Abstract
Background:
Posterior shoulder stretching exercises (PSSEs) aim to reduce posterior shoulder tightness (PST). Position modification of traditional PSSEs has been suggested to minimize inadequate control of scapular and glenohumeral rotation, possibly leading to increased subacromial impingement.
Hypothesis:
Modified PSSEs will have positive effects on shoulder mobility, pain, and dysfunction.
Study Design:
Randomized controlled trial.
Level of Evidence:
Level 1.
Methods:
A total of 67 symptomatic patients with subacromial impingement syndrome (SIS) and shoulder internal rotation asymmetry were randomly assigned to 3 groups: modified cross-body stretch (MCS) (n = 22; treatment program + MCS), modified sleeper stretch (MSS) (n = 22; treatment program + MSS), and a control group (n = 23; treatment program consisting of only modalities, range of motion [ROM], and strength training but no PSSEs) for 4 weeks. Pain, PST, shoulder rotation ROM, and dysfunction were evaluated.
Results:
Pain, PST, shoulder rotation ROM, function, and disability improved in all groups (P < 0.05). The MCS and MSS groups had better results compared with the control group with regard to pain with activity, internal rotation ROM, function, and disability (P < 0.05). There was no significant difference between the stretching groups (P > 0.05).
Conclusion:
All treatments improved pain, shoulder mobility, function, and disability in patients with SIS. However, modified PSSEs in addition to a treatment program was superior to the treatment program alone (without PSSEs) in improving pain with activity, internal rotation ROM, and dysfunction. Moreover, stretching provided clinically significant improvements.
Clinical Relevance:
Modified PSSEs, in addition to a treatment program, are beneficial for patients with SIS. Both modified cross-body and sleeper stretches are safe and efficacious for improving shoulder mobility, pain, and dysfunction.
Keywords: physical therapy, rehabilitation, shoulder, exercise, stretching
Subacromial impingement syndrome (SIS) is the most common cause of shoulder pain and dysfunction.18 Research has focused on the effects of posterior shoulder tightness (PST) on shoulder pain and SIS symptoms in recent years.24 PST causes anterior-superior translation of the humeral head over the glenoid fossa10 and may lead to SIS, reducing the subacromial space during upper extremity elevation.1,14 PST has been associated with a decrease in glenohumeral internal rotation (IR) range of motion (ROM), and decreased glenohumeral IR ROM has been detected in individuals with SIS.1 Posterior shoulder stretching exercises (PSSEs) have been suggested for IR deficits.13
Physical therapy with exercises is effective in reducing pain and disability in patients with SIS.21 Attention should be given to ensuring adequate posterior shoulder flexibility before strengthening exercises are initiated.14 Shoulder mobility can be increased by reducing the anterior-superior migration of the humeral head. Cross-body or sleeper stretch outcomes are equivocal.14,16
In previous studies, PSSEs have been applied in traditional positions.14,24 However, Wilk et al25 reported that modification of these positions was necessary because of the inadequate control of both scapular and glenohumeral rotations, possibly leading to increased subacromial impingement. Therefore, the purpose of this study was to investigate the effects of 2 different modified PSSEs25 on shoulder mobility, pain, and dysfunction in patients with SIS having glenohumeral internal rotation deficit (GIRD). We hypothesized that both modified PSSEs would have positive effects on shoulder mobility, pain, and dysfunction.
Methods
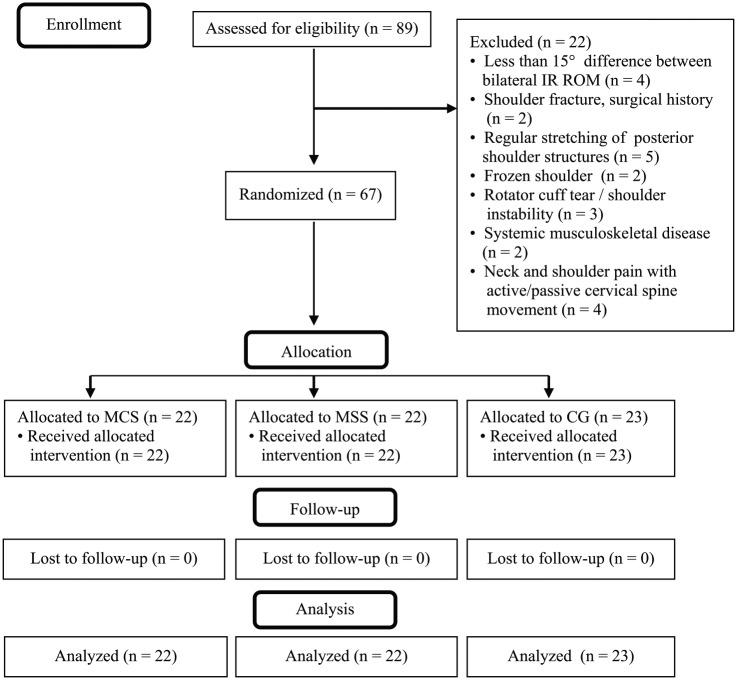
A total of 67 patients (mean age, 52.94 ± 11.05 years) with SIS and GIRD (IR ROM of the SIS side <15° compared with the other shoulder)2 were randomly assigned (Random.org; Randomness and Integrity Services) to 3 groups. The modified cross-body stretch (MCS) group (n = 22) received a treatment program plus MCS exercise, the modified sleeper stretch (MSS) group (n = 22) received a treatment program plus MSS exercise, and the control group received a treatment program consisting of modalities, ROM, and strength training but no PSSE (n = 23) (Figure 1).
Figure 1.
CONSORT (Consolidated Standards of Reporting Trials) flow diagram of study population. CG, control group; IR, internal rotation; MCS, modified cross-body stretching group; MSS, modified sleeper stretching group; ROM, range of motion.
Written informed consent was obtained from participants before taking part in the study. The study was approved by the ethics committee of Dokuz Eylül University (No. 1542-GOA-2014/21-11). Inclusion criteria were the following: ≥18 years of age, SIS diagnosis, no history of shoulder injuries/symptoms requiring treatment other than SIS, diagnosis of GIRD,2 shoulder pain less than 7 out of 10 on the visual analog scale (VAS) for pain, and ≥3 of 5 impingement tests positive.15 Participants were excluded if they had ≥50% limitation of passive shoulder ROM in ≥2 planes of motion, history of fracture involving the upper extremity, shoulder surgery, full-thickness rotator cuff tear, shoulder instability, systemic musculoskeletal disease, or shoulder pain with cervical spine motion or if they were regularly performing PSSEs.
Pain at rest and activity was measured on a 10-cm VAS ranging from 0 (no pain) to 10 (worst pain imaginable).3 Shoulder function was assessed with the Turkish version of the Constant-Murley Score (CMS),6 with a possible total score of 100 points, indicating excellent function. Disability level was assessed with the Turkish version of the QuickDASH (short version of the Disabilities of the Arm, Shoulder and Hand Score) questionnaire,7 with a total score ranging from 0 (no disability) to 100 (severe disability). Shoulder mobility was measured using a bubble inclinometer (baseline).
To avoid bias, the investigator performing the measurements was not allowed to read the results on the inclinometer throughout the testing period. A trained assistant, blinded to group assignment, read and recorded the results. Results of 3 repetitions of each measurement were averaged (intrarater reliability, intraclass correlation coefficient [ICC 3, k] = 0.96-0.99)11 In our study, based on test-retest in 10 patients, test-retest reliability (ICC 3, k) was determined to be 0.99, 0.99, and 0.98 for PST, IR ROM, and external (ER) ROM, respectively.
PST was measured in a side-lying position. The physical therapist passively abducted the humerus to 90° while maintaining no humeral rotation and 90° of elbow flexion. Meanwhile, the lateral border of the scapula was maintained in a fully adducted position throughout the test. The movement was ended if the scapula could not be further stabilized and/or movement of the humerus stopped11 (Figure 2).
Figure 2.

PST measurement.
IR ROM was assessed in a prone position, and ER ROM in a supine position. The arm was supported on the table in 90° of shoulder abduction and elbow flexion. At the end of the active movements, the inclinometer was placed on the distal forearm proximal to the radiocarpal joint and the measurement was recorded11 (Figure 3, a and b). Total rotation ROM (TR ROM) was calculated by summing shoulder IR and ER ROM values. Measurements were taken at the first day of treatment and the day after 20 sessions were completed.
Figure 3.
(a) Measurement of IR ROM. (b) Measurement of ER ROM.
The treatment program21 consisted of 20 minutes of hot application; 20 minutes of high-frequency (50-100 Hz), low-intensity (not painful), small pulse width (50-200 μs) conventional transcutaneous electrical nerve stimulation; and 5 minutes of 1-MHz, 1.5-W/cm2 continuous ultrasound to the shoulder area on weekdays. Wand exercises, posture exercises, and Codman exercises (10 repetitions of each) and upper trapezius stretching (5 repetitions) were performed as 1 set. Strength training was performed for the scapular stabilizers, rotator cuff, and deltoid muscles when appropriate using an elastic band (3 sets of 10 repetitions with 1-minute rest between sets). When 3 sets were performed easily, resistance was increased by changing the band color.
MCS was performed in a side-lying position to limit scapular abduction. The forearms were aligned, with the opposite arm on top to limit the ER of the humerus, and the humerus was moved into horizontal adduction using the opposite arm25 (Figure 4). MSS was performed in a side-lying position; the body was rolled 20° to 30° posteriorly to reduce symptoms of pain, and the humerus was moved into IR using the opposite arm25 (Figure 5). One set of 5 repetitions of a 30-second stretch was performed.25
Figure 4.
(a) MCS with the help of physical therapist. (b) Self-MCS.
Figure 5.
(a) MSS with the help of physical therapist. (b) Self-MSS.
Exercises were performed once a day, every day, for 4 weeks (5 days under physical therapist supervision and 2 days at home).
Statistical Analysis
An a priori sample size calculation was performed (GPower, Version 3.0.10).8 The difference between the 2 measurements for shoulder IR ROM was expected to be 9.6°, with 11° SD,13 and 63 participants were required to determine the significant difference with 80% power (5% type I error) (21 participants per group). The normal distribution of the continuous data was determined using Kolmogorov-Smirnov analysis. Age, height, body weight, and body mass index among groups were compared with 1-way analysis of variance (ANOVA), and sex was compared using the χ2 test. Two-way ANOVA (mixed-model, 2(time) × 3(group), repeated measures) was used to determine changes in dependent variables from baseline to posttreatment measurements. F values were used based on sphericity assumed. Then, 1-way ANOVA was used to determine the effect of group on changes in outcome measures. Post hoc analysis using the Bonferroni method was performed, with an adjusted α level of 0.0167. All statistics were calculated using SPSS software (Version 20.0; IBM Corp). Significance level was determined as P < 0.05. Effect sizes were calculated and interpreted according to the Cohen guidelines (small, 0.01; medium, 0.06; large, 0.14). In post hoc power analyses, ≥0.80 was accepted as sufficient to show significant differences.4
Results
All groups had similar demographic and anthropometric characteristics (P > 0.05) (Table 1) and baseline outcome measurements (P > 0.05) except pain at rest (P = 0.01). Table 2 shows mean values for outcome measurements, and Table 3 presents the F values, effect sizes, and post hoc power results of the 2-way ANOVA analysis.
Table 1.
Demographic and anthropometric characteristics of the participants a
| Participant Characteristics | MCS (n = 22) | MSS (n = 22) | CG (n = 23) | P |
|---|---|---|---|---|
| Age, y | 51.64 ± 13.15 | 52.09 ± 10.23 | 55 ± 9.7 | 0.54 b |
| Height, cm | 162.68 ± 7.23 | 166.27 ± 8.08 | 163.48 ± 6.06 | 0.22 b |
| Weight, kg | 77.98 ± 12.21 | 72.64 ± 11.81 | 77.67 ± 15.13 | 0.32 b |
| Body mass index, kg/m2 | 29.69 ± 4.83 | 26.31 ± 4.23 | 28.94 ± 4.81 | 0.56 b |
| Sex, n (male/female) | 14/8 | 13/9 | 18/5 | 0.35 c |
CG, control group; MCS, modified cross-body stretch group; MSS, modified sleeper stretch group.
Values are presented as mean ± SD unless otherwise indicated.
One-way analysis of variance.
Chi-square test.
Table 2.
Outcome measurements among groups a
| Outcome Measure | Group | Before Treatment | After Treatment | ∆ (% Change) | |
|---|---|---|---|---|---|
| Pain, cm | Pain at rest | MCS | 1.45 ± 1.96 | 0.13 ± 0.35 | −1.31 ± 1.75 (–93.00 ± 12.01) |
| MSS | 2.23 ± 2.36 | 0.40 ± 0.95 | −1.81 ± 1.89 (–87.17 ± 20.58) | ||
| CG | 3.43 ± 2.21 | 2.78 ± 2.21 | −0.65 ± 1.43 (–19.44 ± 38.98) | ||
| Pain during activity | MCS | 4.95 ± 1.25 | 1.59 ± 1.05 | −3.36 ± 1.21 (–68.93 ± 20.32) | |
| MSS | 5.45 ± 0.96 | 2.45 ± 1.14 | −3 ± 1.48 (–53.03 ± 23.70) | ||
| CG | 5.13 ± 1.48 | 4.35 ± 1.82 | −0.78 ± 1.24 (–15.83 ± 23.92) | ||
| Shoulder rotation ROM, deg | IR ROM | MCS | 47.82 ± 10.13 | 69.41 ± 9.43 | 21.59 ± 9.46 (50.52 ± 32.37) |
| MSS | 39.55 ± 14.65 | 61.64 ± 12.35 | 22.09 ± 8.97 (70.66 ± 52.28) | ||
| CG | 45.39 ± 12.90 | 54.22 ± 13.54 | 8.83 ± 8.58 (22.47 ± 24.85) | ||
| ER ROM | MCS | 64.18 ± 26.20 | 76.32 ± 20.30 | 12.14 ± 15.15 (46.36 ± 106.82) | |
| MSS | 60.23 ± 26.10 | 70.64 ± 22.28 | 10.41 ± 13.81 (30.05 ± 45.67) | ||
| CG | 59.19 ± 25.74 | 71.26 ± 18.44 | 12.07 ± 14.67 (29.46 ± 46.78) | ||
| TR ROM | MCS | 144.95 ± 27.38 | 111.55 ± 30.84 | 33.41 ± 15.34 (35.36 ± 26.22) | |
| MSS | 137.68 ± 27.20 | 106.05 ± 37.58 | 31.64 ± 16.75 (40.80 ± 36.28) | ||
| CG | 123.09 ± 27.71 | 104.88 ± 35.65 | 18.20 ± 18.24 (27.19 ± 40.31) | ||
| PST, deg | MCS | 49.68 ± 8.21 | 71.59 ± 9.19 | 21.90 ± 9.09 (46.66 ± 23.48) | |
| MSS | 47.95 ± 15.83 | 70.14 ± 12.95 | 22.18 ± 9.24 (56.39 ± 41.05) | ||
| CG | 49.35 ± 13.80 | 58.78 ± 9.99 | 9.43 ± 9.78 (26 ± 33.57) | ||
| Shoulder function and disability | CMS score | MCS | 60.16 ± 14.21 | 76.30 ± 14.68 | 16.14 ± 10.96 (30.17 ± 27.84) |
| MSS | 51.66 ± 12.68 | 70.07 ± 10.49 | 18.41 ± 8.18 (41.39 ± 32.57) | ||
| CG | 53.48 ± 11.35 | 60.85 ± 12.01 | 7.37 ± 9.62 (16.10 ± 22.79) | ||
| QuickDASH score | MCS | 45.52 ± 19.42 | 19.40 ± 14.79 | −26.12 ± 20.09 (–54.45 ± 31.38) | |
| MSS | 51.76 ± 15.44 | 24.69 ± 15.67 | −27.07 ± 13.36 (–53.65 ± 23.51) | ||
| CG | 51.19 ± 18.89 | 39.12 ± 20.31 | −12.08 ± 14.66 (–22.93 ± 25.97) |
Values are presented as mean ± SD unless otherwise indicated.
Δ, change between 2 measurements; CG, control group; CMS, Constant-Murley score; ER, external rotation; IR, internal rotation; MCS, modified cross-body stretch group; MSS, modified sleeper stretch group; PST, posterior shoulder tightness; QuickDASH, shortened version of the Disabilities of the Arm, Shoulder and Hand questionnaire; ROM, range of motion; TR, total rotation.
Table 3.
Results of the 2-way ANOVA (mixed-model, repeated-measures) analysis
| Outcome Measure | F | P | Partial η2 | Post Hoc Power | |||
|---|---|---|---|---|---|---|---|
| Pain, cm | Pain at rest | Within-participant effects | Time effect a | 36.90 | <0.001 | 0.37 | 1.00 |
| Time-group interaction | 2.66 | 0.08 | 0.08 | 0.99 | |||
| Between-participant effects a | 12.38 | <0.001 | 0.28 | 1.00 | |||
| Pain during activity | Within-participant effects | Time effect a | 219.10 | <0.001 | 0.77 | 1.00 | |
| Time-group interaction a | 25.48 | <0.001 | 0.44 | 1.00 | |||
| Between-participant effects a | 9.15 | <0.001 | 0.22 | 0.99 | |||
| Shoulder rotation ROM, deg | IR ROM | Within-participant effects | Time effect a | 252.87 | <0.001 | 0.80 | 1.00 |
| Time-group interaction a | 15.78 | <0.001 | 0.33 | 1.00 | |||
| Between-participant effects a | 4.01 | 0.02 | 0.11 | 0.84 | |||
| ER ROM | Within-participant effects | Time effect a | 42.09 | <0.001 | 0.40 | 1.00 | |
| Time-group interaction | 0.10 | 0.91 | 0.01 | 0.28 | |||
| Between-participant effects | 0.36 | 0.70 | 0.01 | 0.12 | |||
| TR ROM | Within-participant effects | Time effect a | 181.80 | <0.001 | 0.74 | 1.00 | |
| Time-group interaction a | 5.52 | 0.01 | 0.15 | 1.00 | |||
| Between-participant effects | 1.26 | 0.29 | 0.04 | 0.37 | |||
| PST, deg | Within-participant effects | Time effect a | 206.52 | <0.001 | 0.76 | 1.00 | |
| Time-group interaction a | 5.52 | 0.01 | 0.15 | 1.00 | |||
| Between-participant effects | 1.89 | 0.16 | 0.06 | 0.54 | |||
| Shoulder function and disability | CMS score | Within-participant effects | Time effect a | 140.29 | <0.001 | 0.69 | 1.00 |
| Time-group interaction a | 8.25 | 0.001 | 0.20 | 1.00 | |||
| Between-participant effects a | 5.20 | 0.01 | 0.14 | 0.93 | |||
| QuickDASH score | Within-participant effects | Time effect a | 119.65 | <0.001 | 0.65 | 1.00 | |
| Time-group interaction a | 6.03 | 0.004 | 0.29 | 1.00 | |||
| Between-participant effects a | 3.74 | 0.03 | 0.10 | 0.79 | |||
ANOVA, analysis of variance; CMS, Constant-Murley score; ER, external rotation; IR, internal rotation; PST, posterior shoulder tightness; QuickDASH, shortened version of the Disabilities of the Arm, Shoulder and Hand questionnaire; ROM, range of motion; TR, total rotation.
Indicates a statically significant effect.
Pain
For pain intensity at rest and activity, there was a significant effect of time, with all groups showing a decrease. For pain at rest, there was no significant time-group interaction but there was a significant difference between groups when groups were compared across various time points. However, 1-way ANOVA revealed no significant effect of group on change in pain at rest (F = 7.712; P > 0.05). For pain during activity, there was a significant time-group interaction and there was a significant difference between groups when groups were compared across various time points. One-way ANOVA revealed a significant effect of group on changes in pain during activity (F = 23.19; P < 0.001). Post hoc analyses revealed a significant difference in change for pain during activity between the MCS and control group (P < 0.001) and MSS and control group (P < 0.001). There was no significant difference between stretching groups (P > 0.05).
Shoulder Rotation ROM
Internal Rotation ROM
For IR ROM, there was a significant effect of time, with all groups showing an increase. There was also a significant time-group interaction. There was a significant difference between groups when groups were compared across various time points. One-way ANOVA revealed a significant effect of group on changes in IR ROM (F = 15.78; P < 0.001). Post hoc analyses revealed a significant difference in changes in IR ROM between the MCS and control group (P < 0.001) and MSS and control group (P < 0.001). There was no significant difference between stretching groups (P > 0.05).
External Rotation ROM
For ER ROM, there was a significant effect of time, with all groups showing an increase. There was no significant time-group interaction. There was no significant difference between groups when the groups were compared across various time points.
Total Rotation
For TR ROM, there was a significant effect of time, with all groups showing an increase. There was also a significant time-group interaction. There was no significant difference between groups when the groups were compared across various time points.
Posterior Shoulder Tightness
For PST, there was a significant effect of time, with all groups showing a decrease (higher values indicate improvement). There was also a significant time-group interaction. There was no significant difference between groups when the groups were compared across various time points.
Shoulder Function and Disability
For CMS and QuickDASH scores, there was a significant effect of time, with all groups showing an increase. There was also a significant time-group interaction. There was a significant difference between groups when the groups were compared across various time points. For CMS, 1-way ANOVA revealed a significant effect of group on change in CMS score (F = 8.25; P = 0.001). Post hoc analyses revealed a significant difference for change in CMS score between the MCS and control groups (P = 0.01) and the MSS and control groups (P = 0.001). No significant difference was found between stretching groups (P > 0.05).
For the QuickDASH, 1-way ANOVA revealed a significant effect of group on change in score (F = 6.03; P = 0.004). Post hoc analyses revealed a significant difference for change in QuickDASH score between the MCS and control groups (P = 0.016) and the MSS and control groups (P = 0.01). No significant difference was found between stretching groups (P > 0.05).
Discussion
Pain at rest decreased in all groups, probably because of the treatment program.21 Conversely, pain with activity decreased more in the stretching groups. Moreover, a clinically significant improvement for pain at rest was only seen in the MSS group and for pain with activity in the stretching groups (minimal clinically important difference [MCID], 1.4 cm).22 As dynamic conditions can have more potential to narrow the subacromial space compared with resting conditions, leading to more pain,23 correct biomechanics with appropriate PSSE may be effective, especially for pain during activity. The findings of Cools et al5 support our results. They found a decrease in pain with activity after 3 weeks of traditional PSSEs in athletes with SIS. In the only study investigating the effects of modified PSSEs on pain, modified PSSEs decreased pain in throwers. However, clinical conditions of the throwers were not clear, stretching repetitions were not standard, and only posttreatment values were presented.19
IR ROM increased more in the stretching groups compared with the control group. The inflexibility of the posterior shoulder structures causes anterior-superior migration of the humeral head as well as scapular protraction and anterior tilt.10,12 Possible subacromial compression related to this migration has been associated with limited IR ROM.10,14 By increasing the flexibility of the posterior shoulder structures with modified PSSE, these negative biomechanical changes can be avoided. However, our proposition should be interpreted with caution since we did not perform a biomechanical analysis. Four weeks of cross-body stretching improved IR ROM in athletically active patients with GIRD compared with healthy controls, but sleeper stretching did not.14 With the same exercise prescription, we found that both stretches improved IR ROM similarly, and the gains were significant compared with no stretching. Appropriate exercise prescription and stabilization of the scapula during both modified PSSEs could enhance the effectiveness of stretching.14 Another reason for the discrepancy in these results could be the study populations. Our population was composed of SIS patients with GIRD, which can be considered a study strength.14 MCS increased IR ROM compared with MSS in throwers with PST. Acute reduction in the viscosity of the muscle-tendon unit may be the reason of this improvement.19 Mine16 found that acute modified sleeper stretching and traditional cross-body stretching were equally effective in GIRD and PST in asymptomatic participants.16 Future studies comparing the effects of traditional and modified stretches in SIS patients are needed.
We found similar clinically significant improvement for PST in all groups (minimal detectable change [MDC], 8°).11 This result, which contradicts the greater improvement in IR ROM found in the stretching groups, can be attributed to the fact that different test positions stretch different structures.20 The capsule and glenohumeral ligament are primarily stretched by IR, but the capsule and posterior portion of the deltoid muscle are stretched by horizontal adduction movement.17 The lack of a study using our PST test to evaluate the effects of modified PSSEs makes it difficult to compare our results directly.
ER ROM and TR ROM increased in all groups similarly. We did not expect any additional effect of stretching on ER ROM16 because stretching aimed to improve posterior shoulder flexibility. Our treatment program may have provided ER ROM improvement. However, TR ROM improvement could be expected in stretching groups due to increased IR ROM. While the improvement in TR ROM in the stretching groups was greater than that in the control group, the lack of a significant difference between groups may be attributable to insufficient power (0.36). Further studies with larger sample sizes may demonstrate potential benefits of stretching on TR ROM.
In terms of the QuickDASH score, there was a clinically significant change in stretching groups (MCID, 15.91 points).9 In terms of CMS scores, true change occurred only in the MSS group (MDC, 16.4 points).6 Stretching can affect glenohumeral and scapular kinematics and therefore change the size of the subacromial space.12 Thus, soft tissue compression in the subacromial space can be removed, reducing the level of pain, and the upper extremity can be used more in functional activities. An increase in the acromiohumeral distance was found after 6 weeks of sleeper stretching in overhead athletes.12 Based on the aforementioned mechanisms, both modified PSSEs may have the potential to reduce subacromial pressure, which could lead to decreased pain and increased function. However, further studies to prove these proposed mechanisms are needed.
Acute PSSEs did not change shoulder function after shoulder surgery.20 A 3-week PSSE program was effective in increasing shoulder function in overhead athletes with SIS.5 Although the results of 4 weeks of stretching may be considered preliminary, our results support the need for a longer stretching period to ensure significant gains. In contrast, 4 weeks of sleeper stretch did not improve shoulder function in overhead athletes with PST.2 However, they evaluated shoulder function using a VAS instead of a composite functional score. To clarify the subject, future studies should compare the effects of different stretching periods on shoulder function.
Limitations
A major limitation of this study is the lack of blinding of the therapist; however, it was not possible because it was a thesis study. However, we took precautions to avoid bias. The investigator who performed the measurements was blinded to the device measurements throughout the study. A trained assistant read and recorded them. The participants did not know there were 3 treatment groups or which group they were in. The relatively short period of stretching and the lack of long-term follow-up after the stretching intervention are other significant limitations. Last, a nontreatment control group was not included because of ethical reasons.
Conclusion
The modified posterior shoulder stretches added to the treatment program consisting of modalities, ROM, and strength training are beneficial for patients with SIS having GIRD. All treatments improved pain, shoulder mobility, function, and disability. The modified stretches in addition to the treatment program were superior to the treatment program without PSSE in improving pain with activity, IR ROM, function, and disability. Stretches were equally effective, and stretching exercises provided clinically significant improvements.
Footnotes
The authors report no potential conflicts of interest in the development and publication of this article.
References
- 1. Borstad JD, Mathiowetzb KM, Mindayc LE, Prabhu B, Christopherson DE, Ludewig PM. Clinical measurement of posterior shoulder flexibility. Man Ther. 2007;12:386-389. [DOI] [PubMed] [Google Scholar]
- 2. Chepeha JC, Magee DJ, Bouliane M, Sheps D, Beaupre L. Effectiveness of a posterior shoulder stretching program on university-level overhead athletes: randomized controlled trial. Clin J Sport Med. 2018;28:146-152. [DOI] [PubMed] [Google Scholar]
- 3. Clark P, Lavielle P, Martinez H. Learning from pain scales: patient perspective. J Rheumatol. 2003;30:1584-1588. [PubMed] [Google Scholar]
- 4. Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- 5. Cools AM, Johansson FR, Cagnie B, Cambier DC, Witvrouw EE. Stretching the posterior shoulder structures in subjects with internal rotation deficit: comparison of two stretching techniques. Shoulder Elbow. 2012;4:56-63. [Google Scholar]
- 6. Çelik D. Turkish version of the modified Constant-Murley score and standardized test protocol: reliability and validity. Acta Orthop Traumatol Turc. 2016;50:69-75. [DOI] [PubMed] [Google Scholar]
- 7. Düger T, Yakut E, Öksüz Ç, et al. Kol, Omuz ve El Sorunları (Disabilities of the Arm, Shoulder and Hand–DASH) Anketi Türkçe uyarlamasının güvenirliği ve geçerliği. Fizyoter Rehabil. 2006;17:99-107. [Google Scholar]
- 8. Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39:175-191. [DOI] [PubMed] [Google Scholar]
- 9. Franchignoni F, Vercelli S, Giordano A, Sartorio F, Bravini E, Ferriero G. Minimal clinically important difference of the disabilities of the arm, shoulder and hand outcome measure (DASH) and its shortened version (QuickDASH). J Orthop Sports Phys Ther. 2014;44:30-39. [DOI] [PubMed] [Google Scholar]
- 10. Harryman DT, 2nd, Sidles JA, Clark JM, McQuade KJ, Gibb TD, Matsen FA., 3rd Translation of the humeral head on the glenoid with passive glenohumeral motion. J Bone Joint Surg Am. 1990;72:1334-1343. [PubMed] [Google Scholar]
- 11. Kolber MJ, Saltzman S, Beekhuizen K, Cheng MS. The reliability and minimal detectable change of inclinometric shoulder mobility measurements. Physiother Theory Pract. 2009:25:572-581. [DOI] [PubMed] [Google Scholar]
- 12. Maenhout A, Van Eessel V, Van Dyck L, Vanraes A, Cools A. Quantifying acromiohumeral distance in overhead athletes with glenohumeral internal rotation loss and the influence of a stretching program. Am J Sports Med. 2012;40:2105-2112. [DOI] [PubMed] [Google Scholar]
- 13. Manske RC, Meschke M, Porter A, Smith B, Reiman M. A randomized controlled single-blinded comparison of stretching versus stretching and joint mobilization for posterior shoulder tightness measured by internal rotation motion loss. Sports Health. 2010;2:94-100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. McClure P, Balaicuis J, Heiland D, Broersma ME, Thorndike CK, Wood A. A randomized controlled comparison of stretching procedures for posterior shoulder tightness. J Orthop Sports Phys Ther. 2007;37:108-114. [DOI] [PubMed] [Google Scholar]
- 15. Michener LA, Walsworth MK, Doukas WC, Murphy KP. Reliability and diagnostic accuracy of 5 physical examination tests and combination of tests for subacromial impingement. Arch Phys Med Rehabil. 2009;90:1898-1903. [DOI] [PubMed] [Google Scholar]
- 16. Mine K. Immediate effects of two types of stretching techniques on glenohumeral internal rotation deficit and posterior shoulder tightness; a crossover randomised controlled trial. J Phys Ther Sports Med. 2017;1:19-24. [Google Scholar]
- 17. Muraki T, Aoki M, Uchiyama E, Murakami G, Miyamoto S. The effect of arm position on stretching of the supraspinatus, infraspinatus, and posterior portion of deltoid muscles: a cadaveric study. Clin Biomech (Bristol, Avon). 2006;21:474-480. [DOI] [PubMed] [Google Scholar]
- 18. Ostor AJK, Richards CA, Prevost AT, Speed CA, Hazleman BL. Diagnosis and relation to general health of shoulder disorders presenting to primary care. Rheumatology. 2005;44:800-805. [DOI] [PubMed] [Google Scholar]
- 19. Rao MS, Tejitha S. Comparison of 3 stretching protocols for posterior shoulder tightness in throwers. Int J Physiother Res. 2016;4:1429-1435. [Google Scholar]
- 20. Salamh PA, Kolber MJ, Hegedus EJ, Cook CE. The efficacy of stretching exercises to reduce posterior shoulder tightness acutely in the postoperative population: a single blinded randomized controlled trial. Physiother Theory Pract. 2018;34:111-120. [DOI] [PubMed] [Google Scholar]
- 21. Steuri R, Sattelmayer M, Elsig S, et al. Effectiveness of conservative interventions including exercise, manual therapy and medical management in adults with shoulder impingement: a systematic review and meta-analysis of RCTs. Br J Sports Med. 2017;51:1340-1347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Tashjian RZ, Deloach J, Porucznik CA, Powell AP. Minimal clinically important differences (MCID) and patient acceptable symptomatic state (PASS) for visual analog scales (VAS) measuring pain in patients treated for rotator cuff disease. J Shoulder Elbow Surg. 2009;18:927-932. [DOI] [PubMed] [Google Scholar]
- 23. Thompson MD, Landin D, Page PA. Dynamic acromiohumeral interval changes in baseball players during scaption exercises. J Shoulder Elbow Surg. 2011;20:251-258. [DOI] [PubMed] [Google Scholar]
- 24. Turgut E, Duzgun I, Baltaci G. Stretching exercises for subacromial impingement syndrome: effects of 6-week program on shoulder tightness, pain, and disability status. J Sport Rehabil. 2018;27:132-137. [DOI] [PubMed] [Google Scholar]
- 25. Wilk KE, Hooks TR, Macrina LC. The modified sleeper stretch and modified cross-body stretch to increase shoulder internal rotation range of motion in the overhead athlete. J Orthop Sports Phys Ther. 2013;43:891-894. [DOI] [PubMed] [Google Scholar]