Abstract
Background:
Cannabis use and major depressive disorder (MDD) are common and often comorbid in adolescents, but the nature and directionality of the relationship between these two conditions remains obscure.
Methods:
We examined results from the National Survey on Drug Use and Health. Weighted demographics were compared between adolescents with a history of cannabis use (N=14,873) and never users (N=73,079). Weighted logistic regression controlling for demographic variables and other substance use was used to determine the relationship between cannabis use frequency and MDD.
Results:
Adolescents with any history of cannabis use had significantly higher rates of lifetime and past year MDD, MDD with severe role impairment, and past year suicide attempt (p<0.001). Comparing use frequency groups in the adjusted model revealed that heavy users (weekly or greater use) had significantly lower predicted prevalence of lifetime and past year MDD, and past year MDD with severe role impairment compared to light users and those who used cannabis >1 year ago. Rates of reported past year suicide attempt did not differ significantly by cannabis use frequency.
Conclusions:
Adolescents with any cannabis use history have significantly higher rates of MDD. However, the directionality between frequency of use and MDD is counter to what was expected.
Keywords: Adolescent, cannabis, major depressive disorder, risk factors, Comorbidity
1.0. Introduction
Cannabis use is common among adolescents and is often co-morbid with major depressive disorder (MDD) (Hayatbakhsh et al., 2007; Mojtabai et al., 2016). The increasing potency of cannabis over the past two decades has also raised questions about its effects in young people and whether this poses an added risk for the development of psychiatric symptoms via cumulative exposure (ElSohly et al., 2016). Whether there is a causal relationship between cannabis use and MDD, and the direction of this relationship remain a matter of debate. The adolescent period of development provides key insights to this question given that it is common time of onset for both substance use and depressive disorders.
There are three prevailing hypotheses about the temporal relationship between cannabis use and depression, and existing data are mixed. The “depression first” hypothesis suggests that depression predisposes teens to cannabis use, and that cannabis use may be partially driven by attempts to “self-medicate” depressive symptoms (Khantzian, 1997). Evidence to support this includes findings from prospective research showing that 9th graders reporting depressive symptoms were more likely to initiate cannabis use by 12th grade, and that cumulative depression predicted earlier initiation of cannabis use in boys ages 9–12 (Hooshmand et al., 2012, Cerdá et al. 2013). Another theory is that cannabis use produces brain changes that increase susceptibility to MDD (Cousijn et al., 2012). Prospective cohort studies as well as recent meta-analyses have found that cannabis consumption in adolescence is associated with increased risk of depressive disorders and suicidal ideation later in life (Borges et al., 2016; Gobbi et al., 2019; Patton et al., 2002). A third hypothesis implicates confounding factors such as socioeconomic status, shared generic vulnerability to both cannabis use and major depression, or the use of other drugs rather than cannabis in itself as precipitants of mental health problems (Macleod et al., 2004). Notably, these potential explanatory pathways between cannabis use and depressive disorders are not necessarily mutually exclusive (Womack et al., 2016; Zhang & Wu, 2014).
Prior studies examining this topic have typically utilized small groups or samples of adolescents in treatment for cannabis use disorder (CUD) and/or MDD. This neglects a large subset of individuals who never present for treatment or who have used cannabis but do not meet criteria for CUD. Given a repeatedly observed relationship between cannabis use and MDD, we would expect to see a positive relationship between total cannabis dose and MDD. Frequency of use can serve as a crude proxy for dose, thereby providing some information about whether such a dose-response relationship may be present. The present study thus seeks to determine whether there is an association between cannabis use frequency and MDD by examining adolescents in a large representative sample with diverse patterns of use.
2.0. Methods
2.1. Sample
The US National Surveys on Drug Use and Health (NSDUH) is an annual nationwide survey directed by the Substance Abuse and Mental Health Services Administration. It samples the civilian noninstitutionalized population aged 12 years or older to obtain statistical information about substance use in the US. The survey also includes mental health questions. Data were collected via computer-assisted self-interview, with less sensitive measures such as demographics assessed by computer-assisted personal interview by a field interviewer. Adolescents and young adults were intentionally oversampled.
We used the 2012–2017 NSDUH public use data sets, which provided a sample of 90,314 respondents age 12–17. The mean annual adolescent response rate for this time period was 79.08%. 97.38% of adolescents who participated in the survey answered MDD questions. Only participants who had complete data for all outcome measures were included here, resulting in a total sample size of 87,952.
2.2. Measures
Sociodemographic characteristics –
Demographic characteristics included age, gender, race, and combined household income.
Frequency of cannabis use –
Cannabis use frequency was assessed by asking the number of days participants used cannabis in the past year and past month. We stratified adolescents with any lifetime cannabis use into four categories: 1) past-year abstainers (0 days of use in the past year), 2) light users (1–12 days of use in past year), 3) moderate users (13–51 days of use), and 4) heavy users (≥52 days).
Use of other substances –
Respondents reported whether they had used other substances including alcohol and other illicit drugs in the past year.
Depression –
Lifetime MDD and past year major depressive episode (MDE) were assessed using a structured clinical interview based on the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition criteria (America Psychiatric Association, 1994). Adolescents who met criteria for past year MDE completed the Sheehan Disability Scale to assess interference in functioning as a result of MDD symptoms. Role functioning was measured on an 11-point scale, from 0 (no interference) to 10 (very severe interference) in four domains: school/work, family relationships, chores at home, and social functioning. Adolescents with any scale score ≥7 were coded as having MDD with severe role impairment. Participants also indicated whether they received any past year treatment for MDD including medications or psychotherapy.
2.3. Statistical analysis
Analyses were completed using Stata 13. Taylor Series methods via the Stata “SVYSET” and “SVY” procedures were used to account for complex survey design and implement recommended weighting procedures. Weighted chi-square analyses were used to compare prevalence of demographic characteristics and rates of depression between teens who did and did not report any prior cannabis use.
Weighted logistic regression was performed to assess the relationship between cannabis use frequency in the past year and four different outcomes: lifetime MDD, past year MDD, past year MDD with severe role impairment, and past year suicide attempt. Independent variables included age, sex, race, household income, past year cannabis use frequency, past year alcohol use, and past year use of illicit drugs other than cannabis. For each regression, predictive margins were calculated to provide covariate-adjusted prevalence or probability of each outcome by dose frequency.
3.0. Results
The weighted prevalence of sample demographics, cannabis use frequency, and depression characteristics of cannabis users and never users in the sample are reported in the appendix in Supplementary Table 1. Compared to never users, adolescents with any history of cannabis use were older (15.8 ± 0.01 vs. 14.3 ± 0.01 years), were less likely to be female (47.6% vs. 49.2%), and had a higher prevalence of any past year alcohol use (73.5 vs. 14.3%) or use of illicit substances other than cannabis (29.0 vs. 4.4%). Of the respondents who reported any lifetime cannabis use, 33.1% were light users (1–12 days of use in the past year), 14.6% reported moderate use (13–51 days of use), and 32.7% reported heavy use (≥ 52 days). 19.7% of adolescents with a history of cannabis use reported past year cannabis abstinence. Rates of lifetime and past year MDD, past year suicide attempt, and MDD with severe role impairment were significantly higher in adolescents with a history of lifetime cannabis use versus never users (p<0.001).
Results from the weighted logistic regression analyses examining cannabis use frequency and outcomes related to MDD are summarized in Table 1 (unadjusted odds ratios are available in the appendix in Supplementary Table 2). Predictive margins calculated from this model are shown in Figure 1, with higher values indicating higher prevalence of the respective outcome when adjusted for other covariates. All cannabis user groups had higher predicted prevalence of lifetime MDD than never users. Comparing those with any history of cannabis use, heavy users had significantly lower predicted prevalence of lifetime MDD compared to light users and users who abstained in the past year (0.172 (95% CI=0.157–0.185, vs. 0.222 (95% CI=0.208–0.236), vs. 0.243 (95% CI=0.219–0.268)). For past year MDD and past year MDD with role impairment, trends were similar but more pronounced in that predictive margins for heavy users were not significantly different from those of never users (0.119 (95% CI 0.106–0.132) vs. 0.108 (95%CI = 0.104–0.111)). However, despite any differences in rates of past year MDD in heavy users, individuals with any cannabis use history all had significantly higher odds of past year suicide attempt and this did not differ significantly between low and high frequency users (OR ranged from 2.06–2.53 compared to never users).
Table 1.
Logistic regression analyses for lifetime and past year MDD, past year MDD with severe role impairment, and past year suicide attempt, with respective predictive margins of cannabis use frequency. Adjusted odds ratios (OR) and predictive margins are shown with 95% confidence intervals (CI).
| Lifetime MDD | Past year major depressive episode | Past year episode w/severe role impairment | Past year suicide attempt | |||||
|---|---|---|---|---|---|---|---|---|
| Variable | OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p |
| Age | 1.16 (0.15–1.18) | <0.001 | 1.14 (1.12–1.16) | <0.001 | 1.13 (1.11–1.15) | <0.001 | 1.07 (1.03–1.11) | 0.001 |
| Sex | ||||||||
| Male | Referent | Referent | Referent | Referent | ||||
| Female | 3.37 (3.20–3.56) | <0.001 | 3.63 (3.43–3.85) | <0.001 | 3.86 (3.59–4.15) | <0.001 | 4.82 (4.20–5.53) | <0.001 |
| Race | ||||||||
| Caucasian | Referent | Referent | Referent | Referent | ||||
| African American | 0.75 (0.69–0.81) | <0.001 | 0.71 (0.65–0.77) | <0.001 | 0.69 (0.62–0.78) | <0.001 | 0.86 (0.76–0.98) | 0.081 |
| Other | 1.02 (0.96–1.09) | 0.502 | 1.00 (0.93–1.09) | 0.938 | 0.96 (0.88–1.05) | 0.353 | 1.05 (0.93–1.20) | 0.408 |
| Annual Household Income | ||||||||
| < $50,000 | Referent | Referent | Referent | Referent | ||||
| ≥ $50,000 | .96 (0.91.02) | 0.178 | 1.01 (0.96–1.07) | 0.535 | 0.99 (0.93–1.06) | 0.843 | 0.85 (0.75–0.96) | 0.021 |
| Past Year Alcohol Use | ||||||||
| No | Referent | Referent | Referent | Referent | ||||
| Yes | 1.45 (1.35–1.55) | <0.001 | 1.46 (1.35–1.59) | <0.001 | 1.49 (1.35–1.64) | <0.001 | 1.55 (1.32–1.83) | <0.001 |
| Past year illicit drugs | ||||||||
| No | Referent | Referent | Referent | Referent | ||||
| Yes | 2.05 (1.87–2.22) | <0.001 | 2.21 (2.00–2.43) | <0.001 | 2.52 (2.29–2.78) | <0.001 | 3.25 (2.83–3.72) | <0.001 |
| Past year cannabis use frequency | ||||||||
| Never users | Referent | Referent | Referent | Referent | ||||
| Cannabis use >1 year ago | 1.88 (1.61–2.19) | <0.001 | 1.86 (1.58–2.19) | <0.001 | 1.84 (1.55–2.19) | <0.001 | 2.53 (2.01–3.19) | <0.001 |
| Light past year use | 1.65 (1.49–1.82) | <0.001 | 1.66 (1.47–1.87) | <0.001 | 1.76 (1.54–2.01) | <0.001 | 2.39 (1.90–3.02) | <0.001 |
| Moderate past year use | 1.46 (1.25–1.72) | <0.001 | 1.39 (1.14–1.68) | 0.001 | 1.39 (1.11–1.74) | 0.005 | 2.06 (1.59–2.67) | <0.001 |
| Heavy past year use | 1.16 (1.04–1.31) | 0.011 | 1.13 (0.98–1.31) | 0.096 | 1.15 (0.97–1.37) | 0.101 | 2.09 (1.62–2.48) | <0.001 |
Fig. 1.
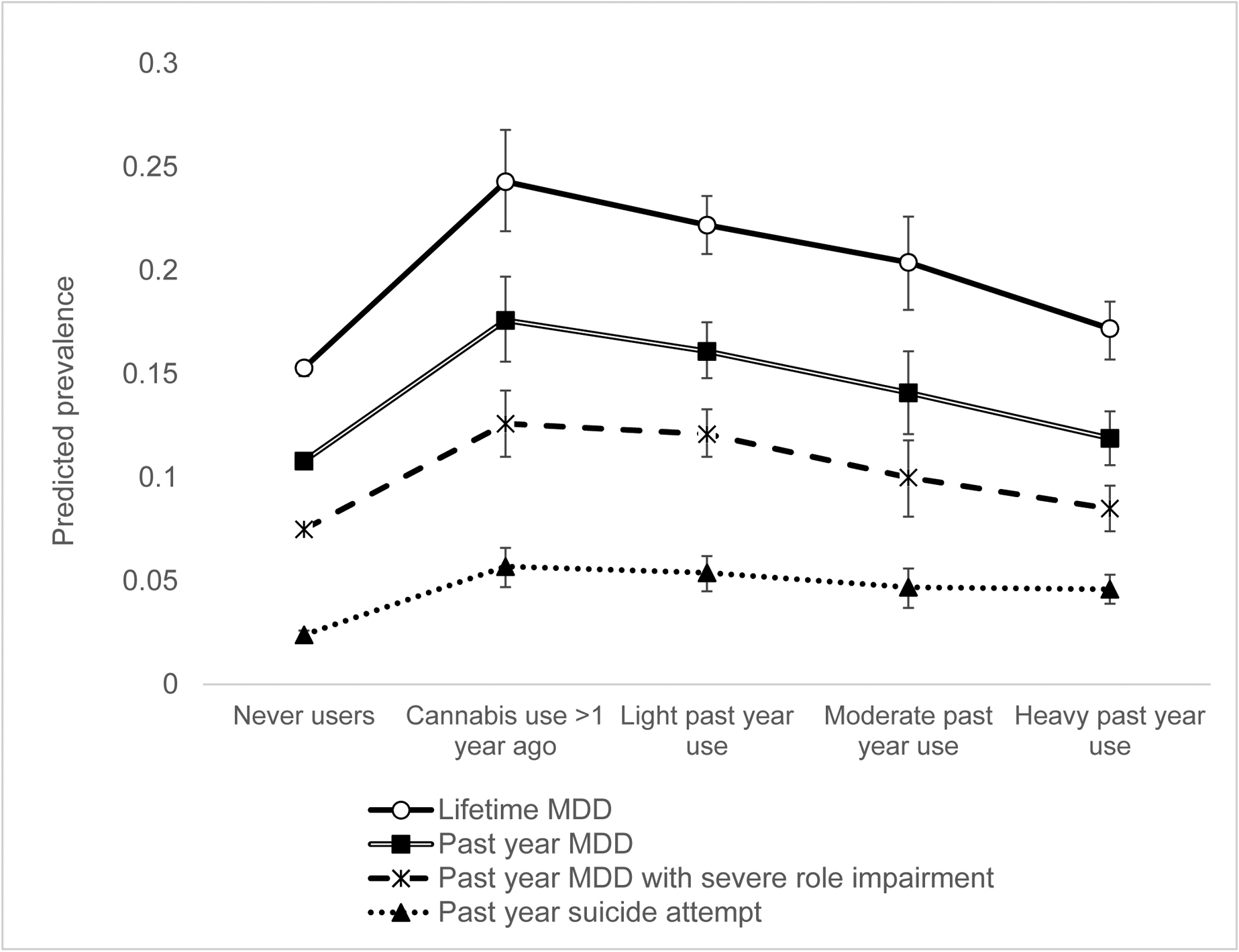
Predictive margins ± 95% confidence interval for depression and suicide attempt outcomes by cannabis use frequency. Plotted values represent predicted prevalence of specified outcome when adjusted for sociodemographic variables and past year use of substances other than cannabis.
Finally, weighted prevalence of past year treatment for depression (medications and/or psychotherapy) among those with past year MDD was significantly higher among cannabis users compared to never users (47.85% vs 38.7%, p<0.001), with heavy users having the highest reported rates (51.16%).
4.0. Discussion
Consistent with existing research, adolescents with a lifetime history of cannabis exposure were significantly more likely to meet criteria for lifetime and past year MDD, past year MDD with severe role impairment, and past year suicide attempt when compared to adolescents without a lifetime history of cannabis exposure. However, the striking finding from these analyses is that among cannabis users, higher frequency use in the past year was associated with lower rates of lifetime and past year MDD compared to lower frequency users and those who reported last using cannabis greater than 1 year ago. In fact, when adjusting for other covariates, heavy cannabis use was not associated with significantly different odds of past year MDD compared to never users. Although NSDUH does not provide data on depression severity, we approximated this using the past year MDD with severe role impairment variable. Similarly, higher frequency users reported lower rates of MDD with severe role impairment compared to less frequent users, and were not significantly different from never users.
Though higher frequency users had lower rates of past year MDD, rates of past year suicide attempt were no different when compared to other users. 20.9% of cannabis users with reported past year suicide attempt did not meet criteria for past year MDD. Anxiety or other psychiatric disorders may explain this finding. This may also reflect an association between cannabis use and impulsive behavior among adolescents (Solowij et al., 2012).
These findings regarding frequency of cannabis use and depression are unexpected and counter-intuitive. Given that adolescents who have used any cannabis are also more likely to have depression, one would expect that this would then demonstrate some form of a dose relationship – that is, that there would be increased prevalence or severity of depression associated with more cannabis use. However, the present findings show the opposite relationship in the subgroup of persons with a history of cannabis use – more frequent cannabis use was associated with lower depression metrics.
There are at least three explanations for these unexpected findings. The results could be interpreted to show either: 1) that there is a spurious relationship between the frequency of cannabis use and depression (as well as severity of depression) for adolescents that have used cannabis; 2) that the limitations of NSDUH mean we are unable to determine the relationship between cannabis use and depression in adolescents; or, 3) the relationship between cannabis use and depression in adolescents is complicated and more nuanced than a simple positive linear relationship between cannabis use and depression.
Considering each of these three explanations, first, it seems unlikely that the findings are simply spurious, as the present analyses were consistent with other studies in finding that there were higher rates of depression in persons with any cannabis use. It seems clear that depression and a history of cannabis use covary. Second, it may be the case that the NSDUH limitations are the issue with interpreting the present findings; for example, a person who uses cannabis once a day for 52 days may be more similar to a person who uses multiple times a day for 40 days, when considering the severity of use (but would be considered different in the present analyses). Unfortunately, NSDUH does not provide sufficient granularity of data to test different models of severity, and assessing cannabis use severity is inherently difficult (e.g., in normalizing the size of a dose consumed). Finally, our findings could reflect heterogeneity in cannabis users, with some adolescents using for subjective relief of depression, and others using for social or other factors. Previous studies on motives for cannabis use in adolescents and young adults have identified coping and social factors as significant predictors of cannabis use and dependence (Simons et al., 1998; Chabrol et al. 2005). Additionally, differences in rates of treatment for depression may be contributing to the observed results.
Consistent with other studies, our analyses identified use of alcohol and illicit drugs other than cannabis as significant risk factors for all depression-related outcomes. Female sex was also strongly associated with all depression outcomes, and the association was somewhat greater in magnitude than expected (Mojtabai et al., 2016). Others have previously identified sex differences in the relationship between substance use and depression among adolescents (Poulin et al., 2005; Shrier et al., 2001). Further research is needed to investigate the relationship between sex and cannabis use frequency on depressive symptomatology.
While the present findings raise further questions about the relationship between severity of cannabis use and severity of depression among adolescents with cannabis use, clinicians should be aware that even remote cannabis use in an adolescent suggests a higher likelihood of depression. Careful screening for depression in an adolescent with any history of cannabis use should be conducted. These findings also suggest that there may be different subgroups of adolescents with a cannabis use history, and raise intriguing questions about how these groups may vary in their underlying reasons for using cannabis. The limitations of NSDUH may constrain further work in understanding these subgroups, but this work provides a starting point for further prospective research on the relationship between cannabis use frequency and affective disorders in adolescence.
Supplementary Material
Highlights.
Depression is more prevalent among adolescents with cannabis use compared to never users.
Among cannabis users, higher frequency of use was associated with lower rates of depression.
Consistent with prior research, female sex, past year alcohol use, and illicit drug use other than cannabis were associated with depression and suicide attempt.
Acknowledgments
The authors wish to thank Linda Felch for her assistance with statistical analysis, and the reviewers for their helpful suggestions for strengthening this paper.
Role of funding source
This research was supported by the National Institute on Drug Abuse (NIDA) T32 Award (DA07209). The content is solely the responsibility of the authors and does not necessarily reflect the views of NIDA or the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest
NG has no conflicts to declare. ECS has consulted, done work for, or served on advisory boards to the following organizations: Analgesic Solutions, Caron, Indivior, Medscape, The Oak Group, Otsuka, Pinney Associates, and Up To Date.
References
- American Psychiatric Association. 2000. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR). 10.1176/appi.books.9780890423349 [DOI]
- Borges G, Bagge CL, Orozco R, 2016. A literature review and meta-analyses of cannabis use and suicidality. J. Affect. Disord 195, 63–74. 10.1016/j.jad.2016.02.007 [DOI] [PubMed] [Google Scholar]
- Cerdá M, Bordelois PM, Keyes KM, Galea S, Koenen KC, Pardini D, 2013. Cumulative and recent psychiatric symptoms as predictors of substance use onset: does timing matter? Addiction 108, 2119–2128. 10.1111/add.12323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chabrol H, Ducongé E, Casas C, Roura C, Carey KB, 2005. Relations between cannabis use and dependence, motives for cannabis use and anxious, depressive and borderline symptomatology. Addict. Behav 30, 829–840. 10.1016/j.addbeh.2004.08.027 [DOI] [PubMed] [Google Scholar]
- Cousijn J, Wiers RW, Ridderinkhof KR, van den Brink W, Veltman DJ, Goudriaan AE, 2012. Grey matter alterations associated with cannabis use: Results of a VBM study in heavy cannabis users and healthy controls. Neuroimage 59, 3845–3851. 10.1016/j.neuroimage.2011.09.046 [DOI] [PubMed] [Google Scholar]
- ElSohly MA, Mehmedic Z, Foster S, Gon C, Chandra S, Church JC, 2016. Changes in Cannabis Potency Over the Last 2 Decades (1995–2014): Analysis of Current Data in the United States. Biol. Psychiatry 79, 613–619. 10.1016/j.biopsych.2016.01.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gobbi G, Atkin T, Zytynski T, Wang S, Askari S, Boruff J, Ware M, Marmorstein N, Cipriani A, Dendukuri N, Mayo N, 2019. Association of Cannabis Use in Adolescence and Risk of Depression, Anxiety, and Suicidality in Young Adulthood. JAMA Psychiatry 76, 426 10.1001/jamapsychiatry.2018.4500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayatnakhsh MR, Najman JM, Jamrozik K, Mamun AA, Alati R, Bor W, 2007. Cannabis and Anxiety and Depression in Young Adults. J. Am. Acad. Child Adolesc. Psychiatry 46, 408–417. 10.1097/chi.0b013e31802dc54d [DOI] [PubMed] [Google Scholar]
- Hooshmand S, Willoughby T, Good M, 2012. Does the Direction of Effects in the Association Between Depressive Symptoms and Health-Risk Behaviors Differ by Behavior? A Longitudinal Study Across the High School Years. J. Adolesc. Heal 50, 140–147. 10.1016/j.jadohealth.2011.05.016 [DOI] [PubMed] [Google Scholar]
- Khantzian EJ, 1997. The Self-Medication Hypothesis of Substance Use Disorders: A Reconsideration and Recent Applications. Harv. Rev. Psychiatry 4, 231–244. 10.3109/10673229709030550 [DOI] [PubMed] [Google Scholar]
- Macleod J, Oakes R, Copello A, Crome I, Egger M, Hickman M, Oppenkowski T, Stokes-Lampard H, Smith GD, 2004. Psychological and social sequelae of cannabis and other illicit drug use by young people: a systematic review of longitudinal, general population studies. Lancet 363, 1579–1588. 10.1016/s0140-6736(04)16200-4 [DOI] [PubMed] [Google Scholar]
- Mojtabai R, Olfson M, Han B, 2016. National Trends in the Prevalence and Treatment of Depression in Adolescents and Young Adults. Pediatrics 138, e20161878–e20161878. 10.1542/peds.2016-1878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patton GC, 2002. Cannabis use and mental health in young people: cohort study. BMJ 325, 1195–1198. 10.1136/bmj.325.7374.1195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poulin C, Hand D, Boudreau B, Santor D, 2005. Gender differences in the association between substance use and elevated depressive symptoms in a general adolescent population. Addiction 100, 525–535. 10.1111/j.1360-0443.2005.01033.x [DOI] [PubMed] [Google Scholar]
- Shrier LA, Harris SK, Sternberg M, Beardslee WR, 2001. Associations of Depression, Self-Esteem, and Substance Use with Sexual Risk among Adolescents. Prev. Med. (Baltim) 33, 179–189. 10.1006/pmed.2001.0869 [DOI] [PubMed] [Google Scholar]
- Simons J, Correia CJ, Carey KB, Borsari BE, 1998. Validating a five-factor marijuana motives measure: Relations with use, problems, and alcohol motives. J. Couns. Psychol 45, 265–273. 10.1037//0022-0167.45.3.265 [DOI] [Google Scholar]
- Solowij N, Jones KA, Rozman ME, Davis SM, Ciarrochi J, Heaven PCL, Pesa N, Lubman DI, Yücel M, 2011. Reflection impulsivity in adolescent cannabis users: a comparison with alcohol-using and non-substance-using adolescents. Psychopharmacology (Berl). 219, 575–586. 10.1007/s00213-011-2486-y [DOI] [PubMed] [Google Scholar]
- Womack SR, Shaw DS, Weaver CM, Forbes EE, 2016. Bidirectional associations between cannabis use and depressive symptoms from adolescence through early adulthood among at-risk young men. Journal of studies on alcohol and drugs. 77, 287–297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang X, Wu L, 2014. Suicidal ideation and substance use among adolescents and young adults: A bidirectional relation? Drug Alcohol Depend. 142, 63–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


