Abstract
Objective
To evaluate long-term associations between early childhood hyperactivity and conduct problems (CP), measured using Strengths and Difficulties Questionnaire (SDQ) and risk of injury in early adolescence.
Design
Data linkage between a longitudinal birth cohort and routinely collected electronic health records.
Setting
Consenting Millennium Cohort Study (MCS) participants residing in Wales and Scotland.
Patients
3119 children who participated in the age 5 MCS interview.
Main outcome measures
Children with parent-reported SDQ scores were linked with hospital admission and Accident & Emergency (A&E) department records for injuries between ages 9 and 14 years. Negative binomial regression models adjusting for number of people in the household, lone parent, residential area, household poverty, maternal age and academic qualification, child sex, physical activity level and country of interview were fitted in the models.
Results
46% of children attended A&E or were admitted to hospital for injury, and 11% had high/abnormal scores for hyperactivity and CP. High/abnormal or borderline hyperactivity were not significantly associated with risk of injury, incidence rate ratio (IRR) with 95% CI of the high/abnormal and borderline were 0.92 (95% CI 0.74 to 1.14) and 1.16 (95% CI 0.88 to 1.52), respectively. Children with borderline CP had higher injury rates compared with those without CP (IRR 1.31, 95% CI 1.09 to 1.57).
Conclusions
Children with high/abnormal hyperactivity or CP scores were not at increased risk of injury; however, those with borderline CP had higher injury rates. Further research is needed to understand if those with difficulties receive treatment and support, which may reduce the likelihood of injuries.
Keywords: longitudinal data linkage, routine data, Strengths and Difficulties Questionnaire, hospital admission, A&E attendance
What is already known on this topic?
Childhood injury is a leading cause of avoidable mortality and morbidity and disproportionately affects children from disadvantaged backgrounds.
Children with behavioural difficulties have an increased immediate injury risk.
What this study adds?
This longitudinal data linkage study found no association between high levels of behavioural difficulties in early childhood and risk of injury in early adolescence.
Children with borderline conduct problems are at higher long-term injury risk.
Further work is needed to delineate the persistence of behavioural difficulties through childhood and their relation to support received and subsequent injury risk.
Introduction
Injury is the leading cause of mortality and ill-health in adolescence.1 2 It is more common among children from disadvantaged backgrounds and hence contributes to health inequalities.3 Every year around two million of the overall injury-related visits to Accident & Emergency (A&E) departments involve children and young people in the UK.4 Investigating modifiable factors associated with increased risk of injury is important to inform appropriate prevention strategies.
Boys, and children involved in higher level of physical activity, in families with a higher poverty level and of younger mothers are at increased risk of childhood injury.5–8 Attention-deficit hyperactive disorder (ADHD) is one of the most common neuropsychiatric disorders of childhood, with an incidence of 3% to 7% in school-aged children.9 It is characterised by a higher level of hyperactivity, impulsivity and inattention; children with ADHD are known to be accident-prone with almost a twofold increased risk of injury than children without ADHD.10 ADHD is diagnosed according to the core symptoms appearing in the DSM-5 (Diagnostic and Statistical Manual of Mental Disorders).11 Treatment comprises medication such as stimulants or selective norepinephrine reuptake inhibitors such as atomoxetine along with parent training programmes and cognitive–behavioural therapy. Children with ADHD are often unable to estimate the risks associated with their activities, elevating their risk of injuries. Previous research has suggested that hyperactivity measured by the Strengths and Difficulties Questionnaire (SDQ) is associated with an increased risk of unintentional injury.12 13 Conduct problems (CP) is another externalising behavioural difficulty, which can be conceptualised as antisocial, defiant, aggressive and criminal behavioural pattern in children, which can elevate their injury risk.11 12 The overall lifetime prevalence of CP is estimated at 9.5%,14 but in school-aged children it is around 3%15 and it is twice as prevalent in boys than girls. Treatment for CP is focused on parent training, family therapy, school behavioural supports with medication prescribed only if treating coexisting ADHD. Previous research suggests that CP is not associated with injury risk after adjusting for ADHD.16
To date, the risk association between behavioural difficulty and injury has only been investigated over relatively short periods of follow-up13 17–20 and it is unclear whether reported associations persist. Previous research also largely relied on self/proxy reports of injury, rather than objective records of injury such as A&E, general practice (GP) or hospital admission (HA) records,13 17–20 which might be affected by recall bias.21 We aimed to explore the relationship between early childhood behaviour (as measured by the SDQ), at the age of 5 years, and the risk of injury in early adolescence to identify children who might be at increased risk of future injury.
Methods
Sample
Data were analysed from the Millennium Cohort Study (MCS), a UK-wide nationally representative longitudinal birth cohort of 18 819 singleton children born between September 2000 and January 2002.22 Parents were first interviewed in the home when their child was around 9 months old, with subsequent interviews held at 3, 5, 7 and 11 years of age. At age 7, parents gave written consent to link MCS records to their child’s routine health records up to their 14th birthday. There were 13 681 singleton children who participated in the age 7 survey, 1951 and 1598 of whom were living in Wales and Scotland, respectively, at the time of interview. Consent for health record linkage was obtained for 3304 singleton children (1839 from Wales and 1465 from Scotland).
Linked cohort
Consented singleton children who participated in the third MCS survey at age 5 years were linked anonymously to their HAs and the A&E department attendances occurring between the ages of 9 and 14 years. The anonymised MCS birth cohort was linked to routinely collected health datasets stored within the privacy protecting Secure Anonymised Information Linkage (SAIL) Databank.23 24 The linkage procedure has been described in detail elsewhere.25 Of 3304 consented singleton children, 3269 were linked with their electronic health records (EHRs), of whom 1838 were from Wales and 1431 from Scotland. The study population comprised 3119 children who participated in the age 5 survey in Wales and Scotland and were linked to their health data (figure 1).
Figure 1.
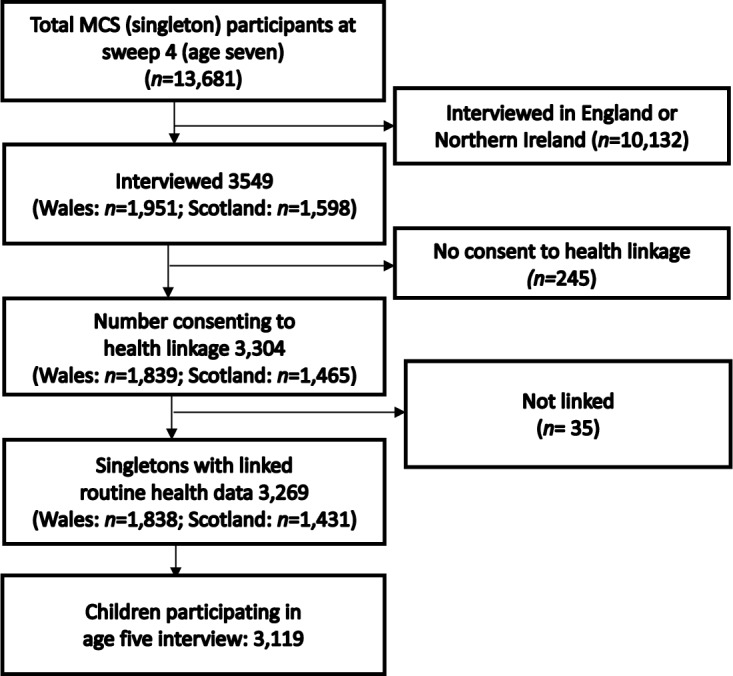
Flow chart of participants. MCS, Millennium Cohort Study.
Exposure variables
Child behavioural difficulties were assessed by parent-reported SDQ when children were 5 years old. The SDQ is an internationally validated and widely used screening tool to measure child and adolescent behavioural and emotional difficulties.26 27 In this study, two SDQ subscales were examined: hyperactivity and inattention (restless/overactive, constantly fidgeting, easily distracted, cannot stop and think before acting, lack of attention span) and CP (often has temper, tantrums, disobedience, fights with/bullies other children, often lies or cheats, steals). Each subscale has scores between 0 and 10 with higher scores indicating greater level of difficulty. In this study, we used Goodman’s proposed categorisation to assign children into one of three groups: ‘normal’ (hyperactivity: 0–5; CP: 0–2;), ‘borderline’ (hyperactivity: 6; CP: 3) or ‘high/abnormal’ (hyperactivity: 7–10; CP: 4–10).28 In this study, analyses were performed for all children who had valid hyperactivity (n=3095) and CP (n=3100) scores.
Outcome variable
The outcome variable was the frequency of injury-related HAs and/or A&E attendances occurring between the age of 9 and 14 years. We identified HA from the Patient Episode Database for Wales (PEDW) and Scottish Morbidity Records dataset for Wales and Scotland, respectively. An injury-related inpatient HA was identified from emergency admissions with an injury diagnosis International Classification of Diseases, version 10 (ICD-10) code appearing in the first diagnostic position, indicating that injury was the primary cause of admission.29 ICD-10 codes are provided in online supplementary appendix table A1.
archdischild-2019-317271supp001.pdf (77.3KB, pdf)
We identified A&E attendances from the Emergency Department dataset (EDDS) and the Scottish Accident and Emergency version 2 (A&E2) dataset for Wales and Scotland respectively. Data were collected in EDDS from 2009 and in A&E2 from 2007 onwards. To harmonise the data from both countries, the study focused on A&E attendances recorded from 2009. In addition to the ICD-10 codes, the alphanumeric treatment and diagnosis codes which map to an injury type have been included in the study30 31 to identify the A&E attendances (refer to online supplementary appendix tables A2 and A3). In this study, simultaneous presence of a patient in both harmonised HA and A&E datasets on the same day, which presumably indicates the transfer from A&E to hospital, has been considered as one record. The data were available as aggregated frequencies of injury-related HAs or A&E attendance per child between ages 9 and 14.
archdischild-2019-317271supp002.pdf (69KB, pdf)
archdischild-2019-317271supp003.pdf (76.4KB, pdf)
Covariates
The covariates considered here as confounders in the associations between child behavioural difficulties and injury risk include child’s sex, maternal age at child’s birth, maternal highest academic and vocational qualification (derived by National Vocational Qualifications standard), lone parent carer, household poverty (household income less than 60% of national median using modified Organisation for Economic Co-operation and Development scale), number of people in the household, residential area (using 2005 Rural/Urban Area Classification) and the child’s physical activity level (number of days per week they were involved in sports/exercise). With the exception of sex and maternal age at child’s birth (which were collected from age 9 months MCS interview data), these covariates were derived from age 5 MCS interview data.
Statistical analysis
We used negative binomial regression models, as the outcome variable was overdispersed, as indicated by the conditional variances being at least twice the conditional means across all categories of both hyperactivity and CP (see online supplementary appendices 4 and 5). For each SDQ scale, ‘normal’ was the reference group compared with the ‘borderline’ and ‘high/abnormal’ groups in each model. We adjusted these models for the covariates described in the previous section (model 1) and considered models with hyperactivity and CP as main exposure variables as well as a covariate (model 2). We did not contrast these two models in terms of goodness-of-fit criteria, as we were interested principally in the results from model 2, whereas model 1 offered a comparator in terms of the possible changes in the risk measure when the other exposure variable was included as a covariate. Sex-stratified models (models 3 and 4) for each exposure variable were also fitted due to higher levels of hyperactivity and CP in boys and higher levels of injury in boys in general. The models’ results were parameterised using incidence rate ratios (IRRs) with 95% CIs. Data preparation including extraction, cleaning and linkage were performed in Structured Query Language on IBM DB2 platform, with all statistical analyses performed in R version 3.3.2.32 All the models’ parameters were estimated adjusting for survey and non-response consent weights to account for oversampling, attrition between consent and non-consent to data linkage in the MCS. Survey and non-response consent weights were obtained via predicted probabilities obtained from logistic regression models taking the stratified cluster sampling design into account and adjusting for low representation of children from Wales, Scotland and Northern Ireland, disadvantaged areas and areas with high proportions of ethnic minority groups. The detailed methodological approach to derive the weight variable has been explained elsewhere.33
archdischild-2019-317271supp005.pdf (121.5KB, pdf)
archdischild-2019-317271supp004.pdf (121.8KB, pdf)
Results
Table 1 shows the demographic characteristics of the 3119 consented singleton children who participated in the third survey.
Table 1.
Characteristics of all children with linked EHRs in the study population
| n=3119* (weighted %)† |
|
| Hyperactivity | |
| Normal | 2563 (82.8) |
| Borderline | 204 (6.5) |
| High/abnormal | 328 (10.6) |
| Conduct Problems | |
| Normal | 2404 (76.1) |
| Borderline | 391 (13.4) |
| High/abnormal | 305 (10.5) |
| Sex | |
| Boy | 1604 (51.3) |
| Girl | 1515 (48.7) |
| No of people in the household | |
| 2 | 169 (6.4) |
| 3 | 564 (18.3) |
| 4 | 1420 (43.9) |
| five or more | 966 (31.4) |
| Lone parent | |
| Lone | 586 (20.4) |
| Non-lone | 2533 (79.6) |
| Residential area | |
| Rural | 756 (26.1) |
| Urban | 2360 (73.9) |
| Household poverty | |
| OECD 60% median or above | 2213 (69.1) |
| Below OECD 60% median | 894 (30.9) |
| Maternal education | |
| Degree | 635 (19.3) |
| Diplomas in Higher Education | 344 (9.9) |
| Advanced/Advanced Subsidiary/Subsidiary levels | 401 (14.4) |
| Ordinary level/General Certificate of Secondary Education | 1248 (40.0) |
| Other | 77 (2.4) |
| None | 407 (14.0) |
| Physical activity level | |
| 3 or more days a week | 411 (14.6) |
| 2 days a week | 581 (18.5) |
| 1 day a week | 872 (27.7) |
| Less often or not at all | 1246 (39.1) |
| Country | |
| Wales | 1750 (36.3) |
| Scotland | 1369 (63.7) |
| Median (IQR) | |
| Maternal age at birth (years) | 29 (24–33) |
*Missing data: hyperactivity (24, unweighted %=0.8); CP (19, unweighted %=0.6); living area (less than 5); poverty indicator (12, unweighted %=0.4); maternal education (7, unweighted %=0.2); physical activity level (9, unweighted %=0.3); maternal age at birth (less than 5).
†Weighting was based on 1 minus the probability of non-consent, multiplied by the age 7 survey weights for data linkage and scaled to the sum of the number of consenting children.
CP, conduct problem; EHR, electronic health record; OECD, Organisation for Economic Co-operation and Development.
Between ages 9 and 14 years, around 46% children had at least one HA or A&E attendance for injury (table 2). There were 2904 records of injury of which 6% were HAs and 94% were A&E attendances.
Table 2.
Number of children with injury records and number of injury-related hospital admissions or A&E attendance records combined by country
| Country | No of children with injury (out of n=3119) |
Injury admissions/attendances between 9 and 14 years |
| Wales | 866 | 1782 (HA=104; A&E=1678) |
| Scotland | 562 | 1122 (HA=70; A&E=1052) |
| Total | 1428 (45.78%) | 2904 (HA=174; A&E=2730) |
A&E, Accident & Emergency; HA, hospital admission.
Associations between SDQ scores and the risk of injury
Hyperactivity at age 5 was not associated with a higher risk of injury in adolescence after adjusting for confounders (table 3). Unadjusted borderline hyperactivity, rather than high/abnormal, were associated with injury (IRR=1.34, 95% CI 1.01 to 1.77). However, this risk attenuated after adjusting for confounding variables, and this effect was similar when CP was included as a covariate.
Table 3.
IRRs for association between hyperactivity and CPs at age 5 and subsequent hospital admissions or A&E attendances for injury between ages 9 and 14 years
| Unadjusted | Adjusted (model 1)* | Adjusted (model 2)† | ||||
| IRR (95% CI) | P value | IRR (95% CI) | P value | IRR (95% CI) | P value | |
| Hyperactivity | ||||||
| Normal | 1 | 1 | 1 | |||
| Borderline | 1.34 (1.01 to 1.77) | 0.040 | 1.21 (0.92 to 1.59) | 0.169 | 1.16 (0.88 to 1.52) | 0.299 |
| High | 1.10 (0.91 to 1.34) | 0.321 | 0.98 (0.81 to 1.19) | 0.837 | 0.92 (0.74 to 1.14) | 0.435 |
| CPs | ||||||
| Normal | 1 | 1 | 1 | |||
| Borderline | 1.38 (1.16 to 1.65) | <0.001 | 1.31 (1.09 to 1.59) | 0.003 | 1.31 (1.10 to 1.57) | 0.003 |
| High | 1.26 (1.02 to 1.56) | 0.029 | 1.12 (0.90 to 1.39) | 0.307 | 1.12 (0.89 to 1.42) | 0.326 |
*Model 1: Adjusted for child’s sex, number of people in household, lone parent, residential area, household poverty, maternal education, physical activity level, maternal age at child’s birth and country of the respondents.
†Model 2: Adjusted for child’s sex, number of people in household, lone parent, residential area, household poverty, maternal education, physical activity level, maternal age at child’s birth, country of the respondents, CP (in case of hyperactivity) and hyperactivity (in case of CP).
A&E, Accident & Emergency; CP, conduct problem; IRR, incidence rate ratio.
High/abnormal CP at age 5 were not associated with higher risk of injury in adolescence once adjustment was made for confounding factors (sex, demographic, family factors and socioeconomic variables). However, borderline CP were associated with a higher rate of injury, even when adjusting for confounding factors and hyperactivity (IRR 1.31, 95% CI 1.10 to 1.57). This was especially true for girls with borderline CP (IRR 1.37, 95% CI 1.04 to 1.8), see table 4.
Table 4.
IRRs for association between hyperactivity and conduct problems at age 5 and subsequent hospital admissions or A&E attendances for injury between ages 9 and 14 years: sex-stratified models
| Boys | Girls | |||||||
| Adjusted (model 3)* | Adjusted (model 4)† | Adjusted (model 3)* | Adjusted (model 4)† | |||||
| IRR (95% CI) | P value | IRR (95% CI) | P value | IRR (95% CI) | P value | IRR (95% CI) | P value | |
| Hyperactivity | ||||||||
| Normal | 1 | 1 | 1 | 1 | ||||
| Borderline | 1.05 (0.72 to 1.53) | 0.810 | 1.00 (0.70 to 1.44) | 0.982 | 1.42 (0.91 to 2.21) | 0.119 | 1.33 (0.86 to 2.06) | 0.194 |
| High | 0.98 (0.77 to 1.25) | 0.888 | 0.93 (0.72 to 1.20) | 0.571 | 0.99 (0.70 to 1.39) | 0.937 | 0.91 (0.62 to 1.33) | 0.618 |
| Conduct problems | ||||||||
| Normal | 1 | 1 | 1 | 1 | ||||
| Borderline | 1.27 (0.97 to 1.66) | 0.088 | 1.28 (0.98 to 1.67) | 0.068 | 1.38 (1.06 to 1.81) | 0.017 | 1.37 (1.04 to 1.80) | 0.023 |
| High | 1.07 (0.83 to 1.38) | 0.602 | 1.10 (0.85 to 1.42) | 0.465 | 1.24 (0.81 to 1.91) | 0.318 | 1.20 (0.78 to 1.85) | 0.396 |
*Model 3:Adjusted for number of people in the household, lone parent, residential area, household poverty, maternal education, physical activity level, maternal age at child’s birth and country of the respondents.
†Model 4: Adjusted for number of people in the household, lone parent, residential area, household poverty, maternal education, physical activity level, maternal age at child’s birth and country of the respondents and also adjusted for conduct problems (in case of hyperactivity) and hyperactivity (in case of conduct problems).
A&E, Accident & Emergency; IRR, incidence rate ratio.
Discussion
Our findings suggest that children with high hyperactivity and CP do not have an increased risk of subsequent injury in early adolescence. However, borderline CP, especially in girls, were associated with a greater risk of injury in adolescence. These findings differ from existing studies,12 13 19 which suggested a significant association between hyperactivity, CP and risk of injury. It is possible that these difficulties do not persist throughout childhood, reflecting either spontaneous resolution or, potentially, the effects of interventions, which include pharmacological or cognitive–behavioural treatments34 and this may reduce the subsequent injury risk over time. On the other hand, children with borderline disruptive behaviours may not get equivalent family support, parent training/family therapy and school behavioural support. Clinical guidelines for children with behavioural problems have been shown to be inconsistent and difficult to implement due to high caseloads, time pressure and lack of specialised staff.35 This may result in children with borderline problems not receiving adequate support with potential implications for persistence or worsening of their problems.
Strengths and limitations
A strength of the current study is the longitudinal linkage between routinely collected EHRs with longitudinal survey data25 which allowed us to examine prospectively recorded injury occurring between 4 and 9 years following assessment of behavioural difficulties. In the current study, we used objective measures of injury and were able to include a longer period of follow-up of the participants, thereby overcoming some of the limitations of previous studies.
However, our study does rely on parent-reported SDQ data. It is possible that parent-reported behaviours may reflect parental perceptions and their ability to cope with child behaviours and so may be subject to bias, for example, parents who are less able to cope or mothers with psychological distress may overestimate their child’s behavioural difficulties.20 36 This may explain why some high/abnormal children were not at risk of injury as their difficulties could have been overestimated by parents. Comparison with teacher assessment would have helped to validate the exposure SDQ measures.
Finally, due to the unavailability of the A&E data prior to 2009, the study included the injury records of participants’ between the ages of 9 and 14. Intervention before age 9 due to high rate of injury can reduce the subsequent injury risk, hence data prior to 2009 would have enabled us to investigate the mediating effect of early injury history on the injury risk in adolescence. In this study, GP data were not included; as we did not have GP data for participants from Scotland, we considered that A&E attendances were less likely to include ‘worried well’ parents. This study considered the first diagnostic code within PEDW to identify the cause of admission and disregarded the secondary or other diagnostic positions to avoid the inclusion of pre-existing comorbidities. This might underestimate some injuries, which were wrongly placed when recorded. In this study, the data were available at an aggregated level per child and the time to injury was not taken into consideration within the current study design. Hence we were not able to distinguish between children with many injuries over a short time frame compared with those who have had them over a longer period. In this study, the missing data for the behavioural difficulties were excluded from the analysis; however, due to the small amount of the missing data, the impact of this exclusion is negligible. Additionally, the study does not capture any injuries that do not result in any healthcare contacts; therefore, the observed association between the behavioural difficulties and injury may have been underestimated.
Conclusion
We found no evidence that high/abnormal levels of hyperactivity or CP at school entry are associated with injury risk in later childhood/early adolescence. There is some evidence that borderline CP is associated with injury risk, especially for girls. Children identified as having significant hyperactivity or CP might have received early support or treatment mitigating their risk of long-term injury in adolescence. However, those with borderline problems may also be at risk but do not receive necessary support thus maintaining their risk of injuries. Further research is needed to clarify the relation of interventions to behavioural trajectories in early childhood and to investigate whether this modifies future injury risk.
Acknowledgments
The authors are grateful to the Centre for Longitudinal Studies, UCL Institute of Education, NHS Information Standards Division and the UK Data Service. This study makes use of anonymised data held in the Secure Anonymised Information Linkage (SAIL) Databank.
Footnotes
Twitter: @residl_deviance
Contributors: RAL and SB designed the study. AB prepared and analysed the data within the SAIL Databank with support from Mario Cortina-Borja, Karen Tingay and Lucy Griffiths. AB and SB wrote the manuscript and all authors contributed to critically appraising and reviewing the manuscript. All authors approved the final manuscript.
Funding: This work was supported by the Wellcome Trust (grant no 087389/B/08/Z), Farr Institute of Health Informatics Research from the Medical Research Council (MR/K006584/1 and MR/K006525/1), Health Data Research UK (grant ref: NIWA1), Administrative Data Research – UK (ES/S007393/1), National Centre for Population Health and Wellbeing Research and Asthma UK Centre for Applied Research (AUK-AC-2012-01).
Competing interests: None declared.
Patient consent for publication: Not required.
Ethics approval: Ethics approval for the fourth survey of the MCS was received from the Northern and Yorkshire Research Ethics Committee (07/MRE03/32). This study was approved by the SAIL Information Governance Review Panel in Wales and the Public Benefit and Privacy Panel for Health and Social Care in Scotland.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available in a public, open access repository.
References
- 1. Deal LW, Gomby DS, Zippiroli L, et al. Unintentional injuries in childhood: analysis and recommendations. Future Child 2000;10:4–22. 10.2307/1602823 [DOI] [PubMed] [Google Scholar]
- 2. Prevention WHOD of I & V The injury Chartbook: a graphical overview of the global burden of injuries. Geneva: World Health Organization, 2003. [Google Scholar]
- 3. Orton E, Kendrick D, West J, et al. Persistence of health inequalities in childhood injury in the UK; a population-based cohort study of children under 5. PLoS One 2014;9:e111631 10.1371/journal.pone.0111631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. National Institute for Health and Clinical Excellence Unintentional injuries: prevention strategies for under 15S, 2010. Available: https://www.nice.org.uk/Guidance/PH29 [Accessed 4 Jul 2018].
- 5. Cheng TL, Fields CB, Brenner RA, et al. Sports injuries: an important cause of morbidity in urban youth. Pediatrics 2000;105:e32 10.1542/peds.105.3.e32 [DOI] [PubMed] [Google Scholar]
- 6. Cubbin C, Smith GS. Socioeconomic inequalities in injury: critical issues in design and analysis. Annu Rev Public Health 2002;23:349–75. 10.1146/annurev.publhealth.23.100901.140548 [DOI] [PubMed] [Google Scholar]
- 7. Orton E, Kendrick D, West J, et al. Independent risk factors for injury in pre-school children: three population-based nested case-control studies using routine primary care data. PLoS One 2012;7:e35193 10.1371/journal.pone.0035193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Villalba-Cota J, Trujillo-Hernández B, Vásquez C, et al. Causes of accidents in children aged 0–14 years and risk factors related to the family environment. Ann Trop Paediatr 2004;24:53–7. 10.1179/027249304225013259 [DOI] [PubMed] [Google Scholar]
- 9. Cormier E. Attention deficit/hyperactivity disorder: a review and update. J Pediatr Nurs 2008;23:345–57. 10.1016/j.pedn.2008.01.003 [DOI] [PubMed] [Google Scholar]
- 10. Barkley RA. Attention-deficit hyperactivity disorder : A Handbook for diagnosis and treatment. 4th edn Guilford Publications, 2014. [Google Scholar]
- 11. American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders: DSM-5TM. 5th edn Arlington: American Psychiatric Publishing, Inc, 2013. [Google Scholar]
- 12. Lalloo R, Sheiham A. Risk factors for childhood major and minor head and other injuries in a nationally representative sample. Injury 2003;34:261–6. 10.1016/S0020-1383(02)00277-2 [DOI] [PubMed] [Google Scholar]
- 13. Keyes KM, Susser E, Pilowsky DJ, et al. The health consequences of child mental health problems and parenting styles: unintentional injuries among European schoolchildren. Prev Med 2014;67:182–8. 10.1016/j.ypmed.2014.07.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Nock MK, Kazdin AE, Hiripi EVA, et al. Prevalence, subtypes, and correlates of DSM-IV conduct disorder in the National comorbidity survey replication. Psychol Med 2006;36:699–710. 10.1017/S0033291706007082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Fairchild G, Hawes DJ, Frick PJ, et al. Conduct disorder. Nat Rev Dis Primers 2019;5 10.1038/s41572-019-0095-y [DOI] [PubMed] [Google Scholar]
- 16. Schwebel DC, Roth DL, Elliott MN, et al. Association of Externalizing behavior disorder symptoms and injury among fifth graders. Acad Pediatr 2011;11:427–31. 10.1016/j.acap.2011.03.003 [DOI] [PubMed] [Google Scholar]
- 17. Bijur P, et al. Behavioral predictors of injury in school-age children. Arch Pediatr Adolesc Med 1988;142:1307–12. 10.1001/archpedi.1988.02150120061041 [DOI] [PubMed] [Google Scholar]
- 18. Rowe R, Maughan B, Goodman R, et al. Childhood psychiatric disorder and unintentional injury: findings from a national cohort study. J Pediatr Psychol 2004;29:119–30. 10.1093/jpepsy/jsh015 [DOI] [PubMed] [Google Scholar]
- 19. Lalloo R, Sheiham A, Nazroo JY. Behavioural characteristics and accidents: findings from the health survey for England, 1997. Accid Anal Prev 2003;35:661–7. 10.1016/S0001-4575(02)00044-1 [DOI] [PubMed] [Google Scholar]
- 20. Constant A, Dulioust J, Wazana A, et al. Utility of self-reported mental health measures for preventing unintentional injury: results from a cross-sectional study among French schoolchildren. BMC Pediatr 2014;14:2 10.1186/1471-2431-14-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Harel Y, Overpeck MD, Jones DH, et al. The effects of recall on estimating annual nonfatal injury rates for children and adolescents. Am J Public Health 1994;84:599–605. 10.2105/AJPH.84.4.599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Connelly R, Platt L. Cohort profile: UK millennium cohort study (mcs). Int J Epidemiol 2014;43:1719–25. 10.1093/ije/dyu001 [DOI] [PubMed] [Google Scholar]
- 23. Ford DV, Jones KH, Verplancke J-P, et al. The Sail Databank: building a national architecture for e-health research and evaluation. BMC Health Serv Res 2009;9:157 10.1186/1472-6963-9-157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Lyons RA, Jones KH, John G, et al. The Sail databank: linking multiple health and social care datasets. BMC Med Inform Decis Mak 2009;9:3 10.1186/1472-6947-9-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Tingay KS, Bandyopadhyay A, Griffiths L, et al. Linking consented cohort and routinely collected health data to enhance investigations into childhood obesity, asthma, infections, immunisations, and injuries. Int J Popul Data Sci 2019;4 10.23889/ijpds.v4i1.579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Croft S, Stride C, Maughan B, et al. Validity of the strengths and difficulties questionnaire in preschool-aged children. Pediatrics 2015;135:e1210–9. 10.1542/peds.2014-2920 [DOI] [PubMed] [Google Scholar]
- 27. Goodman A, Goodman R. Strengths and difficulties questionnaire as a dimensional measure of child mental health. J Am Acad Child Adolesc Psychiatry 2009;48:400–3. 10.1097/CHI.0b013e3181985068 [DOI] [PubMed] [Google Scholar]
- 28. Goodman R. Scoring the Strengths and Difficulties Questionnaire for age 4–17. Zugriff Am 2014;17. [Google Scholar]
- 29. World Health Organization International statistical classification of diseases and related health problems, 10th revision (ICD-10). Geneva: World Health Organ, 1992. http://www.who.int/classifications/icd/en/ (accessed 11 Jun 2018). [Google Scholar]
- 30. Lyons RA, Turner S, Lyons J, et al. All Wales Injury Surveillance System revised: development of a population-based system to evaluate single-level and multilevel interventions. Inj Prev 2016;22:i50–5. 10.1136/injuryprev-2015-041814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. NHS Wales Data Dictionary NHS Wales data dictionary. accident and emergency diagnosis types, 2017. Available: http://www.datadictionary.wales.nhs.uk/#!WordDocuments/accidentandemergencydiagnosistypes.htm [Accessed 20 Nov 2018].
- 32. R Core Team R: a language and environment for statistical computing, 2018. Available: https://www.r-project.org/ [Accessed 22 Nov 2018].
- 33. Sera F, Griffiths L, Dezateux C, et al. Technical report on the enhancement of Millennium Cohort Study data with linked electronic health recordsTechnical report on the enhancement of Millennium Cohort Study data with linked electronic health records; derivation of consent weights 2018.
- 34. Abikoff H, Klein RG. Attention-deficit hyperactivity and conduct disorder: comorbidity and implications for treatment. J Consult Clin Psychol 1992;60:881–92. 10.1037/0022-006X.60.6.881 [DOI] [PubMed] [Google Scholar]
- 35. Gatej A-R, Lamers A, van Domburgh L, et al. Perspectives on clinical guidelines for severe behavioural problems in children across Europe: a qualitative study with mental health clinicians. Eur Child Adolesc Psychiatry;57 10.1007/s00787-019-01365-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Fergusson DM, Lynskey MT, Horwood LJ. The effect of maternal depression on maternal ratings of child behavior. J Abnorm Child Psychol 1993;21:245–69. 10.1007/BF00917534 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
archdischild-2019-317271supp001.pdf (77.3KB, pdf)
archdischild-2019-317271supp002.pdf (69KB, pdf)
archdischild-2019-317271supp003.pdf (76.4KB, pdf)
archdischild-2019-317271supp005.pdf (121.5KB, pdf)
archdischild-2019-317271supp004.pdf (121.8KB, pdf)


