Abstract
Background
China implemented a partial two-child policy (2013) followed by a universal two-child policy (2015), replacing the former one-child policy mandated by the government. The changes affect many aspects of China’s population as well as maternal and infant health, but their potential impact on birth defects (BDs) remains unknown. In this study, we investigated the associations of these policy changes with BDs in Zhejiang Province, China.
Methods and findings
We used data from the BD surveillance system in Zhejiang Province, China, which covers 90 hospitals in 30 urban districts and rural counties, capturing one-third of the total births in this province. To fully consider the time interval between conception and delivery, we defined the one-child policy period as data from 2013 (births from October 2012 to September 2013), the partial two-child policy period as data from 2015 (births from October 2014 to September 2015), and the universal two-child policy period as data from 2017 (births from October 2016 to September 2017). Data from 2009 and 2011 were also used to show the changes in the proportion of births to women with advanced maternal age (35 years and older) prior to the policy changes. Main outcome measures were changes in the proportion of mothers with advanced maternal age, prevalence of BDs, rankings of BD subtypes by prevalence, prenatal diagnosis rate, and live birth rate of BDs over time. A total of 1,260,684 births (including live births, early fetal losses, stillbirths, and early neonatal deaths) were included in the analyses. Of these, 644,973 (51.16%) births were to women from urban areas, and 615,711 (48.84%) births were to women from rural areas. In total, 135,543 (10.75%) births were to women with advanced maternal age. The proportion increased by 85.68%, from 8.52% in 2013 to 15.82% in 2017. However, it had remained stable prior to policy changes. Overall, 23,095 BDs were identified over the policy changes (2013–2017). The prevalence of BDs during 2013, 2015, and 2017 was 245.95, 264.86, and 304.36 per 10,000 births, respectively. Trisomy 21 and other chromosomal defects increased in both risk and ranking from 2013 to 2017 (crude odds ratio [95% confidence interval] 2.13 [1.75–2.60], from ranking 10th to 5th, and 3.63 [2.84–4.69], from ranking 16th to 6th, respectively). The prenatal diagnosis rate increased by 3.63 (2.2–5.1) percentage points (P < 0.001), from 31.10% to 34.72%, and identification of BDs occurred 1.88 (1.81–1.95) weeks earlier (P < 0.001). The live birth rate for infants with BDs born before 28 gestational weeks increased from 1.29% to 11.45%. The major limitations of this observational study include an inability to establish causality and the possible existence of unknown confounding factors, some of which could contribute to BDs.
Conclusions
In this study, we observed significant increases in maternal age and the prevalence of total and age-related anomalies following China’s new two-child policy. Increases in live birth rate for infants with BDs born before 28 gestational weeks suggest that healthcare for very preterm births with BDs may be warranted in the future, as well as updating the definition of perinatal period.
In an observational study, Xiaohui Zhang and colleagues investigate the changes in maternal age and prevalence of congenital anomalies during the enactment of China's universal two-child policy (2013-2017) in Zhejiang Province, China.
Author summary
Why was this study done?
China's birth policy has changed dramatically in recent years, from a one-child policy to a partial two-child policy to the current universal two-child policy. These changes affect many aspects of the Chinese population as well as maternal health.
Birth defects (BDs) or congenital anomalies are structural or functional anomalies occurring in a fetus or newborn and are the leading causes of infant death globally. There are considerable debates on the effects of China's birth policy changes. However, the associations of these changes with BDs are unclear.
What did the researchers do and find?
We used data from the BD surveillance system of Zhejiang Province, including 1.26 million births, to investigate the associations of birth policy changes with BDs.
We found that the proportion of births to women with advanced maternal age (35 years and over) increased by 85.68% with policy changes, from 8.52% in 2013 to 15.82% in 2017. We also found obvious increases in the prevalence of total and age-related anomalies.
The prenatal diagnosis rate also increased over time. Furthermore, the live birth rate for infants with BDs born before 28 gestational weeks increased sharply.
What do these findings mean?
Our findings suggest that, with relaxation of China’s one-child policy, greater attention is needed for women with advanced maternal age and infants with BDs born before 28 gestational weeks.
The major limitations of this observational study include an inability to establish causality and the possible existence of unknown confounding factors, some of which could contribute to BDs.
Introduction
Because China had a resident population of more than 962 million people in 1979 [1], the Chinese government initiated a one-child policy in that year based on fears of overpopulation and related economic, social, and environmental challenges [2]. However, rapid socioeconomic development, a decline in the total fertility rate, pressures owing to an aging population, sex-ratio imbalance, and workforce shortages over recent decades have resulted in increased public awareness of these issues [3]. In November 2013, the Chinese government launched a partial two-child policy, which encouraged couples to have a second child if either parent was a singleton. Following this, a universal two-child policy was officially declared in October 2015, meaning that all families in China are entitled to have two children [4]. By 2016, hospital surveillance data indicated that the number of live births had soared to 17.86 million per year, reflecting a 7.9% increase over 2015 [5].
Some questions remain about the impacts of the birth policy changes on maternal and infant health. To date, the impact of birth policy changes on women’s reproductive decisions, delivery mode, pregnancy complications, pregnancy age, and birth outcomes has been reported [6–11]. An association between certain maternal characteristics and birth defects (BDs) has also been reported, such as maternal age, maternal parity, use of assisted reproductive technology, and diabetes mellitus [12–15]. However, few studies have conducted a comprehensive investigation of the epidemiology of BDs with respect to the birth policy changes in China. BDs or congenital anomalies are defined as structural or functional anomalies occurring in a fetus or newborn and are the leading causes of infant death globally [16–20].
Zhejiang Province is located in southeastern China and is at the forefront of the country’s socioeconomic development, boasting the country’s leading maternal and child health system. In 2015, Zhejiang Province had a resident population of 55.39 million and was ranked fourth in the country for its gross regional product (GRP) (USD 688.56 billion). Moreover, the maternal mortality rate in this province was the lowest in China [1,21]. A BD surveillance system has been in operation in the province since 1990. In this study, we explored and compared BDs in all births before and after the birth policy changes using data from the BD surveillance system of Zhejiang Province, China. We aimed to gain a better understanding of BDs among infants born at all gestational weeks and whether these might be associated with the birth policy changes.
Methods
Study design and population
This was an observational study based on monitoring data from the provincial BD surveillance system in Zhejiang Province, China. To investigate the associations of BDs and policy changes, we planned to conduct this study after obtaining data for 2017. There was no prespecified analysis plan. To fully consider the time interval between conception and delivery, we defined the period of the one-child policy (introduced in 1979) as the data from 2013 (births from October 2012 to September 2013), that of the partial two-child policy (introduced in November 2013) as the data from 2015 (births from October 2014 to September 2015), and the period of the universal two-child policy (introduced in October 2015) period as the data from 2017 (births from October 2016 to September 2017). The system records all births, including live birth, early fetal loss (embryonic or fetal death before 28 gestational weeks), stillbirths (fetal death at 28 gestational weeks or later), and early neonatal deaths (infant death within 7 days after birth). In this study, a total of 1,260,684 births were included. Of these, 644,973 (51.16%) births were to women from urban areas, and 615,711 (48.84%) births were to women from rural areas. In total, 135,543 (10.75%) births were to women aged 35 years and over. Among the total births, 844,503 births were recorded in the surveillance system for the years 2013, 2015, and 2017, representing the periods of birth policy changes in China. The remaining data comprised that from 2009 and 2011, representing periods prior to birth policy changes, to better understand the influence of birth policy changes on maternal age. This study was approved by the Ethics Committee of the Women's Hospital, Zhejiang University School of Medicine (number: 2018KY036).
Data collection
We used data from a hospital-based BD surveillance system in Zhejiang Province. The system covers 90 hospitals from 30 of 89 urban districts and rural counties in this province. The sampling strategy for hospital surveillance was as follows: There are 11 cities in Zhejiang Province. In each city, two to four districts and counties were recruited according to population size and rural and urban distribution. In each selected district or county, hospitals were recruited according to number of births. Annual births captured in this system included one-third of total births in Zhejiang Province. For births with BDs, individual information was collected. However, for births without BDs, no information at the individual level was recorded; only the distribution of birth characteristics was obtained. Mothers of the infants included in this study received routine prenatal care visits at least five to 10 times throughout their pregnancy, according to the prenatal care regulation released by China's Ministry of Health [22]. Individual information relating to births with BDs was collected using a structured form, which included maternal characteristics, antenatal screening, BD diagnosis, birth information, and birth outcomes. Pediatricians and obstetricians with standardized training in BD diagnosis and data collection reviewed the clinical records and extracted data from the maternal health information using the form. Quality control with respect to data completeness, coverage, and validity was performed monthly by staff of the surveillance hospitals, twice a year in local maternal and child health hospitals, and annually at the Women’s Hospital of Zhejiang University School of Medicine.
Criteria of BD diagnosis and variables definition
BDs were diagnosed by obstetricians and pediatricians using ultrasound, genetic, pathology, and laboratory testing. The diagnoses covered 25 BD subtypes based on the International Statistical Classification of Diseases and Related Health Problems 10th Revision (Q00-Q99) [23], including congenital heart defects (CHDs), congenital malformation of the urinary system, cleft lip with cleft palate, cleft lip without cleft palate, cleft palate without cleft lip, polydactyly, syndactyly, congenital hydrocephalus, congenital talipes equinovarus, congenital microtia, other malformation of the external ear as a whole, trisomy 21 syndrome, other chromosomal abnormalities as a whole, hypospadias, anencephaly, spina bifida, encephalocele, omphalocele, limb reduction defects, congenital atresia of the rectum and anus, congenital diaphragmatic hernia, gastroschisis, congenital esophageal atresia, conjoined twins, and exstrophy of the urinary bladder.
We applied commonly used definitions for maternal characteristics [11,24]. Nulliparous was defined as women who had not previously given birth at or after 28 completed weeks of gestation. Advanced maternal age was defined as women aged 35 years or older at delivery. Early fetal loss was defined as embryonic or fetal deaths before 28 gestational weeks. Stillbirth was defined as fetal deaths at 28 gestational weeks or later. Early neonatal deaths were defined as infant death within 7 days after birth. Multiple congenital anomalies were defined as two or more isolated anomalies occurring in a fetus or newborn.
Statistical analysis
Continuous variables are presented as means and standard deviation (SD), and categorical variables are presented as number (N) and percentage. The prevalence of BDs is presented as the number of BDs per 10,000 births. Changes in the characteristics of total births and births with BDs were tested using analysis of variance (ANOVA) for continuous variables and chi-square tests for categorical variables. Cramér’s V and η2 (eta square) were calculated in chi-squared tests and ANOVA, respectively, to estimate effect sizes. Bonferroni correction was performed in multiple comparisons among the time periods. Trend analysis was used to track characteristics over the time frame of policy changes. Line plots and histograms were drawn to show changes in the distribution of women with advanced maternal age over time. In addition to 2013, 2015, and 2017, corresponding surveillance data from 2009 and 2011 were also used in the line plots and histograms to represent periods prior to policy changes in investigating the changes in advanced maternal age. In age-stratified analyses, crude odds ratios (ORs) and 95% confidence intervals (CIs) were calculated to examine the association of policy changes with risk of BDs in each maternal age group, with the one-child policy period being defined as the reference group. BDs with multiple anomalies were divided into subtypes of isolated malformations to calculate the prevalence and live birth rate and ranked in descending order by prevalence. Crude ORs and 95% CIs were also calculated to examine the association of policy changes with the risk of BD subtypes in total births, with the one-child policy period being defined as the reference group. Analysis of BDs was conducted among total BDs, as well as births with BDs occurring before and after 28 gestational weeks, separately, according to the definition of the perinatal period in China [25]. All statistical analyses were performed using Stata version 13 (StataCorp, College Station, TX, United States). P values < 0.05 (two-sided) were considered statistically significant and are otherwise indicated.
Results
Characteristics of total births and changes in the prevalence of BDs
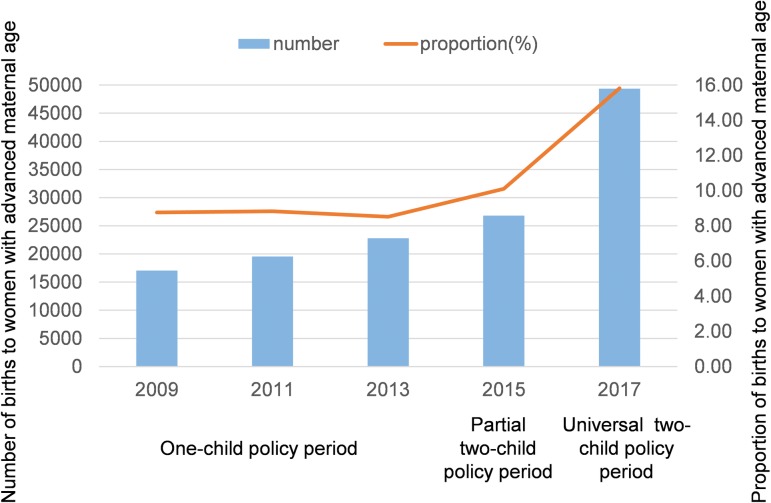
A total of 1,260,684 births were included: 194,712 births in 2009, 221,469 births in 2011, 267,126 births in 2013, 265,277 births in 2015, and 312,100 births in 2017. Changes in birth characteristics over the period of policy changes (in 2013, 2015, and 2017) are shown in Table 1. An increase of 44,974 births occurred over this period. We also observed significant changes in the distributions of maternal age, maternal region, infant sex, and number of embryos (all P < 0.001). The proportion of women who lived in urban areas and the proportion of female infants increased. The proportion of births to women aged 30–34 and ≥35 years increased, whereas the proportion of births to women aged 20–24 and <20 years decreased from 2013 to 2017. The proportion of births to women aged ≥35 years increased by 85.68% with policy changes, from 8.52% in 2013 to 15.82% in 2017; however, no significant increase in the corresponding data was found from 2009 to 2013 prior to changes in the birth policy (Fig 1). The number of BDs increased from 6,570 during the one-child policy period to 9,499 during the universal two-child policy period, whereas the prevalence of BDs increased from 245.95 per 10,000 births to 304.36 per 10,000 births (OR = 1.24, 95% CI 1.21–1.29, P < 0.001) (Table 1). Among BDs, the proportion of multiple anomalies increased from 5.77% during the one-child policy period to 10.36% during the universal two-child policy period (OR = 1.89, 95% CI 1.67–2.14, P < 0.001). Among all BDs, the proportion of BDs among infants born before 28 gestational weeks increased from 16.59% during the one-child policy period to 23.31% during the universal two-child policy period (OR = 1.53, 95% CI 1.41–1.66, P < 0.001).
Table 1. Changes in birth characteristics over the period of policy changes (in 2013, 2015, and 2017).
| Variables | One-child policy period (2013) | Partial two-child policy period (2015) | Universal two-child policy period (2017) | Cramér’s V | P value | |||
|---|---|---|---|---|---|---|---|---|
| N | Percent | N | Percent | N | Percent | |||
| Total births | 267,126 | 100.00 | 265,277 | 100.00 | 312,100 | 100.00 | - | - |
| Maternal age | 0.105 | <0.001 | ||||||
| <20 | 8,623 | 3.23 | 7,841 | 2.96 | 5,849 | 1.87 | ||
| 20–24 | 64,392 | 24.20 | 51,051 | 19.34 | 46,192 | 14.91 | ||
| 25–29 | 116,384 | 43.75 | 117,648 | 44.56 | 125,566 | 40.52 | ||
| 30–34 | 54,962 | 20.58 | 61,935 | 23.35 | 85,124 | 27.27 | ||
| ≥35 | 22,765 | 8.52 | 26,802 | 10.10 | 49,369 | 15.82 | ||
| Maternal region | 0.032 | <0.001 | ||||||
| Urban | 136,193 | 50.98 | 136,049 | 51.29 | 169,789 | 54.40 | ||
| Rural | 130,933 | 49.02 | 129,228 | 48.71 | 142,311 | 45.60 | ||
| Infant sex* | 0.006 | <0.001 | ||||||
| Male | 141,430 | 52.95 | 140,268 | 52.88 | 163,037 | 52.24 | ||
| Female | 125,447 | 46.96 | 124,772 | 47.03 | 148,693 | 47.64 | ||
| Unknown | 194 | 0.07 | 208 | 0.08 | 331 | 0.11 | ||
| No information | 55 | 0.02 | 29 | 0.01 | 39 | 0.01 | ||
| Number of embryos | 0.005 | <0.001 | ||||||
| Single birth | 263,230 | 98.54 | 261,028 | 98.40 | 307,129 | 98.41 | ||
| Multiple births | 3,896 | 1.46 | 4,249 | 1.60 | 4,971 | 1.59 | ||
| Total BDs | 6,570 | 245.95# | 7,026 | 264.86# | 9,499 | 304.36# | 0.015 | <0.001 (trend) |
| Total | 6,570 | 100.00 | 7,026 | 100.00 | 9,499 | 100.00 | ||
| Gestational age | 0.076 | <0.001 (trend) | ||||||
| Born before 28 weeks | 1,090 | 16.59 | 1,248 | 17.76 | 2,214 | 23.31 | ||
| Born at 28 weeks or later | 5,480 | 83.41 | 5,778 | 82.24 | 7,285 | 76.69 | ||
| Type | 0.069 | <0.001 (trend) | ||||||
| Multiple anomalies | 379 | 5.77 | 558 | 7.94 | 984 | 10.36 | ||
| Isolated anomalies | 6,191 | 94.23 | 6,468 | 92.06 | 8,515 | 89.64 | ||
P values and Cramér’s V were derived from chi-squared tests. Ptrend was derived from trend analyses.
*Unknown indicates that infant sex could not be identified; no information indicates missing data on infant sex.
# Prevalence of total BDs presented as number of total BDs per 10,000 births.
Abbreviation: BD, birth defect
Fig 1. Changes in the number and percentage of births to women with advanced maternal age (≥35 years) before and after policy changes.
Bars indicate the number of births to women with advanced maternal age; the line indicates the percentage. Chi-squared tests with Bonferroni correction were performed in multiple comparisons over years. Significant differences in all pairwise comparisons from 2013 to 2017 were observed; no significant increase in all pairwise comparisons from 2009 to 2013 was found (P < 0.0125, adjusted using Bonferroni correction, 0.05/4 tests).
After stratification by maternal age, the higher risk of BDs over the policy change time frame remained significant (Table 2). During the universal two-child policy period, the risk of BDs among births to women in the age groups 20–24, 25–29, 30–34, and ≥35 years was significantly increased compared with during the one-child policy period (20–24 years: OR = 1.38, 95% CI 1.28–1.49, P < 0.001; 25–29 years: OR = 1.22, 95% CI 1.16–1.28, P < 0.001; 30–34 years: OR = 1.11, 95% CI 1.04–1.18, P = 0.002; and ≥35 years: OR = 1.16, 95% CI 1.06–1.27, P < 0.001). In the partial two-child policy period, the prevalence of BDs among births to women aged 20–24 years (OR = 1.15, 95% CI 1.07–1.25, P < 0.001) and ≥35 years (OR = 1.13, 95% CI 1.02–1.24, P = 0.015) was also significantly higher than that during the one-child policy period.
Table 2. Crude ORs (95% CI) for the association between birth policy changes and BDs, stratified by maternal age groups (in 2013, 2015, and 2017).
| Age groups | One-child policy period (2013) | P value | Partial two-child policy period (2015) | P value | Universal two-child policy period (2017) | P value |
|---|---|---|---|---|---|---|
| Total | 1 | - | 1.08 (1.04–1.12) | <0.001 | 1.24 (1.21–1.29) | <0.001 |
| <20 | 1 | - | 1.20 (0.99–1.46) | 0.060 | 1.11 (0.90–1.38) | 0.319 |
| 20–24 | 1 | - | 1.15 (1.07–1.25) | <0.001 | 1.38 (1.28–1.49) | <0.001 |
| 25–29 | 1 | - | 1.05 (1.00–1.11) | 0.058 | 1.22 (1.16–1.28) | <0.001 |
| 30–34 | 1 | - | 0.98 (0.91–1.05) | 0.546 | 1.11 (1.04–1.18) | 0.002 |
| ≥35 | 1 | - | 1.13 (1.02–1.24) | 0.015 | 1.16 (1.06–1.27) | <0.001 |
ORs and 95% CIs were calculated from exposures (policy changes) and cases (BDs). P values were derived from chi-squared tests.
Abbreviations: BD, birth defect; CI, confidence interval; OR, odds ratio
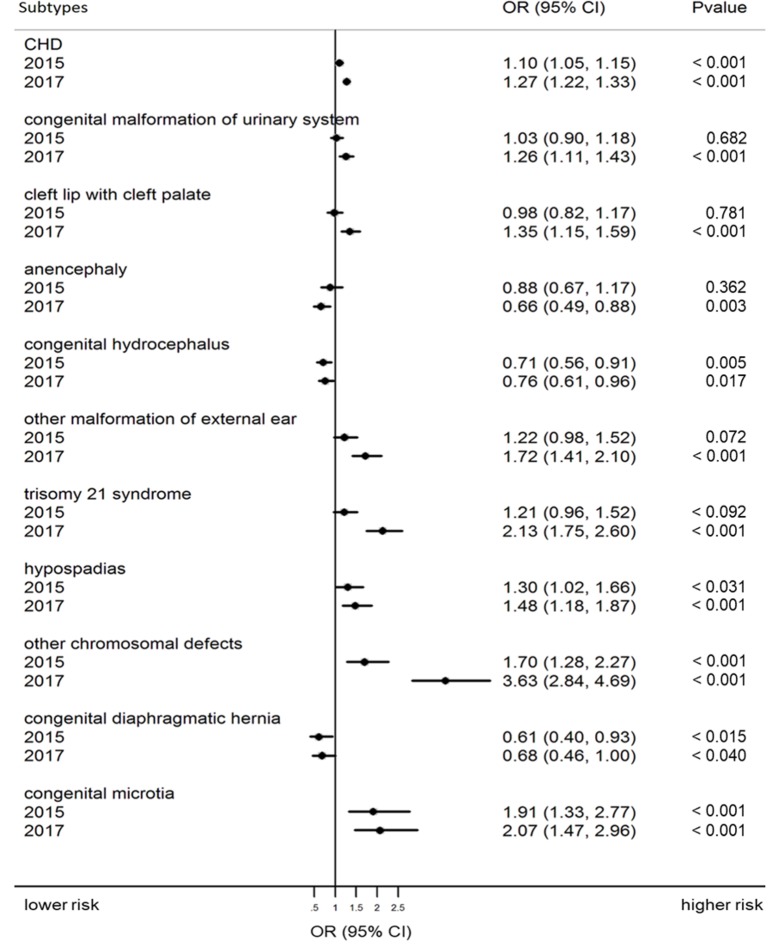
Changes in prevalence and ranking of BD subtypes
Changes in the risks of BD subtypes across policy changes are presented as ORs (95% CI) with P values in S1 Table. Subtypes with significant changes are shown in Fig 2. In the partial and universal two-child policy period, the risk of CHD (partial: OR = 1.10, 95% CI 1.05–1.15, P < 0.001; universal: OR = 1.27, 95% CI 1.22–1.33, P < 0.001), hypospadias (partial: OR = 1.30, 95% CI 1.02–1.66, P = 0.031; universal: OR = 1.48, 95% CI 1.18–1.87, P < 0.001), other chromosomal defects (partial: OR = 1.70, 95% CI 1.28–2.27, P < 0.001; universal: OR = 3.63, 95% CI 2.84–4.69, P < 0.001), and congenital microtia (partial: OR = 1.91, 95% CI 1.33–2.77, P < 0.001; universal: OR = 2.07, 95% CI 1.47–2.96, P < 0.001) increased significantly compared with risks in the one-child policy period. During the universal two-child policy period, the risk of congenital malformation of the urinary system (OR = 1.26, 95% CI 1.11–1.43, P < 0.001), cleft lip with cleft palate (OR = 1.35, 95% CI 1.15–1.59, P < 0.001), other malformation of the external ear (OR = 1.72, 95% CI 1.41–2.10, P < 0.001), and trisomy 21 syndrome (OR = 2.13, 95% CI 1.75–2.60, P < 0.001) also increased significantly compared with risk during the one-child policy period. In the partial and universal two-child policy periods, the risk of congenital hydrocephalus (partial: OR = 0.71, 95% CI 0.56–0.91, P = 0.005; universal: OR = 0.76, 95% CI 0.61–0.96, P = 0.017) and congenital diaphragmatic hernia (partial: OR = 0.61, 95% CI 0.40–0.93, P = 0.015; universal: OR = 0.68, 95% CI 0.46–1.00, P = 0.040) decreased significantly compared with risk in the one-child policy period. The risk of anencephaly also decreased significantly during the partial two-child policy period in comparison with risk in the one-child policy period (OR = 0.66, 95% CI 0.49–0.88, P = 0.003). Table 3 shows the prevalence and ranking of the 25 main types of BD in total births over the period of policy changes. The top four types of BD were the same in all periods: CHD, polydactyly, congenital malformation of the urinary system, and cleft lip with cleft palate. CHDs remained the leading BD across all study periods, with the prevalence increasing from 143.00 per 10,000 births in the one-child policy period to 181.38 per 10,000 births in the universal two-child policy period. CHDs made up 55.12% of the total BDs in the one-child policy period, 56.34% in the partial two-child policy period, and 55.61% in the universal two-child policy period. Trisomy 21 and other chromosomal defects (highlighted in yellow in Table 3) moved up in ranking over the period of policy changes, from 10th and 16th, respectively, in 2013 to fifth and sixth, respectively, in 2017. The ranking of neural tube defects (NTDs) declined, including anencephaly, spina bifida, and encephalocele (highlighted in light purple in Table 3).
Fig 2. Crude ORs (95% CI) and P values for the association between birth policy changes and prevalence of BD subtypes with significant changes in total births (in 2013, 2015, and 2017).
ORs and 95% CIs were calculated from exposures (policy changes) and cases (BDs), with 2013 being defined as the reference group. P values were derived from chi-squared tests. Abbreviations: CHD, congenital heart defect; CI, confidence interval; OR, odds ratio.
Table 3. Ranking of 25 BD subtypes in total BDs over the period of policy changes (in 2013, 2015 and 2017).
| Ranking | One-child policy period (2013) | Partial two-child policy period (2015) | Universal two-child policy period (2017) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| BD subtypes | N | Prevalence (per 10,000 births) | BD subtypes | N | Prevalence (per 10,000 births) | BD subtypes | N | Prevalence (per 10,000 births) | |
| 1 | CHD | 3,820 | 143.00 | CHD | 4,173 | 157.31 | CHD | 5,661 | 181.38 |
| 2 | Polydactyly | 508 | 19.02 | Polydactyly | 532 | 20.05 | Polydactyly | 631 | 20.22 |
| 3 | Congenital malformation of urinary system | 420 | 15.72 | Congenital malformation of urinary system | 429 | 16.17 | Congenital malformation of urinary system | 619 | 19.83 |
| 4 | Cleft lip with cleft palate | 256 | 9.58 | Cleft lip with cleft palate | 248 | 9.35 | Cleft lip with cleft palate | 405 | 12.98 |
| 5 | NTDs | 217 | 8.12 | NTDs | 189 | 7.12 | Trisomy 21 syndrome | 360 | 11.53 |
| Anencephaly | 113 | 4.23 | Anencephaly | 99 | 3.73 | ||||
| Spina bifida | 71 | 2.66 | Spina bifida | 54 | 2.04 | ||||
| Encephalocele | 33 | 1.24 | Encephalocele | 36 | 1.36 | ||||
| 6 | Syndactyly | 171 | 6.40 | Other malformation of external ear | 186 | 7.01 | Other chromosomal defects | 339 | 10.86 |
| 7 | Congenital hydrocephalus | 165 | 6.18 | Trisomy 21 syndrome | 174 | 6.56 | Other malformation of external ear | 309 | 9.90 |
| 8 | Congenital talipes equinovarus | 155 | 5.80 | Syndactyly | 166 | 6.26 | Congenital talipes equinovarus | 221 | 7.08 |
| 9 | Other malformation of external ear | 154 | 5.77 | Congenital talipes equinovarus | 164 | 6.18 | NTDs | 211 | 6.76 |
| Anencephaly | 87 | 2.79 | |||||||
| Spina bifida | 72 | 2.31 | |||||||
| Encephalocele | 52 | 1.67 | |||||||
| 10 | Trisomy 21 syndrome | 145 | 5.43 | Hypospadias | 157 | 5.92 | Hypospadias | 211 | 6.76 |
| 11 | Cleft lip without cleft palate | 142 | 5.32 | Cleft lip without cleft palate | 150 | 5.65 | Syndactyly | 202 | 6.47 |
| 12 | Hypospadias | 122 | 4.57 | Other chromosomal defects | 135 | 5.09 | Congenital hydrocephalus | 147 | 4.71 |
| 13 | Cleft palate without cleft lip | 107 | 4.01 | Congenital hydrocephalus | 117 | 4.41 | Cleft lip without cleft palate | 140 | 4.49 |
| 14 | Limb reduction defects | 106 | 3.97 | Cleft palate without cleft lip | 112 | 4.22 | Congenital atresia of rectum and anus | 119 | 3.81 |
| 15 | Congenital atresia of rectum and anus | 82 | 3.07 | Limb reduction defects | 105 | 3.96 | Cleft palate without cleft lip | 117 | 3.75 |
| 16 | Other chromosomal defects | 80 | 2.99 | Congenital microtia | 91 | 3.43 | Congenital microtia | 116 | 3.72 |
| 17 | Omphalocele | 67 | 2.51 | Congenital atresia of rectum and anus | 83 | 3.13 | Limb reduction defects | 108 | 3.46 |
| 18 | Congenital diaphragmatic hernia | 64 | 2.40 | Omphalocele | 79 | 2.98 | Omphalocele | 86 | 2.76 |
| 19 | Gastroschisis | 54 | 2.02 | Gastroschisis | 47 | 1.77 | Gastroschisis | 63 | 2.02 |
| 20 | Congenital microtia | 48 | 1.80 | Congenital diaphragmatic hernia | 39 | 1.47 | Congenital diaphragmatic hernia | 51 | 1.63 |
| 21 | Congenital esophageal atresia | 34 | 1.27 | Congenital esophageal atresia | 22 | 0.83 | Congenital esophageal atresia | 39 | 1.25 |
| 22 | Conjoined twins | 13 | 0.49 | Conjoined twins | 6 | 0.23 | Conjoined twins | 22 | 0.70 |
| 23 | Exstrophy of urinary bladder | 0 | 0.00 | Exstrophy of urinary bladder | 3 | 0.11 | Exstrophy of urinary bladder | 2 | 0.06 |
Note: yellow indicates chromosomal defects, and light purple indicates NTDs.
Abbreviations: BD, birth defect; CHD, congenital heart defect; NTD, neural tube defect
In further analyses by gestational age, chromosomal defects consistently ranked high in infants with BDs born before 28 gestational weeks (S2 Table). Correspondingly, these were ranked relatively low among BDs in infants born at 28 gestational weeks or later (S3 Table).
Changes in the characteristics of total births with BDs
Table 4 presents the characteristics of total births with BDs. Significant differences in the distributions of maternal age, gravidity, parity, maternal region, birth weight, number of embryos, BD prognosis, and time of diagnosis were found over the years of policy changes (all P < 0.05). Among total BDs, the proportion of births with BDs to women aged 30–34 and ≥35 increased by 18.32% and 73.22%, respectively, whereas the proportion of births with BDs to women aged 20–24 and 25–29 decreased from 2013 to 2017. The prenatal diagnosis rate increased by 3.6 percentage points (95% CI 2.2–5.1, P < 0.001), from 31.10% in 2013 to 34.72% in 2017. The average time of prenatal diagnosis was 1.88 weeks earlier (95% CI 1.81–1.95, P < 0.001) from 2013 to 2017.
Table 4. Changes in characteristics of total infants with BDs (in 2013, 2015, and 2017).
| Variables | One-child policy period (2013) | Partial two-child policy period (2015) | Universal two-child policy period (2017) | Cramér’s V/η2 | P Value | |||
|---|---|---|---|---|---|---|---|---|
| N/mean | Percent | N/mean | Percent | N/mean | Percent | |||
| Total BDs | 6,570 | 100.00 | 7,026 | 100.00 | 9,499 | 100.00 | - | |
| Age | 0.093 | <0.001 | ||||||
| <20 | 210 | 3.20 | 228 | 3.25 | 158 | 1.66 | ||
| 20–24 | 1,416 | 21.55 | 1,291 | 18.37 | 1,390 | 14.63 | ||
| 25–29 | 2,729 | 41.54 | 2,900 | 41.28 | 3,567 | 37.55 | ||
| 30–34 | 1,467 | 22.33 | 1,618 | 23.03 | 2,510 | 26.42 | ||
| ≥35 | 748 | 11.39 | 989 | 14.08 | 1,874 | 19.73 | ||
| Gravidity (5 missing) | 0.082 | <0.001 | ||||||
| 1 | 2,597 | 39.53 | 2,504 | 35.64 | 2,868 | 30.19 | ||
| ≥2 | 3,973 | 60.47 | 4,522 | 64.36 | 6,626 | 69.75 | ||
| Parity (5 missing) | 0.011 | <0.001 | ||||||
| Nulliparous | 635 | 9.67 | 716 | 10.19 | 897 | 9.44 | ||
| Multiparous | 5,935 | 90.33 | 6,310 | 89.81 | 8,597 | 90.55 | ||
| Maternal region (2 missing) | 0.207 | <0.001 | ||||||
| Urban | 3,102 | 47.21 | 4,108 | 58.47 | 6,803 | 71.62 | ||
| Rural | 3,468 | 52.79 | 2,918 | 41.53 | 2,694 | 28.36 | ||
| Infant sex | 0.012 | 0.068 | ||||||
| Male | 3,540 | 53.88 | 3,869 | 55.07 | 5,224 | 55.00 | ||
| Female | 2,815 | 42.85 | 2,935 | 41.77 | 3,928 | 41.35 | ||
| Unknown | 213 | 3.24 | 222 | 3.16 | 347 | 3.65 | ||
| No information | 2 | 0.03 | 0 | 0.00 | 0 | 0.00 | ||
| Low birth weight (75 missing) | 2,586 | 39.52 | 2,923 | 41.60 | 4,056 | 42.92 | 0.028 | <0.001 |
| Number of embryos | 0.034 | <0.001 | ||||||
| Single birth | 6,203 | 94.41 | 6,520 | 92.80 | 8,989 | 94.63 | ||
| Multiple births | 367 | 5.59 | 506 | 7.20 | 510 | 5.37 | ||
| Prognosis (26 missing) | 0.021 | <0.001 | ||||||
| Live birth | 4,754 | 72.39 | 5,260 | 74.86 | 6,893 | 72.74 | ||
| Early fetus loss and stillbirths | 1,718 | 26.16 | 1,672 | 23.80 | 2,486 | 26.23 | ||
| Early neonatal deaths | 95 | 1.45 | 94 | 1.34 | 97 | 1.02 | 0.017 | 0.013 (trend) |
| Time of diagnosis (4 missing) | 0.053 | <0.001 | ||||||
| Postpartum | 4,527 | 68.90 | 4,995 | 71.09 | 6,197 | 65.24 | ||
| Prenatal | 2,043 | 31.10 | 2,031 | 28.91 | 3,298 | 34.72 | ||
| Week (225 missing) | 25.97* | 6.36 | 25.13# | 5.93 | 24.26$ | 5.81 | 0.011 | <0.001 |
Cramér’s V and corresponding P values were derived from chi-squared tests. η2 and corresponding P values were derived from ANOVA. Ptrend was derived from trend analyses.
*Significant differences between one-child policy period and universal two-child policy period, P < 0.05.
#Significant differences between one-child policy period and partial two-child policy period, P < 0.05.
$Significant differences between partial two-child policy period and universal two-child policy period, P < 0.05.
Abbreviations: ANOVA, analysis of variance; BD, birth defect
Changes in BDs among infants born before 28 gestational weeks
Table 5 presents characteristics of infants with BDs who were born before 28 gestational weeks. There were significant differences over the time frame of policy changes in birth weight and the distributions of maternal age, gravidity, parity, maternal region, infant sex, number of births, BD prognosis, and time of diagnosis (all P < 0.05). Compared with the one-child policy period, birth weight was 45.13 grams (95% CI 14.28–75.99, P = 0.004) lower in the partial two-child policy and 65.95 grams (95% CI 38.81–93.08, P < 0.001) lower in the universal two-child policy periods. The proportion of births to women aged ≥35 years approximately doubled, from 12.66% during the one-child policy period to 25.02% in the universal two-child policy period. The change was much greater than that in total BDs (from 11.39% to 19.73%, Table 4). More than 96.39% of infants with BDs who were born before 28 gestational weeks were diagnosed prenatally. The average time of prenatal diagnosis was significantly earlier in the universal two-child policy period than in the partial two-child policy period (P < 0.05). The live birth rate for BDs in infants born before 28 gestational weeks increased sharply, from 1.29% during the one-child policy period to 11.45% during the universal two-child policy period. The proportion of early fetal loss decreased during this time.
Table 5. Changes in characteristics of infants with BDs born before 28 gestational weeks (in 2013, 2015 and 2017).
| Variables | One-child policy period (2013) | Partial two-child policy period (2015) | Universal two-child policy period (2017) | Cramér’s V /η2 | P value | |||
|---|---|---|---|---|---|---|---|---|
| N/mean | Percent/SD | N/mean | Percent/SD | N/mean | Percent/SD | |||
| BDs born before 28 weeks | 1,090 | 100.00 | 1,248 | 100.00 | 2,214 | 100.00 | - | - |
| Maternal age | 0.112 | <0.001 | ||||||
| <20 | 21 | 1.93 | 37 | 2.96 | 27 | 1.22 | ||
| 20–24 | 232 | 21.28 | 220 | 17.63 | 331 | 14.95 | ||
| 25–29 | 445 | 40.83 | 505 | 40.46 | 758 | 34.24 | ||
| 30–34 | 254 | 23.30 | 292 | 23.40 | 544 | 24.57 | ||
| ≥35 | 138 | 12.66 | 194 | 15.54 | 554 | 25.02 | ||
| Gravidity | 0.120 | <0.001 | ||||||
| 1 | 425 | 38.99 | 429 | 34.38 | 574 | 25.93 | ||
| ≥2 | 665 | 61.01 | 819 | 65.63 | 1,640 | 74.07 | ||
| Parity | 0.152 | <0.001 | ||||||
| Nulliparous | 556 | 51.01 | 610 | 48.88 | 774 | 34.96 | ||
| Multiparous | 534 | 49.00 | 638 | 51.12 | 1,440 | 65.05 | ||
| Maternal region | 0.178 | <0.001 | ||||||
| Urban | 515 | 47.25 | 729 | 58.41 | 1,521 | 68.70 | ||
| Rural | 575 | 52.75 | 519 | 41.59 | 693 | 31.30 | ||
| Infant sex | 0.054 | <0.001 | ||||||
| Male | 460 | 42.20 | 610 | 48.88 | 1,141 | 51.54 | ||
| Female | 436 | 40.00 | 430 | 34.46 | 742 | 33.51 | ||
| Unknown | 194 | 17.80 | 208 | 16.67 | 331 | 14.95 | ||
| Birth weight (68 missing) | 737.29* | 387.94 | 692.15# | 368.10 | 671.34 | 360.97 | 0.005 | 0.023 |
| Number of embryos | 0.018 | <0.001 | ||||||
| Single birth | 1,055 | 96.79 | 1,217 | 97.52 | 2,158 | 97.47 | ||
| Multiple births | 35 | 3.21 | 31 | 2.48 | 56 | 2.53 | ||
| Prognosis (15 missing) | 0.197 | <0.001 | ||||||
| Live birth | 14 | 1.29 | 28 | 2.24 | 252 | 11.45 | ||
| Early fetus loss | 1,071 | 98.35 | 1,208 | 96.79 | 1,942 | 88.27 | ||
| Time of diagnosis (1 missing) | 0.063 | <0.001 | ||||||
| Postpartum | 24 | 2.20 | 45 | 3.61 | 31 | 1.40 | ||
| Prenatal | 1,066 | 97.80 | 1,203 | 96.39 | 2,182 | 98.60 | ||
| Week (152 missing) | 21.66 | 3.90 | 21.84 | 3.49 | 21.53$ | 3.86 | 0.001 | <0.001 |
Cramér’s V and corresponding P values were derived from chi-squared tests. η2 and corresponding P values were derived from ANOVA.
*Significant differences between one-child policy period and universal two-child policy period, P < 0.05.
#Significant differences between one-child policy period and partial two-child policy period, P < 0.05.
$Significant differences between partial two-child policy period and universal two-child policy period, P < 0.05.
Abbreviation: ANOVA, analysis of variance; BD, birth defect; SD, standard deviation
Discussion
Using data from over 1.26 million births in 90 representative hospitals of Zhejiang Province, we found that the proportion of women with advanced maternal age increased by 85.68% with policy changes, from 8.52% in 2013 to 15.82% in 2017, whereas it remained stable prior to the policy changes. The proportion of mothers living in urban areas also increased. For changes in BDs, we found significant increases in the prevalence of total and age-related BDs over the years of policy changes. According to the analysis by maternal age, risks of total BDs increased in women aged 20–24, 25–29, 30–34, and ≥35 over the years of policy changes. In terms of BD subtypes, CHD remained the predominant abnormality in the period of changing birth policy, with an increasing trend in prevalence. For birth outcomes, infants with BDs born before 28 gestational weeks demonstrated a sharp increase in the live birth rate throughout the period of policy changes.
Among our findings, of particular interest was the sharp increase in the proportion of women with advanced maternal age across the birth policy changes (8.52% in the one-child policy period to 15.82% in the universal two-child policy period). Although postponing childbirth has increased globally [26,27], the new birth policy in China may have encouraged fertility desires and behaviors among older women. To better identify the effects of these birth policy changes, we reviewed data for the proportion of childbearing women aged ≥35 years before initiation of the new policies. This proportion remained stable from 2009 to 2013, prior to policy changes. However, births to women over age 35 years increased sharply from 2013 to 2017, once the two-child policies were introduced. This finding was also evidenced in Chinese national surveillance data showing that births to women older than 35 years increased from 7.8% to 10.9% since relaxation of the one-child policy [11].
In 2017 (the universal two-child policy period), BDs affected 304.36 per 10,000 births in Zhejiang Province. This prevalence is comparable with reports from the US National Birth Defects Prevention Network (NBDPN), European Surveillance of Congenital Anomalies (EUROCAT), and the national prevalence of Thailand (200–300 per 10,000 births); this prevalence is lower than the national level of Korea (446.3 per 10,000 births) and arctic regions of Russia (361 per 10,000 births) [17,18,28–32]. The variations among the different studies may be attributable to differences in sociodemographic characteristics, inclusion criteria, diagnostic technologies, and methods of case ascertainment. Most countries or regions included in the NBDPN and EUROCAT registries have active population-based programs with multiple data resources and long-term follow-up [17,18]. Although the BD registry in Thailand is hospital based, it includes live births within 1 year after birth [32]. Our study used a hospital-based BD tracking system registering live births, stillbirths, and pregnancy terminations for fetal anomaly at any gestational age.
In terms of BD subtypes among all births, the four most frequent subtypes did not change with changes in the birth policy. CHDs were the most common defect, which is consistent with many previous studies [29,32,33]. The prevalence of CHDs was 181.38 per 10,000 births in 2017, which is far higher than those in most other areas. Of every 10,000 births, 100 births in the US, 65.9 in India, and 137.1 in Norway have CHDs [28,33–36]. Most regions of Zhejiang Province have easy access to echocardiography for routine pediatric examination of newborns. Some diagnoses of CHDs may be revised with increased age of the child. For example, EUROCAT recommends reporting an atrial septum defect 6 months postpartum [18]. Thus, there might be some heterogeneity in CHDs across different studies and an overestimation of CHDs in our study, and the development of diagnostic technology might contribute to the increase in prevalence of CHD.
An increase in congenital anomalies, such as trisomy 21 and other chromosomal anomalies, was found in our study. This finding was consistent with our previous study [37]. Increased maternal age could be one of the explanations. In the present study, the prevalence of trisomy 21 increased from 5.43 in 2013 to 11.53 per 10,000 births in 2017. Globally, the prevalence of trisomy 21 varies among regions; for example, 10.03 per 10,000 births in Europe, 14 per 10,000 births in Austria, 14.5 per 10,000 births in the US, and 1.99 per 10,000 perinatal births in China [17,18,38–40]. However, the proportion of births to women aged ≥35 years in our study in 2017 (15.82%) was similar to that in Austria during 1980–2013 (14%) and slightly lower than Europe (19%) but was much higher than national data for China collected in 2011 (9.20%) [39,40].
As a well-known risk factor [41], increased maternal age might explain part—but not all—of the increases in BDs in the total population and in the older maternal age group and the increase in chromosomal defects. However, there were other explanations, given that the risks for BDs remained increased not only in the older maternal age groups but also in the young maternal age groups following policy changes. Improvements in prenatal screening and prenatal diagnostic technology, as well as changes in the socioeconomic status of parents, could be important factors explaining the increase in total BDs and BD subtypes across all maternal age groups. Coinciding with the start of the two-child policy in 2016, the Chinese government approved noninvasive prenatal testing at the national level. In Zhejiang Province, access to healthcare, maternal serum, and ultrasound screening in the first and second trimesters, as well as clinical assessment prenatally and at birth, have become routinely available and have been improved [42]. Moreover, awareness of prenatal healthcare among women has grown. These factors may also contribute to the increase in total BDs and BD subtypes and the prenatal diagnosis rate of BDs in this study. Our observation that a higher proportion of mothers live in urban areas with birth policy changes (Table 1) might contribute to the increases in BDs because of the more developed diagnostic technology and higher accessibility to healthcare facilities in cities. Previous studies have also reported that lower income, lower educational level, and certain occupations of parents, such as working in cleaning or healthcare occupations, are associated with higher risks for BD subtypes [15,43]. Further studies with detailed information on socioeconomic status are thus needed to determine whether socioeconomic status plays a role in the association between birth policy changes and BDs. Other factors, e.g., increasing multiple births, genetic changes, and environmental exposures, might also contribute to the results [28–30,44]. The impact of improved technology on the surveillance system over time could also have contributed to the increase in total BDs and BD subtypes. For example, the development of diagnostic technologies may have improved the detection rate for minor malformations and chromosomal defects. The development of information technology may also have improved the quality of surveillance.
Conversely, the findings of our study indicate that certain BD subtypes decreased. Enhanced public awareness regarding the prevention of severe BDs from the parents and the measures that have been developed and adopted by the government could be two possible explanations for this finding. Folic acid intake by women before conception and during the first trimester of their pregnancies has been found to be efficacious in preventing NTDs in their offspring [45]. The Zhejiang government provided free folic acid and free consultation service on BD prevention in premarital tests. The finding of a decrease in NTDs was consistent with those of studies worldwide [46,47] and could be attributed to the promotion of folic acid intervention and to greater compliance with the guidelines among parents. Furthermore, in response to possible challenges relating to the birth policy changes, the Chinese government has implemented free prepregnancy screening in rural areas at a national scale and funded a disease-screening program for newborns in poor areas that commenced in 2013 [48,49]. In addition, the improvement in the health literacy of individuals has encouraged greater utilization of healthcare facilities. Other factors associated with these BD subtypes may also have contributed to their decrease. For example, previous studies have reported that genetic and lifestyle factors and socioeconomic status are associated with NTD [50,51]. Further studies are needed to investigate whether these factors play roles in the decrease in certain BD subtypes with birth policy changes.
With the progress in prenatal diagnosis and treatment for infants with BDs, a consistently high live birth rate for total BDs was found in this study (Table 4). In particular, the live birth rate among infants with BDs born before 28 gestational weeks increased from 1.29% during the one-child policy period to 11.45% during the universal two-child policy period. In Europe and the US, the reported BD prevalence includes births irrespective of gestational age [17,18]. However, most studies or monitoring reports of BDs or stillbirths in China have mainly focused on births at 28 completed weeks or later [24,28,34] because the perinatal period starts at 28 complete weeks in China [25]. Nevertheless, WHO suggests that in some developed countries, the perinatal period commences at 22 completed weeks’ gestation [52]. A study in Beijing showed that NTDs at 28 weeks represented only 29.1% of those diagnosed at 13 weeks, highlighting the importance of BD detection prior to 28 completed weeks’ gestation [53]. However, there are few data on BDs in infants born before 28 weeks’ gestation in China. In our study, among those infants from this group who lived, the proportion of CHDs, chromosomal anomalies, and body surface anomalies increased over the time frame of the policy changes. The current Chinese literature on BDs predominantly focuses on perinatal, live births in China [28,34,54,55]. Studies on infants born before 28 gestational weeks whose BDs were identified in the pre-prenatal period are scarce. To better estimate the burden of disease due to BDs, pre-prenatal anomalies, particularly those among infants born at an early gestational age, merit additional attention.
This study has two main strengths. First, the large sample size led to stable and reliable study results. The total number of more than 1.26 million births allowed us to accurately identify several rare BDs. Second, the analysis focused on BDs in three independent periods in line with the birth policy changes. This provides a comprehensive estimation of the associations of policy changes with BDs, yielding evidence for governmental support and resource allocation. There were several limitations of our study as well. First, this observational study could not prove a causal association between the increasing BD prevalence and policy changes. Second, the data used in this study were from a hospital-based BD registry system in Zhejiang. Although a multistage sampling method was used to select hospitals, and the hospital delivery rate in Zhejiang Province was already close to 100% in 2015 [56], a potential lack of representativeness exists. The generalizability of the findings to some other areas of China might be limited owing to the large variation among provinces in socioeconomic development and cultural characteristics. Third, we were unable to identify the infants with BDs born to women who decided to become pregnant based on policy changes because we lacked information on parity of births without BDs. Finally, BDs are multifactorial disorders [16]. However, we could not perform a multivariate analysis for other factors associated with BDs because no individual information for births without BDs was collected—for example, socioeconomic factors, individual genetic backgrounds, and environmental determinants. Further studies are therefore needed to determine whether these factors play a role in the associations between birth policy changes and BDs.
We observed significant changes in maternal characteristics, such as a near double increase in advanced maternal age, and the changes of BDs after the implementation of China’s new two-child policy. Despite the increase in overall prevalence of BDs, CHDs, and chromosomal anomalies, there has been a reduction in lethal anomalies. The increases in risks for BDs in younger maternal age groups also suggested that some other factors (in addition to advanced maternal age) might contribute to the increases in BDs. The prenatal diagnosis rate for BDs has improved over the time frame of the policy changes. The sharp increase in the live birth rate among infants with BDs born before 28 gestational weeks suggests that healthcare for very preterm infants with BDs, as well as updating the definition of the perinatal period, may be warranted in the future. In addition, advocating for improved healthcare for infants with BDs is urgent. Further studies on long-term associations between these birth policy changes and BDs are needed in the future.
Supporting information
STROBE, strengthening the reporting of observational studies in epidemiology.
(DOCX)
BD, birth defect; CI, confidence interval; OR, odds ratio.
(DOCX)
BD, birth defect.
(DOCX)
BD, birth defect.
(DOCX)
Acknowledgments
We would like to thank all the obstetricians, pediatricians, and participants involved in the BD surveillance system for their generous help during the data gathering process.
Abbreviations
- ANOVA
analysis of variance
- BD
birth defect
- CHD
congenital heart defect
- CI
confidence interval
- EUROCAT
European Surveillance of Congenital Anomalies
- GRP
gross regional product
- NBDPN
National Birth Defects Prevention Network
- NTD
neural tube defect
- OR
odds ratio
- SD
standard deviation
Data Availability
The data cannot be shared publicly because we are obligated to protect the privacy of participants within the BD surveillance system of Zhejiang Province, China. Data are available from Chronic Disease Research Institute, School of Public Health, and Women’s Hospital, Zhejiang University School of Medicine, (zjfb@zju.edu.cn), for researchers who meet the criteria for access to confidential data.
Funding Statement
This work was supported by grants from the Cyrus Tang Foundation [419600-11102], the China Medical Board (CMB) Collaborating Program [12-108 and 15-216], and the National Key Research and Development Plan [2018YFC1002700 and 2018YFC1002702]. SZ is funded by the Cyrus Tang Foundation (http://www.tangfoundation.org/) and CMB Collaborating Program (https://chinamedicalboard.org/). XZ works in a project that is supported by the National Key Research and Development Plan. The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.National Bureau of Statistics of China [Internet]. Beijing: National Bureau of Statistics of China; 2019 [cited 2019 Oct 8]. Available from: http://data.stats.gov.cn/english/.
- 2.Jiang Q, Li S, Feldman MW. China’s Population Policy at the Crossroads: Social Impacts and Prospects. Asian J Soc Sci. 2013;41: 193–218. 10.1163/15685314-12341298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Feng W, Gu B, Cai Y. The End of China’s One-Child Policy. Stud Fam Plann. 2016;47: 83–86. 10.1111/j.1728-4465.2016.00052.x [DOI] [PubMed] [Google Scholar]
- 4.Zeng Y, Hesketh T. The effects of China’s universal two-child policy. Lancet. 2016;388: 1930–1938. 10.1016/S0140-6736(16)31405-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.2016 National Economic and Social Development Statistical Bulletin of the People's Republic of China [Internet]. Beijing: National Bureau of Statistics of China; 2017 [cited 2020 Feb 6]. Available from: http://www.stats.gov.cn/tjsj/zxfb/201702/t20170228_1467424.html.
- 6.Schwank SE, Gu C, Cao Z, Andersson E, Jiang H, Ding Y, et al. China’s child policy shift and its impact on Shanghai and Hangzhou women’s decision-making. Int J Womens Health. 2018;10: 639–648. 10.2147/IJWH.S172804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhao J, Shan N, Yang X, Li Q, Xia Y, Zhang H, et al. Effect of second child intent on delivery mode after Chinese two child policy implementation: a cross sectional and prospective observational study of nulliparous women in Chongqing. BMJ Open. 2017;7: e018823 10.1136/bmjopen-2017-018823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang E, Hesketh T. Large reductions in cesarean delivery rates in China: a qualitative study on delivery decision-making in the era of the two-child policy. BMC Pregnancy Childbirth. 2017;17: 405 10.1186/s12884-017-1597-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang H-X, Zhao Y-Y, Wang Y-Q. Analysis of the Characteristics of Pregnancy and Delivery before and after Implementation of the Two-child Policy. Chin Med J (Engl). 2018;131: 37–42. 10.4103/0366-6999.221268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zeng C, Yang M, Ding Y, Duan S, Zhou Y. Placenta accreta spectrum disorder trends in the context of the universal two-child policy in China and the risk of hysterectomy. Int J Gynaecol Obstet. 2018;140: 312–318. 10.1002/ijgo.12418 [DOI] [PubMed] [Google Scholar]
- 11.Liang J, Mu Y, Li X, Tang W, Wang Y, Liu Z, et al. Relaxation of the one child policy and trends in caesarean section rates and birth outcomes in China between 2012 and 2016: observational study of nearly seven million health facility births. BMJ. 2018;360: k817 10.1136/bmj.k817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yang M, Fan X-B, Wu J-N, Wang J-M. Association of assisted reproductive technology and multiple pregnancies with the risks of birth defects and stillbirth: A retrospective cohort study. Sci Rep. 2018;8: 8296 10.1038/s41598-018-26567-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McNeese ML, Selwyn BJ, Duong H, Canfield M, Waller DK. The association between maternal parity and birth defects. Birth Defects Res A Clin Mol Teratol. 2015;103: 144–156. 10.1002/bdra.23360 [DOI] [PubMed] [Google Scholar]
- 14.Ameen SK, Alalaf SK, Shabila NP. Pattern of congenital anomalies at birth and their correlations with maternal characteristics in the maternity teaching hospital, Erbil city, Iraq. BMC Pregnancy Childbirth. 2018;18: 501 10.1186/s12884-018-2141-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Correa A, Gilboa SM, Besser LM, Botto LD, Moore CA, Hobbs CA, et al. Diabetes mellitus and birth defects. Am J Obstet Gynecol. 2008;199: 237.e1–237.e9. 10.1016/j.ajog.2008.06.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Christianson A, Howson CP, Modell B. March of Dimes global report on birth defects. White Plains, New York: March of Dimes Birth Defects Foundation; 2006. [cited 2019 Jan 22]. Available from: http://www.marchofdimes.com/downloads/Birth_Defects_Report-PF.pdf. [Google Scholar]
- 17.Centers for Disease Control and Prevention [Internet]. Data & Statistics on Birth Defects. Atlanta: Centers for Disease Control and Prevention; 2018. April 30 [cited 2019 Jan 10]. Available from: https://www.cdc.gov/ncbddd/birthdefects/data.html. [Google Scholar]
- 18.European Commission [Internet]. Cases and prevalence (per 10,000 births) for all full member registries from 2012 to 2016. EUROCAT. European Commission; 2019 [cited 2019 Jan 10]. Available from: http://www.eurocat-network.eu/accessprevalencedata/prevalencetables
- 19.Bairoliya N, Fink G. Causes of death and infant mortality rates among full-term births in the United States between 2010 and 2012: An observational study. PLoS Med. 2018;15: e1002531 10.1371/journal.pmed.1002531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ko HS, Kim DJ, Chung Y, Wie JH, Choi SK, Park IY, et al. A national cohort study evaluating infant and fetal mortality caused by birth defects in Korea. BMJ Open. 2017;7: e017963 10.1136/bmjopen-2017-017963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liang J, Li X, Kang C, Wang Y, Kulikoff XR, Coates MM, et al. Maternal mortality ratios in 2852 Chinese counties, 1996–2015, and achievement of Millennium Development Goal 5 in China: a subnational analysis of the Global Burden of Disease Study 2016. Lancet. 2019;393: 241–252. 10.1016/S0140-6736(18)31712-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.China’s Ministry of Health. Prenatal Care Regulation. Jun 23, 2011 [cited 2019 Mar 4]. Available from: http://www.nhc.gov.cn.
- 23.International Statistical Classification of Diseases and Related Health Problems 10th Revision [Internet]. In: ICD-10 Version:2016. Geneva: World Health Organization; [cited 2019 Mar 4]. Available from: https://icd.who.int/browse10/2016/en#/XVII.
- 24.Zhu J, Liang J, Mu Y, Li X, Guo S, Scherpbier R, et al. Sociodemographic and obstetric characteristics of stillbirths in China: a census of nearly 4 million health facility births between 2012 and 2014. Lancet Glob Health. 2016;4: e109–118. 10.1016/S2214-109X(15)00271-5 [DOI] [PubMed] [Google Scholar]
- 25.Xie X, Gou W, Lin Z, Di W, Ma D, Kong B. Prenatal Examination and Antenatal Care. Obstetrics and Gynecology. 8th ed Beijing: People’s Health Publishing House; 2013. p. 142. [Google Scholar]
- 26.Behboudi-Gandevani S, Ziaei S, Farahani FK, Jasper M. The Perspectives of Iranian Women on Delayed Childbearing: A Qualitative Study. J Nurs Res. 2015;23: 313–321. 10.1097/JNR.0000000000000084 [DOI] [PubMed] [Google Scholar]
- 27.Goisis A, Sigle-Rushton W. Childbearing Postponement and Child Well-being: A Complex and Varied Relationship? Demography. 2014;51: 1821–1841. 10.1007/s13524-014-0335-4 [DOI] [PubMed] [Google Scholar]
- 28.Xie D, Yang T, Liu Z, Wang H. Epidemiology of Birth Defects Based on a Birth Defect Surveillance System from 2005 to 2014 in Hunan Province, China. PLoS ONE. 2016;11: e0147280 10.1371/journal.pone.0147280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Morris JK, Springett AL, Greenlees R, Loane M, Addor M-C, Arriola L, et al. Trends in congenital anomalies in Europe from 1980 to 2012. PLoS ONE. 2018;13: e0194986 10.1371/journal.pone.0194986 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Postoev VA, Nieboer E, Grjibovski AM, Odland JØ. Prevalence of birth defects in an Arctic Russian setting from 1973 to 2011: a register-based study. Reprod Health. 2015;12: 3 10.1186/1742-4755-12-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ko J-K, Lamichhane DK, Kim H-C, Leem J-H. Trends in the Prevalences of Selected Birth Defects in Korea (2008–2014). Int J Environ Res Public Health. 2018;15: 923 10.3390/ijerph15050923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pangkanon S, Sawasdivorn S, Kuptanon C, Chotigeat U, Vandepitte W. Establishing of National Birth Defects Registry in Thailand. J Med Assoc Thai. 2014;97 Suppl 6: S182–8. [PubMed] [Google Scholar]
- 33.Bhide P, Gund P, Kar A. Prevalence of Congenital Anomalies in an Indian Maternal Cohort: Healthcare, Prevention, and Surveillance Implications. PLoS ONE. 2016;11: e0166408 10.1371/journal.pone.0166408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wu L, Li B, Xia J, Ji C, Liang Z, Ma Y, et al. Prevalence of congenital heart defect in Guangdong province, 2008–2012. BMC Public Health. 2014;14: 152 10.1186/1471-2458-14-152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Leirgul E, Fomina T, Brodwall K, Greve G, Holmstrøm H, Vollset SE, et al. Birth prevalence of congenital heart defects in Norway 1994–2009—A nationwide study. Am Heart J. 2014;168: 956–964. 10.1016/j.ahj.2014.07.030 [DOI] [PubMed] [Google Scholar]
- 36.Egbe A, Uppu S, Lee S, Stroustrup A, Ho D, Srivastava S. Temporal Variation of Birth Prevalence of Congenital Heart Disease in the United States. Congenit Heart Dis. 2015;10: 43–50. 10.1111/chd.12176 [DOI] [PubMed] [Google Scholar]
- 37.Zhang X-H, Qiu L-Q, Ye Y-H, Xu J. Chromosomal abnormalities: subgroup analysis by maternal age and perinatal features in zhejiang province of China, 2011–2015. Ital J Pediatr. 2017;43 10.1186/s13052-017-0363-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Maxwell S, Bower C, O’Leary P. Impact of prenatal screening and diagnostic testing on trends in Down syndrome births and terminations in Western Australia 1980 to 2013. Prenat Diagn. 2015;35: 1324–1330. 10.1002/pd.4698 [DOI] [PubMed] [Google Scholar]
- 39.Loane M, Morris JK, Addor M-C, Arriola L, Budd J, Doray B, et al. Twenty-year trends in the prevalence of Down syndrome and other trisomies in Europe: impact of maternal age and prenatal screening. Eur J Hum Genet. 2013;21: 27–33. 10.1038/ejhg.2012.94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Deng C, Yi L, Mu Y, Zhu J, Qin Y, Fan X, et al. Recent trends in the birth prevalence of Down syndrome in China: impact of prenatal diagnosis and subsequent terminations. Prenat Diagn. 2015;35: 311–318. 10.1002/pd.4516 [DOI] [PubMed] [Google Scholar]
- 41.Goldberg MF. Reducing Birth Defect Risk in Advanced Maternal Age. JAMA. 1979;242: 2292–2294. 10.1001/jama.1979.03300210018013 [DOI] [PubMed] [Google Scholar]
- 42.Department of Maternal and Child Health [Internet]. Circular of the General Office of the State Health and Family Planning Commission on standardizing and orderly Prenatal screening and diagnosis of Fetal Free DNA in Peripheral Blood of pregnant Women. Beijing: Department of Maternal and Child Health; 2016. [cited 2019 May 9]. Available from: http://www.nhc.gov.cn/fys/s3581/201611/0e6fe5bac1664ebda8bc28ad0ed68389.shtml?from=groupmessage&isappinstalled=0. [Google Scholar]
- 43.Brender J, Suarez L, Hendricks K, Baetz RA, Larsen R. Parental Occupation and Neural Tube Defect-Affected Pregnancies Among Mexican Americans. J Occup Environ Med. 2002;44: 650–656. 10.1097/00043764-200207000-00011 [DOI] [PubMed] [Google Scholar]
- 44.Zhang X-H, Qiu L-Q, Huang J-P. Risk of birth defects increased in multiple births. Birth Defects Res A Clin Mol Teratol. 2011;91: 34–38. 10.1002/bdra.20725 [DOI] [PubMed] [Google Scholar]
- 45.Castillo-Lancellotti C, Tur JA, Uauy R. Impact of folic acid fortification of flour on neural tube defects: a systematic review. Public Health Nutr. 2013;16: 901–911. 10.1017/S1368980012003576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Khoshnood B, Loane M, de Walle H, Arriola L, Addor M-C, Barisic I, et al. Long term trends in prevalence of neural tube defects in Europe: population based study. BMJ. 2015;351: h5949 10.1136/bmj.h5949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zhang T-N, Gong T-T, Chen Y-L, Wu Q-J, Zhang Y, Jiang C-Z, et al. Time trends in the prevalence and epidemiological characteristics of neural tube defects in Liaoning Province, China, 2006–2015: A population-based study. Oncotarget. 2017;8: 17092–17104. 10.18632/oncotarget.15060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Department of Maternal and Child Health [Internet]. Circular of the Ministry of Finance of the State population and Family Planning Commission on promoting the full coverage of the National Free Pre-pregnancy Health examination Project. Beijing: Department of Maternal and Child Health; 2013. [cited 2019 Jan 10]. Available from: http://www.nhc.gov.cn/fys/s3589/201307/0ca30a6cbe7146fba86b0bf9211be576.shtml. [Google Scholar]
- 49.Department of Maternal and Child Health [Internet]. The project of newborn screening in poor area in 2013, China. Beijing: Department of Maternal and Child Health; 2013. [cited 2019 Dec 2]. Available from: http://www.nhc.gov.cn/fys/s3585/201311/4ce5a095f552423d82fcd0738cc13102.shtml. [Google Scholar]
- 50.Zheng J, Lu X, Liu H, Zhao P, Li K, Li L. MTHFD1 polymorphism as maternal risk for neural tube defects: a meta-analysis. Neurol Sci. 2015;36: 607–616. 10.1007/s10072-014-2035-7 [DOI] [PubMed] [Google Scholar]
- 51.Desrosiers TA, Siega-Riz AM, Mosley BS, Meyer RE, National Birth Defects Prevention Study. Low carbohydrate diets may increase risk of neural tube defects. Birth Defects Res. 2018;110: 901–909. 10.1002/bdr2.1198 [DOI] [PubMed] [Google Scholar]
- 52.World Health Organization [Internet]. Maternal and perinatal health. Geneva, Switzerland: World Health Organization; [cited 2019 Jan 28]. Available from: https://www.who.int/maternal_child_adolescent/topics/maternal/maternal_perinatal/en/.
- 53.Jin L, Jin L, Yu J, Xu Y, Liu H, Ren A. Prevalence of Neural Tube Defects and the Impact of Prenatal Diagnosis in Three Districts of Beijing, China. Paediatr Perinat Epidemiol. 2017;31: 293–300. 10.1111/ppe.12354 [DOI] [PubMed] [Google Scholar]
- 54.Pei L, Kang Y, Zhao Y, Yan H. Prevalence and risk factors of congenital heart defects among live births: a population-based cross-sectional survey in Shaanxi province, Northwestern China. BMC Pediatr. 2017;17: 18 10.1186/s12887-017-0784-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zhao W, Chen F, Wu M, Jiang S, Wu B, Luo H, et al. Postnatal Identification of Trisomy 21: An Overview of 7,133 Postnatal Trisomy 21 Cases Identified in a Diagnostic Reference Laboratory in China. PLoS ONE. 2015;10: e0133151 10.1371/journal.pone.0133151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Zhang Y, Zhou Y, Li H, Gao Y, Zhang Y, Luo S, et al. Secular trends of institutional delivery rate in China from 1996 to 2015. Natl Med J China. 2017;97: 1337–1342. 10.3760/cma.j.issn.0376-2491.2017.17.014 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
STROBE, strengthening the reporting of observational studies in epidemiology.
(DOCX)
BD, birth defect; CI, confidence interval; OR, odds ratio.
(DOCX)
BD, birth defect.
(DOCX)
BD, birth defect.
(DOCX)
Data Availability Statement
The data cannot be shared publicly because we are obligated to protect the privacy of participants within the BD surveillance system of Zhejiang Province, China. Data are available from Chronic Disease Research Institute, School of Public Health, and Women’s Hospital, Zhejiang University School of Medicine, (zjfb@zju.edu.cn), for researchers who meet the criteria for access to confidential data.