.1186/s13058-016-0799-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Siddharth S, Sharma D. Racial disparity and triple-negative breast cancer in African-American women: A multifaceted affair between obesity, biology, and socioeconomic determinants. Cancers (Basel) 2018;10:E514. doi: 10.3390/cancers10120514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dietze EC, Chavez TA, Seewaldt VL. Obesity and triple-negative breast cancer: Disparities, controversies, and biology. Am J Pathol. 2018;188:280–290. doi: 10.1016/j.ajpath.2017.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zhao X, Qu J, Sun Y, Wang J, Liu X, Wang F, Zhang H, Wang W, Ma X, Gao X, Zhang S. Prognostic significance of tumor-associated macrophages in breast cancer: A meta-analysis of the literature. Oncotarget. 2017;8:30576–30586. doi: 10.18632/oncotarget.15736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jeong H, Hwang I, Kang SH, Shin HC, Kwon SY. Tumor-associated macrophages as potential prognostic biomarkers of invasive breast cancer. J Breast Cancer. 2019;22:38–51. doi: 10.4048/jbc.2019.22.e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Valeta-Magara A, Gadi A, Volta V, Walters B, Arju R, Giashuddin S, Zhong H, Schneider RJ. Inflammatory breast cancer promotes development of M2 tumor-associated macrophages and cancer mesenchymal cells through a complex chemokine network. Cancer Res. 2019;79:3360–3371. doi: 10.1158/0008-5472.CAN-17-2158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wang N, Liu W, Zheng Y, Wang S, Yang B, Li M, Song J, Zhang F, Zhang X, Wang Q, Wang Z. CXCL1 derived from tumor-associated macrophages promotes breast cancer metastasis via activating NF-κB/SOX4 signaling. Cell Death Dis. 2018;9:880. doi: 10.1038/s41419-018-0876-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Liu Y, Zheng H, Li Q, Li S, Lai H, Song E, Li D, Chen J. Discovery of CCL18 antagonist blocking breast cancer metastasis. Clin Exp Metastasis. 2019;36:243–255. doi: 10.1007/s10585-019-09965-2. [DOI] [PubMed] [Google Scholar]
- 50.Little AC, Pathanjeli P, Wu Z, Bao L, Goo LE, Yates JA, Oliver CR, Soellner MB, Merajver SD. IL-4/IL-13 stimulated macrophages enhance breast cancer invasion via Rho-GTPase regulation of synergistic VEGF/CCL-18 signaling. Front Oncol. 2019;9:456. doi: 10.3389/fonc.2019.00456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Cassetta L, Fragkogianni S, Sims AH, Swierczak A, Forrester LM, Zhang H, Soong DYH, Cotechini T, Anur P, Lin EY, et al. Human tumor-associated macrophage and monocyte transcriptional landscapes reveal cancer-specific reprogramming, biomarkers, and therapeutic targets. Cancer Cell. 2019;35:588–602.e510. doi: 10.1016/j.ccell.2019.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gupta S, Jain A, Syed SN, Pflüger-Müller B, Leisegang MS, Weigert A, Brandes RP, Ebersberger I, Brüne B, Namgaladze D. IL-6 augments IL-4-induced polarization of primary human macrophages through synergy of STAT3, STAT6 and BATF transcription factors. Oncoimmunology. 2018;7:e1494110. doi: 10.1080/2162402X.2018.1494110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Xu X, Ye J, Huang C, Yan Y, Li J. M2 macrophage-derived IL6 mediates resistance of breast cancer cells to hedgehog inhibition. Toxicol Appl Pharmacol. 2019;364:77–82. doi: 10.1016/j.taap.2018.12.013. [DOI] [PubMed] [Google Scholar]
- 54.Tandon I, Sharma NK. Macrophage flipping from foe to friend: A matter of interest in breast carcinoma heterogeneity driving drug resistance. Curr Cancer Drug Targets. 2019;19:189–198. doi: 10.2174/1568009618666180628102247. [DOI] [PubMed] [Google Scholar]
- 55.Sudhakaran M, Sardesai S, Doseff AI. Flavonoids: New frontier for immuno-regulation and breast cancer control. Antioxidants (Basel) 2019;8:E103. doi: 10.3390/antiox8040103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Han R, Gu S, Zhang Y, Luo A, Jing X, Zhao L, Zhao X, Zhang L. Estrogen promotes progression of hormone-dependent breast cancer through CCL2-CCR2 axis by upregulation of Twist via PI3K/AKT/NF-κB signaling. Sci Rep. 2018;8:9575. doi: 10.1038/s41598-018-27810-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Dutta P, Sarkissyan M, Paico K, Wu Y, Vadgama JV. MCP-1 is overexpressed in triple-negative breast cancers and drives cancer invasiveness and metastasis. Breast Cancer Res Treat. 2018;170:477–486. doi: 10.1007/s10549-018-4760-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Yao M, Fang W, Smart C, Hu Q, Huang S, Alvarez N, Fields P, Cheng N. CCR2 chemokine receptors enhance growth and cell-cycle progression of breast cancer cells through SRC and PKC Activation. Mol Cancer Res. 2019;17:604–617. doi: 10.1158/1541-7786.MCR-18-0750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ling Z, Yang X, Chen X, Xia J, Cheng B, Tao X. CCL2 promotes cell migration by inducing epithelial-mesenchymal transition in oral squamous cell carcinoma. J Oral Pathol Med. 2019;48:477–482. doi: 10.1111/jop.12869. [DOI] [PubMed] [Google Scholar]
- 60.Xu W, Wei Q, Han M, Zhou B, Wang H, Zhang J, Wang Q, Sun J, Feng L, Wang S, et al. CCL2-SQSTM1 positive feedback loop suppresses autophagy to promote chemoresistance in gastric cancer. Int J Biol Sci. 2018;14:1054–1066. doi: 10.7150/ijbs.25349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wang T, Zhan Q, Peng X, Qiu Z, Zhao T. CCL2 influences the sensitivity of lung cancer A549 cells to docetaxel. Oncol Lett. 2018;16:1267–1274. doi: 10.3892/ol.2018.8769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sarin N, Engel F, Rothweiler F, Cinatl J, Michaelis M, Frötschl R, Fröhlich H, Kalayda GV. Key players of cisplatin resistance: towards a systems pharmacology approach. Int J Mol Sci. 2018;19:E767. doi: 10.3390/ijms19030767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Regan DP, Coy JW, Chahal KK, Chow L, Kurihara JN, Guth AM, Kufareva I, Dow SW. The angiotensin receptor blocker losartan suppresses growth of pulmonary metastases via AT1R-independent inhibition of CCR2 signaling and monocyte recruitment. J Immunol. 2019;202:3087–3102. doi: 10.4049/jimmunol.1800619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lu J, Zhong H, Chu T, Zhang X, Li R, Sun J, Zhong R, Yang Y, Alam MS, Lou Y, et al. Role of anlotinib-induced CCL2 decrease in anti-angiogenesis and response prediction for nonsmall cell lung cancer therapy. Eur Respir J. 2019;53:1801562. doi: 10.1183/13993003.01562-2018. [DOI] [PubMed] [Google Scholar]
- 65.Yao Z, Zhang J, Zhang B, Liang G, Chen X, Yao F, Xu X, Wu H, He Q, Ding L, Yang B. Imatinib prevents lung cancer metastasis by inhibiting M2-like polarization of macrophages. Pharmacol Res. 2018;133:121–131. doi: 10.1016/j.phrs.2018.05.002. [DOI] [PubMed] [Google Scholar]
- 66.Liu H, Wang SH, Chen SC, Chen CY, Lin TM. Zoledronic acid blocks the interaction between breast cancer cells and regulatory T-cells. BMC Cancer. 2019;19:176. doi: 10.1186/s12885-019-5379-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ku WT, Tung JJ, Lee TJ, Lai KC. Long-term exposure to oroxylin a inhibits metastasis by suppressing CCL2 in oral squamous cell carcinoma Cells. Cancers (Basel) 2019;11:E353. doi: 10.3390/cancers11030353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wang D, Yue DL, Wang D, Chen XF, Yin XY, Wang YP, Yang L, Zhang Y. Aspirin inhibits cell stemness of esophageal cancer by downregulation of chemokine CCL2. Zhonghua Zhong Liu Za Zhi. 2018;40:744–749. doi: 10.3760/cma.j.issn.0253-3766.2018.10.005. (In Chinese) [DOI] [PubMed] [Google Scholar]
- 69.Iwamoto H, Izumi K, Natsagdorj A, Naito R, Makino T, Kadomoto S, Hiratsuka K, Shigehara K, Kadono Y, Narimoto K, et al. Coffee diterpenes kahweol acetate and cafestol synergistically inhibit the proliferation and migration of prostate cancer cells. Prostate. 2019;79:468–479. doi: 10.1002/pros.23753. [DOI] [PubMed] [Google Scholar]
- 70.Ishii N, Araki K, Yokobori T, Hagiwara K, Gantumur D, Yamanaka T, Handa T, Tsukagoshi M, Igarashi T, Watanabe A, et al. Conophylline suppresses pancreatic cancer desmoplasia and cancer-promoting cytokines produced by cancer-associated fibroblasts. Cancer Sci. 2019;110:334–344. doi: 10.1111/cas.13847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Shen H, He M, Lin R, Zhan M, Xu S, Huang X, Xu C, Chen W, Yao Y, Mohan M, Wang J. PLEK2 promotes gallbladder cancer invasion and metastasis through EGFR/CCL2 pathway. J Exp Clin Cancer Res. 2019;38:247. doi: 10.1186/s13046-019-1250-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Zhou L, Jiang Y, Liu X, Li L, Yang X, Dong C, Liu X, Lin Y, Li Y, Yu J, et al. Promotion of tumor-associated macrophages infiltration by elevated neddylation pathway via NF-κB-CCL2 signaling in lung cancer. Oncogene. 2019;38:5792–5804. doi: 10.1038/s41388-019-0840-4. [DOI] [PubMed] [Google Scholar]
- 73.Ding M, He SJ, Yang J. MCP-1/CCL2 Mediated by autocrine loop of PDGF-BB promotes invasion of lung cancer cell by recruitment of macrophages via CCL2-CCR2 axis. J Interferon Cytokine Res. 2019;39:224–232. doi: 10.1089/jir.2018.0113. [DOI] [PubMed] [Google Scholar]
- 74.Tong J, Shen Y, Zhang Z, Hu Y, Zhang X, Han L. Apigenin inhibits epithelial-mesenchymal transition of human colon cancer cells through NF-κB/Snail signaling pathway. Biosci Rep. 2019;39:BSR20190452. doi: 10.1042/BSR20190452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Lee HH, Jung J, Moon A, Kang H, Cho H. Antitumor and anti-invasive effect of apigenin on human breast carcinoma through suppression of IL-6 expression. Int J Mol Sci. 2019;20:E3143. doi: 10.3390/ijms20133143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Xu M, Li D, Yang C, Ji JS. MicroRNA-34a inhibition of the TLR signaling pathway Via CXCL10 suppresses breast cancer cell invasion and migration. Cell Physiol Biochem. 2018;46:1286–1304. doi: 10.1159/000489111. [DOI] [PubMed] [Google Scholar]
- 77.Zhang J, Chen J, Guan GW, Zhang T, Lu FM, Chen XM. Expression and clinical significance of chemokine CXCL10 and its receptor CXCR3 in hepatocellular carcinoma. Beijing Da Xue Xue Bao Yi Xue Ban. 2019;51:402–408. doi: 10.19723/j.issn.1671-167X.2019.03.005. (In Chinese) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Guo J, Xiao Y, Iyer R, Lu X, Lake M, Ladror U, Harlan J, Samanta T, Tomlinson M, Bukofzer G, et al. Empowering therapeutic antibodies with IFN-α for cancer immunotherapy. PLoS One. 2019;14:e0219829. doi: 10.1371/journal.pone.0219829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Wu Y, Yuan L, Lu Q, Xu H, He X. Distinctive profiles of tumor-infiltrating immune cells and association with intensity of infiltration in colorectal cancer. Oncol Lett. 2018;15:3876–3882. doi: 10.3892/ol.2018.7771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Fang S, Xu T, Xiong M, Zhou X, Wang Y, Haydu LE, Ross MI, Gershenwald JE, Prieto VG, Cormier JN, et al. Role of immune response, inflammation, and tumor immune response-Related cytokines/chemokines in melanoma progression. J Invest Dermatol. 2019;139:2352–2358.e3. doi: 10.1016/j.jid.2019.03.1158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Nieto JC, Zamora C, Porcel JM, Mulet M, Pajares V, Muñoz-Fernandez AM, Calvo N, Espinosa I, Pascual-García M, Bielsa S, Vidal S. Migrated T lymphocytes into malignant pleural effusions: An indicator of good prognosis in lung adenocarcinoma patients. Sci Rep. 2019;9:2996. doi: 10.1038/s41598-018-35840-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Kang SH, Keam B, Ahn YO, Park HR, Kim M, Kim TM, Kim DW, Heo DS. Inhibition of MEK with trametinib enhances the efficacy of anti-PD-L1 inhibitor by regulating anti-tumor immunity in head and neck squamous cell carcinoma. Oncoimmunology. 2019;8:e1515057. doi: 10.1080/2162402X.2018.1515057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Tokunaga R, Zhang W, Naseem M, Puccini A, Berger MD, Soni S, McSkane M, Baba H, Lenz HJ. CXCL9, CXCL10, CXCL11/CXCR3 axis for immune activation-A target for novel cancer therapy. Cancer Treat Rev. 2018;63:40–47. doi: 10.1016/j.ctrv.2017.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Morrison K, Challita-Eid PM, Raitano A, An Z, Yang P, Abad JD, Liu W, Lortie DR, Snyder JT, Capo L, et al. Development of ASG-15ME, a novel antibody-drug conjugate targeting SLITRK6, a new urothelial cancer biomarker. Mol Cancer Ther. 2016;15:1301–1310. doi: 10.1158/1535-7163.MCT-15-0570. [DOI] [PubMed] [Google Scholar]
- 85.Lin JK, Chen YC, Huang YT, Lin-Shiau SY. Suppression of protein kinase C and nuclear oncogene expression as possible molecular mechanisms of cancer chemoprevention by apigenin and curcumin. J Cell Biochem Suppl. 1997;28-29:39–48. doi: 10.1002/(SICI)1097-4644(1997)28/29+<39::AID-JCB5>3.0.CO;2-X. [DOI] [PubMed] [Google Scholar]
- 86.Alhalabi O, Rafei H, Shah A, Siefker-Radtke A, Campbell M, Gao J. Targeting advanced urothelial carcinoma-developing strategies. Curr Opin Oncol. 2019;31:207–215. doi: 10.1097/CCO.0000000000000532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Sanford T, Porten S, Meng MV. Molecular analysis of upper tract and bladder urothelial carcinoma: Results from a microarray comparison. PLoS One. 2015;10:e0137141. doi: 10.1371/journal.pone.0137141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Birt DF, Walker B, Tibbels MG, Bresnick E. Anti-mutagenesis and anti-promotion by apigenin, robinetin and indole-3-carbinol. Carcinogenesis. 1986;7:959–963. doi: 10.1093/carcin/7.9.1617. [DOI] [PubMed] [Google Scholar]
- 89.Birt DF, Mitchell D, Gold B, Pour P, Pinch HC. Inhibition of ultraviolet light induced skin carcinogenesis in SKH-1 mice by apigenin, a plant flavonoid. Anticancer Res. 1997;17:85–91. [PubMed] [Google Scholar]
- 90.Sharma A, Ghani A, Sak K, Tuli HS, Sharma AK, Setzer WN, Sharma S, Das AK. Probing into therapeutic anti-cancer potential of apigenin: Recent trends and future directions. recent pat inflamm Allergy Drug Discov. 2019 Aug 16; doi: 10.2174/1872213X13666190816160240. doi: 10.2174/1872213X13666190816160240 (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 91.Ginwala R, Bhavsar R, Chigbu DI, Jain P, Khan ZK. Potential role of flavonoids in treating chronic inflammatory diseases with a special focus on the anti-inflammatory activity of apigenin. Antioxidants (Basel) 2019;8:E35. doi: 10.3390/antiox8020035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Chen Z, Tian D, Liao X, Zhang Y, Xiao J, Chen W, Liu Q, Chen Y, Li D, Zhu L, Cai S. Apigenin combined with gefitinib blocks autophagy flux and induces apoptotic cell death through inhibition of HIF-1α, c-Myc, p-EGFR, and glucose metabolism in EGFR L858R+T790M-mutated H1975 cells. Front Pharmacol. 2019;10:260. doi: 10.3389/fphar.2019.00260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Chen X, Xu H, Yu X, Wang X, Zhu X, Xu X. Apigenin inhibits in vitro and in vivo tumorigenesis in cisplatin-resistant colon cancer cells by inducing autophagy, programmed cell death and targeting m-TOR/PI3K/Akt signalling pathway. J BUON. 2019;24:488–493. [PubMed] [Google Scholar]
- 94.Gao AM, Zhang XY, Hu JN, Ke ZP. Apigenin sensitizes hepatocellular carcinoma cells to doxorubic through regulating miR-520b/ATG7 axis. Chem Biol Interact. 2018;280:45–50. doi: 10.1016/j.cbi.2018.01.009. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and/or analyzed during the current study are available in the Gene Expression Omnibus repository (https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE133968).