Abstract
OBJECTIVE:
To assess the gingival parameters in the clear aligner treatment versus the three other types of brackets, i.e., conventional metal, conventional ceramic, and metal self-ligating.
MATERIALS AND METHODS:
Eighty patients coming for regular appointments undergoing orthodontic treatment were included. They were further divided into four groups with 20 patients in each: Group one underwent conventional brackets (CB) treatment; Group two had conventional ceramic brackets (CCB); Group three was treated with self-ligating (SL) brackets; Group four underwent with clear aligner (CA) treatment. Inclusion criteria were any patient with a minimum age of 18 years having Class II, Class III skeletal relationship, undergoing orthodontic treatment for at least 6 months with fixed orthodontic appliances (FOA) on both arches. While smokers, pregnant, diabetics, or those taking medication affecting gingival health or having cardiovascular diseases were excluded. Also excluded were patients who used antiseptic solutions or mouthwash during the past 6 months, underwent any periodontal treatments in the past 6 months, or who had fixed bridges and crowns or extensive restorations close to the gingival margins. Seven indices, namely plaque index, gingival index, gingival bleeding index, sulcus bleeding index, papillary bleeding index, basic periodontal examination index, and bleeding on probing index, were recorded for all groups.
RESULTS:
Mean age for Group 1 with CB was 26.65 ± 5.15 years, whereas it was 27.65 ± 8.15 years for Group 2 with CCB, and 26.85 ± 5.19 for Group 3 with SB. Group-4 with CA treatment had a mean age of 26.85 ± 4.83 years. Multivariate analysis and a Bonferroni correction was performed (P = 0.008). CA treatment has better periodontal parameter values compared with the CB and the CCB groups, and no significance difference with the SL brackets group.
CONCLUSION:
CA treatment has better periodontal indices levels compared to other types of orthodontic treatments such as CB and the CCB groups; no significant difference with the SL brackets group. Importance should be given to oral hygiene instructions before, during, and after the treatment.
Keywords: Clear aligners, conventional braces, fixed appliances, periodontal indices, plaque, self-ligating
Introduction
The aim of an orthodontic treatment is aesthetics and to improve the appearance of the person's smile which serves as the main motivation for individuals looking for such treatment.[1] The orthodontic treatment, however, requires the use of fixed brackets, metal wires, and certain other components which inadvertently render tooth-cleaning cumbersome. Keeping a good oral hygiene while large areas are covered by the orthodontic appliance gets rather challenging at times.[2] The orthodontic appliance itself gives the plaque more retentive areas to accumulate on, which combined with lack of proper oral hygiene procedures affects the periodontal tissues in a destructive manner.[2]
Malocclusion affects the periodontal health playing a role in plaque accumulation. Good occlusion and mastication functions are simulators to gingival tissue and the attachment apparatus. In cases where the occlusion function is improper, the chances of plaque retention and calculus existence are high, which in turn makes the patient more vulnerable to gingival inflammations and dental caries, especially cervical. Once gingival inflammation and dental caries set in, it might lead to bone loss supporting the functional teeth and narrowing of the membrane of periodontal tissue.
Supportive tissue such as bone and ligaments play an important role in tooth movement during orthodontics treatment since these treatments typically require inducing bone turnover to make the tooth move within the bone. Gingival health is considered as one of the important aspects affecting the rate of success in any orthodontic treatment; it is imperative to keep the oral health of the patient within good levels to prevent any inflammation and periodontal damage to gingiva and the supportive tissue.
The presence of plaque in the oral cavity further leads to a change in the bacterial shift. Qualitative changes in the microbiota are characterized by the growth of putative periodontal pathogens.[3] Some studies mentioned that the fixation of orthodontic appliance leads to a change in the subgingival microbial content which an increased risk of periodontal diseases.[4]
Plaque is a biofilm containing bacterial aggregates which attaches to the teeth providing it with nutrients and protection from the host defenses which make a stable environment.[5,6] Ninety percent of the plaque cells are Streptococci and/or Actinomyces.[7] Plaque accumulation includes microorganisms on the surface of the tooth caused by electrostatic interactions and Van der Waals forces, depending on the type of surface and its capacity to retain microorganisms.[8,9]
The attachment in orthodontic patients is mainly associated with the an increased risk of S. mutants and Lactobacilli colonization,[10] which further leads to periodontal diseases or loss of the supportive tissue around the moving teeth, ultimately causing failure of orthodontic treatment. The orthodontic treatment is further compromised by side effects including qualitative bacterial shift, which is associated with gingivitis and an increase in pocket depth as well as in the BOP index.
Different bracket types have different physical characteristics and clinical properties, affecting the amount of biofilm accumulation on the orthodontics device components, and consequently, gingivitis and plaque formation. Conventional brackets are used with some other components such as the elastomeric and metal ligature to fix the metal wire inside the bracket's slot. On the other hand, self-ligating brackets are type of orthodontic brackets, which can open and close the wire slot, not requiring additional elastomeric or metal ligature to clasp the wire inside braces slot.
Treatment using conventional brackets causes a higher rate of plaque accumulation coupled with the trouble of periodontal cleaning or maintaining oral hygiene.[11,12,13]
Some manufactures and researchers proposed modifying the conventional brackets into self-ligating brackets to overcome the disadvantages of the former type.[14,15,16] According to those manufactures, self-ligating brackets are less susceptible to the changes in the bacterial shift owing to their different shape and lack of metal ligatures and elastomeric in them.[17]
In 1999, a new technique within orthodontic treatment was introduced showing removable appliance being able to progressively move the teeth depending on a prior computerized treatment plan.[18] This kind of treatment considerably reduced the side effects of both self-ligating and conventional brackets by doing away with usual areas of plaque accumulation.
It remains to be seen, however, whether the adhesion of microorganisms and the shift in the plaque is reduced enough in the self-ligating brackets, which will give the orthodontic practitioner confidence to treat patients with a minimum number of periodontal diseases. It must be noted here that the clear aligner treatment is not applicable in all kinds of orthodontic treatment, which usually leads the dentists back to the use of CB and SL brackets.
There is not enough data about periodontal status in orthodontic patients in this region. The purpose of this research is to determine the gingival condition of orthodontic patients with different types of brackets and clear aligner therapy, using clinical assessment of seven gingival parameters.
Materials and Methods
It was a cross-sectional study of patients undergoing active orthodontics treatment of different types (CB, SL, CA, CCB) from different hospitals during December 2015 to February 2016. We chose equal number of participant's from each gender to eliminate such bias in our study. Eighty patients, 40 males and 40 females, were included in the study. Patients were grouped into four groups:
Group I: 20 patients (13 males, 7 females) with a mean age of 26.65 ± 5.15 years, treated with metal conventional edgewise brackets (Equilibrium 2, Dentaurum, Inspringen, Germany) ligated with a stainless-steel wire
Group II: 20 patients (9 males, 11 females) with a mean age of 27.65 ± 8.15 years, treated with ceramic conventional brackets (Damon Clear smile, USA)
Group III: 20 (10 males, 10 females) patients with a mean age of 26.85 ± 5.19 years, treated with self-ligating brackets (Tomy international Inc., Japan)
Group IV: 20 patients (8 males, 12 females) with a mean age of 26.85 ± 4.83 years treated with clear aligner treatment (Angle Align, China/Invisalign, USA).
Patients were screened and selected using the following criteria:
Inclusion: any patient with a minimum age of 18 years having Class II, Class III skeletal relationship and undergoing orthodontic treatment for at least 6 months with fixed orthodontic appliances (FOA) on both arches. Exclusion: smokers, pregnant, diabetics, or those taking medication affecting gingival health or having cardiovascular diseases were excluded. Also excluded were patients who used antiseptic solutions or mouthwash during the past 6 months, underwent any periodontal treatments in the past 6 months, or who had fixed bridges and crowns or extensive restorations close to the gingival margins.
The nature of the study was elaborated to the patients explaining the possibility of using anonymous data for study requirements. Patients were made satisfied with clear replies to any concerns they had. They were provided with a consent form prior to their clinical assessment, and were asked to sign only if they agree to participate in the study. Clinical assessments took place in different hospitals for patients who came for regular appointments.
For our study, we used the following seven periodontal indices to predict the periodontal health in all groups:
Plaque index (PI) by Silness and Loe in 1964
Gingival index (GI)
Gingival bleeding index (GBI) by Carter and Barnes (1974)
Sulcus bleeding index (SBI) 1971, Muhlemann and Son
Papillary bleeding index (PBI)
Basic periodontal examination (BPE) index
Bleeding on probing (BOP) index.
All indices were collected using special periodontal charts designed especially for the research. One calibrated examiner carried out all clinical assessments.
Statistical analysis
We used statistical Package social sciences (SPSS 22.0, Chicago IL, USA) for data analysis. Descriptive analysis was carried out to report on frequencies, mean, and standard deviation. Multivariate and a Bonferroni correction were performed (P value =< 0.008).
Results
A total of 80 patients, 40 male and 40 female, with a mean age of 27 years ± 5.88 were enrolled in the study over time. After excluding some participants, they were subdivided into four groups. The first treatment group contained 13 males and 7 females, with a mean age of 26.65 ± 5.15 years were treated with metal conventional brackets (Equilibrium2, Dentaurum, Inspringen, Germany) ligated with a stainless-steel wire. The second group consisted of 9 males and 11 females with mean age of 27.65 ± 8.15 years treated with ceramic conventional brackets (Damon Clear smile, USA/3M clarity, USA). The third group comprised 10 males and 10 females patients with a mean age of 26.85 ± 5.19 treated with self-ligating brackets (Tomy international Inc., Japan), whereas a fourth group with 8 males and 12 females had a mean age of 26.85 ± 4.83 years, and were treated with clear aligner treatment (Angle Align, China/Invisalign) [Figure 1 and Table 1].
Figure 1.
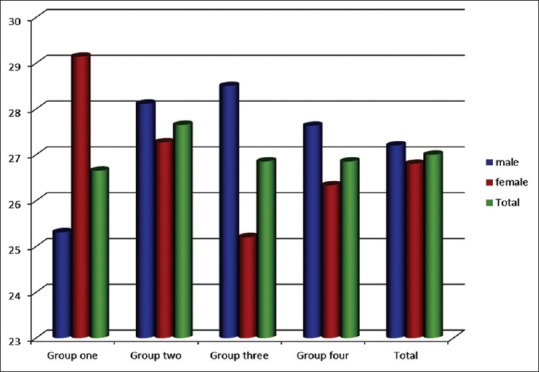
Age and gender distribution of the four groups
Table 1.
Age group and gender distribution of the four groups
| Group name | Group/age | Male | Female | Total |
|---|---|---|---|---|
| Group 1 | n | 13 | 7 | 20 |
| Age (years) | 25.3±3.8 | 29.1±6.6 | 26.6±5.1 | |
| Group 2 | n | 9 | 11 | 20 |
| Age | 28.1±7.4 | 27.2±9.0 | 27.6±8.1 | |
| Group 3 | n | 10 | 10 | 20 |
| Age | 28.5±3.0 | 25.2±6.5 | 26.8±5.1 | |
| Group 4 | n | 8 | 12 | 20 |
| Age | 27.6±5.2 | 26.3±4.7 | 26.8±4.8 | |
| Total | n | 40 | 40 | 80 |
| Age | 27.2±4.9 | 26.8±1.0 | 27±5.8 |
Plaque index
The mean PI in the first group was 1.7; in the second group it was 1.6; for the third group it was 1.5; and 0.2 for the fourth group [Table 2].
Table 2.
Periodontal indices and differences of P value of the four groups
| Indices | Group | n | Mean | SD | 1 vs 2 | 1 vs 3 | 1 vs 4 | 2 vs 3 | 2 vs 4 | 3 vs 4 |
|---|---|---|---|---|---|---|---|---|---|---|
| PI | 1 | 20 | 1.7145 | 0.36215 | 0.198 | 0.033 | 0.000 | 0.388 | 0.000 | 0.000 |
| 2 | 20 | 1.5663 | 0.49612 | |||||||
| 3 | 20 | 1.4671 | 0.33339 | |||||||
| 4 | 20 | 0.2034 | 0.18343 | |||||||
| Total | 80 | 1.2378 | 0.70330 | |||||||
| GI | 1 | 20 | 1.2622 | 0.67947 | 0.010 | 0.002 | 0.000 | 0.560 | 0.000 | 0.000 |
| 2 | 20 | 0.8541 | 0.49963 | |||||||
| 3 | 20 | 0.7642 | 0.48007 | |||||||
| 4 | 20 | 0.0080 | 0.02462 | |||||||
| Total | 80 | 0.7221 | 0.65913 | |||||||
| GBI | 1 | 20 | 11.2500 | 2.76967 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.370 |
| 2 | 20 | 4.2000 | 3.88790 | |||||||
| 3 | 20 | 0.7000 | 1.12858 | |||||||
| 4 | 20 | 0.0005 | 0.00224 | |||||||
| Total | 80 | 4.0376 | 5.09008 | |||||||
| SBI | 1 | 20 | 1.9140 | 0.68797 | 0.004 | 0.000 | 0.000 | 0.000 | 0.000 | 0.018 |
| 2 | 20 | 1.3196 | 0.93427 | |||||||
| 3 | 20 | 0.4951 | 0.53863 | |||||||
| 4 | 20 | 0.0053 | 0.02023 | |||||||
| Total | 80 | 0.9335 | 0.97033 | |||||||
| PBI | 1 | 20 | 1.6316 | 0.72593 | 0.019 | 0.000 | 0.000 | 0.002 | 0.000 | 0.015 |
| 2 | 20 | 1.1516 | 0.88115 | |||||||
| 3 | 20 | 0.5036 | 0.56073 | |||||||
| 4 | 20 | 0.0051 | 0.02015 | |||||||
| Total | 80 | 0.8230 | 0.88162 | |||||||
| PDI | 1 | 20 | 2.2036 | 0.56083 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.339 |
| 2 | 20 | 1.0822 | 0.64409 | |||||||
| 3 | 20 | 0.1390 | 0.14886 | |||||||
| 4 | 20 | 0.0071 | 0.01479 | |||||||
| Total | 80 | 0.8580 | 0.98291 | |||||||
| BOP | 1 | 20 | 0.7065 | 0.09674 | 0.193 | 0.825 | 0.704 | 0.129 | 0.094 | 0.873 |
| 2 | 20 | 3.0961 | 11.51093 | |||||||
| 3 | 20 | 0.3028 | 0.10093 | |||||||
| 4 | 20 | 0.0113 | 0.01788 | |||||||
| Total | 80 | 1.0292 | 5.77720 |
P<0.008 is a significant difference
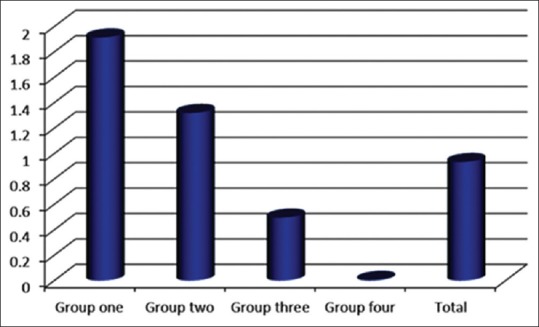
There was a significant difference between groups 1 and 4 (P value = 0.00), groups 2 and 4 (P value = 0.00), and between groups 3 and 4. There was no significance difference, however, between groups 1 and 2 (P value = 0.19), groups 1 and 3 (P value = 0.03), and group 2 and 3 (P value = 0.38) [Figure 2].
Figure 2.
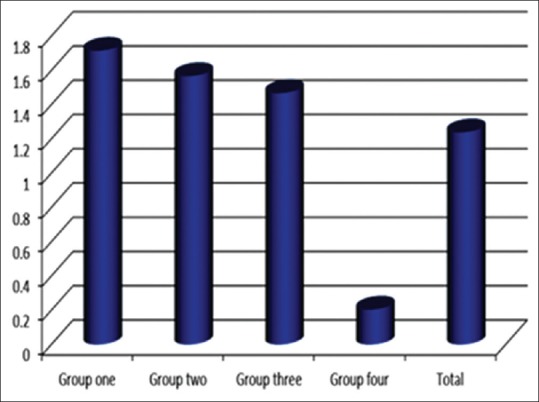
Bar diagram representing PI in four groups
Gingival index
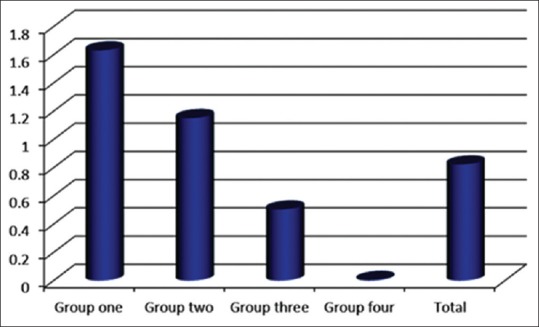
The mean GI in the first group was 1.26; in the second group it was 0.85; for the third group it was 0.76; and 0.008 in the fourth group [Table 2].
There was a significant difference between groups 1 and 3 (P value = 0.00), groups 1 and 4 (P value = 0.00), groups 2 and 4 (P value = 0.00), and groups 3 and 4 (P value = 0. 00). There was no significance difference between groups 1 and 2 (P value = 0.01), and groups 2 and 3 (P value = 0.560) [Figure 3].
Figure 3.
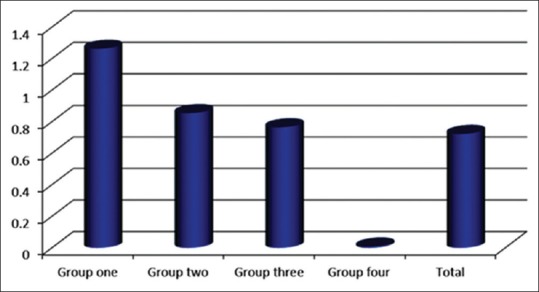
Bar diagram representing GI in four groups
Gingival bleeding index
The mean GBI in the first group was 11.25; in the second group it was 4.2; for third group it was 0.7; and 0.00 in the fourth group [Table 2].
There was significant difference between groups 1 and 2 (P value = 0.00), groups 1 and 3 (P value = 0.00), groups 1 and 4 (P value = 0.00), groups 2 and 3 (P value = 0.00), groups 2 and 4 (P value = 0.00). There was no significance difference between groups 3 and 4 (P value = 0.37) [Figure 4].
Figure 4.
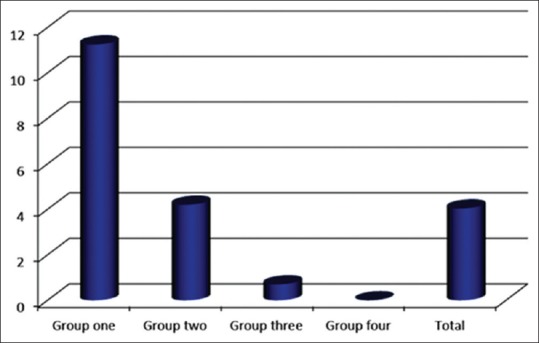
Bar diagram representing GBI in four groups
Sulcus bleeding index
The mean SBI in the first group was 1.91, in the second group it was 1.32, for the third group it was 0.49, and 0.005 for fourth group [Table 2]. There was a significant difference between groups 1 and 3 (P value = 0.00), groups 1 and 4 (P value = 0.00), and groups 2 and 4 (P value = 0.00). There was no significance difference between groups 1 and 2 (P value = 0.004), groups 2 and 3 (P value = 0.00), and between groups 3 and 4 (P value = 0.018) [Figure 5].
Figure 5.
Bar diagram representing SBI in four groups
Papillary bleeding index
The mean PBI in the first group was 1.63, in the second group it was 1.15, for the third group it was 0.5, and 0.0051 for the fourth group [Table 2].
There was statistical difference between groups 1 and 2 (P value = 0.019), groups 1 and 3 (P value = 0.00), groups 2 and 4 (P value = 0.00), and between groups 1 and 4 (P value = 0.00). There was no statistical difference between groups 2 and 3 (P value = 0.002) and between groups 3 and 4 (P value = 0.015) [Figure 6].
Figure 6.
Bar diagram representing PBI in four groups
Basic periodontal examination index
The mean BPE index in the first group was 2.2, in the second group it was 1.08, for the third group it was 0.14, and 0.007 for the fourth group [Table 2].
There was a statistical difference between groups 1 and 2 (P value = 0.000), groups 1 and 3 (P value = 0.00), groups 1 and 4 (P value = 0.00), groups 2 and 3 (P value = 0.00), and between groups 2 and 4 (P value = 0.00). There was no significant difference between groups 3 and 4 (P value = 0.34) [Figure 7].
Figure 7.
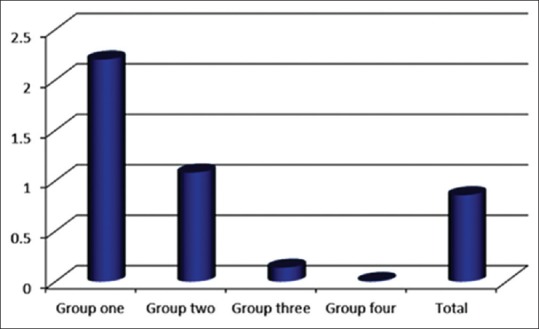
Bar diagram representing BPE in four groups
Bleeding on probing index
The mean BOP index in the first group was 0.71, in the second group it was 0.1, for the third group it was 0.30, and 0.01 for the fourth group [Table 2].
There was no significance difference between groups 1 and 2 (P value = 0.19). There was no significant difference between groups 1 and 3 (P value = 0.82), groups 1 and 4 (P value = 0.70), groups 2 and 3 (P value = 0.13), groups 2 and 4 (P value = 0.09), and between groups 3 and 4 (P value = 0.87) [Figures 8 and 9].
Figure 8.
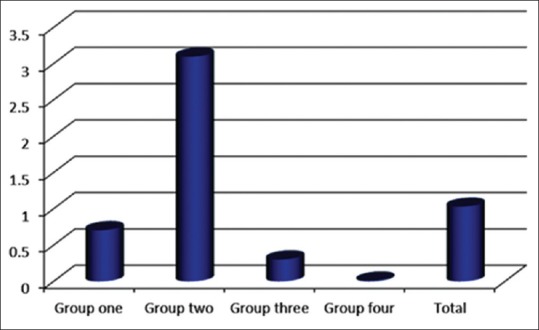
Bar diagram representing BOP in four groups
Figure 9.
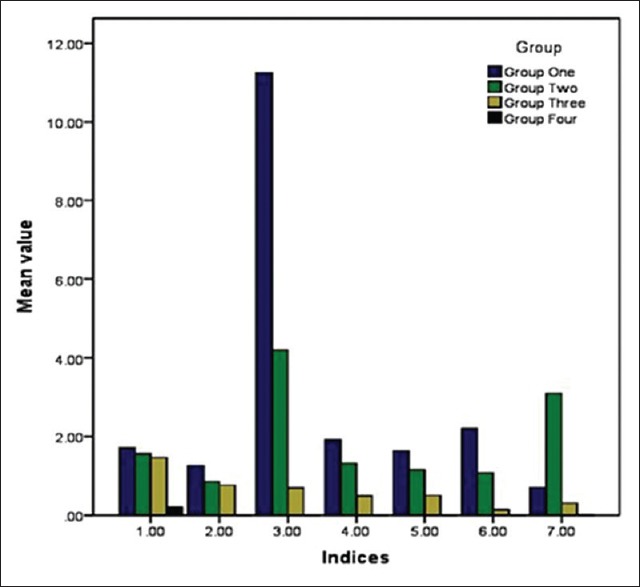
The distribution of the seven indices in the four groups
Discussion
Conventional brackets (CB) cause complications in terms of creating retention and increasing the accumulation of plaque.[19,20] In a study, during orthodontic treatment, patients with CB showed an increase level of plaque accumulation and lower levels of oral hygiene.[21,22] Other studies showed the effects on gingival health related to plastics and bonding material, which act as the retention site.[23] An increase in the plaque levels leads to enamel demineralization, which shows up as white spots, and higher levels of caries and inflammation of gingival tissues. The presence of metal ligation wires in the conventional orthodontic patients plays a role in the accumulation of dental plaque.[24]
In our study, the data showed that the PI level in the CB group was higher than the other groups in the study. The difference was significant between the CB, CCB, and CA group.
We conclude that, in CA treatment, the plaque levels were much lower than patients wearing the CB. In our data, we figured that the CA group shows better levels in all 7 indices recorded, which could be explained by the ease of access and better oral hygiene. Our findings are similar to the results reported by another recent study from 2015.[25] The study further showed significant difference between CA and SL group in PI and GI, commenting that the SL treatment also leads to better oral hygiene, which is explained by less number of modules needed to hold the brackets as well as less angels and wings. A study conducted by Pellegrini et al. in 2009 reported similar results.[26]
The BOP shows no difference in any of our groups, which might be explained by patient compliance of hygienic instructions.
The CA group of our study showed better indices levels, leading to better oral and gingival health during the treatment period, as well as better results aesthetically and functionally. A recent review reported CA treatment having good level of periodontal health indices compared with CB treatment.[27]
The BPE index in our CB group was higher and the CCB group had a significant difference over the CB. It was also higher in SL group having a statistically significant difference over the CCB group. There was no significant difference between the CA and the SL group, which could be explained by SL indices levels being lower than the CB groups and owing to the fact that SL brackets are less in size and need less accessories comparing to the CB, leading to less and similar numbers of the indices in CA.
We also noticed that, most of our female patients preferred CA treatment since it gives them an aesthetic smile during the treatment period, which is not achievable by using the metal brackets.
Even though the periodontal indices were lower in our patients with CB appliances, CB remains reliable option, as the CA treatment cannot resolve all kind of orthodontics problems.
Our study shows the important of the oral hygiene instructions and the periodontal health during the orthodontics treatment to achieve better results. We believe this is the first study to use the BPE index to assess the periodontal health in orthodontics patients.
Because our study is the first study to assess periodontal levels in patients undergoing CA orthodontic treatments in this region, we recommend further studies comparing CA periodontal health with other orthodontics treatment options. However, one of the limitations of our study are the number of patients with CA is less because of the higher cost of such treatment.
Conclusion
Compared to the same levels in the conventional brackets, the clear aligners treatment showed better periodontal indices levels (PI, GI, GBI, SBI, PBI, BPE, BOP), and in the case of self ligating brackets, it shows no significant difference comparing with clear aligners, implying that the self ligation brackets are better than other types of brackets and less than clear aligners in numbers but not significantly, due to the less accessories needed and modules (o-ties –ligature etc) and its smaller sized brackets and the absence of wings and sharp angels which reduces the accumulation of food comparing with conventional brackets which leads to better periodontal indices, clear aligners is recommended as this treatment eases the oral hygiene procedures leads to better oral hygiene.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Shaw W, O’brien K, Richmond S. Quality control in orthodontics: Factors influencing the receipt of orthodontic treatment. Br Dent J. 1991;170:66–8. doi: 10.1038/sj.bdj.4807421. [DOI] [PubMed] [Google Scholar]
- 2.Kitada K, De Toledo A, Oho T. Increase in detectable opportunistic bacteria in the oral cavity of orthodontic patients. Int J Dent Hyg. 2009;7:121–5. doi: 10.1111/j.1601-5037.2008.00333.x. [DOI] [PubMed] [Google Scholar]
- 3.Pejda S, Varga ML, Milosevic SA, Mestrovic S, Slaj M, Repic D, et al. Clinical and microbiological parameters in patients with self-ligating and conventional brackets during early phase of orthodontic treatment. Angle Orthod. 2012;83:133–9. doi: 10.2319/010412-8.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nasir N, Ali S, Bashir U, Ullah A. Effect of orthodontic treatment on periodontal health. Pak Oral Dent J. 2011;31:109–12. [Google Scholar]
- 5.Ahn SJ, Kho HS, Lee SW, Nahm DS. Roles of salivary proteins in the adherence of oral streptococci to various orthodontic brackets. J Dent Res. 2002;81:411–5. doi: 10.1177/154405910208100611. [DOI] [PubMed] [Google Scholar]
- 6.ME M, AA F, MI B. Importancia de la terapia básica pre-tratamiento ortodóncico. Rev Facultad Odontol (UBA) 2011:26. [Google Scholar]
- 7.Socransky SS, Haffajee AD. Periodontal microbial ecology. Periodontol. 2005;38:135–87. doi: 10.1111/j.1600-0757.2005.00107.x. [DOI] [PubMed] [Google Scholar]
- 8.Naranjo AA, Triviño ML, Jaramillo A, Betancourth M, Botero JE. Changes in the subgingival microbiota and periodontal parameters before and 3 months after bracket placement. Am J Orthod Dentofacial Orthop. 2006;130:275. doi: 10.1016/j.ajodo.2005.10.022. [DOI] [PubMed] [Google Scholar]
- 9.Arendorf T, Addy M. Candidal carriage and plaque distribution before, during and after removable orthodontic appliance therapy. J Clin Periodontol. 1985;12:360–8. doi: 10.1111/j.1600-051x.1985.tb00926.x. [DOI] [PubMed] [Google Scholar]
- 10.Davis SM, Plonka AB, Fulks BA, Taylor KL, Bashutski J, editors. Consequences of orthodontic treatment on periodontal health: Clinical and microbial effects. Semin Orthodont Elsevier. 2014 [Google Scholar]
- 11.Pandis N, Vlachopoulos K, Polychronopoulou A, Madianos P, Eliades T. Periodontal condition of the mandibular anterior dentition in patients with conventional and self-ligating brackets. Orthod Craniofac Res. 2008;11:211–5. doi: 10.1111/j.1601-6343.2008.00432.x. [DOI] [PubMed] [Google Scholar]
- 12.Baka ZM, Basciftci FA, Arslan U. Effects of 2 bracket and ligation types on plaque retention: A quantitative microbiologic analysis with real-time polymerase chain reaction. Am J Orthod Dentofacial Orthop. 2013;144:260–7. doi: 10.1016/j.ajodo.2013.03.022. [DOI] [PubMed] [Google Scholar]
- 13.van Gastel J, Quirynen M, Teughels W, Coucke W, Carels C. Longitudinal changes in microbiology and clinical periodontal variables after placement of fixed orthodontic appliances. J Periodontol. 2008;79:2078–86. doi: 10.1902/jop.2008.080153. [DOI] [PubMed] [Google Scholar]
- 14.Gomes SC, Varela CC, Da Veiga SL, Rösing CK, Oppermann RV. Periodontal conditions in subjects following orthodontic therapy. A preliminary study. Eur J Orthod. 2007;29:477–81. doi: 10.1093/ejo/cjm050. [DOI] [PubMed] [Google Scholar]
- 15.Karkhanechi M, Chow D, Sipkin J, Sherman D, Boylan RJ, Norman RG, et al. Periodontal status of adult patients treated with fixed buccal appliances and removable aligners over one year of active orthodontic therapy. Angle Orthod. 2012;83:146–51. doi: 10.2319/031212-217.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Abbate DG, Caria MP, Montanari P, Mannu C, Orrù G, Caprioglio A, et al. Periodontal health in teenagers treated with removable aligners and fixed orthodontic appliances. J Orofac Orthop. 2015;76:240–50. doi: 10.1007/s00056-015-0285-5. [DOI] [PubMed] [Google Scholar]
- 17.Germano F, Bramanti E, Arcuri C, Cecchetti F, Cicciù M. Atomic force microscopy of bacteria from periodontal subgingival biofilm: Preliminary study results. Eur J Dent. 2013;7:152. doi: 10.4103/1305-7456.110155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Boyd RL, Miller R, Vlaskalic V. The Invisalign system in adult orthodontics: Mild crowding and space closure cases. J Clin Orthodont. 2000;34:203–12. [Google Scholar]
- 19.Øgaard B, Rølla G, Arends J. Orthodontic appliances and enamel demineralization: Part 1. Lesion development. Am J Orthod Dentofacial Orthop. 1988;94:68–73. doi: 10.1016/0889-5406(88)90453-2. [DOI] [PubMed] [Google Scholar]
- 20.Atack NE, Sandy JR, Addy M. Periodontal and microbiological changes associated with the placement of orthodontic appliances. A review. J Periodontol. 1996;67:78–85. doi: 10.1902/jop.1996.67.2.78. [DOI] [PubMed] [Google Scholar]
- 21.Balenseifen JW, Madonia JV. A study of dental plaque in orthodontic patients. J Dent Res. 1970;49:320–4. doi: 10.1177/00220345700490022101. [DOI] [PubMed] [Google Scholar]
- 22.Heintze SD, Jost-Brinkmann PG, Loundos J. Effectiveness of three different types of electric toothbrushes compared with a manual technique in orthodontic patients. Am J Orthod Dentofacial Orthop. 1996;110:630–8. doi: 10.1016/s0889-5406(96)80040-0. [DOI] [PubMed] [Google Scholar]
- 23.Sakamaki ST, Bahn AN. Effect of orthodontic banding on localized oral lactobacilli. J Dent Res. 1968;47:275–9. doi: 10.1177/00220345680470021301. [DOI] [PubMed] [Google Scholar]
- 24.Türkkahraman H, Sayin M, Bozkurt FY, Yetkin Z, Kaya S, Önal S. Archwire ligation techniques, microbial colonization, and periodontal status in orthodontically treated patients. Angle Orthod. 2005;75:231–6. doi: 10.1043/0003-3219(2005)075<0227:ALTMCA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 25.Levrini L, Mangano A, Montanari P, Margherini S, Caprioglio A, Abbate GM. Periodontal health status in patients treated with the Invisalign® system and fixed orthodontic appliances: A 3 months clinical and microbiological evaluation. Eur J Dent. 2015;9:404. doi: 10.4103/1305-7456.163218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pellegrini P, Sauerwein R, Finlayson T, McLeod J, Covell DA, Maier T, et al. Plaque retention by self-ligating vs elastomeric orthodontic brackets: Quantitative comparison of oral bacteria and detection with adenosine triphosphate-driven bioluminescence. Am J Orthod Dentofacial Orthop. 2009;135:426. doi: 10.1016/j.ajodo.2008.12.002. [DOI] [PubMed] [Google Scholar]
- 27.Rossini G, Parrini S, Castroflorio T, Deregibus A, Debernardi CL. Periodontal health during clear aligners treatment: A systematic review. Eur J Orthod. 2015;37:539–43. doi: 10.1093/ejo/cju083. [DOI] [PubMed] [Google Scholar]


