Abstract
The objective of this study was to investigate the association between objectively measured patterns of sedentary behavior (SB) and physical activity (PA) and frailty status in Japanese community-dwelling older adults. Data was from 65-75 years older adults from the baseline of Itoshima Frail Study were used. Frailty was assessed using a Japanese version of the FRAIL scale. SB and PA were measured using an accelerometer. Multinomial logistic regression and receiver operating characteristic curve analyses were used to investigate the associations of SB and PA patterns with frailty status. Of the total 819 older adults, half were female (51.8%). The prevalence of robust, pre-frailty and frailty was 60.2%, 27.8%, and 12.0%, respectively. SB variables including total sedentary time, sedentary time in bouts of ≥ 10 min and ≥ 30 min, and mean sedentary bout duration were not associated with frailty status. Except LPA and moderate-to-vigorous physical activity (MVPA) in bouts of < 10 min, PA variables including total MVPA time, MVPA in bouts of ≥ 10 min (bouted MVPA), and steps were significantly associated with lower prevalence of frailty. Area under the curves (AUCs) of total MVPA time, bouted MVPA, and steps were 0.64 (P < 0.001), 0.67 (P < 0.001), and 0.66 (P < 0.001), respectively. The optimal cut-off value of total MVPA time, bouted MVPA, and steps to discriminate between frailty and non-frailty were 43.25 min/day, 9.13 min/day, and 3841 steps/day, respectively. Higher levels of total MVPA time, bouted MVPA, and daily steps were negatively associated with frailty. Lower amounts of bouted MVPA (70 min/week) or steps (4000 steps/day) may be achievable initial targets in older adults for frailty management.
Key points.
This is the first study to investigate the associations between objective patterns of SB, PA and frailty status screened by the FRAIL-J in Japanese community-dwelling older adults.
Higher levels of total MVPA time, bouted MVPA, and steps were negatively associated with frailty.
Bouted MVPA might be more effective on frailty management compared to sporadic MVPA.
9.13 min/day of bouted MVPA, 3841 steps/day of daily step, and 43.25 min/day of total MVPA, represent the optimal cut-off value to discriminate between frailty and non-frailty.
Key words: Frailty, FRAIL scale, older adults, sedentary behavior, physical activity, step
Introduction
Frailty is defined as a medical syndrome that can increase the risk of adverse outcomes including all-cause mortality (Chang and Lin, 2015), hospitalization (Kojima, 2016), and disability (Vermeiren et al., 2016). Meanwhile, previous studies have demonstrated that frailty is a dynamic condition and frailty status can transition between better and worse over time (Lee et al., 2014). This aspect of frailty presents an opening for potential preventative and restorative interventions. Lifestyle is considered one of the main keystones in the development of frailty, and a healthy lifestyle can help older adults to manage frailty (Feng et al., 2017). As a common component of lifestyle, daily sedentary behavior (SB) and physical activity (PA) may play an important role in the development of frailty (Kehler et al., 2018a; 2018b).
One recent review summarized the epidemiological evidence concerning the impact of SB on frailty (Kehler et al., 2018b). In this review, almost all studies used subjective assessment of SB such as TV watching time or self-reported sedentary or inactive lifestyle found a significant negative association between SB and frailty indicted that promoting physical activity may be a feasible way to prevent frailty. However, evidence of the association between objective assessment of SB and frailty was inconsistent. Of all studies that examined the association between objectively measured total sedentary time and frailty among community-dwelling older adults (Bastone Ade et al., 2015; Blodgett et al., 2015; Castaneda-Gameros et al., 2018; Del Pozo-Cruz et al., 2017; Jansen et al., 2015; Kehler et al., 2018a; Manas et al., 2018; Nagai et al., 2018; Song et al., 2015), only three studies found significant associations (Blodgett et al., 2015; Del Pozo-Cruz et al., 2017; Song et al., 2015). One reason causing this inconsistency might be most studies conventionally operationalize sedentary time as total sedentary time without considering SB accumulation patterns. Indeed, increasing evidence showed that the SB accumulated in different length bouts (prolonged uninterrupted bouts vs. short bouts) might result in distinct health outcomes (Bellettiere et al., 2019; Diaz et al., 2017). In a recent study of Toledo Healthy Study on Aging (THSA), no significant association was found between the duration of SB bouts lasting ≥ 10 min and the score of the Frailty Trait Scale (Del Pozo-Cruz et al., 2017). However, a significant association was found between the duration of SB bouts lasting ≥ 30 min and the levels of frailty in females from the National Health and Nutrition Examination Survey (NHANES) (Kehler et al., 2018a, Kehler et al., 2019). Therefore, further studies are needed to examine whether the association between SB and frailty depends on the bout length definition.
As for the association between objective assessment of PA and frailty, a recent review found that a higher amount of total moderate-to-vigorous physical activity (MVPA) time was consistently associated with frailty (Kehler and Theou, 2019). Although WHO recommended that older adults aged 65 years and older should accumulate at least 150 minutes of MVPA per week in bouts ≥ 10 min (WHO, 2010), meeting such recommendation may be challenging, especially in the older adult with frailty (Blodgett et al., 2015). A recent systematic review found that both MVPA in bouts of ≥ 10 min (bouted MVPA) and <10 min (sporadic MVPA) is associated with favorable health outcomes such as BMI, body fatness, and all-cause mortality, which suggest bouts of any duration may have health-enhancing effects (Jakicic et al., 2019). Accordingly, the recent U.S. guidelines that bouted or sporadic MVPA can provide important benefits and highlight the potential health benefits of light physical activity (LPA) in older adults (Piercy et al., 2018). However, it is still less clear how bouted or sporadic MVPA and LPA are related to frailty.
Japan has the largest proportion of the elderly population and has the most rapid aging rate than that of any other country, while the life expectancy is the highest in the world (Arai et al., 2015). Moreover, according to a recent systematic review and meta-analysis, the prevalence of frailty in Japan was lower than in other countries (7.5% vs 9.9%) (Kojima et al., 2017). Comprehensively examine the associations of objectively assessed different patterns of SB and PA with frailty in Japan may provide a unique insight into the management of frailty. Thus, the purposes of the present study were to investigate if different SB, PA patterns and the number of steps are associated with frailty status and tried to determine the optimal cut-off value of PA and SB variables, and steps to discriminate between frailty and non-frailty in Japanese community-dwelling older adults.
Methods
Participants
Cross-sectional data were derived from the baseline survey of the Itoshima Frail Study (IFS), which was carried out from September to December in 2017. The design of IFS has been described in detail elsewhere (Chen et al., 2020). Briefly, the IFS is an ongoing community-based prospective study in Itoshima City, located in northwest Japan. Its aiming is to explore modifiable lifestyle factors causing/protecting against frailty. The inclusion criteria of IFS were primary residents of Itoshima city, aged 65-75 years, who were not certified as requiring nursing care by the National Long-term Care Insurance System. Of approximately 10,000 older adults, 5,000 were randomly selected according to the residential area, sex, and age. A set of study information sheets and questionnaires were mailed to subjects, inviting them to community centers for further assessments. Of the 5,000 individuals contacted, 1,631 submitted questionnaires and 949 completed further assessments, for a response rate of 32.6% and 19.0%, respectively. Of the 949 subjects, we excluded 19 individuals who did not have accelerometer data, 69 individuals with less than 4 days of valid accelerometer data, and 42 individuals with missing data of covariates. This study was approved by the Institutional Review Board of the K. University, Japan. All participants provided written informed consent.
Frailty measure
Frailty status was assessed by a Japanese version of the FRAIL scale (FRAIL-J, Table 1), which has shown good reliability and construct validity in our previous study (Chen et al., 2020). The FRAIL-J includes two biological components (fatigue and loss of weight), two functional components (resistance and ambulation) and one deficit accumulation component (illness). The total score ranges from 0-5 points, with one point assigned to each component. Although the original FRAIL scale set a 3-point score as the cut-off point to identify frailty, our previous study showed that, compared to a 3-point cut-off, a 2-point cut-off had better criterion validity and could be the optimal one in Japanese older adults (Chen et al., 2020). Indeed, a 2-point cutoff for the FRAIL scale was also recommended in the Brazilian and Chinese versions (Aprahamian et al., 2017, Dong et al., 2018). Therefore, in the present study, a score of 0 would indicate robust participants, 1 as pre-frailty, and 2-5 as frailty.
Table 1.
Japanese version of FRAIL scale.
| FRAIL-J | |
|---|---|
| Fatigue | In the last 2 weeks have you felt tired without a reason? 1 = Yes, 0 = No. |
| Resistance | Do you normally climb stairs without using handrail or wall for support? 0 = Yes, 1 = No. |
| Ambulation | By yourself and not using aids, do you have any difficulty walking 1 km without resting? 1 = Yes, 0 = No. |
| Illness | The illnesses include hypertension, diabetes, cancer (other than a minor skin cancer), chronic lung disease, heart attack, congestive heart failure, angina, asthma, arthritis, stroke, and kidney disease. The total illnesses (0–11) are recoded as 0–4 = 0 and 5–11 = 1. |
| Loss of weight | Unintentional weight loss > 2–3 kg in the past 6 months. 1 = Yes, 0 = No. |
Frail-J, Japanese FRAIL scale
SB and PA variables
SB and PA were measured objectively using a waist-mounted, tri-axial, accelerometer (Active style Pro HJA-350IT, Omron Healthcare, Kyoto, Japan) for seven consecutive days after the health assessment. The previous study reported that METs determined by the Active Style Pro HJA-350IT were closely correlated with METs calculated by the indirect calorimetry, with an average percentage of differences less than 10%. Accordingly, the Active Style Pro directly estimates the intensity of activities as METs (Ohkawara et al., 2011). Participants were instructed by trained personnel to wear the accelerometer on either side of their waist during their waking hours, and to remove the device only before going to bed or when engaging in water activities. Simple instruction and a log diary were also provided to encourage compliance with accelerometer protocols. Data were recorded in 60-s periods for the data analysis. The SAS macro program provided by the National Cancer Institute (National Cancer Institute, 2015) was modified for our accelerometer to compute daily non-wear time, as described elsewhere (Chen et al., 2017, Honda et al., 2016). Non-wearing time was defined as at least 60 consecutive min of no activity, with an allowable 2 min to reach up to 1.0 METs. Data for participants with at least 4 valid wear days (at least 10 h of wear time per day) were included in the analysis.
Sedentary time was defined as a minute in which activity intensity was ≤ 1.5 METs, for example, resting in the sitting and lying or using computer (Ohkawara et al., 2011). A sedentary bout was defined as a period of sedentary time accumulated without interruption. Previous studies used 10 or 30 min/day as the cut-off value to define prolonged sedentary duration (Del Pozo-Cruz et al., 2017; Kehler et al., 2018a), however, a consensus is still lacking on the best measure of sedentary accumulation patterns. Therefore, apart from 10-min and 30-min bout of sedentary time, mean sedentary bout duration was also calculated by dividing total sedentary time by the total number of sedentary bouts in the present study, with higher values indicating more prolonged accumulation patterns, whereas lower values indicated more interrupted patterns.
LPA was defined as activities of 1.5-3 METs such as laundry, dishwashing, or vacuuming (Ohkawara et al., 2011). MVPA was defined as activities of ≥ 3 METs including walking, jogging, and ascending or descending stairs (Ohkawara et al., 2011). Bouted MVPA was defined as ≥ 10 consecutive min, with an allowance for up to 2 min out of 10 to drop below the MVPA intensity threshold. This was consistent with the values recommended by the WHO physical activity guideline (WHO, 2010). Sporadic MVPA was defined as any MVPA accumulated in < 10 min. In addition, steps per day were also calculated.
Other variables
Socio-demographic characteristics including age, gender, education, living alone (yes/no), smoking (current smoker or not), and drinking (current drinker or not) were collected using questionnaires. Polypharmacy was defined as taking 5 or more prescription medications (yes/no). Cognitive function was measured using the Japanese version of the Montreal Cognitive Assessment (MoCA) (Fujiwara et al., 2010), conducted by the public nurses and trained staff. Instrumental activities of daily living (IADL) were measured using the 5-item subscale of the Tokyo Metropolitan Institute of Gerontology Index of Competence (Koyano et al., 1991). The Japanese version of the Pittsburgh Sleep Quality Index (PSQI) was used to assess sleep (Doi et al., 2000)
Statistical analysis
Descriptive data were summarized means ± standard deviation (SD) for continuous variables and as frequency (percentages) for categorical variables. Differences across frailty status were tested with the Jonckheere-Terpstra trend test for continuous variables, and the Cochran-Armitage trend test for categorical variables. In preliminary analyses, the effects of interaction between SB, PA variables and sex were examined by entering the interaction terms (exposure variables * sex) in age and sex adjusted logistic regression model and all interaction terms were not statistically significant (all P > 0.05). Therefore, all analyses were conducted with men and women together. Multivariable-adjusted multinomial logistic regression analysis analyses were used to investigate the associations between SB, PA patterns and frailty status. The following two models were used to adjust for confounding factors: model 1 included age, sex, education, living alone, drinking and smoking status, polypharmacy, MoCA score, PSQI score, IADL, and accelerometer wear time; model 2 included factors in model 1 plus total MVPA time to SB variables (model 2a), or total sedentary time to PA variables (model 2b). In addition, in order to determine if bouted and sporadic MVPA were independently associated with frailty status, sporadic MVPA and bouted MVPA were added to model 2c. The variance inflation factor (VIF) for all variables was calculated to detect the presence of collinearity. Each covariate had a VIF below 3 in the fully adjusted model 2, which is considered acceptable. Receiver operating characteristic curve (ROC) analysis was used to define the cut-off value of time spent in specific levels of PA and SB variables to differentiate between being frailty and non-frailty when a significant association was observed in the logistic regression analysis. Area under the curve (AUC) represents the ability of a variable in differentiating between frailty and non-frailty. AUC values of > 0.80 are considered good, 0.70-0.79 fair, and < 0.70 poor (Metz, 1978). Optimal cut-off value was determined by the maximum value of the Youden index. ROC analyses were conducted using MedCalc version 19.1 (MedCalc Software, Ostend, Belgium) and other analyses were conducted using SAS version 9.4 (SAS Institute Inc., Cary, N.C., USA). The statistical significance was set at α = 0.05 in two-sided tests.
Results
The characteristics of the study population are presented in Table 2. Of the total 819 older adults, the mean age was 70.9 ± 3.1 years and a half were female (51.8%). In all participants, the prevalence of robust, pre-frailty and frailty was 60.2%, 27.8%, and 12.0%, respectively. On average, participants with frailty were more likely to be women, have a higher ratio of polypharmacy, lower MoCA score, higher PSQI score, shorter total MVPA time and bouted MVPA, and lower daily steps.
Table 2.
Characteristics of the total sample according to frailty status by the FRAIL-J scale.
| Variables | Total (n=819) |
Frailty Status | |||
|---|---|---|---|---|---|
| Robust (n=493) |
Pre-frailty (n=228) |
Frailty (n=98) |
P for trend | ||
| Age, year | 70.9±3.1 | 70.9±3.1 | 70.9±3.1 | 71.1±3.1 | 0.76 |
| Gender, women | 424 (51.8) | 239 (48.5) | 123 (53.9) | 62 (63.7) | 0.006 |
| Living alone | 80 (9.8) | 44 (8.9) | 26 (11.4) | 10 (10.2) | 0.44 |
| Current drinker | 410 (50.1) | 258 (52.3) | 108 (47.4) | 44 (44.9) | 0.10 |
| Current smoker | 59 (7.2) | 44 (8.9) | 9 (4.0) | 6 (6.12) | 0.07 |
| Polypharmacy, ≥5 | 126 (15.4) | 53 (10.8) | 43 (18.9) | 30 (30.6) | <0.001 |
| IADL, ≥1 | 41 (5.0) | 22 (4.5) | 11 (4.8) | 8 (8.16) | 0.19 |
| Education, year | 12.9±2.4 | 12.9±2.4 | 12.9±2.3 | 12.7±2.3 | 0.39 |
| MoCA score, point | 24.3±2.9 | 24.5±2.9 | 24.1±2.9 | 23.6±3.3 | 0.001 |
| PSQI score, point | 4.1±2.8 | 3.8±2.6 | 4.2±3.0 | 5.3±3.2 | <0.001 |
| Total sedentary time, min/day | 456.9±111.3 | 460.1±113.0 | 450.7±104.4 | 455.3±118.7 | 0.49 |
| 10-min bout of sedentary time, min/day | 328.1±113.8 | 331.2±115.6 | 321.5±105.1 | 327.7±124.1 | 0.65 |
| 30-min bout of sedentary time, min/day | 179.7±94.9 | 181.6±96.8 | 175.7±87.3 | 179.1±102.7 | 0.68 |
| Mean sedentary bout duration, min/day | 4.1±0.7 | 4.1±0.7 | 4.1±0.7 | 4.2±0.8 | 0.87 |
| Total LPA time, min/day | 341.0±94.4 | 339.6±93.5 | 342.9±91.3 | 343.2±102.1 | 0.60 |
| Total MVPA time, min/day | 52.3±33.2 | 54.5±33.3 | 52.8±32.5 | 40.5±32.7 | <0.001 |
| Sporadic MVPA, min/day | 31.4±17.9 | 32.0±18.1 | 31.6±16.9 | 27.9±18.9 | 0.14 |
| Bouted MVPA, min/day | 20.9±24.1 | 22.5±24.1 | 21.2±25.1 | 12.6±20.5 | <0.001 |
| Steps per day | 5652.9±2803.3 | 5872.2±2699.7 | 5695.1±2792.8 | 4451.7±3057.0 | <0.001 |
Data shows mean ± SD or n (%). IADL, Instrumental Activity of Daily Living; MoCA, Montreal Cognitive Assessment; PSQI, Pittsburgh Sleep Quality Index; LPA, Light Physical Activity; MVPA, Moderate to Vigorous Physical Activity. Bouted MVPA was defined as ≥ 10 consecutive min, with an allowance for up to 2 min out of 10 to drop below the MVPA intensity threshold. Sporadic MVPA was defined as any MVPA accumulated in < 10 min.
Table 3 shows the association between SB, PA variables and frailty status. In models 1 and 2, total sedentary time, 10-min and 30-min bout of sedentary time, and mean sedentary bout duration was not associated with pre-frailty and frailty. On the other hand, except LPA and sporadic MVPA, PA variables including total MVPA time, bouted MVPA, and steps were significantly associated with frailty, but the associations were not observed for pre-frailty. While sporadic MVPA was significantly associated with frailty in model 1, the association between sporadic MVPA and frailty disappeared after additional adjusted for total sedentary time. The multivariable-adjusted odds ratios (95 % confidence intervals) for frailty were 0.83 (0.75-0.92), 0.81 (0.70-0.92), and 0.80 (0.71-0.89) per 10 min increase in total MVPA time and bouted MVPA, and per additional 1000 steps/day, respectively. AUCs of total MVPA time, bouted MVPA, and steps were significant (P < 0.001) but only weak discriminations (all AUC < 0.7) were observed. The optimal cut-off value of total MVPA time, bouted MVPA, and steps to discriminate between frailty and non-frailty were 43.25 min/day, 9.13 min/day, and 3841 steps/day, respectively (Figure 1).
Table 3.
Associations between patterns of sedentary behavior, physical activity and frailty status assessed by FRAIL-J
| Variables | Model 1 | Model 2 | ||
|---|---|---|---|---|
| Prefrailty | Frailty | Prefrailty | Frailty | |
| Sedentary behavior | ||||
| Total sedentary time, increment per 30 min/day | 0.99 (0.94-1.05) | 1.05 (0.97-1.13) | 0.97 (0.91-1.04)a | 0.95 (0.86-1.04)a |
| 10-min bout of sedentary time, increment per 30 min/day | 0.99 (0.94-1.04) | 1.04 (0.97-1.11) | 0.98 (0.93-1.03)a | 0.98 (0.90-1.05)a |
| 30-min bout of sedentary time, increment per 30 min/day | 1.00 (0.94-1.05) | 1.04 (0.96-1.13) | 0.99 (0.93-1.0)a | 0.98 (0.90-1.07)a |
| Mean sedentary bout duration, increment per 1 min/day | 0.97 (0.77-1.23) | 1.14 (0.83-1.58) | 0.95 (0.75-1.21)a | 1.00 (0.72-1.40)a |
| Physical activity | ||||
| Total LPA time, increment per 10 min/day | 1.01 (0.99-1.03) | 1.00 (0.97-1.03) | 1.01 (0.99-1.03)a | 1.02 (0.99-1.05)a |
| Total MVPA time, increment per 10 min/day | 0.98 (0.94-1.03) | 0.86 (0.79-0.93)** | 0.97 (0.91-1.03)b | 0.83 (0.75-0.92)**b |
| Sporadic MVPA, increment per 10 min/day | 0.99 (0.90-1.09) | 0.86 (0.74-0.99)* | 0.96 (0.85-1.09)b | 0.84 (0.71-1.01)b |
| 0.97 (0.85-1.09)c | 0.88 (0.73-1.05)c | |||
| Bouted MVPA, increment per 10 min/day | 0.97 (0.91-1.04) | 0.80 (0.70-0.91)** | 0.97 (0.90-1.04)b | 0.80 (0.69-0.91)**b |
| 0.97 (0.90-1.04)c | 0.81 (0.70-0.92)**c | |||
| Step, increment per 1000 step/day | 0.98 (0.92-1.04) | 0.82 (0.74-0.90)** | 0.97 (0.90-1.03)b | 0.80 (0.71-0.89)**b |
Data are shown as odds ratios (95%CIs) that Pre-frailty and Frailty compared to the Robust in each model using multinomial logistic regression. LPA, Light Physical Activity; MVPA, Moderate-to-Vigorous Physical Activity. Model 1, adjusted for age, sex, education, living alone, drink and smoke status, polypharmacy, MoCA score, PSQI score, IADL, and wear time.
Model 2, a, additional adjusted total MVPA time
b, additional adjusted total sedentary time
c, additional adjusted bouted MVPA and sporadic MVPA.
*, P<0.05
**, P<0.01. n=819.
Figure 1.
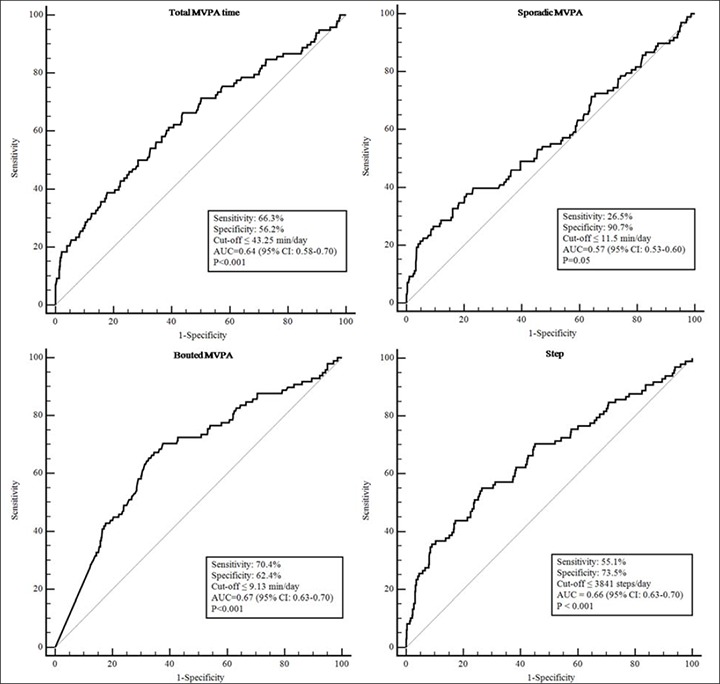
Receiver operating characteristic curves showing the optimal cut-off value of PA variables to discriminate frailty and non-frailty in Japanese community-dwelling older adults. AUC, Area under the curve.
Discussion
To our knowledge, this is the first study to investigate the associations between objectively measured patterns of SB, PA and frailty status screened by the FRAIL-J in Japanese community-dwelling older adults. We found that neither the total sedentary time nor SB patterns were associated with pre-frailty or frailty. Higher levels of total MVPA time, bouted MVPA, and steps were not associated with pre-frailty but associated with frailty. However, the independent association of LPA and sporadic MVPA with frailty was not observed. In addition, our results suggest that 43.25 min/day of total MVPA, 9.13 min/day of bouted MVPA, and 3841 steps/day of daily step represent the optimal cut-off value to discriminate between frailty and non-frailty. The main findings in this study provide evidence concerning how objective PA patterns are associated with frailty which might inform future feasible approaches to managing frailty in older Japanese adults.
The associations between total sedentary time, 10-min bout of sedentary time and frailty found in the present study are consistent with some previous studies (Bastone Ade et al., 2015; Castaneda-Gameros et al., 2018; Jansen et al., 2015; Manas et al., 2018; Nagai et al., 2018) while several inconsistencies are still observed. In contrast to the previous studies (Blodgett et al., 2015; Del Pozo-Cruz et al., 2017; Song et al., 2015), the present study showed that total sedentary time was not associated with frailty. Moreover, although a previous study has reported an inverse association between 30-min bout of sedentary time and 46-item frailty index (FI) in females, no such negative association was observed in the present study (Kehler et al., 2019). The reasons for the discrepancies between these findings and our results are multifaceted. First, participant characteristics may contribute to the discrepancies. For example, the present study only recruited older adults aged 65-75 years, while previous studies also include older adults aged more than 75 years. Second, the different objective measures of SB might be another reason. The present study used a tri-axial accelerometer to assess SB, which may more accurate than a uni-axial accelerometer used in previous studies (Blodgett et al., 2015; Kehler et al., 2018a; Song et al., 2015). Third, the heterogeneity of frailty assessments between the present study and previous studies might be an important reason contributes to the inconsistencies (Aguayo et al., 2017). For example, despite the 46-item FI used in the NHANES study is more comprehensive (Kehler et al., 2018a), it is not easily implemented in settings such as a busy clinic or large-scale epidemiological study, as it requires objectively measured or information such as blood pressure and other parameters. However, the FRAIL scale was simple, self-reported, and has been validated in diverse settings worldwide. Moreover, it is notable that it is comparable to more complex measurements such as FI in predicting mortality and disability. The fourth possible reason is regarding adjustment variables. Different factors inputted in the regression model might affect the final results. For example, total MVPA time was added to the final model to determine the independency of total sedentary time, while some previous studies did not add it (Del Pozo-Cruz et al., 2017; Song et al., 2015). Last, the inconsistencies also might be explained by lifestyle differences between Western counties and Japan. For example, according to a large population study that using tri-axial accelerometer to describe levels of SB and PA in Japanese community-dwelling older adults aged more than 65 years (Chen et al., 2015), the older adults spent 451.6 min/day in SB, 332.5 min/day in LPA, and 37.8 min/day in MVPA, which were somewhat more active than that have been reported in Western countries (Arnardottir et al., 2013, Lohne-Seiler et al., 2014, Kehler et al., 2018a). Thus, further studies should be conducted using the same method to assess SB and frailty to clarify the association between objective SB and frailty in different settings.
Our results found that higher total MVPA time had an association with a reduction in frailty and the optimal cut-off value to discriminate between frailty and non-frailty was 43.25 min/day. However, this value is much higher than the previous study which found total MVPA time of at least 7.5 minutes per day can prevent frailty development among 401 older adults aged 65-82 years (Yuki et al., 2019). One reason why the discrepancy appears might be caused by the different methods of how to define the cut-off value (25th percentile vs ROC analysis). Another main reason might be because the sporadic MVPA which is an essential part of total MVPA time was not associated with frailty in the present study. LPA could be relatively easier to perform for older adults than MVPA and recent guidelines also highlight the potential ability of LPA to benefit the health of older adults (Piercy et al., 2018). However, no significant association between LPA and frailty was observed in the present study. Actually, due to the lack of evidence, the recommendations of LPA such as time and frequency are still unclear, more studies are needed to determine the role and contribution of LPA alone or in combination with MVPA to health outcomes. A recent harmonized meta-analysis study observed non-linear, dose-response associations between PA variables and mortality, the maximal risk reductions for LPA (0.48, 0.38 to 0.63) was observed at 375 min/day, while at 24 min/day for MVPA (0.39, 0.26 to 0.59) (Ekelund et al., 2019). Therefore, according to the above evidence and our results, we considered that MVPA might be a much better choice than LPA for frailty management in Japanese community-dwelling older adults.
In the present study, our results showed that bouted MVPA was associated with frailty after additional adjusted for total sedentary time and sporadic MVPA, while the association between sporadic MVPA and frailty was not significant after additional adjusted for total sedentary time. The same results were also found from the ROC analyses that only the AUC of bouted MVPA was significant and the optimal cut-off value to discriminate between frailty and non-frailty was 9.13 min/day, which was lower than the recommendation of the WHO. These findings showed that bouted MVPA might be more effective on frailty compared to sporadic MVPA. However, it was opposed to a previous cross-sectional study from NHANES that demonstrated sporadic MVPA was associated with a 46-item FI (Kehler et al., 2018a). A recent systematic review found that although there has been an increasing number of studies demonstrated the positive associations between sporadic MVPA and adverse outcomes such as all-cause mortality and multimorbidity, while there are still some studies found only bouted MVPA but not sporadic MVPA was positively associated with adverse outcomes such as incidence of obesity and high-density lipoprotein cholesterol (Jakicic et al. 2019). The benefits of sporadic MVPA positively impact health might be because of its contribution to adding total energy expenditure (Tremblay et al., 2007). Therefore, further study should be conducted to examine the effects of sporadic and bouted MVPA on adverse outcomes under the same total energy expenditure.
As the basic component of PA, daily step is an easy-to-understand metric. A recent systematic primary literature review found that an inverse dose-response relationship of daily steps with important health outcomes, including all-cause mortality, cardiovascular events, and type 2 diabetes (Kraus et al., 2019). In the present study, our findings showed that higher daily steps were negatively associated with frailty. The optimal cut-off value of step to discriminate between frailty and non-frailty was 3841 steps per day, which was lower than the suggestion (5000 steps/day) of recently prospective study among Japanese older adults (Yuki et al., 2019). The discrepancy might be caused by the difference in study populations and statistical analyses such as the difference between the 25th percentile and ROC analysis.
Taken together, our findings indicated that lower amounts of bouted MVPA and steps can also benefit the health of older adults. It is more achievable and feasible compared to the official recommendations that make it be an initial target for older adults. These interesting findings point out a potential intervention method that combines bouted MVPA and steps together. For example, do a 10 min walking of any speed inside or outside every day may be a simple but effective way to manage frailty. However, this value should be further confirmed among older adults in future intervention studies before these observations can be translated into public health guidelines.
There are some limitations to this study. One main limitation was the response bias which relates to the generalizability of the present findings. Participants in this study population were individuals 65-75 years old from just one southwest city in Japan and therefore it was not representative of the older Japanese population. In addition, the response rate was relatively low which could cause bias in interpreting the results since the participants that self-selected to participate in the study may be different from those who did not. For example, a healthier group might have been included in the present study because participants had to attend the community center for assessing physical and cognitive function. Moreover, the cross-sectional design of this study precludes the ability to examine the predictive ability to make causal inferences.
Conclusion
In conclusion, our findings demonstrate a strong relationship between higher levels of total MVPA time, bouted MVPA, steps and frailty screened by FRAIL-J. Lower amounts of bouted MVPA (70 min/week) or steps (4000 steps/day) may be achievable initial targets in older adults for frailty management. This evidence might inform future feasible approaches to managing frailty in Japanese community-dwelling older adults.
Acknowledgements
We acknowledge the Itoshima city for their support with the recruitment of participants. The present study was supported in part by the Japan Agency for Medical Research and Development (AMED). The authors have no conflict of interest directly relevant to the content of the study. The authors declare the present study comply with the current laws of the country in which they were performed.
Biographies

Si CHEN
Employment
Graduate student, Graduate School of Human-Environment Studies, Kyushu University, Fukuoka, Japan
Degree
MSc
Research interests
Exercise epidemiology
E-mail: chensi2jap@yahoo.co.jp

Tao CHEN
Employment
Postdoctoral researcher, Center for Health Science and Counseling, Kyushu University, Fukuoka, Japan
Degree
PhD
Research interests
Exercise epidemiology and biochemistry
E-mail: chentwhy@gmail.com

Hiro KISHIMOTO
Employment
Associate professor, Faculty of Arts and Science, Kyushu University, Fukuoka, Japan
Degree
PhD
Research interests
Exercise epidemiology
E-mail: kishimoto@artsci.kyushu-u.ac.jp

Harukaze YATSUGI
Employment
Graduate student, Graduate School of Human-Environment Studies, Kyushu University, Fukuoka, Japan
Degree
MSc
Research interests
Exercise epidemiology
E-mail: haru19920424@gmail.com

Shuzo KUMAGAI
Employment
Prof., Center for Health Science and Counseling, Kyushu University, Fukuoka, Japan
Degree
PhD
Research interests
Exercise epidemiology and biochemistry
E-mail: shuzo@ihs.kyushu-u.ac.jp
References
- Aguayo G. A., Donneau A. F., Vaillant M. T., Schritz A., Franco O. H., Stranges S., Malisoux L., Guillaume M., Witte D. R. (2017) Agreement between 35 published frailty scores in the general population. American Journal of Epidemiology 186, 420-434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aprahamian I., Cezar N. O. C., Izbicki R., Lin S. M., Paulo D. L. V., Fattori A., Biella M. M., Jacob Filho W., Yassuda M. S. (2017) Screening for frailty with the FRAIL scale: a comparison with the phenotype criteria. Journal of the American Medical Directors Association 18, 592-596. [DOI] [PubMed] [Google Scholar]
- Arai H., Ouchi Y., Toba K., Endo T., Shimokado K., Tsubota K., Matsuo S., Mori H., Yumura W., Yokode M., Rakugi H., Ohshima S. (2015) Japan as the front-runner of super-aged societies: perspectives from medicine and medical care in Japan. Geriatrics & Gerontology International 15, 673-687. [DOI] [PubMed] [Google Scholar]
- Arnardottir N.Y., Koster A., Van Domelen D.R., Brychta R.J., Caserotti P., Eiriksdottir G., Sverrisdottir J.E., Launer L.J., Gudnason V., Johannsson E., Harris T.B., Chen K.Y., Sveinsson T. (2013) Objective measurements of daily physical activity patterns and sedentary behaviour in older adults: Age, Gene/Environment Susceptibility-Reykjavik Study. Age Ageing 42, 222-229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bastone Ade C., Ferriolli E., Teixeira C. P., Dias J. M., Dias R. C. (2015) Aerobic fitness and habitual physical activity in frail and nonfrail community-dwelling elderly. Journal of Physical Activity & Health 12, 1304-1311. [DOI] [PubMed] [Google Scholar]
- Bellettiere J., LaMonte M. J., Evenson K. R., Rillamas-Sun E., Kerr J., Lee I. M., Di C., Rosenberg D. E., Stefanick M., Buchner D. M., Hovell M. F., LaCroix A. Z. (2019) Sedentary behavior and cardiovascular disease in older women: The Objective Physical Activity and Cardiovascular Health (OPACH) Study. Circulation 139, 1036-1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blodgett J., Theou O., Kirkland S., Andreou P., Rockwood K. (2015) The association between sedentary behaviour, moderate-vigorous physical activity and frailty in NHANES cohorts. Maturitas 80, 187-191. [DOI] [PubMed] [Google Scholar]
- Castaneda-Gameros D., Redwood S., Thompson J. L. (2018) Physical activity, sedentary time, and frailty in older migrant women from ethnically diverse backgrounds: a mixed-methods study. Journal of Aging and Physical Activity 26, 194-203. [DOI] [PubMed] [Google Scholar]
- Chang S. F., Lin P. L. (2015) Frail phenotype and mortality prediction: a systematic review and meta-analysis of prospective cohort studies. International Journal of Nursing Studies 52, 1362-1374. [DOI] [PubMed] [Google Scholar]
- Chen S., Chen T., Kishimoto H., Susaki Y., Kumagai S. (2020) Development of a Fried Frailty Phenotype Questionnaire for use in screening community-dwelling older adults. Journal of the American Medical Directors Association 21, 272-276. [DOI] [PubMed] [Google Scholar]
- Chen T., Narazaki K., Honda T., Chen S., Haeuchi Y., Nofuji Y. Y., Matsuo E., Kumagai S. (2015) Tri-axial accelerometer-determined daily physical activity and sedentary behavior of suburban community-dwelling older Japanese adults. Journal of Sports Science & Medicine 14, 507-514. [PMC free article] [PubMed] [Google Scholar]
- Chen T., Kishimoto H., Honda T., Hata J., Yoshida D., Mukai N., Shibata M., Ninomiya T., Kumagai S. (2017) Patterns and levels of sedentary behavior and physical activity in a general Japanese population: The Hisayama Study. Journal of Epidemiology 12, 1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Del Pozo-Cruz B., Manas A., Martin-Garcia M., Marin-Puyalto J., Garcia-Garcia F. J., Rodriguez-Manas L., Guadalupe-Grau A., Ara I. (2017) Frailty is associated with objectively assessed sedentary behaviour patterns in older adults: Evidence from the Toledo Study for Healthy Aging (TSHA). PLoS One 12, e0183911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diaz K. M., Howard V. J., Hutto B., Colabianchi N., Vena J. E., Safford M. M., Blair S. N., Hooker S. P. (2017) Patterns of sedentary behavior and mortality in U.S. middle-aged and older adults: a national cohort study. Annals of Internal Medicine 167, 465-475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doi Y., Minowa M., Uchiyama M., Okawa M., Kim K., Shibui K., Kamei Y. (2000) Psychometric assessment of subjective sleep quality using the Japanese version of the Pittsburgh Sleep Quality Index (PSQI-J) in psychiatric disordered and control subjects. Psychiatry Research 97, 165-172. [DOI] [PubMed] [Google Scholar]
- Dong L., Qiao X., Tian X., Liu N., Jin Y., Si H., Wang C. (2018) Cross-cultural adaptation and validation of the FRAIL scale in Chinese community-dwelling older adults. Journal of the American Medical Directors Association 19, 12-17. [DOI] [PubMed] [Google Scholar]
- Ekelund U., Tarp J., Steene-Johannessen J., Hansen B. H., Jefferis B., Fagerland M. W., Whincup P., Diaz K. M., Hooker S. P., Chernofsky A., Larson M. G., Spartano N., Vasan R. S., Dohrn I. M., Hagstromer M., Edwardson C., Yates T., Shiroma E., Anderssen S. A., Lee I. M. (2019) Dose-response associations between accelerometry measured physical activity and sedentary time and all cause mortality: systematic review and harmonised meta-analysis. BMJ 366, l4570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng Z., Lugtenberg M., Franse C., Fang X., Hu S., Jin C., Raat H. (2017) Risk factors and protective factors associated with incident or increase of frailty among community-dwelling older adults: a systematic review of longitudinal studies. PLoS One 12, e0178383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fujiwara Y., Suzuki H., Yasunaga M., Sugiyama M., Ijuin M., Sakuma N., Inagaki H., Iwasa H., Ura C., Yatomi N., Ishii K., Tokumaru A. M., Homma A., Nasreddine Z., Shinkai S. (2010) Brief screening tool for mild cognitive impairment in older Japanese: validation of the Japanese version of the Montreal Cognitive Assessment. Geriatrics & Gerontology International 10, 225-232. [DOI] [PubMed] [Google Scholar]
- Honda T., Chen S., Yonemoto K., Kishimoto H., Chen T., Narazaki K., Haeuchi Y., Kumagai S. (2016) Sedentary bout durations and metabolic syndrome among working adults: a prospective cohort study. BMC Public Health 16, 888, 1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jakicic J. M., Kraus W. E., Powell K. E., Campbell W. W., Janz K. F., Troiano R. P., Sprow K., Torres A., Piercy K. L. (2019) Association between bout duration of physical activity and health: systematic review. Medicine and Science in Sports and Exercise 51, 1213-1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jansen F. M., Prins R. G., Etman A., van der Ploeg H. P., de Vries S. I., van Lenthe F. J., Pierik F. H. (2015) Physical activity in non-frail and frail older adults. PLoS One 10, e0123168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kehler D. S., Clara I., Hiebert B., Stammers A. N., Hay J. L., Schultz A., Arora R. C., Tangri N., Duhamel T. A. (2018a) The association between bouts of moderate to vigorous physical activity and patterns of sedentary behavior with frailty. Experimental Gerontology 104, 28-34. [DOI] [PubMed] [Google Scholar]
- Kehler D. S., Hay J. L., Stammers A. N., Hamm N. C., Kimber D. E., Schultz A. S. H., Szwajcer A., Arora R. C., Tangri N., Duhamel T. A. (2018b) A systematic review of the association between sedentary behaviors with frailty. Experimental Gerontology 114, 1-12. [DOI] [PubMed] [Google Scholar]
- Kehler D. S., Clara I., Hiebert B., Stammers A. N., Hay J. L., Schultz A., Arora R. C., Tangri N., Duhamel T. A. (2019) Sex-differences in relation to the association between patterns of physical activity and sedentary behavior with frailty. Archives of gerontology and geriatrics, in press. [DOI] [PubMed] [Google Scholar]
- Kehler D. S., Theou O. (2019) The impact of physical activity and sedentary behaviors on frailty levels. Mechanisms of Ageing and Development 180, 29-41. [DOI] [PubMed] [Google Scholar]
- Kojima G. (2016) Frailty as a predictor of hospitalisation among community-dwelling older people: a systematic review and meta-analysis. Journal of Epidemiology and Community Health 70, 722-729. [DOI] [PubMed] [Google Scholar]
- Kojima G., Iliffe S., Taniguchi Y., Shimada H., Rakugi H., Walters K. (2017) Prevalence of frailty in Japan: a systematic review and meta-analysis. Journal of Epidemiology 27, 347-353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koyano W., Shibata H., Nakazato K., Haga H., Suyama Y. (1991) Measurement of competence: reliability and validity of the TMIG Index of Competence. Archives of Gerontology and Geriatrics 13, 103-116. [DOI] [PubMed] [Google Scholar]
- Kraus W. E., Janz K. F., Powell K. E., Campbell W. W., Jakicic J. M., Troiano R. P., Sprow K., Torres A., Piercy K. L. (2019) Daily step counts for measuring physical activity exposure and its relation to health. Medicine and Science in Sports and Exercise 51, 1206-1212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J. S., Auyeung T. W., Leung J., Kwok T., Woo J. (2014) Transitions in frailty states among community-living older adults and their associated factors. Journal of the American Medical Directors Association 15, 281-286. [DOI] [PubMed] [Google Scholar]
- Lohne-Seiler H., Hansen B.H., Kolle E., Anderssen S.A. (2014) Accelerometer-determined physical activity and self-reported health in a population of older adults (65-85 years): a cross-sectional study. BMC Public Health 14, 284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manas A., Del Pozo-Cruz B., Guadalupe-Grau A., Marin-Puyalto J., Alfaro-Acha A., Rodriguez-Manas L., Garcia-Garcia F. J., Ara I. (2018) Reallocating accelerometer-assessed sedentary time to light or moderate-to-vigorous-intensity physical activity reduces frailty levels in older adults: an isotemporal substitution approach in the TSHA Study. Journal of the American Medical Directors Association 19, 185 e181-185 e186. [DOI] [PubMed] [Google Scholar]
- Metz C. E. (1978) Basic principles of ROC analysis. Seminars in Nuclear Medicine 8, 283-298. [DOI] [PubMed] [Google Scholar]
- Nagai K., Tamaki K., Kusunoki H., Wada Y., Tsuji S., Ito M., Sano K., Amano M., Shimomura S., Shinmura K. (2018) Isotemporal substitution of sedentary time with physical activity and its associations with frailty status. Clinical Interventions in Aging 13, 1831-1836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Cancer Institute (2015) SAS programs for analyzing NHANES 2003-2004 accelerometer data (online material). Aavailable from URL: http://appliedresearch.cancer.gov/nhanes_pam/ [Accessed 17 Nov 2015]. [Google Scholar]
- Ohkawara K., Oshima Y., Hikihara Y., Ishikawa-Takata K., Tabata I., Tanaka S. (2011) Real-time estimation of daily physical activity intensity by a triaxial accelerometer and a gravity-removal classification algorithm. The British Journal of Nutrition 105, 1681-1691. [DOI] [PubMed] [Google Scholar]
- Piercy K. L., Troiano R. P., Ballard R. M., Carlson S. A., Fulton J. E., Galuska D. A., George S. M., Olson R. D. (2018) The physical activity guidelines for Americans. Journal of the American Medical Association 320, 2020-2028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh R., Pattisapu A., Emery M. S. (2019) US Physical Activity Guidelines: Current state, impact and future directions. Trends in Cardiovascular Medicine. Epub ahead of print pii: S1050-1738(19)30140-9. [DOI] [PubMed] [Google Scholar]
- Song J., Lindquist L. A., Chang R. W., Semanik P. A., Ehrlich-Jones L. S., Lee J., Sohn M. W., Dunlop D. D. (2015) Sedentary behavior as a risk factor for physical frailty independent of moderate activity: results from the Osteoarthritis Initiative. American Journal of Public Health 105, 1439-1445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tremblay M. S., Esliger D. W., Tremblay A., Colley R. (2007) Incidental movement, lifestyle-embedded activity and sleep: new frontiers in physical activity assessment. Canadian Journal of Public Health 98(Suppl 2), S208-217. [PubMed] [Google Scholar]
- Tremblay M. S., Aubert S., Barnes J. D., Saunders T. J., Carson V., Latimer-Cheung A. E., Chastin S. F. M., Altenburg T. M., Chinapaw M. J. M. (2017) Sedentary Behavior Research Network (SBRN) - Terminology consensus project process and outcome. International Journal of Behavioral Nutrition and Physical activity 14, 1-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tudor-Locke C., Han H., Aguiar E. J., Barreira T. V., Schuna J. M., Jr., Kang M., Rowe D. A. (2018) How fast is fast enough? Walking cadence (steps/min) as a practical estimate of intensity in adults: a narrative review. British Journal of Sports Medicine 52, 776-788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vermeiren S., Vella-Azzopardi R., Beckwee D., Habbig A. K., Scafoglieri A., Jansen B., Bautmans I. (2016) Frailty and the prediction of negative health outcomes: a meta-analysis. Journal of the American medical directors association 17, 1163 e1-1163 e17. [DOI] [PubMed] [Google Scholar]
- WHO (2010) Global Recommendations on physical activity for health. Geneva, Switzerland. [PubMed] [Google Scholar]
- Yuki A., Otsuka R., Tange C., Nishita Y., Tomida M., Ando F., Shimokata H., Arai H. (2019) Daily physical activity predicts frailty development among community-dwelling older Japanese adults. Journal of the American Medical Directors Association 1, 1-5. [DOI] [PubMed] [Google Scholar]


