Abstract
Background
As stroke survival improves, there is an increasing need for effective, low-cost programs to reduce deconditioning and improve mobility.
Objective
To conduct a phase II trial examining whether the community-based Italian Adaptive Physical Activity exercise program for stroke survivors (APA-Stroke) is safe, effective, and feasible in the United States.
Methods
In this single-blind, randomized controlled trial, 76 stroke survivors with mild to moderate hemiparesis >6 months were randomized to either APA-Stroke (N = 43) or Sittercise (N = 33). APA-Stroke is a progressive group exercise regimen tailored to hemiparesis that includes walking, strength, and balance training. Sittercise, a seated, nonprogressive aerobic upper body general exercise program, served as the control. Both interventions were 1 hour, 3 times weekly, in 5 community locations, supervised by exercise instructors.
Results
A total of 76 participants aged 63.9 ± 1.2 years, mean months poststroke 61.8 ± 9.3, were included. There were no serious adverse events; completion rates were 58% for APA-Stroke, 70% for Sittercise. APA-Stroke participants improved significantly in walking speed. Sample size was inadequate to demonstrate significant between-group differences. Financial and logistical feasibility of the program has been demonstrated. Ongoing APA classes have been offered to >200 participants in county Senior Centers since study completion.
Conclusion
APA-Stroke shows great promise as a low-cost, feasible intervention. It significantly increased walking speed. Safety and feasibility in the US context are demonstrated. A pivotal clinical trial is required to determine whether APA-Stroke should be considered standard of care.
Keywords: stroke, exercise, community-based exercise program, rehabilitation
Introduction
Stroke is a leading cause of long-term disability in the United States and globally.1 Over two-thirds of stroke survivors are left with persistent neurological deficits.2 Chief among them is a hemiparetic gait that limits mobility, increases the risk of falls and fractures,3 and propagates disability through physical deconditioning.4 Stroke survivors spend on average 81% of their day in sedentary activities,5 putting them at increased risk of glucose intolerance,6 diabetes and heart disease,5 depression,7 cognitive impairment,8 declining activities of daily living independence,9 subsequent stroke, and death.10 Indeed, the prevalence of disability after stroke increases steadily with time.11
Increasing evidence links exercise to both functional and preventive benefits for chronic stroke survivors. A recent meta-analysis on trials of aerobic exercise (mostly walking) demonstrated consistent benefit in patient’s gait speed and mobility.12 Exercise also improves cardiovascular health,13 indices of insulin sensitivity and glucose tolerance,6,14,15 physical fitness,12,16,17 bone health,18 depression, and social isolation,15,19,20 even years after the stroke.12,15,20 Exercise has the potential to reduce health care costs for this high-risk population. A randomized controlled trial (RCT) comparing 8 weeks of twice weekly supervised outpatient exercise and education against usual care for patients with mild, nondisabling stroke or transient ischemic attack (TIA) demonstrated significantly lower numbers of recurrent strokes and total hospital costs after 3 years 6 months of follow-up.21 Despite the potential preventive benefits of exercise, there is limited experience translating this research into financially realistic community-based programs that do not involve costly professional staffing and medical testing.22
We present the results of a US research program to evaluate safety, effectiveness, and feasibility of the community-based Adaptive Physical Activity program for Stroke (APA-Stroke), developed and evaluated in Italy. After a successful pilot study,20 the safety and effectiveness of APA-Stroke were evaluated in Tuscany by a quasi-experimental design in comparison with usual care.15 Results were confirmed in an independent nonrandomized controlled study conducted in Bologna where stroke survivors were introduced to an APA-Stroke exercise protocol at the conclusion of rehabilitation.23 Significant improvement on the Modified Barthel Index was sustained at 12 months.24
Because the health system, culture of gyms, and population in Tuscany differ from those in the United States in a number of significant ways, we sought to determine whether APA-Stroke would be feasible in the United States. Key questions include (1) Will the APA-Stroke intervention be successful in attracting and retaining heterogeneous participants recruited from US communities? (2) Will the safety and effectiveness* of APA-Stroke generalize to a US community context? (3) Are the outcomes associated with APA-Stroke due to the exercise program or to the attention and social interaction participants receive? (4) Will APA-Stroke be feasible in the United States once the research program ends?
Methods
This was a randomized, single-blind, controlled trial comparing 2 exercise interventions: APA-Stroke and Sittercise, an attention control. See Figure 1 for the CONSORT (Consolidated Standards of Reporting Trials) diagram. The study protocol was reviewed and approved by the internal review boards (IRBs) of the University of Maryland, Baltimore; MedStar National Rehabilitation Hospital (NRH); and the University of Maryland, Baltimore County. Approval of the Veterans Affairs Maryland Health Care System (VAMHCS) Research Committee was also obtained. The RCT was followed by a nonrandomized translation study in which the Howard County Office on Aging and Independence (OoAI) assumed day-to-day operations for APA-Stroke.
Figure 1.
CONSORT (Consolidated Standards of Reporting Trials) flow diagram for the Adaptive Physical Activity (APA) study.
Settings
In the RCT, classes were offered in 5 community locations. These included 4 OoAI Senior Centers, geographically distributed throughout Howard County. Howard County OoAI was selected because it is part of a national network of community organizations serving seniors, and has experience providing exercise programs for this population. A fifth site was a community-based gym affiliated with NRH in Washington, DC, located at Trinity University. The NRH site was selected to increase diversity of the study population and to provide a more traditional setting for a post rehabilitation exercise program.
Lay exercise instructors were recruited by the OoAI and NRH and were trained in the exercise protocols; they were trained to criteria by research staff and monitored regularly during classes. Exercise instructors were expected to maintain pertinent fitness certification (eg, exercise instructor or personal training) from an accredited certifying agency such as the Athletics and Fitness Association of America (AFAA) or American Council on Exercise (ACE). Cardiopulmonary resuscitation (CPR) certification was also required. Typically, instructors were selected who had previous experience delivering fitness programs to the older adult population. Instructors were then given training specific to the exercise protocols.
Research staff monitored the exercise instructors for treatment fidelity using a checklist that included a specific list of exercises, number of repetitions, walking time (for APA), and observation of whether other procedures were followed (such as taking attendance, following the progression, and fostering positive social interaction). Research staff were able to monitor participant progression by comparing the progression card file, maintained by the exercise instructor, with their own class observations. Treatment fidelity was monitored at least monthly, and when deemed necessary, weekly. When a protocol deviation was noted, this was reviewed with the instructor, and the frequency of monitoring increased.
To maintain the single-blind study design, we had one set of research staff who monitored treatment fidelity and another set of blinded raters who conducted patient assessments. The same instructors and community locations were used for both exercise interventions. Blinded raters collected outcome data; they were unaware of group assignments and not involved in any other aspect of the study.
Interventions
Both interventions provided a supervised, community-based group class, offered for 1 hour, 3 times a week, for 6 months, and featured encouragement by the instructor, as well as interaction with other participants. The basic approach to providing encouragement and interaction was the same for both groups and the same instructors taught each group. However, because of the structure of the exercise intervention, the specifics might vary between the 2 groups. This is illustrated by the following description from one of our instructors:
During the seated exercises, for both groups, we had discussions about everyone’s week and what was going on. … The participants were watching each other, providing encouragement and setting examples for their peers to follow. The participants encouraged each other in both classes. During the classes I would check in with the participants at the beginning of class when taking attendance, getting blood pressures, and during seated exercises. In APA classes, I would talk with individuals while they were walking around the track. I would complement them on how they were doing and encourage them to do another repetition or walk a bit further if they felt up to it, or if it was a transition week and they were supposed to increase their repetitions and walking time.
The APA-Stroke program was designed specifically for individuals with hemiparetic gait deficits due to stroke.15 The manualized protocol provides progressive exercise with components of gait, standing and seated coordination exercises. APA-Stroke exercises are done both standing and seated. The standing exercises are designed to improve lower extremity function, strength, and awareness, and are performed holding onto a bar for support and balance. At the beginning of the class, walking is done around the perimeter of the room and starts with a 6-minute stint done at each participant’s comfortable pace. Next, bar exercises are completed, weight shifts (side to side, forward and back), forward, side, and backward stepping, mezzo squats, leg extensions to back forward and side, and marching in place. After completion of the bar exercises, a series of low-intensity exercises of the upper extremity are performed while seated in a chair. The seated exercises in the APA protocol are designed to improve upper extremity function, strength and awareness in addition to facilitating crossing of the midline. The exercises include arm rotation, trunk rotation, reaching for ankles, and sit to stand. Initially, all bar and seated exercises are done with 5 repetitions per side with rest periods as needed. They progress to 8 and then 10 repetitions per side by the end of week 9. At the end of the class, 6 minutes of walking is done with ropes placed on the floor to serve as obstacles for participants to step around. After the first month, both components of the walking program (nonobstacle and obstacle) are lengthened by a minute each per week, until week 13 when walking time reaches 15 minutes. Time spent on other exercises is correspondingly reduced to maintain the 1-hour time frame.
The program includes a homework component. A manual and log were provided to participants. Exercises included walking, raising arms, lower trunk rotations, bridging, leg stretch, and sit to stand. The time suggested for each exercise was progressively increased, for example, the suggested time for walking began at 6 minutes 3 times per week and increased to 12 minutes 3 times per week over the 26 weeks. Subjects were encouraged to bring their logs to class, but homework logs were not evaluated as part of the study.
The APA intervention was customized to promote safety and individual progress. Each individual was assessed before being admitted to the program. Instructors oriented new participants to the class. Some subjects were able to walk longer and complete exercise repetitions from the beginning and others could not fully progress. Instructors maintained a progression file for each subject. Participants were encouraged to do what they could while being safe and staying within their own limits. At the beginning of each class, as participants checked-in, the instructor reviewed expected repetitions and walking time individually, to remind people what their goals were for the day. During the class, the instructor would talk to each individual, and, where appropriate, encourage them to increase walking time or repetitions for specific exercises. When a participant had completed the number of exercises or walking time for the day, they would rest while others continued. When there were too many new or low functioning participants for the instructor to handle safely alone, an assistant was added.
Sittercise was developed by the Howard County OoAI as an exercise class for frail seniors in their day programs. It is a non-progressive exercise manualized protocol designed for general range-of-motion and minor strengthening for the trunk, arms and legs. The exercises are all performed in a seated position and are not designed with the intent of providing any neurotherapeutic benefit. There is no gait component and no attention is paid to improving function or awareness of any of the limbs. There are no exercises that encourage the crossing of midline and no homework component. Exercises included range of motion for upper and lower extremities, upper extremity exercises with light weights, seated marching, seated toe-taps, hand clapping and beach ball toss.
Recruitment
Community-dwelling subjects were recruited from the VAMHCS in Baltimore, Maryland, NRH, and the community at large. Multiple strategies were used in recruitment. Advertisements were posted in outpatient rehabilitation settings, primary care offices, senior housing, retirement centers, hospitals, churches, senior centers, and grocery stores. Announcements were routinely included in OoAI newsletters and resource hotlines. At NRH, subjects were recruited as they completed formal rehabilitation. Personal contacts by study recruitment staff were ongoing. Additional publicity was generated by public service feature stories in local newspapers and TV stations. Recruitment occurred over 52 months.
Screening and Consent
Interested individuals underwent a preliminary phone screening. If they met screening criteria, they underwent functional assessments, physical exam, and informed consenting.
Inclusion and Exclusion Criteria
Inclusion criteria were the following: age ≥40 years; ≥6 months poststroke with a residual hemiparetic gait deficit; completed all conventional inpatient and outpatient therapy; able to complete the 6-Minute Walking Test (6MWT); able to rise unaided from a chair; Berg Balance Scale (BBS) score >36; and cleared by their personal physician to exercise. Exclusion criteria included a history of active, unstable angina; recent (<3 months) myocardial infarction; congestive heart failure (New York Heart Association category II or higher); poorly controlled hypertension (greater than 180/100 mm Hg on 2 readings separated by 5-minute rest); active cancer or other conditions (orthopedic, circulatory, or chronic pain) restricting exercise; severe receptive or global aphasia with inability to follow 2-step commands; comorbid nonstroke neurological disorders that impair mobility; dementia or untreated clinical depression. Patients with depression were referred to their physician for follow-up and could be enrolled once the depression was adequately treated.
Randomization
Qualified individuals, following informed consent, were block randomized to either the APA-Stroke or Sittercise exercise programs at the site that would be most convenient for them to attend. During the start-up period, an initial group of participants were assigned to APA-Stroke. The purpose of this initial group was to allow the research staff and exercise instructors to gain experience with the community group class format, the exercise protocol, subjects with significant levels of disability, and “rolling enrollments” (where new people were added to the class on an ongoing basis). There were 15 participants assigned to APA-stroke prior to initiating randomization. Sittercise classes were initiated as soon as an adequate number of participants were available.
Outcome Measures
The primary functional outcome was gait velocity, measured using the 6MWT.25 Secondary measures included the BBS,26 the Short Physical Performance Battery (SPPB),27 the 30-foot timed walk,28 and the Stroke Impact Scale (SIS) version 3.0.29 For each measure, our interest was in the change over time. Measures were obtained at baseline, 3 months and 6 months after subjects entered the program. Participants were offered the opportunity, space permitting, to continue to attend whichever type of exercise class they preferred at the end of study participation.
For the 6MWT, we measured the total distance walked with participants using the same assistive devices and/or orthoses they use when walking across a parking lot. They were instructed to cover as much distance as they could over a flat 30.5-m (100-foot) walking surface demarcated by traffic cones during the 6-minute time period. Walking a greater distance during the 6MWT reflects improvement in walking speed and endurance.25 Both the 6MWT and the 30-foot walk are well-established for assessing changes in ambulatory capacity and correlate with function in the community and health status.30–32
Safety
Safety was measured using Study Related Adverse Events, which were further classified as Serious Adverse Events (those which required emergency care or subsequent hospitalization) and Other Adverse Events (those not classified as serious).
Retention and Attendance
For this study, retention was defined as the percentage of randomized subjects who completed the 6-month study. Attendance was defined as the number of classes attended during the 6-month study period. Participants who completed the study maintained an average attendance of at least twice per week until the end of the study period, However, 3 subjects who missed sessions in the first 3 months but who maintained regular attendance thereafter were included in the 6-month data. Thus, the APA group at 6 months includes 1 individual who attended only 40 sessions, and the Sittercise group at 6 months includes 1 individual who attended 37 sessions and 1 who attended 41 sessions.
Statistical Methods
Random effects analysis of variance (ANOVA) was used to compare time course of change in outcomes across baseline, 3 months, and 6 months. We computed the slopes of each outcome variable (i.e. rates of change) with the assumption that intercept (baseline) and slopes were randomly distributed within groups to estimate both within group and between group change over time and determined if the slopes were different using unpaired Student’s t tests. This analysis is preferred over standard ANOVA because it uses all of the available data and avoids the potential bias of excluding subjects for whom we have only 3-month data.33 Results were calculated as intention to treat, in that every randomized subject is included in the final analysis.34
The regression model used does not lend itself to calculation of standardized effect sizes, so to estimate a necessary sample size for the primary outcome variable, the 6MWT, we used simulations. Briefly, we randomly selected subjects, with replacement, from the existing dataset to construct 2000 new datasets each having a fixed number of APA and Sittercise subjects. The 2000 datasets were analyzed, and we determined the fraction of the 2000 that showed a significant difference between the response in the APA versus Sittercise interventions. We continuously varied the fixed number of APA and Sittercise subjects (starting with 50 in each group) until we had a sample size for which 80% of the datasets returned a significant (P < .05) difference between the APA and Sittercise interventions.
We also performed a per-protocol analysis, including only subjects at baseline who completed at least 3 months of exercise classes. Within subject change scores, as well as paired t tests on each outcome variable were calculated.
Financial and Logistical Program Feasibility
At the conclusion of the RCT, a nonrandomized translation study, with a separate IRB protocol, was conducted to enable the research staff to transfer the functions of screening potential participants, as well as training and monitoring instructors, to staff at the OoAI. The research protocols for these functions were adapted for local OoAI use. As the OoAI staff assumed responsibility for all program operations, the research team provided review and consultation. Once this transition was completed, the OoAI assumed all financial and administrative responsibility for the program.
Results
Will the APA intervention be successful in attracting and retaining heterogeneous participants recruited from US communities?
The research study attracted and retained a heterogeneous group of subjects. As shown in Figure 1, 95 potential subjects were screened and consented. Nineteen were judged ineligible or declined prior to randomization. The remaining 76 subjects were randomized to APA or Sittercise. Of APA participants, 58% completed the 6-month intervention and functional tests, compared to 70% of Sittercise participants. Seventeen subjects (9 APA and 8 Sittercise) continued after the completion of the 6-month study. There was no statistically significant difference between the retention rate or number of sessions attended for APA as opposed to Sittercise (test for 2 proportions, P = .30).
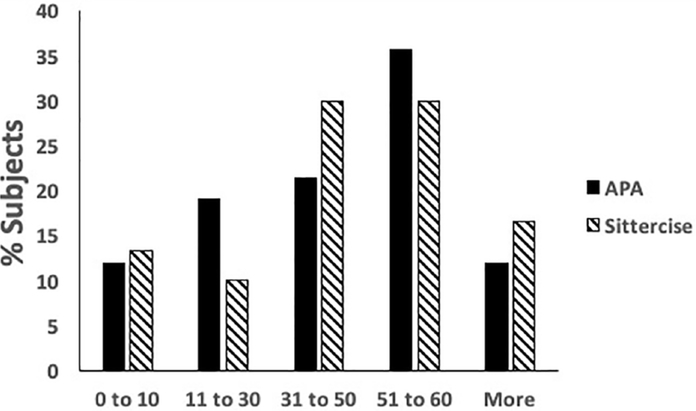
Primary reasons given by subjects for discontinuing participation were intercurrent medical illnesses and transportation. Retention was significantly lower at NRH (P < .04, test for 2 proportions) where difficulty parking, lack of transportation, longer travel times, and generally lower socioeconomic status, posed greater barriers than in Howard County. In Howard County, sites were geographically distributed to maximize access and the county runs a special transportation system for people with disabilities. Although there is a charge for transportation, Howard County is relatively affluent compared to the population served by NRH in the District of Columbia. Attendance records indicate that most participants who dropped out, dropped out after a few sessions. Of the 18 subjects who dropped out of APA, 14 dropped out before 3 months, and of the 10 subjects who dropped out of Sittercise, 7 dropped out before 3 months. As illustrated in Figure 2, the majority of subjects completed more than 50 sessions over the 6-month period. Higher functioning subjects did drop out of Sittercise at a higher rate (see below, however, apart from this, baseline function did not predict attendance—The correlations between 6MWT baseline and days of attendance were not significant for either APA or Sittercise (r2 = .01 and .05, respectively).
Figure 2.
Percentage of subjects in Adaptive Physical Activity (APA) and Sittercise completing numbers of exercise sessions. Maximum possible sessions attended equals 78.
As reported in Table 1, roughly half of the combined Howard County and NRH study population was female. Sixty percent were non-white. Within the parameters of the inclusion/exclusion criteria, participants presented a range of levels of disability. After randomization, the APA and Sittercise groups were well matched. There were no statistically significant differences between the groups in terms of demographics or functional measures at baseline, with the exception of the SPPB subscale for walking (P = .04). The study population was balanced with regard to gender; as expected given the participating sites, African Americans were overrepresented in the study sample compared with the US population. We do not have data on the income or education of the individual subjects; however, Howard County serves a relatively affluent population while NRH has a significant lower income population.
Table 1.
Demographics and Baseline Measures.
| APA |
Sittercise |
||||||
| Variable | n | % | n | % | Pa | ||
| Gender | |||||||
| Female | 21 | 48.8 | 16 | 48.5 | .980 | ||
| Male | 22 | 51.2 | 17 | 51.5 | |||
| Race | |||||||
| White | 17 | 40 | 13 | 39.4 | .060 | ||
| Black | 24 | 57.1 | 14 | 42.4 | |||
| Other | 1 | 2.4 | 6 | 18.2 | |||
| Hemiparesis | |||||||
| Left | 27 | 67.5 | 18 | 58.1 | .410 | ||
| Right | 13 | 32.5 | 13 | 41.4 | |||
| APA |
Sittercise |
||||||
| n | Mean | SE | n | Mean | SE | Pb | |
| Age (years) | 42 | 63.00 | 1.41 | 32 | 65.00 | 2.07 | .137 |
| Years since stroke | 42 | 5.5 | 0.81 | 32 | 4.7 | 1.5 | .630 |
| Berg Balance | 41 | 44.76 | 1.41 | 33 | 43.00 | 1.57 | .408 |
| SPPB | |||||||
| Walk | 42 | 2.60 | 0.19 | 33 | 2.00 | 0.21 | .041 |
| Chair stand | 42 | 1.40 | 0.17 | 33 | 1.33 | 0.19 | .780 |
| Balance | 42 | 2.60 | 0.18 | 33 | 2.73 | 0.20 | .623 |
| Total | 42 | 6.60 | 0.41 | 33 | 6.06 | 0.46 | .392 |
| Six-minute walk (m) | 43 | 189.1 | 14.9 | 33 | 171.7 | 17.0 | .443 |
| SIS | |||||||
| Physical | 36 | 41.00 | 3.82 | 14 | 45.14 | 6.13 | .569 |
| memory | 39 | 64.23 | 6.01 | 26 | 54.69 | 7.36 | .319 |
| emotion | 40 | 76.65 | 3.24 | 28 | 69.54 | 3.87 | .164 |
| commX | 38 | 47.00 | 6.70 | 27 | 52.81 | 7.95 | .578 |
| adl_iadlX | 27 | 61.11 | 4.90 | 16 | 71.00 | 6.37 | .226 |
| mobility | 41 | 74.27 | 4.65 | 25 | 68.12 | 5.95 | .418 |
| handfuncX | 6 | 3.83 | 2.83 | 1 | 1.00 | 6.94 | .721 |
| socialparticX | 38 | 56.18 | 4.42 | 24 | 47.96 | 5.56 | .251 |
| strkrecovery | 42 | 61.90 | 2.96 | 28 | 62.14 | 3.63 | .960 |
| totalscoreX | 42 | 466.62 | 31.13 | 28 | 490.79 | 38.13 | .625 |
| 30-foot walk (m/s) | |||||||
| SlowWkSpd | 41 | 0.60 | 0.04 | 33 | 0.52 | 0.04 | .170 |
| FastWkSpd | 41 | 0.79 | 0.06 | 28 | 0.75 | 0.07 | .631 |
Abbreviations: APA, Adaptive Physical Activity; SPPB, Short Physical Performance Battery; SIS, Stroke Impact Scale; HandfuncX, hand function X; SocialparticX, social participation X; Strkrecovery, stroke recovery; SlowWkSpd, slow walk speed (preferred speed); FastWkSpsd, fastwalk speed; SE, standard error of the mean.
P values compare distribution of subjects in APA versus Sittercise. All P values computed using Pearson’s chi-square analyses except for race, which was analyzed using Fisher’s exact test.
P values compare means of subjects in APA versus Sittercise. All P values computed using one-way analysis of variance.
Will the safety and effectiveness of APA-Stroke, demonstrated in Italy, generalize to a US community context?
The safety record of the Italian APA-Stroke program was replicated in the US study. No study-related serious adverse advents occurred during the study. Minor study-related adverse events were infrequent. A total of 6/43 (13.95%) of APA-Stroke subjects reported minor study related adverse events: faintness (2), shortness of breath (1), chest pain (1), muscle pain (1) or a controlled fall without injury (1). A total of 4/33 (12.12%) of Sittercise subjects reported study-related minor adverse events: muscle pain (2) or experienced a controlled fall without injury (2).
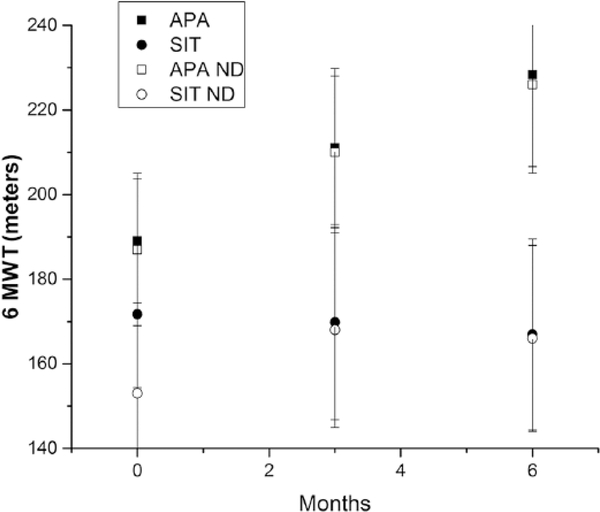
Mean distances walked on the 6MWT for both the APA-Stroke and Sittercise groups are illustrated in Figure 3. Group means and standard errors are plotted for the raw data, as well as for the groups with and without dropouts excluded. The average distance walked in 6 minutes improved from 189 to 228 m for the APA group, and this comparison is not significantly affected by excluding dropouts. The mean distance walked at baseline for those who dropped out of APA prior to 3 months was 191 m, not statistically different from those who continued. However, for the Sittercise group, those who dropped out prior to 3 months walked at baseline an average of 234 m, significantly greater than the average (151 m) for those who continued in Sittercise (t =1.95, P < .05). Thus, exclusion of dropouts depresses the average baseline distance walked by 20 m, for example, the higher functioning subjects dropped out of Sittercise more frequently. The random effects statistical model used to analyze the data adjusts for this difference.
Figure 3.
Mean 6-minute timed walk distances for Adaptive Physical Activity (APA) subjects (squares) and Sittercise subjects (circles) at baseline, 3 months, and 6 months. Filled symbols indicate all subjects, open symbols indicate subjects with dropouts excluded. Error bars indicate standard errors of the mean.
Abbreviations: 6MWT, 6-minute timed walk test; SPPB, Short Physical Performance Battery; SIS, Stroke Impact Scale.
The statistical analysis of the outcome data is presented in Table 2. The slopes of the regression lines obtained from the ANOVA model are multiplied by the 6-month interval to yield mean changes (Delta) in each outcome variable over 6 months for the APA and Sittercise. For the primary outcome variable, the 6MWT, distance over 6 minutes is converted to the clinically important variable, gait speed in cm/s. T-test values are tabulated for the differences between these rates of change and zero (no change) to provide probability estimates and confidence intervals for the changes. The differences between the APA and Sittercise groups are also tabulated and the P values calculated are formally equivalent to the more familiar Group × Time interaction.
Table 2.
Statistical Analysis of Outcome Variables.
| Deltaa | SE | df | t | P | 95% Confidence Limits | |
|---|---|---|---|---|---|---|
| APA 6MWT | 7.6 cm/s | 2.5 | 43 | 3.04 | .004 | 12.6, 2.6 |
| SIT 6MWT | 3.3 cm/s | 2.7 | 43 | 1.25 | .22 | 8.7, −2.1 |
| Difference | 4.3 cm/s | 3.6 | 43 | 1.17 | .25 | 11.5, −2.9 |
| APA 30 ft Walk | 4.6 cm/s | 1.9 | 44 | 2.45 | .02 | 8.4, 0.8 |
| SIT 30 ft Walk | 2.3 cm/s | 2.0 | 44 | 1.15 | .26 | 6.3, −1.7 |
| Difference | 2.3 cm/s | 2.7 | 44 | 0.84 | .41 | 7.7, −3.1 |
| APA SPPB | 0.2 | 0.3 | 43 | 0.62 | .54 | 0.8. −0.4 |
| SIT SPPB | 0.2 | 0.3 | 43 | 0.55 | .59 | 0.8, −0.4 |
| Difference | 0 | 0.5 | 43 | 0.03 | .98 | 1, −1 |
| APA Berg | 1.3 | 1.0 | 44 | 1.23 | .23 | 3.3, −0.7 |
| SIT Berg | 0.2 | 1.1 | 44 | 0.15 | .88 | 2.4, −2.0 |
| Difference | 1.1 | 1.5 | 44 | 0.73 | .47 | 4.1, −1.9 |
| APA SIS total | −3 | 28 | 39 | 0.12 | .90 | 53, −59 |
| SIT SIS total | 27 | 34 | 39 | 0.78 | .44 | 95, −41 |
| Difference | −30 | 44 | 39 | 0.67 | .50 | 58, −114 |
| APA SIS mobility | −0.6 | 4.6 | 38 | 0.13 | .89 | 29.2, 18.8 |
| SIT SIS mobility | 4.1 | 6.5 | 38 | 0.76 | .45 | 50.6, 37.4 |
| Difference | −4.7 | 8.3 | 38 | 0.67 | .51 | 6.3, −26.3 |
Abbreviations: SIT, Sittercise; APA, Adaptive Physical Activity; 6MWT, 6-minute timed walk test; SPPB, Short Physical Performance Battery; SIS, Stroke Impact Scale; SE, standard error of the mean; df, degrees of freedom; SIS.
Delta for each variable is computed by multiplying the slopes obtained for each variable from the random-effects analysis of variance by the 6-month time interval.
The APA group improved significantly (P = .004) on the 6MWT with a mean increase in gait speed of 7.6 cm/s over the 6-month period of the study. The 95% confidence interval for this change was 2.6 to 12.6. Significant improvement was also seen in the 30-foot walk (P = .02). Significant changes were observed neither for the SPPB (P = .54) and Berg (P = .23) nor for the SIS total (P = .90), and SIS mobility subscale (P = .89).
In contrast, the Sittercise group’s speed on the 6MWT did not change significantly (P = .22); nor did their performances in 30-foot walk, SPPB, and BBS. The SIS total score and mobility score also did not improve significantly.
Between group differences were not significantly different on any of the outcome variables measured. The difference of 4.3 cm/s in gait speed for the 6MWT was not statistically different from zero (P = .25), with a 95% confidence interval of −2.9 to 11.5.
With regard to the SIS, a difference emerged between changes observed over time at the different study sites. The change in total SIS score at the NRH site for all subjects (APA and Sittercise) between baseline and 6 months was 50 ± 13, while the change at the Howard County sites was −6 ± 19, significantly different at P = .016 (t score value 2.21). The changes in SIS mobility scores were 15 ± 6 and 2 ± 5, respectively, P = .019 (t score 2.147). No significant differences in changes in gait speed were observed across sites.
In the Tuscan trial, the key measure of balance (BBS) demonstrated significant improvements for the APA-Stroke group at 6 months, both for within-group improvement and when compared with “usual care” controls, whose average BBS declined. To understand why a comparable level of improvement was not seen in the APA-Stroke group in the US trial, we compared the baseline BBS and 6-month change in the BBS, for APA-Stroke participants in the Tuscan and US trials (Table 3). The BBS scores in the Italian APA-Stroke group were, on average, 5.1 points lower at baseline than the US APA group. After 6 months, the Italian APA-Stroke group had improved an average of 5.1 points, so that they were exactly on par with where the US APA-Stroke group started at baseline. This observation may have implications for selection criteria for future research.
Table 3.
Comparison of Baseline Berg Balance Scale (BBS) and 6-Month Change for APA Participants in the US and Italy Research Trials.
| US | Italy | ||
|---|---|---|---|
| Baseline | Change | Baseline | Change |
| (N = 41) | (N = 25) | (N = 49) | (N = 44) |
| (Mean ± SE) | (Mean ± SE) | (Mean ± SE) | (Mean ± SE) |
| 45 ± 1 | 3 ± 2 | 39.9 ± 1.7 | 5.1 ± 1.5 |
Abbreviation: SE, standard error of the mean.
The results of this RCT are reported above using an intention-to-treat analysis. To compare results on the 6MWT with the Italian studies we reanalyzed the data, excluding participants who dropped out prior to 6 months, and using a paired t-test to evaluate change. The change in gait speed was then 6.8 ± 2.8 cm/s for APA-Stroke, significant at P = .02, giving an effect size of 0.47. The comparable values for the APA-Stroke group in Tuscany and Bologna studies were 7.1 and 6.5 cm/s, respectively, while subjects receiving usual care in the Tuscan study actually declined in function.15 The remarkable concordance between these studies gives confidence that this average improvement in gait speed can be expected with an APA intervention. This magnitude of improvement is within the range of the minimally clinically significant difference for patients with chronic diseases (3.9 to 8.5 cm/s).35 The relationship between improvement on the 6MWT in chronic stroke patients and their subjective perception is complex and requires further study.36 The APA intervention in the Tuscan study actually decreased the proportion of subjects classified as severely limited ambulators from 45% to 25%. In the current study, 8 subjects in the APA group were classified as severely impaired ambulators at baseline, and 6 were so classified at 6 months. We note, however, that there is some uncertainty as to the validity of the criterion for severely impaired ambulation.37
Are the outcomes associated with APA-Stroke due to the exercises or to the attention and social interaction participants receive? Would Sittercise, a seated community exercise program already being offered by the OoAI for the frail elderly, work just as well?
Between-group differences (Group × Time) were not significant. A key difference between the results of the current trial and the APA trial in Tuscany, is that the performance of the Tuscan control participants declined with time, allowing statistically significant differences to emerge, whereas the Sittercise subjects in the current study did not decline, so that the absolute difference in gait speed change between the groups was smaller. Our simulations suggest that a study having 155 subjects per group (310 subjects total) would have 80% power to detect a significant difference between APA and Sittercise with a type-I error rate of 5%.
Thus, the study did not have sufficient statistical power to adequately test hypotheses regarding between-group 6-month changes in study outcomes. Our original power calculations, using results from Tuscany where the usual care control group declined, estimated that 88 subjects would need to complete the study to detect statistically significant between group differences for the primary outcome variable (6MWT). Only 91 subjects were enrolled and 48 completed the study—roughly half what would have been needed for sufficient power with our original estimates.
Will APA-Stroke be feasible in the United States once the research program ends? Can community partnerships replicate the role played by the Italian Rehabilitation Service in providing coordination and oversight for the APA-Stroke program?
Feasibility in a US context was assessed based on a determination of whether it was possible for the OoAI to continue offering the APA-Stroke exercise program in local senior centers after conclusion of the RCT. A translation study, requested by the attorneys for the OoAI, assured that the track record for safety could be sustained with OoAI staff assuming responsibility for screening potential participants, and for training and monitoring instructors. There were no study-related serious adverse events during the translation study. For over 3 years, following conclusion of the research program, the OoAI in Howard County Maryland has continued to safely offer classes using the APA-Stroke protocol. Renamed “Better Balance,” the classes are open to participants with a broader range of disabilities than just stroke. Participant recruitment and screening as well as recruitment, training, and fidelity monitoring of instructors is carried out by the OoAI staff. Classes meet at 2 centers and sessions run for 9 to 12 weeks. One exercise instructor teaches a maximum of 12 participants per class.
Discussion
APA-Stroke demonstrated success in attracting and retaining heterogeneous participants in the United States. The overall subject dropout rate was as projected (42%). Retention and attendance were in the range reported in previous community-based exercise programs of 6 months or more duration for stroke38,39 and the frail elderly,40 and is remarkably good for the continued participation over 6 months of a fragile and medically complex population. The 42% dropout rate for APA in the current study also stands in contrast to the up to 65% dropout rate in home exercise programs41 and may represent part of a new model for increasing long-term participation in exercise with therapist engagement.42 Elderly subjects adhere more strongly to supervised exercise programs43 and the APA program potentially could provide therapists with ongoing, longitudinal feedback on patient progress. Perhaps not surprisingly, higher functioning subjects randomized to Sittercise dropped disproportionately, highlighting the difficulty in maintaining participation in an intervention that subjects may perceive as not well tailored to their needs.
Our research staff observed the role of group dynamics in retention, where social bonding and informal mentoring was valued by participants. Attendance, as well as retention, is an important factor in improving patient function through exercise. Koh et al44 found that stroke patients attending greater than 25% of outpatient sessions had better outcomes at 1 year than those who attended less or those who received only a home exercise prescription. A recent RCT on a home exercise program targeted to stroke patients at high fall risk failed to show benefit, but only 25% of the experimental group actually adhered to the program. Post hoc analysis demonstrated that patients with full adherence to the program suffered significantly fewer falls than those who only partially adhered.45 In the present study, the small number of subjects precludes a meaningful analysis of the effects of adherence on improvement in gait speed.
As with most clinical trials, participant recruitment was challenging, highlighting factors that can affect participation in a community exercise research program for stroke survivors. Barriers included clinical providers’ concerns about losing patients to competing health systems and loss of follow-up continuity due to the inclusion criteria that required participants to be >6 months poststroke. This delay may also have limited the effectiveness of APA. Subjects were enrolled in the LEAPS trial within 45 days of stroke.46 In the urban underserved environment of Washington, DC, unreimbursed transportation costs were a particular challenge; reimbursement was statutorily prohibited from reimbursement by our funding agency. This led to high refusal rates by individuals who otherwise were qualified and interested in participating and led to the dropout of participants.
Safety and effectiveness of APA-Stroke, as demonstrated in Italy, can generalize to a US community context. The safety of the APA-Stroke protocol has been well established in Italy15,23 and now replicated in the United States, with appropriate screening of participants, as well as training and monitoring of instructors. The APA group demonstrated significant improvements on the 6MWT and in preferred gait speed, while the Sittercise group did not. This is consistent with the Italian APA research as well as other studies47,48 using short-term supervised exercise training. Another previous study38 employing a once per week intervention supervised by physical therapists supplemented by home exercise also demonstrated comparable increases in the 6MWT.
While between-group differences between APA and Sittercise were not statistically significant in this US study, we attribute this to the small sample size recruited, and the use of an active control, as opposed to the “usual care” control used in the Italian studies. Follow-up evaluations after the end of the study to determine long-term stability of gains in performance were not included due to sample size limitations. This is a limitation of the study and should be addressed in future studies.
Conclusions
APA-Stroke has proven to be safe, feasible, and effective for stroke survivors in home and community settings in three separate trials, conducted in 2 countries featuring very different involvement of the health systems. The APA-Stroke studies provide continuing evidence that, with appropriate screening and exercises, stroke survivors can achieve functional gains. Protocol-specific training and oversight of instructors can ensure participant safety and reassure providers.49
The translational phase of this study provides strong evidence that a community-based exercise program led by lay exercise instructors is sufficiently safe and simple to avoid the need for expensive clinical space and equipment and constant supervision by clinical professionals. APA has the potential to provide a health maintenance intervention that can be offered in community centers, churches, gyms, and retirement communities. By carefully selecting participants, using a simple training program with minimal equipment, and using social interactions to reinforce participation, APA is safe and feasible for community distribution. Moreover, this simple low-cost approach could make access to this program feasible for low-income and underserved communities. We estimate that the per person cost for an APA session can be less than 1/10 the cost of a physical therapy session. Current U.S. guidelines recommend that stroke survivors be referred to ongoing exercise during discharge planning.50 However, the accessibility of fitness centers for people with disabilities remains poor.51 APA-Stroke is consistent with the exercise recommendations developed by the American College of Sports Medicine and the American Physical Therapy Association for maintenance of function and secondary prevention after stroke,52 as well as the Commission on Accreditation of Rehabilitation Facilities,50 and may be useful to Medicare Advantage Plans, assisted living communities, and other population based systems that are interested in preventive health for the elderly.53
Additional improvements could include adding a cardiovascular risk factor management component, or testing whether a tele-presence enhanced home-based version might be equivalent or even superior. Improvements in quality of life (SIS total) for Sittercise participants suggest future research options for nonambulatory populations. The intensity of APA could be increased to include an aerobic component in accordance with recent recommendations.54 The current study was initiated prior to the release of these recommendations, and the APA protocol was specifically designed for community-based implementation to eliminate the need for stress testing, electrocardiography monitoring, and intensive supervision. Starting APA directly after the 8-week aerobic exercise program envisaged by Mackay-Lyons et al.54 could allow for adequate safety screening and still maintain the low-cost structure attractive for community-based implementation. The lack of change in quality-of-life measures (SIS) for the APA group in the current study merits further study, especially because of the obvious social bonding of the participants and long-term adherence. We note that participants in both programs at the NRH site did report significant improvements in quality of life as compared with those at the Howard County sites, suggesting that such programs may be especially valuable for disadvantaged populations.
Finally, we note that a critical design feature for future trials will be that of the control intervention. Our experience suggests that unbiased retention of subjects in the control group may be difficult if subjects do not perceive that the intervention addresses their needs. On the other hand, control interventions that introduce significant exercise, for example, walking from a parking lot on a regular basis, may also introduce effects different from a pure “usual care” control.
Acknowledgments
We wish to acknowledge the support of Starr Sowers, Courtney Barkley, Jennifer Lee, Margot Gianetti, Katie Birger, Fred Ivey, Tara McDonald, Cathy McDonell, Kate Fiske, and Tara Stapleton, among others.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was funded by VA Rehabilitation Research and Development (Project ID # B6329-R).
Footnotes
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
The distinctions between an efficacy study (testing results of an intervention under ideal conditions) and an effectiveness study (a pragmatic trial measuring benefits in a “real world” setting) exist on a continuum.55 We characterize this as an effectiveness study, “designed to evaluate whether interventions produce effects when delivered by endogenous providers … under real world conditions in natural settings with heterogeneous samples.”56
References
- 1.Rosamond W, Flegal K, Friday G, et al. Heart disease and stroke statistics—2007 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2007;115:e69–e171. [DOI] [PubMed] [Google Scholar]
- 2.American Stroke Association, American Heart Association. Heart disease and stroke statistics—2005 update. https://my.clevelandclinic.org/ccf/media/files/heart/1105390918119HDSStats2005Update.pdf. Accessed June 24, 2019.
- 3.Kapral MK, Fang J, Alibhai SM, et al. Risk of fractures after stroke: results from the Ontario Stroke Registry. Neurology. 2017;88:57–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ivey FM, Ryan AS, Hafer-Macko CE, Goldberg AP, Macko RF. Treadmill aerobic training improves glucose tolerance and indices of insulin sensitivity in disabled stroke survivors: a preliminary report. Stroke. 2007;38:2752–2758. [DOI] [PubMed] [Google Scholar]
- 5.Tieges Z, Mead G, Allerhand M, et al. Sedentary behavior in the first year after stroke: a longitudinal cohort study with objective measures. Arch Phys Med Rehabil. 2015;96:15–23. [DOI] [PubMed] [Google Scholar]
- 6.Ivey FM, Ryan AS, Hafer-Macko CE, et al. High prevalence of abnormal glucose metabolism and poor sensitivity of fasting plasma glucose in the chronic phase of stroke. Cerebrovasc Dis. 2006;22:368–371. [DOI] [PubMed] [Google Scholar]
- 7.van de Port IGL, Kwakkel G, Bruin M, Lindeman E. Determinants of depression in chronic stroke: a prospective cohort study. Disabil Rehabil. 2007;29:353–358. [DOI] [PubMed] [Google Scholar]
- 8.Liu-Ambrose T, Best JR, Davis JC, et al. Aerobic exercise and vascular cognitive impairment: a randomized controlled trial. Neurology. 2016;87:2082–2090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ullberg T, Zia E, Petersson J, Norrving B. Changes in functional outcome over the first year after stroke: an observational study from the Swedish stroke register. Stroke. 2015;46:389–394. [DOI] [PubMed] [Google Scholar]
- 10.Fishman EI, Steeves JA, Zipunnikov V, et al. Association between objectively measured physical activity and mortality in NHANES. Med Sci Sports Exerc. 2016;48:1303–1311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Crichton SL, Bray BD, McKevitt C, Rudd AG, Wolfe CD. Patient outcomes up to 15 years after stroke: survival, disability, quality of life, cognition and mental health. J Neurol Neurosurg Psychiatry. 2016;87:1091–1098. [DOI] [PubMed] [Google Scholar]
- 12.Kendall BJ, Gothe NP. Effect of aerobic exercise interventions on mobility among stroke patients: a systematic review. Am J Phys Med Rehabil. 2016;95:214–224. [DOI] [PubMed] [Google Scholar]
- 13.Macko RF, Ivey FM, Forrester LW. Task-oriented aerobic exercise in chronic hemiparetic stroke: training protocols and treatment effects. Top Stroke Rehabil. 2005;12:45–57. [DOI] [PubMed] [Google Scholar]
- 14.Eich HJ, Mach H, Werner C, Hesse S. Aerobic treadmill plus Bobath walking training improves walking in subacute stroke: a randomized controlled trial. Clin Rehabil. 2004;18:640–651. [DOI] [PubMed] [Google Scholar]
- 15.Stuart M, Benvenuti F, Macko R, et al. Community-based adaptive physical activity program for chronic stroke: feasibility, safety, and efficacy of the Empoli model. Neurorehabil Neural Repair. 2009;23:726–734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rimmer JH, Riley B, Creviston T, Nicola T. Exercise training in a predominanttly African-American group of stroke survivors. Med Sci Sports Exerc. 2000;32:1900–1996. [DOI] [PubMed] [Google Scholar]
- 17.Rimmer JH, Wang E. Aerobic exercise training in stroke survivors. Top Stroke Rehabil. 2005;12:17–30. [DOI] [PubMed] [Google Scholar]
- 18.Eng JJ, Pang MYC, Ashe MC. Balance, falls, and bone health: role of exercise in reducing fracture risk after stroke. J Rehabil Res Dev. 2008;45:297–313. [DOI] [PubMed] [Google Scholar]
- 19.Lai SM, Studenski S, Richards L, et al. Therapeutic exercise and depressive symptoms after stroke. J Am Geriatr Soc. 2006;54:240–247. [DOI] [PubMed] [Google Scholar]
- 20.Macko RF, Benvenuti F, Stanhope S, et al. Adaptive physical activity improves mobility function and quality of life in chronic hemiparesis. J Rehabil Res Dev. 2008;45:323–328. [DOI] [PubMed] [Google Scholar]
- 21.Faulkner J, Stoner L, Lanford J, Jolliffe E, Mitchelmore A, Lambrick D. Long-term effect of participation in an early exercise and education program on clinical outcomes and cost implications, in patients with TIA and minor, non-disabling stroke. Transl Stroke Res. 2017;8:220–227. [DOI] [PubMed] [Google Scholar]
- 22.Pang MY, Eng JJ, Dawson AS, McKay HA, Harris JE. A community-based fitness and mobility exercise program for older adults with chronic stroke: a randomized, controlled trial. J Am Geriatr Soc. 2005;53:1667–1674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Taricco M, Dallolio L, Calugi S, et al. ; Esercizio Fisico di Gruppo/2009 Investigators. Impact of adapted physical activity and therapeutic patient education on functioning and quality of life in patients with postacute strokes. Neurorehabil Neural Repair. 2014;28:719–728. [DOI] [PubMed] [Google Scholar]
- 24.Calugi S, Taricco M, Rucci P, et al. ; EFG/2009 Investigators. Effectiveness of adaptive physical activity combined with therapeutic patient education in stroke survivors at twelve months: a non-randomized parallel group study. Eur J Phys Rehabil Med. 2016;52:72–80. [PubMed] [Google Scholar]
- 25.Demers C, McKelvie RS, Negassa A, Yusuf S; RESOLVD Pilot Study Investigators. Reliability, validity, and responsiveness of the six-minute walk test in patients with heart failure. Am Heart J. 2001;142:698–703. [DOI] [PubMed] [Google Scholar]
- 26.Berg K, Wood-Dauphinee S, Williams JI. The Balance Scale: reliability assessment with elderly residents and patients with an acute stroke. Scand J Rehabil Med. 1995;27:27–36. [PubMed] [Google Scholar]
- 27.Guralnik JM, Ferrucci L, Pieper CF, et al. Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. J Gerontol A Biol Sci Med Sci. 2000;55:M221–M231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Perera S, Mody SH, Woodman RC, Studenski SA. Meaningful change and responsiveness in common physical performance measures in older adults. J Am Geriatr Soc. 2006;54:743–749. [DOI] [PubMed] [Google Scholar]
- 29.Rehabilitation Measures Team. Rehab measures: Stroke Impact Scale. https://www.sralab.org/rehabilitation-measures/stroke-impact-scale. Accessed June 24, 2019.
- 30.Studenski S, Perera S, Wallace D, et al. Physical performance measures in the clinical setting. J Am Geriatr Soc. 2003;51:314–322. [DOI] [PubMed] [Google Scholar]
- 31.Studenski S, Perera S, Patel K, et al. Gait speed and survival in older adults. JAMA. 2011;305:50–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schmid A, Duncan PW, Studenski S, et al. Improvements in speed-based gait classifications are meaningful. Stroke. 2007;38:2096–2100. [DOI] [PubMed] [Google Scholar]
- 33.Gueorguieva R, Krystal JH. Move over ANOVA: progress in analyzing repeated-measures data and its reflection in papers published in the Archives of General Psychiatry. Arch Gen Psychiatry. 2004;61310–317. [DOI] [PubMed] [Google Scholar]
- 34.Gupta SK. Intention-to-treat concept: a review. Perspect Clin Res. 2011;2:109–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bohannon RW, Crouch R. Minimal clinically important difference for change in 6-minute walk test distance of adults with pathology: a systematic review. J Eval Clin Pract. 2017;23:377–381. [DOI] [PubMed] [Google Scholar]
- 36.Tang A, Eng JJ, Rand D. Relationship between perceived and measured changes in walking after stroke. J Neurol Phys Ther. 2012;36:115–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dobkin BH, Nadeau SE, Behrman AL, et al. Prediction of responders for outcome measures of Locomotor Experience Applied Post Stroke trial. J Rehabil Res Dev. 2014;51:39–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dean CM, Rissel C, Sherrington C, et al. Exercise to enhance mobility and prevent falls after stroke: the community stroke club randomized trial. Neurorehabil Neural Repair. 2012;26:1046–1057. [DOI] [PubMed] [Google Scholar]
- 39.Tiedemann A, Sherrington C, Dean CM, et al. Predictors of adherence to a structured exercise program and physical activity participation in community dwellers after stroke. Stroke Res Treat. 2012;2012:136525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Brach JS, Perera S, Gilmore S, et al. Effectiveness of a timing and coordination group exercise program to improve mobility in community-dwelling older adults: a randomized clinical trial. JAMA Intern Med. 2017;177:1437–1444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bassett SF. The assessment of patient adherence to physiotherapy rehabilitation. New Zealand J Physiotherapy. 2003;31:60–66. [Google Scholar]
- 42.Morris JH, Williams B. Optimising long-term participation in physical activities after stroke: exploring new ways of working for physiotherapists. Physiotherapy. 2009;95:228–234. [DOI] [PubMed] [Google Scholar]
- 43.Picorelli AM, Pereira LS, Pereira DS, Felicio D, Sherrington C. Adherence to exercise programs for older people is influenced by program characteristics and personal factors: a systematic review. J Physiother. 2014;60:151–156. [DOI] [PubMed] [Google Scholar]
- 44.Koh GC, Saxena SK, Ng TP, Yong D, Fong NP. Effect of duration, participation rate, and supervision during community rehabilitation on functional outcomes in the first poststroke year in Singapore. Arch Phys Med Rehabil. 2012;93:279–286. [DOI] [PubMed] [Google Scholar]
- 45.Batchelor FA, Hill KD, Mackintosh SF, Said CM, Whitehead CH. Effects of a multifactorial falls prevention program for people with stroke returning home after rehabilitation: a randomized controlled trial. Arch Phys Med Rehabil. 2012;93:1648–1655. [DOI] [PubMed] [Google Scholar]
- 46.Nadeau SE, Wu SS, Dobkin BH, et al. ; LEAPS Investigative Team. Effects of task-specific and impairment-based training compared with usual care on functional walking ability after inpatient stroke rehabilitation: LEAPS Trial. Neurorehabil Neural Repair. 2013;27:370–380. [DOI] [PubMed] [Google Scholar]
- 47.Olney SJ, Nymark J, Brouwer B, et al. A randomized controlled trial of supervised versus unsupervised exercise programs for ambulatory stroke survivors. Stroke. 2006;37:476–481. [DOI] [PubMed] [Google Scholar]
- 48.Mudge S, Barber PA, Stott NS. Circuit-based rehabilitation improves gait endurance but not usual walking activity in chronic stroke: a randomized controlled trial. Arch Phys Med Rehabil. 2009;90:1989–1996. [DOI] [PubMed] [Google Scholar]
- 49.Anderson C, Grant RL, Hurley MV. Exercise facilities for neurologically disabled populations—perceptions from the fitness industry. Disabil Health J. 2017;10:157–162. [DOI] [PubMed] [Google Scholar]
- 50.MacDonnell CM. 2011. CARF Stroke Specialty Program Standards Paper presented at: ACRM-ASNR Annual Meeting; October 11–15, 2011; Atlanta, GA. [Google Scholar]
- 51.Calder A, Sole G, Mulligan H. The accessibility of fitness centers for people with disabilities: a systematic review. Disabil Health J. 2018;11:525–536. [DOI] [PubMed] [Google Scholar]
- 52.Billinger SA, Arena R, Bernhardt J, et al. Physical activity and exercise recommendations for stroke survivors: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45:2532–2553. [DOI] [PubMed] [Google Scholar]
- 53.Weinrich M, Stuart M, Benvenuti F. Community-based exercise for chronic disease management: an Italian design for the United States? Neurorehabil Neural Repair. 2014;28: 729–732. [DOI] [PubMed] [Google Scholar]
- 54.Mackaly-Lyons M, Macko R, Eng J, et al. AEROBICS: Aerobic Exercise Recommendations to Optimize Best Practices in Care After Stroke. Ontario, Canada: Heart and Stroke Foundation; 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Gartlehner G, Hansen RA, Nissman D, Lohr KN, Carey TS. A simple and valid tool distinguished efficacy from effectiveness studies. J Clin Epidemiol. 2006;59:1040–1048. [DOI] [PubMed] [Google Scholar]
- 56.Marchand E, Stice E, Rohde P, Becker CB. Moving from efficacy to effectiveness trials in prevention research. Behav Res Ther. 2011;49:32–41. [DOI] [PMC free article] [PubMed] [Google Scholar]