Abstract
Introduction
Glycemic targets and glucose-lowering regimens should be individualized based on multiple factors, including the presence of comorbidities. We examined contemporary patterns of glycemic control and use of medications known to cause hypoglycemia among adults with diabetes across age and multimorbidity.
Research design and methods
We retrospectively examined glycosylated hemoglobin (HbA1c) levels and rates of insulin/sulfonylurea use as a function of age and multimorbidity using administrative claims and laboratory data for adults with type 2 diabetes included in OptumLabs Data Warehouse, 1 January 2014 to 31 December 2016. Comorbidity burden was assessed by counts of any of 16 comorbidities specified by guidelines as warranting relaxation of HbA1c targets, classified as being diabetes concordant (diabetes complications or risk factors), discordant (unrelated to diabetes), or advanced (life limiting).
Results
Among 194 157 patients with type 2 diabetes included in the study, 45.2% had only concordant comorbidities, 30.6% concordant and discordant, 2.7% only discordant, and 13.0% had ≥1 advanced comorbidity. Mean HbA1c was 7.7% among 18–44 year-olds versus 6.9% among ≥75 year-olds, and was higher among patients with comorbidities: 7.3% with concordant only, 7.1% with discordant only, 7.1% with concordant and discordant, and 7.0% with advanced comorbidities compared with 7.4% among patients without comorbidities. The odds of insulin use decreased with age (OR 0.51 (95% CI 0.48 to 0.54) for age ≥75 vs 18–44 years) but increased with accumulation of concordant (OR 5.50 (95% CI 5.22 to 5.79) for ≥3 vs none), discordant (OR 1.72 (95% CI 1.60 to 1.86) for ≥3 vs none), and advanced (OR 1.45 (95% CI 1.25 to 1.68) for ≥2 vs none) comorbidities. Conversely, sulfonylurea use increased with age (OR 1.36 (95% CI 1.29 to 1.44) for age ≥75 vs 18–44 years) but decreased with accumulation of concordant (OR 0.76 (95% CI 0.73 to 0.79) for ≥3 vs none), discordant (OR 0.70 (95% CI 0.64 to 0.76) for ≥3 vs none), but not advanced (OR 0.86 (95% CI 0.74 to 1.01) for ≥2 vs none) comorbidities.
Conclusions
The proportion of patients achieving low HbA1c levels was highest among older and multimorbid patients. Older patients and patients with higher comorbidity burden were more likely to be treated with insulin to achieve these HbA1c levels despite potential for hypoglycemia and uncertain long-term benefit.
Keywords: diabetes, patient-centered care, evidence-based medicine, risk treatment paradox, overtreatment, intensive treatment, intensive control, insulin, sulfonylurea, multimorbidity
Significance of this study.
What is already known about this subject?
Glycemic targets and glucose-lowering regimens should be individualized based on multiple factors, including the presence of comorbidities. Earlier studies revealed high prevalence of intensive glycemic control (ie, low HbA1c levels) and insulin or sulfonylurea use among older patients and patients with chronic kidney disease or dementia, but there are no contemporary data about glycemic control and insulin or sulfonylurea use among patients with these and other diabetes-concordant, diabetes-discordant, and advanced comorbidities.
What are the new findings?
Multimorbidity is common among adults with type 2 diabetes: 45.2% had only diabetes-concordant comorbidities, 30.6% had both concordant and discordant, 2.7% had only discordant, and 13.0% had advanced comorbidities.
The proportion of patients achieving low HbA1c levels, and the odds of doing so using insulin, increased with older age and with accumulation of diabetes-concordant and, to a lesser degree, discordant and advanced comorbidities.
Younger patients and patients with few comorbidities were least likely to achieve low glycemic levels or to be treated with insulin at higher HbA1c levels.
How might these results change the focus of research or clinical practice?
Our study suggests ample opportunity for insulin deintensification among older patients and patients with advanced and/or multiple comorbidities, which may lower their risk of hypoglycemia. Conversely, younger and healthier patients may benefit from treatment intensification and addressing of barriers to optimal diabetes control.
Introduction
Person-centered diabetes care is predicated on aligning glycemic targets and therapeutic regimens with the patient’s clinical situation and preferences for care. This includes the patient’s comorbidities and clinical complexity, life expectancy, and burden of treatment (eg, number, administration complexity, and side effect profiles of glucose-lowering medications required to achieve the desired glycemic targets). Ideally, patients with multiple and/or advanced comorbidities would be treated less intensively, with glycemic targets that prioritize avoidance of symptomatic hypoglycemia and hyperglycemia, while patients with a lesser comorbidity burden and longer life expectancy would be treated more intensively.1–5 However, earlier studies exposed high rates of potential overtreatment among older adults and those who have serious comorbidities.6–13 At the same time, glycemic control among younger adults with diabetes is often worse than among older adults.14 15 Whether this risk/treatment paradox continues to persist in the USA, and how it is affected by age and the type and extent of multimorbidity is unknown.
The American Diabetes Association (ADA), American Geriatrics Society (AGS), and the US Department of Veterans Affairs/Department of Defense (VA/DoD) have identified several health conditions that warrant relaxation of glycemic targets due to their association with heightened hypoglycemia risk, diminished life expectancy, functional impairment, or frailty.1–3 16 17 These and other guidelines, including the National Institute for Health and Care Excellence (NICE), also advise cautious use of insulin and sulfonylurea drugs by older and clinically complex patients, as these can lead to hypoglycemia.2–4 16–18 Optimal alignment of treatment and risks/benefits therefore dictates that intensive glucose-lowering therapy be delivered to people most likely to benefit and least likely to be harmed by it. On the other hand, a more conservative therapeutic approach is appropriate for patients likely to be harmed and/or unlikely to derive meaningful benefit from intensive control, that is, those who are older and clinically complex.
However, different comorbidities have varying effects on diabetes management strategies, on patients’ abilities to successfully manage their condition,19 and their association with hypoglycemia.20 For example, comorbidities can be classified on the basis of their concordance with diabetes, clinical dominance, and presence of symptoms.19 Understanding comorbidity types is important for contextualizing diabetes management and identifying opportunities for more patient-centered, evidence-based care. Of the guideline-specified comorbidities, many are diabetes concordant as they share common pathogenesis, therapeutic goals, or treatment strategies with diabetes; for example, retinopathy, neuropathy, heart failure, myocardial infarction, stroke, chronic kidney disease (CKD), and hypertension. These conditions are comanaged with diabetes and their presence may amplify the desired intensity of diabetes control, though the risk of having these conditions is also increased by uncontrolled diabetes. Conversely, discordant conditions such as chronic obstructive pulmonary disease (COPD), liver disease, falls, incontinence, arthritis, and depression may compete with, rather than augment, diabetes for management focus and prioritization. Finally, advanced or clinically dominant conditions such as end-stage renal disease (ESRD), dementia, and cancer may take precedence over all other disease management, thereby deprioritizing glycemic control.
In the context of increasing prevalence of multimorbidity, growing awareness about the potential harms of overtreatment, and recent availability of glucose-lowering medications that do not cause hypoglycemia, we examined the contemporary landscape of diabetes management across a wide spectrum of morbidity. We focus specifically on the use of insulin and sulfonylurea because of their associated risk for hypoglycemia.20 21 Our goal was to examine treatment regimens overall and among patients who achieved low HbA1c levels as a function of patient age and comorbidity, examining the impact of having diabetes-concordant, discordant, and advanced health conditions.
Methods
Study design
We analyzed deidentified administrative claims data with linked laboratory results from OptumLabs Data Warehouse (OLDW) between 1 January 2014 and 31 December 2016. OLDW includes deidentified medical and pharmacy claims, laboratory results, and enrollment records data for commercial and Medicare Advantage enrollees. The database contains longitudinal health information on enrollees and patients, representing a diverse mixture of ages, ethnicities, and geographic regions across the USA.22 23 Because this study involved statistically deidentified data, it was exempt from Mayo Clinic Institutional Review Board review.
Study population
We identified adults (aged ≥18 years) with type 2 diabetes, an available HbA1c result between 1 January 2015 and 31 December 2015 and ≥12 months of medical and pharmacy claims data before and after that index HbA1c date. If multiple HbA1c results were available in 2015, the latest was used as the index date.
The diagnosis of diabetes was established using Healthcare Effectiveness Data and Information Set criteria applied to 2013–2014 claims.24 Patients with plurality of Evaluation & Management (E&M) diagnosis codes reflecting type 1 diabetes and with claims for bolus insulin, or those with an equal number of E&M codes reflecting type 1 as type 2 diabetes and bolus insulin claims and no sulfonylurea claims, were considered to have type 1 diabetes and therefore excluded.20 25 26 Patients with only gestational diabetes (International Classification of Diseases Ninth Revision (ICD-9) 648.8x, ICD-10 O024.4xx) were not included.
Explanatory variables
Glycemic management was ascertained by (1) age group: 18–44, 45–64, 65–74, ≥75 years; (2) each of the 16 guideline-specified comorbidities; (3) Charlson Comorbidity Index, categorized as 0–1, 2, 3, ≥4; and (4) type of diabetes-specific comorbidity profile: none, concordant conditions only (1, 2, ≥3 total), discordant conditions only (1, 2, ≥3 total), both concordant and discordant conditions (1, 2, ≥3 total), and advanced±concordant/discordant conditions (1, 2, ≥3 total).
The Charlson index weighs comorbid conditions by the strength of their association with 1-year mortality27 28; it has been previously validated for use in diabetes.29 Additionally, specific comorbidities were ascertained from among the 16 health conditions specified by the ADA,1 17 AGS,16 and/or VA/DoD2 3 guidelines using claims from 12 months preceding the index HbA1c date (online supplementary table S1). These were categorized as diabetes concordant (CKD stages 3–4, heart failure, myocardial infarction, hypertension, cerebrovascular disease, proliferative retinopathy, and peripheral neuropathy), discordant (liver disease/cirrhosis, depression, COPD, urinary incontinence, falls, arthritis), or advanced (dementia, ESRD, cancer (excluding non-melanoma skin cancer)) based on the framework delineated by Piette and Kerr.19 Comorbidities were counted within each category and presented as the number of concordant only, discordant only, both concordant and discordant, and advanced±any additional concordant or discordant conditions.
bmjdrc-2019-001007supp001.pdf (95.4KB, pdf)
Outcome
Glycemic management was examined as the proportion of people treated with sulfonylurea (without insulin) or insulin (with or without sulfonylurea), each with or without other glucose-lowering medications, at each HbA1c level for the different age and comorbidity subsets. HbA1c levels were categorized as ≤5.6%, 5.7%–6.4%, 6.5%–6.9%, 7.0%–7.9%, 8.0%–8.9%, 9.0%–9.9%, and ≥10.0%. Diabetes medications were identified from ambulatory pharmacy fills during 100 days preceding the index HbA1c, classified as insulin (basal only, bolus±basal), sulfonylurea, or other (metformin, dipeptidyl peptidase 4 (DPP-4) inhibitors, glucagon-like peptide-1 (GLP-1) receptor agonists, sodium-glucose transport protein 2 (SGLT2) inhibitors, α-glucosidase inhibitors, thiazolidinediones, meglitinides, and amylin analogs).
Independent variables
Patient age, sex, annual household income, and race/ethnicity were identified from OLDW enrollment files.
Statistical analysis
We calculated overall frequencies (percentages) and means (SD) for all patient characteristics, including age, sex, race/ethnicity, annual household income, comorbidities, index HbA1c, and the different glucose-lowering regimens using χ2 and t-tests, as appropriate. HbA1c level categories and use of sulfonylurea and insulin were assessed by age group, each comorbidity, and each comorbidity profile. The main analysis considered comorbidity burden as the total number of concordant, discordant, and advanced comorbidities present. Secondary analyses modeled multimorbidity as a function of (1) the Charlson Comorbidity Index or (2) the presence of concordant only, discordant only, both concordant and discordant, and any advanced comorbidities as compared with none. Variables associated with insulin and sulfonylurea use (age, sex, race/ethnicity, annual household income level, HbA1c level, comorbidity groupings) were examined using logistic regression analysis with results reported as ORs and 95% CIs. All statistical analyses were performed using SAS software V.9.4 (SAS Institute).
Results
Study population
The study population was comprised of 194 157 adults with type 2 diabetes; mean age 66.2 years (SD 11.7), mean HbA1c 7.2% (SD 1.5), 50.9% female, and 58.5% white (table 1). The vast majority (91.5%) had at least one comorbidity in addition to diabetes, with mean 2.1 (SD 1.5) comorbidities overall. Mean Charlson Comorbidity Index was 3.0 (SD 2.3) and 33.5% had Charlson index ≥4. The most common diabetes-concordant comorbidities were hypertension (84.3%), neuropathy (23.6%), cerebrovascular disease (11.9%), and CKD (11.4%). The most common diabetes-discordant comorbidities were arthritis (21.6%), COPD (13.5%), and depression (10.5%). Advanced comorbidities were less prevalent: 9.5% had cancer, 2.7% had dementia, and 1.4% had ESRD.
Table 1.
Study population
| Total (n=194 157) |
|
| Age (years), mean (SD) | 66.2 (11.7) |
| Gender, n (%) | |
| Female | 98 882 (50.9) |
| Male | 95 275 (49.1) |
| Race/ethnicity, n (%) | |
| White | 113 645 (58.5) |
| Black | 31 859 (16.4) |
| Hispanic | 28 985 (14.9) |
| Asian | 11 300 (5.8) |
| Other/unknown | 8368 (4.3) |
| Household income, n (%) | |
| <$40 000 | 59 181 (30.5) |
| $40 000–$49 999 | 18 884 (9.7) |
| $50 000–$59 999 | 16 828 (8.7) |
| $60 000–$74 999 | 20 601 (10.6) |
| $75 000–$99 999 | 25 455 (13.1) |
| ≥$100 000 | 40 098 (20.7) |
| Unknown | 13 110 (6.8) |
| Charlson index, mean (SD) | 3.0 (2.3) |
| Comorbidity count,* mean (SD) | 2.1 (1.5) |
| Comorbidities, n (%) | |
| Dementia | 5184 (2.7) |
| End-stage renal disease | 2783 (1.4) |
| Chronic kidney disease (stages 3–4) | 22 115 (11.4) |
| Myocardial infarction | 7353 (3.8) |
| Heart failure | 18 436 (9.5) |
| Cerebrovascular disease | 23 175 (11.9) |
| Chronic obstructive pulmonary disease | 26 165 (13.5) |
| Cancer | 18 438 (9.5) |
| Cirrhosis | 1764 (0.9) |
| Retinopathy | 3880 (2.0) |
| Neuropathy | 45 910 (23.6) |
| Hypertension | 163 653 (84.3) |
| Arthritis | 42 010 (21.6) |
| Urinary incontinence | 7073 (3.6) |
| Depression | 20 295 (10.5) |
| Falls | 6352 (3.3) |
| HbA1c, mean (SD) | 7.2 (1.5) |
| HbA1c range, n (%) | |
| ≤5.6% | 9960 (5.1) |
| 5.7%–6.4% | 57 246 (29.5) |
| 6.5%–6.9% | 39 624 (20.4) |
| 7.0%–7.9% | 46 014 (23.7) |
| 8.0%–8.9% | 20 054 (10.3) |
| 9.0%–9.9% | 9663 (5.0) |
| ≥10.0% | 11 596 (6.0) |
Patient characteristics ascertained at the time of the index glycosylated hemoglobin (HbA1c) date.
*Comorbidity count was ascertained from among the 16 chronic health conditions specified by clinical practice guidelines as warranting pursuit of more relaxed treatment targets.
Overall, 80.2% had at least one fill for a glucose-lowering medication in the 100 days preceding the index HbA1c; expanding the medication capture period to 12 months did not identify any new pharmacologically treated patients (data not shown). As shown in table 2, 31.9% were treated with medications other than insulin/sulfonylurea, 25.3% with sulfonylurea (no insulin), 9.8% with basal insulin (5.0% without concurrent sulfonylurea and 4.8% with), and 13.1% were treated with bolus±basal insulin (9.5% without concurrent sulfonylurea and 3.6% with). Mean HbA1c achieved was lowest among patients without fills for glucose-lowering medications (6.5%; SD 1.0) and those using non-insulin/sulfonylurea drugs (6.7%; SD 1.0), and was highest among patients treated with bolus±basal insulin, particularly in combination with sulfonylurea (8.5%; SD 1.8).
Table 2.
Glycemic control as a function of age, multimorbidity, and glucose-lowering treatment regimen
| Number (%) of patients (Population n=194 157) |
HbA1c (%) Mean (SD) |
|
| Glucose-lowering treatment regimen | ||
| Sulfonylurea (no insulin) | 49 200 (25.3) | 7.41 (1.39) |
| Basal insulin (no sulfonylurea) | 9782 (5.0) | 7.89 (1.74) |
| Basal insulin+sulfonylurea | 9311 (4.8) | 8.38 (1.72) |
| Bolus±basal insulin (no sulfonylurea) | 18 470 (9.5) | 8.24 (1.77) |
| Bolus±basal insulin+sulfonylurea | 7013 (3.6) | 8.54 (1.82) |
| Other meds only | 61 917 (31.9) | 6.74 (1.04) |
| No fills | 38 464 (19.8) | 6.50 (1.02) |
| Age (years) | ||
| 18–44 | 9638 (5.0) | 7.71 (2.01) |
| 45–64 | 63 055 (32.5) | 7.49 (1.71) |
| 65–74 | 74 418 (38.3) | 7.08 (1.30) |
| ≥75 | 47 046 (24.2) | 6.92 (1.15) |
| Type and degree of multimorbidity | ||
| No comorbidities | 16 562 (8.5) | 7.41 (1.72) |
| Charlson Comorbidity Index | ||
| 0–1 | 69 427 (35.8) | 7.23 (1.53) |
| 2 | 25 565 (13.2) | 7.10 (1.43) |
| 3 | 34 051 (17.5) | 7.26 (1.49) |
| ≥4 | 65 114 (33.5) | 7.19 (1.43) |
| Concordant comorbidities* only | 87 699 (45.2) | 7.30 (1.49) |
| 1 | 56 693 (64.6) | 7.27 (1.49) |
| 2 | 22 293 (25.4) | 7.31 (1.50) |
| ≥3 | 8713 (9.9) | 7.40 (1.50) |
| Discordant comorbidities† only | 5202 (2.7) | 7.06 (1.53) |
| 1 | 4319 (83.0) | 7.10 (1.56) |
| 2 | 786 (15.1) | 6.86 (1.37) |
| ≥3 | 97 (1.9) | 6.62 (1.16) |
| Concordant and discordant comorbidities | 59 384 (30.6) | 7.12 (1.42) |
| 2 | 22 674 (38.2) | 7.07 (1.37) |
| ≥3 | 36 710 (61.8) | 7.15 (1.45) |
| Advanced‡±concordant/discordant comorbidities | 25 310 (13.0) | 7.00 (1.32) |
| 1 | 971 (3.8) | 7.09 (1.48) |
| 2 | 5794 (22.9) | 6.98 (1.27) |
| ≥3 | 18 545 (73.3) | 7.00 (1.33) |
The mean (SD) glycosylated hemoglobin (HbA1c) levels achieved by the study population as a function of age, comorbidity profile, and glucose-lowering treatment regimen.
*Concordant comorbidities included stage 3–4 chronic kidney disease, heart failure, myocardial infarction, hypertension, cerebrovascular disease, proliferative retinopathy, and peripheral neuropathy.
†Discordant comorbidities included cirrhosis, depression, chronic obstructive pulmonary disease, urinary incontinence, falls, and arthritis.
‡Advanced comorbidities included dementia, end-stage kidney disease, and cancer.
Comorbidities and glycemic control
HbA1c levels were inversely associated with age, with highest mean HbA1c among those 18–44 years old (7.7%; SD 2.0) and the lowest among those ≥75 years old (6.9%; SD 1.2) (table 2). The plurality of patients had only diabetes-concordant comorbidities (45.2%), while 30.6% had both concordant and discordant comorbidities, 2.7% had only discordant comorbidities, and 13.0% had at least one advanced comorbid condition. Mean HbA1c was highest among patients with no comorbidities (7.4%; SD 1.7), slightly lower among those with only concordant comorbidities (7.3%; SD 1.5), and much lower among those with discordant only (7.1%; SD 1.5), discordant and concordant (7.1%; SD 1.4), and advanced (7.0; SD 1.3) comorbidities. Moreover, among patients with only discordant comorbidities, mean HbA1c declined as the number of comorbidities increased from 7.1% (SD 1.6) with 1 to 6.6% (SD 1.2) with ≥3.
Comorbidities, HbA1c, and high-risk medication use
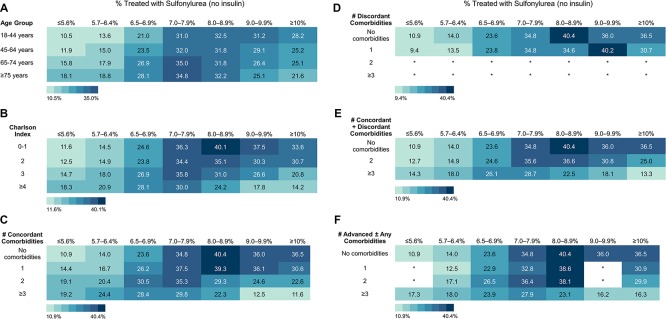
We then examined the proportions of patients within each age and comorbidity category who were treated with either sulfonylurea or insulin as they achieved their respective HbA1c levels, and found opposing trends for the two medication classes. The crude proportion treated with sulfonylurea increased with patient age at low HbA1c levels (<8%), but decreased with age at high HbA1c levels (≥9%) (figure 1A). Indeed, 18.1% of patients ≥75 years old whose HbA1c was ≤5.6% were treated with a sulfonylurea, compared with 10.5% of those 18–44 years old. In contrast, among patients with HbA1c ≥10%, 21.6% of those ≥75 years old were treated with a sulfonylurea compared with 28.2% of those 18–44 years old. We saw similar patterns with increasing Charlson index (figure 1B) and increasing numbers of concordant only (figure 1C), concordant and discordant (figure 1E), and advanced (figure 1F) comorbidities.
Figure 1.
Glycemic control and sulfonylurea use in the context of advanced age and multimorbidity. Shown are the proportions of patients within each hemoglobin A1c (HbA1c) category treated with sulfonylurea (no insulin) as a function of (A) age, (B) Charlson index, (C) number of concordant comorbidities among patients with only concordant comorbidities, (D) number of discordant comorbidities among patients with only discordant comorbidities, (E) number of concordant and/or discordant comorbidities among patients with both, and (F) total number of comorbidities among patients with at least one advanced illness, with or without concurrent concordant and/or discordant conditions.
After adjusting for sex, race/ethnicity, income, and HbA1c level, the odds of sulfonylurea use increased with age and decreased with greater multimorbidity, irrespective of the type of comorbidities present (table 3). Patients ≥75 years old had 36% higher odds of sulfonylurea use than patients 18–44 years old. Compared with patients with no concordant conditions, odds of sulfonylurea use were 0.76 (95% CI 0.73 to 0.79) in the presence of ≥3 concordant comorbidities, and 0.70 (95% CI 0.64 to 0.76) in the presence of ≥3 discordant comorbidities, compared with none. Patients who had an advanced comorbidity had a 10% lower odds of sulfonylurea use than those without.
Table 3.
Factors associated with insulin and sulfonylurea use among US adults with diabetes
| Sulfonylurea (no insulin) | Insulin (±sulfonylurea) | |||
| OR (95% CI) | P value | OR (95% CI) | P value | |
| Age groups | ||||
| 18–44 years | Ref | Ref | ||
| 45–64 years | 1.09 (1.03 to 1.14) | 0.002 | 0.94 (0.89 to 0.99) | 0.03 |
| 65–74 years | 1.27 (1.20 to 1.34) | <0.001 | 0.72 (0.68 to 0.77) | <0.001 |
| ≥75 years | 1.36 (1.29 to 1.44) | <0.001 | 0.51 (0.48 to 0.54) | <0.001 |
| Gender | ||||
| Male | Ref | Ref | ||
| Female | 0.80 (0.78 to 0.82) | <0.001 | 1.10 (1.07 to 1.13) | <0.001 |
| Race | ||||
| White | Ref | Ref | ||
| Black | 1.01 (0.98 to 1.04) | 0.70 | 1.00 (0.97 to 1.04) | 0.89 |
| Hispanic | 1.18 (1.15 to 1.22) | <0.001 | 0.86 (0.83 to 0.89) | <0.001 |
| Asian | 1.23 (1.17 to 1.28) | <0.001 | 0.59 (0.55 to 0.62) | <0.001 |
| Unknown | 0.95 (0.90 to 1.00) | 0.06 | 0.76 (0.72 to 0.82) | <0.001 |
| Household income | ||||
| <$40 000 | Ref | Ref | ||
| $40 000–$49 999 | 1.00 (0.96 to 1.04) | 0.91 | 0.88 (0.84 to 0.92) | <0.001 |
| $50 000–$59 999 | 0.97 (0.94 to 1.01) | 0.19 | 0.88 (0.84 to 0.92) | <0.001 |
| $60 000–$74 999 | 0.93 (0.89 to 0.96) | <0.001 | 0.89 (0.85 to 0.93) | <0.001 |
| $75 000–$99 999 | 0.93 (0.90 to 0.97) | <0.001 | 0.84 (0.80 to 0.87) | <0.001 |
| ≥$100 000 | 0.85 (0.82 to 0.88) | <0.001 | 0.83 (0.80 to 0.86) | <0.001 |
| Unknown | 0.90 (0.85 to 0.94) | <0.001 | 0.97 (0.92 to 1.02) | 0.20 |
| HbA1c range | ||||
| ≤5.6% | 0.52 (0.49 to 0.56) | <0.001 | 0.43 (0.39 to 0.46) | <0.001 |
| 5.7%–6.4% | 0.60 (0.58 to 0.61) | <0.001 | 0.48 (0.46 to 0.50) | <0.001 |
| 6.5%–6.9% | Ref | Ref | ||
| 7.0%–7.9% | 1.46 (1.42 to 1.51) | <0.001 | 2.41 (2.32 to 2.50) | <0.001 |
| 8.0%–8.9% | 1.37 (1.32 to 1.42) | <0.001 | 5.21 (5.00 to 5.43) | <0.001 |
| 9.0%–9.9% | 1.13 (1.08 to 1.19) | <0.001 | 7.82 (7.43 to 8.23) | <0.001 |
| ≥10.0% | 0.99 (0.94 to 1.04) | 0.73 | 9.43 (8.97 to 9.90) | <0.001 |
| Type and degree of multimorbidity | ||||
| Concordant comorbidities | ||||
| 0 | Ref | Ref | ||
| 1 | 1.02 (0.99 to 1.06) | 0.24 | 1.45 (1.39 to 1.51) | <0.001 |
| 2 | 0.96 (0.92 to 1.00) | 0.03 | 2.79 (2.66 to 2.93) | <0.001 |
| ≥3 | 0.76 (0.73 to 0.79) | <0.001 | 5.50 (5.22 to 5.79) | <0.001 |
| Discordant comorbidities | ||||
| 0 | Ref | Ref | ||
| 1 | 0.89 (0.87 to 0.91) | <0.001 | 1.17 (1.14 to 1.20) | <0.001 |
| 2 | 0.76 (0.72 to 0.79) | <0.001 | 1.37 (1.31 to 1.43) | <0.001 |
| ≥3 | 0.70 (0.64 to 0.76) | <0.001 | 1.72 (1.60 to 1.86) | <0.001 |
| Advanced comorbidities | ||||
| 0 | Ref | Ref | ||
| 1 | 0.90 (0.87 to 0.93) | <0.001 | 1.24 (1.20 to 1.29) | <0.001 |
| ≥2 | 0.86 (0.74 to 1.01) | 0.06 | 1.45 (1.25 to 1.68) | <0.001 |
Two multivariable logistic regression analyses examined the odds of (1) sulfonylurea without insulin and (2) insulin with or without sulfonylurea use controlling for patient age, sex, race/ethnicity, annual household income, glycosylated hemoglobin (HbA1c) level, and type of comorbidity profile. In each model, comorbidity burden was reflected by the number of comorbidities within each comorbidity category (ie, diabetes concordant, discordant, and advanced).
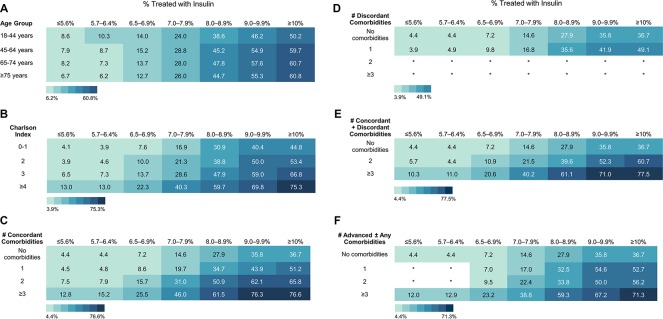
In contrast, prevalence of insulin use within each HbA1c stratum increased as the number of comorbidities increased, also irrespective of how multimorbidity was ascertained (figure 2). For example, 4.4% of patients with HbA1c ≤5.6% and none of the examined comorbidities were treated with insulin, compared with 12.8% of patients with ≥3 concordant comorbidities, 10.3% of patients with both concordant and discordant comorbidities, and 12.0% of patients with ≥3 comorbidities at least one of which was advanced. Among patients with HbA1c ≥10%, 36.7% of those without comorbidities were treated with insulin, compared with 76.6% of patients with ≥3 concordant comorbidities, 77.5% of patients with both concordant and discordant comorbidities, and 71.3% of patients with ≥3 comorbidities at least one of which was advanced. Insulin use trends by age were mixed, with higher proportions of older patients treated with insulin at high HbA1c levels (≥8%), but lower proportions treated with insulin at low HbA1c levels (<7%).
Figure 2.
Glycemic control and insulin use in the context of advanced age and multimorbidity. Shown are the proportions of patients within each hemoglobin A1c (HbA1c) category treated with insulin (with or without sulfonylurea) as a function of (A) age, (B) Charlson index, (C) number of concordant comorbidities among patients with only concordant comorbidities, (D) number of discordant comorbidities among patients with only discordant comorbidities, (E) number of concordant and/or discordant comorbidities among patients with both, and (F) total number of comorbidities among patients with at least one advanced illness, with or without concurrent concordant and/or discordant conditions.
In multivariable analysis (table 3), odds of insulin use decreased significantly with older age and increased with greater multimorbidity: OR 5.50 (95% CI 5.22 to 5.79) for ≥3 concordant comorbidities compared with none; OR 1.72 (95% CI 1.60 to 1.86) for ≥3 discordant comorbidities compared with none; and OR 1.45 (95% CI 1.25 to 1.68) for ≥2 advanced comorbidities compared with none.
We saw similar trends in a secondary analysis where multimorbidity was modeled using the Charlson index (online supplementary table S2). Moreover, in the secondary analysis examining rates of sulfonylurea and insulin use as a function of broader comorbidity phenotypes (ie, whether the patient had only concordant, only discordant, both, or advanced comorbidities; online supplementary table S3), we found that the odds of sulfonylurea use were lowest among patients with advanced (OR 0.78; 95% CI 0.74 to 0.82) or both concordant and discordant (OR 0.81; 95% CI 0.78 to 0.85) comorbidities compared with none. There was no difference between patients with concordant comorbidities only and those with none. In contrast, insulin use was significantly more likely among patients with any category of multimorbidity: 3.3-fold more likely among patients with advanced, 2.9-fold more likely with both concordant and discordant, 2.0-fold more likely with concordant alone, and 1.3-fold more likely with only discordant.
Discussion
Clinical practice guidelines advise against pursuit of low glycemic targets, and caution with use of insulin and sulfonylureas, among patients with complex and very complex health status,1 3–5 16–18 as doing so exposes patients to risk of hypoglycemia without yielding meaningful improvements in health outcomes.30–34 Yet, in a contemporary cohort of 194 157 US adults with type 2 diabetes, we found that older patients and patients with multiple and/or advanced comorbidities frequently achieved very low HbA1c levels using insulin and, to a lesser degree, sulfonylureas. Indeed, patients least likely to benefit from intensive glycemic control and most likely to experience hypoglycemia with insulin therapy (ie, older and multimorbid adults) were most likely to achieve low HbA1c levels and to be treated with insulin to achieve them. In contrast, patients who are likely to benefit from, and less likely to be harmed by, intensive control (ie, younger and healthier adults) more often had high HbA1c levels and were less frequently treated with insulin despite suboptimal glycemic control. The impact of cumulative multimorbidity on insulin use was strongest with diabetes-concordant comorbidities (eg, CKD, cardiovascular disease, retinopathy, and so on), but was still apparent with advanced comorbidities (eg, dementia, ESRD, cancer) and discordant comorbidities (eg, cirrhosis, COPD, depression, and so on), suggesting that the perception of shared treatment goals and potential for disease comanagement may prompt more intensive glucose-lowering strategies that rely on insulin.
The AGS,16 ADA,1 17 and VA/DoD3 clinical practice guidelines have identified a number of comorbid health conditions that contribute to clinical complexity, predispose patients to undesired effects of intensive glucose-lowering therapy (including increased risk of hypoglycemia), make it difficult to manage diabetes, and/or signal underlying frailty or diminished life expectancy. Yet, in our patient population, mean HbA1c levels were lower among patients with comorbidities compared with patients without, especially if the comorbidities were unrelated to diabetes or were advanced: 7.4% with no comorbidities, 7.3% with only concordant comorbidities, 7.1% with only discordant comorbidities (decreasing further as the number of discordant comorbidities increased), and 7.0% with advanced comorbidities. Higher HbA1c levels observed among patients with concordant comorbidities may reflect guideline-recommended relaxation of glycemic targets in these patients, greater difficulty managing diabetes in the setting of existing complications, or longer diabetes duration. This association may also reflect greater risk of having diabetes complications in the setting of poor glycemic control. Low HbA1c levels among patients with discordant and advanced comorbidities are concerning, and suggest an opportunity to de-escalate therapy in the presence of multimorbidity. Importantly, these HbA1c levels reflect HbA1c levels achieved by the patient, not necessarily HbA1c levels pursued by the clinician. Examination of whether clinicians subsequently deintensified or intensified therapy in response to potentially excessive or inadequate treatment, respectively, was beyond the scope of this study.
The odds of insulin use were increased fivefold, independent of HbA1c level, among patients with ≥3 concordant comorbidities compared with patients with none. Patients with concordant comorbidities were also 24% less likely to be treated with a sulfonylurea, suggesting that clinicians may preferentially rely on insulin in this population. This may reflect longer diabetes duration and greater insulin deficiency. Moreover, some diabetes-concordant conditions, most notably CKD, may necessitate use of insulin or sulfonylureas when other medications are inadequate or contraindicated. However, this does not justify the observed attainment of very low HbA1c levels using these drugs. Indeed, nearly 13% of patients who have an advanced comorbidity and achieved HbA1c ≤5.6% or 5.7%–6.4% were treated with insulin, and nearly 18% were treated with a sulfonylurea. We saw similar, high rates of insulin and sulfonylurea use at low HbA1c levels among patients with concordant-only, discordant, and both concordant and discordant comorbidities, though there were relatively few patients in our cohort (2.7%) who had only discordant comorbidities. For patients with concordant comorbidities, attainment of low HbA1c may reflect the clinician’s and/or patient’s desire to slow the progression of existing diabetes complications and/or prevent the onset of others. In addition, patients with diabetes-concordant comorbidities may be more likely to see their healthcare providers for diabetes management, resulting in greater focus on diabetes and higher intensity of treatment. Yet, such encounters also present an opportunity to re-evaluate current care, engage in shared decision-making, and deintensify therapy if the current level of glycemic control is not aligned with evidence or goals of care.
We also examined glycemic management among younger and healthier adults in the context of emerging concerns about increased rates of diabetes-related complications and hyperglycemic emergencies in the younger age groups.15 35 36 Our findings confirmed the presence of a risk/treatment paradox, with overall worse glycemic control and low rates of insulin therapy despite elevated HbA1c levels among younger patients and patients with few comorbidities. Just 46.3% of patients 18–44 years old achieved HbA1c ≤6.9%, compared with 62.5% of patients 75 years and older. Conversely, 23.1% of patients 18–44 years old had HbA1c ≥9.0%, compared with just 5.6% of people ≥75 years old. ADA guidelines recommend insulin therapy when HbA1c levels exceed 10%.18 Yet, even with HbA1c ≥10%, only half of patients 18–44 years old were treated with insulin, compared with 61% of those ≥65 years old. Analogously, only 37% of patients without any of the examined comorbidities and HbA1c ≥10% were treated with insulin, compared with more than 70% of patients with multiple comorbidities. While diabetes management is complex at any age, some of the challenges that young people face may be unique and need to be considered. For instance, younger people with commercial and employer-sponsored insurance are more likely to have high deductible health plans, limited coverage, and/or higher out-of-pocket costs than older adults with Medicare Advantage plans. Younger people may have less contact with healthcare providers and fewer opportunities to intensity treatment. They also have to balance the needs of their diabetes with other responsibilities, such as education, employment, and family. While we considered cumulative clinical complexity in our analyses, we could not capture the intangible work of living with diabetes and the overall burden of disease that people with diabetes face.37
AGS, as part of the American Board of Internal Medicine Choosing Wisely initiative, advised against using medications other than metformin to achieve HbA1c <7.5% in most older adults.38 Similarly, NICE used a higher HbA1c threshold to recommend starting medications associated with heightened hypoglycemia risk.4 In contemporary clinical practice, however, older patients were frequently treated with sulfonylureas and insulin at low HbA1c levels. Sulfonylureas were used by 18%, 19%, and 28% of patients ≥75 years old whose HbA1c levels were ≤5.6%, 5.7%–6.4%, and 6.5%–6.9%, respectively. Similarly, insulin was used by 7%, 6%, and 13%, respectively. Overall, increasing age was independently associated with greater odds of sulfonylurea use and decreasing odds of insulin use, suggesting that clinicians may be more hesitant to treat older adults with insulin but not with sulfonylureas. Finally, the proportions of older and clinically complex patients treated with insulin/sulfonylurea to achieve low HbA1c targets were comparable to earlier studies,7–9 12 despite the increasing availability of medications posing a lower risk of hypoglycemia (DPP-4 inhibitors, GLP-1 receptor agonists, SGLT2 inhibitors) and with additional cardiovascular and renal benefits (GLP-1 receptor agonists, SGLT2 inhibitors)18 than insulin and sulfonylurea. This is consistent with recent findings that older patients and patients with CKD, heart failure, and cardiovascular disease are all less likely to be prescribed SGLT2 inhibitors than younger and healthier people, despite their benefit in these contexts.39 Our study therefore reinforces the age and comorbidity-driven risk/treatment paradox in glucose-lowering therapy.
Our work builds on prior studies of glycemic overtreatment, which heretofore focused primarily on select comorbidities (most often, CKD or dementia)6 9 10 or older adults,7–12 by expanding analysis to wide ranges of age and multimorbidity. This is important, as treatment regimens and goals need to consider the patient’s overall health status, clinical complexity, and disease burden, not a few select comorbidities or chronological age. Similarly, a study by McAlister and colleagues found a similar risk/treatment paradox in glucose and blood pressure management among patients with diabetes (not restricted to type 2) in UK primary care practices between 2003 and 2015 as a function of frailty.13 However, our findings also need to be considered in the context of the study’s limitations. Some health conditions are not reliably captured in claims data, including dementia, incontinence, and falls. Claims also cannot capture disease severity, frailty, symptom burden, or life expectancy. Cases resulting in billed visits and thereby identified in claims are likely to be more severe or sufficiently bothersome to seek medical care, making individualized diabetes management especially important in this context. The prevalence of these conditions is likely much higher than suggested by our study. HbA1c levels may not reliably reflect average glycemia, particularly in patients with anemia of chronic disease, uremia, or cirrhosis.40 Medication capture may also not be complete, and some patients without fills may be treated with medications obtained through low-cost generic drug programs (these would be metformin, sulfonylurea, and human insulin)41 or those obtained as samples. However, because our objective was to identify potentially inappropriate use of sulfonylurea/insulin drugs, missing medication data is likely to underestimate the prevalence of potential overtreatment.
The study population was comprised of commercially insured and Medicare Advantage beneficiaries with prescription drug coverage, and both glycemic control and glucose-lowering treatment regimens likely differ among patients with no or public health coverage who may be more likely to use lower cost medications such as human insulin and sulfonylurea. Similarly, the study cohort is older than the general US population, with 62.5% of patients aged 65 years and older. As such, the prevalence of comorbidities and multimorbidity may be higher in our study than in the general population. Finally, claims data cannot inform us about the patients’ individualized treatment targets, goals and preferences for care, day-to-day blood glucose levels, and conversations that took place between patients and their clinicians all of which can impact treatment decisions.
Nevertheless, our study suggests ample opportunity for treatment deintensification among older patients and patients with advanced and/or multiple comorbidities, which may lower their risk of hypoglycemia. At the same time, younger and healthier adults would benefit from continued focus on improving access to diabetes care and better control of hyperglycemia. Population health management efforts and policy solutions, implemented through performance measurement,42 43 can support individualized diabetes care and align it with scientific evidence and clinical practice guidelines.17 Most importantly, clinicians should continue to engage their patients in shared and informed decision-making, weighing the risks and benefits of glucose-lowering treatment regimens in the specific context of each patient, carefully considering the patient’s comorbidity burden, age, and goals and preferences for care.
Footnotes
Twitter: @RozalinaMD
Contributors: RGM designed the study, interpreted the data, and wrote the manuscript. KJL contributed to the discussion and reviewed/edited the manuscript. HKVH analyzed the data and reviewed/edited the manuscript. NDS supervised the study design and data interpretation, contributed to the discussion, and reviewed/edited the manuscript.
Funding: This work was supported by (RGM): the National Institute of Health-National Institute of Diabetes and Digestive and Kidney Diseases (grant number K23DK114497) and the AARP through the Quality Measure Innovation Grant through a collaboration with OptumLabs and the NQF Measure Incubator; and (NDS): the Agency for Healthcare Research and Quality (grant number 1U19HS024075).
Disclaimer: Study contents are the sole responsibility of the authors and do not necessarily represent the official views of NIH.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data may be obtained from a third party and are not publicly available. The study was conducted using deidentified claims data from OptumLabs Data Warehouse.
References
- 1. ADA American diabetes association standards of medical care in Diabetes—2019. section 6. glycemic targets. Diabetes Care 2019;42:S61–70. [DOI] [PubMed] [Google Scholar]
- 2. VA/DoD Clinical Practice Guideline for the Management of Type 2 Diabetes Mellitus in Primary Care . In: Version 5.0 ed: The Office of Quality, Safety and Value, Department of Veterans Affairs, Washington, DC & Office of Evidence Based Practice, U.S. Army Medical Command, 2017. [Google Scholar]
- 3. Conlin PR, Colburn J, Aron D, et al. . Synopsis of the 2017 U.S. department of Veterans Affairs/U.S. Department of defense clinical practice guideline: management of type 2 diabetes mellitus. Ann Intern Med 2017;167:655–63. 10.7326/M17-1362 [DOI] [PubMed] [Google Scholar]
- 4. NICE National Institute for health and care excellence (NICE) guideline (NG28). type 2 diabetes in adults: management, 2019. [Google Scholar]
- 5. Garber AJ, Abrahamson MJ, Barzilay JI, et al. . Consensus statement by the american association of clinical endocrinologists and american college of endocrinology on the comprehensive type 2 diabetes management algorithm - 2019 executive summary. Endocr Pract 2019;25:69–100. 10.4158/CS-2018-0535 [DOI] [PubMed] [Google Scholar]
- 6. Tseng C-L, Soroka O, Maney M, et al. . Assessing potential glycemic overtreatment in persons at hypoglycemic risk. JAMA Intern Med 2014;174:259–68. 10.1001/jamainternmed.2013.12963 [DOI] [PubMed] [Google Scholar]
- 7. Lipska KJ, Ross JS, Miao Y, et al. . Potential overtreatment of diabetes mellitus in older adults with tight glycemic control. JAMA Intern Med 2015;175:356–62. 10.1001/jamainternmed.2014.7345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Sussman JB, Kerr EA, Saini SD, et al. . Rates of Deintensification of blood pressure and glycemic medication treatment based on levels of control and life expectancy in older patients with diabetes mellitus. JAMA Intern Med 2015;175:1942–8. 10.1001/jamainternmed.2015.5110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Thorpe CT, Gellad WF, Good CB, et al. . Tight glycemic control and use of hypoglycemic medications in older veterans with type 2 diabetes and comorbid dementia. Diabetes Care 2015;38:dc140599–95. 10.2337/dc14-0599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hambling CE, Seidu SI, Davies MJ, et al. . Older people with type 2 diabetes, including those with chronic kidney disease or dementia, are commonly overtreated with sulfonylurea or insulin therapies. Diabet Med 2017;34:1219–27. 10.1111/dme.13380 [DOI] [PubMed] [Google Scholar]
- 11. Arnold SV, Lipska KJ, Wang J, et al. . Use of intensive glycemic management in older adults with diabetes mellitus. J Am Geriatr Soc 2018;66:1190–4. 10.1111/jgs.15335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Maciejewski ML, Mi X, Sussman J, et al. . Overtreatment and Deintensification of diabetic therapy among Medicare beneficiaries. J Gen Intern Med 2018;33:34–41. 10.1007/s11606-017-4167-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. McAlister FA, Lethebe BC, Lambe C, et al. . Control of glycemia and blood pressure in British adults with diabetes mellitus and subsequent therapy choices: a comparison across health states. Cardiovasc Diabetol 2018;17:27 10.1186/s12933-018-0673-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lipska KJ, Yao X, Herrin J, et al. . Trends in drug utilization, glycemic control, and rates of severe hypoglycemia, 2006-2013. Diabetes Care 2017;40:468–75. 10.2337/dc16-0985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Styles E, Kidney RSM, Carlin C, et al. . Diabetes treatment, control, and hospitalization among adults aged 18 to 44 in Minnesota, 2013-2015. Prev Chronic Dis 2018;15:E142 10.5888/pcd15.180255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kirkman MS, Briscoe VJ, Clark N, et al. . Diabetes in older adults: a consensus report. J Am Geriatr Soc 2012;60:2342–56. 10.1111/jgs.12035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. ADA American diabetes association standards of medical care in Diabetes—2019. section 12. older adults. Diabetes Care 2019;42:S139–47. [DOI] [PubMed] [Google Scholar]
- 18. ADA American diabetes association standards of medical care in Diabetes—2019. section 9. pharmacologic approaches to glycemic treatment. Diabetes Care 2019;42:S90–102. [DOI] [PubMed] [Google Scholar]
- 19. Piette JD, Kerr EA. The impact of comorbid chronic conditions on diabetes care. Diabetes Care 2006;29:725–31. 10.2337/diacare.29.03.06.dc05-2078 [DOI] [PubMed] [Google Scholar]
- 20. McCoy RG, Lipska KJ, Van Houten HK, et al. . Association of cumulative multimorbidity, glycemic control, and medication use with hypoglycemia-related emergency department visits and hospitalizations among adults with diabetes. JAMA Netw Open 2020;3:e1919099 10.1001/jamanetworkopen.2019.19099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Silbert R, Salcido-Montenegro A, Rodriguez-Gutierrez R, et al. . Hypoglycemia among patients with type 2 diabetes: epidemiology, risk factors, and prevention strategies. Curr Diab Rep 2018;18:53 10.1007/s11892-018-1018-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Wallace PJ, Shah ND, Dennen T, et al. . Optum Labs: building a novel node in the learning health care system. Health Aff 2014;33:1187–94. 10.1377/hlthaff.2014.0038 [DOI] [PubMed] [Google Scholar]
- 23. OptumLabs OptumLabs and OptumLabs data Warehouse (OLDW) descriptions and citation. Cambridge, MA, 2019. PDF. Reproduced with permission from OptumLabs. [Google Scholar]
- 24. NCQA National Committee for quality assurance (NCQA) healthcare effectiveness data and information set (HEDIS) comprehensive diabetes care. Washington, DC: National Committee for Quality Assurance, 2015: 74–98. [Google Scholar]
- 25. Klompas M, Eggleston E, McVetta J, et al. . Automated detection and classification of type 1 versus type 2 diabetes using electronic health record data. Diabetes Care 2013;36:914–21. 10.2337/dc12-0964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Schroeder EB, Donahoo WT, Goodrich GK, et al. . Validation of an algorithm for identifying type 1 diabetes in adults based on electronic health record data. Pharmacoepidemiol Drug Saf 2018;27:1053–9. 10.1002/pds.4377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Charlson M, Szatrowski TP, Peterson J, et al. . Validation of a combined comorbidity index. J Clin Epidemiol 1994;47:1245–51. 10.1016/0895-4356(94)90129-5 [DOI] [PubMed] [Google Scholar]
- 28. de Groot V, Beckerman H, Lankhorst GJ, et al. . How to measure comorbidity. A critical review of available methods. J Clin Epidemiol 2003;56:221–9. 10.1016/s0895-4356(02)00585-1 [DOI] [PubMed] [Google Scholar]
- 29. McEwen LN, Kim C, Karter AJ, et al. . Risk factors for mortality among patients with diabetes: the translating research into action for diabetes (triad) study. Diabetes Care 2007;30:1736–41. 10.2337/dc07-0305 [DOI] [PubMed] [Google Scholar]
- 30. Patel A, MacMahon S, Chalmers J, et al. . Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med 2008;358:2560–72. 10.1056/NEJMoa0802987 [DOI] [PubMed] [Google Scholar]
- 31. Gerstein HC, Miller ME, Byington RP, et al. . Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med 2008;358:2545–59. 10.1056/NEJMoa0802743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Duckworth W, Abraira C, Moritz T, et al. . Glucose control and vascular complications in veterans with type 2 diabetes. N Engl J Med 2009;360:129–39. 10.1056/NEJMoa0808431 [DOI] [PubMed] [Google Scholar]
- 33. Greenfield S, Billimek J, Pellegrini F, et al. . Comorbidity affects the relationship between glycemic control and cardiovascular outcomes in diabetes: a cohort study. Ann Intern Med 2009;151:854–60. 10.7326/0003-4819-151-12-200912150-00005 [DOI] [PubMed] [Google Scholar]
- 34. Rodríguez-Gutiérrez R, Montori VM. Glycemic control for patients with type 2 diabetes mellitus: our evolving faith in the face of evidence. Circ Cardiovasc Qual Outcomes 2016;9:504–12. 10.1161/CIRCOUTCOMES.116.002901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. McCoy RG, Herrin J, Lipska KJ, et al. . Recurrent hospitalizations for severe hypoglycemia and hyperglycemia among U.S. adults with diabetes. J Diabetes Complications 2018;32:693–701. 10.1016/j.jdiacomp.2018.04.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. CDC Diabetes Data & Statistics. Diabetes Atlas Atlanta, GA: Division of Diabetes Translation, Centers for Disease Control and Prevention, U.S. Dept of Health and Human Services, 2019. Available: https://gis.cdc.gov/grasp/diabetes/DiabetesAtlas.html# [Accessed 30 Dec 2019].
- 37. Spencer-Bonilla G, Quiñones AR, Montori VM, et al. . Assessing the burden of treatment. J Gen Intern Med 2017;32:1141–5. 10.1007/s11606-017-4117-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. AGS, ABIM American geriatrics Society and the American Board of internal medicine choosing wisely initiative: ten things clinicians and patients should question: ABIM, 2015. Available: https://www.choosingwisely.org/wp-content/uploads/2015/02/AGS-Choosing-Wisely-List.pdf [Accessed April 24 2019].
- 39. McCoy RG, Dykhoff HJ, Sangaralingham L, et al. . Adoption of new glucose-lowering medications in the U.S.-The case of SGLT2 inhibitors: nationwide cohort study. Diabetes Technol Ther 2019;21:702–12. 10.1089/dia.2019.0213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Radin MS. Pitfalls in hemoglobin A1c measurement: when results may be misleading. J Gen Intern Med 2014;29:388–94. 10.1007/s11606-013-2595-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Pauly NJ, Brown JD. Prevalence of low-cost generic program use in a nationally representative cohort of privately insured adults. J Manag Care Spec Pharm 2015;21:1162–70. 10.18553/jmcp.2015.21.12.1162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. MNCM Minnesota community measurement data collection guide: optimal diabetes care specifications, 2019 report year (01/01/2018 to 12/31/2018 dates of service. Minneapolis, MN, 2018. [Google Scholar]
- 43. Rodriguez-Gutierrez R, Ospina NS, McCoy RG, et al. . Inclusion of hypoglycemia in clinical practice guidelines and performance measures in the care of patients with diabetes. JAMA Intern Med 2016;176:1714–6. 10.1001/jamainternmed.2016.5046 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjdrc-2019-001007supp001.pdf (95.4KB, pdf)