Abstract
Aim
To determine if ‘Defocus Incorporated Multiple Segments’ (DIMS) spectacle lenses slow childhood myopia progression.
Methods
A 2-year double-masked randomised controlled trial was carried out in 183 Chinese children aged 8–13 years, with myopia between −1.00 and −5.00 D and astigmatism ≤1.50 D. Children were randomly assigned to wear DIMS (n=93) or single vision (SV) spectacle lenses (n=90). DIMS lens incorporated multiple segments with myopic defocus of +3.50 D. Refractive error (cycloplegic autorefraction) and axial length were measured at 6month intervals.
Results
160 children completed the study, n=79 in the DIMS group and n=81 in the SV group. Average (SE) myopic progressions over 2 years were −0.41±0.06 D in the DIMS group and −0.85±0.08 D in the SV group. Mean (SE) axial elongation was 0.21±0.02 mm and 0.55±0.02 mm in the DIMS and SV groups, respectively. Myopia progressed 52% more slowly for children in the DIMS group compared with those in the SV group (mean difference −0.44±0.09 D, 95% CI −0.73 to −0.37, p<0.0001). Likewise, children in the DIMS group had less axial elongation by 62% than those in the SV group (mean difference 0.34±0.04 mm, 95% CI 0.22 to 0.37, p<0.0001). 21.5% children who wore DIMS lenses had no myopia progression over 2 years, but only 7.4% for those who wore SV lenses.
Conclusions
Daily wear of the DIMS lens significantly retarded myopia progression and axial elongation in myopic children. Our results demonstrated simultaneous clear vision with constant myopic defocus can slow myopia progression.
Trial registration number
Keywords: myopia, myopic defocus, myopia control, simultaneous vision, spectacle lens
Introduction
The increasing prevalence of myopia is reaching an alarmingly high level globally.1 2 In many parts of East and Southeast Asia, as many as 70%–80% of young adults are myopic,1–3 and as many as 20% of children are highly myopic, with refractions worse than −6 D.2 Highly myopic eyes have higher risk of developing blinding complications such as retinal degenerations4 5 and glaucoma.6 It is no doubt that epidemic of myopia debilitates both at individual level and public health level.7 8 In fact, myopia is now identified as one of immediate concerns by the WHO’s Global Initiative for the Elimination of Avoidable Blindness.8
Several clinical interventions are currently used for slowing the progression of myopia.9 10 A meta-analysis in efficacy comparison of different interventions for myopia control reported that pharmacological treatment is relatively more effective than optical methods using contact lenses or spectacles.9 10 High-dose (1%) atropine11 eye-drops are highly effective, but the associated side effects, such as photophobia and blurry vision, are not well tolerated. Lower dose (0.01%–0.1%)12–14 atropine yields similar treatment effects with less side effects. Ideally, an intervention for myopia control should be as minimally invasive as possible, making spectacle lenses the ideal alternative option.
Animal studies have provided solid evidence that imposed myopic defocus (MD) inhibits eye growth whereas hyperopic defocus promotes eye growth.15 Studies using chicks,16 17 guinea pigs,18 marmoset19 and rhesus monkey20 have demonstrated that myopic eye growth could be inhibited or reversed by applying MD using dual-power or multifocal lenses. Indeed, MD is likely be the key mechanism that underlies a number of current myopia control strategies, such as orthokeratology21 and multifocal soft contact lenses.22–24
Several years ago, we designed a concentric dual-power soft contact lens called ‘Defocus Incorporated Soft Contact’ (DISC) lens for myopia control which imposes MD on both the central and peripheral retinas.23 The clinical trial has shown the DISC lens wear significantly slowed myopia progression in schoolchildren by 25% over 2 years compared with the single vision (SV) contact lenses and 60% for a subgroup of children who have worn the lenses for more than 8 hours/day.23 We have now designed a spectacle lens based on the MD mechanism for myopia control, and named it as Defocus Incorporated Multiple Segments (DIMS) spectacle lens. This lens provides the same optical stimulus as the DISC lens without the disadvantages inherent with contact lens wear. This study aims to investigate if the DIMS lenses can slow myopia progression in schoolchildren.
Materials and methods
Study design
This study was a prospective, randomised and double-masked clinical trial conducted between August 2014 and July 2017. The subjects were randomly allocated to wear either DIMS spectacle lenses (treatment group) or SV spectacle lenses (control group). Spherical equivalent refraction (SER) and axial length (AL) were measured at baseline and every 6 months over 2 years. The changes in SER and AL between two groups were compared over the study period. Data collection and eye examinations were carried out in the Centre for Myopia Research at the Hong Kong Polytechnic University. Written assent and informed consent were obtained from the children and their parents before participation.
Subjects
Phone screening and visual screening were performed to determine whether the child met the study criteria. One hundred and eighty-three schoolchildren were recruited between August 2014 and July 2015. Inclusion criteria were:
Hong Kong Chinese.
8–13 years old.
SER: −1.00 to −5.00 dioptres (D).
Astigmatism and anisometropia of 1.50 D or less.
Monocular best corrected visual acuity (VA) of 0.00 logMAR (6/6) or better.
Acceptance of random group allocation and the masked study design.
Exclusion criteria were:
Strabismus and binocular vision abnormalities.
Ocular and systemic abnormalities.
Prior experience of myopia control.
Randomisation
Simple randomisation was implemented by the unmasked investigator (UI) by putting subject file numbers (1–200) in a spreadsheet of Excel (Microsoft Office) and creating a column of random numbers for the group allocation. Eligible subjects were then assigned to either group by following a random software sequence generated from Excel.
Sample size calculation
To achieve a 90% power to detect a 0.50D difference (0.70D of SD)23 in myopia progression between two groups with an alpha level of 0.01 (2-tailed); the minimum subject number required in each group was 59. Assuming a dropout rate of about 15%, at least 70 subjects were required in each group.
Intervention and control
The children in the treatment group wore the DIMS spectacle lenses while those in the control group wore ordinary SV spectacle lenses.
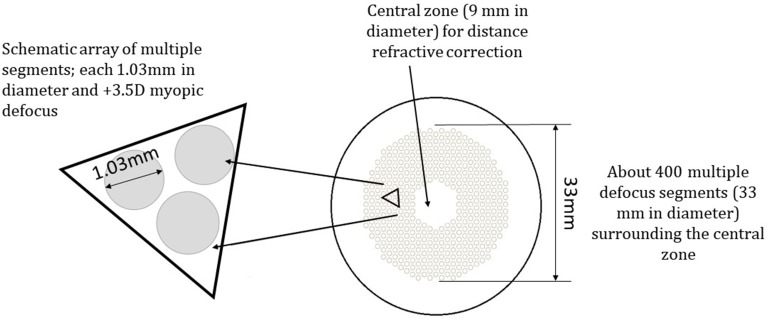
The DIMS lens is a custom-made plastic spectacle lens. It comprises a central optical zone (9 mm in diameter) for correcting distance refractive errors, and an annular multiple focal zone with multiple segments (33 mm in diameter) having a relative positive power (+3.50 D) (figure 1). The diameter of each segment is 1.03 mm. This design simultaneously introduces MD and provides clear vision for the wearer at all viewing distances. There are multiple foci from MD at a plane in front of the retina, which would be received as blur images on the retina.
Figure 1.
The design of the Defocus Incorporated Multiple Segments (DIMS) spectacle lens.
The final distance prescription was determined by the UI using cycloplegic subjective refraction measured by the masked investigator (MI). The lenses were replaced with an updated prescription when the change of SER was more than 0.50 D.
Masking and wear compliance
We adopted the same study protocol in our previous randomised controlled trials using progressive addition lenses25 and the DISC lenses.23 The UI was responsible for group allocation, spectacle-dispensing work, measuring visual performance of lenses, record keeping, data entry and compliance checking. The MI was responsible for refraction and related eye data measurement. Both the children and their parents were masked to group allocation until data analysis was completed. The masking procedures fulfilled the Consolidated Standards of Reporting Trials requirements.26 Prior to the data measurement by MI, the spectacles were removed from the children by the UI.
At spectacles delivery, the children were instructed to wear the spectacles in full-time mode, except during sleeping and taking shower. Wear compliance was monitored and checked by phone calls and questionnaires.
Outcome variables
Refraction and AL under cycloplegia were measured at baseline and at 6-month intervals for 2 years. The primary outcome was myopia progression, which was the difference between the mean cycloplegic SER at the baseline and subsequent 6-month visits for 24 months. The secondary outcome was the change of AL, which was the difference between the mean AL at the baseline and subsequent 6-month visits for 24 months.
One drop of Alcaine 0.5% followed by one to two drops of cyclopentolate HCL 1% were instilled to induce cycloplegia. Cycloplegia was confirmed by measuring the amplitude of accommodation using push-up method when accommodation was 2 D or less. Cycloplegic refraction was measured with an open-field autorefractor (Shin-Nippon NVision-K5001). AL was measured by partial coherence interferometry IOL Master (Carl Zeiss). Average of five measurements of autorefraction and AL for each eye were obtained for analysis.
Other measurements at each follow-up
Other outcomes such as distance and near VA, near phoria and accommodation lag were measured when the children were wearing full correction of distance at each 6-month follow-up.
Visual performance with the experimental lenses was also assessed. Distance and near VA, accommodation, phoria and stereopsis were measured when the subjects collected their spectacles. Vision quality, comfort and frequency of visual symptoms with lens wear were graded by the subjects themselves through questionnaires (online supplementary methods). Data between the two groups were compared.
bjophthalmol-2018-313739supp001.pdf (686KB, pdf)
Statistical analysis
There were no statistically significant differences between data from two eyes, only data of right eyes were used for analyses. Unpaired t-tests were used to compare baseline characteristics between groups when normality assumptions were preserved. Otherwise, Mann-Whitney U test for continuous data and the χ2 test for categorical data were used.
Myopia progression over 2 years was calculated as the difference between SER at the baseline and the 2-year visits. For the subjects completed the study, the changes in SER and AL between two groups were compared using unpaired t-tests. The efficacy of myopia control of DIMS lens (%) was determined by dividing the difference in myopia progression (or axial elongation) between two groups with the myopia progression (or axial elongation) in the SV group, then multiplied by 100%.
Data analysis also followed the intention-to-treated approach for the subjects lost to follow-up. Generalised estimating equations (GEE) were adopted for handling missing data. GEE, with one within-subject factor (time), one between-subject factor (group: DIMS or SV) and their interactions, was used to determine the treatment effect on two main outcomes adjusted for some covariates. These covariates included age, gender, baseline refractive error, near phoria, lag of accommodation, number of myopic parents, time spent on near works and outdoor activities. The significant covariates (p<0.05) were tested for their correlation with the changes of SER and AL independently using Pearson correlation analysis.
Results
Subject profile
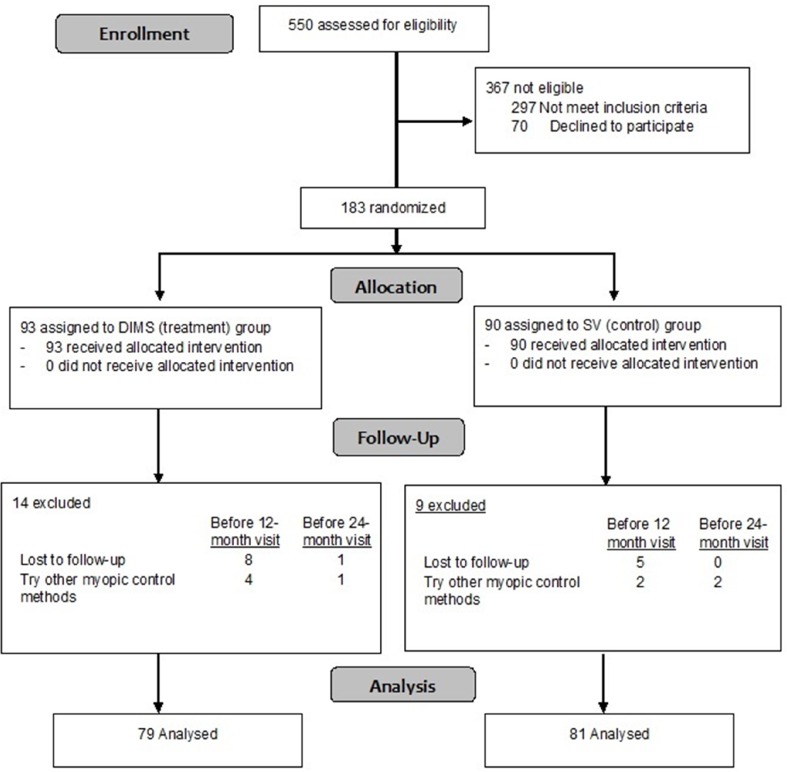
Figure 2 is a flow diagram illustrating the number of subjects recruited, enrolled and dropped out. One hundred and eighty-three eligible schoolchildren participated and were randomly allocated to the DIMS group (n=93) and the SV group (n=90). One hundred and sixty subjects successfully completed the study: 79 (85%) children in the treatment group and 81 (90%) in the control group. The dropout rate was slightly higher in the treatment group (15%) than the control group (10%) (online supplementary eTables 1 and 2). Fourteen out of 23 children dropped out early soon after the baseline data collection.
Figure 2.
A flow diagram of the study design. DIMS, Defocus Incorporated Multiple Segments spectacle lens; SV, single vision spectacle lens.
Both groups showed an overall good compliance and could wear the spectacles full time. The mean daily lens-wearing time in the DIMS group and SV group was 15.5±2.6 and 15.3±2.1 hours, respectively, and was not significantly different.
Baseline characteristics
There were no statistically significant differences between the DIMS and SV groups in the baseline characteristics (p>0.05) (table 1). The mean initial myopia in the DIMS and SV groups was −2.93±1.04 D and −2.70±0.98 D, respectively. The mean initial AL was 24.85±1.59 mm and 24.72±1.30 mm in the DIMS and SV groups, respectively.
Table 1.
Baseline demographics data of all and the completed subjects
| Baseline demographic data, mean (SD) | Mean (SD) | |||
| All | Completed | |||
| DIMS (n=93) | SV (n=90) | DIMS (n=79) | SV (n=81) | |
| Age at enrolment (years) | 10.19±1.46 | 10.01±1.44 | 10.20±1.47 | 10.00±1.45 |
| Gender | ||||
| Male, % (n) | 59.1 (55) | 55.6 (50) | 58.2 (46) | 54.3 (44) |
| Female, % (n) | 40.9 (38) | 44.4 (40) | 41.8 (33) | 45.7 (37) |
| Cycloplegic autorefraction in SER (D) | −2.93±1.04 | −2.70±0.98 | −2.97±0.97 | −2.76±0.96 |
| Axial length (mm) | 24.85±1.59 | 24.72±1.30 | 24.70±0.82 | 24.60±0.83 |
| Corneal power at steep meridian (D) | 44.46±1.67 | 44.39±1.69 | 44.5±1.61 | 44.5±1.65 |
| Corneal power at flat meridian (D) | 43.14±1.41 | 43.09±1.45 | 43.2±1.41 | 43.2±1.44 |
| Near phoria, Δ | −1.96±3.93 | −0.98±3.53 | −2.16±4.07 | −0.15±3.28 |
| Accommodation lag (D) | 0.97±0.49 | 1.06±0.40 | 0.98±0.42 | 1.04±0.35 |
| Myopics parents, n | ||||
| 0 | 3 | 6 | 2 | 5 |
| 1 | 22 | 23 | 18 | 20 |
| 2 | 68 | 61 | 59 | 56 |
Δ, prism dioptres; AL, axial length; D, dioptres;DIMS, Defocus Incorporated Multiple Segments spectacle lens; SER, spherical equivalent refraction; SV, single vision spectacle lens.
Changes in the refraction and AL
Completed subjects
For subjects who completed the 2-year trial (table 2), the mean myopia progression (SE) over 2 years in the DIMS group (n=79) and the SV group (n=81) was −0.38±0.06 D and −0.93±0.06 D, respectively. The total increase in AL was 0.21±0.02 mm and 0.53±0.03 mm, respectively. Schoolchildren wearing DIMS lenses had myopia progression significantly reduced by 59% (mean difference −0.55±0.09 D, p<0.0001) and axial elongation decreased by 60% (mean difference 0.32±0.04 mm, p<0.0001) compared with those wearing SV lenses.
Table 2.
Changes in the cycloplegic spherical equivalent refraction and axial length (from baseline) in the DIMS and the SV groups
| DIMS (n=79) | SV (n=81) | Mean difference (SE) | |
| Time/visit | SER changes in dioptres, mean (SE) | ||
| 6 months | −0.13±0.03 | −0.37±0.04 | −0.24±0.05* |
| 12 months | −0.17±0.05 | −0.55±0.04 | −0.38±0.07* |
| 18 months | −0.31±0.06 | −0.72±0.05 | −0.42±0.08* |
| 24 months | −0.38±0.06 | −0.93±0.06 | −0.55±0.09* |
| Time/visit | Changes in AL (mm), mean (SE) | ||
| 6 months | 0.03±0.01 | 0.20±0.01 | 0.16±0.02* |
| 12 months | 0.11±0.02 | 0.32±0.02 | 0.21±0.02* |
| 18 months | 0.15±0.02 | 0.43±0.02 | 0.27±0.03* |
| 24 months | 0.21±0.02 | 0.53±0.03 | 0.32±0.04* |
*Statistically significant difference between two experimental groups (unpaired t-tests, p<0.0001).
Δ, prism dioptres;D, dioptres;DIMS, Defocus Incorporated Multiple Segments spectacle lens; SER, spherical equivalent refraction; SV, single vision spectacle lens.
All enrolled subjects
Changes in SER
The mean myopia progression over 2 years in the DIMS group (n=93) and the SV group (n=90) was −0.38±0.06 D and −0.85±0.08 D, respectively. Children wearing DIMS lenses had significantly less myopia progression by 55% (mean difference −0.47±0.09 D, p<0.0001).
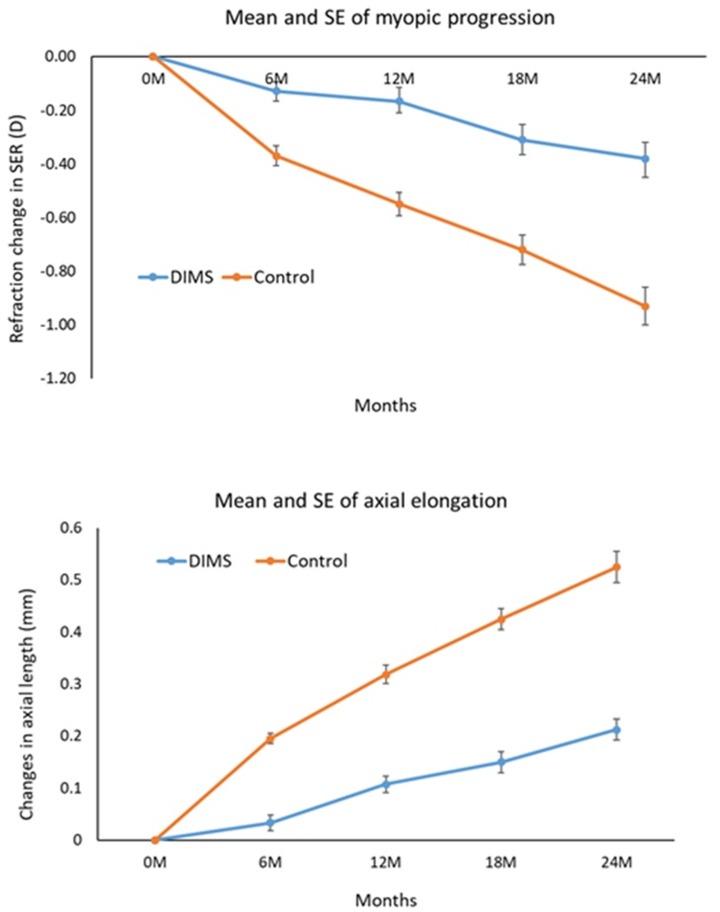
The tests of model effect (online supplementary eTable 3) indicated that group, time and age (p<0.05) had significant association with the magnitude of myopia progression. After model adjustment, the mean myopia progressions were −0.41±0.06 D in the DIMS group and −0.85±0.08 D in the SV group (online supplementary eTable 4). Children wearing DIMS lenses had significantly less myopia progression by 52% (mean difference −0.44±0.09 D, p<0.0001). Controlling for covariates did not greatly change the treatment effect compared with the unadjusted means. The DIMS lens had the greatest effect on slowing myopia progression in the first 6 months, after that, the magnitude slightly decreased at 12-month visit and was sustained to the 24-month visits (figure 3).
Figure 3.
Model-adjusted mean and SE of myopia progression and axial length from baseline to 24 months. DIMS, Defocus Incorporated Multiple Segments; SER, spherical equivalent refraction.
For Pearson correlation analysis, the changes in SER significantly correlated (r2=0.22, p<0.001) with subject’s age in the DIMS group (online supplementary eFigure 1). Myopia progression was slightly slower in older children who wore DIMS lenses. In SV group, no significant correlation was found (r2=0.04, p>0.05).
Changes in AL
The total increase in AL over 2 years was 0.21±0.02 mm and 0.56±0.02 mm in the DIMS and SV groups, respectively. The DIMS lenses significantly slowed axial elongation by 63% (mean difference 0.35 (0.04) mm, p<0.0001) as compared with the SV lenses. Group, time and age were found to be associated with AL changes. Model-adjusted mean changes in AL±SE were 0.21±0.02 mm and 0.55±0.02 mm in the DIMS and SV groups, respectively. The DIMS lens showed a significant effect on slowing axial elongation by 62% (mean difference 0.34±0.03 mm, p<0.0001).
For individual subjects
Seventeen (21.5%) out of 79 children wearing DIMS lenses had no myopia progression over 2 years (online supplementary eFigure 2), which was higher than the SV group (6 of 81, 7%). Likewise, 14% of the children wearing DIMS lenses had no axial elongation whereas all children in the SV group had axial elongation (online supplementary eFigure 3).
Visual performance with lens wear
There were no statistically significant differences between the two lens types in influencing VA and accommodation (unpaired t-test, p>0.05) (online supplementary eTable 5), except stereoacuity (p=0.04). However, the mean difference was only 5 s of arc, which is not clinically significant.
Discussion
Children wearing the DIMS spectacle lenses had myopia progression significantly reduced by 52% and axial elongation by 62% over 2 years when compared with those wearing SV lenses. The greatest treatment effect was observed during the first 6 months of lens wear. It was due to the higher myopia progression in the SV group during this time, otherwise the treatment effect was quite consistent over the 2 years (figure 3, online supplementary eTable 4). The treatment effect with the DIMS lens was similar to that achieved with 6–8 hours daily wear of DISC lens, at around 50%–60%.23 These findings are consistent with our previous animal studies17 18 and the clinical trial of the DISC lens,22 that the principle of employing MD does retard eye growth and myopia progression.
The DIMS lens design showed much better effect on slowing childhood myopia progression than existing progressive addition lenses (10%–35%),25 27–31 spectacle lens with peripheral defocus32 and contact lens33 (34%) designed for reducing relative peripheral hyperopia (online supplementary eTable 6). The efficacy of myopia control is comparable to those of orthokeratology (60%),10 21 prismatic bifocal spectacle lenses (about 50%)34 and bifocal soft contact lenses (50%–60%)10 23 35 and relatively less when compared with high and low-dose atropine (70+%).11–14
The DIMS lenses have slowed myopia progression, and have stopped myopia progression in some children (online supplementary eFigures 2 and 3). 21.5% of children in the DIMS group had no myopia progression over 2 years whereas only 7.4% in the control group. About 13% of children in the DIMS group still showed considerable progression in terms of refraction (>1 D). Such variations in retardation effect have been observed with prismatic bifocal spectacles, Cheng et al 34 showed that prismatic bifocals were more effective in the children with low accommodative lag. Also, they found that age, initial myopia and parental myopia were associated with the treatment effect. In contrast, in our study the magnitude of treatment effect was not dependent on lag of accommodation, initial myopia nor parental myopia.
Analysis of model effects indicated that age was the only associated factor that exhibited significant effect on myopia progression, and the effect of myopia control with DIMS lenses was greater in older children (aged 10–13) (online supplementary eFigure 1). About 80% of the DIMS wearers who had considerable myopia progression were younger children aged 8–9 years. We speculate that variations in treatment effect of the DIMS lenses may be due to different retinal profile or peripheral refraction among the children.36 If there is a high amount of peripheral hyperopia, the amount of effective MD at the peripheral retina will be less, and thereby minimising the treatment effect.
In our previous study, wearing time was found to be a significant factor in determining the treatment effect of DISC lenses.23 No such correlation was found in the present study. This is probably a result of the overall higher compliance, that the subjects were able to wear their assigned spectacle lenses constantly, with over 15 hours/day. The dropout rate in this study was much lower (13%) than that in our previous study using the DISC lenses (42%).23
The findings of visual performance (online supplementary eTable 5 and eFigure 4) showed that the DIMS lens could provide good vision at distance and near comparable to conventional SV spectacle lenses. Although some subjects initially noticed the slight blurriness at the mid-peripheral field, they fully adapted to the lenses in a few days. The symptoms (score below 2) such as ghost image, dizziness and headache seldom occurred during DIMS lens wear (online supplementary eFigure 5). No treatment-related adverse event was reported.
The current report includes only the first 2-year result, when the third year of the study is ongoing. Also, the current study is limited to Chinese children, further study will be needed to determine the treatment effect of the DIMS lenses in other ethnic populations. DIMS and SV lens could hardly be differentiated by their appearance unless the lens was tilted and the multiple segments may be observed from the reflection of a light source. Most children were not aware of the multiple segments features. A few children in the treatment group might recognise the multiple segments but they had no particular difficulties in using the lens as their previous spectacle lenses. Nevertheless, the study could not be totally masked for some subjects. Our study did not include children with over −5 D of myopia. The retardation effect on myopia progression in high myopes was yet to be determined. Further investigation is also required, in particular, to determine its optimal effectiveness in preventing myopia progression and incidence.
Conclusions
Daily wear of the DIMS lens significantly slowed myopia progression and axial elongation in myopic schoolchildren as compared with wearing SV spectacle lenses. They provided good vision while presenting simultaneous MD to the eyes. This intervention is simple to use and is the least invasive method compared with pharmacological or contact lens treatments. The DIMS spectacle lens offers an alternative treatment modality for myopia control.
Acknowledgments
The authors thank the employees of HOYA who participated in the calculation, ordering and manufacturing of the lenses. HOYA provided the spectacles and lenses for the study. We are grateful for advice from Professor Ian Morgan and Dr Maureen Boost, statistical advice from Dr Paul Lee and Ms Yee Mui Kwok in liaison with the parents.
Footnotes
Contributors: All the authors listed have been involved in the undertaking of the clinical trial with emphasis on various aspects, from the conception of the lens design, fabrication of the lens and registration of the clinical trial and preparation of clinical protocol to data collection and analysis, interpretation and conclusions. A few manuscripts are now in preparation by the author team.
Funding: This was a collaborative research supported by HOYA, Tokyo, Japan (PolyU grant numbers H-ZG3B and 1-87LK). In addition to the financial support, the sponsor also provided manufacturing spectacle lenses and frames. It was a joint collaboration in the design of the DIMS lens.
Competing interests: None. Patents titled ‘Spectacle Lens' in China (CN104678572 B) and in USA (US10268050 B2) were issued on 27 April 2018 and 23 April 2019 respectively.
Patient consent for publication: Not required.
Ethics approval: All aspects of the study met the tenets of the Declaration of Helsinki and were approved by the Human Subjects Ethics Subcommittee of the Hong Kong Polytechnic University.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Data are available upon request.
References
- 1. Morgan IG, Ohno-Matsui K, Saw S-M. Myopia. The Lancet 2012;379:1739–48. 10.1016/S0140-6736(12)60272-4 [DOI] [PubMed] [Google Scholar]
- 2. Holden BA, Fricke TR, Wilson DA, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology 2016;123:1036–42. 10.1016/j.ophtha.2016.01.006 [DOI] [PubMed] [Google Scholar]
- 3. Lam CS-Y, Lam C-H, Cheng SC-K, et al. Prevalence of myopia among Hong Kong Chinese schoolchildren: changes over two decades. Ophthalmic Physiol Opt 2012;32:17–24. 10.1111/j.1475-1313.2011.00886.x [DOI] [PubMed] [Google Scholar]
- 4. Vongphanit J, Mitchell P, Wang JJ. Prevalence and progression of myopic retinopathy in an older population. Ophthalmology 2002;109:704–11. 10.1016/S0161-6420(01)01024-7 [DOI] [PubMed] [Google Scholar]
- 5. Cheng SCK, Lam CSY, Yap MKH. Prevalence of myopia-related retinal changes among 12-18 year old Hong Kong Chinese high myopes. Ophthalmic Physiol Opt 2013;33:652–60. 10.1111/opo.12082 [DOI] [PubMed] [Google Scholar]
- 6. Xu L, Wang Y, Wang S, et al. High myopia and glaucoma susceptibility the Beijing eye study. Ophthalmology 2007;114:216–20. 10.1016/j.ophtha.2006.06.050 [DOI] [PubMed] [Google Scholar]
- 7. Holden B, Sankaridurg P, Smith E, et al. Myopia, an underrated global challenge to vision: Where the current data takes us on myopia control. Eye 2014;28:142–6. 10.1038/eye.2013.256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Fricke TR, Holden BA, Wilson DA, et al. Global cost of correcting vision impairment from uncorrected refractive error. Bull World Health Organ 2012;90:728–38. 10.2471/BLT.12.104034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Huang J, Wen D, Wang Q, et al. Efficacy comparison of 16 interventions for myopia control in children: a network meta-analysis. Ophthalmology 2016;123:697–708. 10.1016/j.ophtha.2015.11.010 [DOI] [PubMed] [Google Scholar]
- 10. Smith MJ, Walline JJ. Controlling myopia progression in children and adolescents. Adolesc Health Med Ther 2015;6:133–40. 10.2147/AHMT.S55834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Chua W-H, Balakrishnan V, Chan Y-H, et al. Atropine for the treatment of childhood myopia. Ophthalmology 2006;113:2285–91. 10.1016/j.ophtha.2006.05.062 [DOI] [PubMed] [Google Scholar]
- 12. Chia A, Chua W-H, Cheung Y-B, et al. Atropine for the treatment of childhood myopia: safety and efficacy of 0.5%, 0.1%, and 0.01% doses (Atropine for the Treatment of Myopia 2). Ophthalmology 2012;119:347–54. 10.1016/j.ophtha.2011.07.031 [DOI] [PubMed] [Google Scholar]
- 13. Clark TY, Clark RA. Atropine 0.01% Eyedrops Significantly Reduce the Progression of Childhood Myopia. J Ocul Pharmacol Ther 2015;31:541–5. 10.1089/jop.2015.0043 [DOI] [PubMed] [Google Scholar]
- 14. Yam JC, Jiang Y, Tang SM, et al. Low-Concentration Atropine for Myopia Progression (LAMP) Study: A Randomized, Double-Blinded, Placebo-Controlled Trial of 0.05%, 0.025%, and 0.01% Atropine Eye Drops in Myopia Control. Ophthalmology 2019;126:113–24. 10.1016/j.ophtha.2018.05.029 [DOI] [PubMed] [Google Scholar]
- 15. Wallman J, Winawer J. Homeostasis of eye growth and the question of myopia. Neuron 2004;43:447–68. 10.1016/j.neuron.2004.08.008 [DOI] [PubMed] [Google Scholar]
- 16. Liu Y, Wildsoet C. The effect of two-zone concentric bifocal spectacle lenses on refractive error development and eye growth in young chicks. Invest Ophthalmol Vis Sci 2011;52:1078–86. 10.1167/iovs.10-5716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Tse DY, Lam CS, Guggenheim JA, et al. Simultaneous defocus integration during refractive development. Invest Ophthalmol Vis Sci 2007;48:5352–9. 10.1167/iovs.07-0383 [DOI] [PubMed] [Google Scholar]
- 18. McFadden SA, Tse DY, Bowrey HE, et al. Integration of defocus by dual power Fresnel lenses inhibits myopia in the mammalian eye. Invest Ophthalmol Vis Sci 2014;55:908–17. 10.1167/iovs.13-11724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Benavente-Perez A, Nour A, Troilo D. The effect of simultaneous negative and positive defocus on eye growth and development of refractive state in marmosets. Invest Ophthalmol Vis Sci 2012;53:6479–87. 10.1167/iovs.12-9822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Arumugam B, Hung L-F, To C-H, et al. The effects of simultaneous dual focus lenses on refractive development in infant monkeys. Invest Ophthalmol Vis Sci 2014;55:7423–32. 10.1167/iovs.14-14250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Cho P, Cheung S-W. Retardation of myopia in Orthokeratology (ROMIO) study: a 2-year randomized clinical trial. Invest Ophthalmol Vis Sci 2012;53:7077–85. 10.1167/iovs.12-10565 [DOI] [PubMed] [Google Scholar]
- 22. Anstice NS, Phillips JR. Effect of dual-focus soft contact lens wear on axial myopia progression in children. Ophthalmology 2011;118:1152–61. 10.1016/j.ophtha.2010.10.035 [DOI] [PubMed] [Google Scholar]
- 23. Lam CSY, Tang WC, Tse DY-Y, et al. Defocus incorporated soft contact (DISC) lens slows myopia progression in Hong Kong Chinese schoolchildren: a 2-year randomised clinical trial. Br J Ophthalmol 2014;98:40–5. 10.1136/bjophthalmol-2013-303914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Aller TA, Liu M, Wildsoet CF. Myopia control with bifocal contact lenses: a randomized clinical trial. Optom Vis Sci 2016;93:344–52. 10.1097/OPX.0000000000000808 [DOI] [PubMed] [Google Scholar]
- 25. Edwards MH, Li RW-H, Lam CS-Y, et al. The Hong Kong progressive lens myopia control study: study design and main findings. Invest Ophthalmol Vis Sci 2002;43:2852–8. [PubMed] [Google Scholar]
- 26. Altman DG. Better reporting of randomised controlled trials: the CONSORT statement. BMJ 1996;313:570–1. 10.1136/bmj.313.7057.570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Gwiazda J, Hyman L, Hussein M, et al. A randomized clinical trial of progressive addition lenses versus single vision lenses on the progression of myopia in children. Invest Ophthalmol Vis Sci 2003;44:1492–500. 10.1167/iovs.02-0816 [DOI] [PubMed] [Google Scholar]
- 28. Hasebe S, Ohtsuki H, Nonaka T, et al. Effect of progressive addition lenses on myopia progression in Japanese children: a prospective, randomized, double-masked, crossover trial. Invest Ophthalmol Vis Sci 2008;49:2781–9. 10.1167/iovs.07-0385 [DOI] [PubMed] [Google Scholar]
- 29. Yang Z, Lan W, Ge J, et al. The effectiveness of progressive addition lenses on the progression of myopia in Chinese children. Ophthalmic Physiol Opt 2009;29:41–8. 10.1111/j.1475-1313.2008.00608.x [DOI] [PubMed] [Google Scholar]
- 30. Correction of Myopia Evaluation Trial 2 Study Group for the Pediatric Eye Disease Investigator Group Progressive-addition lenses versus single-vision lenses for slowing progression of myopia in children with high accommodative lag and near esophoria. Invest Ophthalmol Vis Sci 2011;52:2749–57. 10.1167/iovs.10-6631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Berntsen DA, Sinnott LT, Mutti DO, et al. A randomized trial using progressive addition lenses to evaluate theories of myopia progression in children with a high lag of accommodation. Invest Ophthalmol Vis Sci 2012;53:640–9. 10.1167/iovs.11-7769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Sankaridurg P, Donovan L, Varnas S, et al. Spectacle lenses designed to reduce progression of myopia: 12-month results. Optom Vis Sci 2010;87:631–41. 10.1097/OPX.0b013e3181ea19c7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Sankaridurg P, Holden B, Smith E, et al. Decrease in rate of myopia progression with a contact lens designed to reduce relative peripheral hyperopia: one-year results. Invest Ophthalmol Vis Sci 2011;52:9362–7. 10.1167/iovs.11-7260 [DOI] [PubMed] [Google Scholar]
- 34. Cheng D, Woo GC, Drobe B, et al. Effect of bifocal and prismatic bifocal spectacles on myopia progression in children: three-year results of a randomized clinical trial. JAMA Ophthalmol 2014;132:258–64. 10.1001/jamaophthalmol.2013.7623 [DOI] [PubMed] [Google Scholar]
- 35. Chamberlain P, Back A, Lazon P, et al. 3 year effectiveness of a dual-focus 1 day soft contact lens for myopia control. Contact Lens and Anterior Eye 2018;41:S71–S72. 10.1016/j.clae.2018.03.097 [DOI] [Google Scholar]
- 36. Sng CCA, Lin X-Y, Gazzard G, et al. Peripheral refraction and refractive error in Singapore Chinese children. Invest Ophthalmol Vis Sci 2011;52:1181–9. 10.1167/iovs.10-5601 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bjophthalmol-2018-313739supp001.pdf (686KB, pdf)