Abstract
Poor recovery among older adults with hip fractures can occur despite successful surgical repair and rehabilitation, suggesting other factors might play a role in recovery, such as social factors. The aim of this scoping review was to provide an overview of the literature on the role of social factors in older adult’s recovery after hip fracture. This review followed the York Framework and its modifications and recent reporting guidelines. Two independent researchers searched main medical databases (CINAHL, EMBASE, Medline, PsyclNFO and the Cochrane libraries) from inception to June 2017, for studies investigating social factors and recovery post hip fracture. Studies were excluded if they were qualitative, perspective papers or if participants were < 65 years or they were not living in the community. We screened 2,503 unique abstracts in total and 19 studies fulfilled the inclusion criteria. Social factors investigated in the included studies were social support, socioeconomic factors and living arrangement. We classified outcomes in the studies into three subgroups: physical functional recovery, mortality and other outcomes (pain, hospital length of stay and quality of life). We found evidence that social support and socioeconomic factors (e.g. socioeconomic status) were significantly associated with an increase in functional recovery, a decrease in mortality and other outcomes, but conflicting evidence was found for the effect of one’s living arrangement. Only two included studies were randomised controlled trials. To conclude, social factors, such as social support and socioeconomic status, affect physical functional recovery and mortality in older adults with hip fractures. However, this is an under researched area that lacks rigorously designed studies and would benefit from more studies with rigorous designs.
Keywords: fragility fractures, review, social determinants of health
1 |. INTRODUCTION
A hip fracture is a common and serious consequence of falls and osteoporosis in older adults with prevalence on the rise in a continuously ageing population (Bergström et al., 2009; Frost, Nguyen, Black, Eisman, & Nguyen, 2011). Hip fractures are associated with high rates of mortality, morbidity and disability, with 1-year mortality rates ranging from 14% to 58% (Johnell & Kanis, 2004; Schnell, Friedman, Mendelson, Bingham, & Kates, 2010). Hip fractures are also economically burdensome for patients, their families, healthcare, providers and the broader healthcare system (Lahtinen et al., 2017; Wiktorowicz, Goeree, Papaioannou, Adachi, & Papadimitropoulos, 2001). Poor recovery after hip fracture can occur despite successful surgical repair and traditional rehabilitation, which suggests that there are other factors contributing to favourable and unfavourable recovery outcomes (Beaupre et al., 2013; Reimers & Laflamme, 2007; Shyu, Liang, Wu, Cheng, & Chen, 2010).
The focus of medical management after hip fracture has been mainly physical rehabilitation; however, recent studies have identified that other nonphysical factors can play a critical role in the recovery process, such as social factors (Scheffers-Barnhoorn et al., 2017). There is growing evidence that social factors play a role in recovery (Gruber-Baldini et al., 2003; Petrella, Payne, Myers, Overend, & Chesworth, 2000; Reimers & Laflamme, 2007; Shyu et al., 2010; Visschedijk, Achterberg, Van Balen, & Hertogh, 2010). Currently these factors are not commonly considered, evaluated and/or managed in hip fracture rehabilitation programmes (Beaupre et al., 2013; Petrella et al., 2000; Sylliaas et al., 2012). Emerging evidence supports that incorporating social factors into the model of rehabilitative care for patients post hip fracture could be important for improving recovery outcomes, reducing mortality and economic burden and ensuring an improved quality of life post fracture for this growing population of individuals (Beaupre et al., 2013; Gruber-Baldini et al., 2003; Petrella et al., 2000; Reimers & Laflamme, 2007; Shyu et al., 2010; Visschedijk et al., 2010). However, there is also conflicting evidence about the importance of social factors in recovery with some studies showing little support for its role or benefit in the recovery process (Egan, Warren, Hessel, & Gilewich, 1992; Marottoli, Berkman, & Cooney, 1992).
These conflicting research findings warrant reviewing all available evidence to better understand the role social factors play in recovery for older adults after a hip fracture. This relationship is also important to understand and better inform best practices, specifically rehabilitation protocols that potentially address both physical and nonphysical factors (including social factors), to improve post fracture recovery rates. The objective of this scoping review was to summarise the current state of knowledge on the role of social factors in the recovery of community-dwelling older adults post hip fracture. We hypothesised that social factors have a significant relationship with different recovery outcomes, including functional outcomes, mortality and other outcomes such as pain, hospital length of stay and health-related quality of life.
2 |. METHODS
A scoping review was conducted following the guidelines of Arksey and O’Malley (the York Framework) (Arksey & O’Malley, 2005) and its modifications (Levac, Colquhoun, & O’Brien, 2010) to systematically review the role of social factors in the recovery of older adults patients after hip fractures. The PRISMA extension for scoping reviews reporting guidelines has been followed in this report (Tricco et al., 2018).
Following widespread practice in health domains, we use the term ‘social’ to refer to economic as well as social factors that are known to influence health (National Research Council (US), Institute of Medicine (US), Woolf SH, Aron L, 2013). For the purposes of this study, we modified Public Health Agency of Canada’s definition of social factors and we defined them as a group of social and economic factors within the broader determinants of health that are relevant to a person’s place in society (Public Health Canada, 2018). These include socioeconomic position, social exclusion, social capital, employment and work, housing and education (Public Health Canada, 2018). The influence of the physical environment was not included here.
2.1 |. Data sources and search
Five major databases (CINAHL, EMBASE, Medline, PsyclNFO and the Cochrane libraries) were searched by a health librarian to find articles discussing the relationship between social factors and recovery after a hip fracture. All databases were searched from inception until June 27, 2017. We decided to keep the search as broad as possible to ensure we do not miss any relevant title. Thus, an extensive list of Medical Subject Headings and keywords were used to capture the wide variety of terms that can be used to encapsulate social factors (See Appendix 1 for a sample search strategy). We also hand searched the references of included studies and relevant reviews, and searched abstracts proceedings whenever available.
2.2 |. Study inclusion and exclusion criteria
Studies were included when social factors, such as social network size, marital status or social support available, were investigated as influencing recovery outcomes from hip fracture in those 65 years old or older. Studies were excluded if the results were not reported separately for those 65 years or older and when the study population was not community dwelling before and after the fracture. We also excluded any study focused solely on physical factors (e.g. muscle strength) without studying the effect of social factors, qualitative studies and perspective papers (i.e. commentaries/opinion pieces without primary data). There were no language, design (within our inclusion criteria) or date restrictions.
2.3 |. Data screening, extracting and analysis
Abstracts from the primary search were downloaded into Endnote software (EndNote X7), duplicates were removed, and abstracts were screened by two independent researchers. The two researchers discussed the results to ensure agreement on included articles. The full text for eligible abstracts was retrieved and reviewed independently by the two researchers for eligibility.
Data from all confirmed eligible studies were extracted using a standardised data-extraction form, which was piloted using a subset of articles and then refined. Included articles went through data extraction independently by the two researchers with follow-up discussion to ensure agreement. When any disagreements arose at any step a third reviewer was consulted. Data extracted included general study information (year, language, study setting, type of publication, purpose), methods and design (study design, sampling method, number of participants, gender split, age, length of study, social factors investigated, outcome measures, intervention used), results (significant findings, relationship found) and original author conclusion (main conclusions, implications for practice, implications for research, implication for policy, limitations, directions for future research).
The two independent reviewers met to ensure data extracted yielded the same findings. Finally, the data were critically analysed to look for trends and variances. Using content analysis, social factors and outcomes used in the studies to measure recovery were categorised into subtypes of social factors and subcategories of outcomes.
3.1 |. RESULTS
3.1 |. Literature search
A primary search of databases yielded 3,558 records. After duplicates were removed, 2,503 potentially eligible abstracts were screened. The screening yielded 68 articles, which went through full-text reading to confirm eligibility. Subsequently, 19 articles fulfilled the inclusion criteria and were included in this scoping review (see Figure 1 for PRISMA flowchart for an overview of the search process).
FIGURE 1.
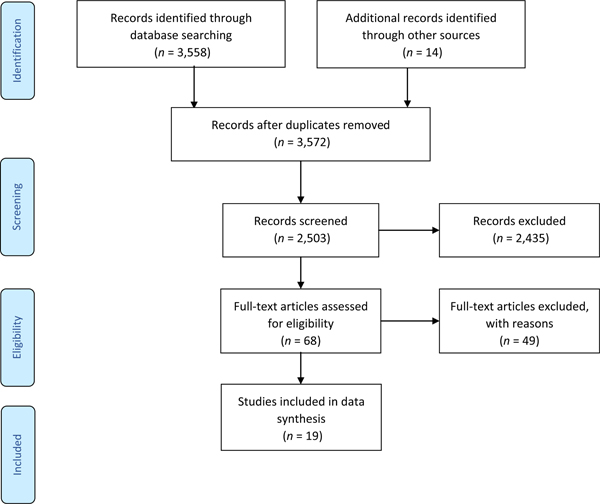
PRISMA flow diagram [Colour figure can be viewed at wileyonlinelibrary.com]
3.2 |. Characteristics of the included articles
Table 1 presents a summary of the characteristics of the included studies. Included studies were two randomised controlled trials, one cross-sectional exploratory study, one retrospective observational cohort study, one record linkage study and 14 prospective cohort studies. The overall sample size of the included papers ranged from 40 to 171,570 participants (Gambatesa et al., 2013; Thorne, Johansen, Akbari, Williams, & Roberts, 2016), and the mean age of participants ranged from 76.6 (SD: 7.4) to 85.5 (SD: 5.8) years old. For longitudinal studies (excluding secondary analysis studies), the duration of studies ranged from 3 weeks to 18 months, with many studies having multiple follow-up assessment time points (e.g. at 0, 30, 90 and 365 days post fracture) (Orive et al., 2016; Thorne et al., 2016). Studies represent a wide range of geographical locations: Canada, Denmark, Finland, Italy, Korea, Norway, Portugal, Spain, United Kingdom and the United States of America (see Figure 2). All studies collected data on post-fracture outcomes except for two studies that also looked at pre-fracture subjective recalled outcomes (Cobey et al., 1976; Mortimore et al., 2008). Fifteen studies primarily investigated the relationship between social factors and recovery post hip fracture, whereas four studies looked at social factors as a secondary objective (Hongisto, Nuotio, Luukkaala, Vaisto, & Pihlajamaki, 2016; Morghen et al., 2011; Orive et al., 2016; Sylliaas et al., 2012).
TABLE 1.
Characteristics of included studies
| Authors (year) | Study design | N | Women (%) | Age (range and/or mean [SD]) | Social factors under study | Was the relationship for social factors significant? | Summary of the relationship found between social factors and outcomes | Length of follow-up (months) |
|---|---|---|---|---|---|---|---|---|
| Cobey et al., 1976 | Prospective observational cohort | 89 | 75 | 65–91 | Participation—getting out of the home prior to injury | Yes | Participation prior to fracture was correlated with recovery as measured by modification of a functional activity scale developed by Katz | 6 |
| Magaziner et al., 1990 | Prospective observational cohort | 340 | 83.50 | 78.1 ± 7.1 | Social network | Yes | Greater contact with ones social network is positively associated with recovery in three areas (walking ability, physical dependence and instrumental dependence). | 12 |
| Egan et al., 1992 | Prospective observational cohort | 61 | 78.70 | 76.6 ± 7.4 | Role loss (investigated using the Role Checklist) and social support (investigated using part 2 of the Personal Resource Questionnaire) | No | Dependence in ADL’s at home was not significantly related to role loss (different roles in life). | 0.7 (3 weeks) |
| Marottoli et al., 1992 | Prospective observational cohort | 118 | 72.03 | 65+; 78.2 | Social support (social network size, number of sources of emotional or task support, marital status and social activities) | No | At 6 weeks and 6-months fewer sources of emotional support at baseline was not statistically significant as a predictor of better physical function. | 6 |
| Marottoli et al., 1994 | Prospective observational cohort | 120 | 71.67 | 65+; not given | Social network and support measures (social network size, number of sources of emotional or task support, marital statusand social activities) | No for the majority of factors | Measures were not associated with an increase or decrease risk of mortality. Being unmarried was the only social support measure that trended towards institutionalisation. | 6 |
| Oh & Feldt, 2000 | Prospective observational cohort | 70 | 88.60 | 65+; 84.12 | Social supportas measured using a modified Norbeck Social Support Questionnaire | Yes | Perceptions of network size and instrumental support at discharge were correlated with functional status, as measured by the Functional Status Index, at 2 months following discharge. | 2 |
| Cree et al., 2001 | Prospective observational cohort | 367 | 79 | 65+; 82 | Social support determined by whether the respondent had someone to rely on for help when needed; measured by the Older Americans Resources and Services (OARS) | Yes | Functional dependence among patients of low mental function is predicted by social support. | 3 |
| Cresci, 2001 | Cross-sectional exploratory |
73 | 100.0 | 65+; 81 ±6.87 | Informational support (used the modified Inventory of Socially Supportive Behaviors (ISSB) provided by natural support systems | Yes | Informational support was a significant predictor of post injury functional status | N.A. |
| Allegrante et al., 2007 | Randomised control trial | 59 | 76.27 | 65+; 77 ±8 | Multi-faceted rehab approach: a motivational video and social contact with an age-matched peer who had recovered from hip fracture | Yes | Intervention arm had a significant positive change in the role-physical scale as compared to the control. | 6 |
| Mortimore et al., 2008 | Prospective observational cohort | 674 | 77.40 | 65+; 81.1 ± 7.4 | Interaction with social network | Yes | Infrequent contact with family or friends before hip fracture are at higher risk of dying than are those who have frequent contact. | 24 |
| Morghen et al., 2011 | Prospective observational cohort | 280 | 88.40 | 65+; 80.2 ± 6.8 | Living arrangement | No | Living alone was not significant predictor of failure to recover walking independence at discharge | 12 |
| Sylliaas et al., 2012 | Prospective observational cohort | 277 | 82 | 65+; 82.4 ± 6.5 | Living arrangement | No | Living arrangement was not a significant predictor of either ADL or IADL | 3 |
| Gambatesa et al., 2013 | Randomised control Trial | 40 | 92.50 | 70+; 80.8 ±6.5 | Counselling (as a social support) | Yes | Counselling had a positive impact on health-related quality of life on all patients, but in a more relevant way if patients were low functioning upon admittance to the ward. | 1 |
| Orive et al., 2016 | Prospective observational cohort | 740 | 79.07 | 65 and older; not given | Home status, institutional support at baseline, independence level and income | Yes | Predictors of worsening pain at 6 months and/or 18 months included living in a home-care situation or nursing home before the fracture. Social predictors of deterioration in function at 6 months and/or 8 months included lower income. | 18 |
| Hongisto et al., 2016 | Prospective observational cohort | 841 | 78.10 | 65 and older; 81.9 ± 6.77 | Living with somebody, previous living arrangement | Yes | Living with somebody prior to hip fracture was protective against institutionalisation at 1 year. Institutionalisation at 1 and 4 months after hip fracture considerably increased the risk of death and permanent institutionalisation 12 months after hip fracture. | 12 |
| Kristensen etal.,2017 | Prospective population-based cohort study | 25,354 | 49 | 65 and older; not given | Socioeconomic markers: education, income, cohabiting status and migrant status | Yes (for some) | Patients with higher education had a lower 30-day mortality risk. Level of family income was associated with lower 30-day mortality. Patients with both high education and high income had a lower risk of acute readmission. | 1 |
| Landeiro et al., 2016 | Prospective observational cohort | 278 | 79.50 | 75+; 85.5 ±5.8 | Social isolation | Yes | Being isolated or at a high risk of social isolation, was significantly associated with delayed discharges. | 0.4 (13 days on average) |
| Shin et al., 2016 | Retrospective cohort study | 5,441 | 71 | 65 and older; not given | SES (income) | Yes | Mean survival time was longer as the income level increased | 120 (this is retrospective database study with 11 years of follow-up for some patients) |
| Thorne et al., 2016 (Wales) | Record linkage study —database study | 11,098 | 73.25 | 80.4 ± 11.1 | Social demographics: income, employment, health and disability, education, barriers to housing and services, crime, living environment | Yes for social deprivation and mortality rates | Social deprivation (based on the social demographics indicated) was significantly associated with increased mortality in the most deprived quintile compared with the least deprived quin- tile at 90 and 365 days in Wales | 12 |
| Thorne et al., 2016 (England) | Record linkage study—database study | 171,570 | 72.85 | 80.7 ± 11.6 | Social demographics: income, employment, health and disability, education, barriers to housing and services, crime, living environment | Yes for social deprivation and mortality rates | Social deprivation was significantly associated with increased mortality in the most deprived quintile compared with the least deprived quintile at 30, 90 and 365 days in England. | 12 |
Abbreviations: ADL, activities of daily living; IADL, instrumental activities of daily living.
FIGURE 2.
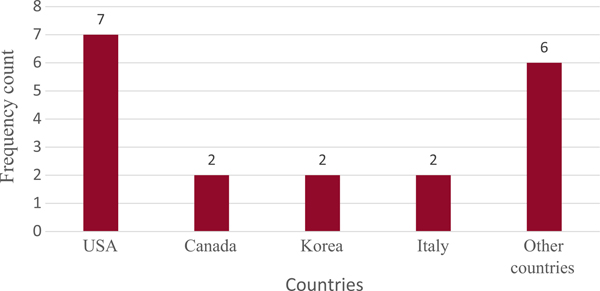
Count of included studies by country. Other include countries: Denmark, Finland, Norway, Portugal, Spain, United Kingdom [Colour figure can be viewed at wileyonlinelibrary.com]
3.3 |. Social factors under study
We found ten social factors under study in the included articles, which we grouped into three main categories/themes:
Social support: (a) intervention to increase social contact (Magaziner, Simonsick, Kashner, Hebel, & Kenzora, 1990), (b) number of social outings (Cobey et al., 1976), (c) reported size of social network (Cresci, 2001; Marottoli, Berkman, Leo-Summers, & Cooney, 1994; Mortimore et al., 2008; Oh & Feldt, 2000), (d) and social isolation (Landeiro, Gray, & Leal, 2016).
Socioeconomic factors: (a) income (Kristensen, Thillemann, Pedersen, Soballe, & Johnsen, 2017; Orive et al., 2016; Shin et al., 2016; Thorne et al., 2016), (b) employment (Allegrante et al., 2007), (c) education and training (Allegrante et al., 2007; Kristensen et al., 2017; Shin et al., 2016; Thorne et al., 2016), (d) barriers to housing (as an indicator of social deprivation) (Thorne et al., 2016), (e) and neighbourhood crime rate (as an indicator of social deprivation) (Thorne et al., 2016).
Living arrangement/institutionalisation (Hongisto et al., 2016; Morghen et al., 2011; Orive et al., 2016; Sylliaas et al., 2012; Thorne et al., 2016).
Table 2 summarises all measurement tools (outcome measures) used for social factors in included studies.
TABLE 2.
Measurement tools (outcome measures) for social factors
| Social theme | Measurement tool |
|---|---|
| Social support | |
| 1. Increase in social contact | 1. Self-report at 2 months follow-up |
| 2. Number of social outings | 2. Self-report |
| 3. Reported size of social network | 3. Inventory of Socially Supportive Behaviors (ISSB) |
| 4. Social isolation | 4. Lubben social network scale |
| Socioeconomic status | |
| 1. Income | 1. Data from pre-existing database |
| 2. Employment | 2. Data from pre-existing database |
| 3. Education and training | 3. Data from pre-existing database |
| 4. Barriers to housing | 4. Data from pre-existing database |
| 5. Neighbourhood crime rate (Thorne et al., 2016) | 5. Data from pre-existing database |
| Living arrangement | |
| 1. Living arrangement/Institutionalisation | 1. Self-report/Chart review |
3.4 |. Reported outcomes
Reported outcomes associated with social factors across studies were divided into three categories:
Physical functional recovery: There were eleven articles investigated the relationship between social factors and physical functional recovery after hip fracture (Allegrante et al., 2007; Cobey et al., 1976; Cree, Carriere, Soskolne, & Suarez-Almazor, 2001; Cresci, 2001; Egan et al., 1992; Magaziner et al., 1990; Marottoli et al., 1992; Morghen et al., 2011; Oh & Feldt, 2000; Orive et al., 2016; Sylliaas et al., 2012). The following outcome measures were used: the role-physical of the 36-Item Short Form Health Survey (SF-36) (Allegrante et al., 2007), the physical summary domain of 12-Item Short Form Health Survey (SF-12) (Physical Composite Scale scores [PCS-12]) (Sylliaas et al., 2012), Lawton-Brody Instrumental Activities of Daily Living (IADL) Scale (Orive et al., 2016), Barthel Activities of Daily Living (ADL) Index (Cree et al., 2001; Kristensen et al., 2017; Orive et al., 2016; Sylliaas et al., 2012), the Nottingham Extended ADL scale (NEADL) (Sylliaas et al., 2012), adapted functional activity scale ‘Katz index’ (Cobey et al., 1976) and informal questions on ADL and IADL (Egan et al., 1992).
Mortality: There were six articles that investigated mortality (Hongisto et al., 2016; Kristensen et al., 2017; Marottoli et al., 1994; Mortimore et al., 2008; Shin et al., 2016; Thorne et al., 2016) as measured by death records at various time points post fracture (30 days, 2 months, 6 months, 1 year).
Other outcomes: There were six articles investigated other outcomes including: pain, measured by visual analogue scale (VAS) (Orive et al., 2016), health-related quality of life as measured by the SF-36 total score (Gambatesa et al., 2013), hospital length of stay in days (Kristensen et al., 2017; Landeiro et al., 2016) and two articles that investigated the effect on institutionalisation after hip fracture (Hongisto et al., 2016; Marottoli et al., 1994).
Table 3 summarises all outcome measures in included studies.
TABLE 3.
Outcome measures in included studies
| Outcome/Construct | Measurement tool |
|---|---|
| Physical functional recovery | 1. The role-physical of the SF-36 |
| 2. The physical domain of SF-12 (PCS-12) | |
| 3. Lawton-Brody Instrumental Activities of Daily Living (IADL) Scale | |
| 4. Barthel Activities of Daily Living (ADL) Index (BI) | |
| 5. The Nottingham Extended ADL scale (NEADL) | |
| 6. Adapted functional activity scale ‘Katz index’, including subscales from the OARS Multidimensional Functional Assessment Questionnaire (OMFAQ) and the functional status index | |
| 7. Recovery of walking independence (12/15 at the BI walking sub-item) | |
| Mortality | 1. Assessed through databases (time intervals: 30 days, 2 months, 6 months, 1 year) |
| Pain | 1. Instrument short form (WOMAC-SF)-the self-reported pain (PD-W) aspect |
| 2. Visual analogue scale (VAS) | |
| Health-related quality of life | 1. Short Form-36 |
| 2. Health-related Quality of Life (HRQOL) | |
| Length of stay | 1. Chart review—number of days discharged |
3.5 |. Relationship between social factors and outcomes (divided by social factors)
3.5.1 |. General descriptions of the relationships
In the included 19 articles, we found 23 reports (i.e. test of a relationship) of associations (and/or significant differences) of social factors and recovery. Eighteen (n = 18) out of the 23 reports indicated that there is a significant association between the given social factor(s) under investigation and recovery outcomes after hip fractures or significant difference in recovery based on these factors (Allegrante et al., 2007; Cobey et al., 1976; Cree et al., 2001; Cresi, 2001; Gambatesa et al., 2013; Kristensen et al., 2017; Landeiro et al., 2016; Magaziner et al., 1990; Oh & Feldt, 2000; Orive et al., 2016; Shin et al., 2016; Thorne et al., 2016). The remaining five reports indicated that there is no significant association, correlation or significant difference with respect to the social factor and functional outcome under investigation (Egan et al., 1992; Marottoli et al., 1992, 1994; Morghen et al., 2011; Sylliaas et al., 2012). Overall, these five reports tended to have smaller sample sizes than the rest of included studies, which might have influenced the results.
3.5.2 |. Detailed findings by social themes and outcome
Social support
Overall, the results showed that more social support tended to predict better health outcomes after hip fracture.
Physical functional recovery.
Looking at social support and physical functional recovery, most papers showed a significant positive relationship between the two variables, more social support tended to predict better physical functional recovery. Six studies found social support, as measured by social contact, number of social outings prior to fracture, perception of social network size, marital status and/or amount of informational support available, to be significantly associated with increased physical functional recovery (Allegrante et al., 2007; Cobey et al., 1976; Cree et al., 2001; Cresci, 2001; Magaziner et al., 1990; Oh & Feldt, 2000). One non-significant association was found between decreased social support, as measured by loss of life roles, and physical functional recovery, as measured by dependence in ADLs (Egan et al., 1992). Another report found a non-significant relationship between emotional support and functional outcome (Marottoli et al., 1992).
Mortality.
Looking at social support and mortality, there was one report of social support demonstrating a significant association with mortality, where participants who had less social contact prior to fracture had increased risk of mortality (Mortimore et al., 2008).
Other outcomes.
One article looked at various aspects of social support, including social network size, number of sources of emotional or task support, marital status and social activities, and only being married was significantly associated with not being institutionalised post hip fracture (Marottoli et al., 1994). Counselling, as a social intervention, was found to significantly impact health-related quality of life of hip fracture patients (Gambatesa et al., 2013). Finally, social isolation was significantly associated with delayed hospital discharge after the facture (Landeiro et al., 2016).
Socioeconomic status
All socioeconomic factors found throughout included studies established significant relationship with physical functional outcomes, mortality and other outcomes.
Physical functional recovery.
One study found a significant association with physical functional recovery, with lower socioeconomic markers predicting worse physical functional outcomes post hip fracture (Orive et al., 2016).
Mortality.
Three studies (included four reports) found significant associations with mortality (Kristensen et al., 2017; Shin et al., 2016; Thorne et al., 2016). Lower education and lower family income were significantly associated with mortality (Kristensen et al., 2017; Shin et al., 2016). Social deprivation, as measured by social demographics (e.g. income, employment, education and training skills, barriers to housing and neighbourhood crime), was also significantly associated with increased mortality (Thorne et al., 2016).
Other outcomes.
One article found that patients with both high education and high income had a lower risk of acute hospital readmission (Kristensen et al., 2017).
Living arrangement
Living arrangement had conflicting results with three studies showing a significant positive relationship between living arrangement and the reported outcome measure (mortality and other outcomes), and two others finding no significant associations with functional recovery.
Physical functional recovery.
Two reports found living alone pre-fracture was not a significant predictor of physical functional recovery, as measured by recovering walking independence or ADL/IADLs post fracture (Morghen et al., 2011; Sylliaas et al., 2012).
Mortality.
One study found that institutionalisation at 1 and 4 months after hip fracture considerably increased the risk of death 12 months after hip fracture (Hongisto et al., 2016).
Other outcomes.
One study found that living in a nursing home compared to those living independently pre-fracture was associated with higher reported pain post fracture (Orive et al., 2016). Finally, One report found that living with someone/or living independently without home-care services prior to surgery was protective against institutionalisation at 1 year post hip fracture (Hongisto et al., 2016).
3.6 |. Relationship between outcomes and social factors
We can look at and classify the same results using the outcome categories. Most reports (7 out of 11) that investigated functional recovery, all six reports investigated mortality after hip fracture, and all six articles that included other outcomes found significant associations between social factors and their respective outcomes. Table 4 sum-marises the main findings.
TABLE 4.
The impact of various social factors and their effect on outcomes
| Outcome category | Social theme | ||
|---|---|---|---|
| Social support | Socioeconomic status | Living arrangement | |
| Physical functioning | Eight reports investigated how social support affected physical functional outcome. Six found a significant relationship with functioning measures (e.g. activities of daily living, functional questionnaires) (Allegrante et al., 2007; Cobey et al., 1976; Cree et al., 2001; Cresci, 2001; Magaziner et al., 1990; Oh & Feldt, 2000) and 2 did not (Egan et al., 1992; Marottoli et al., 1992). | One report found on socioeconomic status found a significant improvement to functional outcome (Orive et al., 2016). | Two reports did not find a relationship between living arrangement and functional outcomes (Morghen et al., 2011; Sylliaas et al., 2012) |
| Mortality | One report was found and showed significant positive relationship between lack of social support (i.e. infrequent contact) and mortality (Mortimore et al., 2008). | Four reports (in 3 studies) of a significant positive relationship between socioeconomic status and mortality, with lower socioeconomic markers predicting increased mortality post hip fracture (Kristensen et al., 2017; Shin et al., 2016; Thorne et al., 2016). | One report found a significant positive relationship between living arrangement (i.e. institutionalisation) and mortality (Hongisto et al., 2016). |
| Other outcomes | Three reports found a significant relationship between a social intervention (counselling) and health-related quality of life (Gambatesa et al., 2013), between social isolation and delay in hospital discharge (Landeiro et al., 2016) and between being married and institutionalisation post hip fracture (Marottoli et al., 1994). | One study found that patients with both high education and high income had a lower risk of acute readmission (Kristensen et al., 2017). | Two reports found a significant positive relationship for living arrangement with pain (Orive et al., 2016) and institutionalisation (Hongisto et al., 2016). |
3.7 |. Interventional Studies
Two interventional studies revealed significant positive effects on recovery of patients with hip fracture when the interventions incorporated social intervention (Allegrante et al., 2007; Gambatesa et al., 2013). The first was a randomised controlled study, which introduced counselling in the form of client-centred therapy twice a week for 45 min per session over a period of 30 days, as a form of social support and the authors found that it had a significant positive impact on health-related quality of life of all patients (Gambatesa et al., 2013). Furthermore, the study found that pain levels decreased in those receiving counselling versus the control group (Gambatesa et al., 2013).
The second interventional study implemented a multi-faceted recovery protocol, which included a social support component (Allegrante et al., 2007). Social support was applied, through a postoperative motivational patient videotape, entitled ‘Getting Up Again, Getting Better’, which were delivered to the patient prior to hospital discharge, as well as an in-hospital supportive visit by a recovered hip fracture patient of similar age who had received training in peer counselling and whose visit was intended to model successful recovery and provide social support (Allegrante et al., 2007). The study found the intervention group had a significant positive change in the role-physical scale, of the SF-36, as compared to those in the control group (Allegrante et al., 2007). It is not possible to pool the data from these two studies since the interventions and the outcomes measures used here are different.
4 |. DISCUSSION
Despite the increase in hip fracture events and the fact that social factors demonstrate the potential for aiding the recovery from hip fracture, this topic has rarely been researched, with our search results only procuring 19 papers on the topic. However, within these 19 papers there appears to be a common theme in support of our hypothesis, where social factors are associated with patient recovery outcomes post hip fracture in adults 65 years of age or over.
Social support, socioeconomic factors and living arrangement were the main themes that emerged as social factors affecting recovery outcomes, as measured by physical functional outcomes, mortality and other outcome measures.
The majority of included studies have shown that both a higher level of social support and a better socioeconomic status have a positive effect on the physical functional recovery post hip fracture in individuals over 65 years old (Allegrante et al., 2007; Cobey et al., 1976; Cree et al., 2001; Cresci, 2001; Magaziner et al., 1990; Oh & Feldt, 2000). Social support is a highly variable term, however, common social factors emerged throughout the literature (i.e. social contact, social outings, social network size, marital status, informational support and human contact) as factors to enhance patients recovery post fracture (Allegrante et al., 2007; Cobey et al., 1976; Cree et al., 2001; Cresci, 2001; Magaziner et al., 1990; Oh & Feldt, 2000). Interpreting the cumulative results and paralleling the findings of Allegrante et al., 2007, we postulate that a likely mechanism behind social support is its positive effect on self-efficacy (Allegrante et al., 2007). Self-efficacy has the potential to act as a protective factor, as low self-efficacy, potentially caused by the injury and its consequences, may cause a patient to restrict functioning and negate rehabilitation gains (Petrella et al., 2000). Through social interaction one may receive increased encouragement leading to better psychosocial health, higher confidence or self-efficacy, which could increase compliance to physical rehabilitation programmes and prevent future falls (Allegrante et al., 2007; Magaziner et al., 1990). Social contact may also help alleviate feelings of depression or anxiety, which could be a barrier to patients increasing functional capacity (Scheffers-Barnhoorn et al., 2017).
Socioeconomic status was associated with both physical functional recovery and mortality from hip fracture (Kristensen et al., 2017; Shin et al., 2016; Thorne et al., 2016). Income, employment, education skills and training are all socioeconomic factors that have been studied and found to influence recovery from hip fracture.
Few studies investigated living arrangement before fracture and after discharge from the hospital and its role in recovery after a hip fracture and the results we found were inconsistent. Many factors affect residence, whether pre or after fracture, which makes living arrangement only a proxy for other social and economic factors. In order to examine living arrangements per se, it is necessary to consider reasons for living arrangement. Thus, the role of living arrangement requires further studies to determine its specific effect on recovery from hip fracture.
4.1 |. Implications and future directions
These findings suggest that the recovery programmes for a patient after a hip fracture should not solely focus on the physical aspects and that practitioners can potentially make a meaningful impact on a patient’s recovery by attending to social factors. Hip fracture management should not be limited to only surgery and physical rehabilitation, but social support and psychiatric disorders could also be addressed as needed (Atay, Aslan, Burc, Demirci, & Atay, 2016). It is important to encourage patients to have a quick return to the community, where they should have adequate services available and strategies in place to promote social inclusion (Landeiro et al., 2016). We found only two interventional studies tested the effect of incorporating social factors into rehabilitation programmes, and both revealed significant positive effects on recovery of hip fracture patients (Allegrante et al., 2007; Gambatesa et al., 2013). As shown in this review, patients with good social support systems are more likely to return to independent living and recover their functional ability faster than those with poor social support. For instance incorporating social support into rehabilitation programme could take the form of educating patients and their caregivers on the importance of social and emotional support (i.e. informational support) (Cresci, 2001) and encouraging them to make further social contacts and engage in social activities with their peers when possible. Rehabilitation programmes could offer an extended follow- up phone calls to provide a client-centred counselling to address patients problems, connect them with local resources and answer their questions (Allegrante et al., 2007). This review provides objective information on some of the factors that might be included in the social support interventions when designed. This will help to determine which type of social support is most beneficial at increasing physical functional recovery from hip fracture and/or decreasing mortality from hip fracture. Policy makers could also use the findings from this review to incorporate some of the suggested social interventions into the service plans provided by healthcare systems.
Further investigation is needed to reveal the exact mechanism relating socioeconomic status and hip fracture survival. Revealing these mechanisms should help find the appropriate support measures to increase the probability of survival among patients with low socioeconomic status (Shin et al., 2016). More high-quality studies (e.g. randomised control trials) are needed, specifically studies that implement specific types of social support interventions, such as utilizing age-matched peers who have recovered successfully from hip fracture and telephone contact with peers.
4.2 |. Strengths and limitations
This review has many strengths. First, to the best of our knowledge, this is the first review to summarise evidence on the relationship between social factors and recovery after a hip fracture. Second, almost all steps in the review were completed by two reviewers independently and a third reviewer was consulted in cases of disagreement, which increased the validity of the results. Finally, our search was comprehensive since we did not impose any restrictions on languages, date or study design within our inclusion criteria. Limitations in this study include the lack of studies with rigorous designs, such as randomised controlled trails, to guide our findings and clinical practices. For many of the studies, their results are limited by their small sample size, which decreased power and significance level of the research and therefore affected our findings (Gambatesa et al., 2013; Rathbun et al., 2016). Furthermore, several studies assessed functional status using proxy report, which may be less accurate than an objective evaluation administered by a trained professional (Cenzer et al., 2016; Cree et al., 2001; Hongisto et al., 2016; Mortimore et al., 2008). Another limitation was that we did not search qualitative or grey literature. Finally, given the variability in measuring and reporting outcomes, it was challenging to amalgamate results quantitatively.
In summary, the main findings of this review are that social factors, specifically social support and socioeconomic status seem to influence the physical functional recovery and the mortality rates of individuals 65 and over post hip fracture. However, this is an under researched area and more in-depth studies are needed to look precisely what aspect of social support leads to positive recovery from hip fracture and through which mechanism.
What is known
Hip fractures are associated with high rates of mortality, morbidity and disability.
There is conflicting evidence on the importance of social factors in recovery.
While some studies show little support for social factors’ role in the recovery process, emerging evidence supports a significant role for them, which warrants reviewing available evidence collectively.
What does this add
We found that social factors, specifically social support and socioeconomic status, influence the physical functional recovery and the mortality rates post hip fracture of individuals 65 years and over.
This is an under researched area and more in-depth studies are needed to investigate through which mechanism(s) social factors influence recovery after hip fracture.
APPENDIX 1. Sample search strategy
Using Medline; Performed June 27, 2017 at 10:00 a.m.
| Search Terms Used: |
|---|
| Femoral fracture |
| Hip fracture |
| Femoral neck fracture |
| Femur fracture |
| Socioeconomic factors |
| Sociological factors |
| Social environment |
| Community networks |
| Social support |
| Social |
| Connectedness |
Footnotes
CONFLICT OF INTEREST
We have no conflict of interest to declare.
REFERENCES
- Allegrante JP, Peterson MGE, Cornell CN, MacKenzie CR, Robbins L, Horton R, … Charlson ME (2007). Methodological challenges of multiple-component intervention: Lessons learned from a randomized controlled trial of functional recovery after hip fracture. HSS Journal, 3(1), 63–70. 10.1007/s11420-006-9036-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arksey H, & O’Malley L. (2005). Scoping studies: Towards a methodological framework. International Journal of Social Research Methodology, 8(1), 19–32. 10.1080/1364557032000119616 [DOI] [Google Scholar]
- Atay TM, Aslan A, Burc H, Demirci D, & Atay T. (2016). Is depression associated with functional recovery after hip fracture in the elderly? Journal of Orthopaedics, 13(2), 115–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beaupre LA, Binder EF, Cameron ID, Jones CA, Orwig D, Sherrington C, & Magaziner J. (2013). Maximising functional recovery following hip fracture in frail seniors. Best Practice & Research Clinical Rheumatology, 27(6), 771–788. 10.1016/j.berh.2014.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergström U, Jonsson H, Gustafson Y, Pettersson U, Stenlund H, & Svensson O. (2009). The hip fracture incidence curve is shifting to the right. Acta Orthopaedica, 80(5), 520–524. 10.3109/17453670903278282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cenzer IS, Tang V, Boscardin WJ, Smith AK, Ritchie C, Wallhagen M, … Covinsky KE (2016). One-Year Mortality After Hip Fracture: Development and Validation of a Prognostic Index. Journal of the American Geriatrics Society, 64(9), 1863–1868. 10.1111/jgs.14237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cobey JC, Cobey JH, Conant L, Weil UH, Greenwald WF, & Southwick WO (1976). Indicators of recovery from fractures of the hip. Clinical Orthopaedics and Related Research, (117), 258–262. 10.1097/00003086-197606000-00033 [DOI] [PubMed] [Google Scholar]
- Cree M, Carriere KC, Soskolne CL, & Suarez-Almazor M. (2001). Functional dependence after hip fracture. American Journal of Physical Medicine & Rehabilitation, 80(10), 736–743. 10.1097/00002060-200110000-00006 [DOI] [PubMed] [Google Scholar]
- Cresci K. (2001). The relationship between informational support and post-injury functional status in older women recovering from a hip fracture. Educational Gerontology, 27(3–4), 281–295. 10.1080/036012701750194996 [DOI] [Google Scholar]
- Egan M, Warren SA, Hessel PA, & Gilewich G. (1992). Activities of Daily Living after Hip Fracture: Pre- and Post Discharge. The Occupational Therapy Journal of Research, 12(6), 342–356. 10.1177/153944929201200602 [DOI] [Google Scholar]
- Frost SA, Nguyen ND, Black DA, Eisman JA, & Nguyen TV (2011). Risk factors for in-hospital post-hip fracture mortality. Bone, 49(3), 553–558. https://doi.org/10.1016Zj.bone.2011.06.002 [DOI] [PubMed] [Google Scholar]
- Gambatesa M, D’Ambrosio A, D’Antini D, Mirabella L, DeCapraris A, luso S, …Cinnella G. (2013). Counseling, quality of life, and acute postoperative pain in elderly patients with hip fracture. J Multidiscip Healthc, 6, 335–346. 10.2147/JMDH.S48240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruber-Baldini AL, Zimmerman S, Morrison RS, Grattan LM, Hebel JR, Dolan MM, … Magaziner J. (2003). Cognitive impairment in hip fracture patients: Timing of detection and longitudinal follow-up. Journal of the American Geriatrics Society, 51(9), 12271236. 10.1046/j.1532-5415.2003.51406.x [DOI] [PubMed] [Google Scholar]
- Hongisto MT, Nuotio M, Luukkaala T, Vaisto O, & Pihlajamaki HK (2016). Does cognitive/physical screening in an outpatient setting predict institutionalization after hip fracture? BMC Musculoskeletal Disorders, 17(1), 1–11. 10.1186/s12891-016-1272-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnell O, & Kanis JA (2004). An estimate of the worldwide prevalence, mortality and disability associated with hip fracture. Osteoporosis International, 15(11), 897–902. 10.1007/s00198-004-1627-0 [DOI] [PubMed] [Google Scholar]
- Kristensen PK, Thillemann TM, Pedersen AB, Soballe K, & Johnsen SP (2017). Socioeconomic inequality in clinical outcome among hip fracture patients: A nationwide cohort study. Osteoporosis International, 28(4), 1233–1243. 10.1007/s00198-016-3853-7 [DOI] [PubMed] [Google Scholar]
- Lahtinen A, Leppilahti J, Vähänikkilä H, Harmainen S, Koistinen P, Rissanen P, & Jalovaara P. (2017). Costs after hip fracture in independently living patients: A randomised comparison of three rehabilitation modalities. Clinical Rehabilitation, 31(5), 672–685. 10.1177/0269215516651480 [DOI] [PubMed] [Google Scholar]
- Landeiro F, Gray AM, & Leal J. (2016). Delayed discharges and social isolation in countries with ageing populations: England versus Portugal. European Geriatric Medicine, 7, S221. [Google Scholar]
- Levac D, Colquhoun H, & O’Brien KK (2010). Scoping studies: Advancing the methodology. Implementation Science, 5, 69–69. 10.1186/1748-5908-5-69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magaziner J, Simonsick EM, Kashner TM, Hebel JR, & Kenzora JE (1990). Predictors of functional recovery one year following hospital discharge for hip fracture: A prospective study. The Journal of Gerontology, 45(3), M101–M107. 10.1093/geronj/45.3.M101 [DOI] [PubMed] [Google Scholar]
- Marottoli RA, Berkman LF, & Cooney LM (1992). Decline in physical function following hip fracture. Journal of the American Geriatrics Society, 40(9), 861–866. 10.1111/jM532-5415.1992.tb01980.x [DOI] [PubMed] [Google Scholar]
- Marottoli RA, Berkman LF, Leo-Summers L, & Cooney LM (1994). Predictors of mortality and institutionalization after hip fracture: The New Haven EPESE cohort. Established Populations for Epidemiologic Studies of the Elderly. American Journal of Public Health, 84(11), 1807–1812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morghen S, Bellelli G, Manuele S, Guerini F, Frisoni GB, & Trabucchi M. (2011). Moderate to severe depressive symptoms and rehabilitation outcome in older adults with hip fracture. International Journal of Geriatric Psychiatry, 26(11), 1136–1143. 10.1002/gps.2651 [DOI] [PubMed] [Google Scholar]
- Mortimore E, Haselow D, Dolan M, Hawkes WG, Langenberg P, Zimmerman S, & Magaziner J. (2008). Amount of social contact and hip fracture mortality. Journal of the American Geriatrics Society, 56(6), 1069–1074. 10.1111/j.1532-5415.2008.01706.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Research Council (US), Institute of Medicine (US), Woolf SH, Aron L. (2013). Social factors health in international perspective: Shorter lives, poorer health, (Vol. 6). Washington DC: National Academies Press (US). [PubMed] [Google Scholar]
- Oh H, & Feldt KS (2000). The prognostic factors for functional recovery in elders with hip fracture. Nursing and Health Sciences, 2(4). 237–242. 10.1046/j.1442-2018.2000.00065.x [DOI] [Google Scholar]
- Orive M, Anton-Ladislao A, García-Gutiérrez S, Las Hayas C, González N, Zabala J, & Quintana JM (2016). Prospective study of predictive factors of changes in pain and hip function after hip fracture among the elderly. Osteoporosis International, 27(2), 527536. 10.1007/s00198-015-3267-y [DOI] [PubMed] [Google Scholar]
- Petrella RJ, Payne M, Myers A, Overend T, & Chesworth B. (2000). Physical function and fear of falling after hip fracture rehabilitation in the elderly. American Journal of Physical Medicine & Rehabilitation, 79(2), 154–160. 10.1097/00002060-200003000-00008 [DOI] [PubMed] [Google Scholar]
- Public Health Canada. (2018). Social determinants of health and health inequalities. Available from: https://www.canada.ca/en/public-health/services/healthpromotion/population-health/what-determines-health.html
- Rathbun AM, Shardell M, Orwig D, Gruber-Baldini AL, Ostir G, Hicks GE, …Magaziner J. (2016). Effects of prefracture depressive illness and postfracture depressive symptoms on physical performance after hip fracture. Journal of the American Geriatrics Society, 64(11), e171–e176. 10.1111/jgs.14487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reimers A, & Laflamme L. (2007). Hip fractures among the elderly: Personal and contextual social factors that matter. Journal of Trauma, 62(2), 365–369. 10.1097/01.ta.0000221669.26191.59 [DOI] [PubMed] [Google Scholar]
- Scheffers-Barnhoorn MN, van Haastregt JCM, Schols JMGA, Kempen GIJM, van Balen R, Visschedijk JHM, …van Eijk M. (2017). A multi-component cognitive behavioural intervention for the treatment of fear of falling after hip fracture (FIT-HIP): Protocol of a randomised controlled trial. BMC Geriatrics, 17(1), 71 10.1186/s12877-017-0465-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnell S, Friedman SM, Mendelson DA, Bingham KW, & Kates SL (2010). The 1-year mortality of patients treated in a hip fracture program for elders. Geriatric Orthopaedic Surgery & Rehabilitation, 1(1), 6–14. 10.1177/2151458510378105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shin J, Choi Y, Lee SG, Kim W, Park EC, & Kim TH (2016). Relationship between socioeconomic status and mortality after femur fracture in a Korean population aged 65 years and older: Nationwide retrospective cohort study. Medicine, 95(49), e5311 10.1097/MD.0000000000005311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shyu YI, Liang J, Wu CC, Cheng HS, & Chen MC (2010). An interdisciplinary intervention for older Taiwanese patients after surgery for hip fracture improves health-related quality of life. BMC Musculoskeletal Disorders, 11, 225 10.1186/1471-2474-11-225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sylliaas H, Thingstad P, Wyller TB, Helbostad J, Sletvold O, & Bergland A. (2012). Prognostic factors for self-rated function and perceived health in patient living at home three months after a hip fracture. Disability and Rehabilitation, 34(14), 1225–1231. 10.3109/09638288.2011.643333 [DOI] [PubMed] [Google Scholar]
- Thorne K, Johansen A, Akbari A, Williams JG, & Roberts SE (2016). The impact of social deprivation on mortality following hip fracture in England and Wales: A record linkage study. Osteoporosis International, 27(9), 2727–2737. 10.1007/s00198-016-3608-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, ... Straus SE (2018). Prisma extension for scoping reviews (prisma-scr): Checklist and explanation. Annals of Internal Medicine, 169(7), 467–473. 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- Visschedijk J, Achterberg W, Van Balen R, & Hertogh C. (2010). Fear of falling after hip fracture: A systematic review of measurement instruments, prevalence, interventions, and related factors. Journal of the American Geriatrics Society, 58(9), 1739–1748. 10.1111/j.1532-5415.2010.03036.x [DOI] [PubMed] [Google Scholar]
- Wiktorowicz ME, Goeree R, Papaioannou A, Adachi JD, & Papadimitropoulos E. (2001). Economic implications of hip fracture: Health service use, institutional care and cost in Canada. Osteoporosis International, 12(4), 271–278. 10.1007/s001980170116 [DOI] [PubMed] [Google Scholar]


