Abstract
Background:
Although obtaining medical consent is an important skill, many residents may have knowledge gaps in understanding key concepts of informed consent or may lack awareness of serious procedural risks. The objective of this study was to see if formal education makes a difference in anesthesiology residents' ability to obtain an informed consent.
Methods:
Thirty-four first-year anesthesiology residents (CA1s) were randomized into either a control group or study group. The control group learned how to obtain consent for general anesthesia the current way, which is by observing senior residents or faculty. The study group received additional formal education, which included a video, a narrated lecture, and a quiz. Afterwards, both groups were observed obtaining informed consent on patients receiving general anesthesia. The investigators used a checklist consisting of 10 important items that the resident had to fulfill for a proper informed consent. To minimize bias, neither the control group nor the study group was shown the checklist.
Results:
Overall, the study group did significantly better than the control group in fulfilling the 10 items on the checklist (median 0.90 vs 0.70; P < .001). There were statistical differences on 4 key components: identifying all persons on the anesthesia team (76.5% vs 5.9%, P < .0001), explaining why general anesthesia is necessary (82.4% vs 35.3%, P < .0134), explaining the risks and benefits of general anesthesia (94.1% vs 47.1%, P < .0066), and discussing the risks and benefits of blood transfusion (70.59% vs 29.4%, P < .0381).
Conclusions:
This study shows that formal instruction on informed consent enhances residents' ability to obtain an informed consent.
Keywords: Informed consent, medical education, anesthesiology residents, teaching anesthesiology residents, teaching informed consent
Introduction
Informed consent for anesthesia is an exchange between the patient and physician in, which information including the benefits of anesthesia, associated risks, and alternatives are discussed so patients are aware of all the necessary information to make an informed decision.1 Although obtaining consent is an essential skill, many residents receive very little to no formal education on this subject.2,3 Most residents learn from observing coresidents or faculty.2–4 There may be knowledge gaps in understanding key concepts of informed consent or lack of awareness of serious procedural risks. It would be difficult to discern these deficiencies without formal assessment of knowledge or skills on informed consent. Several studies show that trainees actually wanted more curricular attention and training on informed consent.2,4–6 The objective of this study was to assess if formal education on informed consent had a significant effect on our anesthesiology residents' ability to obtain a complete and thorough informed consent.
Materials and Methods
This study was approved by both the Baylor College of Medicine and Harris Health IRB committees and conducted over a 2-week period between the end of July and early August of 2017 and 2018.
Participants
Thirty-four first-year anesthesiology residents (CA1s) were block randomized using the PLAN procedure in SAS v 9.4 (SAS, Cary, NY) into two groups: the control group and the study group. The control group consisted of CA1s who learned how to obtain consent for general anesthesia in the current way, which is by observing senior residents and faculty. The study group, consisting of the remaining CA1s who, in addition to observing the senior residents and faculty, received formal education.
Study Group Education
The formal education for the study group included watching a video of a physician obtain an informed consent from a simulated patient, a narrated lecture, and a quiz. The lecture explained the elements of informed consent, standard disclosure requirements as well as other important considerations such as using an interpreter and consenting Jehovah's Witness patients for blood transfusion. The quiz questions were included to highlight and reinforce the concepts (Table 1). The study materials were distributed to the study group, who were allowed to watch the videos as many times as needed to learn the material. However, the frequency was not tracked for the purposes of this study. A week afterward, the observers watched both groups as they obtained informed consent on patients receiving general anesthesia. Only patients receiving general anesthesia were included in this study to decrease the confounding variable of differences in CA1s knowledge pertaining to general versus other modes of anesthesia. Other exclusions include patients who lacked the capacity or competence to consent for himself or herself. The observers were limited to two specific faculty anesthesiologists who observed and graded all of the residents. Both had experience in residency curriculum development and did extensive research for the informed consent material. They used a checklist consisting of 10 important items that the resident had to fulfill to obtain proper informed consent (Table 2). Many of the items were similar to what the American Board of Anesthesiology (ABA) expects residents to demonstrate on the Communications & Professionalism portion of the APPLIED examination.7 We encompassed most of the major points listed for the Objective Structure Clinical Examination (OSCE) for informed consent; however, for the purposes of our study, we only included general anesthesia cases. We did not give residents the opportunity to present alternatives because they were new trainees who may not have been familiar with all the different anesthesia techniques. In addition, since we are a trauma hospital with higher incidence of blood transfusions, we wanted to ensure that our residents learned how to discuss the risks and benefits of blood transfusions. Neither the control group nor the study group was shown the checklist before they were observed. At the conclusion of the observation, if the resident had not completed all the salient points on the checklist, the faculty anesthesiologist filled in the gaps so the patient would have all the information.
Table 1.
Sample of Quiz Questions
| Which of the following is the main ethical principle of informed consent? |
| A. Justice/Equity |
| B. Autonomy |
| C. Beneficence |
| D. Nonmaleficence |
| Which of the following is NOT an element of a valid informed consent? |
| A. Capacity |
| B. Coercion |
| C. Voluntariness |
| D. Disclosure |
| Which of the following should the patient always be consented for in regard to an anesthesia consent? |
| A. General anesthesia |
| B. Monitored anesthesia care (MAC) |
| C. Moderate sedition |
| D. Epidural anesthesia |
Table 2.
Observation Checklist for Informed Consent
| Component | Yes | No |
|---|---|---|
| 1. Introduces himself/herself to the patient. | ||
| 2. Identifies all persons on the anesthesia team who will be involved in the patient's care. | ||
| 3. Explains why general anesthesia is needed. | ||
| 4. Explains the sequence of events for general anesthesia. | ||
| 5. Explains the risks and benefits of general anesthesia. | ||
| 6. Discusses the possibility and risks/benefits of blood transfusion. | ||
| 7. Elicits and adequately answers questions from the patient. | ||
| 8. Uses lay terms for all explanations. | ||
| 9. Obtains affirmative consent without coercion. | ||
| 10. Communicates in a clear and professional manner. |
Immediately after the observation, all of the residents were given a brief survey on paper (Table 3) asking about their confidence level in obtaining an informed consent and opinion on the formal education for those who had received it. Yes or no responses were collectively calculated as a straight percentage, while confidence levels were measured on a scale of 1 to 5, with 5 being very confident.
Table 3.
Survey Questions
| 1. How confident are you in obtaining an informed consent? |
| 1 = Not confident |
| 2 = Somewhat confident |
| 3 = Neutral |
| 4 = Confident |
| 5 = Very confident |
| 2. Do you believe that formal instruction in residency training would help you in obtaining informed consent? Yes or No |
| 3. For those of you who received formal instruction: |
| a) Did you find the lecture informative? Yes or No |
| b) Did you learn anything new about informed consent? Yes or No |
| c) Do you feel that it has improved the way you obtain consent? Yes or No |
| d) Do you feel that all residents should have formal instruction on how to obtain informed consent at the beginning of residency? Yes or No |
| e) After receiving formal instruction, how confident are you in obtaining an informed consent? |
| 1 = Not confident |
| 2 = Somewhat confident |
| 3 = Neutral |
| 4 = Confident |
| 5 = Very confident |
Statistical Methods
A sample size of 34 subjects (17 in each group) was estimated for this study to provide 80% power to detect a standard effect size of 1 unit using an independent, two-sample t test assuming alpha = 0.05 (two-sided) and homogeneous variances. The responses to the components were summarized as frequencies with percentages, and the evaluation scores were summarized using medians (25, 75). Because box plots, Q-Q plots, and the Shapiro-Wilks test indicated that the scores were not normally distributed, the Wilcoxon rank sum test was used to test for significant differences in scores between treatment arms. The Fisher exact test was used to compare individual consent items between the two treatment arms. Statistical significance was assessed at the two-sided 0.05 level for all hypothesis tests.
Results
There were statistically significant differences in the study group on four key components: identifying all persons on the anesthesia team (76.5% vs 5.9%, P < .0001), explaining why general anesthesia is necessary (82.4% vs 35.3%, P = .013), explaining the risks and benefits of general anesthesia (94.1% vs 47.1%, P = .007), and discussing the risks and benefits of blood transfusion (70.6% vs 29.4%, P = .04) (Table 4).
Table 4.
Key Components of Anesthesiology Consent
| All | Arm | |||||
|---|---|---|---|---|---|---|
| Control | Study | |||||
| N | % | N | % | N | % | |
| All | 34 | 100.00 | 17 | 100.00 | 17 | 100.00 |
| Q1 Introduces himself/herself to the patient | ||||||
| Yes | 32 | 94.12 | 15 | 88.24 | 17 | 100.00 |
| No | 2 | 5.88 | 2 | 11.76 | … | … |
| Q2 Identifies all persons on the anesthesia team | ||||||
| Yes | 14 | 41.18 | 1 | 5.88 | 13 | 76.47 |
| No | 20 | 58.82 | 16 | 94.12 | 4 | 23.53 |
| Q3 Explains why general anesthesia is needed | ||||||
| Yes | 20 | 58.82 | 6 | 35.29 | 14 | 82.35 |
| No | 14 | 41.18 | 11 | 64.71 | 3 | 17.65 |
| Q4 Explains the sequence of events for general anesthesia | ||||||
| Yes | 31 | 91.18 | 15 | 88.24 | 16 | 94.12 |
| No | 3 | 8.82 | 2 | 11.76 | 1 | 5.88 |
| Q5 Explains the risks and benefits of general anesthesia | ||||||
| Yes | 24 | 70.59 | 8 | 47.06 | 16 | 94.12 |
| No | 10 | 29.41 | 9 | 52.94 | 1 | 5.88 |
| Q6 Discusses the possibility and risks/benefits of blood transfusion | ||||||
| Yes | 17 | 50.00 | 5 | 29.41 | 12 | 70.59 |
| No | 17 | 50.00 | 12 | 70.59 | 5 | 29.41 |
| Q7 Elicits and adequately answers questions from the patient | ||||||
| Yes | 34 | 100.00 | 17 | 100.00 | 17 | 100.00 |
| Q8 Uses lay terms for all explanations | ||||||
| Yes | 34 | 100.00 | 17 | 100.00 | 17 | 100.00 |
| Q9 Obtains affirmative consent without coercion | ||||||
| Yes | 34 | 100.00 | 17 | 100.00 | 17 | 100.00 |
| Q10 Communicates in a clear and professional manner | ||||||
| Yes | 34 | 100.00 | 17 | 100.00 | 17 | 100.00 |
Both groups showed no difference on four other components: (1) eliciting and answering questions from the patient, (2) using lay terms for all explanations, (3) obtaining affirmative consent without coercion, and (4) communicating in a clear and professional manner.
Overall, the participants in the study arm did significantly better than the control arm (P < .001) when the proportion of questions completed by the two groups was considered. The median interquartile range for the study arm was 90% (90,100) compared with 70% (60,80) in the control group (Figure 1).
Figure.
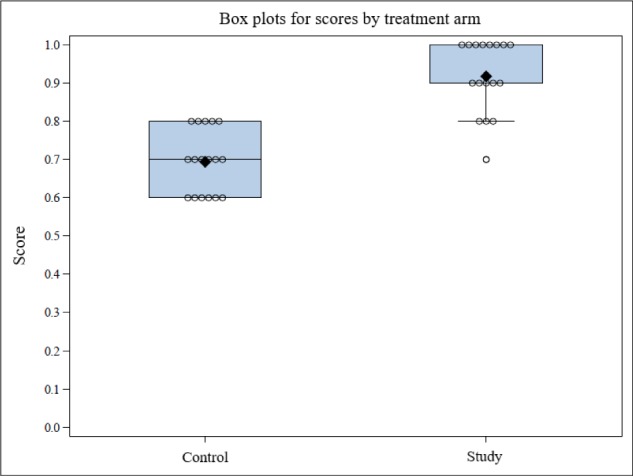
Box plots for scores by treatment arm. Interquartile score was used to assess the proportion of questions answered by the two groups with the treatment arm on the x-axis and the interquartile score on the y-axis.
The survey results showed that 100% of the residents who participated in the study believed that formal instruction in residency training would help them in obtaining a proper informed consent. Of the residents in the study group, all of them felt that the formal instruction they received was informative and had a positive impact on their consent skills. In addition, the majority of residents in the study group reported higher confidence levels in obtaining informed consent pre- versus post education.
Discussion
Formally educating residents about informed consent helps by explaining and standardizing the process so residents do not leave out important information that may influence the patient's decision. Patients should always have all the risks and benefits of a procedure explained in lay terms and have all their questions answered thoroughly before a procedure. Shared decision-making upholds patient autonomy and strengthens the patient physician relationship.
In our study, we found that identifying all persons on the anesthesia team was infrequently done in the control group. One reason may have been that the CA1 assumed the other persons on the anesthesia team introduced themselves at a separate time before surgery. However, there was no way to track this. We believed that the resident obtaining the consent was responsible for informing the patient of every person who would be taking part in the patient's care because patients should know who is taking care of them and understand the role of each person involved in their care. It was recently mandated by the Massachusetts Board of Registration in Medicine that attending physicians must inform the patient of everyone who will participate in the procedure.8
There was also a significant improvement in the study group in terms of explaining the risks and benefits of general anesthesia and blood transfusions. If the residents only explained the risks and not the benefits (or vice versa), it was not counted as being done correctly. Interestingly, it was noted that more residents explained the risks of general anesthesia versus the benefits. In their study on obstetrics and gynecology (OB/GYN) trainees, Propst et al2 found that increasing PGY level was associated with a higher likelihood of discussing procedure specific risks. This may be because new OB/GYN residents are not as familiar with all the risks for the many different procedures they perform. Anesthesia residents, however, learn the risks for general anesthesia, which are essentially the same for every surgery.
Residents are often asked to obtain consent very early in their training. Probst et al2 also make the point that newer trainees may not fully understand procedure complications or alternatives. Their study showed that ninety 90% of the 281 OB/GYN residents they surveyed admitted that they obtained consent without understanding all of the risks.2 Another study surveyed different-level pediatric residents, showing a higher percentage of interns felt that they needed more education on how to obtain informed consent versus upper-level residents.4
Formal education of the informed consent is also known to improve resident confidence in obtaining informed consent. In a study involving first-year surgery residents, Koller et al9 showed that formal training on informed consent improved their knowledge and comfort level in obtaining the consent. The majority of our study group also reported a higher self-confidence level after receiving formal education.
Limitations of this study include observer bias. Since the residents were aware that they were being observed, residents may have conducted an informed consent discussion more elaborately from their usual way, thereby minimizing potential differences. Secondly, we did not use an already published checklist validated for use. We included the major components outlined by the American Board of Anesthesiology for the OSCE on informed consent with minor modifications, such as the omission of alternative options and the addition of risks/benefits of blood transfusion. Since we included only consents where there were no alternatives to general anesthesia, the results may have been more positive because they were not complicated by explanations of a different anesthetic modality.
Another limitation is we did not collect data on residents' prior experience in obtaining informed consents. If a resident had formal instruction on informed consent during internship or in another medical specialty prior to anesthesia residency, it may have positively affected their performance in the study.
Despite limitations, this study suggests that residents perform a more thorough informed consent if exposed to a dedicated curriculum of a lecture, video, and quiz compared with traditional, observation-only training. Future study will include long-term follow-up observations to study skill retention.
References
- 1.O'Leary CE. Informed consent: principles and practice. ASA Monitor. 2010;74:20–21. 45. [Google Scholar]
- 2.Propst K, O'Sullivan DM, Ulrich A, Tunitsky-Bitton E. Informed consent education in obstetrics and gynecology: a survey study. J Surg Educ. 2018 doi: 10.1016/j.jsurg.2018.12.005. In press. [DOI] [PubMed] [Google Scholar]
- 3.Loughran D. Surgical consent: the world's largest Chinese whisper? A review of current surgical consent practices. J Med Ethics. 2015;41:206–10. doi: 10.1136/medethics-2013-101931. [DOI] [PubMed] [Google Scholar]
- 4.Nickels AS, Tilburt JC, Ross LF. Pediatric resident preparedness and educational experiences with informed consent. Acad Pediatrics. 2016;16:298–304. doi: 10.1016/j.acap.2015.10.001. [DOI] [PubMed] [Google Scholar]
- 5.Roberts LW, Geppert CM, Warner TD et al. Bioethics principles, informed consent, and ethical care for special populations: curricular needs expressed by men and women physicians-in-training. Psychosomatics. 2005;46:440–50. doi: 10.1176/appi.psy.46.5.440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Thompson BM, Sparks RA, Seavey J et al. Informed consent training improves surgery resident performance in simulated encounters with standardized patients. Am J Surg. 2015;210:578–84. doi: 10.1016/j.amjsurg.2014.12.044. [DOI] [PubMed] [Google Scholar]
- 7.American Board of Anesthesiologists Content outline: APPLIED examination. http://www.theaba.org/PDFs/APPLIED-Exam/APPLIED-OSCE-ContentOutline Accessed March 28, 2019.
- 8.State of Massachusetts, Board of Registration in Medicine Executive summary Chapter 2.00 of the Board of Medicine regulations. https://www.mass.gov/files/documents/2019/08/09/ExecutiveSummaryChapter2.00.pdf Accessed December 15, 2019.
- 9.Koller SE, Moore RF, Goldberg MB et al. An informed consent program enhances surgery resident education. J Surg Educ. 2017;74:906–13. doi: 10.1016/j.jsurg.2017.02.002. [DOI] [PubMed] [Google Scholar]


