INTRODUCTION
The United States is facing an opioid epidemic. From 1999 to 2010, the number of opioid prescriptions quadrupled.1 In tandem, the number of patients who died in the US from opioid analgesic-related overdoses also quadrupled, from 4,030 to 16,551 patients.1 Roughly 40% of opioids prescribed are related to episodes of surgical care, and recent data suggests that 6% of patients undergoing either major or minor elective surgical procedures develop long-term opioid dependence. 2–4 Therefore, defining best practices in postoperative outpatient opioid prescribing is a critical opportunity to mitigate against our current epidemic.
Although opioid analgesics are commonly used to manage postoperative pain, there are few accepted guidelines for outpatient prescribing. There is no standardized approach to teach pain management within surgical training programs or continuing medical education efforts, and much of physician prescribing behavior is dictated by peer behavior. Although normative values regarding opioid consumption after surgery remain unknown for many procedures, current studies among patients undergoing common general surgery procedures suggest that physicians overprescribe. 5 For example, about 58% of patients prescribed opioids after urologic procedures have leftover medication, and 89% of these patients retain their leftover medication at home.6 Leftover medications at home increase the potential for non-medical use, with over two-thirds of non-medical opioid users reporting obtaining drugs from a friend or relative.7 In this context, understanding the factors that could reduce excess opioid prescribing, while providing effective pain relief, could provide a pragmatic strategy to tailor postoperative pain management.
Given the lack of standardized guidelines to direct surgeons regarding prescription opioids, it is possible that surgeons prescribe postoperative analgesics to mitigate the probability of refill across a variety of patients, including chronic opioid users and new persistent users. To study this, we examined the probability of prescription opioid refills among a sample of adults undergoing elective surgery using a large dataset of employer-based insurance claims. We specifically examined the factors correlated with a single refill following surgery to highlight opportunities in which the initial prescription could be tailored to patient needs. We hypothesized that increased initial opioid prescription would lead to a decrease in probability of refill.
METHODS
Data Source and Study Cohort
We analyzed OptumInsight claims data, a nationwide private insurance claims database. OptumInsight data contain patients’ demographic information, insurance coverage and eligibility, utilization of inpatient and outpatient services, outpatient pharmacy claims, and health risk assessment data. We selected patients between ages 18 to 64 years old who underwent minor surgeries (varicose vein removal, laparoscopic appendectomy, hemorrhoidectomy, laparoscopic cholecystectomy, transurethral prostate surgeries, thyroidectomy, parathyroidectomy, and carpal tunnel) or major surgery (bariatric surgery, colectomy, incisional hernia repair, reflux surgery, and hysterectomy) between 2013 and 2014. These procedures were identified using International Classification of Disease, Ninth Revision, Clinical Modification (ICD-9-CM) procedure codes and Current Procedural Terminology (CPT) codes (Appendix 1). We restricted our sample to patients who were opioid naïve, which was defined as those patients who had not filled a prescription for an opioid medication within the 12 months prior to the date of surgery. Opioid medications were identified by National Drug Codes (NDC) from pharmacy claims within Optum files. Patients were also required to have filled an initial opioid prescription within 30 days postoperatively. We also specifically excluded patients with more than two prescriptions within 30 days after surgery, as we presumed that these patients would be likely to refill their prescription regardless of initial amount prescribed.
Outcomes
Our outcome of interest was the refill of any prescription opioid medication within 30 postoperative days. The outcome variable was dichotomous, “0” for patients having only one postoperative prescription, otherwise, “1” if having one additional refill of opioid prescription after the initial postoperative opioid prescription within 30 days after surgery.
Exposure variable
Our primary explanatory variable of interest was the total opioid measured in oral morphine equivalents (OME) provided in the initial postoperative prescription. OMEs were calculated based on the contents of the prescription and the number of pills provided. 8
Patient Factors
We included patient sociodemographic factors including age, gender, race/ethnicity, education level, and patient’s residence as one of nine regions in the U.S. Age was included as a continuous variable, and gender was coded as male or female. Race and ethnicity was categorized as white, black, Hispanic, or other. Education level was classified as less than high school, high school graduate, some college, college or higher, or unknown education level.
Patient comorbid conditions as well as tobacco use history were also obtained from claims data. Comorbidities were weighted as an index score using the Charlson index.9 We also included mental health disorders, including adjustment disorders, anxiety, mood disorders, suicide or self-harm, disruptive, personality, psychosis, other mental health disorders, and alcohol or substance abuse disorders based on ICD-9 codes (Appendix 2). Pain disorders, including arthritis, back, neck, other pain were also captured using ICD-9-CM diagnosis codes in the claims within one year prior to surgery (Appendix 3). History of smoking was identified using both ICD-9-CM diagnosis codes and the smoking status found in OptumInsight Health Risk Assessment data, in which the value 1 and 2 were assumed to be indicators of present or past smoking history.
Analysis
We used descriptive statistics to assess the patient characteristics of the study population and determined the incidence of a single refill within 30 days after surgery. We used logistic regression models to predict the likelihood of having an additional refill and the primary explanatory variable of interest, initial OME prescribed, while controlling for patients’ characteristics, including type of procedure, age, gender, race, education, region, comorbid conditions, tobacco use, mental health disorders, and co-existing pain disorders. The estimated probability of having a refill by initial OME prescribed was stratified by type of procedure. Statistical analyses were conducted using STATA, version 14.0 (StataCorp).
RESULTS
Patient characteristics for our study population are detailed in Table 1. Of 26,520 opioid naïve patients included in this study, the majority of patients underwent minor surgery (81.2%), and 18.8% underwent major surgery. Our cohort was 65.1% female and 34.9% male, with a mean age of 44.5. In our cohort, 22% of patients had a history of tobacco use, 14.9% had a history of anxiety disorders, and 15.1% had a history of mood disorders. Many patients had a pre-existing diagnosis of pain disorders, with 44.5% with arthritis and 38.4% with other pain conditions.
Table 1:
Demographic Characteristics of the Study Cohort
| No. of Cases | % of Total | |
|---|---|---|
| Total Number of Opioid Naïve Patients | 26,520 | |
| Patient with Postoperative Refill | 2,300 | 8.7% |
| Surgery Type | ||
| Major Surgery | 4,980 | 18.8% |
| Minor Surgery | 21,540 | 81.2% |
| Age (Mean and Std Dev) | 44.5 (12.0) | |
| Gender | ||
| Male | 9249 | 34.9% |
| Female | 17271 | 65.1% |
| Race/Ethnicity | ||
| White | 19,126 | 72.1% |
| African-American | 2,326 | 8.8% |
| Hispanic | 3,175 | 12.0% |
| Others | 1,893 | 7.1% |
| Education | ||
| <12th Grade | 133 | 0.5% |
| High School | 7056 | 26.6% |
| Some College | 14462 | 54.5% |
| College or more | 4657 | 17.6% |
| Missing/Unknown | 212 | 0.8% |
| Region | ||
| East North Central | 4748 | 17.9% |
| East South Central | 1074 | 4.0% |
| Middle Atlantic | 1766 | 6.7% |
| Mountain | 2693 | 10.2% |
| New England | 788 | 3.0% |
| Pacific | 1584 | 6.0% |
| South Atlantic | 5994 | 22.6% |
| West North Central | 3580 | 13.5% |
| West South Central | 4280 | 16.1% |
| Missing/Unknown | 13 | 0.0% |
| Comorbidities | ||
| Charlson Comorbidity Index (Mean & StdDev) | 0.78 (1.43) | |
| History of Tobacco use | ||
| Yes | 5837 | 22.0% |
| No | 20683 | 78.0% |
| Mental Health Disorder | ||
| Adjustment Disorders | 1186 | 4.5% |
| Anxiety Disorders | 3956 | 14.9% |
| Mood Disorders | 4002 | 15.1% |
| Suicide or self-harm | 82 | 0.3% |
| Disruptive Disorders | 716 | 2.7% |
| Personality Disorders | 56 | 0.2% |
| Psychosis Disorders | 138 | 0.5% |
| Other Disorders | 904 | 3.4% |
| Alcohol or Substance Abuse Disorders | 589 | 2.2% |
| Pain Disorders | ||
| Arthritis | 11811 | 44.5% |
| Back | 6076 | 22.9% |
| Neck | 3219 | 12.1% |
| Other Pain Conditions | 10187 | 38.4% |
| Median Initial OME [Interquartile range] | 200 [112.5] | |
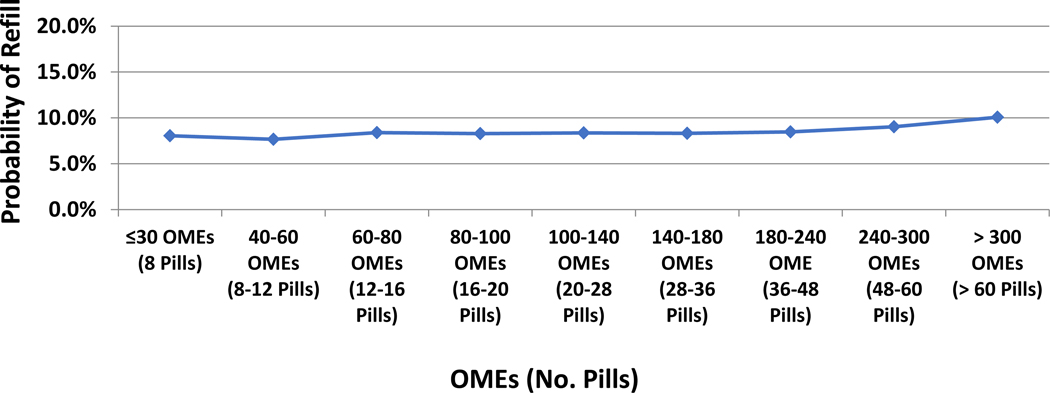
We observed that 8.67% of patients refilled their prescriptions within 30 days of surgery (Figure 1). Among patients who refilled their prescription a single time, patients who underwent reflux surgery (19.8%), hemorrhoidectomy (17.2%), and colectomy (17.0%) were most likely to refill (Table 2). The procedures with patients the least probability of a single postoperative refill were parathyroidectomy (2.8%), thyroidectomy (4.7%), varicose vein removal (6.8%), laparoscopic appendectomy (6.8%), and prostatectomy (6.8%).
Figure 1.
Probability of Refill by Initial OME Prescribed
Table 2:
Number and Percent of Patients with Refill and Initial Median OMEs Prescribed by Type of Procedure
| Procedure | # Cases | % Cases w/Refill | Median Initial OMEs Prescribed | Initial OME Interquartile Range (Q1-Q3) | |
|---|---|---|---|---|---|
| Major Surgery | Bariatric Surgery | 1212 | 9.5% | 213 | 158 |
| Colectomy | 206 | 17.0% | 225 | 150 | |
| Incisional Hernia repair | 459 | 14.8% | 225 | 170 | |
| Reflux surgery | 91 | 19.8% | 225 | 136.4 | |
| Hysterectomy | 3012 | 13.4% | 225 | 150 | |
| Minor Surgery | Varicose vein removal | 59 | 6.8% | 200 | 112.5 |
| Laparoscopic Appendectomy | 5262 | 6.8% | 200 | 75 | |
| Hemorrhoidectomy | 1850 | 17.2% | 225 | 170 | |
| Laparoscopic Cholecystectomy | 10114 | 6.8% | 200 | 90 | |
| Prostatectomy | 294 | 8.2% | 150 | 125 | |
| Thyroidectomy | 1181 | 4.7% | 180 | 75 | |
| Parathyroidectomy | 387 | 2.8% | 150 | 90 | |
| Carpal Tunnel Surgery | 2393 | 8.4% | 180 | 120 | |
| TOTAL | 26520 | 8.7% | 200 | 112.5 |
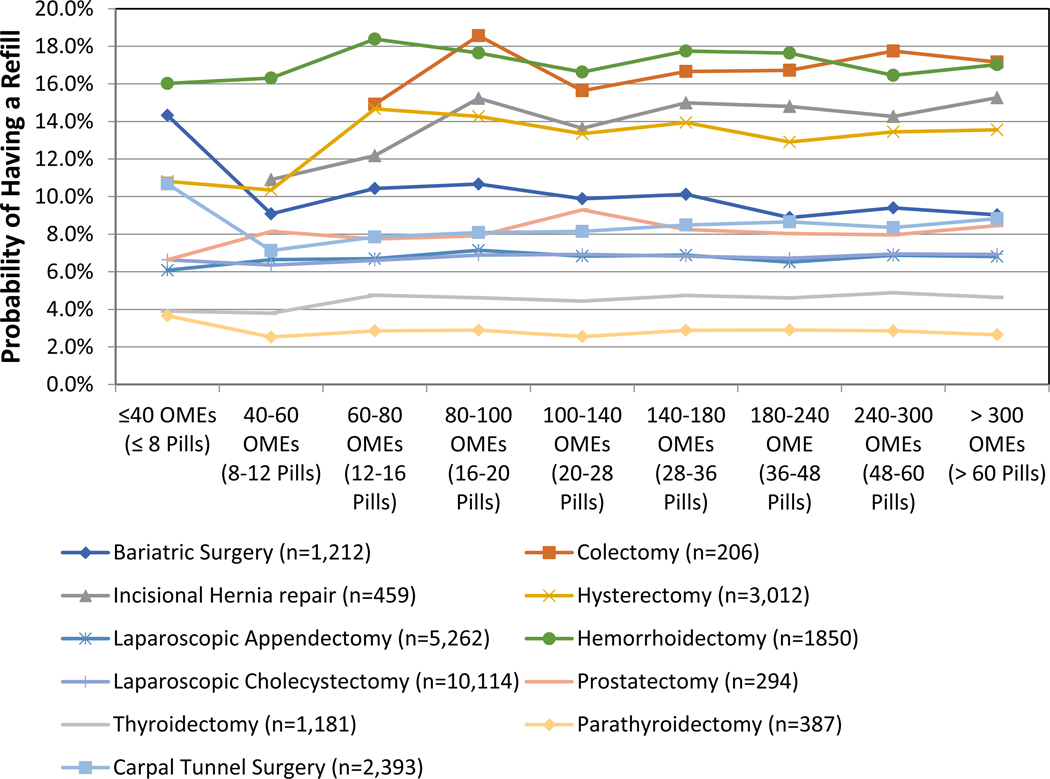
Counter to our hypothesis, the probability of a single postoperative refill did not change significantly with an increase with initial OME prescribed. Instead, the probability of refill increased slightly to 9.03% and 10.08%, when patients were prescribed 240–300 OME (48–60 pills) and over 300 (>60 pills), respectively. When stratified by procedure, small differences were observed. For example, patients undergoing hemorrhoidectomy were most likely to require an additional refill, with a probability ranging from 16% - 18.4% across OMEs. Parathyroidectomy patients were least likely to refill with a range of 2.5% - 3.7% across OMEs (Figure 2). Unlike other procedures, colectomy and hysterectomy procedures demonstrated an increase in probability with increased initial OME.
Figure 2.
Probability of Refill by Initial OME Prescribed and Type of Procedure
Table 3 describes the correlation between the probability of refilling a postoperative opioid prescription and patient attributes (Table 3). Specifically, patients with history of tobacco use were more likely to refill than those without (adjusted OR=1.42, 95% CI: 1.23–1.57). Additionally, patients with mental health disorders, specifically patients with anxiety disorders (adjusted OR=1.30, 95% CI: 1.15 – 1.47), mood disorders (adjusted OR=1.28. 95% CI: 1.13–1.44), and alcohol or substance abuse disorders (adjusted OR=1.43, 95% CI: 1.12–1.84) were more likely to refill their opioid prescription postoperatively, regardless of procedure type. Patients with chronic pain disorders, without a prior opioid prescription, specifically those with arthritis (adjusted OR=1.21, 95% CI: 1.10–1.34) and other pain conditions (adjusted OR=1.19, 95% CI: 1.08–1.30) were more likely to refill their prescriptions regardless of procedure type.
Table 3:
Multivariable Analysis Examining the Probability of Prescription Opioid Refill Within 30 Days of Surgical Procedure.
| Parameter | Pr > ChiSq | Odds Ratio | 95% CI |
|---|---|---|---|
| Constant | <.0001 | ||
| Postoperative Initial OME (natural log transformed) | 0.5962 | 0.975 | (0.890 1.069) |
| Surgery Type (ref:Laparoscopic Cholecystectomy) | |||
| Bariatric Surgery | 0.0404 | 1.258 | (1.010 1.566) |
| Colectomy | <.0001 | 2.876 | (1.967 4.205) |
| Incisional Hernia repair | <.0001 | 2.641 | (2.004 3.481) |
| Reflux surgery | <.0001 | 3.111 | (1.830 5.288) |
| Hysterectomy | <.0001 | 2.285 | (1.990 2.623) |
| Varicose vein removal | 0.7201 | 1.206 | (0.433 3.359) |
| Laparoscopic Appendectomy | 0.6223 | 0.965 | (0.838 1.111) |
| Hemorrhoidectomy | <.0001 | 3.163 | (2.722 3.677) |
| Prostatectomy | 0.1087 | 1.432 | (0.923 2.221) |
| Thyroidectomy | 0.0252 | 0.719 | (0.539 0.960) |
| Parathyroidectomy | 0.0072 | 0.435 | (0.237 0.798) |
| Carpal Tunnel Repair | 0.0056 | 1.276 | (1.074 1.516) |
| Comorbidities | |||
| Charlson Comorbidity Index (Mean) | 0.5474 | 1.010 | (0.978 1.043) |
| History of Tobacco use (ref: No) | |||
| Yes | <.0001 | 1.418 | (1.282 1.567) |
| Mental Health Disorder | |||
| Adjustment Disorders | 0.07 | 1.198 | (0.985 1.458) |
| Anxiety Disorders | <.0001 | 1.303 | (1.154 1.471) |
| Mood Disorders | <.0001 | 1.278 | (1.130 1.444) |
| Suicide or self-harm | 0.9388 | 1.027 | (0.518 2.036) |
| Disruptive Disorders | 0.1716 | 1.181 | (0.930 1.500) |
| Personality Disorders | 0.2422 | 0.530 | (0.183 1.536) |
| Psychosis Disorders | 0.0509 | 0.497 | (0.246 1.003) |
| Other Disorders | 0.6638 | 1.053 | (0.835 1.327) |
| Alcohol or Substance Abuse Disorders | 0.0050 | 1.433 | (1.115 1.842) |
| Pain Disorders | |||
| Arthritis | <.0001 | 1.213 | (1.101 1.337) |
| Back | 0.7622 | 1.017 | (0.910 1.138) |
| Neck | 0.2268 | 0.915 | (0.792 1.057) |
| Other Pain Conditions | 0.0003 | 1.190 | (1.084 1.306) |
Adjusted for age, gender, education, race, and geographic area
DISCUSSION
In this cohort of adults undergoing common surgical procedures, the amount of opioid prescribed in the initial prescription did not correlate with the probability of refilling a prescription, suggesting that other factors are more closely related to the need for additional pills. Moreover, there were small differences in the probability of refill by procedure type, and patients undergoing reflux surgery, colectomy, incisional hernia repair, and hemorrhoidectomy were most likely to refill.
Our findings align with prior literature that demonstrates that opioid use is closely related to patient attributes, and perhaps more related to pre-existing pain and mental health conditions rather than surgical site pain. 10–13 We observed that regardless of procedure type and initial dosing, variation in refill probability is attributable to a range mental health disorders and pre-existing pain, even among patients who did not go on to become prolonged or chronic opioid users. 2 Similarly, Goesling et al. have demonstrated that that symptoms of depression are associated with opioid use, regardless of pain severity, physical functioning, and surgical site pain.13 Patients with mental health conditions may perceive postoperative pain and stress differently, and require greater amounts of opioids following surgery. Moreover, prior research has demonstrated that patients with centralized pain phenotypes and chronic pain conditions may be less responsive to opioids. 12 As such, patients with pain conditions may be more likely to continue to refill opioid prescriptions for symptoms beyond surgical-site pain, and may merit alternative approaches to pain control.14,15
Our study has several notable limitations. First, this analysis was conducted using insurance claims related pharmaceuticals. Although our data provides information on number of pills prescribed in each bottle, the exact quantity taken by each patient is unknown. Additionally, we did not capture those patients for whom opioids were prescribed, but were not filled, and our study results are not generalizable to uninsured patients and patients over the age of 65, who were not captured in our dataset. Finally, although we observed a significant association between comorbid mental health and pain-related, insurance claims likely lack sufficient granularity to precisely predict those patients who will go on to requiring refills. Future studies that prospectively examine the nuances of psychosocial risk factors for opioid use may better illuminate the patient-level predictors correlated with postoperative opioid consumption.
Nonetheless, our findings have several important implications for physicians in practice. First, the lack of impact of initial opioid prescribing on refill probability suggests that clinicians could begin patients on a lower initial prescription to decrease the potential for leftover pills in the home, diversion of those drugs elsewhere, or chronic opioid use. This is further supported by recent evidence that the majority of opioid medications remain unconsumed following common surgical procedures, and prescriptions are frequently provided in excess.5 We also observed that patients with mental health and chronic pain disorders were more likely to refill prescriptions postoperatively. Whereas these patients may experience more pain and discomfort following surgery, it is not clear that higher opioid doses represent an appropriate analgesic regimen. Patients with mental health disorders in particular are prone to opioid misuse and abuse. 16,17 Therefore, surgeons should collaborate with primary care and mental health providers to create an optimal and patient-centered postoperative pain management plan, particularly for patients with these risk factors. Additionally, clinicians should educate patients on opioid alternatives for pain control, particularly among patients prone to take opioids for reasons other than surgical pain. Further research is needed for these underutilized methods for pain control to better address pain, including non-opioid analgesics and cognitive behavioral therapies. Specifically, research on non-pharmaceutical pain control techniques and alternative pharmaceutical interventions such as nonsteroidal anti-inflammatories and acetaminophen could allow for appropriate pain control with fewer adverse events.
Our results, together with prior studies indicating that patients take only a portion of prescribed pills, suggest that many patients may be over-prescribed opioids.5 Overall, our study indicates that an increased quantity of initial prescriptions for opioids did not correlate with a decrease in refill probability. Instead, variation in probability of refill was attributed to psychosocial factors such as anxiety, mood, alcohol or substance abuse, and chronic pain disorders. Going forward, identifying the factors that influence pain, postoperative opioid needs, and satisfaction with recovery will be essential to inform strategies to achieve safe, appropriate opioid prescribing guidelines for common surgical procedures.
Supplementary Material
Acknowledgments
Conflict of Interest/Disclosures: Dr. Waljee receives research funding from the Agency for Healthcare Research and Quality (K08 1K08HS023313-01), the American College of Surgeons, and the American Foundation for Surgery of the Hand; serves as an unpaid consultant for 3M Health Information systems. Drs. Brummett, Englesbe, Waljee and Hu receive funding from the Michigan Department of Health and Human Services. Dr. Brummett reports a patent for Peripheral Perineural Dexmedetomidine licensed to University of Michigan and is a consultant with Tonix. Dr. Brummett receives research funding from Neuros Medical Inc. (Willoughby Hills, Ohio). Grants include: NIH; NIAMS RO1 AR060392; NIDA 1R01 DA038261-01A1; University of Michigan School Dean’s Office- Michigan Genomics Initiative. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the Michigan Department of Health and Human Services.
REFERENCES
- 1.Dowell D, Kunins HV, Farley TA. Opioid analgesics--risky drugs, not risky patients. Jama. 2013;309(21):2219–2220. [DOI] [PubMed] [Google Scholar]
- 2.Brummett CM, Waljee JF, Goesling J, et al. New Persistent Opioid Use After Minor and Major Surgery in U.S. Adults. JAMA surgery. 2017;In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stanek JJ, Renslow MA, Kalliainen LK. The effect of an educational program on opioid prescription patterns in hand surgery: a quality improvement program. J Hand Surg Am. 2015;40(2):341–346. [DOI] [PubMed] [Google Scholar]
- 4.Alam A, Gomes T, Zheng H, Mamdani MM, Juurlink DN, Bell CM. Long-term analgesic use after low-risk surgery: a retrospective cohort study. Arch Intern Med. 2012;172(5):425–430. [DOI] [PubMed] [Google Scholar]
- 5.Hill MV, McMahon ML, Stucke RS, Barth RJ Jr. Wide Variation and Excessive Dosage of Opioid Prescriptions for Common General Surgical Procedures. Ann Surg. 2016. [DOI] [PubMed] [Google Scholar]
- 6.Costello M. Prescription Opioid Analgesics: Promoting Patient Safety with Better Patient Education. Am J Nurs. 2015;115(11):50–56. [DOI] [PubMed] [Google Scholar]
- 7.McCabe SE, West BT, Boyd CJ. Leftover prescription opioids and nonmedical use among high school seniors: a multi-cohort national study. The Journal of adolescent health : official publication of the Society for Adolescent Medicine. 2013;52(4):480–485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Logan J, Liu Y, Paulozzi L, Zhang K, Jones C. Opioid prescribing in emergency departments: the prevalence of potentially inappropriate prescribing and misuse. Med Care. 2013;51(8):646–653. [DOI] [PubMed] [Google Scholar]
- 9.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. [DOI] [PubMed] [Google Scholar]
- 10.Goesling J, Henry MJ, Moser SE, et al. Symptoms of Depression Are Associated With Opioid Use Regardless of Pain Severity and Physical Functioning Among Treatment-Seeking Patients With Chronic Pain. The journal of pain : official journal of the American Pain Society. 2015;16(9):844–851. [DOI] [PubMed] [Google Scholar]
- 11.Janda AM, As-Sanie S, Rajala B, et al. Fibromyalgia Survey Criteria Is Associated with Increased Postoperative Opioid Consumption in Women Undergoing Hysterectomy. Anesthesiology. 2015. [DOI] [PubMed] [Google Scholar]
- 12.Brummett CM, Janda AM, Schueller CM, et al. Survey criteria for fibromyalgia independently predict increased postoperative opioid consumption after lower-extremity joint arthroplasty: a prospective, observational cohort study. Anesthesiology. 2013;119(6):1434–1443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Goesling J, Moser SE, Zaidi B, et al. Trends and Predictors of Opioid Use Following Total Knee and Total Hip Arthroplasty. Pain. 2016;In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brummett CM, Clauw DJ. Flipping the Paradigm: From Surgery-specific to Patient-driven Perioperative Analgesic Algorithms. Anesthesiology. 2015;122(4):731–733. [DOI] [PubMed] [Google Scholar]
- 15.Clauw DJ. Fibromyalgia: A Clinical Review. Jama. 2014;311(5):1547–1555. [DOI] [PubMed] [Google Scholar]
- 16.Sullivan MD, Edlund MJ, Zhang L, Unutzer J, Wells KB. Association between mental health disorders, problem drug use, and regular prescription opioid use. Arch Intern Med. 2006;166(19):2087–2093. [DOI] [PubMed] [Google Scholar]
- 17.Edlund MJ, Steffick D, Hudson T, Harris KM, Sullivan M. Risk factors for clinically recognized opioid abuse and dependence among veterans using opioids for chronic non-cancer pain. Pain. 2007;129(3):355–362. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.