Abstract
Background
In patients at high risk of opportunistic infections who present with isolated.
neurological symptoms, it is lifesaving to consider Central Nervous System Aspergillosis (CNS-A). Ibrutinib use in chronic lymphocytic leukemia (CLL) has previously been associated with CNS-A. We provide a case report of a patient that presented with primary CNS-A on Ibrutinib therapy without any prior pulmonary or local paranasal signs of infection.
Case presentation
74-year-old Caucasian male with CLL and no prior chemotherapy on ibrutinib for 6 months presented with three months of unsteady gait, occipital headache, and confusion. He has a history of pulmonary sarcoidosis on chronic prednisone 5 mg daily and chronic obstructive pulmonary disease (COPD). He was found to have a “brain abscess” on imaging. Emergent craniotomy confirmed Aspergillus and patient was treated with Voriconazole for 6 months. At six-month follow up, repeat magnetic resonance imaging (MRI) confirmed complete resolution of CNS lesion.
Conclusions
Our case reinforces the importance of being vigilant for isolated CNS-A in CLL patients on ibrutinib who present with neurological symptoms and signs, without prior or co-infection of sino-pulmonary tissue.
Keywords: Aspergillosis, Ibrutinib, Chronic lymphocytic leukemia, Aspergillus, Case report
Background
Invasive Aspergillosis (IA) is an opportunistic infection caused by the fungus Aspergillus [1]. Immunocompromised patients are at risk; however, in patients with Chronic Lymphocytic Leukemia (CLL) per se are not thought to be at a higher risk of IA. A 2016 correspondence in New England Journal of Medicine (NEJM) alerted clinicians to be aware of the possibility that ibrutinib use in CLL, even without neutropenia, is rarely associated with CNS-A [2]. Either the lung or paranasal sinuses are typically infected prior to or concomitant with CNS-A and therefore may serve as an etiological clinical clue to the correct diagnosis.
The diagnosis of isolated CNS-A is challenging. Neurological symptoms and signs are variable and an intracranial mass, detected by Computed Tomography (CT) or MRI, is not pathognomonic and easily misattributed to malignancy or abscess. Criteria for proven invasive fungal disease is by tissue biopsy histopathology and culture [3], but may not be possible or deemed safe to accomplish. Early diagnosis and prompt surgical and medical treatment reduces morbidity and mortality. Treatment of CNS-A is surgical excision (resection or removal if possible) of the Aspergillus granuloma and necrotic tissue treatment with anti-aspergillus therapy [4]. Current Infectious Diseases Society of America (IDSA) guidelines recommend voriconazole as the preferred first line anti-aspergillus therapy [5]. Amphotericin B may also be considered in patients intolerant to voriconzole [5].
Case presentation
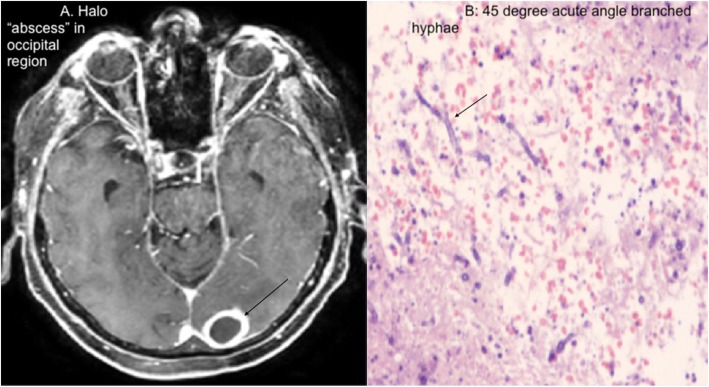
A 74-year-old Caucasian male with CLL and no prior chemotherapy on ibrutinib for 6 months, presented with 3 months of fluctuating, slowly progressive imbalance, unsteady gait, left occipital headache and 1 week of intermittent confusion prior to neurological evaluation. Medical history included: COPD, non-valvular atrial fibrillation (novel oral anticoagulant treated), and pulmonary sarcoidosis on chronic prednisone 5 mg daily. Neurological exam revealed a right upper hemianopsia, unsteady wide based gait. He was afebrile and alert, but mildly confused. Sino- pulmonary exam was normal and no lymphadenopathy or hepatosplenomegaly detected. Basic lab work showed no neutropenia. Head MRI showed a ring enhancing lesion (Fig. 1a) in the left occipital region without sinus abnormalities. An emergent craniotomy to evacuate the brain “abscess” revealed acute 45-degree angle branching hyphae (Fig. 1b), consistent with Aspergillus and confirmed with silver stain and positive culture. Chest CT was without signs of pulmonary aspergillosis or pneumonia and blood cultures were without growth. Transthoracic Echocardiogram performed showed no definitive vegetations. Serum galactomannan levels were not drawn due to lab limitations; however, B-D Glucan levels were positive. Within 72 h of postoperatively initiated voriconazole, his neurological symptoms dramatically improved. At six-month follow-up, repeat MRI confirmed complete resolution of the central nervous system (CNS) lesion and absence of neurological signs and symptoms.
Fig. 1.
a “Halo abscess” in occipital region. b “45-degree acute angle branched hyphae
Discussion and conclusions
Our patient on ibrutinib for CLL and low dose steroids for pulmonary sarcoidosis presented with subacute, neurological symptoms and signs attributed to isolated CNS-A. Aggressive diagnostic surgical and medical treatment led to complete cure.
Case reports predominate the literature. A 2012 meta-analysis compared cases of CNS-A at Massachusetts General Hospital (MGH) (n = 14) with globally published cases (n = 123) from 2000 to 2011 [6]. Of the 14 cases at MGH, none had isolated CNS-A (only 1 had primary discitis) without antecedent pulmonary or paranasal sinus infection. Of the 123 global cases, 22.8% (n = 28/123) did not have an apparent site of extra-CNS infection. Hematogenous dissemination was confirmed from a pulmonary focus in 26.8% (n = 33/123) of cases and direct extension from paranasal sinus infection in 27.6% (n = 34/123) of cases. None had CLL or ibrutinib exposure [6].
Isolated CNS-A cases are rarely documented in CLL patients [7]. Three CNS-A cases were reported in 2016 from the international RESONATE-2 trial, a prospective observational cohort study of 1149 CLL patients in the United States on ibrutinib therapy. All three patients were on steroids and developed CNS-A within 2 months of initiating Ibrutinib [2]. Our case reinforces the importance of being vigilant for isolated CNS-A in CLL patients on ibrutinib who present with neurological symptoms and signs, even without prior or co-infection of sino-pulmonary tissue, as early recognition and treatment can be lifesaving. Prompt neuroimaging prudent to identify if a CNS space occupying lesion was accessible to biopsy.
Management included surgical evacuation with an attempt to remove or at least reduce the infection and voriconazole for 6 months, consistent with IDSA guidelines [5]. Due to limited access to serum voriconazole level testing and slow turnaround time, serum levels were unable to be monitored. However, adequate CNS penetration was clinically documented by absence of neurological signs and symptoms on physical exam with resolution of CNS lesion on MRI at follow-up.
Acknowledgements
Not Applicable.
Ethical approval and consent to participate
This case report was approved by Donald and Barbara Zucker School of Medicine at Hofstra/Northwell Mather Hospital GME Office.
Availability of data
All authors had access to data and material and vouch for its complete accuracy. The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CLL
Chronic lymphocytic leukemia
- CNS-A
Central nervous system aspergillosis
- COPD
chronic obstructive pulmonary disease
- CT
Computer tomography
- IA
Invasive aspergillosis
- IDA
Infectious disease society of America
- MRI
Magnetic resonance imaging
- NEJM
New England journal of medicine
Authors contributions
T.L contributed with literature review, drafting, and revising the final draft. G.K and M.B contributed with drafting and revising the final draft. V.K, H.S, and B.B helped with reviewing, formatting, and revising the final draft of the manuscript. A.K severed as the senior consultant and helped finalize the final draft of the manuscript. All listed authors have read and have approved the manuscript.
Funding
None.
Consent for publication
The patient in this case report gave written consent for their clinical details along with any identifying images to be published in this study.
Competing interests
All authors listed above have no relations with industry or any conflicts of interest to declare.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.About Aspergillosis. Centers for Disease Control and Prevention. 2019. https://www.cdc.gov/fungal/diseases/aspergillosis/definition.html.
- 2.Sharman J. Ibrutinib for chronic lymphocytic leukemia: NEJM. N Engl J Med. 2016;374:1593–1594. doi: 10.1056/NEJMc1600328. [DOI] [PubMed] [Google Scholar]
- 3.Peter Donnelly J, Chen SC, Kauffman CA, et al. Revision and update of the consensus definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer and the mycoses study group education and research consortium. Clin Infect Dis. 2019;1:3–6. doi: 10.1093/cid/ciz1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nadkarni T, Goel A. Aspergilloma of the brain: an overview. J Postgrad Med. 2005;51:S37–S41. [PubMed] [Google Scholar]
- 5.Patterson TF, Thompson GR, et al. Practice guidelines for the diagnosis and Management of Aspergillosis: 2016 update by the infectious diseases society of America. Clin Infect Dis. 2016;63:32–50. doi: 10.1093/cid/ciw444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kourkoumpetis TK, et al. Central nervous system Aspergillosis: A series of 14 cases from a general hospital and review of 123 cases from the literature. Medicine. 2012;91:328–336. doi: 10.1097/MD.0b013e318274cd77. [DOI] [PubMed] [Google Scholar]
- 7.Payot A. Primary central nervous system Aspergillosis: a case report and review of the literature. Clinical Microbiology and Infection, ESCMID. 1999;5:573–576. doi: 10.1111/j.1469-0691.1999.tb00438.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All authors had access to data and material and vouch for its complete accuracy. The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.