Abstract
BACKGROUND
Hepatectomy is the main treatment for patients with hepatocellular carcinoma (HCC) and it has a high possibility for long-term cure potential. But the postoperative mortality and recurrence rates remain high. Since the long-term prognosis of HCC patients is strongly linked to liver function, preoperative assessment of liver function is very important for HCC patients.
AIM
To compare the predictive power of the modified Child-Pugh (MCP) and albumin-bilirubin (ALBI) grades for the long-term outcome of HCC.
METHODS
From January 2010 to June 2017, a total of 204 patients with HCC who underwent surgery at the Second Affiliated Hospital of Chongqing Medical University were enrolled in this retrospective study. Multivariate Cox regression analysis was used to determine the independent predictive factors of survival and relapse. The area under the curve (AUC) was used to evaluate the discriminative performance of the MCP grade and ALBI grade to predict the postoperative overall survival (OS) time and recurrence-free survival (RFS) time.
RESULTS
The median OS and RFS times were 44.0 mo (range: 22.0-74.0 mo) and 22.0 mo (range: 5.0-45.0 mo), respectively. The median OS and RFS times of MCP grades 1, 2, and 3 patients were 60.0, 39.0, and 18.0 mo (P < 0.001) and 36.0, 15.0, and 7.0 mo (P < 0.001), respectively. The median OS and RFS times of ALBI grades 1, 2, and 3 patients were 56.0, 26.0, and 6.0 mo (P < 0.001) and 25.0, 10.0, and 3.0 mo (P = 0.003), respectively. Both the MCP and ALBI grades were more accurate than the Child-Pugh grade for predicting long-term prognosis. Further analysis demonstrated that for both predicting OS and RFS, the MCP grade performed better than the ALBI grade (AUC: 0.642 vs 0.605 for OS; 0.659 vs 0.594 for RFS).
CONCLUSION
The MCP grade is more accurate than the ALBI grade for predicting long-term outcome of patients with HCC.
Keywords: Modified Child-Pugh grade, Albumin-Bilirubin grade, Hepatocellular carcinoma, Prognosis, Hepatectomy, Child-Pugh
Core tip: We discovered that only a few studies have evaluated the predictive power of prealbumin-involving modified Child-Pugh (MCP) grade for the prognosis of patients with hepatocellular carcinoma (HCC). The objective, recognizable, and simple method, the albumin-bilirubin (ALBI) grade, for predicting the long-term prognosis of HCC patients has been widely proven in the international environment. In this study, receiver operating characteristics curve analysis showed that the MCP grade had higher accuracy than the ALBI grade, and the area under the curve of the MCP grade was larger than that of the ALBI grade. The MCP grade may be the best tool for the selection of HCC treatment strategies.
INTRODUCTION
Hepatocellular carcinoma (HCC) is the second most common cancer and the fifth most common cause of cancer-related death in the world[1]. Hepatectomy is the main treatment for HCC[2] and it has a high possibility for long-term cure potential[2-4]. Unfortunately, the postoperative mortality and recurrence rates remain high. It is widely perceived that the prognosis of HCC is related to many clinical factors such as tumor characteristics, vascular invasion, and liver function[5,6]. Thus, evaluating liver function is critical for the prognosis of HCC patients.
The Child-Pugh (C-P) grade is widely used as a standard measure of liver function[7,8] and prognostic tool[9,10]. However, the C-P grading system has some limitations. The two variables of ascites and hepatic encephalopathy are highly subjective, and some indicators such as ascites and albumin are correlated[11,12]. Therefore, as an objective, recognizable, and simple method for evaluating HCC liver function, the albumin-bilirubin (ALBI) grade was proposed and has been widely proven in the international environment[13]. This score includes only two variables, albumin and total bilirubin, and has a preferable prognostic ability for the survival analysis of HCC patients compared with the C-P score[12,14]. Prealbumin (PA) is a new and reliable indicator of liver function. Many studies have confirmed the predictive value of serum PA for liver function[7,15,16] and the long-term prognosis of patients with HCC[16-18]. It has been reported that the integration of PA into the C-P scoring system to form a modified C-P (MCP) scoring system that includes four factors, PA, albumin, total bilirubin, and prothrombin time, and removes the subjective indicators of ascites and hepatic encephalopathy can improve the accuracy of prognosis prediction in HCC patients[19]. However, the relevant data is still not enough. So, based on the fact that both the MCP and ALBI scores are objective, simple, and easy to obtain, we analysed and compared the predictive power of the MCP and ALBI scores for the long-term outcome of hepatectomy patients with HCC. Then, a scoring system with higher accuracy for predicting the overall survival (OS) time and recurrence-free survival (RFS) time of HCC patients can be selected. This will provide a more effective, objective, and simple method to assess the prognosis of HCC patients undergoing hepatectomy and make it easier and more accurate for surgeons to select suitable HCC patients for hepatectomy.
MATERIALS AND METHODS
Patients
We included 204 patients with HCC who underwent hepatectomy from January 2010 to June 2017 at the Second Affiliated Hospital of Chongqing Medical University. The inclusion criteria were as follows: (1) Pathology identified as HCC; (2) No treatment prior to hepatic resection and no other malignancies; and (3) Adequate clinical data that could be assessed in the hospital. In the first year after hepatectomy, all of the patients were followed every 3 mo and then every 6 mo in the following years. The diagnosis of tumour recurrence was based on image findings. The last follow-up was in June 2019 or the day the patient died. And during our follow-up, one patient died due to severe postoperative liver failure on the day of the hepatectomy, and two patients were lost to follow-up. This study was registered at www.chictr.org.cn (ChiCTR1900026738) (Supplementary Table 1 contains study data of this study). The study was in line with the ethical guidelines of 1964 Helsinki Declaration and was approved by the review committee of the Second Affiliated Hospital of Chongqing Medical University.
Data collection
We collected patient data including sex, age, body mass index (BMI), cause of hepatitis, portal hypertension (PH), liver cirrhosis, BCLC (Barcelona Clinic Liver Cancer) stage, and C-P grade. The biochemical indicators were as follows: Serum PA, serum albumin (ALB), total bilirubin (TBIL), prothrombin time (PT), alanine aminotransferase (ALT), alpha-fetoprotein (AFP), international normalised ratio (INR), and platelet count (PLT). The tumor characteristics included the number of tumors, tumor size, portal vein tumor thrombus (PVTT), capsule formation, and differentiation. The intraoperative parameters included surgical bleeding, blood transfusion, type of liver resection, and intraoperative radiotherapy and/or chemotherapy. Based on previous description, the calculation formula of ALBI score was as follows: ALBI = log10 bilirubin × 0.66 + albumin × (-0.085), where the bilirubin is expressed in µmol/L and the albumin in g/L. The ALBI grades were classified as follows: ≤ -2.60, grade 1; > -2.60 to ≤ -1.39, grade 2; and ≥ -1.39, grade 3[13]. For the MCP scoring system, the sex difference was considered using receiver operating characteristics (ROC) curve plots to set the optimal cut-off values for male and female PAs, respectively. The PA levels in the male and female patients ranged from 130 mg/L to 190 mg/L and 120 mg/L to 170 mg/L, respectively, similar to a previous report[19]. The MCP scoring system is shown in Table 1.
Table 1.
Modified Child-Pugh scoring system
| Item |
Score |
||
| 1 | 2 | 3 | |
| TBIL, µmol/L | < 34 | 34-51 | > 51 |
| ALB, g/L | > 35 | 28-35 | < 28 |
| Prothrombin time prolongation, s | < 4 | 4-6 | > 6 |
| PA for males, mg/L | > 190 | 130-190 | < 130 |
| PA for females, mg/L | > 170 | 120-170 | < 120 |
MCP-1 (score = 4), MCP-2 (score = 5), and MCP-3 (score = 6).
Statistical analysis
mean ± SD or median (quartile range) is used to present the continuous variables. The categorical variables are presented as n (%) and were compared via the χ2 test or Fisher's exact test. Kaplan-Meier analysis was used to evaluate the OS and RFS rates and the independent predictive factors for survival and relapse were determined by multivariate Cox regression analysis. The cut-off value was determined via the ROC curve. Areas under the ROC curves (AUCs) were used to evaluate the accuracy of the MCP and ALBI scoring systems to predict the postoperative survival time and RFS time in the HCC patients. The difference was considered statistically significant at P < 0.05. All of the statistical analyses were conducted using SPSS 20.0 software. The statistical methods of this study were reviewed by Jian Gao, who is both the corresponding author and the biomedical statistician of this article.
RESULTS
Patient characteristics
A total of 204 patients with HCC who underwent hepatectomy were enrolled in this study, and the median follow-up time was 36 mo. As shown in Table 2, there were 174 (85.3%) males and 30 (14.7%) females with a mean age of 52.0 ± 11.4 years. Most of the patients (85.3%) had a viral hepatitis B background, 120 (58.8%) patients had liver cirrhosis, and most patients (72.5%) have been implanted with radiation particles (I125 or I131) or chemotherapy pumps during the surgery. Of the 204 patients, 113 (55.4%) had BCLC stage 0 or A disease, 62 (30.4%) had stage B, and 29 (14.2%) had stage C; and 187 (91.7%) were classified as C-P grade A, 17 (8.3%) were classified as B, and there was no patient classified as grade C. According to the ALBI grade, 136 (66.7%) had grade 1, 66 (32.4%) had grade 2, and only 2 (0.9%) had grade 3. For the MCP grade, 110 (53.9%), 52 (25.5%), and 42 (20.6%) patients were classified as grades 1, 2, and 3, respectively. The median OS and RFS times were 44.0 mo and 22.0 mo, respectively.
Table 2.
Baseline characteristics of the 204 patients
| Variable | All patients (n = 204) |
| Sex (male/female) | 174/30 |
| Age, yr | 52.0 ± 11.4 |
| BMI, kg/m2 | 23.2 ± 3.6 |
| Cause of hepatitis (Hepatitis B/C/Others) | 174/2/28 |
| PH (yes/no) | 48/156 |
| Liver cirrhosis (yes/no) | 120/84 |
| P grade (A/B) | 187/17 |
| BCLC stage (0 or A/B/C) | 113/62/29 |
| PA, mg/L | 198.5 (149.3-238.0) |
| ALB, g/L | 41.0 ± 4.7 |
| TBIL, μmol/L | 13.3 (9.7-18.3) |
| PT, s | 13.7 (13.0-14.5) |
| ALT, U/L | 36.0 (26.3-56.0) |
| AFP, μg/L | 76.4 (9.02-1082.5) |
| INR | 1.0 (0.98-1.1) |
| PLT, × 109/L | 135.0 (99.8-181.0) |
| Number of tumors (1/2/≥3) | 161/27/16 |
| Tumor size, cm | 4.0 (3.0-6.5) |
| PVTT (yes/no) | 30/174 |
| Capsule formation (yes/no) | 27/177 |
| Differentiation (well/poor) | 81/123 |
| Surgical bleeding, mL | 300 (180-575) |
| Blood transfusion (yes/no) | 68/136 |
| Type of liver resection (minor/major) | 159/45 |
| Intraoperative radiotherapy and/or chemotherapy (yes/no) | 148/56 |
| ALBI grade (1/2/3) | 136/66/2 |
| MCP grade (1/2/3) | 110/52/42 |
| Overall survival time, mo | 44.0 (22.0-74.0) |
| Recurrence-free survival time, mo | 22.0 (5.0-45.0) |
BMI: Body mass index; PH: Portal hypertension; C-P: Child-Pugh; BCLC: Barcelona Clinic Liver Cancer; PVTT: Portal vein tumor thrombus; MCP: Modified Child-Pugh; ALBI: Albumin-bilirubin. Type of liver resection: Minor, ≤ 3 liver segments; major, ≥ 4 liver segments. Intraoperative radiotherapy: Implanted with radiation particles I125 or I131. Intraoperative chemotherapy: Implanted with a chemotherapy pump.
Comparison of the characteristics of three groups in ALBI grade and MCP grade
Statistically significant differences between the three groups in each grade were found for the following variables: In the MCP grade groups for gender (P = 0.038), BMI (P = 0.008), ALT (P = 0.026), C-P grade (P < 0.001), BCLC (P = 0.01), blood transfusion (P = 0.045), and surgical bleeding (P = 0.019), in addition to PA, albumin, total bilirubin, and prothrombin time (P < 0.001) that are included in this grade; in the ALBI grade groups for INR (P = 0.012), C-P grade (P < 0.001), BCLC stage (P = 0.013), number of tumours (P = 0.008), tumour size (P = 0.049), blood transfusion (P = 0.006), and type of liver resection (P = 0.011), in addition to PA, albumin, total bilirubin, and prothrombin time (P < 0.001) that are the variables included in this grade (Supplementary Table 1).
Prognostic factors for OS and RFS
The median OS time and RFS time of the whole cohort were 44.0 mo (range: 22.0-74.0 mo) and 22.0 mo (range: 5.0-45.0 mo), respectively. In order to identify the potential prognostic indicators for the OS and RFS, we included the variables in the univariate analysis with P < 0.05 into the multivariable cox regression analysis (Table 3). As demonstrated by univariate analyses, age, INR, tumor size, surgical bleeding, blood transfusion, hepatectomy type, PVTT, differentiation, C-P grade, BCLC stage, ALBI grade, and MCP grade were significant indicators for OS; except for the indicator of age, the other factors mentioned above were significant indicators for RFS, but liver cirrhosis was not the predictor of OS or RFS. Next, a multivariable regression analysis was conducted to further define the significant independent predictors. As shown in Table 3, age [P = 0.002, hazard ratio (HR) = 1.853], differentiation (P < 0.001, HR = 2.230), BCLC stage B (P = 0.012, HR = 2.635), and MCP grade 2 (P = 0.008, HR = 1.864) or 3 (P = 0.030, HR = 2.005) were the independent predictors of OS. For RFS, surgical bleeding (P = 0.027, HR = 2.246), BCLC stage B (P = 0.012, HR = 2.635), and MCP grade 2 (P = 0.002, HR = 1.830) were the independent predictors.
Table 3.
Univariate and multivariate analyses of prognostic factors for overall survival and recurrence-free survival
| Variables |
Overall survival |
Recurrence-free survival |
||||
|
Univariate |
Multivariate |
Univariate |
Multivariate |
|||
| P value | HR (95%CI) | P value | P value | HR (95%CI) | P value | |
| Sex (M/F) | 0.595 | 0.962 | ||||
| Age (> 50/< 50 yr) | 0.020 | 1.853 (1.243-2.761) | 0.002 | 0.071 | ||
| BMI (≥ 24/<24 kg/m2) | 0.596 | 0.770 | ||||
| Cause of hepatitis (HBV/HCV/others) | 0.269 | 0.422 | ||||
| ALT (> 40/≤ 40 U/L) | 0.255 | 0.069 | ||||
| AFP (≥ 400/< 400 μg/L) | 0.111 | 0.092 | ||||
| INR (≥ 1.3/< 1.3) | < 0.001 | 0.009 | ||||
| PLT (≥ 100/< 100 × 109/L) | 0.392 | 0.713 | ||||
| Number of tumors (single/≥ 2) | 0.243 | 0.065 | ||||
| Tumor size (≥ 5/< 5 cm) | < 0.001 | < 0.001 | ||||
| Blood transfusion (yes/no) | 0.001 | 0.003 | ||||
| Surgical bleeding (> 400/≤ 400 mL) | 0.005 | 0.003 | 1.437 (1.004-2.058) | 0.048 | ||
| Types of liver resection (minor/major) | < 0.001 | < 0.001 | ||||
| Intraoperative radiotherapy and/or chemotherapy (yes/no) | 0.649 | 0.430 | ||||
| PVTT (yes/no) | < 0.001 | 0.005 | ||||
| Capsule formation (yes/no) | 0.408 | 0.374 | ||||
| Differentiation (good/poor) | 0.004 | 2.230 (1.452-3.426) | < 0.001 | 0.029 | ||
| PH (yes/no) | 0.809 | 0.542 | ||||
| Liver cirrhosis (yes/no) | 0.944 | 0.896 | ||||
| Child-Pugh grade (A/B) | < 0.001 | 0.001 | ||||
| BCLC stage (0 or A/B/C) | < 0.001 | < 0.001 | ||||
| 0 or A | 1 | 1 | ||||
| B | 2.635 (1.235-5.622) | 0.012 | 2.246 (1.095-4.607) | 0.027 | ||
| ALBI grade (1/2/3) | < 0.001 | 0.003 | ||||
| MCP grade | < 0.001 | < 0.001 | ||||
| 1 | 1 | 1 | ||||
| 2 | 1.864 (1.174-2.959) | 0.008 | 1.830 (1.246-2.687) | 0.002 | ||
| 3 | 2.005 (1.071-3.753) | 0.030 | ||||
BMI: Body mass index; PH: Portal hypertension; C-P: Child-Pugh; BCLC: Barcelona Clinic Liver Cancer; PVTT: Portal vein tumor thrombus; ALBI: Albumin-Bilirubin; MCP: Modified Child-Pugh. Type of liver resection: Minor, ≤ 3 liver segments; major, ≥ 4 liver segments. Intraoperative radiotherapy: Implanted with radiation particles I125 or I131. Intraoperative chemotherapy: Implanted with a chemotherapy pump.
Discriminatory power of MCP grade and ALBI grade for OS and RFS
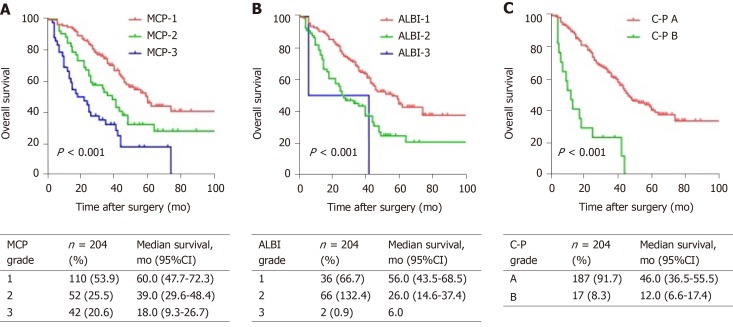
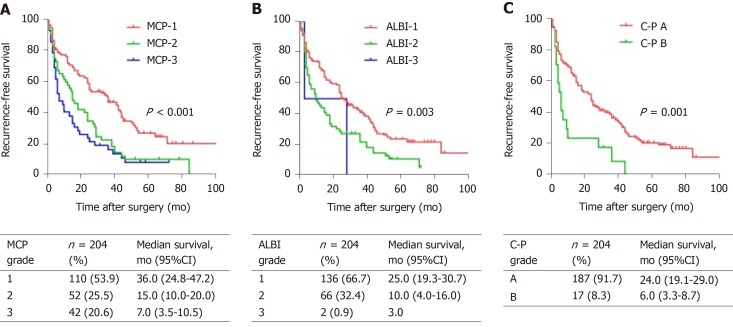
The Kaplan-Meier curves of the OS and RFS showed a significant discrimination between the patients in different C-P, MCP, and ALBI grades (P < 0.05) (Figure 1). Visual observation of the OS curves indicated that compared with the C-P score, the MCP and ALBI scores had more significant differences in various groups, and the difference in MCP grade displayed a superior over ALBI grade. The median OS times of grades 1, 2, and 3 patients were 60.0, 39.0, and 18.0 mo, and those of ALBI grades 1, 2, and 3 patients were 56.0, 26.0, and 6.0 mo, respectively. Similarly, MCP also demonstrated a greater advantage for predicting RFS than C-P grade and ALBI grade (Figure 2). The median RFS times of MCP grades 1, 2, and 3 patients were 36.0, 15.0, and 7.0 mo, respectively, and those of ALBI grades 1, 2, and 3 patients were 25.0, 10.0, and 3.0 mo, respectively.
Figure 1.
Kaplan-Meier curves of the overall survival of the 204 hepatocellular carcinoma patients who underwent hepatectomy in the present study. A: Stratified by MCP grade; B: Stratified by ALBI grade; C: Stratified by C-P grade. OS was significantly different among the subgroups stratified by these variables (P < 0.05). Associated tables display the median survival for each grade. MCP: Modified Child-Pugh; ALBI: Albumin-bilirubin; C-P: Child-Pugh; CI: Confidence interval.
Figure 2.
Kaplan-Meier curves for the recurrence-free survival of the 204 hepatocellular carcinoma patients who underwent hepatectomy in the present study. A: Stratified by MCP grade; B: Stratified by ALBI grade; C: Stratified by C-P grade. RFS was significantly different among the subgroups stratified by these variables (P < 0.05). Associated tables display the median survival for each grade. MCP: Modified Child-Pugh; ALBI: Albumin-bilirubin; C-P: Child-Pugh; CI: Confidence interval.
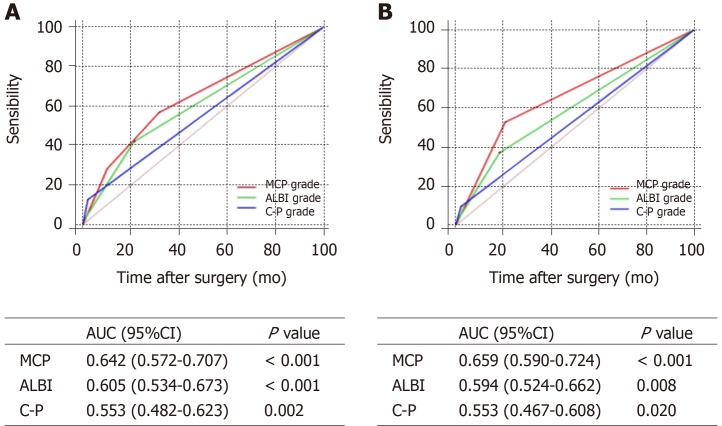
The analyses of the ROC curves found that both the MCP and ALBI grades had greater ability to predict the OS and RFS times compared with the C-P grade (Figure 3). For the OS (Figure 3A), the AUC of the MCP grade was 0.642 (95%CI: 0.572-0.707), which was larger than that of the ALBI grade (AUC = 0.605; 95%CI: 0.534-0.673), although the difference was not statistically significant (P = 0.263). For the RFS (Figure 3B), we observed the same advantages; the AUC was 0.659 (95%CI: 0.590-0.724) for the MCP grade, and 0.594 (95%CI: 0.524-0.662) for the ALBI grade, and the difference was statistically significant (P = 0.038). The differences of the AUCs between the two grades seemed not obvious and the discriminatory power may be a little weak, but regardless of the OS or RFS, the MCP grade displayed a slight advantage over the ALBI grade.
Figure 3.
Comparisons of the area under curve for overall survival and recurrence-free survival predictions among the MCP, ALBI, and C-P grades using receiver operating characteristics curves. A: Overall survival; B: Recurrence-free survival. MCP: Modified Child-Pugh grade; ALBI: Albumin-bilirubin grade; C-P: Child-Pugh grade; AUC: Area under the curve; CI: Confidence interval.
DISCUSSION
The long-term outcome of liver cancer patients is closely related to liver function[5,6]. The estimation of liver function reserve is key for HCC patients before hepatic resection. The C-P grade is widely used to estimate liver function[7,8]. Compared with the C-P grade, the MCP and ALBI grades are more objective, simpler, and easier to obtain[19,20]. Based on the same advantages of the two scoring systems mentioned above, and the little data on the MCP grade, we conducted this study to analyse and compare the predictive power of the MCP score and ALBI score for the long-term outcome of HCC patients and to provide clinicians with a more objective, simpler, and more discriminative scoring system.
This study demonstrated the advantages of the MCP and ALBI scores in the long-term outcome of HCC patients compared with the C-P score. As shown in Figure 3, both the visual inspection and formal statistical analyses demonstrated that the MCP grade had better discrimination in assessing the OS and RFS of HCC patients than the ALBI grade. This study found several strengths of the MCP grading systems compared to the ALBI grading systems. First, PA was included in the MCP classification. Huang et al[7] demonstrated a close correlation between PA and liver function in HCC patients undergoing hepatectomy, while Jia et al[16] proposed that PA can help predict the long-term prognosis of patients after hepatectomy. As Wen et al[19] reported, the integration of PA into the C-P grading system to form the MCP grading systems can improve the accuracy of postoperative prognosis prediction in HCC patients, and our study is in agreement with this result. Second, the univariate analysis displayed that both the ALBI grade and MCP grade were the predictors of OS or RFS, but the further multivariable regression analysis showed that the independent predictor was MCP grade. Third, the Kaplan-Meier curves showed that the MCP grade had a preferable prognostic discrimination ability (Figures 1 and 2). The median survival time predicted with the MCP grading system was much longer than that with the ALBI grading system, and the median survival time in the same grade could even differ by more than 10 mo (such as grade 2: 39.0 mo vs 26.0 mo for OS; grade 1: 36 mo vs 25 mo for RFS). Fourth, the MCP grading system had a more favorable patient distribution compared to the ALBI grading system, whose weight tended to be grade 1 (66.7%), and there were only two patients in grade 3. This might have been related to the fact that the liver function of the HCC patients with ALBI grade 3 was too poor to treat by surgery. But the distribution of MCP grades was relatively uniform. The proportions of MCP grades 1, 2, and 3 patients were 53.9%, 25.5%, and 20.6%, respectively. Finally, the ROC curve of the MCP grade had higher accuracy than the ALBI grade, and the AUC of the MCP grade was larger than the ALBI grade, which further validated that the MCP grade had a better predictive value for the long-term prognosis of HCC patients than the ALBI grade.
There are several limitations to this study. First, the total number of patients was small and all were from one single centre; therefore, larger and multicentre studies are needed to further validate the results. Second, as a retrospective study, it was hard to avoid selection bias. Further prospective studies on the MCP grading system are necessary.
In conclusion, the current study suggests that the MCP grade is more advantageous than the ALBI grade for predicting postoperative long-term outcomes in patients with HCC, and the MCP grade could be conducive to the selection of HCC treatment strategies. This may benefit more HCC patients.
ARTICLE HIGHLIGHTS
Research background
Liver resection is the main treatment for hepatocellular carcinoma (HCC) patients and it has a high possibility for long-term cure potential. But the postoperative mortality and recurrence rates remain high. Since the long-term prognosis of HCC patients is strongly linked to liver function, preoperative assessment of liver function is very important.
Research motivation
The main aim of this study was to compare the predictive power of the modified Child-Pugh (MCP) and albumin-bilirubin (ALBI) grades for the long-term outcome of HCC.
Research objectives
We can provide a more effective, objective, and simple method to assess the prognosis of HCC patients undergoing hepatectomy and makes it easier and more accurate for surgeons to select suitable HCC patients for hepatectomy.
Research methods
A total of 204 patients with HCC who underwent surgery were enrolled in this retrospective study, the median follow-up time was 36 mo. Multivariate Cox regression analysis was used to determine the independent predictive factors for survival and relapse. The area under the curve was used to evaluate the discriminative performance of the MCP grade and ALBI grade to predict the postoperative overall survival (OS) time and recurrence-free survival (RFS) time.
Research results
Both the MCP and ALBI grades were more accurate than the Child-Pugh grade for predicting long-term prognosis. And further analysis demonstrated that for both predicting OS and RFS, the MCP grade performed better than the ALBI grade. This can provide a more effective, objective, and simple tool for the selection of HCC treatment strategies.
Research conclusions
We found that the new grading system, MCP grade, had predictive value for the long-term prognosis of HCC patients after hepatectomy. Both the MCP and ALBI scoring systems are objective, simple, and discriminative, and the ALBI grade has been widely proven in the international environment for predicting the long-term prognosis of HCC patients. We hypothesized that the MCP grade is superior to the ALBI grade in predicting the prognosis of HCC patients. In this study, we adopted the traditional method to prove the hypothesis, and we found a new phenomenon in which there was no patient in Child-Pugh grade C, and there were few patients in ALBI grade 3, but the patient distribution of MCP grade was relatively uniform. And eventually through the patient distribution, Kaplan-Meier curves and ROC curves of the MCP and ALBI grades and so on, we confirmed the hypothesis that the MCP grade is superior to the ALBI. But in this study, the sample size is not very large, the patients were from one clinical center, and it is a retrospective study, so in the future, we can further confirm the value of MCP in predicting the prognosis of HCC patients through larger samples, multi-center studies and prospective studies. When evaluating liver function of HCC patients before surgery, we should pay more attention to the serum PA levels of patients, and we can choose the MCP grade to assess the prognosis of patients.
Research perspectives
Larger samples, multi-center studies and prospective studies are needed to further validate the value of the MCP grade for the long-term prognosis of HCC patients. And how to improve the liver function of the HCC patients with a higher MCP grade to further improve the prognosis of HCC patients after surgery remains a question that needs to be answered in future studies.
ACKNOWLEDGEMENTS
We would like to thank Mr. Xiao-Peng Hu and Miss Jing Lei for their help in the preparation of this manuscript.
Footnotes
Institutional review board statement: The study was reviewed and approved by the ethics committee of the Second Affiliated Hospital of Chongqing Medical University (No. 2018-025).
Informed consent statement: All study participants gave their informed consent prior to study enrollment (by written or verbal).
Conflict-of-interest statement: None declared.
Manuscript source: Unsolicited Manuscript
Peer-review started: November 28, 2019
First decision: December 28, 2019
Article in press: January 11, 2020
Specialty type: Gastroenterology and hepatology
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Zhang KQ, Tzamaloukas AHH, Dogrul ABB S-Editor: Wang YQ L-Editor: Wang TQ E-Editor: Li X
Contributor Information
Feng Huang, Second Clinical College, Chongqing Medical University, Chongqing 400010, China.
Jian Gao, Department of Gastroenterology, Second Affiliated Hospital, Chongqing Medical University, Chongqing 400010, China. 982213482@qq.com.
References
- 1.Forner A, Reig M, Bruix J. Hepatocellular carcinoma. Lancet. 2018;391:1301–1314. doi: 10.1016/S0140-6736(18)30010-2. [DOI] [PubMed] [Google Scholar]
- 2.European Association for the Study of the Liver. Electronic address: easloffice@easloffice.eu. European Association for the Study of the Liver. EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma. J Hepatol. 2018;69:182–236. doi: 10.1016/j.jhep.2018.03.019. [DOI] [PubMed] [Google Scholar]
- 3.Bruix J, Sherman M American Association for the Study of Liver Diseases. Management of hepatocellular carcinoma: an update. Hepatology. 2011;53:1020–1022. doi: 10.1002/hep.24199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.European Association For The Study Of The Liver. European Organisation For Research And Treatment Of Cancer. EASL-EORTC clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol. 2012;56:908–943. doi: 10.1016/j.jhep.2011.12.001. [DOI] [PubMed] [Google Scholar]
- 5.op den Winkel M, Nagel D, Sappl J, op den Winkel P, Lamerz R, Zech CJ, Straub G, Nickel T, Rentsch M, Stieber P, Göke B, Kolligs FT. Prognosis of patients with hepatocellular carcinoma. Validation and ranking of established staging-systems in a large western HCC-cohort. PLoS One. 2012;7:e45066. doi: 10.1371/journal.pone.0045066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Llovet JM, Brú C, Bruix J. Prognosis of hepatocellular carcinoma: the BCLC staging classification. Semin Liver Dis. 1999;19:329–338. doi: 10.1055/s-2007-1007122. [DOI] [PubMed] [Google Scholar]
- 7.Huang L, Li J, Yan JJ, Liu CF, Wu MC, Yan YQ. Prealbumin is predictive for postoperative liver insufficiency in patients undergoing liver resection. World J Gastroenterol. 2012;18:7021–7025. doi: 10.3748/wjg.v18.i47.7021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Verslype C, Rosmorduc O, Rougier P ESMO Guidelines Working Group. Hepatocellular carcinoma: ESMO-ESDO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2012;23 Suppl 7:vii41–vii48. doi: 10.1093/annonc/mds225. [DOI] [PubMed] [Google Scholar]
- 9.Shetty K, Rybicki L, Carey WD. The Child-Pugh classification as a prognostic indicator for survival in primary sclerosing cholangitis. Hepatology. 1997;25:1049–1053. doi: 10.1002/hep.510250501. [DOI] [PubMed] [Google Scholar]
- 10.Christensen E. Prognostic models including the Child-Pugh, MELD and Mayo risk scores--where are we and where should we go? J Hepatol. 2004;41:344–350. doi: 10.1016/j.jhep.2004.06.005. [DOI] [PubMed] [Google Scholar]
- 11.Durand F, Valla D. Assessment of the prognosis of cirrhosis: Child-Pugh versus MELD. J Hepatol. 2005;42 Suppl:S100–S107. doi: 10.1016/j.jhep.2004.11.015. [DOI] [PubMed] [Google Scholar]
- 12.Na SK, Yim SY, Suh SJ, Jung YK, Kim JH, Seo YS, Yim HJ, Yeon JE, Byun KS, Um SH. ALBI versus Child-Pugh grading systems for liver function in patients with hepatocellular carcinoma. J Surg Oncol. 2018;117:912–921. doi: 10.1002/jso.24992. [DOI] [PubMed] [Google Scholar]
- 13.Johnson PJ, Berhane S, Kagebayashi C, Satomura S, Teng M, Reeves HL, O'Beirne J, Fox R, Skowronska A, Palmer D, Yeo W, Mo F, Lai P, Iñarrairaegui M, Chan SL, Sangro B, Miksad R, Tada T, Kumada T, Toyoda H. Assessment of liver function in patients with hepatocellular carcinoma: a new evidence-based approach-the ALBI grade. J Clin Oncol. 2015;33:550–558. doi: 10.1200/JCO.2014.57.9151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Amisaki M, Uchinaka E, Morimoto M, Tokuyasu N, Sakamoto T, Honjo S, Saito H, Fujiwara Y. Post-operative albumin-bilirubin grade predicts long-term outcomes among Child-Pugh grade A patients with hepatocellular carcinoma after curative resection. Hepatobiliary Pancreat Dis Int. 2018;17:502–509. doi: 10.1016/j.hbpd.2018.07.011. [DOI] [PubMed] [Google Scholar]
- 15.Shenkin A. Serum prealbumin: Is it a marker of nutritional status or of risk of malnutrition? Clin Chem. 2006;52:2177–2179. doi: 10.1373/clinchem.2006.077412. [DOI] [PubMed] [Google Scholar]
- 16.Jia RR, Zhong JH, Huo RR, Su QB, Xiang X, Zhao FL, Qin ZB, Chen JH, Liao YY, Ma L, Xiang BD, Zhang CY, Li LQ. Correlation between serum prealbumin and prognosis of patients with hepatocellular carcinoma after hepatectomy. J Surg Oncol. 2019;119:794–800. doi: 10.1002/jso.25378. [DOI] [PubMed] [Google Scholar]
- 17.Li JD, Xu XF, Han J, Wu H, Xing H, Li C, Yu JJ, Zhou YH, Gu WM, Wang H, Chen TH, Zeng YY, Lau WY, Wu MC, Shen F, Yang T. Preoperative prealbumin level as an independent predictor of long-term prognosis after liver resection for hepatocellular carcinoma: a multi-institutional study. HPB (Oxford) 2019;21:157–166. doi: 10.1016/j.hpb.2018.06.1803. [DOI] [PubMed] [Google Scholar]
- 18.Liao YY, Teng CL, Peng NF, Jia RR, Cui J, Chen K, Ma L, Xiang BD, Zhong JH, Li LQ. Serum Prealbumin is Negatively Associated with Survival in Hepatocellular Carcinoma Patients after Hepatic Resection. J Cancer. 2019;10:3006–3011. doi: 10.7150/jca.30903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wen X, Yao M, Lu Y, Chen J, Zhou J, Chen X, Zhang Y, Lu W, Qian X, Zhao J, Zhang L, Ding S, Lu F. Integration of Prealbumin into Child-Pugh Classification Improves Prognosis Predicting Accuracy in HCC Patients Considering Curative Surgery. J Clin Transl Hepatol. 2018;6:377–384. doi: 10.14218/JCTH.2018.00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pinato DJ, Sharma R, Allara E, Yen C, Arizumi T, Kubota K, Bettinger D, Jang JW, Smirne C, Kim YW, Kudo M, Howell J, Ramaswami R, Burlone ME, Guerra V, Thimme R, Ishizuka M, Stebbing J, Pirisi M, Carr BI. The ALBI grade provides objective hepatic reserve estimation across each BCLC stage of hepatocellular carcinoma. J Hepatol. 2017;66:338–346. doi: 10.1016/j.jhep.2016.09.008. [DOI] [PubMed] [Google Scholar]