Abstract
This guideline presents reference limits for use in echocardiographic practice, updating previous guidance from the British Society of Echocardiography. The rationale for change is discussed, in addition to how the reference intervals were defined and the current limitations to their use. The importance of interpretation of echocardiographic parameters within the clinical context is explored, as is grading of abnormality. Each of the following echo parameters are discussed and updated in turn: left ventricular linear dimensions and LV mass; left ventricular volumes; left ventricular ejection fraction; left atrial size; right heart parameters; aortic dimensions; and tissue Doppler imaging. There are several important conceptual changes to the assessment of the heart’s structure and function within this guideline. New terminology for left ventricular function and left atrial size are introduced. The British Society of Echocardiography has advocated a new approach to the assessment of the aortic root, the right heart, and clarified the optimal methodology for assessment of LA size. The British Society of Echocardiography has emphasized a preference to use, where feasible, indexed measures over absolute values for any chamber size.
Keywords: 2D echocardiography, guidelines, reference ranges
Introduction
The British Society of Echocardiography (BSE) has previously provided reference values and guidelines for chamber quantification through the provision of posters, pocket guides and the EchoCalc app (1, 2). These were based on joint publications by the American Society of Echocardiography (ASE) and the European Association of Cardiovascular Imaging (EACVI), originally published in 2005 (3). Newer right heart data were derived from guidelines published in 2010 (4). The ASE and EACVI subsequently updated their guidelines in 2015 (5, 6). Since that time further research has been published, using prospective data collection, on which the BSE has chosen to base the current recommendations upon.
For the current guidance, the BSE has chosen, in some instances, to deviate from the combined European and American guidance for our own reference intervals. There were several reasons for this. Principally, the BSE wanted to ensure that the reference ranges were derived from the most contemporaneous and prospectively acquired data; that reference ranges were derived from evidence that best applies to the British population; and finally ensure that echo guidance and cut-offs reflect practice within the UK. This document will outline the approach taken by the BSE in producing the up-to-date British guidelines, in addition to detailed explanatory notes regarding each parameter in turn. Reference intervals for the parameters in Table 1 are described in the main document and summarised in Supplementary Table 1 (see section on supplementary materials given at the end of this article). Diastolic parameters will be covered in a separate guideline.
Table 1.
Echocardiographic parameters covered by the BSE 2019 guidelines.
| BSE reference intervals 2019 |
|---|
| Linear left ventricular dimensions and LV mass |
| Left ventricular volumes |
| Left ventricular ejection fraction |
| Left atrial volume |
| Indexed right ventricular end diastolic area |
| Indexed/non-indexed right atrial area |
| Right ventricle and right ventricular outflow tract diameter |
| Right ventricular fractional area change |
| Aortic root dimensions |
| Tissue Doppler: mitral annular s′ and right ventricular s′ |
The overarching objectives of this document were to:
Provide a simple, practical reference document and guide for everyday use by our members.
Enable appropriate interpretation of values into a clinically relevant report.
Encourage the holistic interpretation of measurements – no single number should define normality or pathology.
The BSE acknowledges that the changes suggested within this document may result in some individuals who were previously labelled as having an echocardiographic abnormality now being considered as normal (and vice versa). Although this can present a challenge to clinicians, the changes are necessary and are reflective of the current evidence-base. The BSE advocates that echo departments discuss the new reference limits with end-users, including cardiologists and other clinicians, to ensure that the changes suggested within this document are rationalised and that patient care is not adversely affected.
Methods
Source data
A reference interval for any echocardiographic parameter should be derived from a population of apparently normal individuals: that is to say, a group of individuals who are devoid of overt cardiovascular disease. It is preferred if individuals with multiple risk factors for cardiovascular disease (for example, a history of smoking or strong family history of coronary disease) are excluded as they may have as yet undiagnosed cardiac abnormalities that could influence the results. Once the population has been defined, adequate numbers of ‘normal’ participants across the spectrum of ages and body sizes are needed to ensure that the reference limits can be considered representative of the population at large. Studies ideally should be prospectively recruited and not identified from retrospective review of echo databases. There should be clear echo protocols such that each parameter is obtained using optimized views and best practice. In the perfect scenario, echo images would be reported in a core-lab, or dedicated independent echo-lab, to guarantee that the analysis of images and therefore the results are consistent. Finally, the individuals included in the reference data should reflect the population to which the ranges will then be applied.
The ASE/EACVI guidance from 2015 extracted echo data from several large databases to derive reference intervals (5, 6). This was commendable as it maximizes the number of participants, but for some parameters results in suboptimal methodology: for example, left ventricular ejection fraction (LVEF) from the apical four-chamber view was obtained from more than 2000 individuals, but the biplane LVEF intervals were derived from around 500 patients. In addition, including data from multiple sources means that the echocardiographic methods for all subjects were not necessarily uniform, nor was quality assured with the use of a dedicated independent echo-lab. Finally, some results were obtained from a North American population and therefore may not be completely applicable to the British population.
Two major studies presenting useful echocardiographic reference intervals have been published subsequent to the joint ASE/EACVI guidance. The first of these was the Normal Reference Ranges for Echocardiography (NORRE) dataset which has resulted in multiple publications (7, 8, 9, 10). The NORRE project included over 700 individuals, and the study design and execution fulfil many of the ideal criteria outlined above. Participants were prospectively recruited, with pre-defined echo protocols. All echo data were analysed by a core-lab, ensuring consistency of results. The included individuals were free from both overt cardiovascular disease and had low clinical probability of latent disease, were not taking any cardio-active medication, and all had lab testing for hyperglycaemia, dyslipidaemia, and renal function. Competitive athletes and obese individuals were excluded. Care was taken to ensure that sufficient numbers of individuals from all age categories were included. This study was a European collaborative project and therefore the results can be considered applicable to the UK population (7).
The second study was the EchoNormal project, a large meta-analysis of more than 50,000 individuals of differing ethnicities, obtained from over 40 different studies undertaken worldwide (11). After exclusions, more than 22,000 participants were used to define reference intervals. The results from the EchoNormal project provide a valuable insight into ethnic variation, and age-dependent changes of echo parameters. It is commendable that the cohort used in EchoNormal was large. However, the meta-analysis design means that the inclusion criteria for each of the 43 studies included were not necessarily identical, and the definition of ‘normal’ was not uniform. Echo images were analysed in the individual centres, and therefore consistency could not be guaranteed. For some parameters (including ventricular volumes and LVEF), data from one or more centres were excluded as it appeared to deviate significantly from the results seen elsewhere, which raises questions regarding validity. Finally, a large proportion of the participants were not European, and therefore the relevance to a UK population is less clear.
For these reasons, the current BSE reference intervals were in large part derived from the NORRE dataset.
Defining reference intervals
This guideline proposes reference intervals for echocardiography. These are not the same as ‘normal ranges’, and it is of paramount importance to understand the difference as this necessarily affects the way in which the ranges produced within this document are applied in day-to-day practice.
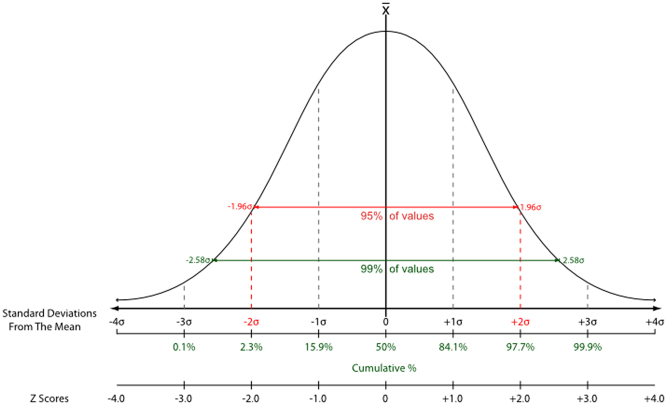
Statistical convention used throughout the literature states that a reference interval includes 95% of the normal population (Fig. 1). By definition, this excludes the remaining ‘normal 5%’ who appear at the upper and lower extreme. If the parameter in question is normally distributed, the 95% reference intervals can be obtained from the data using the mean ± 1.96 × standard deviation. However, for almost a century, 1.96 has been rounded to 2, which covers 95.4% of the population (12). Thus:
Figure 1.
The normal distribution curve. Using a combination of the population mean and standard deviation, reference limits can be calculated. A range of values encompassing 2 standard deviations above and below the population mean includes 96.4% of all ‘normal’ subjects. Similarly, 3 standard deviations encompass 99.7% of the normal population.
Upper reference limit (URL) = mean value+(2 × standard deviation)
Lower reference limit (LRL) = mean value – (2 × standard deviation)
It is a frequent misconception that if an individual parameter falls outside of the reference limits it should always be considered as abnormal. If we take the example of left ventricular (LV) dimensions: using the above methodology, it is expected that 4.6% of all normal patients will have values that are either above the upper reference limit or below the lower reference limit. In clinical practice, more importance is often applied to one extreme: practitioners may consider an increased LV size as clinically more relevant than a reduced size. Even in this scenario, a substantial number of individuals (2.3% of ‘normal’ patients) will have LV dimensions that are above the URL. It is therefore essential to interpret any value that falls outside of the reference limits within the clinical context, rather than immediately consider them as abnormal.
Similarly, it is also possible for a parameter to fall within the reference interval, and yet, it may not actually be ‘normal’ for that individual. For example, a patient may be noted to have an LVEF result that drops from 65 to 55% on sequential measurements. Although both of these LVEF values are within the ‘normal reference limit’, in this case, it is quite possible that there is an underlying pathological process and incipient LV systolic dysfunction. It is therefore of paramount importance that echocardiographic values, whether they are superficially normal or not, are always interpreted in the clinical context. If a patient has had previous echo studies, comparison between historical and contemporary findings is of significant clinical utility.
The above statistical methodology has been applied to the NORRE data to derive reference limits for most echocardiographic parameters. Detailed explanations are provided where the BSE has deviated from this practice.
Grading of abnormality
Once an echocardiographic value falls outside of the reference intervals, it is common practice to consider the parameter in question as being ‘mildly, moderately or severely’ abnormal (bearing in mind that, as discussed above, the normal/mildly abnormal zone will have some overlap). There are several reasons why this approach is useful: it helps to give an idea as to the magnitude of abnormality to the referring clinician, it may provide use in monitoring of disease progression, or it may provide information as to prognosis for a particular disease. To a clinician, an abnormality labelled as ‘severe’ will usually demand attention and probably treatment (i.e. it should not be ignored).
The partition between a ‘mild and moderate’, or ‘moderate and severe’ abnormality can be defined in a number of ways. Perhaps the ideal method would be to define the severity of the abnormality according to prognostic significance: progression from mild to moderate to severe abnormality would be associated with clear impact on cardiovascular outcomes from contemporary studies. In reality, however, most echocardiographic parameters such as LVEF or LA size display a continuous association with survival (i.e. as the LVEF gets progressively lower, survival is progressively poorer (13)), and specific cut-offs are defined more for clinical simplicity and utility as opposed to being genuinely disease defining. A different methodology would be to define partitions according to clinical intervention(s) available at specific points.
Another frequent practice is to define these partitions as a function of the standard deviation and the mean. Just as the upper reference limit is usually two standard deviations above the mean, the partition between mild and moderate abnormality is defined as three standard deviations above the mean, and the moderate/severe threshold as four standard deviations above the mean. This is akin to paediatric cardiologist’s use of Z-scores, where the Z-score is the number of standard deviations from the mean (14). Although superficially this approach may not appear to have clinical relevance, it has value in providing information as to how frequently this magnitude of variation would be expected within a normal population. Taking the example of LV dimensions: just as 2.3% of normal individuals will have an LV size above the upper reference limit, a tiny proportion of normal individuals (just 0.15% of the normal population) would have values in the ‘moderate’ range using this methodology. Furthermore, essentially no normal patients would ever be expected to have LV dimensions in the ‘severe’ range (Fig. 1). This further re-iterates the clinical approach that once an individual parameter is close to severely abnormal immediate clinical attention is warranted.
Within these guidelines, grading ranges have been provided only where they have clinical utility.
Normal variation
Many, if not all, echocardiographic parameters vary according to gender, body habitus (either height, weight or both), ethnicity, fitness, and age. If all these variables were factored into every single measurement, reporting times would become unreasonable, and the associated reference tables would be unwieldy. We have attempted to include as many useful variables as is practical, whilst maintaining the simplicity for busy echo practitioners. However, this has necessarily led to some compromises.
One compromise is regarding age-related variations. Several echocardiographic criteria (for example left and right ventricular size and LVEF) vary with normal aging, whereas others (including left and right atrial volumes and LV mass) do not (8). The BSE believes that it would be impractical to divide reference tables to account for this variation in some but not all parameters, particularly if the absolute difference is often so small as to be clinically insignificant. This compromise approach re-iterates the need to interpret values that are slightly outside the reference limits with caution, particularly if they are obtained in patients at the extremes of age.
Echocardiographic parameters are usually indexed according to BSA. For certain parameters, such as left atrial (LA) volumes, there is a wealth of evidence that this approach is reasonable (15, 16). For others, this approach may not be as useful. For example, although the NORRE dataset published indexed values for internal LV dimensions and LA diameter, neither of these are routinely used in clinical practice. The absolute LV internal diameter is a predictor of outcomes in mitral and aortic valve disease and is used to guide timing of surgical intervention (17, 18, 19). There is less data to support the use of indexed values in this regard. Therefore, the BSE has chosen to publish indexed values only for those parameters where there is a clear clinical indication for this approach.
In obese patients, caution is advised when interpreting indexed values, particularly as the NORRE database excluded individuals with a BMI >30 kg/m2. The metabolic demand of fatty tissue is considerably lower than muscle, and therefore, obesity is less likely to drive changes in chamber size or wall thickness. In essence, indexing for body surface area (BSA) when individuals are very overweight may result in an underestimation of the degree of cardiac remodelling (20).
Limitations
There are three patient cohorts in whom these reference tables may not be applicable. These are non-Caucasian individuals, athletes, and pregnant patients.
The NORRE dataset included healthy Caucasian volunteers only, and therefore, the values provided in the tables will not be as reliable in individuals of different ethnic origin (7). For example, there is some evidence that individuals of Afro-Caribbean or Asian descent differ from Caucasian counterparts with regards LV mass values (11).
The BSE has chosen not to include ethnicity-specific reference intervals for several reasons. Firstly, as we discussed earlier, currently available ethnicity-specific data from EchoNormal is not as robust as NORRE. As yet unpublished data from the upcoming World Alliance of Societies of Echocardiography Normal Values Study (WASE trial, presented in abstract form) suggests that in addition to ethnicity, the country in which an individual lives results in important echocardiographic variation. For example, individuals of Chinese descent differ considerably if they live in China compared to those that live in Europe. Similar inter-country variation was seen with all ethnicities. This further reinforces the BSE’s belief that using data obtained from China or Asia to derive reference intervals for individuals living in the UK would not be valid. Secondly, an ethnic-specific approach would necessarily require all sonographers to ask for a patient’s ethnic origin prior to undertaking an echo exam, which could be considered unreasonable. Thirdly, it is likely that individuals of mixed heritage would not fit solely into one dataset or another, which would introduce further difficulties when asking patients regarding their ethnicity and subsequently interpreting the echo findings.
Therefore, the BSE proposes that the presented reference tables are used for patients of all ethnicities but reminds sonographers to be aware of potential variation secondary to ethnicity. Although the available data are not sufficient to derive specific reference limits, the following could be considered within the clinical context:
Individuals of Afro-Caribbean descent appear to be very similar to Caucasians with regards LV volumes and function. LV mass, however, may be marginally higher, and therefore a ‘mild’ increase in LV mass should be interpreted with caution and within the clinical context.
Individuals of East Asian or Indian origin may have a tendency towards slightly smaller LV volumes. As such it is possible that LV volumes approaching the proposed upper reference limits may in fact be slightly abnormal for such ethnic groups and should be interpreted within the clinical context.
There are insufficient data to provide advice regarding the effects of ethnicity on LA volume or right heart size at this time.
Echocardiography in athletes should also be interpreted with caution. Participation in competitive sport results in remodelling and morphological alterations of the heart, including increases in: LV dimensions and volumes, right ventricular (RV) dimensions, LV mass, and LA volumes (21, 22, 23, 24). The magnitude of these morphological alterations appears to be linked to both the volume and type of exercise undertaken. There is no practical or widely accepted way in which the effects of exercise on cardiac structure can be readily standardized or accounted for. NORRE actively excluded individuals who participated in competitive sport. For this reason, sonographers and clinicians should be cognizant of these potential influences when interpreting the echocardiographic findings of such individuals (23).
Finally, caution is advised when using these reference tables to interpret echocardiographic studies in pregnant women. Physiological cardiac adaptation during pregnancy includes enlargement of the left and right ventricles and the atria, in addition to changes in left and right ventricular function (25). NORRE excluded pregnant individuals from the study.
Timing
Timing of measurements is critical. ECG timings can vary with the lead used and is affected by conduction defects and coronary artery disease (26). The 2015 chamber guidelines and many textbooks have varying definitions (5, 6). The definitions from the EACVI/ASE/Industry Task Force paper on standardising deformation imaging have thus been adopted as follows (27).
Ventricular end systole
The timing of ventricular end systole is taken as the frame where the aortic valve initially closes. This coincides with a closure click on the pulsed-wave Doppler tracing of aortic valve flow. When obtaining images from the apical 2- or 4-chamber views, end-systole is defined as the frame prior to mitral valve opening (5, 6). In addition, this is the point at which maximal volume of the LA should be obtained.
Ventricular end diastole
The timing of ventricular end diastole is taken as the frame before the mitral valve closes. Surrogates for this are the frame with the largest LV cavity size (diameter or volume), the start of the ECG QRS complex, or the ECG R-wave (a common trigger for analysis software).
BSE reference intervals
The following section outlines the new BSE reference limits for left and right heart parameters, combined with explanations of the methodology, decision-making process, and discussions regarding the potential clinical impact of the new reference intervals. Where appropriate, we have described the methodology by which some of the measurements should be acquired, but for a more detailed description regarding the echocardiographic measurements and how they should be obtained, please see the BSE minimum dataset (28).
Left ventricular linear dimensions and LV mass
New reference intervals for linear LV dimensions and LV mass are presented in Table 2. LV dimensions should be obtained from the parasternal long-axis (PLAX) window preferentially using 2D imaging. The BSE would discourage the use of M-mode measurements as routine, although they are acceptable if the long-axis of the left ventricle is perpendicular to the angle of incidence of the ultrasound beam. LV mass should be calculated using the linear method from 2D imaging and reported after indexing to BSA (8).
Table 2.
Linear left ventricular dimensions and mass.
| Normal | Mild | Moderate | Severe | |
|---|---|---|---|---|
| Males | ||||
| LV dimensions | ||||
| LVIDd (mm) | 37–56 | 57–61 | 61–65 | >65 |
| LVIDs (mm) | 22–41 | 41–45 | 46–50 | >50 |
| IVSd (mm) | 6–12 | – | – | – |
| LVPWd (mm) | 6–12 | – | – | – |
| LV mass | ||||
| LVMi (g/m2) | 40–110 | 111–127 | 128–145 | >145 |
| LV mass (g) | 72–219 | – | – | – |
| Females | ||||
| LV dimension | ||||
| LVIDd (mm) | 35–51 | 52–55 | 56–59 | >59 |
| LVIDs (mm) | 20–37 | 38–42 | 43–46 | >46 |
| IVSd (mm) | 5–11 | – | – | – |
| LVPWd (mm) | 6–12 | – | – | – |
| LV mass | ||||
| LVMi (g/m2) | 33–99 | 98–115 | 116–131 | >131 |
| LV mass (g) | 51–173 | – | – | – |
IVSd, inter-ventricular septal thickness in diastole; LV, mass calculated using the linear method; LVIDd, left ventricular internal diameter in diastole; LVIDs, left ventricular internal diameter in systole; LVMi, left ventricular mass index; LVPWd, left ventricular posterior wall thickness in diastole.
The BSE has chosen to publish an upper reference limit only for wall thickness measures with no separate partitions for mild, moderate, or severe changes, as using standard deviations to define partitions would result in such narrow ranges that they would be clinically meaningless.
LV wall thickness by itself does not define an individual as having left ventricular hypertrophy (LVH). Rather, the presence or absence of LVH is determined from LV mass after indexing to BSA. Wall thickness measurements, combined with the LV internal diameter in diastole, can be used to determine the relative wall thickness (RWT) using the following formula:
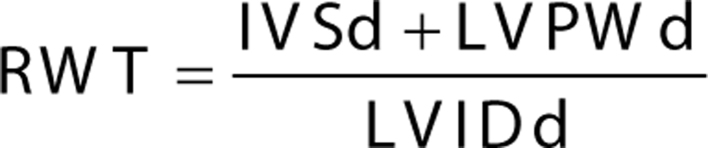 |
The combination of indexed LV mass and relative wall thickness can be used to define LV geometry (Fig. 2). In the context of an increased mass, an RWT > 0.42 defines the pattern of LVH as being ‘concentric’. If the RWT is ≤0.42, the pattern of LVH is ‘eccentric’. The pattern of LVH provides an insight into the underlying pathophysiological state. Concentric LVH is characteristically seen in patients with increased afterload such as aortic stenosis or hypertension. Eccentric LVH is more likely to be seen in scenarios with increased LV pre-load and associated compensatory hypertrophy, such as chronic aortic regurgitation (AR) or mitral regurgitation (MR).
Figure 2.
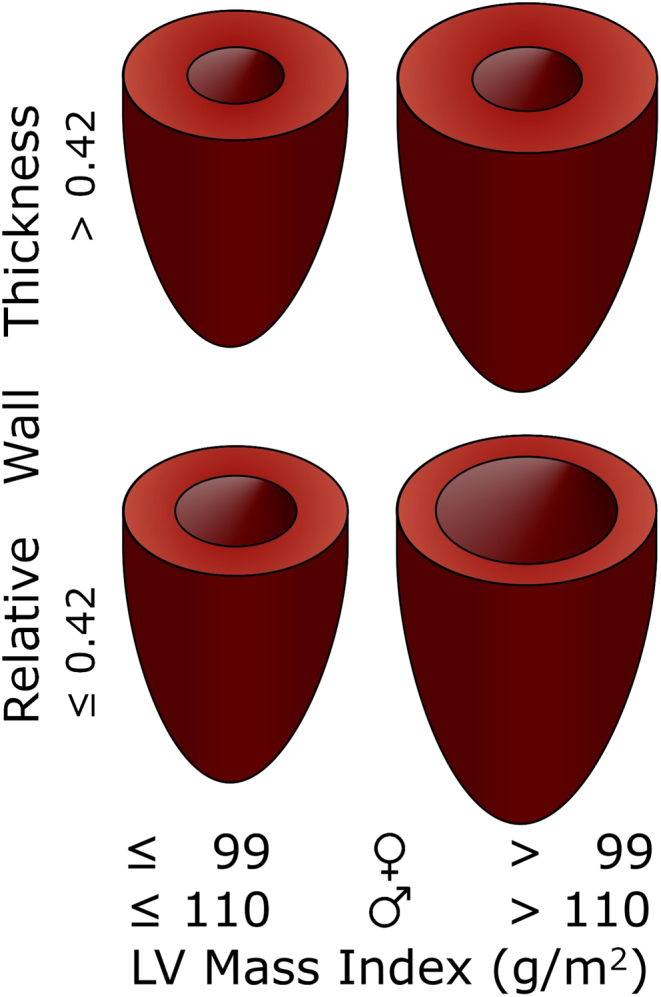
LV geometry determined by indexed LV mass and relative wall thickness.
A common misconception is that concentric LVH is synonymous with uniform thickening of the myocardial walls. It is possible to have localised or focal areas of increased wall thickness in patients with concentric LVH, just as there may be uniform thickening of muscle in patients with eccentric LVH.
If LV mass is normal (i.e. the patient does not have LVH), an RWT > 0.42 demonstrates the presence of ‘concentric remodelling’. This can be thought of as a pre-hypertrophy state and may help to identify individuals who would benefit from identification and optimization of risk factors (i.e. hypertension) (6).
Left ventricular volumes
Reference intervals for LV volumes are presented in Table 3. Left ventricular volumes should be obtained using 2D imaging from the apical 4- and 2-chamber windows using the biplane Simpson’s method. When obtaining LV volumes using the biplane method, care should be taken to ensure that the apical 4- and 2-chamber windows are separated by 60° of rotation (and not 90° as is sometimes assumed). In addition, it is paramount that the LV is not foreshortened. Volumes should be reported after indexing to BSA.
Table 3.
Left ventricular volumes.
| Normal | Mildly dilated | Moderately dilated | Severely dilated | |
|---|---|---|---|---|
| Males | ||||
| LVEDVi (mL/m2) | 30–79 | 80–91 | 92–103 | >103 |
| LVESVi (mL/m2) | 9–31 | 32–36 | 37–42 | >42 |
| LVEDV (mL) | 53–156 | – | – | – |
| LVESV (mL) | 15–62 | – | – | – |
| Females | ||||
| LVEDVi (mL/m2) | 29–70 | 71–81 | 82–91 | >91 |
| LVESVi (mL/m2) | 8–27 | 28–32 | 33–37 | >37 |
| LVEDV (mL) | 46–121 | – | – | – |
| LVESV (mL) | 13–47 | – | – | – |
Volumes obtained using the biplane Simpson’s method.
LVEDV(i), left ventricular end-diastolic volume (indexed); LVESV(i), left ventricular end-systolic volume (indexed).
Left ventricular ejection fraction
Summary
Reference intervals for LVEF are the same for males and females (Table 4).
LVEF should be derived from 2D volume data using the biplane Simpson’s method.
Normal LVEF is defined as an EF ≥55%.
Patients with an LVEF between 50 and 54% are defined as having ‘borderline low LVEF’.
Patients with an LVEF between 36 and 49% are defined as having ‘impaired LVEF’. The BSE discourages use of the terms ‘mild’ or ‘moderate’.
These reference intervals do not apply to values of LVEF obtained using 3D imaging. If EF is obtained using 3D imaging, these should be compared to vendor-specific reference intervals.
Table 4.
Left ventricular ejection fraction.
| Severely impaired LVEF | Impaired LVEF | Borderline low LVEF | Normal LVEF | |
|---|---|---|---|---|
| Males and females | ||||
| LVEF (%) | ≤35% | 36–49% | 50–54% | ≥55% |
LVEF derived using the biplane Simpson’s method.
Rationale and discussion
LVEF should be derived using the biplane Simpson’s method from 2D volumes, obtained from the apical 4- and 2-chamber views as described above. It is essential that values for LVEF are not derived from foreshortened or poorly obtained volumetric data. The BSE has chosen to keep reference intervals the same for males and females (Table 4).
Within the NORRE dataset, there was a statistically significant difference between males and females with regards to ejection fraction values (8). For males, the lower reference limit was 53.5%, whereas for females, the value was 54.5%. The P value for the difference between men and women was 0.009. Despite the statistical difference between genders, the absolute difference is so small as to be clinically insignificant. It would be very unusual to report echocardiographic-derived EF values with a purported accuracy of 1%: accepted inter-operator variability of LVEF measurements are often in the order of 5%. Additionally, for men and women alike, there was a statistically significant increase in LVEF with aging: for women under 40 years of age, the lower reference limit was 53.9%, whereas for women over 60 years of age, this limit was 55.1%. Again, for practical purposes, these differences are clinically insignificant.
Given this, the BSE chose to keep LVEF reference intervals the same for men and women, with normal LVEF defined as a value ≥55%.
The BSE chose to define ‘severely impaired LVEF’ as an LVEF ≤35% for both males and females. This is in contrast to the joint ASE/EACVI guidance, which classifies ‘severely abnormal LVEF’ as <30% (5, 6). The rationale for the BSE decision is one of clinical utility. There is a large body of evidence demonstrating that therapeutic drugs used in the management of left ventricular systolic dysfunction are of prognostic value when LVEF is ≤35%. This includes ACE-inhibitors, B-blockers, mineralocorticoid receptor antagonists, angiotensin receptor antagonists, If-channel inhibitors, and angiotensin receptor-neprilysin inhibitors (29, 30, 31, 32, 33, 34, 35, 36, 37, 38). Furthermore, in UK practice, device therapy for heart failure, including CRT and ICD, are also indicated when the LVEF is 35% or below (38, 39, 40, 41). Although it is true to state that a lower ejection fraction is associated with a poorer prognosis (13), there are no additional therapeutic interventions either mandated or available only after LVEF falls below 30%. For these reasons, in the opinion of the BSE, the most useful threshold for severely impaired LVEF is ≤35% as this provides clarity for clinicians and sonographers alike.
A change is also advocated for LVEF values between 35 and 55%. The BSE has chosen to depart from the tradition of splitting this group into ‘mild’ or ‘moderate’ bands and have defined individuals with an EF between 50 and 54% as ‘borderline low LVEF’, and those patients with values between 36 and 49% as ‘impaired LVEF’. The rationale for this approach is as follows.
As outlined in the ‘defining reference limits’ section, the method by which the LRL for LVEF is calculated means that 2.3% of normal individuals will fall below the threshold and may consequently (and incorrectly) be labelled as having LV systolic impairment. This can have important consequences upon that individual: for example, with regards obtaining life insurance, or impacting career decisions. However, it is also true to state that within this cohort there are patients whose prognosis is constrained (42). Too much emphasis has been placed on LVEF as the sole arbiter of normal systolic function. Just as no one parameter defines diastolic function, LVEF similarly cannot provide a binary normal/abnormal cut off for systolic function. The BSE has therefore highlighted that patients with an EF between 50 and 54% have ‘borderline low LVEF’. The sonographer and clinician require more information before labelling such a patient as having normal or abnormal systolic function. This is akin to the traffic light system advocated for MRI reference intervals derived from the UK biobank cohort (43). Additional information to help determine whether a patient is normal may include LV volumes and tissue Doppler imaging (s′ and e′), prior echo reports, clinical history, cardiovascular symptoms, family history, and a functional assessment. Recommending repeating the echo after a 6–12-month interval may be required.
Once LVEF falls below 50%, this corresponds to three standard deviations below the mean. It is therefore exceptionally unlikely that a normal individual would have an EF below this value (fewer than 0.15% of the normal population). As such, those patients with values between 36 and 49% should all be classed as having ‘impaired LVEF’ and the ejection fraction quoted. All patients within the ‘impaired LVEF’ cohort have reduced left ventricular systolic function and such a finding should prompt a comprehensive clinical assessment and discussion with the patient.
An LVEF of 50% has important implications in both heart failure and valvular heart disease management, re-enforcing the use of this threshold as a clinically relevant cut-off. When the LVEF is below 50%, there remains a reasonable body of evidence that therapeutic agents may be of value in improving survival (44, 45, 46). Similarly, observational data have suggested that cardiovascular survival and outcomes are significantly poorer once LVEF is lower than 50% (42). A cut-off for LVEF of 50% therefore ensures that all individuals who may benefit from heart failure therapy are included in the ‘impaired LVEF’ group. This range is similar to that proposed by the European Society of Cardiology who have defined a ‘heart failure with mid-range ejection fraction’ group in whom it is reasonable to consider medical therapy whilst accepting that further research is required (38, 47). Conversely, even in patients with clinical heart failure and LVEF values of >50% (heart failure with preserved ejection fraction; HFpEF), there is no evidence to support that routine use of heart failure medications improves survival (38).
The BSE discourages use of the terms ‘mild’ or ‘moderate’ reduction in LVEF.
Previously, inter-observer variation would often result in patients alternating between the mild and moderate categories without this having any clinical meaning. The current methodology will hopefully allow more consistency with regards reporting within the range of LVEF between 36 and 49%.
With regards 3D volumetric assessment and 3D-derived ejection fraction, the BSE stresses that reference intervals for 2D-derived ejection fraction do not apply to 3D results: for example, an ejection fraction of 56% derived using 3D software is not necessarily normal, and comparison with vendor-specific reference intervals should be used.
Left atrial size
Summary
Reference limits for LA volume are the same for males and females.
LA volume should be obtained from apical 4- and 2-chamber windows using the biplane Simpson’s method and indexed for BSA.
An LA volume index (LAVi) of <34 mL/m2 is normal.
An LAVi between 34 and 38 mL/m2 is a borderline result.
An LAVi of >38 mL/m2 is abnormal.
The area-length (A-L) method should not be used interchangeably with the Simpson’s method. BSE reference intervals for LA volume do not apply to values obtained using the A-L method.
Routine use of linear LA dimensions is not encouraged, but may be used in some clinical scenarios.
Rationale and discussion
Reference limits for left atrial size are presented in Table 5. LA volume should be obtained from apical 4- and 2-chamber windows (separated by 60° of rotation), optimised for LA assessment, using the biplane Simpson’s method. Maximal LA volume should be obtained from the frame immediately prior to mitral valve opening. Values should be reported after indexing for BSA.
Table 5.
LA volume.
| Normal | Borderline | Dilated | |
|---|---|---|---|
| Males and females | |||
| LAVi (ml/m2) | <34 | 34–38 | >38 |
LA volume obtained using biplane Simpson’s method.
Although absolute LA volumes are usually larger in males than females, this difference is entirely neutralised when indexing for BSA. As such, routine assessment of indexed LA volumes allows a single reference limit for both males and females to be utilized (8). Indexed LA volumes are linked to adverse prognosis and poor cardiovascular outcomes, supporting the routine use of this measure in patients (15, 16, 48, 49, 50, 51, 52).
There were two particularly interesting observations reported within the NORRE dataset. Firstly, the NORRE investigators examined two widely used but differing methods to assess LA volume on all included subjects: the biplane method of discs (Simpson’s method) and the biplane area-length method. Consistent with earlier comparative studies of these two methods, NORRE demonstrated that the area-length technique produces values for LA volume systematically larger than those obtained using the Simpson’s method (8, 53). Given this, it is evident that these two methodological approaches to the assessment of LA volume are not inter-changeable as is often assumed, and different reference limits should be applied to each.
Unfortunately, this observation creates a number of potential conflicts in echocardiographic practice, as previous guidelines from the ASE, EACVI and BSE have not differentiated between these two methods. For example, when assessing for diastolic dysfunction, an LAVi of >34 mL/m2 is one marker for the presence of elevated filling pressures (54). It is possible, therefore, that an individual could have an LAVi above this limit if the area-length method were used, but below this limit if the Simpson’s method were chosen.
The second interesting observation from NORRE is that LA volumes in the normal population were significantly larger than previous work has suggested, which appears to conflict with the published association between increased LA volumes and poor prognosis. From the NORRE data, the upper reference limit for LAVi using the Simpson’s method is 38 mL/m2 and using the area-length method it is 42 mL/m2. For comparison, in previous observational work of unselected patients, an LAVi of >40 mL/m2 (obtained using the area-length method) is associated with considerably poorer survival. Even those subjects with an LAVi of >34 mL/m2 have significantly worse outcomes (16).
The explanation for this discrepancy is not clear. Although it is well recognized that athletes can develop enlarged atria, the NORRE protocol excluded such individuals from the study (7, 24, 55). Nor does it seem likely that undiagnosed diastolic dysfunction is an explanation: the proportion of individuals with an LAVi of >34 mL/m2 was similar across the age categories.
Given the robust nature of patient inclusion and echo analysis, the NORRE results are compelling and strongly suggest that the range of normality for LA volume is larger than previously thought. The results also suggest that there is a substantial overlap between physiological and pathophysiological LA remodelling.
The BSE has chosen to advocate a compromise approach that acknowledges the results of NORRE, but also ensures that an LA volume sufficient for identifying patients with diastolic dysfunction is highlighted.
A consensus view was therefore achieved within the writing committee. Using the biplane Simpson’s method, normal LAVi is ≤34 mL/m2. Values between 34 and 38 mL/m2 should be considered ‘borderline’: as an isolated finding such a result is normal. In the presence of additional indicators for diastolic dysfunction, for example, an elevated E/e′, an LAVi within this range should be considered a marker of elevated filling pressures. An LAVi of more than 38 mL/m2 is enlarged.
Finally, the BSE does not advocate the routine use of linear LA dimensions, although left atrial diameter may still be used in some clinical scenarios, including risk-assessment in hypertrophic cardiomyopathy (56).
The right heart
Summary
The BSE advocates the routine use of indexed right ventricular end-diastolic (RVED) area, and indexed RA area.
Conventional linear measurements including RV basal diameter (RVD1) and right ventricular outflow tract diameter (RVOT) should additionally be obtained in all patients.
Updated reference limits for linear dimensions are substantially different from previous BSE guidance and contemporary joint ASE/EACVI guidelines.
Rationale and discussion
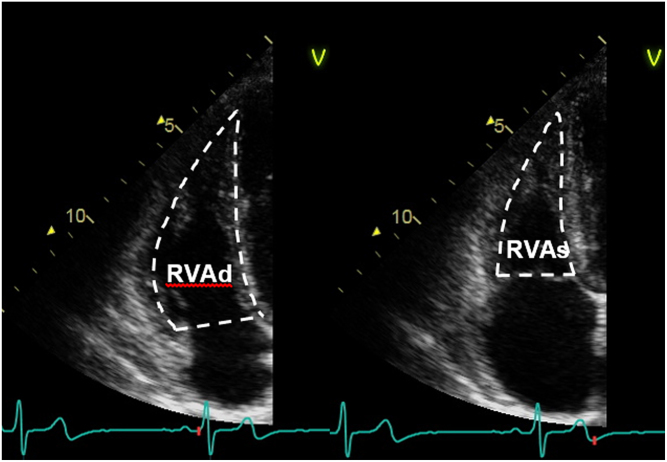
For the first time, the BSE is advocating use of indexed parameters in the routine assessment of both right ventricular (RV) and right atrial (RA) size. These parameters are the indexed right ventricular end-diastolic (RVED) area (Fig. 3) and the indexed RA area. This proposed methodology acknowledges that the right heart varies according to body habitus and brings echocardiographic reporting of right heart size more in keeping with the accepted method of reporting left heart chamber size. These newer measures should be combined with conventional linear assessment in all patients. Conventional measures include the RV outflow tract (RVOT) dimensions, obtained from the parasternal short axis (PSAX) window (Fig. 4), and RV body dimensions (Fig. 5), which should be obtained from the RV-focussed view. Remember that the RV-focussed view is not necessarily the same as the standard 4-chamber view, but is adjusted such that the diameter of the RV is maximised, whilst keeping the imaging plane through the centre of the LV cavity (4).
Figure 3.
Assessment of RV size and fractional area change (FAC). From the RV-focussed apical 4-chamber window, a contour should be traced from the lateral tricuspid annulus along the free wall to the apex, and back along the interventricular septum to the medial tricuspid valve annulus. This should be undertaken at end-diastole (left panel), and the area indexed to BSA, providing us with indexed RV end-diastolic area. This process can be repeated in end-systole (right panel), from which we can derive the FAC as follows: FAC = (RVA diastole − RVA systole)/RVA diastole × 100%.
Figure 4.
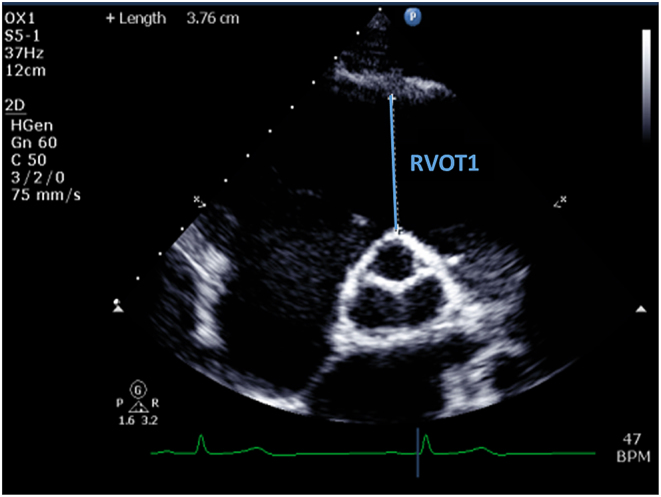
RVOT assessment (RVOT1). From the PSAX window, and in end-diastole, measurement should be made from the anterior aortic wall directly up to the RVOT free wall (at the level of the aortic valve). The PSAX view is more reproducible than RVOT PLAX.
Figure 5.
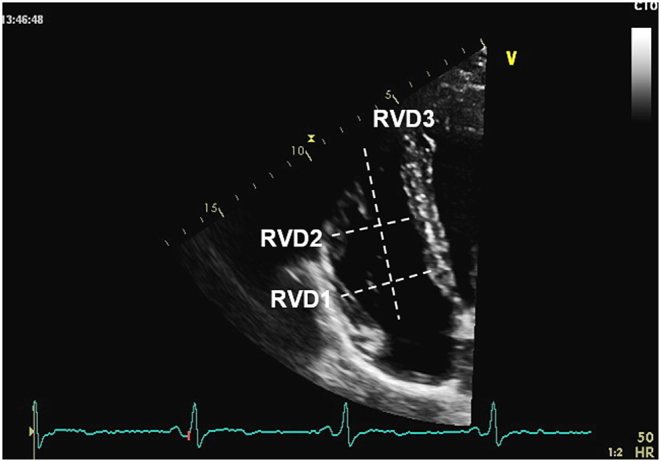
RV body measurements. All measurements should be obtained at end-diastole in the RV-focused apical 4-chamber view. RVD1: Basal RV diameter. Measured at the maximal transverse diameter in the basal one third of the RV. RVD2: Mid RV diameter measured at the level of the LV papillary muscles. RVD3: RV length, from the plane of the tricuspid annulus to the RV apex.
Reference limits for right heart measurements and fractional area change (FAC) are presented in Table 6.
Table 6.
Right heart parameters.
| Normal | |
|---|---|
| Males | |
| Indexed values | |
| RVED area (cm2/m2) | ≤13.6 |
| RA area (cm2/m2) | ≤11 |
| Absolute values | |
| RVOT proximal (mm) | 24–44 |
| RVOT distal (mm) | 16–29 |
| RVD1 (mm) | 26–47 |
| RVD2 (mm) | 19–42 |
| RVD3 (mm) | 55–87 |
| RA area (cm2) | ≤22 |
| Right heart function | |
| FAC (%) | ≥30 |
| Females | |
| Indexed values | |
| RVED area (cm2/m2) | ≤12.6 |
| RA area (cm2/m2) | ≤11 |
| Absolute values | |
| RVOT proximal (mm) | 20–42 |
| RVOT distal (mm) | 14–28 |
| RVD1 (mm) | 22–43 |
| RVD2 (mm) | 17–35 |
| RVD3 (mm) | 51–80 |
| RA area (cm2) | ≤19 |
| Right heart function | |
| FAC (%) | ≥35 |
FAC, fractional area change; RA, right atrial; RVD1, right ventricular basal diameter in diastole; RVD2, right ventricular mid-point diameter in diastole; RVD3, right ventricular length in diastole; RVED, right ventricular end-diastolic area, obtained from the RV-optimised apical 4-chamber view; RVOT distal, right ventricular outflow tract at the level of the pulmonary valve from the parasternal short axis window; RVOT proximal, proximal right ventricular outflow tract obtained from the parasternal short axis view.
The anatomy of the right heart, and RV in particular, is complex. All three components of the RV cannot be visualised from a single echocardiographic plane and therefore it is imperative that sonographers do not rely on a single measure to define the presence or absence of RV enlargement. Moreover, in some patients there can be relative enlargement of one RV component (for example, the outflow tract), whereas the main body of the RV may be normal. To account for this complexity, the BSE suggests that indexed RVED area is combined with basal RV dimensions and an assessment of RVOT size in all patients.
The BSE accepts that routine indexing of right heart parameters is not yet widespread, and indeed these measurements are not included within the BSE minimum dataset (28). However, indexed parameters account for both gender and body habitus and are physiologically more robust. The NORRE study obtained indexed right heart parameters within its dataset, from which the BSE propose an upper reference limit for indexed RVED area of 13.6 cm2/m2 (males) and 12.6 cm2/m2 (females), with an upper reference limit for indexed RA area of 11 cm2/m2 for both men and women.
A potential limitation of indexed right heart area parameters is that the inter-observer variability is inferior to conventional linear measurements (8). For this reason, the BSE advocates that the indexed area is combined with conventional linear measures in all patients.
Reference limits for linear dimensions have also been updated using the NORRE data. With regards the RV basal diameter (RVD1), the BSE defines the upper reference limit for males as 47 mm, whereas for females the URL is 43 mm. These values are larger than the currently published reference limit of 41 mm for both men and women. The ASE defined the current value in 2010, using pooled data from 10 studies, including a combined total of 376 individuals (4). The most contemporaneous joint American and European guidance derived most right heart dimensions from fewer than 700 subjects (5, 6). The NORRE dataset by itself includes more than 700 individuals, in addition to having the benefits of consistency of inclusion and analysis outlined previously. Furthermore, the ASE/EACVI upper reference limit for RV size is universal (i.e. the same for both males and females), thereby suggesting that gender (and by inference, BSA) does not influence RV size, which seems fundamentally unlikely. The 2010 ASE guidance published a range of potential values for the upper reference limit, acknowledging that there is a degree of uncertainty in any statistical modelling (4). This range was 39–45 mm, and 41 mm was the mid-point of this range. Using NORRE the combined URL for men and women was 43.7 mm, which falls within this previously published range, confirming that the current values are not dramatically different from what may have been expected.
The upper reference limit for the RV mid-point diameter is now 42 mm (males) and 35 mm (females). Again, these are slightly larger than the previous guidance, but for all the reasons outlined above, there is no fundamental conflict with previously published data.
The RVOT should be measured using 2D imaging from the PSAX window. Using the NORRE dataset, the upper reference limits for the RVOT demonstrate substantial differences from previously accepted guidelines: in males the URL is 44 mm, whereas for females it is 42 mm. This is larger than previously described, when the universal cut-off for both men and women was 35 mm. It is not immediately apparent why the current results appear to be larger than earlier work had suggested. For the distal RVOT, the current reference limits are very similar to previously published guidance.
RV fractional area change is a useful tool to assess RV function. NORRE demonstrated that there is a significant difference between men and women with regards values for FAC: for males the lower reference limit is 30% whereas for females it is 35%.
Clinical implications
Two potential clinical impacts of the new reference intervals for the right heart are in the echocardiographic assessment of pulmonary hypertension (PH) and arrhythmogenic right ventricular cardiomyopathy (ARVC).
A major criterion for the diagnosis of ARVC is the presence of regional RV wall motion abnormalities, combined either with impaired RV function (defined as an FAC of ≤33%), or an enlarged RV. This latter was defined as an RVOT proximal diameter of ≥36 mm measured from the PSAX window (57). It appears challenging to rationalize this major criterion with the new reference intervals for the RV. However, size of the RVOT in and of itself is not sufficient to qualify as a major criterion for the diagnosis of ARVC. Regional wall motion abnormalities of the RV are the pre-requisite finding, and only when these are seen does size subsequently play a role. Similarly, minor criteria for the diagnosis of ARVC include an RVOT diameter of between 32 and 36 mm or a fractional change of ≤40% (both in the context of regional abnormalities of RV contractility). These minor criteria for RVOT dimensions and RV function both fall within the previously published reference limits. The apparent conflict between the current reference intervals and diagnosis of ARVC is therefore not new.
With regards pulmonary hypertension, recent guidance by the BSE mirrors earlier work from the EACVI (58, 59). The principle of the PH guidance is to quantify the likelihood of pulmonary hypertension being present, rather that reporting absolute values of pulmonary artery (PA) pressure. The probability of PH is based primarily upon the tricuspid regurgitation (TR) maximal velocity, although the presence of two additional echo characteristics can subsequently increase the likelihood of pulmonary hypertension being present. Most of these additional echo characteristics are unaffected by the new right heart reference limits. The exception is a right atrial area of >18 cm2, which would now be defined as a normal finding within the current reference intervals for both males and females.
We believe that this guideline change is exceptionally unlikely to affect clinical practice. According to the NORRE data, fewer than 5% of males, and an estimated 3% of normal females would be expected to have an RA area of >18 cm2. In these individuals, it would need further supportive echo evidence of PH to potentially alter the overall likelihood of pulmonary hypertension being present. These additional echo characteristics are also very unlikely to occur in normal individuals: for example, a pulmonary acceleration time of <105 ms would be expected to occur in fewer than 2.5% of normal patients. Therefore, the combined probability of both an RA area >18 cm2 and a pulmonary acceleration time <105 ms occurring by chance in a normal individual is less than 1 in 1000.
Although the reference intervals for linear right heart dimensions do vary from historic guidance, this likely reflects that the source of previous data was somewhat limited, and NORRE has substantially increased our understanding of normal right heart chamber dimensions. Remember, even though the upper limit for RV size has now increased, if the RV is seen to be larger than the left ventricle, this should prompt further consideration.
Aortic dimensions
Summary
Aortic dimensions should be measured using 2D imaging from the PLAX window.
Indices should be obtained using the inner-edge to inner-edge (IE-IE) methodology in end-diastole, defined as the onset of the QRS complex.
All values should be indexed to height and not BSA.
For those echo labs that currently employ the leading-edge to leading-edge (LE-LE) technique, it is reasonable to continue doing so for continuity and consistency.
The BSE suggests that echo labs include the method of assessment within the echo report to ensure transparency for clinicians.
Rationale and discussion
Reference limits for the recommended measurements for aortic root dimensions are presented in Table 7. Aortic dimensions should be obtained using the IE-IE technique in end-diastole, defined as the onset of the QRS complex (Fig. 6). Aortic indices should be indexed for height and not BSA as was previously recommended.
Table 7.
Normal indexed aortic root dimensions.
| Male | Female | |
|---|---|---|
| Sinus of Valsalva (mm/m) | 13.8–21.8 | 13.1–20.7 |
| Sino-tubular junction (mm/m) | 11.4–18.6 | 11.0–17.8 |
| Proximal ascending aorta (mm/m) | 11.5–19.9 | 11.4–19.8 |
Inner edge to inner edge methodology; indexed to height; obtained in end-diastole (onset of QRS). Proximal ascending aorta measures obtained 1 cm above the sino-tubular junction.
Figure 6.
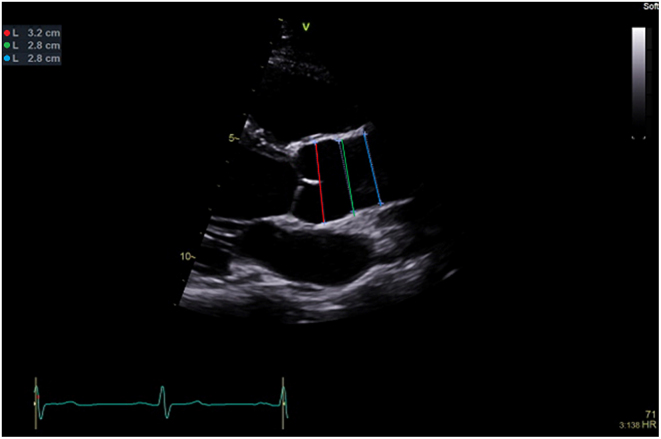
Assessment of aortic root dimensions. The measurements should be obtained using the inner-edge to inner-edge methodology in end diastole (defined as the onset of the QRS). Measurements should be obtained at three levels including: sinus of Valsalva (red line); sino-tubular junction (green line); proximal ascending aorta defined as the region 1 cm above the sino-tubular junction (blue line). If there is enlargement above this level the maximal dimension should be measured and stated in report. Measurements should be reported after indexing for height.
Historical measurements of aortic root size used the LE-LE methodology owing to the poor resolution available at the time. This dimension is neither the outer nor the inner size of the aorta, but has resulted in reference values and cut-offs for therapy (such as aortic root replacement) that are embedded in contemporary guidance (60). Conversely, there is evidence that measurements of the aortic root using the IE-IE methodology is more readily obtained and more reproducible (61). Previous BSE guidance has advocated the IE-IE technique, and therefore, to maintain consistency, the current guidance advises ongoing use of this approach. The BSE suggests that echo labs document how aortic root dimensions are obtained within echo reports, particularly if a decision has been made to alter the methodological approach.
On average, aortic dimensions are 1.2 mm smaller when using IE-IE compared to LE-LE. The BSE believes that this is unlikely to have a significant impact on clinical decision-making: patients who are close to the cut-off for surgery invariably undergo additional imaging such as CT or MRI. These modalities can confirm the true maximal aortic size, but also have the advantage of being able to visualise the entire aorta (a necessary step before surgery) and obtain a true co-axial slice through the aorta. CT also has the potential to obtain information on the coronary arteries, which may avoid the need for invasive angiography.
The aorta should be measured at end-diastole, as this measurement is more reproducible, at least in part owing to the clear timing reference, whereas mid-systole is less easy to define (61). This will make echo surveillance with sequential measurements of a dilating aorta more reproducible. Aortic dimensions obtained in diastole are consistently smaller than corresponding measurements made in systole (10, 61). If the aorta in question is approaching the point at which intervention is required, the BSE suggests that corroborative measurements are made with an additional imaging modality.
Traditionally, nomograms have been used to present reference intervals in a visually appealing way as it varies against a dependent variable, such as BSA. The aortic root diameter has been compared against three age-specific nomograms derived from a single paper by Roman et al. (62). Despite the authors’ recommending the use of their nomogram for children only, the adult versions have been included in virtually all chamber guidelines and textbooks ever since (5, 6, 63, 64). These adult nomograms have some limitations: small sample size, poorly defined ‘normal’ subjects, bias to BSA (which is adversely affected by obesity), and finally a sharp jump in results when the subject turns 40 owing to a change in the equation used. These problems have been well described elsewhere (65).
In the subsequent 25 years, many studies have attempted to improve on this. Devereux et al. have derived equations for aortic root dimensions from 1207 apparently normal subjects (66). However, the data were derived from a mixture of studies, including the original Roman group. The methodology was not pre-specified, with the aortic root occasionally measured from the apical three-chamber view, which is not used routinely in practice and is unlikely to be comparable to results from the parasternal long-axis window.
The NORRE dataset obtained data for normal aortic root values at four different levels, including the Sinus of Valsalva, the ST-junction, and the proximal ascending aorta (also referred to as the tubular ascending aorta) using both LE-LE and the IE-IE methodology. Additionally, NORRE obtained data for aortic dimensions both in end-diastole (defined as the onset of the QRS complex) and mid-systole, which corresponds to maximal aortic dimensions (10). Consequently, there is a vast array of data from which reference limits can be derived.
NORRE, along with earlier work by Oxborough et al., demonstrated that aortic root dimensions are best correlated to height and not BSA (10, 61). This is a change from the currently accepted practice and will have potential benefits in overweight individuals. Indexing to height also results in similar reference limits for younger and older individuals alike and therefore greatly simplifies the reference intervals.
For those echo departments currently utilising the LE-LE methodology, it is reasonable to continue this practice for consistency. New reference limits for the LE-LE methodology are presented in Table 8.
Table 8.
Normal indexed aortic root dimensions (leading edge-leading edge methodology).
| Male | Female | |
|---|---|---|
| Sinus of Valsalva (mm/m) | 14.8–23.2 | 14.1–22.1 |
| Sino-tubular junction (mm/m) | 12.6–19.8 | 12.2–19.4 |
| Proximal ascending aorta (mm/m) | 12.6–21.4 | 12.3–21.1 |
Leading edge to leading edge methodology; indexed to height; obtained in end-diastole (onset of QRS). Proximal ascending aorta measures obtained 1 cm above the sino-tubular junction.
Tissue Doppler imaging
Tissue Doppler imaging (TDI) is a useful technique that is both robust and reproducible. Values for the left heart should be obtained as the average of medial and lateral mitral annular systolic velocities, and obtained during a breath hold in end-expiration. Values are similar for both men and women, but vary according to age (Table 9).
Table 9.
Normal tissue Doppler parameters.
| Normal | |
|---|---|
| Males and females | |
| Mean mitral annular s′ (cm/s) | |
| 20–40 years | ≥6.4 |
| 40–60 years | ≥5.7 |
| >60 years | ≥4.9 |
| RV s′ (cm/s) | |
| All ages | ≥9 |
Right ventricular TDI values should be obtained from the lateral RV annulus. RV indices are similar for males and females and do not vary significantly according to age (Table 9).
Strain values
The BSE has chosen not to include reference limits for strain parameters. Unfortunately, there is still significant inter-vendor variability, such that a single reference interval would not suffice for all practitioners. Additionally, it is not clear whether different versions of strain software give comparable results. Individual vendors currently provide reference intervals for specific platforms and software versions.
Despite this, strain imaging is more widespread and has increasing clinical utility in echocardiographic practice. Strain tools are of value when used sequentially on a single individual in order to help identify whether there have been subclinical changes in LV performance. Such an example would be when monitoring the effect of chemotherapy on LV systolic function (67). Given the current vendor- and even software-version variations in strain, it is important that this is documented in the report and every effort made to provide continuity between assessments. If a vendor’s measurement tools are upgraded, old studies should be re-measured before they are used for comparison.
Summary
The BSE believe that the current guidance provides robust reference intervals for use in day-to-day practice in UK echo labs. This report contains guidance only and should also be used in conjunction with clinical assessment and interpretation. The reference intervals within should not be used as the sole reason for making clinical decisions for individual patients.
Supplementary Material
Declaration of interest
David Oxborough and Vishal Sharma are members of the editorial board of Echo Research and Practice. They were not involved in the editorial or peer review process of this paper, on which they are listed as authors. The other authors have nothing to disclose.
Funding
This work did not receive any specific grant from any funding agency in the public, commercial or not-for-profit sector.
Acknowledgements
The authors’ would like to thank Dr Mark Belham for his thoughts and assistance, and the Education Committee of the British Society for Echocardiography for their support. They also acknowledge the authors of NORRE who provided clarification of their published data in order for us to finalise the BSE reference limits.
References
- 1.British Society of Echocardiography. EchoCalc for iPhone. London, UK: British Society of Echocardiography, 2015. (available at: https://apps.apple.com/us/app/echocalc/id468166426) [Google Scholar]
- 2.British Society of Echocardiography. EchoCalc for android. London, UK: British Society of Echocardiography, 2014. (available at: https://play.google.com/store/apps/details?id=bse.echocalc) [Google Scholar]
- 3.Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, Picard MH, Roman MJ, Seward J, Shanewise JS, et al Recommendations for chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. Journal of the American Society of Echocardiography 2005. 18 1440–1463. ( 10.1016/j.echo.2005.10.005) [DOI] [PubMed] [Google Scholar]
- 4.Rudski LG, Lai WW, Afilalo J, Hua L, Handschumacher MD, Chandrasekaran K, Solomon SD, Louie EK, Schiller NB. Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. Journal of the American Society of Echocardiography 2010. 23 685–713; quiz 786. ( 10.1016/j.echo.2010.05.010) [DOI] [PubMed] [Google Scholar]
- 5.Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, Flachskampf FA, Foster E, Goldstein SA, Kuznetsova T, et al Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Journal of the American Society of Echocardiography 2015. 28 1.e14–39.e14. ( 10.1016/j.echo.2014.10.003) [DOI] [PubMed] [Google Scholar]
- 6.Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, Flachskampf FA, Foster E, Goldstein SA, Kuznetsova T, et al Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. European Heart Journal: Cardiovascular Imaging 2015. 16 233–270. ( 10.1093/ehjci/jev014) [DOI] [PubMed] [Google Scholar]
- 7.Lancellotti P, Badano LP, Lang RM, Akhaladze N, Athanassopoulos GD, Barone D, Baroni M, Cardim N, Gomez De Diego JJ, Derumeaux G, et al Normal reference ranges for echocardiography: rationale, study design, and methodology (NORRE study). European Heart Journal: Cardiovascular Imaging 2013. 14 303–308. ( 10.1093/ehjci/jet008) [DOI] [PubMed] [Google Scholar]
- 8.Kou S, Caballero L, Dulgheru R, Voilliot D, De Sousa C, Kacharava G, Athanassopoulos GD, Barone D, Baroni M, Cardim N, et al Echocardiographic reference ranges for normal cardiac chamber size: results from the NORRE study. European Heart Journal: Cardiovascular Imaging 2014. 15 680–690. ( 10.1093/ehjci/jet284) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Caballero L, Kou S, Dulgheru R, Gonjilashvili N, Athanassopoulos GD, Barone D, Baroni M, Cardim N, Gomez De Diego JJ, Oliva MJ, et al Echocardiographic reference ranges for normal cardiac Doppler data: results from the NORRE study. European Heart Journal: Cardiovascular Imaging 2015. 16 1031–1041. ( 10.1093/ehjci/jev083) [DOI] [PubMed] [Google Scholar]
- 10.Saura D, Dulgheru R, Caballero L, Bernard A, Kou S, Gonjilashvili N, Athanassopoulos GD, Barone D, Baroni M, Cardim N, et al Two-dimensional transthoracic echocardiographic normal reference ranges for proximal aorta dimensions: results from the EACVI NORRE study. European Heart Journal Cardiovascular Imaging 2017. 18 167–179. ( 10.1093/ehjci/jew053) [DOI] [PubMed] [Google Scholar]
- 11.Poppe KK, Doughty RN, Gardin JM, Hobbs FDR, McMurray JJV, Nagueh SF, Senior R, Thomas L, Whalley GA, Aune E, et al Ethnic-specific normative reference values for echocardiographic LA and LV size, LV mass, and systolic function: the EchoNoRMAL study. JACC: Cardiovascular Imaging 2015. 8 656–665. ( 10.1016/j.jcmg.2015.02.014) [DOI] [PubMed] [Google Scholar]
- 12.Fisher RA. Statistical methods for research workers. 4th edn. Edinburgh, UK: Oliver & Boyd, 1932. [Google Scholar]
- 13.Solomon SD, Anavekar N, Skali H, McMurray JJV, Swedberg K, Yusuf S, Granger CB, Michelson EL, Wang D, Pocock S, et al Influence of ejection fraction on cardiovascular outcomes in a broad spectrum of heart failure patients. Circulation 2005. 112 3738–3744. ( 10.1161/CIRCULATIONAHA.105.561423) [DOI] [PubMed] [Google Scholar]
- 14.Chubb H, Simpson JM. The use of Z-scores in paediatric cardiology. Annals of Pediatric Cardiology 2012. 5 179–184. ( 10.4103/0974-2069.99622) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tsang TSM, Barnes ME, Gersh BJ, Bailey KR, Seward JB. Left atrial volume as a morphophysiologic expression of left ventricular diastolic dysfunction and relation to cardiovascular risk burden. American Journal of Cardiology 2002. 90 1284–1289. ( 10.1016/s0002-9149(02)02864-3) [DOI] [PubMed] [Google Scholar]
- 16.Tsang TSM, Abhayaratna WP, Barnes ME, Miyasaka Y, Gersh BJ, Bailey KR, Cha SS, Seward JB. Prediction of cardiovascular outcomes with left atrial size: is volume superior to area or diameter? Journal of the American College of Cardiology 2006. 47 1018–1023. ( 10.1016/j.jacc.2005.08.077) [DOI] [PubMed] [Google Scholar]
- 17.Bonow RO, Dodd JT, Maron BJ, O'Gara PT, White GG, McIntosh CL, Clark RE, Epstein SE. Long-term serial changes in left ventricular function and reversal of ventricular dilatation after valve replacement for chronic aortic regurgitation. Circulation 1988. 78 1108–1120. ( 10.1161/01.cir.78.5.1108) [DOI] [PubMed] [Google Scholar]
- 18.Enriquez-Sarano M, Tajik AJ, Schaff HV, Orszulak TA, McGoon MD, Bailey KR, Frye RL. Echocardiographic prediction of left ventricular function after correction of mitral regurgitation: results and clinical implications. Journal of the American College of Cardiology 1994. 24 1536–1543. ( 10.1016/0735-1097(94)90151-1) [DOI] [PubMed] [Google Scholar]
- 19.Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Fleisher LA, Jneid H, Mack MJ, McLeod CJ, O'Gara PT, et al 2017 AHA/ACC focused update of the 2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice guidelines. Circulation 2017. 135 e1159–e1195. ( 10.1161/CIR.0000000000000503) [DOI] [PubMed] [Google Scholar]
- 20.Dewey FE, Rosenthal D, Murphy DJ, Jr, Froelicher VF, Ashley EA. Does size matter? Clinical applications of scaling cardiac size and function for body size. Circulation 2008. 117 2279–2287. ( 10.1161/CIRCULATIONAHA.107.736785) [DOI] [PubMed] [Google Scholar]
- 21.Paterick TE, Gordon T, Spiegel D. Echocardiography: profiling of the athlete’s heart. Journal of the American Society of Echocardiography 2014. 27 940–948. ( 10.1016/j.echo.2014.06.008) [DOI] [PubMed] [Google Scholar]
- 22.D’Ascenzi F, Pelliccia A, Solari M, Piu P, Loiacono F, Anselmi F, Caselli S, Focardi M, Bonifazi M, Mondillo S. Normative reference values of right heart in competitive athletes: a systematic review and meta-analysis. Journal of the American Society of Echocardiography 2017. 30 845.e2–858.e2. ( 10.1016/j.echo.2017.06.013) [DOI] [PubMed] [Google Scholar]
- 23.Oxborough D, Augustine D, Gati S, George K, Harkness A, Mathew T, Papadakis M, Ring L, Robinson S, Sandoval J, et al A guideline update for the practice of echocardiography in the cardiac screening of sports participants: a joint policy statement from the British Society of Echocardiography and Cardiac Risk in the Young. Echo Research and Practice 2018. 5 G1–G10. ( 10.1530/ERP-17-0075) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McClean G, George K, Lord R, Utomi V, Jones N, Somauroo J, Fletcher S, Oxborough D. Chronic adaptation of atrial structure and function in elite male athletes. European Heart Journal Cardiovascular Imaging 2015. 16 417–422. ( 10.1093/ehjci/jeu215) [DOI] [PubMed] [Google Scholar]
- 25.Regitz-Zagrosek V, Roos-Hesselink JW, Bauersachs J, Blomström-Lundqvist C, Cífková R, De Bonis M, Iung B, Johnson MR, Kintscher U, Kranke P, et al 2018 ESC guidelines for the management of cardiovascular diseases during pregnancy. European Heart Journal 2018. 39 3165–3241. ( 10.1093/eurheartj/ehy340) [DOI] [PubMed] [Google Scholar]
- 26.Mada RO, Lysyansky P, Daraban AM, Duchenne J, Voigt JU. How to define end-diastole and end-systole? Impact of timing on strain measurements. JACC: Cardiovascular Imaging 2015. 8 148–157. ( 10.1016/j.jcmg.2014.10.010) [DOI] [PubMed] [Google Scholar]
- 27.Voigt JU, Pedrizzetti G, Lysyansky P, Marwick TH, Houle H, Baumann R, Pedri S, Ito Y, Abe Y, Metz S, et al Definitions for a common standard for 2D speckle tracking echocardiography: consensus document of the EACVI/ASE/Industry Task Force to standardize deformation imaging. European Heart Journal: Cardiovascular Imaging 2015. 16 1–11. ( 10.1093/ehjci/jeu184) [DOI] [PubMed] [Google Scholar]
- 28.Wharton G, Steeds R, Allen J, Phillips H, Jones R, Kanagala P, Lloyd G, Masani N, Mathew T, Oxborough D, et al A minimum dataset for a standard adult transthoracic echocardiogram: a guideline protocol from the British Society of Echocardiography. Echo Research and Practice 2015. 2 G9–G24. ( 10.1530/ERP-14-0079) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.SOLVD Investigators, Yusuf S, Pitt B, Davis CE, Hood WB, Cohn JN. Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure. New England Journal of Medicine 1991. 325 293–302. ( 10.1056/NEJM199108013250501) [DOI] [PubMed] [Google Scholar]
- 30.Garg R, Yusuf S. Overview of randomized trials of angiotensin-converting enzyme inhibitors on mortality and morbidity in patients with heart failure. Collaborative Group on ACE Inhibitor Trials. JAMA 1995. 273 1450–1456. ( 10.1001/jama.273.18.1450) [DOI] [PubMed] [Google Scholar]
- 31.Pitt B, Zannad F, Remme WJ, Cody R, Castaigne A, Perez A, Palensky J, Wittes J. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. Randomized Aldactone Evaluation Study Investigators. New England Journal of Medicine 1999. 341 709–717. ( 10.1056/NEJM199909023411001) [DOI] [PubMed] [Google Scholar]
- 32CIBIS-II Investigators and Committees.The Cardiac Insufficiency Bisoprolol Study II (CIBIS-II): a randomised trial. Lancet 1999. 353 9–13. ( 10.1016/S0140-6736(98)11181-9) [DOI] [PubMed] [Google Scholar]
- 33.Packer M, Coats AJ, Fowler MB, Katus HA, Krum H, Mohacsi P, Rouleau JL, Tendera M, Castaigne A, Roecker EB, et al Effect of carvedilol on survival in severe chronic heart failure. New England Journal of Medicine 2001. 344 1651–1658. ( 10.1056/NEJM200105313442201) [DOI] [PubMed] [Google Scholar]
- 34.Granger CB, McMurray JJV, Yusuf S, Held P, Michelson EL, Olofsson B, Ostergren J, Pfeffer MA, Swedberg K. & CHARM Investigators and Committees. Effects of candesartan in patients with chronic heart failure and reduced left-ventricular systolic function intolerant to angiotensin-converting-enzyme inhibitors: the CHARM-Alternative trial. Lancet 2003. 362 772–776. ( 10.1016/S0140-6736(03)14284-5) [DOI] [PubMed] [Google Scholar]
- 35.Swedberg K, Komajda M, Böhm M, Borer JS, Ford I, Dubost-Brama A, Lerebours G, Tavazzi L. & SHIFT Investigators. Ivabradine and outcomes in chronic heart failure (SHIFT): a randomised placebo-controlled study. Lancet 2010. 376 875–885. ( 10.1016/S0140-6736(10)61198-1) [DOI] [PubMed] [Google Scholar]
- 36.Swedberg K, Komajda M, Böhm M, Borer J, Robertson M, Tavazzi L, Ford I. & SHIFT Investigators. Effects on outcomes of heart rate reduction by ivabradine in patients with congestive heart failure: is there an influence of beta-blocker dose? Findings from the SHIFT (Systolic Heart failure treatment with the I(f) inhibitor ivabradine Trial) study. Journal of the American College of Cardiology 2012. 59 1938–1945. ( 10.1016/j.jacc.2012.01.020) [DOI] [PubMed] [Google Scholar]
- 37.McMurray JJV, Packer M, Desai AS, Gong J, Lefkowitz MP, Rizkala AR, Rouleau JL, Shi VC, Solomon SD, Swedberg K, et al Angiotensin-neprilysin inhibition versus enalapril in heart failure. New England Journal of Medicine 2014. 371 993–1004. ( 10.1056/NEJMoa1409077) [DOI] [PubMed] [Google Scholar]
- 38.Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, Falk V, González-Juanatey JR, Harjola VP, Jankowska EA, et al ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. European Heart Journal 2016. 37 2129–2200. ( 10.1093/eurheartj/ehw128) [DOI] [PubMed] [Google Scholar]
- 39.Bristow MR, Saxon LA, Boehmer J, Krueger S, Kass DA, De Marco T, Carson P, DiCarlo L, DeMets D, White BG, et al Cardiac-resynchronization therapy with or without an implantable defibrillator in advanced chronic heart failure. New England Journal of Medicine 2004. 350 2140–2150. ( 10.1056/NEJMoa032423) [DOI] [PubMed] [Google Scholar]
- 40.Cleland JGF, Daubert JC, Erdmann E, Freemantle N, Gras D, Kappenberger L, Tavazzi L. & Cardiac Resynchronization-Heart Failure (CARE-HF) Study Investigators. The effect of cardiac resynchronization on morbidity and mortality in heart failure. New England Journal of Medicine 2005. 352 1539–1549. ( 10.1056/NEJMoa050496) [DOI] [PubMed] [Google Scholar]
- 41.National Institute for Health and Care Excellence. Implantable cardioverter defibrillators and cardiac resynchronisation therapy for arrhythmias and heart failure. Technology appraisal guidance [TA314]. London, UK: NICE, 2014. (available at: https://www.nice.org.uk/guidance/ta314) [Google Scholar]
- 42.Tsao CW, Lyass A, Larson MG, Cheng S, Lam CSP, Aragam JR, Benjamin EJ, Vasan RS. Prognosis of adults with borderline left ventricular ejection fraction. JACC: Heart Failure 2016. 4 502–510. ( 10.1016/j.jchf.2016.03.003) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Petersen SE, Aung N, Sanghvi MM, Zemrak F, Fung K, Paiva JM, Francis JM, Khanji MY, Lukaschuk E, Lee AM, et al Reference ranges for cardiac structure and function using cardiovascular magnetic resonance (CMR) in Caucasians from the UK Biobank population cohort. Journal of Cardiovascular Magnetic Resonance 2017. 19 18 ( 10.1186/s12968-017-0327-9) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cohn JN, Archibald DG, Ziesche S, Franciosa JA, Harston WE, Tristani FE, Dunkman WB, Jacobs W, Francis GS, Flohr KH. Effect of vasodilator therapy on mortality in chronic congestive heart failure. Results of a Veterans Administration Cooperative study. New England Journal of Medicine 1986. 314 1547–1552. ( 10.1056/NEJM198606123142404) [DOI] [PubMed] [Google Scholar]
- 45.Taylor AL, Ziesche S, Yancy C, Carson P, D'Agostino R, Ferdinand K, Taylor M, Adams K, Sabolinski M, Worcel M, et al Combination of isosorbide dinitrate and hydralazine in blacks with heart failure. New England Journal of Medicine 2004. 351 2049–2057. ( 10.1056/NEJMoa042934) [DOI] [PubMed] [Google Scholar]
- 46.Flather MD, Shibata MC, Coats AJS, Van Veldhuisen DJ, Parkhomenko A, Borbola J, Cohen-Solal A, Dumitrascu D, Ferrari R, Lechat P, et al Randomized trial to determine the effect of nebivolol on mortality and cardiovascular hospital admission in elderly patients with heart failure (SENIORS). European Heart Journal 2005. 26 215–225. ( 10.1093/eurheartj/ehi115) [DOI] [PubMed] [Google Scholar]
- 47.Lam CSP, Solomon SD. The middle child in heart failure: heart failure with mid-range ejection fraction (40–50%). European Journal of Heart Failure 2014. 16 1049–1055. ( 10.1002/ejhf.159) [DOI] [PubMed] [Google Scholar]
- 48.Rossi A, Cicoira M, Zanolla L, Sandrini R, Golia G, Zardini P, Enriquez-Sarano M. Determinants and prognostic value of left atrial volume in patients with dilated cardiomyopathy. Journal of the American College of Cardiology 2002. 40 1425 ( 10.1016/s0735-1097(02)02305-7) [DOI] [PubMed] [Google Scholar]
- 49.Beinart R, Boyko V, Schwammenthal E, Kuperstein R, Sagie A, Hod H, Matetzky S, Behar S, Eldar M, Feinberg MS. Long-term prognostic significance of left atrial volume in acute myocardial infarction. Journal of the American College of Cardiology 2004. 44 327–334. ( 10.1016/j.jacc.2004.03.062) [DOI] [PubMed] [Google Scholar]
- 50.Sabharwal N, Cemin R, Rajan K, Hickman M, Lahiri A, Senior R. Usefulness of left atrial volume as a predictor of mortality in patients with ischemic cardiomyopathy. American Journal of Cardiology 2004. 94 760–763. ( 10.1016/j.amjcard.2004.05.060) [DOI] [PubMed] [Google Scholar]
- 51.Osranek M, Bursi F, Bailey KR, Grossardt BR, Brown RD, Jr, Kopecky SL, Tsang TS, Seward JB. Left atrial volume predicts cardiovascular events in patients originally diagnosed with lone atrial fibrillation: three-decade follow-up. European Heart Journal 2005. 26 2556–2561. ( 10.1093/eurheartj/ehi483) [DOI] [PubMed] [Google Scholar]
- 52.Le Tourneau T, Messika-Zeitoun D, Russo A, Detaint D, Topilsky Y, Mahoney DW, Suri R, Enriquez-Sarano M. Impact of left atrial volume on clinical outcome in organic mitral regurgitation. Journal of the American College of Cardiology 2010. 56 570–578. ( 10.1016/j.jacc.2010.02.059) [DOI] [PubMed] [Google Scholar]
- 53.Ujino K, Barnes ME, Cha SS, Langins AP, Bailey KR, Seward JB, Tsang TSM. Two-dimensional echocardiographic methods for assessment of left atrial volume. American Journal of Cardiology 2006. 98 1185–1188. ( 10.1016/j.amjcard.2006.05.040) [DOI] [PubMed] [Google Scholar]
- 54.Nagueh SF, Smiseth OA, Appleton CP, Byrd BF, III, Dokainish H, Edvardsen T, Flachskampf FA, Gillebert TC, Klein AL, Lancellotti P, et al Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Journal of the American Society of Echocardiography 2016. 29 277–314. ( 10.1016/j.echo.2016.01.011) [DOI] [PubMed] [Google Scholar]
- 55.Iskandar A, Mujtaba MT, Thompson PD. Left atrium size in elite athletes. JACC: Cardiovascular Imaging 2015. 8 753–762. ( 10.1016/j.jcmg.2014.12.032) [DOI] [PubMed] [Google Scholar]
- 56.Authors/Task Force members, Elliott PM, Anastasakis A, Borger MA, Borggrefe M, Cecchi F, Charron P, Hagege AA, Lafont A, Limongelli G, et al 2014 ESC Guidelines on diagnosis and management of hypertrophic cardiomyopathy: the Task Force for the Diagnosis and Management of Hypertrophic Cardiomyopathy of the European Society of Cardiology (ESC). European Heart Journal 2014. 35 2733–2779. ( 10.1093/eurheartj/ehu284) [DOI] [PubMed] [Google Scholar]
- 57.Marcus FI, McKenna WJ, Sherrill D, Basso C, Bauce B, Bluemke DA, Calkins H, Corrado D, Cox MGPJ, Daubert JP, et al Diagnosis of arrhythmogenic right ventricular cardiomyopathy/dysplasia: proposed modification of the task force criteria. Circulation 2010. 121 1533–1541. ( 10.1161/CIRCULATIONAHA.108.840827) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Augustine DX, Coates-Bradshaw LD, Willis J, Harkness A, Ring L, Grapsa J, Coghlan G, Kaye N, Oxborough D, Robinson S, et al Echocardiographic assessment of pulmonary hypertension: a guideline protocol from the British Society of Echocardiography. Echo Research and Practice 2018. 5 G11–G24. ( 10.1530/ERP-17-0071) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Galiè N, Humbert M, Vachiery JL, Gibbs S, Lang I, Torbicki A, Simonneau G, Peacock A, Vonk Noordegraaf A, Beghetti M, et al 2015 ESC/ERS guidelines for the diagnosis and treatment of pulmonary hypertension. Revista Espanola de Cardiologia 2016. 69 177 ( 10.1016/j.rec.2016.01.002) [DOI] [PubMed] [Google Scholar]
- 60.Erbel R, Aboyans V, Boileau C, Bossone E, Bartolomeo RD, Eggebrecht H, Evangelista A, Falk V, Frank H, Gaemperli O, et al 2014 ESC Guidelines on the diagnosis and treatment of aortic diseases: document covering acute and chronic aortic diseases of the thoracic and abdominal aorta of the adult. The Task Force for the Diagnosis and Treatment of Aortic Diseases of the European Society of Cardiology (ESC). European Heart Journal 2014. 35 2873–2926. ( 10.1093/eurheartj/ehu281) [DOI] [PubMed] [Google Scholar]
- 61.Oxborough D, Ghani S, Harkness A, Lloyd G, Moody W, Ring L, Sandoval J, Senior R, Sheikh N, Stout M, et al Impact of methodology and the use of allometric scaling on the echocardiographic assessment of the aortic root and arch: a study by the Research and Audit Sub-Committee of the British Society of Echocardiography. Echo Research and Practice 2014. 1 1–9. ( 10.1530/ERP-14-0004) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Roman MJ, Devereux RB, Kramer-Fox R, O’Loughlin J. Two-dimensional echocardiographic aortic root dimensions in normal children and adults. American Journal of Cardiology 1989. 64 507–512. ( 10.1016/0002-9149(89)90430-x) [DOI] [PubMed] [Google Scholar]
- 63.Hiratzka LF, Bakris GL, Beckman JA, Bersin RM, Carr VF, Casey DE, Eagle KA, Hermann LK, Isselbacher EM, Kazerooni EA, et al 2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with thoracic aortic disease. Executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, American College of Radiology, American Stroke Association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of Thoracic Surgeons, and Society for Vascular Medicine. Anesthesia and Analgesia 2010. 111 279–315. ( 10.1213/ANE.0b013e3181dd869b) [DOI] [PubMed] [Google Scholar]
- 64.Goldstein SA, Evangelista A, Abbara S, Arai A, Asch FM, Badano LP, Bolen MA, Connolly HM, Cuéllar-Calàbria H, Czerny M, et al Multimodality imaging of diseases of the thoracic aorta in adults: from the American Society of Echocardiography and the European Association of Cardiovascular Imaging: endorsed by the Society of Cardiovascular Computed Tomography and Society for Cardiovascular Magnetic Resonance. Journal of the American Society of Echocardiography 2015. 28 119–182. ( 10.1016/j.echo.2014.11.015) [DOI] [PubMed] [Google Scholar]
- 65.Cantinotti M, Giordano R, Clemente A, Assanta N, Murzi M, Murzi B, Crocetti M, Marotta M, Scalese M, Kutty S, et al Strengths and limitations of current adult nomograms for the aorta obtained by noninvasive cardiovascular imaging. Echocardiography 2016. 33 1046–1068. ( 10.1111/echo.13232) [DOI] [PubMed] [Google Scholar]
- 66.Devereux RB, de Simone G, Arnett DK, Best LG, Boerwinkle E, Howard BV, Kitzman D, Lee ET, Mosley TH, Weder A, et al Normal limits in relation to age, body size and gender of two-dimensional echocardiographic aortic root dimensions in persons ≥15 years of age. American Journal of Cardiology 2012. 110 1189–1194. ( 10.1016/j.amjcard.2012.05.063) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Plana JC, Galderisi M, Barac A, Ewer MS, Ky B, Scherrer-Crosbie M, Ganame J, Sebag IA, Agler DA, Badano LP, et al Expert consensus for multimodality imaging evaluation of adult patients during and after cancer therapy: a report from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Journal of the American Society of Echocardiography 2014. 27 911–939. ( 10.1016/j.echo.2014.07.012) [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.



 This work is licensed under a
This work is licensed under a