Abstract
Introduction
This is the first published study on decompression illness (DCI) and its treatment in Finland. Diving conditions are demanding, as even in the summer the water temperature below 20 meters’ sea/fresh water (msw/mfw) is 4–10°C. Technical diving has become more popular over the years, so the emphasis of this study was to describe DCI in technical divers and compare it with non-technical recreational divers.
Methods
This study includes by estimation over 95% of all hyperbaric oxygen-treated DCI patients during the years 1999–2018 (n = 571). The cases were divided into technical divers (n = 200) and non-technical divers (n = 371). We focused on the differences between these two groups. Technical diving was defined as the usage of mixed breathing gases, closed circuit rebreather diving or planned decompression diving.
Results
The mean annual number of treated DCI cases in Finland was 29 (range 16–38). The number of divers treated possibly indicate a shift towards technical diving. Technical dives were deeper and longer and were mainly performed in cold water or an overhead environment. Technical divers were more likely to utilize first aid 100% oxygen (FAO2) and sought medical attention earlier than non-technical divers. Symptom profiles were similar in both groups. Recompression was performed using USN Treatment Table Six in the majority of the cases and resulted in good final outcome. Eighty two percent were asymptomatic on completion of all recompression treatment(s).
Conclusion
This 20-year observational study indicates a shift towards technical diving, and hence a more demanding and challenging style of diving among Finnish divers, with a surprisingly constant number of DCI cases over the years. There is still need for improvement in divers’ education in use of FAO2 for DCI symptoms. Fortunately, the outcome after recompression therapy is generally successful.
Keywords: Decompression sickness, Diving, Arctic diving, Hyperbaric oxygen treatment, First aid oxygen, Epidemiology
Introduction
Decompression illness (DCI) is a collective term embracing two dysbaric disorders.[ 1] Decompression sickness (DCS – caused by evolution of bubbles from dissolved inert gas) is the most common based on symptomatology.[ 1 , 2] In addition, arterial gas embolism (AGE – caused by introduction of air to the systemic circulation by pulmonary barotrauma) can cause serious neurological manifestations (typically multifocal cerebral dysfunction). Because of concerns that it may be difficult to distinguish clinically between DCS and AGE in some cases, the collective term DCI is often used in clinical studies such as this.[ 3] Thus, the DCI terminology is adopted here, although it is acknowledged the vast majority of cases in this series almost certainly have DCS as the underlying pathology.
The incidence of DCI (per dive) varies from 0.010% to 0.095% in different diver populations[ 1] and was recently reported as 0.0041% in a cohort of recreational divers.[ 4] The gold standard treatment for DCI is recompression in a hyperbaric chamber with administration of hyperbaric oxygen during the treatment.[ 1] Different treatment protocols have been suggested but the most commonly used one includes intermittent breathing of pure medical oxygen at a pressure of 284 kPa.[ 5 , 6] In Finland the US Navy Treatment Table 6 (USN TT6)[ 1] and an extended version of the same table, are the most commonly used. Hyperbaric oxygen treatment (HBOT) decreases the size of and removes inert gas bubbles, by increasing the off-gassing gradient.[ 1] It also increases tissue oxygenation in potentially injured tissues. HBOT for DCI is effective when instituted promptly. Most patients become asymptomatic or have only minor residual symptoms after the treatment.[ 1]
To our knowledge, there are no previous studies describing the diving, contributing factors, or the outcome after recompression among divers treated for DCI in Finland. The unique characteristic of this population is that the majority of dives were performed in arctic conditions that differ significantly from those in most other parts of the world; even in summer, the water temperature is 4–10°C in the usual recreational diving depths, i.e., below 20 metres' sea/fresh water (msw/mfw). Cold is an acknowledged risk factor for DCI[ 7 , 8] as it impairs peripheral blood circulation and thus off-gassing of inert breathing gas.
The purpose of this study was to describe different factors associated with DCI in Finland for a 20-year time period between 1999 and 2018. During this time the popularity of technical diving has increased in the recreational diving community; since the divers and diving profiles in technical and non-technical recreational diving differ significantly from each other, we studied the difference between these two groups.
Methods
PATIENT POPULATION
This retrospective study examined treated DCI cases over the period 1999 to 2018. Until 2015 over half (60%) of these patients were treated at the Hyperbaric Center Medioxygen in Helsinki, and the remaining patients at Turku University Hospital, especially if the patients required critical care. Since 2016 practically all Finnish DCI patients requiring recompression were treated at Turku University Hospital. During the study follow-up time, there have been only sporadic anecdotal DCI cases that were treated in the Finnish military facilities, in the Rescue Department or in private recompression chambers. The exact number of these patients is unknown, but they are less than 5% of the total Finnish DCI cases.
DATA COLLECTION
Ethical approval for the study was granted by National Institute for Health and Welfare, Helsinki, Finland (THL/285/5.05.00/2016). The study is compliant with the latest version of Declaration of Helsinki.
Data were collected from the medical records of the two aforementioned medical facilities. Previously, case record data collection was less systematic, with missing data, but later became more structured. The total number of retrieved DCI patient cases was 581, but 10 patients were excluded: in two patients the diagnosis of DCI could not be confirmed, in two patients data were missing from the case summary, and six patients were breath-hold divers who were treated for DCI-resembling symptoms. Hence, the final number of cases was 571.
DIVER POPULATION AND GROUPS
For the sake of this analysis these patients were divided to two groups: technical divers (tech; n = 200) and non-technical divers (non-tech; n = 371). A technical diver was defined as: 1) using mixed breathing gases (trimix, n = 71), 2) using a closed circuit rebreather (CCR, n = 39), 3) using air or nitrox and performing planned decompression diving with decompression stops using either air, nitrox or oxygen as an accelerated decompression gas (n = 90). A highly qualified diver (n = 307) was defined as a certification level of Confédération Mondeale des Activitiés Subaquatiques (CMAS) P3 or equivalent or higher, e.g., dive master, instructor, cave, trimix, etc. Less qualified divers (n = 203) possessed CMAS P1-2 (open water diver, advanced open water diver, rescue diver) level certification. In 61 cases there was no information about the certification level.
DIVING ENVIRONMENT
In this study the cold-water diving was performed in areas where water temperature in the diving depths is 4–10°C even in summer, i.e., Scandinavia. Warm water diving was defined as dives in Southern Europe, Asia or Africa. The diving environment was described as either as open water or overhead environment (waterfilled mine or cave).
STATISTICAL ANALYSIS
Statistical analyses were conducted with the IBM SPSS Statistics program (IBM Corp, Armonk (NY), USA), version 24. Continuous variables were assessed for normality using the Shapiro-Wilk test, group comparisons were done using Student’s t-test for normally distributed variables and the Mann-Whitney U test for non-normally distributed variables. Dichotomous variables were compared using the Chi-square test. A P-value of 0.05 or smaller was considered significant.
Results
EPIDEMIOLOGY
During the study period of 1999 to 2018 the number of recompressed DCI patients in Finland has varied in the range of 16 to 38 cases annually, with an average of 29 cases requiring recompression per year. A noteworthy trend is the increasing number of cases in technical divers over the years, as shown in Table 1. This probably reflects an increasing popularity of technical diving in the Finnish cohort diving community.
Table 1. The number of divers treated for DCI during the study in two-yearly groups, with specification of dive type and gas used during the incident dive. There was a shift towards technical diving in the later years seen in the number of technical divers treated for DCI. Complete data was available from all divers in this study: n = 571 .
| Divers | 1999–2000 | 2001–2002 | 2003–2004 | 2005–2006 | 2007–2008 | 2009–2010 | 2011–2012 | 2013–2014 | 2015–2016 | 2017–2018 |
| Non-technical | ||||||||||
| Air | 37 | 32 | 44 | 33 | 30 | 36 | 35 | 25 | 26 | 30 |
| Nitrox | 0 | 0 | 1 | 7 | 6 | 6 | 11 | 7 | 4 | 1 |
| Total | 37 | 32 | 45 | 40 | 36 | 42 | 46 | 32 | 30 | 31 |
| Technical | ||||||||||
| Air | 1 | 1 | 3 | 3 | 4 | 3 | 3 | 2 | 6 | 5 |
| Nitrox | 2 | 3 | 2 | 9 | 8 | 3 | 2 | 3 | 14 | 13 |
| Trimix | 1 | 4 | 6 | 9 | 11 | 8 | 9 | 4 | 7 | 12 |
| Rebreather | 0 | 1 | 0 | 2 | 6 | 5 | 9 | 3 | 6 | 7 |
| Total | 4 | 9 | 11 | 23 | 29 | 19 | 23 | 12 | 33 | 37 |
DIVERS
Demographic data are shown in Table 2. When compared to non-technical divers, technical divers were more likely to be male (87% vs. 73%, P < 0.001), older (mean (SD): 38 (8) years vs. 35 (8) years, P < 0.001) and more highly qualified (93% vs. 41%, P < 0.001). There was no difference in between the groups in underlying medical conditions that would normally prohibit diving nor in previous medication use. Smoking was similar in both groups, and was comparable to the general population.[ 9] The rate of previously treated DCI was rather high in both groups (43% vs. 34%, P = 0.081), showing that divers continue diving after successful treatment of DCI.
Table 2. Baseline characteristics for divers treated for DCI in Finland 1999–2018. Data are n (%) unless otherwise specified. Information on 'previous DCI' was available for technical: n = 135 and non-technical divers: n = 194, and on 'qualification level ≥ P3' for technical: n = 175 and non-technical divers: n = 132. Percentages for these two parameters are based on these available data. For other parameters information was available from all divers in this study: n = 571 .
| Males | Age mean (range) | Qualification ≥ P3 | Underlying disease | Medical treatment | Smoking | Previous DCI | |
| All | 446 (78) | 36 (18–62) | 307 (60) | 82 (14) | 65 (11) | 51 (9) | 123 (37) |
| Non-technical | 272 (73) | 35 (18–62) | 132 (41) | 56 (15) | 40 (11) | 32 (9) | 65 (34) |
| Technical | 174 (87) | 38 (18–62) | 175 (93) | 26 (13) | 25 (13) | 19 (10) | 58 (43) |
INCIDENT DIVE
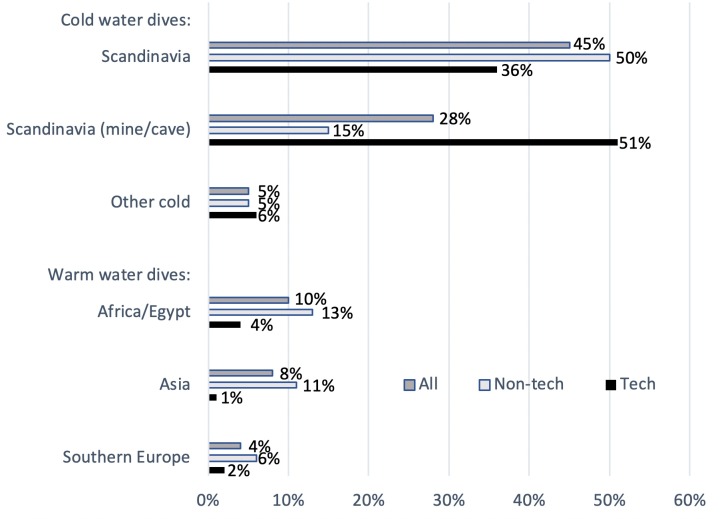
Detailed information of the diving location is given separately for technical and non-technical divers in Figure 1. The incident dive that resulted in DCI was defined as a technical dive in 35% of the cases. Divers were using trimix (36%) or CCR (20%) in 56% of these cases. Technical divers were diving in a cold-water environment in 93% of cases compared to 70 % of non-technical divers (P < 0.001). The median maximum depth of the dive was 45 msw/mfw for technical divers (range: 11–209) vs. 25 msw/mfw (range 4–56) for non-technical divers (P < 0.001), and the median duration of the dive for technical dives was 65.5 minutes (range: 17–420) vs. 35 minutes (range: 4–238) for non-technical dives (P < 0.001). A particular feature in Finnish diving is the large number of dives performed in overhead flooded old mines or quarries. The popularity of these diving locations is explained by the improved visibility in water as compared to seaside or lake locations. Although diving conditions are rather stable in these sites, they are still demanding, with 4°C water temperature all year round and an overhead environment. Over half (51%) of DCI cases in the technical diving group arose from dives performed in these mines.
Figure 1.
Diving location of the incident dive, for the whole group and separately for technical and non-technical dives. Cold water dives and warm water dives are presented under their own headings. ‘Scandinavia’ does not include mine/cave dives in Scandinavia, these are presented as a separate group. ‘Other cold’ includes cold dives in other locations, e.g., deep-sea dives and dives in northern countries outside Scandinavia. Information was available from tech: n = 193 and non-tech: n = 349. The percentages are based on these available data
CONTRIBUTING FACTORS
Assessment of potential predisposing factors was performed during the interview with the diver and the diving profile was evaluated when available (Figure 2). Contributing factors could be elucidated in 76% of the cases. Predisposing factors included: consecutive diving days (technical: 52% vs. non-technical: 54%, P = NS); multiple dives per day (technical: 21% vs. non-technical: 47%, P < 0.001); and flying after diving (technical: 14% vs. non-technical: 38%, P < 0.001). These are common features of diving vacations and diving safaris in the warm water environment. Fast ascent rates were reported in 50% of DCI cases in the non-technical patients (vs. technical: 21 %, P < 0.001). In the technical diving group the deeper and longer dives per se may have contributed to the risk of DCI. Other risk factors in the technical group were: consecutive diving days (52%); dehydration (technical: 27% vs. non-technical: 13 %, P = 0.001) during these long dives; and cold water (technical: 10% vs. non-technical 5%, P = NS), which causes reduced peripheral tissue perfusion, reducing inert gas elimination in these tissues.
Figure 2.
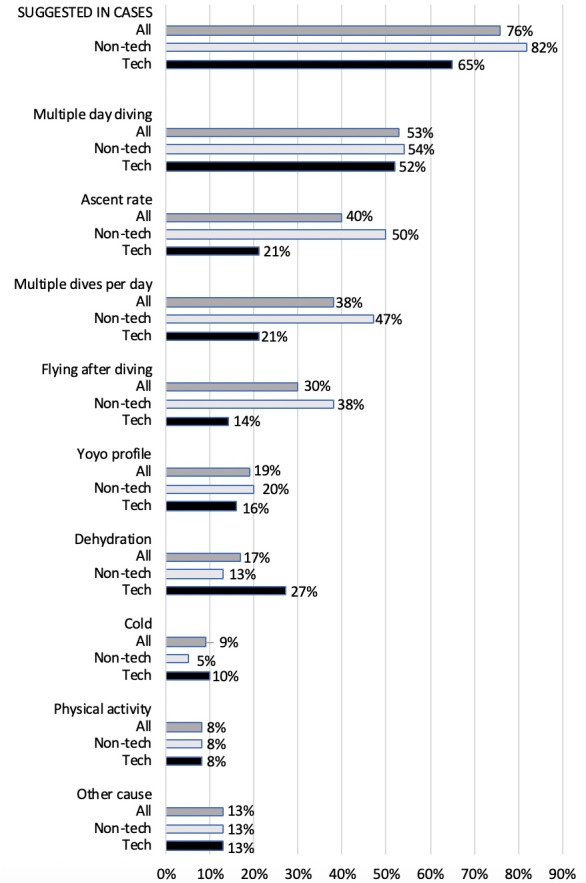
Suggested contributing factors for DCI. The first three bars ‘suggested in cases’ show the percentages of divers to whom one or more contributing factors were suggested. The other columns show this information for different possible factors separately. ‘Other causes’ include travelling by road over high mountains (which is quite usual for Finnish divers on diving trips in Norway), technical problems during diving, problems with the breathing gas and acute medical conditions. Data are presented for all divers, and for subgroups technical and non-technical dives separately. Information was available from all divers in this study: n = 571
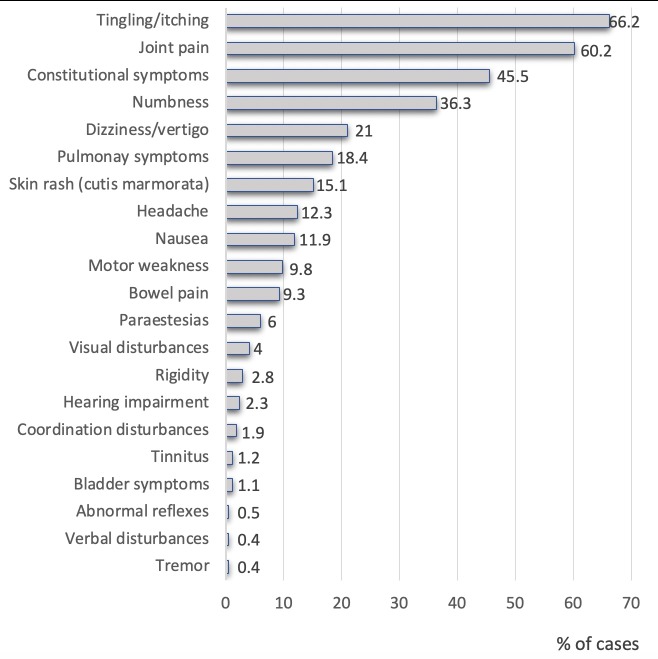
SYMPTOMS AND TREATMENT OF DCI
Presenting symptoms are shown in Figure 3. Tingling/itching was the most common symptom (66.2% of cases) followed by musculoskeletal pain (60.2%), constitutional symptoms (tiredness, light-headedness, excessive fatigue and malaise, 45.5%), numbness (36.3%) and dizziness/vertigo (21%). More serious manifestations included pulmonary symptoms (18.4%) and neurological symptoms (17.7%), subdivided into motor weakness (9.8%), visual disturbances (4%), coordination disturbances (1.9%), bladder symptoms (1.1%), abnormal reflexes (0.5%) and verbal disturbances (0.4%).
Figure 3.
Percentage of cases experiencing particular symptoms prior to the first recompression treatment. Constitutional symptoms include tiredness, light-headedness, inappropriate fatigue and malaise. Information was available from all divers in this study: n = 571
To determine possible differences in DCI symptoms in technical versus non-technical divers, we compared the symptom data of the last three years, when the data was more comprehensive (2016 to 2018, all treated in Turku University Hospital). Significant differences were seen in the prevalence of tingling/itching (technical: 49% vs. non-technical: 69%, P = 0.05), skin rash or cutis marmorata (technical: 40% vs. non-technical: 19%, P < 0.05) and headache (technical: 4% vs. non-technical: 17%, P < 0.05).
First aid oxygen (FAO2) was utilized on-site before admission to the hyperbaric chamber in 31% of all patients. However, 52% of technical divers had used FAO2 compared to only 19% of non-technical divers (P < 0.001). This most likely reflects the availability of the oxygen on-site and the level of diving education. Median delay to recompression was 24 h (range: 1–510) in technical divers compared to 48 h (range: 1–1008) in non-technical divers (P < 0.001).
Primary treatment protocols were similar; most of the divers (79%) were treated with USN TT6 with or without extensions. Divers received more than one HBOT session in 55% of cases but there was no difference between the groups. Mean number of additional recompressions was 1.36 (range: 0–15). Additional recompressions followed different protocols over the years. Previously, the most commonly used protocol was 90–104 minutes at 243–253 kPa. Lately, the most common protocol has been either the USN TT6 or USN TT5 when patients had residual symptoms after the primary treatment.
Clinical outcomes were generally good. After HBOT, 82% of the patients were completely asymptomatic in both groups. Mild residual symptoms were present in 14% and the rate of unfit-to-dive was 4%. The latter group included the divers that had decided voluntarily themselves, especially for psychological reasons, not to return to diving. Additional reasons were clinical, and included, for example, permanent hearing impairment or vestibular residua.
Discussion
To our knowledge, this is the first study describing DCI in Finnish divers, with the majority of dives performed in an arctic diving environment. Throughout the year diving occurs in a very cold environment, which provides additional challenges to the divers. This study suggests a likely increase in number of divers using mixed breathing gases and/or closed-circuit rebreather diving in these arctic conditions. However, the annual number of DCI cases treated with recompression has remained at a constant level over the years. The increment of technical dives corresponds to deeper and longer dives, which translates to an increased risk of DCI in the well-educated divers.
Compared to a similar large study from Denmark,[ 10] this study reports a higher number of DCI cases per year (mean: 29 in Finland vs. 14 in Denmark[ 10]), even though the population of these two countries is similar. However, there are no statistics on the numbers of divers or diving activity in Denmark or Finland, and without an accurate denominator of this nature it is difficult to interpret the different numbers of DCI cases recompressed in the two countries. In addition, many Finns receive their certification abroad, and hence are not recorded at all in the Finnish statistics.
In this study, the recompressed divers were similar to those in the Danish study[ 10] and another large study from New Zealand.[ 11] The majority of the divers were males, with 78% vs. 79%[ 10] vs. 81%[ 11 and the mean age was 36 years vs. 35.5 years[ 10] vs. 33.6 years.[ 11] The special feature of this study of DCI patients requiring recompression therapy was the significant number of technical divers. In the New Zealand study, only 3.4% of the divers were using mixed gases in comparison to our study. Similarly, only 1% of New Zealand patients were using closed-circuit rebreathers compared to 6.8% of Finnish patients. The depth of the incident dive was similar in our non-technical group (25 msw/mfw) to that of the New Zealand cohort (25.8 msw/mfw), whereas the technical divers went deeper in the present study. Combining this with the effects of cold, it can be concluded that Finnish divers developing DCI tend to perform very demanding dives which may provide an explanation why we have not witnessed the decrease in the number of the DCI cases demonstrated in New Zealand or Denmark. The Danish study provided no details of the incident dive nor the breathing gases used. Interestingly, 37% of Finnish DCI patients in this study had previously been recompressed for DCI, indicating that these divers were strongly committed to diving or have a tendency to risky diving procedures.
The most common symptoms of DCI in this study were tingling/itching, musculoskeletal pain, constitutional symptoms, numbness and dizziness/vertigo. This finding is similar to previous reports, although the prevalence of the symptoms varies.[ 1 , 10 , 11] When analysing the subgroups (technical vs. non-technical) over the last three years of the study, the prevalence of most symptoms was similar in both groups. Only tingling/itching, skin rash/cutis marmorata and headache were demonstrated to have significantly different prevalence between the groups. The similarity of symptoms in both groups was an unexpected finding, as it could have been anticipated that in the long and deep dives (i.e., technical dives) the slow tissues would have absorbed more inert gas and when ascending in arctic diving conditions, due to decreased blood flow in peripheral tissues, could have exaggerated bubble formation in supersaturated tissues.
Usage of FAO2 is still relatively uncommon, even though oxygen provider courses have been available for several years and many training organizations are requiring this certification when progressing through training levels.
In this study, only 31% of the divers had received FAO2. However, the proportion was significantly higher in technical divers. This was most likely due to better availability of breathing grade oxygen on the dive site. It is also possible that many mild DCI cases never encounter medical facilities as the divers treat the symptoms with normobaric oxygen or in-water recompression. The use of FAO2 in this study corresponds with earlier studies, which illustrated that 23–47% of divers were provided with FAO2 prior to HBOT.[ 12 , 13] USN TT6 with or without extension was the most commonly used treatment in all three studies (79% vs. 69%[ 10] vs. 65%[ 11]). The rate of required additional recompressions was also comparable (1.36 vs. 1.27[ 11).
In this study, HBOT was effective, evidenced by cases reaching complete (82%) or near complete (96%) recovery. This differs from previous reports, which have demonstrated an elevated rate of residual symptoms at hospital discharge (22–55%).[ 10 , 14 - 17] One explanation for this could be the difference in the re-treatment protocols. Furthermore, if the hospital discharge occurs within 12 hours after treatment, mild re-occurring DCI symptoms might still be absent, as symptoms often re-occur 12–24 hours after HBOT.[ 18] Most patients in this study were asymptomatic after only one or two treatments. If required, patients with residual or recurring symptoms were treated up to 15 times until symptoms had disappeared or a plateau in symptom improvement was reached. For the repetitive HBOT protocol there is no gold standard, although HBOT per se is recommended.[ 1]
An interesting finding is the high number of divers previously treated for DCI in both groups. It is possible that this could partly be explained with a good treatment outcome. A diver that recovers completely from DCI is more likely to continue diving compared to one that has residual symptoms. It is also plausible that the Finnish diving population contains a high proportion of motivated and focused enthusiasts who dive a lot and are therefore more likely to suffer problems. Highly motivated divers tend to continue diving after an adverse event. The high proportion of technical divers lends credibility to this theory.
During the 20-year observation period the HBOT re-treatment protocol has varied. The majority of the patients in this study received a shorter secondary treatment of 90 minutes at 243 kPa similar to other studies.[ 11 , 19] Recently, the preferred protocol for re-treatment in this population has been the USN TT6, with or without an extension, or USN TT5. Although not statistically significant, there have been observations that the USN TT6 confers better clinical outcomes than 90 minutes HBOT at 200 kPa irrespective of the severity of symptoms,[ 20] but this was a comparison of the protocols as a primary treatment rather than in re-treatment. Another comparison of primary treatment with shorter treatment tables (e.g., USN TT5) compared to longer tables (e.g., USN TT6) demonstrated better outcomes for the longer tables,[ 21] but again, it must be emphasized that this comparison was in primary treatment. When considering repetitive treatments, however, the cumulative and toxic effects of oxygen (i.e., UPTD, Unit Pulmonary Toxic Dose) should also be taken into account.[ 22 , 23]
LIMITATIONS
There are some limitations in this retrospective study. The long observation time was associated with many changes in data collection and treatment protocols. Previously, data collection was unstructured, resulting in a number of missing data points in the early cases. Also, the treatment protocols, particularly for re-treatments, were changing over the study period. Additionally, no systematic long-term follow-up of DCI patients to evaluate the final outcome is available. Some divers with residual symptoms after the HBOT may have completely recovered.
Conclusions
Although this study indicates an increasing popularity of technical diving in the Finnish diving community and a shift towards more demanding dives, the annual number of DCI cases has been constant. A marked observation is that DCI occurs in well-trained Finnish divers, who are performing challenging dives in all-year-around arctic conditions. Recently, half of the DCI cases requiring recompression therapy among technical divers occurred after dives in water-filled caves or quarries. Most divers recover well after treated DCI and a high rate of previously treated DCI in both technical and non-technical divers suggests that motivated divers continue diving after successful treatment of DCI. There is a need for improvement in the education of divers regarding the use of FAO2 in treatment of DCI symptoms. Availability of FAO2 on the dive site and by the dive operators should be mandatory.
Footnotes
Acknowledgements
We thank Kari Keski-Saari, RN and Eveliina Loikas, RN from the National Hyperbaric Unit of Turku University Hospital for their help in data collection.
Conflict of interest and funding: nil
Contributor Information
Richard V Lundell, Diving Medical Centre, Centre for Military Medicine, Finnish Defence Forces, Helsinki, Finland; Helsinki University, Helsinki, Finland.
Olli Arola, National Hyperbaric Oxygen Therapy Center, Intensive Care Unit, Turku University Hospital, Turku, Finland.
Jari Suvilehto, Hyperbaric Center Medioxygen, Helsinki, Finland.
Juha Kuokkanen, Hyperbaric Center Medioxygen, Helsinki, Finland.
Mika Valtonen, National Hyperbaric Oxygen Therapy Center, Intensive Care Unit, Turku University Hospital, Turku, Finland.
Anne K Räisänen-Sokolowski, Helsinki University, Helsinki, Finland; Hyperbaric Center Medioxygen, Helsinki, Finland; Department of Pathology, HUSLAB, Helsinki University Hospital, Helsinki, Finland.
References
- Vann RD, Butler FK, Mitchell SJ, Moon RE. Decompression illness . Lancet . 2011;377(9760):153–64. doi: 10.1016/S0140-6736(10)61085-9. [DOI] [PubMed] [Google Scholar]
- Xu W, Liu W, Huang G, Zou Z, Cai Z, Xu W. Decompression illness: clinical aspects of 5278 consecutive cases treated in a single hyperbaric unit . PLoS One. 2012;7(11):e50079. doi: 10.1371/journal.pone.0050079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell SJ. DCS or DCI? The difference and why it matters . Diving Hyperb Med. 2019;49:152–3. doi: 10.28920/dhm49.3.152-153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hubbard M, Davis FM, Malcolm K, Mitchell SJ. Decompression illness and other injuries in a recreational dive charter operation . Diving Hyperb Med. 2018;48:218–23. doi: 10.28920/dhm48.4.218-223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moon RE, Gorman DF. Decompression sickness. In: Neuman TS, Thom SR, editors. . Physiology and medicine of hyperbaric oxygen therapy. Philadelphia (PA): Saunders; 2008. p. 283- 319. [Google Scholar]
- Bennett MH, Mitchell SJ, Young D, King D. . The use of deep tables in the treatment of decompression illness: The Hyperbaric Technicians and Nurses Association 2011 workshop . Diving Hyperb Med. 2012; 42: 171- 80. Online supplement available from: https://www.eubs.org/documents/DHM%20Sep2012%20Suppl%20Treatment%20tables.pdf. [PubMed] [Google Scholar]
- Gerth WA. On diver thermal status and susceptibility to decompression sickness . Diving Hyperb Med. 2015;45:208. [PubMed] [Google Scholar]
- Pendergast DR, Senf CJ, Fletcher MC, Lundgren CE. Effects of ambient temperature on nitrogen uptake and elimination in humans . Undersea Hyperb Med. 2015;42:85–94. [PubMed] [Google Scholar]
- Finnish institute for health and welfare . Smoking in Finland. Smoking among adult population. Date of issue: 2018 March 14. Available from: https://thl.fi/en/web/alcohol-tobacco-and-addictions/tobacco/smoking-in-finland cited 2019 June 10.
- Svendsen Juhl C, Hedetoft M, Bidstrup D, Jansen EC, Hyldegaard O. Decompression illness treated in Denmark 1999–2013 . Diving Hyperb Med. 2016;46:87–91. [PubMed] [Google Scholar]
- Haas RM, Hannam JA, Sames C, Schmidt R, Tyson A, Francombe M, et al. Decompression illness in divers treated in Auckland, New Zealand, 1996-2012 . Diving Hyperb Med. 2014;44:20–5. [PubMed] [Google Scholar]
- Bessereau J, Genotelle N, Brun PM, Aboab J, Antona M, Chenaitia H, et al. Decompression sickness in urban divers in France . Int Marit Health. 2012;63:170–3. [PubMed] [Google Scholar]
- Longphre JM, Denoble PJ, Moon RE, Vann RD, Freiberger JJ. First aid normobaric oxygen for the treatment of recreational diving injuries . Undersea Hyperb Med. 2007;34:43–9. [PubMed] [Google Scholar]
- Kot J, Sićko Z, Michalkiewicz M, Lizak E, Góralczyk P. Recompression treatment for decompression illness: 5-year report (2003-2007) from National Centre for Hyperbaric Medicine in Poland . Int Marit Health. 2008;59:69–80. [PubMed] [Google Scholar]
- Gempp E, Blatteau JE. Risk factors and treatment outcome in scuba divers with spinal cord decompression sickness . J Crit Care. 2010;25:236–42. doi: 10.1016/j.jcrc.2009.05.011. [DOI] [PubMed] [Google Scholar]
- Blatteau JE, Gempp E, Simon O, Coulange M, Delafosse B, Souday V, et al. Prognostic factors of spinal cord decompression sickness in recreational diving: retrospective and multicentric analysis of 279 cases . Neurocrit Care. 2011;15:120–7. doi: 10.1007/s12028-010-9370-1. [DOI] [PubMed] [Google Scholar]
- Aharon-Peretz J, Adir Y, Gordon CR, Kol S, Gal N, Melamed Y. Spinal cord decompression sickness in sport diving . Arch Neurol. 1993;50:753–6. doi: 10.1001/archneur.1993.00540070065017. [DOI] [PubMed] [Google Scholar]
- Tempel R, Severance HW. Proposing short-term observation units for the management of decompression illness . Undersea Hyperb Med. 2006;33:89–94. [PubMed] [Google Scholar]
- Bennett MH, Lehm JP, Mitchell SJ, Wasiak J. Recompression and adjunctive therapy for decompression illness . Cochrane Database Syst Rev. 2012;(5):CD005277. doi: 10.1002/14651858.CD005277.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hadanny A, Fishlev G, Bechor Y, Bergan J, Friedman M, Maliar A, et al. Delayed recompression for decompression sickness: retrospective analysis . PLoS One. 2015;10(4):e0124919. doi: 10.1371/journal.pone.0124919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sayer MD, Ross JA, Wilson CM. Analyses of treatment for divers with actual or suspected decompression illness . Diving Hyperb Med. 2009;39:126–32. [PubMed] [Google Scholar]
- Thorsen E, Aanderud L, Aasen TB. Effects of a standard hyperbaric oxygen treatment protocol on pulmonary function . Eur Respir J. 1998;12:1442–5. doi: 10.1183/09031936.98.12061442. [DOI] [PubMed] [Google Scholar]
- Donald KW. Oxygen poisoning in man . Br Med J. 1947;1(4506):667; passim. [PMC free article] [PubMed] [Google Scholar]