Abstract
Background
Access to and utilisation of quality maternal and child healthcare services is generally recognized as the best way to reduce maternal and child mortality.
Objectives
We evaluated whether the introduction of a voluntary family health insurance programme, combined with quality improvement of healthcare facilities [The Community Health Plan (TCHP)], and the introduction of free access to delivery services in all public facilities [Free Maternity Services programme (FMS)] increased antenatal care utilisation and use of facility deliveries among pregnant women in rural Kenya.
Methods
TCHP was introduced in 2011, whilst the FMS programme was launched in 2013. To measure the impact of TCHP, percentage points (PP) changes in antenatal care utilisation and facility deliveries from the pre-TCHP to the post-TCHP period between the TCHP programme area and a control area were compared in multivariable difference-in-differences analysis. To measure the impact of the FMS programme, PP changes in antenatal care utilisation and facility deliveries from the pre-FMS to the post-FMS period in the pooled TCHP programme and control areas was assessed in multivariable logistic regression analysis. Data was collected through household surveys in 2011 and 2104. Households (n=549) were randomly selected from the member lists of 2 dairy companies, and all full-term pregnancies in the 3.5 years preceding the baseline and follow-up survey among women aged 15–49 at the time of pregnancy were eligible for this study (n=295).
Results
Because only 4.1% of eligible women were insured through TCHP during pregnancy, any increase in utilisation attributable to the TCHP programme could only have come about as a result of the quality improvements in TCHP facilities. Antenatal care utilisation significantly increased after TCHP was introduced (14.4 PP; 95% CI: 4.5–24.3; P=0.004), whereas no effect was observed of the programme on facility deliveries (8.8 PP; 95% CI: -14.1 to +31.7; P=0.450). Facility deliveries significantly increased after the introduction of the FMS programme (27.9 PP; 95% CI: 11.8–44.1; P=0.001), but antenatal care utilisation did not change significantly (4.0 PP; 95% CI: -0.6 to +8.5; P=0.088).
Conclusion
Access to the FMS programme increased facility deliveries substantially and may contribute to improved maternal and new-born health and survival if the quality of delivery services is sustained or further improved. Despite low up-take, TCHP had a positive effect on antenatal care utilisation among uninsured women by improving the quality of existing healthcare facilities. An alignment of the two programmes could potentially lead to optimal results.
Funding
The study was funded by the Health Insurance Fund (http://www.hifund.org/), through a grant from the Dutch Ministry of Foreign Affairs.
Keywords: Free Maternity Services programme, maternal and child healthcare utilisation rural, Kenya, a dairy farmer population-based study
Introduction
The maternal mortality ratio (MMR) in Kenya was estimated at 510 deaths per 100,000 live births and neonatal mortality was estimated at 22 deaths per 1,000 live births in 2015,1 whilst the Sustainable Development Goals targets for 2030 are 70 per 100,000 and 12 per 1,000, respectively. 2 Access to and utilisation of quality maternity and child health services is generally recognized as the best way to lower maternal and neonatal mortality.3,4,5
The Kenyan demographic health surveys from 2008–2009 and 2014 showed high antenatal care utilisation, with 92% and 96% of women receiving antenatal care from a skilled provider (doctor, nurse, or midwife), respectively. 6,7 About half of these women made the 4 visits recommended by the World Health Organization. However, even though facility delivery showed a large increase between 2008–2009 and 2014, still only 43% and 61% of women reported a facility delivery in these years, respectively. 6,7 Showing that that there is room for development and evaluation of novel interventions.
In 2011, Africa Air Rescue insurance Kenya, the Health Insurance Fund and Pharm Access Foundation introduced The Community Healthcare Plan (TCHP) to improve access to affordable and quality healthcare for dairy farmers and their families in rural Nandi North, Kenya. TCHP integrates the provision of private health insurance (demand side) with improvement of quality of care offered by healthcare facilities (supply side).
In 2013, Kenya's President Kenyatta signed the Health Bill 2013 that waived fees for maternity services in all public facilities under the name of Free Maternity Services (FMS) programme. This programme aimed to lower the national neonatal and maternal mortality rates.8
We evaluated whether the TCHP and FMS programmes increased antenatal care utilisation and facility deliveries among pregnant women in rural Nandi County, Kenya.
Methods
Study setting, study area, and the TCHP and FMS programmes
Nandi County is situated in the Western region of Kenya with a total population of 752,965 based on the 2009 National Population and Housing Census. The 2008–2009 Kenyan demographic health survey reported that in Nandi County, 91.5% of women made at least one antenatal care visit with a skilled provider, as opposed to no visits or visits with a community health worker or traditional birth attendant, and 42.6% of women delivered in a healthcare facility.6
On 1 April 2011, TCHP began providing health insurance to dairy farmer households of Tanykina Dairy Company, a cooperative of dairy farmers in Nandi North (TCHP programme area). In the 2 months before the insurance was introduced, the programme facilitated quality improvements in 7 participating healthcare facilities (3 public, 3 private, and 1 public referral hospital). Dairy farmer households of Lelbren Dairy Company in Nandi East were chosen as the TCHP control study group, as they were comparable to dairy farmer households in the TCHP programme area in terms of socio-demographic and socio-economic characteristics. Before the introduction of the programme, the healthcare facilities in both areas provided similar quality services.
Enrolment in the TCHP insurance scheme was voluntary and on a family basis. Covered maternity services included antenatal care, delivery including caesarean section, neonatal care, and pharmacy costs for prescribed medication. At the time of this study, the insurance premium was 300 Kenyan Shilling (KSh) for a basic package and 1,100 KSh for a comprehensive package per family per month, which corresponded to ∼0.9% and ∼3.3% of average monthly household consumption, respectively, among the surveyed households before the introduction of TCHP. The basic package gave access to out-patient primary and maternity care up to a referral level and the comprehensive package additionally gave access to inpatient care up to a referral level.
Quality and efficiency of healthcare were monitored through independent audits by an international quality improvement and assessment body called SafeCare9, a partnership between the Pharm Access Foundation, the American Joint Commission International and the Council for Health Services Accreditation of Southern Africa. Prior to participation in TCHP, SafeCare would conduct a baseline assessment of a healthcare facility and formulate a quality improvement plan, which subsequently was implemented by the facility. Examples of quality improvement interventions included implementation of treatment guidelines and protocols for waste management, and hospital infection control, training of staff in guideline-based care and adequate medical file keeping, hospital renovation, upgrading of laboratory equipment, and training of laboratory staff in basic laboratory testing, and assurance of continuous essential drug supplies. SafeCare monitored the progress on quality improvement through annual follow-up assessments collecting scores using the SafeCare Quality Standards.10,11
On 1 June 2013, the national FMS programme was introduced by the Kenyan government. After the launch of the FMS programme delivery care services, including caesarean delivery, were free of charge in all public healthcare facilities (delivery costs would be reimbursed by the government directly to providers). It was assumed that the facilities would cover the costs of antenatal care visits from their FMS budget such that it would be free of charge to all pregnant women, as well.
Additionally, women in the study area also had access to National Health Insurance Fund (NHIF) health insurance since 1966. At the time of this study, NHIF offered both in-patient and out-patient health insurance to all Kenyan citizens. The in-patient scheme was compulsory for formal sector workers and their family members and premiums were dependent on income, whereas for informal sector workers it was voluntary. The out-patient scheme was available for civil servants only. The inpatient scheme covered maternity services, comparable to the coverage under the TCHP scheme.
Upon his re-election in October 2017, President Kenyatta indicated that he wanted all Kenyans to have comprehensive health insurance within 5 years. NHIF was tasked with this promise. Hereto, NHIF introduced SupaCover, a comprehensive health insurance package covering both outpatient and inpatient care to formal sector employees as well as the informal sector.
Study design, data collection, and participants
We applied a quasi-experimental controlled before-after design to measure the impact of the TCHP programme 3.5 years after its introduction. Additionally, since the FMS programme was launched in the whole country, including in the TCHP control area, a before-after design was used to measure the effect of the FMS programme 1.5 years after it was launched.
Based on the Tanykina and Lelbren Dairy Company member lists, a random representative sample of 1,200 households was drawn from the TCHP programme and control areas. A baseline survey was carried out among the 1,200 households in February 2011, shortly before the introduction of TCHP. A follow-up survey was carried out among a smaller random subsample of 549 households in November 2014. In this study we used the baseline and follow-up data of these 549 households only. A fixed sample size of 549 households would allow us to measure a minimum impact of a 12.7 percentage points (PP) increase in the outcomes, with a power of 80% using a twotailed test and a 0.05 level of significance. Households were included in the surveys after written informed consent was obtained from the individual adult household members. For members younger than 18 years consent was obtained from the household head.
In addition, 25 in-depth stakeholder interviews about the TCHP, FMS, and NHIF programmes were conducted in November 2014. Stakeholder interviews were conducted with directors of healthcare facilities in Nandi County, government officials, and employees from Tanykina Dairy Company, TCHP, and NHIF.
The 3.5 years prior to the baseline survey were defined as pre-TCHP period (1 September 2007–28 February 2011) and the 3.5 years after its introduction were defined as post-TCHP period (1 May 2011–31 October 2014). Within the post-TCHP period, the 2 years prior to the FMS programme was launched were defined as pre-FMS period (1 March 2011–31 May 2013) and the 1.5 years after its launch were defined as post-FMS period (1 June 2013–31 October 2014).
All reported pregnancies and deliveries (full-term pregnancies) between 1 September 2007 and 31 October 2014 from women aged 15 to 49 years at the time of pregnancy were eligible for this study (repeated cross-sections).
Ethical clearance
Ethical approval for the study was obtained from the Kenyan Medical Research Institute in Nairobi, Kenya (16/09/2014, KEMRI/RES/7/3/1).
Outcomes
Antenatal care utilisation was defined as making at least 1 antenatal care visit at a healthcare facility and facility delivery was defined as delivery in any healthcare facility, as reported by the women during the household surveys. If a woman delivered twice during the follow-up-period (n=6), then only her most recent delivery was included in the analyses, as within the baseline-period only information of the last delivery was available.
Statistical analysis
We measured the intention-to-treat impact of the TCHP programme as very few eligible women were enrolled in the TCHP insurance scheme during the post-TCHP period. All women living in the TCHP programme area had the opportunity to utilise improved quality maternal and child health services in the upgraded TCHP facilities, regardless their enrolment in the TCHP health insurance, although uninsured women had to pay for these services. The intention-to-treat approach considers all women to be in the intervention group irrespective of whether they were insured through the TCHP scheme, which therefore avoids the bias introduced by voluntary insurance uptake and incorporates the independent effect of the quality improvements on uninsured women. Difference-in-differences analysis wasused to estimate the intention-to-treat impact, as the percentage points (PP) change in antenatal care utilisation and facility deliveries from the pre-TCHP period to the post-TCHP period in the TCHP programme area, adjusted for the change in the TCHP control area (see the Supplementary Data for more information on the specified difference-in-differences model).11,12,13,14
As the FMS programme was introduced in both areas, the effect of the FMS programme was estimated by a before-after comparison of the outcome variables in the pooled TCHP programme and control areas. Logistic regression analysis was used to estimate the effect of the FMS programme,15 as the PP change in antenatal care utilisation and facility deliveries from the pre-FMS period to the post-FMS period (see the Supplementary Data for more information on the specified logistic model). The effect of being enrolled in NHIF health insurance was also estimated in this analysis. Since most women had mandatory insurance with NHIF through work in the formal sector, selection bias-as a result of women who enrolled in the NHIF insurance scheme because they expected to get pregnant in the near future and consequently wanted to use NHIF for maternal healthcare utilisation-does not pose a problem here.
Confounders were selected based on Gabrysch and Campbell's conceptual framework.16 This framework distinguishes four sets of variables related to maternal and child healthcare utilisation, namely perceived needs (age, parity, and complications during previous deliveries), socio-demographic factors (religion and ethnicity), socio-economic factors (marital status, female household head, educational level household head, household consumption, daily per capita consumption below US$2, and NHIF enrolment status), and physical accessibility (distance to nearest health facility). Educational level of the household head and household consumption were included at their baseline value to avoid endogeneity problems. In the multivariable analyses, all a-priori selected confounders were included, irrespective of whether they were statistically significant. In addition, all analyses were corrected for heteroscedasticity. Data was analysed using STATA, version 12.1 (StataCorp LP, College Station, Texas, USA).
Results
Participants
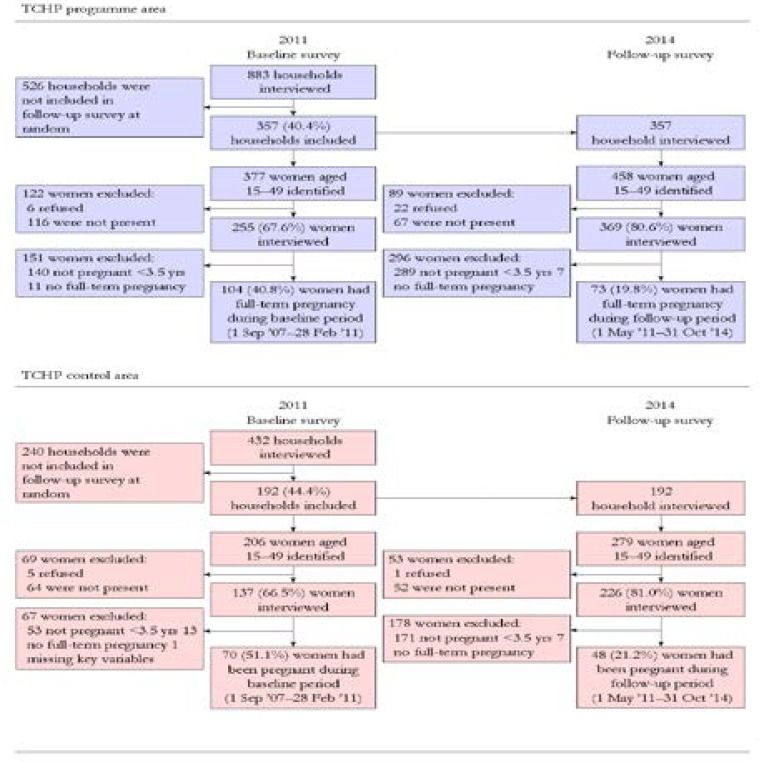
Within the 549 surveyed households, 44.4% of 392 interviewed women of reproductive age had a full-term pregnancy during the pre-TCHP period[40.8% (n=255) in the TCHP programme area and 51.1% (n=137) in the TCHP control area] and 20.3% of 594 interviewed women of reproductive age had a full-term pregnancy during the post-TCHP period [19.8% (n=369) in the TCHP programme area and 21.2% (n=226) in the TCHP control area] (Figure 1).
In both areas the fertility rate dropped by 54.2% over time (51.5% in the TCHP programme area and 58.4% in the TCHP control area). At follow-up, 56.0% of reproductive women reported to currently use birth control methods to prevent pregnancy or to space birth (59.0% in the TCHP programme area and 52.8% in the TCHP control area, data were not collected at baseline).
Non-response rates (due to absence or refusal to take the survey) among women of reproductive age were similar in the TCHP programme and the control areas at baseline [32.4% (n=377) vs 33.5% (n=206), respectively, P=0.781] and at follow-up [19.4% (n=458) vs 19.0% (n=279), respectively, P=0.884].
Population characteristics
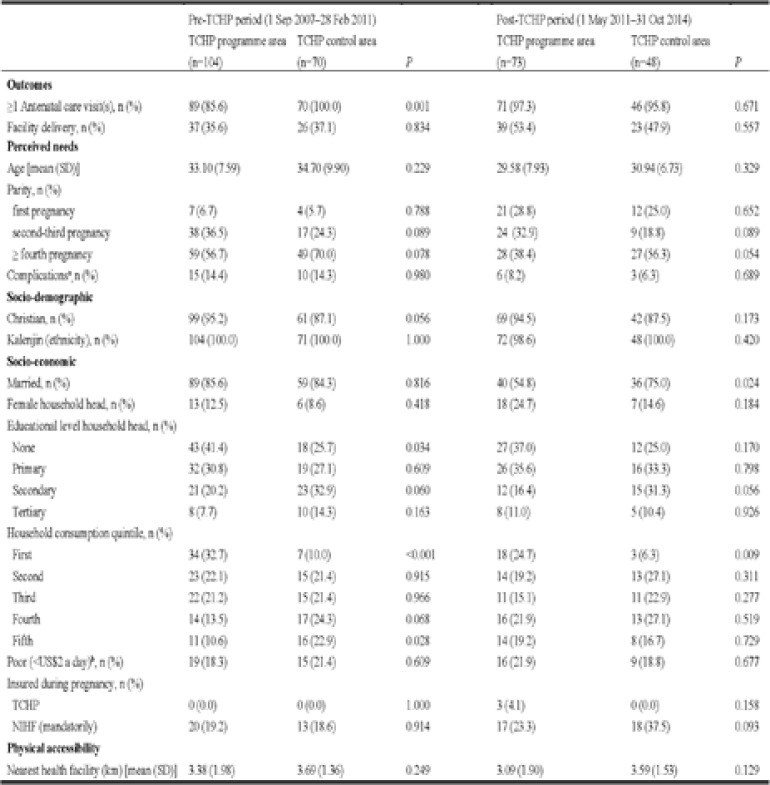
Whilst the TCHP programme and control areas were well balanced for most characteristics, significant differences were observed with respect to the distribution of education of the household head and household consumption before the introduction of the TCHP programme (Table 1).
Table 1.
Characteristics of women who reported a pregnancy in the pre-TCHP period (1 Sep 2007–28 Feb 2011) or post-TCHP period (1 May 2011–31 Oct 2014), by area (TCHP programme versus TCHP control)
Significantly more women in the TCHP programme area were living with a household head without any education (P=0.034) and were living in a household with total household consumption in the lowest quintile (P<0.001). In addition, women in the Pre-TCHP group (i.e. women who reported a pregnancy in the 3.5 years prior to the baseline survey) and women in the Post-TCHP group (i.e. women who reported a pregnancy in the 3.5 years prior to the follow-up survey) were comparable, as they had similar observed characterises before the introduction of the TCHP programme (Table S1).
Table S1.
Characteristics of women in both areas before the introduction of the TCHP programme (TCHP baseline), by period (pre-TCHP group versus post- TCHP group): test for comparability of repeated cross-sections in the TCHP programme evaluation
| Pooled areas | |||
| Pre-TCHP group | Post-TCHP group | ||
| TCHP baseline characteristics | (n=174) | (n=121) | P |
| Socio-demographic | |||
| Christian, n (%) | 160 (92.0) | 111 (91.7) | 0.946 |
| Kalenjin (ethnicity), n (%) | 174 (100.0) | 120 (99.2) | 0.231 |
| Socio-economic | |||
| Married, n (%) | 148 (85.1) | 29/36 (80.6)b | 0.502 |
| Female household head, n (%) | 19 (10.9) | 10/97 (10.3)c | 0.877 |
| Educational level household head, n (%) | |||
| None | 61 (35.1) | 39 (32.2) | 0.615 |
| Primary | 51 (29.3) | 41 (34.7) | 0.328 |
| Secondary | 44 (25.3) | 27 (22.3) | 0.558 |
| Tertiary | 18 (10.3) | 13 (10.7) | 0.931 |
| Household consumption quintile, n (%) | |||
| First | 41 (23.6) | 21 (17.4) | 0.199 |
| Second | 38 (21.8) | 27 (22.3) | 0.923 |
| Third | 37 (21.3) | 22 (18.2) | 0.517 |
| Fourth | 31 (17.8) | 29 (24.0) | 0.198 |
| Fifth | 27 (15.5) | 22 (18.2) | 0.547 |
| Poor (<US$2 a day)a, n (%) | 34 (19.5) | 25 (20.7) | 0.814 |
| Insured during pregnancy, n (%) NIHF (mandatorily) |
33 (19.0) | 27/58 (46.6)d | <0.001 |
| Physical accessibility | |||
| Nearest health facility (km) [mean (SD)] | 3.51 (1.76) | 3.29 (1.77) | 0.307 |
Daily per capita consumption below US$2 a day.
TCHP baseline info was observed for only 29 out of 121 women.
TCHP baseline info was observed for 97 out of 121 women.
TCHP baseline info was observed for only 58 out of 121 women.
Moreover, women in the Pre-FMS group (i.e. women who reported a pregnancy in the 2 years prior to the introduction of the FMS programme) and women in the Post-FMS group (i.e. women who reported a pregnancy in the 1.5 years after the introduction of the FMS programme) were also comparable, as they had similar characteristics, as observed before the introduction of the FSM programme (Table S2).
Table S2.
Characteristics of women in both areas before the introduction of the FMS programme (FMS baseline), by period (pre-FMS group versus post-FMS group): test for comparability of repeated cross-sections in the FMS programme evaluation
| Pooled areas | |||
| Pre-FMS group | Post-FMS group | ||
| FMS baseline characteristics | (n=57) | (n=64) | P |
| Socio-demographic | |||
| Christian, n (%) | 51 (89.5) | 60 (93.8) | 0.398 |
| Kalenjin (ethnicity), n (%) | 57 (100.0) | 63 (98.4) | 0.347 |
| Socio-economic | |||
| Married, n (%) | 41 (71.9) | 35 (54.7) | 0.051 |
| Female household head, n (%) | 8 (14.0) | 17 (26.6) | 0.091 |
| Educational level household head, n (%) | |||
| None | 13 (22.8) | 26 (40.6) | 0.037 |
| Primary | 23 (40.4) | 19 (29.7) | 0.222 |
| Secondary | 14 (24.6) | 13 (20.1) | 0.579 |
| Tertiary | 7 (12.3) | 6 (9.4) | 0.610 |
| Household consumption quintile, n (%) | |||
| First | 9 (15.8) | 12 (18.8) | 0.671 |
| Second | 13 (22.8) | 14 (21.9) | 0.903 |
| Third | 8 (14.0) | 14 (21.9) | 0.268 |
| Fourth | 17 (29.8) | 12 (18.8) | 0.157 |
| Fifth | 10 (17.5) | 12 (18.8) | 0.865 |
| Poor (<US$2 a day)a, n (%) | 11 (19.3) | 14 (21.9) | 0.729 |
| Insured during pregnancy, n (%) NIHF (mandatorily) |
19 (33.3) | 16 (25.0) | 0.317 |
| Physical accessibility | |||
| Nearest health facility (km) [mean (SD)] | 3.47 (1.71) | 3.13 (1.82) | 0.292 |
Source/Notes: 2014 household survey. Data are number (%) of women or mean (SD) (for distance to nearest health facility).
Daily per capita consumption below US$2 a day.
Before the introduction of TCHP in the TCHP programme area, 18.9% of 175 women with a full-term pregnancy during the pre-TCHP period were already (mandatorily) insured with NHIF [19.2% (n=104) in the TCHP programme area and 18.6% (n=70) in the TCHP control area] (Table 1).
TCHP insurance enrolment
In the TCHP programme area, 3 of 73 women with a full-term pregnancy during the post-TCHP period were insured with TCHP during pregnancy, including at the time of delivery. One of these 3 women was also mandatory insured with NHIF. Only 1 woman used her TCHP insurance for antenatal care visits and delivery, whereas the other 2 women went to a non-TCHP facility for their antenatal care visits and delivered either in this non-TCHP facility or at home. The woman insured with both TCHP and NHIF went to a non-TCHP facility for her antenatal care visits and delivery.
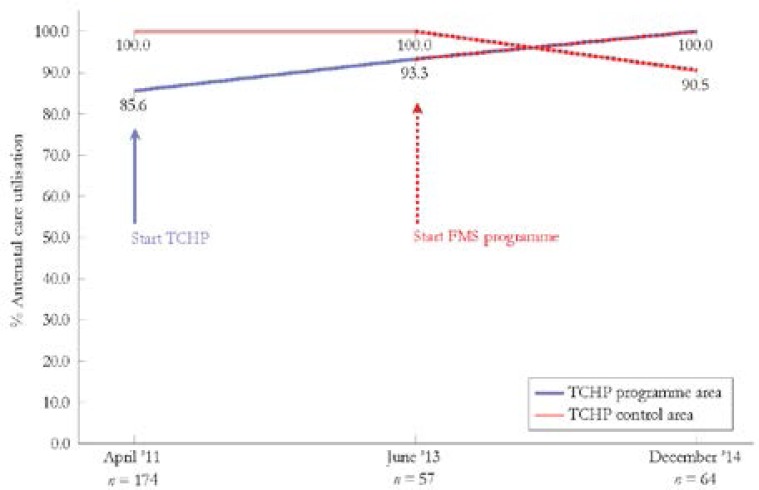
Antenatal care utilisation
Antenatal care utilisation during the pre-TCHP period was significantly lower among women in the TCHP programme area, compared to the TCHP control area (P<0.001) (Table 1). Antenatal care utilisation in the TCHP programme area increased from 85.6% of women (n=104) during the pre-TCHP period to 93.3% (n=30) after the introduction of the TCHP programme and then continued to grow to 100.0% (n=43) after the introduction of the FMS programme (Figure 2). In the TCHP control area antenatal care utilisation was consistently high at 100% (n=97) up to the introduction of the FMS programme and decreased to 90.5% (n=21) after the introduction of the FMS programme.
Of the 71 women who made antenatal care visits during the post-TCHP period in the TCHP programme area, 50.7% made between 1 and 3 antenatal care visits and 49.3% made at least 4 visits (data were not collected at baseline). Of the 46 women who made antenatal care visits during the post-TCHP period in the TCHP control area, 50.0% made between 1 and 3 visits and 50.0% made 4 or more visits.
Before the introduction of the FMS programme, women in both areas (n=57) reported to have paid on average 45 KSh in public facilities and 231 KSh in private facilities for their antenatal care visits in total, whereas women paid on average 135 KSh in public facilities and 73 KSh in private facilities in total after the introduction of the FMS programme (n=64).
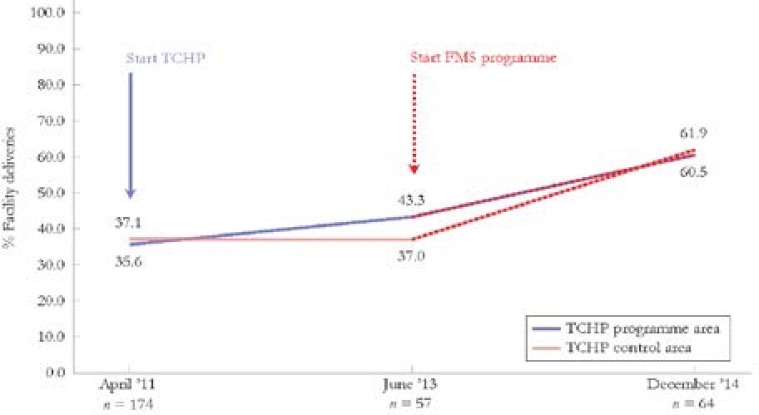
Facility deliveries
The percentage of women who delivered in a facility in the TCHP programme area increased from 35.6% (n=104) during the pre-TCHP period to 43.3% (n=30) after the introduction of the TCHP programme and then further increased to 60.5% (n=43) after the introduction of the FMS programme (Figure 3). In the TCHP control area facility deliveries remained stable, 37.1% (n=70) at baseline and 37.0% (n=27) after the introduction of TCHP, and then increased to 61.9% (n=21) after the introduction of the FMS programme.
Before the introduction of the FMS programme, women in both areas (n=57) reported to have paid on average 775 KSh in public facilities and 1368 KSh in private facilities for the delivery, whereas women paid on average 0 KSh in public facilities and 1529 KSh in private facilities after the introduction of the FMS programme (n=64). The main reasons for not delivering in a health facility before the introduction of the FMS programme were ‘the contractions came too suddenly’ (53.3%) and ‘tradition to deliver at home with traditional birth attendant’ (20.0%) (data were not collected at baseline). The main reasons for not delivering in a health facility after the introduction of the FMS programme also were ‘the contractions came to suddenly’ (53.6%) and ‘tradition to deliver at home with traditional birth attendant’ (17.9%).
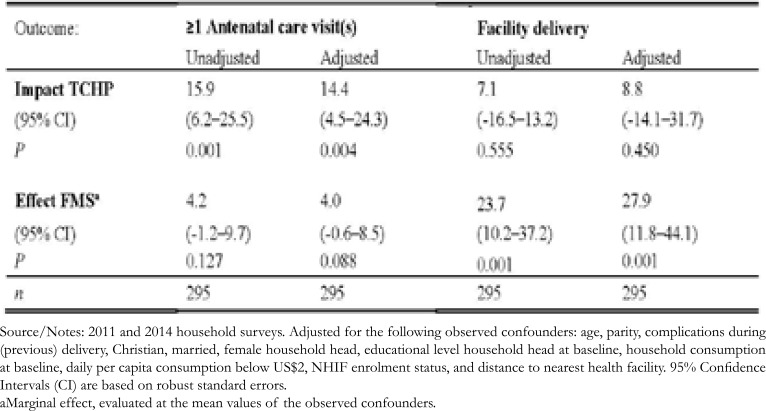
Intention-to-treat impact of the TCHP programme
After adjusting for observed confounders, the increase in antenatal care utilisation from the pre-TCHP period to the post-TCHP period was 14.4 PP (95% CI: 4.5–24.3; P=0.004) greater in the TCHP programme area than the change in the TCHP control area (Table 2). We did not find a significant effect of the TCHP programme on facility deliveries (8.8 PP; 95% CI: -14.1 to +31.7; P=0.450).
Table 2.
Estimated effect of the TCHP and FMS programmes on antenatal care utilisation and facility delivery
Source/Notes: 2011 and 2014 household surveys. Adjusted for the following observed confounders: age, parity, complications during (previous) delivery, Christian, married, female household head, educational level household head at baseline, household consumption at baseline, daily per capita consumption below US$2, NHIF enrolment status, and distance to nearest health facility. 95% Confidence Intervals (CI) are based on robust standard errors.
a Marginal effect, evaluated at the mean values of the observed confounders.
Effect of the FMS programme
We did not find a significant effect of the FMS programme on antenatal care utilisation (4.0 PP; 95% CI: -0.6 to +8.5; P=0.088) (Table 2). However, facility deliveries significantly increased after the introduction of the FMS programme by 27.9 PP (95% CI: 11.8–44.1; P=0.001).
Enrolment in NHIF was not significantly associated with antenatal care utilisation (1.8%; 95% CI: -3.4 to +6.9; P=0.503) or facility delivery (7.1%; 95% CI: -10.7 to +25.0; P=0.435).
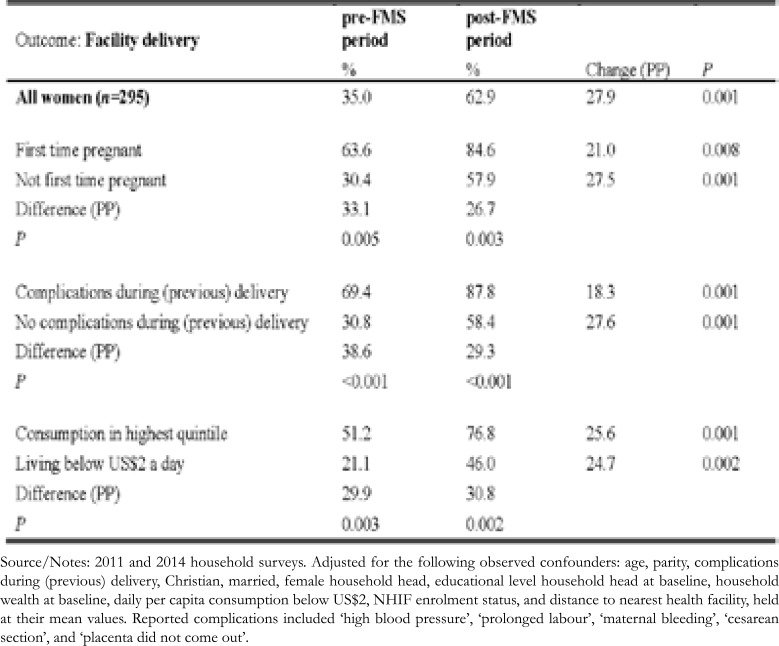
Pre-specified subgroup analyses indicated that the probability of facility delivery was highest among women who were pregnant for the first time and women who experienced complications during their (previous) delivery, whereas the probability was lowest among women living below US$2 a day, both before and after the introduction of the FMS programme (Table 3). The increase in facility deliveries as a result of the FMS programme was significant among all subgroups, but was highest among multiparous women (27.5 PP) and women who did not experience complications during their (previous) delivery (27.6 PP). Women with consumption in the highest quintile and women living below US$2 a day showed a similar increase in facility delivery (25.6 PP vs 24.7 PP, respectively). However, after the introduction of the FMS programme women living below US$2 a day still had a significantly lower probability of delivering in a facility than women with consumption in the highest quintile (46.0% vs 76.8%, respectively, P=0.002) (Table 3).
Table 3.
Estimated probability and changes in probabilities of facility delivery, by subgroups
Source/Notes: 2011 and 2014 household surveys. Adjusted for the following observed confounders: age, parity, complications during (previous) delivery, Christian, married, female household head, educational level household head at baseline, household wealth at baseline, daily per capita consumption below US$2, NHIF enrolment status, and distance to nearest health facility, held at their mean values. Reported complications included ‘high blood pressure’, ‘prolonged labour’, ‘maternal bleeding’, ‘cesarean section’, and ‘placenta did not come out’.
Discussion
This study provides evidence that the FMS programme was positively associated with facility deliveries among women living in Nandi County. The number of facility deliveries increased by 27.9 PP (or 75%) after the introduction of the FMS programme. This finding is in line with the findings of another study that also assessed the impact of the FMS programme on utilisation of maternal health services.17 This suggests that there is a high latent demand for facility deliveries among women in Nandi county-and likely in the rest of Kenya, as well-and that the government programme is at least partly able to address this demand.
Stakeholder interviews with hospital staff indicated that, even though the number of deliveries substantially increased after introduction of the FMS programme in public facilities, the number of staff members was not increased and supplies were running out and were not replenished, resulting in a decline in the quality of delivery care provided by these facilities (data not shown).18,19 A study among facility staff at the maternity unit of 2 public facilities indicated major implementation challenges of the FMS programme, as well, including inadequate supplies, staff shortage, lack of motivation among health workers, and overwhelming workload.20 Increasing access to facility deliveries will have a less beneficial effect on maternal and child health and survival if the available healthcare is of poor quality. Thus, the FMS programme should also focus on sustaining and improving quality of care.
We did not find an effect of the FMS programme on antenatal care utilisation. We observed that in practise most facilities did not cover the costs of antenatal care from their FMS budget, and that the average total costs of antenatal care visits even increased in public facilities after the introduction of the FMS programme, whereas the average total costs in private facilities decreased. This might have resulted in women abstaining from making antenatal care visits in public facilities and instead making these visits in private facilities after the introduction of the FMS programme, in particular in the upgraded TCHP facilities.
On the other hand, antenatal care utilisation did significantly increase after the introduction of the TCHP programme. However, as only 3 women were insured with TCHP during pregnancy, this impact of the TCHP programme could only be a result of (uninsured) women who chose to make use of improved quality maternal and child healthcare services in the upgraded TCHP facilities. In depth interviews indeed indicated that before the introduction of the TCHP programme women would travel to the nearest public referral hospital as they did not trust the available antenatal care services nearby (data not shown). The TCHP programme ensured that quality maternal services became available closer to their homes, reducing travel costs.
However, even though we saw a small increase in facility deliveries in the TCHP programme area after the introduction of TCHP, we were not able to calculate reliable estimates of the effect of TCHP on facility deliveries, because our sample was too small to measure impacts below a 12.7 PP increase.
Limitations of the study
The high utilisation of antenatal care in the TCHP control area, which was at a maximum and could only remain stable or decrease and hence is not an optimal comparator. However, excluding the women without antenatal care utilisation during the post-TCHP period in the control area (n=2) only slightly attenuated the TCHP impact to a 10.0 PP increase (95% CI: 2.1 to 17.9; P=0.014), after adjusting for observed confounders. This shows that antenatal care utilisation also significantly increased in the TCHP programme area in a scenario where antenatal care utilisation in the TCHP control area remained stable at 100%. Moreover, given that the TCHP programme area was poorer and lower educated at baseline, compared to the TCHP control area, it seems plausible that the catch up effect in antenatal care utilisation could have been brought about by the TCHP programme.
Another limitation of this study was the lack of a control area in the FMS programme evaluation, as the FMS programme was introduced in the whole of Kenya. Lacking a control group makes it impossible to disentangle the increase in facility delivery as a result of the introduction of the FMS programme from any increase or decrease that potentially would have happened over time naturally. However, we could calculate the change in hospital deliveries in the TCHP control area over time before the introduction of the FMS programme and extrapolate, where we exclude the TCHP programme area in this calculation as any change there could have been a result of the introduction of the TCHP programme. This calculation shows that there was no change in facility deliveries in the years before the introduction of the FMS programme (see also Figure 3), which would suggest that a natural increase would not have occurred and that the FMS programme effect was likely accurately estimated.
The 54.2% drop in fertility rate in both areas could be the result of a 54.8% increase in the use of contraceptives between 2009 and 2014 in Nandi County, as observed in the 2008/2009 and 2014 Demographic and Health Surveys.6,7
We do not know why enrolment in TCHP among households with pregnant women was low. However, with 1 out of 3 women already (mandatorily) enrolled in NHIF as well as delivery care services provided free of charge by the government in all public facilities it turned out difficult for the TCHP programme to increase enrolment among households. An additional explanation could be TCHP being a family insurance and not an individual insurance. For example, another study that assessed the impact of a similar insurance programme in rural Nigeria, but with insurance enrolment at an individual level showed that insurance enrolment was high among pregnant women (up to 72%), whereas enrolment was substantially lower among men, non-pregnant women, and children.11 This suggests that pregnant women are likely to enrol in insurance, but do potentially less so when the whole household needs to enrol. Potential reasons for this could be that the costs of enrolling the whole household do not weigh up against the benefits of the pregnant woman being insured or that to enrol the whole household was unaffordable.
Conclusion
Previous studies demonstrated that the best way to bring down high maternal and neonatal mortality is to increase access to and utilisation of quality antenatal and delivery care, including emergency obstetric care.3,4,5 We showed that the FMS programme significantly increased the number of facility deliveries and that the TCHP programme significantly increased antenatal care utilisation. In theory, the FMS programme of the Kenyan government makes the inclusion of maternal care in an insurance package redundant and the TCHP programme and the government programme are at risk of competing with each other. However, as the TCHP programme also includes quality upgrades for the participating clinics and hospitals, a further alignment of the two programmes could potentially lead to synergistic results regarding the health of mother and child.
Ethics
Ethical approval for the study was obtained from the Kenyan Medical Research Institute in Kenya. Households were included in the surveys after written informed consent was obtained from the individual adult household members. Consent was obtained from the head of household for those under 18.
Conflicts of interest statement
None declared.
References
- 1.WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division, author. The World Bank data: maternal mortality ratio (modeled estimate, per 100,000 live births) [Internet] Geneva: World Health Organization; 2015. [Cited 2018 Jan 4] Available from: https://data.worldbank.org/indicator/SH.STA.MMRT. [Google Scholar]
- 2.United Nations, author. Introduction and proposed goals and targets on sustainable development for the Post2015 development agenda [Internet] New York City: United Nations; [Cited 2017 Jul 15] Available from: http://sustainabledevelopment.un.org/focussdgs.html. [Google Scholar]
- 3.Bulatao RA, Ross JA. Which health services reduce maternal mortality? Evidence from ratings of maternal health services. Tropical Medicine and International Health. 2003;8:710–721. doi: 10.1046/j.1365-3156.2003.01083.x. [DOI] [PubMed] [Google Scholar]
- 4.Campbell OMR, Graham WJ, Lancet Maternal Survival Series steering group Strategies for reducing maternal mortality: getting on with what works. Lancet. 2006;368:1284–1299. doi: 10.1016/S0140-6736(06)69381-1. [DOI] [PubMed] [Google Scholar]
- 5.Bhutta ZA, Ali S, Cousens S, et al. Interventions to address maternal, newborn, and child survival: what difference can integrated primary health care strategies make? The Lancet. 2008;372:972–989. doi: 10.1016/S0140-6736(08)61407-5. [DOI] [PubMed] [Google Scholar]
- 6.Kenya National Bureau of Statistics, author. Kenya Demographic and Health Survey 2008-09 [Internet] Nairobi: Kenya National Bureau of Statistics; 2010. [Cited 2017 Jul 16] Available from: https://dhsprogram.com/pubs/pdf/fr229/fr229.pdf. [Google Scholar]
- 7.Kenya National Bureau of Statistics, author. Kenya Demographic and Health Survey 2014 [Internet] Nairobi: Kenya National Bureau of Statistics; 2015. [Cited 2017 Jul 16] Available from: https://dhsprogram.com/pubs/pdf/fr308/fr308.pdf. [Google Scholar]
- 8.Ministry of Public Health and Sanitation, author. Status of implementation of free maternity services (FMS) program in the devolved health system in Kenya [Internet] Nairobi: Ministry of Public Health and Sanitation; 2015. [Cited 2017 Jul 16] Available from: http://publications.universalhealth2030.org/ref/37690886318ba047a95afd368aaf646f. [Google Scholar]
- 9.SafeCare, author. SafeCare website. [Internet] Amsterdam: SafeCare; [Cited 2018 Jan 31] Available from: http://www.safe-care.org/ [Google Scholar]
- 10.Hendriks ME, Wit FW, Akande TM, et al. Effect of health insurance and facility quality improvement on blood pressure in adults with hypertension in Nigeria: a population-based study. JAMA Internal Medicine. 2014;174:555–563. doi: 10.1001/jamainternmed.2013.14458. [DOI] [PubMed] [Google Scholar]
- 11.Brals D, Aderibigbe SA, Wit FW, et al. The effect of health insurance and health facility-upgrades on hospital deliveries in rural Nigeria: a controlled interrupted time-series study. Health Policy and Planning. 2017;32(7):990–1001. doi: 10.1093/heapol/czx034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee M, Kang C. Identification for difference in differences with crosssection and panel data. Economics Letters. 2006;92:270–276. [Google Scholar]
- 13.Blundell R, Dias MC. Alternative approaches to evaluation in empirical microeconomics. Journal of Human Resources. 2009;44:565–640. [Google Scholar]
- 14.Wooldridge JM. Econometric Analysis of Cross Section and Panel Data. Cambridge, MA: MIT Press; 2010. [Google Scholar]
- 15.Cameron AC, Trivedi PK. Microeconometrics using stata. College Station, TX: Stata press; 2010. [Google Scholar]
- 16.Gabrysch S, Campbell OM. Still too far to walk: Literature review of the determinants of delivery service use. BMC Pregnancy Childbirth. 2009;9:34. doi: 10.1186/1471-2393-9-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Njuguna J, Kamau N, Muruka C. Impact of free delivery policy on utilization of maternal health services in county referral hospitals in Kenya. BMC Health Services Research. 2017;17:429. doi: 10.1186/s12913-017-2376-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.van der List M, Nelissen HE, Brals D, et al. Healthcare initiatives in Nandi County: dairy farmers and their families' use of various healthcare initiatives, including The Community Healthcare Plan [Unpublished report] Amsterdam: Amsterdam Institute for Global Health and Development and Amsterdam Institute for International Development; 2016. [Google Scholar]
- 19.Nelissen HE, van der List M, Brals D, et al. Evaluation of The Community Healthcare Plan in Nandi North, Kenya: enrollment and dropout [Unpublished report] Amsterdam: Amsterdam Institute for Global Health and Development and Amsterdam Institute for International Development; 2016. [Google Scholar]
- 20.Wamalwa EW. Implementation challenges of free maternity services policy in Kenya: the health workers' perspective. Pan African Medical Journal. 2015;22:375. doi: 10.11604/pamj.2015.22.375.6708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kenya National Bureau of Statistics, author. Kenya Demographic and Health Survey 2014 [Internet] Nairobi: Kenya National Bureau of Statistics; 2015. [Cited 2017 Jul 16] Available from: https://dhsprogram.com/pubs/pdf/fr308/fr308.pdf. [Google Scholar]