Abstract
Traditionally congenital muscular torticollis is treated with a neck incision which results in a neck scar. The purpose of this study was to evaluate the effectiveness of the transaxillary subcutaneous endoscopic sternocleidomastoid muscle division for the treatment of congenital muscular torticollis. This is a prospective study of 7 children with torticollis treated surgically by the transaxillary endoscopic approach in the department of Pediatric Surgery between 2014 and 2018. The age at operation ranged from 5.5 to 9 years, mean 7.3 (SD ± 1.3) years. The mean operation time was 65 min. The complete muscular release was successfully completed using the endoscopic approach. There were no major complications. All patients improved in gaze angle, lateral tilt and range of motion. There was no cosmetically unacceptable scar visible at the surgical sites in all patients during follow up. All families were pleased with the cosmetic outcome. The transaxillary subcutaneous endoscopic technique can be applied as a surgical approach for children with muscular torticollis an alternative to traditional open methods. It is a technically feasible procedure in children, provides excellent cosmesis and moreover avoids scarring on the neck.
Keywords: Congenital muscular torticollis, Surgical treatment, Stealth surgery, Subcutaneous endoscopic technique
Introduction
Congenital muscular torticollis (CMT) is a postural deformity of head and neck principally resulting from a unilateral shortening of sternocleidomastoid (SCM) muscle identified at birth or within few weeks thereafter. The incidence of CMT is 0.3–1.9% [1]. It is the third most common musculoskeletal anomaly after dislocation of the hip and clubfoot [2].
In long standing or delayed management, secondary contractures occur in the platysma, neck muscles, and deep fasciae of the neck. This results in an ocular gaze tilt, alteration in facial symmetry and significant permanent craniofacial deformities [3, 4]. These patients suffer both functional and cosmetic problems [5]. Early diagnosis and physical therapy is the key to successful treatment. Surgical treatment is implemented in cases who failed to improve after conservative measures. Conventionally it is treated by open surgical technique. Even though the incisions are placed in skin creases to prevent unpleasant scars, it is something that cannot be predicted and the results may be unattractive to the patient and the family. Subcutaneous endoscopic techniques necessitate performing laparoscopic subcutaneous division of sternal and clavicular head of the sternocleidomastoid muscle. This approach replaces the larger incisions on the neck to smaller incisions and placing them in inconspicuous areas [6, 7]. We present a subcutaneous endoscopic surgery to treat torticollis in children.
Methods
Seven children with CMT were prospectively studied between the years 2014 and 2018 in the Pediatric surgery unit. The children older than five years with muscle contracture as the cause of their torticollis were included in this study. The indications for surgery were a persistent head tilt, deficits of passive rotation of the neck > 15°, and lateral bending of the neck. All the patients had failed to improve by various methods of conservative management. The children with underlying ocular, neurological, and skeletal pathology causing neck deformity were excluded from the study. Patients who had undergone neck surgery previously were also excluded. Preoperative assessment included the age and gender of the child, any history of swelling in the neck in infancy and the side of involvement. The degree of neck tilt and range of motion of the neck were recorded. Plain radiographs of the cervical spine were taken to exclude congenital bony deformities and atlanto-axial pathology. A horizontal gaze angle of 90° was recorded as normal. The angle between the gaze line and 90° is taken as gaze angle. The deviation of the chin from the midsternal plumb line was documented as a measure of translation deformity (normal = 0 mm) (Fig. 1).
Fig. 1.

Clinical photograph of 5.8-years-old girl, with left side, torticollis showing measurement for gaze angle and translational deformity measurements. Line A: axis through the outer canthus of both eyes. Line B: vertical line through the tip of the chin Line C: vertical plumb line through the midsternal point. The angle between Line A and C is a measure of gaze angle in degrees. The horizontal deviation of chin (Line B) from the plumb line (Line C) denotes an amount of translational deformity
Surgical Technique
All procedures were performed under general anesthesia and endotracheal intubation. The patients were positioned supine with the neck hyperextended with a shoulder roll in place. The ipsilateral arm is abducted to 90°. The sternal notch, the sternocleidomastoid muscle, and the clavicle were identified and marked on the overlying skin as landmarks. A 5-mm incision was made in the ipsilateral anterior axilla parallel to the lateral border of the pectoralis major muscle. The initial subcutaneous plane is made with an artery forcep which was carried over the top of the pectoralis fascia. A veress needle was introduced, and the subcutaneous space was insufflated with CO2, and a 5-mm 30° telescope was inserted. The place is carefully expanded to form cavernous subcutaneous space. An additional two 3-mm ports were placed at 1 inch on either side of the first port at the lateral border of the pectoralis major muscle. With a 3-mm monopolar hook cautery and maryland dissector the sternal and clavicular end of the muscle was divided (Fig. 2).All the gas was squeezed out of the subcutaneous space, and a tight compression dressing was kept for two to three days.
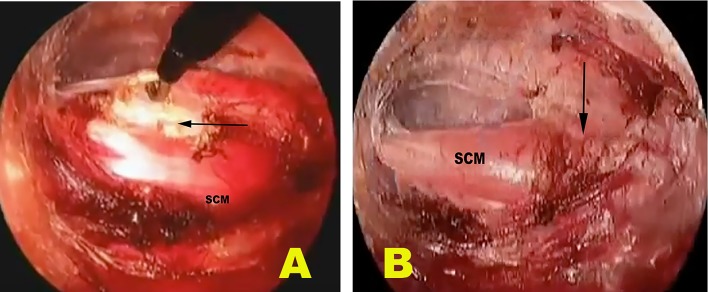
Fig. 2.
Showing the endoscopic view during operation. (A) in process (B) after complete division of the sternal and clavicular heads of sternocleidomastoid muscle
In the postoperative period, an active and passive physiotherapy program was initiated after one week. Immobilization with a torticollis brace was applied for three months. The children were assessed at 1, 3 and 6 months’ and followed up yearly. The child was assessed for wound healing, passive range of motion of the neck, lateral tilt, gaze angle, and lateral column of the neck. The results were graded as excellent, good, and poor based on subjective and objective criteria.
Statistical Analysis
The data of the present study were recorded into the computers and after its proper validation, check for error, coding & decoding were compiled and analyzed using the software SPSS 20 for windows. Appropriate univariate and bivariate analysis was carried out using the Student t- test for the continuous variable and Chi square (χ2) test for categorical variables or Fischer’s exact test. All means are expressed as the mean ± standard deviation for continuous data, while qualitative information is expressed in proportion with a percentage. The critical levels of significance of the results were considered at 0.05 levels i.e. P < 0.05 was considered significant.
Results
A total of 7 cases of congenital muscular torticollis met the inclusion criteria during the study period. Four were females. The age at operation ranged from 5.5 to 9 years, mean 7.3 (SD ± 1.3) years. The right side was involved in 5 patients. The demographic characteristic of the cohort is shown in (Table 1). All procedures were completed successfully using the endoscopic method. There were no conversions to open surgery. The mean operation time was 65 min (range 45–90 min). Blood loss ranged from 5 to 10 ml. The hospital stay was 24 h. There were no intraoperative complications, ecchymosis or subcutaneous emphysema. The mean follow-up time was 36.6 months. Complete muscular release as determined by pre-operative and postoperative range of motion measurements was achieved in all of the patients. Preoperative and postoperative gaze angle, rotational and translational defects are shown in Table 2. Cosmetic improvement in the form of a reduction in head tilt and chin deviation was present in all patients (Fig. 3). Post-operative head tilt was fully corrected in six patients, while one had mild residual tilt. There was no infection, hematoma, or loss of neck contour. No injuries to major blood vessels or nerves were encountered. All incisions healed without scar hypertrophy. All of the patients were pleased with the result. There was no cosmetically unacceptable scar visible at the surgical sites in seven patients during follow up. There was no recurrence of deformity requiring any further surgery.
Table 1.
Showing the demographic characteristics of the cohort
| Number of patients | 7 |
| Age at surgery (mean ± SD) years | 7.3 ± 1.3 |
| Gender (M/F) | 3/4 |
| Side (R/L) | 5/2 |
| Number of patients available for follow up | 7 |
| Follow up period (Mean ± SD) months | 36.6 ± 15.7 |
Table 2.
Showing comparative analysis of parameters before and after operation
| Clinical parameters | Preoperative | Postoperative |
|---|---|---|
| Rotational deficit (mean ± SD) degrees | 19.5 ± 7.9 | 5.7 ± 0.7 (p < 0.001) |
| Gaze angle (mean ± SD) degrees | 73.4 ± 5.9 | 89 ± 1.3 |
| Translational deformity (Mean ± SD) mm | 21.7 ± 5.6 | 1.7 ± 2.4 |
| Neck muscle band | All | 1 |
| Scar (inconspicuous) | All |
Fig. 3.
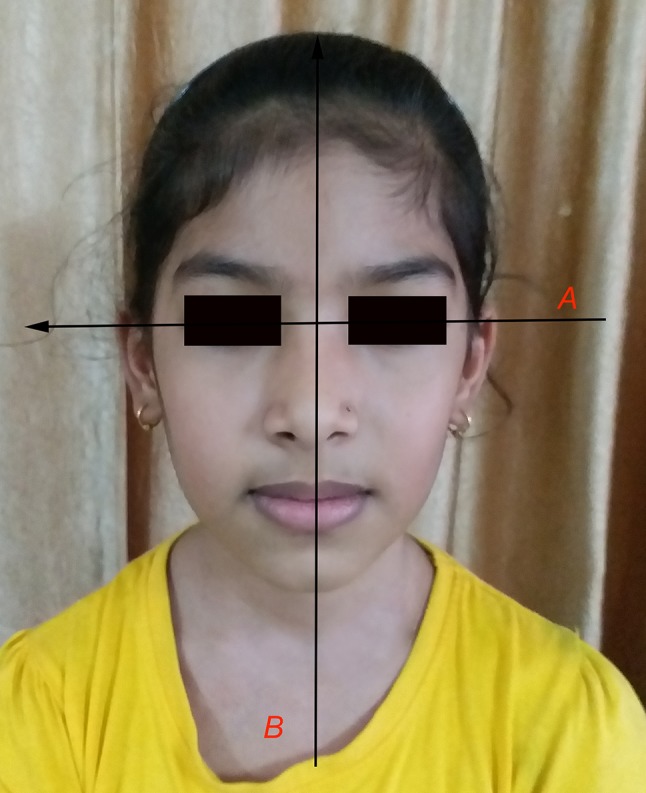
Complete correction of translational deformity to 0 mm and gaze angle to horizontal 90° at follow up
Discussion
The factors attributed in the etiology are an abnormal intrauterine position of the fetus and bleeding in sternocleidomastoid muscle due to birth trauma and subsequent hematoma and fibrosis [8]. It presents as a tight SCM muscle, limited neck motion, head tilt, and ipsilateral facial asymmetry. Untreated cases develop severe disfiguration due to mandibular hypoplasia, facial hemi hypoplasia and skeletal deformity of the face. Most cases of CMT resolve completely either spontaneously or with conservative measures. A schedule of stretching exercises in children before 1 year of age is the initial form of treatment with positive outcomes over 90% is seen [9]. Botulinum toxin A has been recommended in refractory cases to aid correction by physiotherapy. Surgical release of the sternocleidomastoid muscle is recommended for patients who fail to respond to physiotherapy. The optimum period for surgical therapy is 1–4 years of age to achieve the best result [10]. Conventionally, contracture release of congenital muscular torticollis has been done in an open manner. Surgical procedures include unipolar release, bipolar release, release with Z-plasty, partial or complete muscle resection. Burnstein and Cohen described an endoscopic approach to the division of the SCM using a retroauricular endoscopic access point [11]. This approach, however, places the spinal accessory and greater auricular nerves at risk for injury [11]. Dutta and Tang et al. reported their technique of transaxillary subcutaneous endoscopic release of the sternocleidomastoid muscle for treatment of CMT [12, 13].
Surgical scars of the face and the neck can have a lifelong impact on the self-esteem and socialisation of patients [12]. Scarring can cause significant inconvenience, especially in patients prone to hypertrophic scar and keloid formation. Contemplating this, all measures are to be taken to avoid scar formation. The customary open operation causes a permanent scar in the neck, which did not fulfill the high esthetic needs of patients with CMT [14].
Transaxillary subcutaneous endoscopic surgery transfers the scarring associated with neck surgery to the axilla, which is inconspicuous and easily hidden [12]. There are no major neural and vascular structures during the tunneling in a transaxillary approach for torticollis. Care should be taken while tunneling to make sure the plain is above the pectoralis fascia and not to traverse through the platysma [7]. Advantage of endoscopic surgery was improved visualization and exposure, and the use of 3-mm instruments provided excellent maneuverability in the restricted space. However, this technique has a learning curve, longer operative times during the initial period and need for specialised instrumentation and resources [15].Once the surgeon has passed the learning curve, the operative time gradually reduces. In this study we have taken three precautions (1) good cavernous space was created to enhance the space for the movement of the instruments (2) meticulous diathermy to prevent hematoma formation (3) and the use of the cold light source to prevent skin bums.
In our series, no serious complications had occurred, so we accept that this surgical method is clinically achievable and productive. The improved cosmesis and patient satisfaction, at last adjust the marginally increased expense. At follow-up, 85.7% of the patients rated as either good or excellent. The limitations of our study were the absence of a control group of patients treated by other surgical methods. Therefore, we can’t ensure that this surgical approach offers fewer complications and better outcomes than an open technique. In the future, randomized controlled trials to compare conservative treatment and different surgical methods will be needed to determine which treatment providesbetter results, the lower morbidity, and higher patient satisfaction.
Conclusion
The transaxillary subcutaneous endoscopic approach has the advantage of improved visualization, greater precision of dissection, and neck scarring is absent with small scars in the axillary folds. Given the safety and efficacy seen with the 7 cases we studied, this technique has remarkable promise. However, a larger series should be studied before definite general recommendations can be given.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Cheng JC, Wong MW, Tang SP, Chen TM, Shum SL, Wong EM. Clinical determinants of the outcome of manual stretching in the treatment of congenital muscular torticollis in infants. A prospective study of eight hundred and twenty-one cases. J Bone Joint Surg Am. 2001;83:679–687. doi: 10.2106/00004623-200105000-00006. [DOI] [PubMed] [Google Scholar]
- 2.Bredenkamp JK, Hoover LA, Berke GS, Shaw A. Congenital muscular torticollis. A spectrum of disease. Arch Otolaryngol Head Neck Surg. 1990;116(2):212–216. doi: 10.1001/archotol.1990.01870020088024. [DOI] [PubMed] [Google Scholar]
- 3.Hollier L, Kim J, Grayson BH, McCarthy JG. Congenital muscular torticollis and the associated craniofacial changes. Plast Reconstr Surg. 2000;105:827–835. doi: 10.1097/00006534-200003000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Bhaskar A, Harish U, Desai H. Congenital muscular torticollis: use of gaze angle and translational deformity in assessment of facial asymmetry. Indian J Orthop. 2017;51(2):123–130. doi: 10.4103/ortho.IJOrtho_114_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cheng JCY, Tang SP, Chen TMK. The clinical presentation and outcome of treatment of congenital muscular torticollis in infants. A study of 1,086 cases. J Pediatr Surg. 2000;35:1091–1096. doi: 10.1053/jpsu.2000.7833. [DOI] [PubMed] [Google Scholar]
- 6.Pricola KL, Dutta S. Stealth surgery: subcutaneous endoscopic excision of benign lesions of the trunk and lower extremity. J Pediatric Surg. 2010;45:840–844. doi: 10.1016/j.jpedsurg.2009.12.016. [DOI] [PubMed] [Google Scholar]
- 7.Teja VS, Agarwal P, Bagdi RK. Stealth surgery: subcutaneous endoscopic excision of benign lesions of head, neck and trunk in children. J Minim Access Surg. 2017;13(2):109–112. doi: 10.4103/0972-9941.201729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Demirbilek S, Atayurt HF. Congenital muscular torticollis and sternomastoid tumor: results of nonoperative treatment. J Pediatr Surg. 1999;34:549–551. doi: 10.1016/S0022-3468(99)90070-2. [DOI] [PubMed] [Google Scholar]
- 9.Seyhan N, Jasharllari L, Keskin M, Savacı N. Efficacy of bipolar release in neglected congenital muscular torticollis patients. Musculo Skelet Surg. 2012;96:55–57. doi: 10.1007/s12306-011-0170-3. [DOI] [PubMed] [Google Scholar]
- 10.Canale ST, Griffin DW, Hubbard CN. Congenital muscular tortikollis: a long term follow up. J Bone Joint Surg Am. 1982;64:810–816. doi: 10.2106/00004623-198264060-00002. [DOI] [PubMed] [Google Scholar]
- 11.Burnstein FD, Cohen SR. Endoscopic surgical treatment for congenital muscular torticollis. Plast Reconstr Surg. 1998;101:20–24. doi: 10.1097/00006534-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 12.Dutta S, Albanese CT. Transaxillary subcutaneous endoscopic release of the sternocleidomastoid muscle for treatment of persistent torticollis. J Pediatr Surg. 2008;43:447–450. doi: 10.1016/j.jpedsurg.2007.10.008. [DOI] [PubMed] [Google Scholar]
- 13.Tang S, Yang Y, Mao YZ. Endoscopic transaxillary approach for congenital muscular torticollis. J Pediatr Surg. 2010;45:2191–2194. doi: 10.1016/j.jpedsurg.2010.06.027. [DOI] [PubMed] [Google Scholar]
- 14.Wang JL, Qi W, Liu Y. Endoscopic release of congenital muscular torticollis with radiofrequency in teenagers. J Orthop Surg Res. 2018;3:1–6. doi: 10.1186/s13018-018-0801-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hsiao A, Pimpalwar A. Subcutaneoscopic excision of external angular dermoid cysts: our covert scar approach in 11 cases. Eur J Pediatr Surg. 2019;29(03):239–242. doi: 10.1055/s-0038-1636942. [DOI] [PubMed] [Google Scholar]