Abstract
Background
The sacroiliac joints (SIJs), the largest axial joints in the body, sit in between the sacrum and pelvic bones on either side. They connect the spine to the pelvis and thus facilitate load transfer from the lumbar spine to the lower extremities. The majority of low back pain (LBP) is perceived to originate from the lumbar spine; however, another likely source of LBP that is mostly overlooked is the SIJ. This study (Parts I and II) aims to evaluate the clinical and biomechanical literature to understand the anatomy, biomechanics, sexual dimorphism, and causes and mechanics of pain of the SIJ leading to conservative and surgical treatment options using instrumentation. Part II concludes with the mechanics of the devices used in minimal surgical procedures for the SIJ.
Methods
A thorough review of the literature was performed to analyze studies related to normal SIJ mechanics, as well as the effects of sex and pain on SIJ mechanics.
Results
A total of 65 studies were selected related to anatomy, biomechanical function of the SIJ, and structures that surround the joints. These studies discussed the effects of various parameters, gender, and existence of common physiological disorders on the biomechanics of the SIJ.
Conclusions
The SIJ lies between the sacrum and the ilium and connects the spine to the pelvic bones. The SIJ transfers large bending moments and compression loads to lower extremities. However, the joint does not have as much stability of its own against the shear loads but resists shear due the tight wedging of the sacrum between hip bones on either side and the band of ligaments spanning the sacrum and the hip bones. Due to these, sacrum does not exhibit much motion with respect to the ilium. The SIJ range of motion in flexion-extension is about 3°, followed by axial rotation (about 1.5°), and lateral bending (about 0.8°). The sacrum of the female pelvis is wider, more uneven, less curved, and more backward tilted, compared to the male sacrum. Moreover, women exhibit higher mobility, stresses/loads, and pelvis ligament strains compared to male SIJs. Sacroiliac pain can be due to, but not limited to, hypo- or hypermobility, extraneous compression or shearing forces, micro- or macro-fractures, soft tissue injury, inflammation, pregnancy, adjacent segment disease, leg length discrepancy, and prior lumbar fusion. These effects are well discussed in this review. This review leads to Part II, in which the literature on mechanics of the treatment options is reviewed and synthesized.
Keywords: sacroiliac joint, anatomy, biomechanics, sexual dimorphism, causes of pain, surgery
BACKGROUND
One of the most overlooked sources of low back pain (LBP) is the sacroiliac joint (SIJ) due to its complex nature and the fact that presumed radicular pain syndromes could be linked to the SIJ.1 The SIJ is the largest axial joint in the body that connects the spine to the pelvis and thus transfers load between the lumbar spine and the lower extremities.2,3 However, the joint does not have as much stability against the shear loads. There are several ligaments across the joint that support and limit the movement of the SIJ. The tight wedging of the sacrum between the hip bones and the band of ligaments surrounding the SIJs provide resistance to shear loads. Several of the largest and most powerful muscles of the body also surround the SIJ; however, these muscles don't produce its active movements.
The sacrum can move with respect to the ilium in 6 degrees of freedom, although this motion is minimal, and the joint's hyper- or hypo-mobility may cause pain emanating from the joint region. Sexual dimorphism exists in the pelvis. Men tend to have a relatively long and narrow pelvis, with a longer and more conical pelvic cavity than that of women.4 These sex differences also reflect in the biomechanics of the joint: the female SIJ has higher mobility, and more stresses, loads, and pelvis-ligament strains, compared to the male SIJ.5
Recent studies have reported a higher prevalence of LBP due to the SIJ, with some reports having estimated that the SIJ is the actual source of pain in 15% to 30% of cases.6–8 From an anatomical perspective, pathologic changes and injuries specific to different SIJ structures can result in SIJ pain. These changes or disorders include, but are not limited to, capsular and ligamentous tension, hypo- or hypermobility, extraneous compression or shearing forces, micro- or macro-fractures, soft tissue injury, and inflammation.2
Due to the high importance of the SIJ to LBP, this Part I review addresses basic anatomy, function, biomechanics, and mechanisms of pain in the SIJ. The review leads to the need for treatment options and thus Part II narrates the mechanics of treatment options specific to SIJ.
ANATOMY
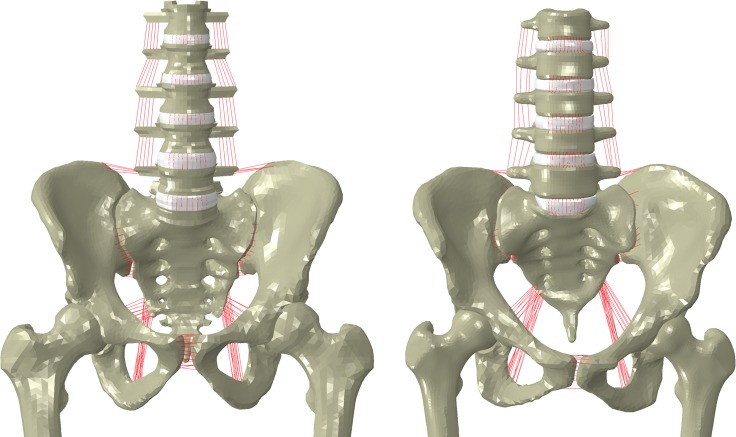
The SIJ, the largest axial joint in the body, connects the spine to the pelvis, which allows load transfer between the lumbar spine and the lower extremities.2,3 The SIJ lies between the sacrum and the ilium, spanning about 1 to 2 mm in width and a joint on either side of the sacrum is held together by a fibrous capsule (Figures 1 and 2).
Figure 1.
Articular surfaces of the sacroiliac joint.10
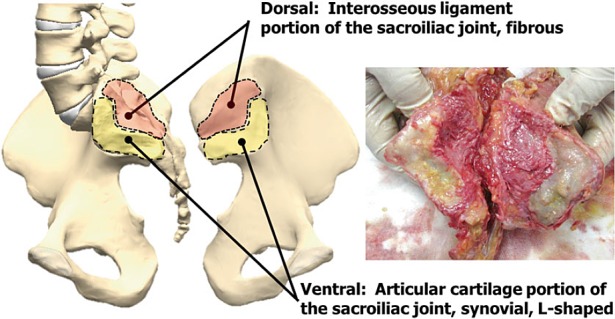
Figure 2.
(a) Posterior view, (b) anterior view and (c) sacroiliac joint cut in transverse plane. 1, 2: superior and inferior iliolumbar ligaments, respectively; 3: sacrospinous ligament; 4: sacrotuberous ligament; 5: posterior sacroiliac ligaments; 6: anterior sacroiliac ligaments; 7: sacroiliac joint; 8: interosseous ligament.11
The sacral side of the joint is covered with hyaline cartilage that is thicker (1.18 mm) than iliac cartilage (0.8 mm), which appears more fibro-cartilaginous.9 The iliac cortical bone is thicker than the sacral cortical bone (0.36 mm vs. 0.23 mm). Thus, cartilage and cortical bone thicknesses have a reverse relationship. No relationship between age and cortical bone thickness was observed by Dall et al.10 Regarding bone density, iliac cancellous bone density was greater than sacral bone in all anterior, central, and posterior parts of the joint.
Ligaments
Several ligaments depicted in Figure 2 support and limit the movement of the SIJ (see 7, Figure 2). These ligaments include the interosseous sacroiliac ligament (8), the posterior and anterior ligaments (5 and 6), and the sacrotuberous (4), sacrospinous (3) and iliolumbar ligaments (1 and 2). The interosseous ligament (8), also known as the axial ligament, connects the sacrum and ilium at the S1 and S2 levels. The long posterior sacroiliac ligament (5) is quite strong and consists of multiple bundles that pass from the lateral crest of the sacrum to the posterior superior iliac spine and the posterior end of the iliac crest. The anterior sacroiliac ligament (6) is a thin ligament. It is weaker than the posterior ligament and runs over the joint obliquely from sacrum to ilium. The sacrotuberous ligament (4) is located at the inferior-posterior part of the pelvis and runs from sacrum to the ischial tuberosity. The sacrospinous ligament's (3) attachment is behind that of the sacrotuberous ligament, and it connects the outer edge of the sacrum and coccyx to the ischia of the ilium. The iliolumbar ligament (1 and 2) originates from the tip of the fifth lumbar vertebral body to the iliac crest.11 The long posterior sacroiliac ligament (5) can stretch in periods of reduced lumbar lordosis, such as during pregnancy. Table 1 summarizes sacroiliac joint ligaments, locations, and functions.
Table 1.
Sacroiliac joint (SIJ) ligaments, locations, and functions.10
|
Ligament |
Location |
Primary Restraint |
| Posterior ligaments (5) | Posterior superior iliac spine to sacral tubercles | Sacral extension |
| Long ligament | ||
| Short ligament | ||
| Sacrotuberous (4) | Posterior superior iliac spine and sacrum to ischial tuberosity | Sacral flexion |
| Sacrospinous (3) | Apex of the sacrum to ischial spine | Sacral flexion |
| Anterior ligament (6) | Crosses ventral and caudal aspect of SIJ | Sacral flexion, axial rotation |
| Interosseous (8) | Between sacrum and ilium dorsal to SIJ | Sacral flexion, axial rotation |
| Iliolumbar (1 and 2) | Transverse process of L5 to the iliac tuberosity and crest | Lateral side bending |
| Ventral band | Ventral band | |
| Dorsal band | Forward flexion | |
| Sacroiliac part | Dorsal band |
Muscles
While no muscles are designed to act on the SIJ to produce active movements, the joint is still surrounded by some of the largest and most powerful muscles of the body. These muscles include the erector spinae, psoas, quadratus lumborum, piriformis, abdominal obliques, gluteals, hamstrings, and pelvic floor muscles (levator ani and coccygeus muscles). While they do not act directly on the SIJ, the muscles that cross the joint act on the hip or the lumbar spine.12,13 Movements of the SIJ are indirectly produced by gravity and muscles acting on the trunk and lower limbs rather than active movements of the sacrum.11 However, pelvic floor muscles (levator ani and coccygeus muscles) act to stabilize the joints. Table 2 summarizes sacroiliac joint muscles, their actions, and their effect on SIJ.
Table 2.
Sacroiliac joint (SIJ) muscles, actions, and effect on SIJ.10
|
Muscle |
Primary Action |
Effect on SIJ |
| Erector spinae | Bilateral: back extension Unilateral: side bending |
Hydraulic amplifier effect |
| Iliocostalis lumborum | ||
| Longissimus thoracis | ||
| Multifidus | Back extension, side bending, rotation | Imparts sacral flexion, force closure of SIJ with deep abdominals |
| Gluteus maximus | Hip extension, hip lateral rotation | Stabilizes SIJ |
| Piriformis | Hip lateral rotation | May alter SIJ motion via direct attachment to the ventral aspect of the sacrum |
| Biceps femoris | Hip extension, knee flexion | Long head: Imparts sacral extension via attachment to the sacrotuberous ligament |
| Deep abdominals | Compression of abdominal cavity | Forces closure of SIJ |
| Transversus abdominis | ||
| Iliacus | Hip flexion (open chain) and tilts pelvis/ sacrum ventrally (closed chain) | Synchronous tilting of the pelvis and sacrum ventrally (closed chain) |
| Pelvic floor | Support pelvic viscera | Imparts sacral extension |
| Levator ani | ||
| Coccygeus |
Summary
The SIJ, the largest axial joint in the body, lies between the sacrum and the ilium and connects the spine to the pelvis. It allows load transfer from the lumbar spine to the lower extremities. The iliac side of SIJ has thinner cartilage, thicker cortical bone, and greater cancellous bone density than the sacral side. There are several ligaments and pelvic floor muscles (levator ani and coccygeus muscles) across the joint that support and limit the movement and mobility of the SIJ and helps in transmitting shear forces. The SIJ is surrounded by some of the largest and most powerful muscles of the body; however, these muscles are not designed to produce active movements.
FUNCTION AND BIOMECHANICS
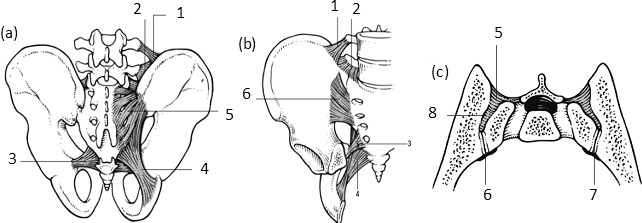
The relatively flat shape of the SIJ along with its ligaments transfers large bending moments and compression loads; however, the joint does not have as much stability against shear loads. The self-bracing mechanism consists of forces produced by muscles and ligaments, which are normal to the joint surface and loading mode of the pelvis. (This, in turn, increases compression across the SIJ and thus helps in resisting shear loads.) Figures 3a and 3b show the loading mode of the pelvis due to gravity and the free-body diagram of the self-bracing mechanism that involves normal and tangential forces of the joint surface, hip joint force, and muscle or ligament force, respectively. The friction coefficient of the SIJ surfaces is about 0.4 without grooves and ridges. Grooves and ridges allow additional resistance to protect the joint against shearing.14 It was shown that the transversus abdominis and the pelvic floor muscles (levator ani and coccygeus muscles) play a major role in SIJ stability as they increase the compression load across the SIJ to resist shear loads.15
Figure 3.
(a) Pelvis free-body diagram due to gravity. Trunk weight (Fg) and hip joint forces (Fv). (b) Free-body diagram of the self-bracing effect of the sacroiliac joint. Sacroiliac joint reaction force: normal (Fn) and tangential (Ff), ligament or muscle force (Fl), and hip joint force (Fv).14
Goudzward et al16 conducted a study on 12 human cadavers to assess the effect of the iliolumbar ligament on SIJ stability. Four different cases were tested: intact iliolumbar ligament, random dissection of iliolumbar ligament, further dissection of iliolumbar ligament, and a complete cut of the iliolumbar ligament. The rotations in the sagittal plane in response to various moments applied to the pelvis were determined. The sacral and iliac bones were fixed to the table, and a traction device to generate a tension in a string applied different moments. Eight light-reflecting markers helped to calculate the rotations in response to applied loads. The ventral side of the iliolumbar ligament decreased SIJ stability in the sagittal plane. The dorsal side and sacroiliac parts of the IL did not play significant roles in providing SIJ stability16. However, preserving the iliolumbar ligament would help to stabilize the L5-to-sacrum segment.17
The posterior sacroiliac ligaments contribute most to SIJ mobility, while the anterior sacroiliac ligament has little influence.18 The motion of the ilium with respect to the sacrum is known as nutation and counternutation, which equate to anterior sacral tilt and posterior sacral tilt, respectively. The sacrotuberous and sacrospinous ligaments resist nutation, while the long dorsal ligaments resist counternutation of the joint.19 During pregnancy, with increased laxity of SIJ ligaments, the pain is mostly experienced in long dorsal ligament due to its counteraction to the counternutation.20 Men also experience pain in this region due to its superficial location, which puts asymmetric stress on the SIJ. Although not desirable, flattening of lumbar lordosis brings about a decrease in SIJ nutation.21
A cadaveric study was done by Wang et al22 to calculate SIJ motion and the influence of anterior and posterior ligaments on SIJ stability. Four female specimens were subjected to 5 different magnitudes of eccentric compressive loads (a combination of compression, bending moment, and forward shear due to inclination angle) through the sacrum. The main motions of the sacrum were lateral rotation and nutation, which were less than 1.2°. Transverse portions of anterior sacroiliac ligament and posterior sacroiliac ligament resist lateral rotation. Also, nutation is prevented by the superior portion of the anterior and lower portion of posterior ligaments (ie, shear-resisting couple). Dissection of these 2 ligaments had a significant influence on joint stability, which decreased. Interosseous ligaments were the strongest ligaments, but their contributions to the joint's translations were quite small.
Hammer et al23 predicted that SIJ cartilage and ligaments play a significant role in pelvic stability. An increase in SIJ cartilage and interosseous ligament, iliolumbar ligament, anterior sacroiliac ligament, and posterior sacroiliac ligament stiffness values led to a decrease in the pelvic motion with highest strains at the interosseous ligament. Pubic ligaments had the least effect on the pelvic motion. These ligaments contributed to transferring loads horizontally at the acetabulum and ilium. In contrast, increasing stiffness of sacrospinous and sacrotuberous ligaments had the opposite effect, leading to an increase in the pelvic motion. They also facilitated vertical load transfer followed by sacrum translation. Moreover, in a standing position, the ligaments' strains were higher than in sitting position.
Eichenseer et al20 also evaluated the correlation between ligament stiffness and SIJ stress and motion. They showed that by decreasing ligaments' stiffness, stress and motion at the SIJ would increase. Moreover, interosseous ligaments had the highest strains under different spine motions, confirming the findings of Hammer et al.
Dujardin et al24 assessed the SIJ micromotion under a compression load applied at the ischial tuberosity. Sectioning of the sacrospinous and sacrotuberous ligaments decreased SIJ stability. Buyruk et al,25 using Doppler imaging of vibrations, showed that left and right SIJ stiffness value are different under various loading conditions. These findings suggest that there is asymmetry in the SIJ stiffness, and it may lead to the low back and pelvic pain. Rothkotter et al26 indicated that the SIJ ligamentous structure failed at 3368 N under transverse loading, and the corresponding displacement ranged from 5.5 to 6.6 mm. They reported that the self-bracing mechanism of the SIJ worked better under dorso-cranial loading than other loading directions.
Summary
The SIJ transfers large bending moments and compression loads to lower extremities; however, the joint per se does not have as much stability against the shear loads. Wedging of the sacrum and the ligaments' band afford the resistance to shear loads. Grooves and ridges allow additional resistance to protect the joint against shearing. It is shown that ventral side of the iliolumbar ligament, posterior sacroiliac ligaments, interosseous ligaments, and sacrotuberous and sacrospinous ligaments play a major role in SIJ stability, whereas pubic ligaments and anterior sacroiliac ligaments and dorsal side of iliolumbar ligaments have least effect on pelvic stability.
RANGE OF MOTION
The sacrum can move with respect to the ilium in all directions, although motion magnitudes are minimal (Figure 4). The lumbosacral pivot point is the intersection of the middle osteo-ligamentous column and the lumbosacral intervertebral disc. Placing instrumentation posterior and extending anteriorly of this pivot would provide rotational stability.4
Figure 4.
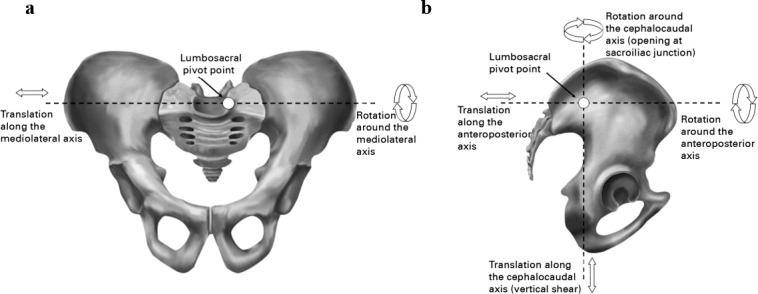
Pelvis 6 degrees of movement and lumbosacral pivot point, (a) coronal plane, (b) sagittal plane.27
While the primary function of the SIJ is to absorb and transmit forces from the spine to the pelvis, the joint is also responsible for facilitating parturition and limiting rotation around the medio-lateral axis.2,3 The SIJ is unique such that it is rather stable, and the motion of the joint is minimal.9 The magnitude of the range of motion (ROM) of the SIJ has been debated and studied extensively. The SIJ motion has been evaluated using different techniques, such as roentgen stereophotogrammetric, radiostereometric, ultrasound, and Doppler techniques.28,29 The SIJ rotations in different planes and translations along axes do not exceed ° to 3° and 2 mm, respectively.9,30 The joint's ROM in flexion-extension is about 3°. Axial rotation of the SIJ is about 1.5°, and lateral bending is about 0.8°.12 As the characteristics of the SIJ change with age, these values undergo changes.31,32 A series of cadaveric studies by Vleeming et al33,34 reported that flexion and extension rarely exceeded 2°, with an upper limit of 4°. Brunner et al35 reported that the maximum ROM, based on cadaver data, for men and women was 1.2° and 2.8°, respectively. Another study, by Sturesson et al,28 involved measuring SIJ movements in 25 patients diagnosed with SIJ pain. All movements were incredibly small with translations never exceeding 1.6 mm and an upper limit of 3° in rotations. This study also found that no differences in ROM between symptomatic and asymptomatic SIJs, which led the authors to conclude that 3-dimensional motion analysis is not a useful tool for identifying painful SIJs in most patients.28 Jacob et al36 reported mobility of SIJs of 15 healthy people using 3-dimensional stereo-photogrammetric technique. The average total rotation and translation were 1.7° and 0.7 mm, respectively. Finally, in an attempt to understand the load-displacement behavior of single and paired SIJs, Miller et al12 quantified rotations about all 3 axes for one and both ilia fixed, and with static test loads applied in the superior, lateral, anterior, and posterior directions. Movements in all planes with one leg fixed ranged between 2 and 7.8 times those measured with both legs fixed.
Summary
The sacrum can move with respect to the ilium in 6 degrees of freedom, although this motion is minimal. It is shown that the SIJ ROM is greatest in flexion-extension (about 3°), followed by axial rotation (about 1.5°), and lateral bendings (about 0.8°). The male and female SIJ ROM values are also different with the maximum ROM of 1.2° degrees (men) and 2.8° (women). Moreover, the average translation of the joint is about 0.7 mm and seldom exceeds 2 mm. In addition, the motion of the SIJ while standing on one leg is higher than when standing on both legs.
SEXUAL DIMORPHISM
Sexual dimorphism exists in the pelvis with the male pelvis being larger, a distinction that decreases in the later years of childhood. While the sacral base articular facet for the fifth lumbar vertebra occupies more than a third of the width of the sacral base in men, it occupies less than a third in women. Compared to the male sacrum, the female sacrum is wider, more uneven, less curved, and more backward tilted. Men tend to have a relatively long and narrow pelvis, with a longer and more conical pelvic cavity than that of women (Figure 5; Table 3). Women have a wider sciatic notch, and their acetabula are wider apart than those of men. In the second decade of life, women develop a groove in the iliac bone, the paraglenoidal sulcus, which usually does not occur in men. Such sex-related differences in the development of the SIJ can lead to a higher rate of SIJ misalignment in young women.21
Figure 5.
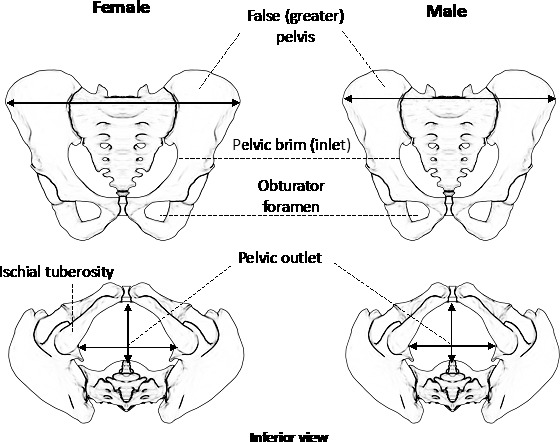
Comparison of the female and male pelvis: (top) brim (inlet) and (bottom) pelvic outlet.37
Table 3.
A biomechanical comparison of the female and male sacroiliac joint (SIJ).37
|
Biomechanical Aspects |
Female |
Male |
| SIJ motions | More rotational | More translational |
| Angular range of motions | Higher (Up to 2.8°) | Lower (Up to 1.2°) |
| Sacral cartilage | Thicker | Thinner |
| Iliac bone cortical layer | Thinner | Thicker |
| SIJ surface area | Lesser | Greater |
| Pelvis | Wider, shorter | Narrower, taller |
| Sciatic notch | Wider | Narrower |
| Acetabula | Wider | Narrower |
| Pubic angle | Larger (90° to 100°) | Smaller (50° to 80°) |
| Interosseous sacroiliac ligament | Larger | Smaller |
| Anterior sacroiliac ligaments | Smaller | Larger |
| Posterior sacroiliac ligaments | Smaller | Larger |
Female sacral cartilage (1.92 mm) is thicker than male (1.71 mm); however, they are not significantly different. Moreover, female iliac cortical bone is thinner than male iliac cortical bone.12
According to a study by Ebraheim and Biyani,38 the SIJ surface area is relatively greater in adult men than women, which consequentially allows men to withstand greater loads. While the average auricular surface area for women has been reported to range from 10.7 to 14.2 cm2,12,38 with an upper limit of 18 cm2,19 this ligamentous area for men is approximately 22.3 cm2.12 Another reason that men can withstand greater load may be that men possess significantly higher lumbar isometric strength, almost twice that of women, thus requiring more significant load transfers through the SIJs.39,40
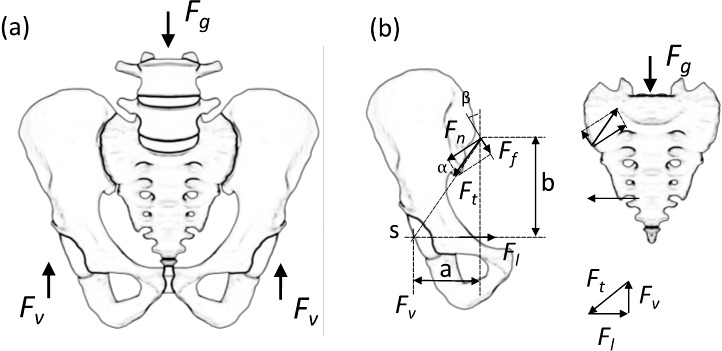
Joukar et al5 studied the biomechanical differences between male and female SIJs using finite element analysis (Figure 6). The female SIJ had higher mobility, stresses, loads, and pelvis ligament strains compared to the male SIJ. This could be a possible reason for the higher incidence of SIJ pain and the pelvic stress fracture in women.
Figure 6.
Finite element models of male (left) and female (right) of spine, pelvis, and femur.
The male and female SIJ angular ROMs are different, with the maximum ROM of 1.2° (men) and 2.8° (women).
Another significant influence on the development of particular SIJ form is the center of gravity, which is located in different positions for men and women. Compared to men, who have a more ventral center of gravity, the center of gravity in women commonly passes in front of or through the SIJ.41,42 This difference implies that men would have a greater lever arm than women, accounting for the higher loads on the joints and stronger SIJs in men.21 This characteristic also may explain why men have more restricted mobility, as the average movement for men is approximately 40% less than that of women.21,43,44
The increased mobility of the SIJ in women may be due to individual anatomical correlations. Two features that allow for higher mobility in women are the less pronounced curvature of the SIJ surfaces and a greater pubic angle compared to men. While men typically have a pubic angle of between 48° and 81°, women have an average pubic angle of 82° (64° to 100°).45 A possible reason for these differences is the facilitation of parturition in women, which involves the influence of hormones such as relaxin.2,3,46 Under the effect of relaxin, relative symphysiolysis appears to occur, and both of these factors loosen the SIJ fibrous apparatus, thus increasing mobility.21 While these unique aspects of the SIJ provide women with the necessary ability to give birth, they also may predispose women to a greater risk of pelvic pain.47–50 One factor that plays a major role in determining the severity of this predisposition involves the laxity of the female SIJs during pregnancy. According to a study by Damen et al,51 women who experience asymmetric laxity of the SIJs during pregnancy are 3 times more likely to develop moderate to severe pelvic girdle pain than women who experience symmetric laxity. As the particular form of the SIJ differs immensely between men and women, it becomes rather clear that women are more likely to develop pelvic girdle pain, and are therefore at greater risk of experiencing LBP.
Summary
Sexual dimorphism exists in the pelvis with the female sacrum being wider, more uneven, less curved, and more backward tilted. Men tend to have a relatively long and narrow pelvis, with a longer and more conical pelvic cavity than that of women. Briefly, women have a higher ROMs, thicker sacral cartilage, thinner iliac cortical bone, smaller SIJ surface area, larger interosseous sacroiliac ligaments, and smaller anterior and posterior sacroiliac ligaments. Moreover, women have higher mobility, greater stresses, greater loads, and more pelvis ligament strains compared to men. Another big difference is the influence of hormones such as relaxin in women, which increases the mobility of the SIJ by providing ligament laxity for giving birth. In summary, women are more prone to the incidences of SIJ and pelvic pain due to high mobility.
CAUSES OF SIJ PAIN
From an anatomical perspective, pathologic changes and injuries specific to different SIJ structures can result in SIJ pain. These changes include, but are not limited to, capsular and ligamentous tension, hypo- or hypermobility, extraneous compression or shearing forces, micro- or macro-fractures, soft tissue injury, and inflammation.2 The mechanism of SIJ injury primarily is due to a combination of axial loading and abrupt rotation.52 SIJ pain may also be due to injuries sustained from falling directly on the buttocks, and collisions during sports or driving. Prior medical procedures may also play a role in SIJ pain and dysfunction.
Several studies have reported that prior lumbar fusion can directly increase angular motion and stresses across the patient's SIJ, and these parameters are strongly correlated to the specific lumbar levels (one or more) fused.53 It is well known that the surgical arthrodesis at one level causes degeneration of an adjacent segment—adjacent segment disease/disorder.53–56
Limb length discrepancy (LLD), is another potential contributor to SIJ pain. Several authors have reported the correlation between LLD, LBP, and SIJ dysfunction.2,57–59 Due to the length discrepancy, the mechanical alignment of the SIJs become increasingly imbalanced, resulting in uneven load distribution across both SIJs.2,57,59
Kiapour et al60 quantified the changes in load distribution through the SIJ as a result of LLDs of 1, 2, and 3 cm. The peak loads and stresses on both legs were higher than that of the intact or normal model, with a greater magnitude consistently occurring on the longer-leg side. Furthermore, as the length discrepancies increased from 1 to 3 cm, the stresses across the SIJ increased accordingly.
Apart from injuries, prior lumbar fusion, and LLD, several other factors contribute to the gradual development of SIJ pain. These include joint infection, spondylo-arthropathies such as ankylosing spondylitis, inflammatory bowel disease,2 gait abnormalities,61 scoliosis,62 and excessive exercise.63 Regardless of the cause, the association of pain with SIJ dysfunction is rather consistent. Table 4 summarizes the causes of intra-articular and extra-articular SIJ pain.
Table 4.
Causes of intra-articular and extra-articular SIJ pain.65
| Intra-articular Pain |
| Arthritis |
| Spondyloarthropathy |
| Malignancies |
| Trauma |
| Infection |
| Extra-articular Pain |
| Ligamentous injury |
| Bone fractures |
| Malignancies |
| Myofascial pain |
| Enthesopathy |
| Trauma |
| Pregnancy |
During pregnancy, many hormonal and biomechanical changes occur, contributing to ligament laxity. One of the leading musculoskeletal changes is the increase in the mass of uterus and breasts that cause anterior displacement of the center of gravity. This effect heightens joint loads (eg, increases hip joint anterior torque by 8 times) and is aggravated by the laxity of other ligaments and other joints, which may contribute to pain and risk of injury.64
OVERALL SUMMARY
The SIJs are complex joints sitting in between the sacrum and iliac bone on either side of the pelvis. The joints play a vital role in transmitting upper body loads to lower extremities via the hip joints. The wedging of the sacrum in between pelvic bones, irregular and rough surface of the joint itself, and tight banding due to ligaments and pelvic floor muscles (levator ani and coccygeus muscles) make the SIJ extremely stable. SIJ pain can be due to, but is not limited to, capsular and ligamentous tension, hypo- or hypermobility, extraneous compression or shearing forces, and host of other factors. Other sources of pain are the surgical arthrodesis at one level causing degeneration of an adjacent segment, LLD, and spondylo-arthropathies. There are anatomical differences between the male and female pelvis, including SIJ characteristics. As well as these differences, in women, ligaments become lax during pregnancy. These factors may make women more prone to LBP. To restore quality of life and alleviate LBP due to SIJs, conservative and surgical treatments are available. Part II of the manuscript reviews the mechanics of the devices used in minimal surgical procedures.
REFERENCES
- 1.Weksler N, Velan GJ, Semionov M, et al. The role of sacroiliac joint dysfunction in the genesis of low back pain: the obvious is not always right. Arch Orthop Trauma Surg. 2007;127(10):885–888. doi: 10.1007/s00402-007-0420-x. [DOI] [PubMed] [Google Scholar]
- 2.Cohen SP. Sacroiliac joint pain: a comprehensive review of anatomy, diagnosis, and treatment. Anesth Analg. 2005;101(5):1440–1453. doi: 10.1213/01.ANE.0000180831.60169.EA. [DOI] [PubMed] [Google Scholar]
- 3.Dietrichs E. Anatomy of the pelvic joints—a review. Scand J Rheumatol Suppl. 1991;88:4–6. [PubMed] [Google Scholar]
- 4.McCord DH, Cunningham BW, Shono Y, Myers JJ, McAfee PC. Biomechanical analysis of lumbosacral fixation. Spine (Phila Pa 1976) 1992;17(8 Suppl):S235–S243. doi: 10.1097/00007632-199208001-00004. [DOI] [PubMed] [Google Scholar]
- 5.Joukar A, Shah A, Kiapour A, et al. Sex specific sacroiliac joint biomechanics during standing upright: a finite element study. Spine (Phila Pa 1976) 2018;43(18):E1053–E1060. doi: 10.1097/BRS.0000000000002623. [DOI] [PubMed] [Google Scholar]
- 6.Lingutla KK, Pollock R, Ahuja S. Sacroiliac joint fusion for low back pain: a systematic review and meta-analysis. Eur Spine J. 2016;25(6):1924–1931. doi: 10.1007/s00586-016-4490-8. [DOI] [PubMed] [Google Scholar]
- 7.Sachs D, Capobianco R. One year successful outcomes for novel sacroiliac joint arthrodesis system. Ann Surg Innov Res. 2012;6(1):13. doi: 10.1186/1750-1164-6-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schwarzer AC, Aprill CN, Bogduk N. The sacroiliac joint in chronic low back pain. Spine (Phila Pa 1976) 1995;20(1):31–37. doi: 10.1097/00007632-199501000-00007. [DOI] [PubMed] [Google Scholar]
- 9.Foley BS, Buschbacher RM. Sacroiliac joint pain: anatomy, biomechanics, diagnosis, and treatment. Am J Phys Med Rehabil. 2006;85(12):997–1006. doi: 10.1097/01.phm.0000247633.68694.c1. [DOI] [PubMed] [Google Scholar]
- 10.Dall BE, Eden SV, Rahl MD. Surgery for the Painful, Dysfunctional Sacroiliac Joint. Cham, Switzerland: Springer International Publishing; 2015. [Google Scholar]
- 11.Ombregt L, Bisschop P, Ter Veer HJ . Applied anatomy of the sacroiliac joint. In: Ombregt L, Bisschop P, Ter Veer HJ, editors. A System of Orthopedic Medicine. 694. London, England: W.B. Saunders; 1995. [Google Scholar]
- 12.Miller JA, Schultz AB, Andersson GB. Load-displacement behavior of sacroiliac joints. J Orthop Res. 1987;5(1):92–101. doi: 10.1002/jor.1100050112. [DOI] [PubMed] [Google Scholar]
- 13.Solonen KA. The sacroiliac joint in the light of anatomical, roentgenological and clinical studies. Acta Orthop Scand Suppl. 1957;27:1–127. [PubMed] [Google Scholar]
- 14.Snijders CJ, Vleeming A, Stoeckart R. Transfer of lumbosacral load to iliac bones and legs. Part 1: biomechanics of self-bracing of the sacroiliac joints and its significance for treatment and exercise. Clin Biomech (Bristol, Avon) 1993;8(6):285–294. doi: 10.1016/0268-0033(93)90002-Y. [DOI] [PubMed] [Google Scholar]
- 15.Pel JJ, Spoor CW, Pool-Goudzwaard AL, Hoek van Dijke GA, Snijders CJ. Biomechanical analysis of reducing sacroiliac joint shear load by optimization of pelvic muscle and ligament forces. Ann Biomed Eng. 2008;36(3):415–424. doi: 10.1007/s10439-007-9385-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pool-Goudzwaard A, Hoek van Dijke G, Mulder P, Spoor C, Snijders C, Stoeckart R. The iliolumbar ligament: its influence on stability of the sacroiliac joint. Clin Biomech (Bristol, Avon) 2003;18(2):99–105. doi: 10.1016/s0268-0033(02)00179-1. [DOI] [PubMed] [Google Scholar]
- 17.Yamamoto I, Panjabi MM, Oxland TR, Crisco JJ. The role of the iliolumbar ligament in the lumbosacral junction. Spine (Phila Pa 1976) 1990;15(11):1138–1141. doi: 10.1097/00007632-199011010-00010. [DOI] [PubMed] [Google Scholar]
- 18.Vrahas M, Hern TC, Diangelo D, Kellam J, Tile M. Ligamentous contributions to pelvic stability. Orthopedics. 1995;18(3):271–274. doi: 10.3928/0147-7447-19950301-09. [DOI] [PubMed] [Google Scholar]
- 19.Sashin D. A critical analysis of the anatomy and pathological changes of the sacroiliac joints. JBJS. 1930;12(4):891–910. [Google Scholar]
- 20.Eichenseer PH, Sybert DR, Cotton JR. A finite element analysis of sacroiliac joint ligaments in response to different loading conditions. Spine (Phila Pa 1976) 2011;36(22):E1446–E1452. doi: 10.1097/BRS.0b013e31820bc705. [DOI] [PubMed] [Google Scholar]
- 21.Vleeming A, Schuenke MD, Masi AT, Carreiro JE, Danneels L, Willard FH. The sacroiliac joint: an overview of its anatomy, function and potential clinical implications. J Anat. 2012;221(6):537–567. doi: 10.1111/j.1469-7580.2012.01564.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang M, Dumas GA. Mechanical behavior of the female sacroiliac joint and influence of the anterior and posterior sacroiliac ligaments under sagittal loads. Clin Biomech (Bristol, Avon) 1998;13(4–5):293–299. doi: 10.1016/s0268-0033(98)00088-6. [DOI] [PubMed] [Google Scholar]
- 23.Hammer N, Steinke H, Lingslebe U, et al. Ligamentous influence in pelvic load distribution. Spine J. 2013;13(10):1321–1330. doi: 10.1016/j.spinee.2013.03.050. [DOI] [PubMed] [Google Scholar]
- 24.Dujardin FH, Roussignol X, Hossenbaccus M, Thomine JM. Experimental study of the sacroiliac joint micromotion in pelvic disruption. J Orthop Trauma. 2002;16(2):99–103. doi: 10.1097/00005131-200202000-00005. [DOI] [PubMed] [Google Scholar]
- 25.Buyruk HM, Stam HJ, Snijders CJ, Vleeming A, Lameris JS, Holland WP. The use of color Doppler imaging for the assessment of sacroiliac joint stiffness: a study on embalmed human pelvises. Eur J Radiol. 1995;21(2):112–116. doi: 10.1016/0720-048x(95)00704-t. [DOI] [PubMed] [Google Scholar]
- 26.Rothkotter HJ, Berner W. Failure load and displacement of the human sacroiliac joint under in vitro loading. Arch Orthop Trauma Surg. 1988;107(5):283–287. doi: 10.1007/BF00451508. [DOI] [PubMed] [Google Scholar]
- 27.Berber O, Amis AA, Day AC. Biomechanical testing of a concept of posterior pelvic reconstruction in rotationally and vertically unstable fractures. J Bone Joint Surg Br. 2011;93(2):237–244. doi: 10.1302/0301-620X.93B2.24567. [DOI] [PubMed] [Google Scholar]
- 28.Sturesson B, Selvik G, Uden A. Movements of the sacroiliac joints. A roentgen stereophotogrammetric analysis. Spine (Phila Pa 1976) 1989;14(2):162–165. doi: 10.1097/00007632-198902000-00004. [DOI] [PubMed] [Google Scholar]
- 29.Vlaanderen E, Conza NE, Snijders CJ, Bouakaz A, De Jong N. Low back pain, the stiffness of the sacroiliac joint: a new method using ultrasound. Ultrasound Med Biol. 2005;31(1):39–44. doi: 10.1016/j.ultrasmedbio.2004.09.014. [DOI] [PubMed] [Google Scholar]
- 30.Zheng N, Watson LG, Yong-Hing K. Biomechanical modelling of the human sacroiliac joint. Med Biol Eng Comput. 1997;35(2):77–82. doi: 10.1007/BF02534134. [DOI] [PubMed] [Google Scholar]
- 31.Walker JM. The sacroiliac joint: a critical review. Phys Ther. 1992;72(12):903–916. doi: 10.1093/ptj/72.12.903. [DOI] [PubMed] [Google Scholar]
- 32.White AA, Panjabi MM. Clinical Biomechanics of the Spine 2nd ed. Philadelphia: JB Lippincott; 1990. [Google Scholar]
- 33.Vleeming A, Van Wingerden JP, Dijkstra PF, Stoeckart R, Snijders CJ, Stijnen T. Mobility in the sacroiliac joints in the elderly: a kinematic and radiological study. Clin Biomech (Bristol, Avon) 1992;7(3):170–176. doi: 10.1016/0268-0033(92)90032-Y. [DOI] [PubMed] [Google Scholar]
- 34.Vleeming A, Van Wingerden JP, Snijders CJ, Stoeckart R, Stijnen T. Load application to the sacrotuberous ligament; influences on sacroiliac joint mechanics. Clin Biomech. 1989;4(4):204–209. [Google Scholar]
- 35.Brunner C, Kissling R, Jacob HA. The effects of morphology and histopathologic findings on the mobility of the sacroiliac joint. Spine (Phila Pa 1976) 1991;16(9):1111–1117. doi: 10.1097/00007632-199109000-00017. [DOI] [PubMed] [Google Scholar]
- 36.Jacob HA, Kissling RO. The mobility of the sacroiliac joints in healthy volunteers between 20 and 50 years of age. Clin Biomech (Bristol, Avon) 1995;10(7):352–361. doi: 10.1016/0268-0033(95)00003-4. [DOI] [PubMed] [Google Scholar]
- 37.Tortora GJ, Derrickson BH. Introduction to the Human Body: The Essentials of Anatomy and Physiology. New York, NY: Wiley; 2006. 7th ed. [Google Scholar]
- 38.Ebraheim NA, Biyani A. Percutaneous computed tomographic stabilization of the pathologic sacroiliac joint. Clin Orthop Relat Res. 2003;(408):252–255. doi: 10.1097/00003086-200303000-00033. [DOI] [PubMed] [Google Scholar]
- 39.Graves JE, Pollock ML, Carpenter DM, et al. Quantitative assessment of full range-of-motion isometric lumbar extension strength. Spine (Phila Pa 1976) 1990;15(4):289–294. doi: 10.1097/00007632-199004000-00008. [DOI] [PubMed] [Google Scholar]
- 40.Masi AT. Do sex hormones play a role in ankylosing spondylitis? Rheum Dis Clin North Am. 1992;18(1):153–176. [PubMed] [Google Scholar]
- 41.Bellamy N, Park W, Rooney PJ. What do we know about the sacroiliac joint? Semin Arthritis Rheum. 1983;12(3):282–313. doi: 10.1016/0049-0172(83)90011-2. [DOI] [PubMed] [Google Scholar]
- 42.Tichauer ER, Miller M, Nathan IM. Lordosimetry: a new technique for the measurement of postural response to materials handling. Am Ind Hyg Assoc J. 1973;34(1):1–12. doi: 10.1080/0002889738506800. [DOI] [PubMed] [Google Scholar]
- 43.Sturesson B, Uden A, Vleeming A. A radiostereometric analysis of movements of the sacroiliac joints during the standing hip flexion test. Spine (Phila Pa 1976) 2000;25(3):364–368. doi: 10.1097/00007632-200002010-00018. [DOI] [PubMed] [Google Scholar]
- 44.Sturesson B, Uden A, Vleeming A. A radiostereometric analysis of the movements of the sacroiliac joints in the reciprocal straddle position. Spine (Phila Pa 1976) 2000;25(2):214–217. doi: 10.1097/00007632-200001150-00012. [DOI] [PubMed] [Google Scholar]
- 45.Karakas HM, Harma A, Alicioglu B. The subpubic angle in sex determination: anthropometric measurements and analyses on Anatolian Caucasians using multidetector computed tomography datasets. J Forensic Leg Med. 2013;20(8):1004–1009. doi: 10.1016/j.jflm.2013.08.013. [DOI] [PubMed] [Google Scholar]
- 46.Ross J. Is the sacroiliac joint mobile and how should it be treated? Br J Sports Med. 2000;34(3):226. doi: 10.1136/bjsm.34.3.226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Borell U, Fernstrom I. The movements at the sacro-iliac joints and their importance to changes in the pelvic dimensions during parturition. Acta Obstet Gynecol Scand. 1957;36(1):42–57. doi: 10.3109/00016345709158023. [DOI] [PubMed] [Google Scholar]
- 48.Brooke R. The sacro-iliac joint. J Anat. 1924;58(Pt 4):299–305. [PMC free article] [PubMed] [Google Scholar]
- 49.Chamberlain WE. The symphysis pubis in the roentgen examination of the sacroiliac joint. Am J Roentgenol Radium Ther. 1930;24(6):621–625. [Google Scholar]
- 50.Hisaw FL. The influence of the ovary on the resorption of the pubic bones of the pocket gopher, Geomys bursarius. J Exp Zool. 1925;42(4):411–441. [Google Scholar]
- 51.Damen L, Buyruk HM, Guler-Uysal F, Lotgering FK, Snijders CJ, Stam HJ. Pelvic pain during pregnancy is associated with asymmetric laxity of the sacroiliac joints. Acta Obstet Gynecol Scand. 2001;80(11):1019–1024. doi: 10.1034/j.1600-0412.2001.801109.x. [DOI] [PubMed] [Google Scholar]
- 52.Dreyfuss PC, Cole AJ, Pauza K. Sacroiliac joint injection techniques. Phys Med Rehabil Clin North Am. 1995;6(4):785–813. [Google Scholar]
- 53.Ivanov AA, Kiapour A, Ebraheim NA, Goel V. Lumbar fusion leads to increases in angular motion and stress across sacroiliac joint: a finite element study. Spine (Phila Pa 1976) 2009;34(5):E162–E169. doi: 10.1097/BRS.0b013e3181978ea3. [DOI] [PubMed] [Google Scholar]
- 54.Ha KY, Lee JS, Kim KW. Degeneration of sacroiliac joint after instrumented lumbar or lumbosacral fusion: a prospective cohort study over five-year follow-up. Spine (Phila Pa 1976) 2008;33(11):1192–1198. doi: 10.1097/BRS.0b013e318170fd35. [DOI] [PubMed] [Google Scholar]
- 55.Hilibrand AS, Robbins M. Adjacent segment degeneration and adjacent segment disease: the consequences of spinal fusion? Spine J. 2004;4(6 Suppl):190S–194S. doi: 10.1016/j.spinee.2004.07.007. [DOI] [PubMed] [Google Scholar]
- 56.Park P, Garton HJ, Gala VC, Hoff JT, McGillicuddy JE. Adjacent segment disease after lumbar or lumbosacral fusion: review of the literature. Spine (Phila Pa 1976) 2004;29(17):1938–1944. doi: 10.1097/01.brs.0000137069.88904.03. [DOI] [PubMed] [Google Scholar]
- 57.Golightly YM, Tate JJ, Burns CB, Gross MT. Changes in pain and disability secondary to shoe lift intervention in subjects with limb length inequality and chronic low back pain: a preliminary report. J Orthop Sports Phys Ther. 2007;37(7):380–388. doi: 10.2519/jospt.2007.2429. [DOI] [PubMed] [Google Scholar]
- 58.Schuit D, McPoil TG, Mulesa P. Incidence of sacroiliac joint malalignment in leg length discrepancies. J Am Podiatr Med Assoc. 1989;79(8):380–383. doi: 10.7547/87507315-79-8-380. [DOI] [PubMed] [Google Scholar]
- 59.Winter RB, Pinto WC. Pelvic obliquity. Its causes and its treatment. Spine (Phila Pa 1976) 1986;11(3):225–234. [PubMed] [Google Scholar]
- 60.Kiapour A, Abdelgawad AA, Goel VK, Souccar A, Terai T, Ebraheim NA. Relationship between limb length discrepancy and load distribution across the sacroiliac joint—a finite element study. J Orthop Res. 2012;30(10):1577–1580. doi: 10.1002/jor.22119. [DOI] [PubMed] [Google Scholar]
- 61.Herzog W, Conway PJ. Gait analysis of sacroiliac joint patients. J Manipulative Physiol Ther. 1994;17(2):124–127. [PubMed] [Google Scholar]
- 62.Schoenberger M, Hellmich K. Sacroiliac dislocation and scoliosis. Hippokrates. 1964;35:476–479. [PubMed] [Google Scholar]
- 63.Marymont JV, Lynch MA, Henning CE. Exercise-related stress reaction of the sacroiliac joint. An unusual cause of low back pain in athletes. Am J Sports Med. 1986;14(4):320–323. doi: 10.1177/036354658601400414. [DOI] [PubMed] [Google Scholar]
- 64.Fitzgerald CM, Segal N. Musculoskeletal health in pregnancy and postpartum. Cham, Switzerland: Springer International Publishing; 2015. [Google Scholar]
- 65.Holmes SL, Cohen SP, Cullen MFL, Kenny CD, Wain HJ, Davis SA. Pain Medicine: An Interdisciplinary Case-Based Approach. Oxford, Englad: Oxford University Press; 2015. Sacroiliac joint pain; pp. 160–182. [Google Scholar]