Abstract
Objective
Evaluate the effect of a policy to deliver at 39 weeks for class III obesity.
Methods
Retrospective cohort study of women with class III obesity delivering ≥37 weeks pre- (May 2012-April 2014) and post-policy (September 2014-August 2016). Primary outcome was cesarean rate. Secondary outcomes included maternal morbidities and a neonatal morbidity composite. Modified Poisson regression was utilized to adjust for demographic differences between groups.
Results
1210 patients, 580 pre- and 630 post-policy. Pre- and post-policy, cesarean rate was similar (41.6% vs. 47.1%, risk ratio [RR] 1.13 [95% confidence interval {CI} 1.00–1.29], adjusted RR [aRR] 1.03 [95% CI 0.92–1.14). In adjusted comparisons of women undergoing labor induction, parous women had lower (aRR 0.62; 95% CI 0.41–0.94) but nulliparous women had higher (aRR 1.32; 95% CI 1.04–1.68) cesarean rates post-policy (p for interaction = 0.01). Rates of chorioamnionitis, endometritis, and cesarean wound infection were not different between groups. Composite neonatal morbidity was not different between pre- and post-policy groups.
Conclusion
A policy of delivery at 39 weeks for class III obesity did not affect overall cesarean rate or rates of maternal or neonatal morbidity. Further investigation should evaluate subsets of women who may have a higher cesarean rate with this policy.
Keywords: Class III obesity, pregnancy, labor induction, delivery timing, pregnancy outcomes
Introduction
The incidence of obesity in the United States has continued to rise in recent years, now comprising 36.5% of American adults1. Obesity, defined as a body mass index (BMI) ≥30 kg/m2, is an established risk factor for a variety of pregnancy complications including hypertensive disorders, gestational diabetes, fetal macrosomia, postpartum endometritis, and stillbirth.2–6 Furthermore, the risk of stillbirth (and other complications) rises with increasing BMI in a dose-dependent manner.7 A large 2014 study by Yao et al found that throughout gestation, the risk of stillbirth increased in a linear fashion for women with overweight, class I, and class II obesity. However, women with class III obesity (BMI ≥40) had a risk of stillbirth that increased more sharply with advancing gestational age, suggesting that class III obesity affects stillbirth differently compared to lesser obesity.8
Though induction of labor previously was thought to increase the risk of cesarean delivery (likely due to being compared to spontaneous labor in past analyses),9,10 recent cohort studies have suggested a decreased rate of cesarean delivery when comparing elective induction of labor with expectant management in the general population.11,12 Importantly, the recently published ARRIVE trial found that, compared with expectant management, induction of labor at 39 weeks in nulliparous low-risk women was associated with a lower rate of cesarean delivery13. However, data are limited regarding otherwise elective term delivery of patients with obesity and, specifically, regarding term delivery for the indication of class III obesity.
Based on the previously described study from Yao and colleagues,8 and well before the results of the ARRIVE trial were available, in an effort to minimize the risk of stillbirth in this high-risk population, the Section of Maternal-Fetal Medicine at the University of Oklahoma Health Sciences Center implemented a practice change in June 2014 to deliver women with class III obesity at 39 weeks gestation, even if there was no other indication. We sought to compare maternal and neonatal outcomes in all term deliveries before and after implementation of this change in practice, particularly with regard to cesarean delivery rate. Since we suspected that early term birth rates might be affected by the policy, we included all term births in the analyses. We hypothesized that the cesarean delivery rate would not differ between the two time periods. Our maternal and neonatal outcomes were formulated to match those used in the ARRIVE trial in order to facilitate comparison.
Methods
We performed a retrospective cohort study comparing all women with class III obesity who delivered at ≥37 weeks gestation at our institution during the pre-policy (May 2012-April 2014) and post-policy (September 2014-August 2016) periods. If a single patient had multiple deliveries within the study period, only the first delivery was included. We excluded subsequent pregnancies from the same subject because including them would violate the assumption for statistical tests that each pregnancy is independent. We also excluded women delivering during the month before and the three months after the policy change, so as to allow for some variability in the timing of uptake of the new policy by providers. Clinical exclusion criteria were multifetal gestation, known fetal anomalies, and fetal demise prior to 37 weeks.
We examined baseline maternal demographic characteristics in each group. The primary outcome was rate of cesarean delivery, evaluated overall and among the subset of women who attempted vaginal delivery. Secondary outcomes included several measures of maternal morbidity (chorioamnionitis, endometritis, wound infection, third/fourth degree perineal laceration, postpartum hemorrhage, ICU admission, venous thromboembolism, and blood transfusion) as well as a composite measure of neonatal morbidity and mortality (consisting of fetal or neonatal death; intubation, continuous positive airway pressure or high-flow nasal cannula for ventilation or cardiorespiratory support within the first 72 hours of life; Apgar score at five minutes of less than four; neonatal encephalopathy; seizures; sepsis; meconium aspiration syndrome; birth trauma [bone fractures, brachial plexus palsy, other neurologic injury, retinal hemorrhage, facial nerve injury]; intracranial or subgaleal hemorrhage; or hypotension requiring pressor support). All baseline maternal medical and obstetrical comorbidities and maternal and neonatal outcomes were obtained by individual chart review and defined as diagnosed clinically and documented in the medical record. Fetal growth restriction was defined as estimated fetal weight by ultrasound of less than the tenth percentile for gestational age. Nulliparous women were those without a prior delivery at or beyond 20 weeks gestation. At our institution, method of labor induction is at the discretion of the attending physician. This is most often accomplished using a Foley bulb or misoprostol for cervical ripening, followed by oxytocin. The dinoprostone insert and dinoprostone gel were also used for cervical ripening during the study period, but less commonly. Maternal charts were reviewed and outcomes obtained by four Maternal-Fetal Medicine or OB/GYN physicians (SLP, MEM, JSL, and MFL-D), and neonatal charts were reviewed and outcomes obtained by two Neonatalogy physicians (FV and CBA).
Continuous variables were compared using Student’s t test or Wilcoxon rank sum test for those with and without normal distributions, respectively. Categorical variables were compared using chi square or Fisher’s exact tests. Modified Poisson regression was used to calculate risk ratios and 95% confidence intervals adjusted for maternal age, race/ethnicity, parity, body mass index, prior cesarean delivery, cervical ripening (yes/no), induction of labor, and payor. Interactions between the policy period (post- vs pre-policy) and parity (parous vs nulliparous) were examined by adding an interaction term to the regression model. A p-value less than 0.05 was considered significant. Sensitivity analyses were conducted by replicating all analyses after excluding patients who delivered in the early term period (37–38 weeks), and by excluding patients with prior cesarean deliveries from analyses examining cesarean delivery outcomes.
Assuming a baseline rate of cesarean delivery of 40% in the study group, detection of a 25% reduction (to 30%) would require a sample size in each cohort of 356. Using conservative estimates of about 4000 deliveries per year, a rate of class III obesity of 8%, and 60% of such patients meeting enrollment criteria, we calculated that we would have data available for review for at least 384 mother-infant pairs in each two-year cohort. The study protocol was approved by the Institutional Review Board at the University of Oklahoma Health Sciences Center.
Results
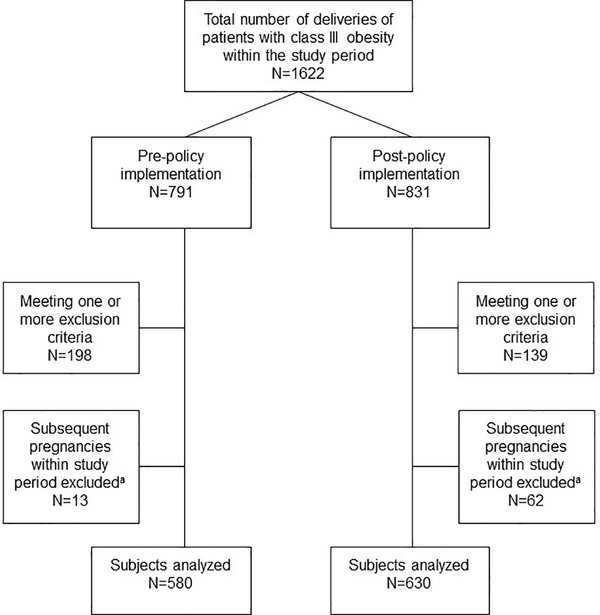
A total of 1210 mother-infant pairs met enrollment criteria and were included in our analysis, 580 in the pre-policy cohort and 630 in the post-policy cohort. See Figure 1 for a flow diagram showing details of patients excluded to reach the final analyzed sample size. Though most baseline maternal demographic characteristics were no different between cohorts, rates of prior cesarean, gestational hypertension, and fetal growth restriction were significantly higher in the post-policy group while spontaneous labor occurred less frequently (Table 1). As would be expected, the mean gestational age at delivery was significantly different between groups (p=0.003). These mean values were less than two days different, but the policy change did shift the time period in which patients delivered—the numbers of early term deliveries (37w0d-38w6d) were similar between groups (29.8% pre-policy compared to 31.0% post-policy, p=0.25), but after policy implementation, more patients delivered at 39 weeks (39w0d-39w6d; 38.6% pre-policy compared to 50.0% post-policy, p<0.001) and fewer patients delivered at 40w0d or more (31.6% pre-policy compared to 19.1% post-policy, p<0.001).
Figure 1.
Flow diagram showing details of patients excluded to arrive at analyzed sample size.
aWe excluded subsequent pregnancies from the same subject, since including them would violate the assumption for statistical tests that each pregnancy is independent.
Table 1.
Characteristics of patients with Class III obesity who delivered at term before or after implementation of a policy of delivery at 39 weeks gestation.
| Pre-Policy Change (n=580) | Post-Policy Change (n=630) | p | |
|---|---|---|---|
| Maternal Age (years) | 27.5 ± 5.8 | 28.2 ± 5.5 | 0.05 |
| Gestational Age (days) | 275.4 ± 8.2 | 273.8 ± 7.3 | 0.0003 |
| Body Mass Index (kg/m2) | 46.1 ± 5.7 | 45.6 ± 5.3 | 0.06 |
| Race/Ethnicity | 0.14 | ||
| White | 290 (50.0) | 334 (53.0) | |
| African American | 116 (20.0) | 118 (18.7) | |
| Hispanic | 142 (24.5) | 129 (20.5) | |
| American Indian | 23 (4.0) | 28 (4.4) | |
| Other | 9 (1.6) | 21 (3.3) | |
| Payor Status | 0.10 | ||
| Commercial | 161 (27.8) | 202 (32.1) | |
| Government/Self | 419 (72.2) | 428 (67.9) | |
| Nulliparousa | 180 (31.0) | 176 (27.9) | 0.24 |
| Prior Cesarean | 132 (22.8) | 201 (31.9) | 0.0004 |
| Chronic Hypertensionb | 122 (21.0) | 131 (20.8) | 0.92 |
| Gestational Hypertension | 71 (12.2) | 117 (18.6) | 0.002 |
| Preeclampsia | 0.06 | ||
| Severe | 33 (5.7) | 38 (6.0) | |
| Not Severe | 35 (6.0) | 20 (3.2) | |
| Diabetes | 0.10 | ||
| Pregestational | 28 (4.8) | 46 (7.3) | |
| Gestational | 73 (12.6) | 64 (10.2) | |
| Fetal Growth Restrictionc | 0 (0.0) | 8 (1.3) | 0.008 |
| Labor Type | <0.0001 | ||
| Spontaneous | 203 (35.0) | 148 (23.5) | |
| Induction with cervical ripening | 159 (27.4) | 183 (29.0) | |
| Induction with oxytocin alone | 94 (16.2) | 127 (20.2) | |
| Pre-labor cesarean delivery | 124 (21.4) | 172 (27.3) | |
Abbreviations used: kg=kilogram, m=meter.
Body mass index at the time of delivery is reported.
Data are reported as mean ± standard deviation or n (%) and analyzed using Student’s t test, Fisher’s exact test, Wilcoxon rank sum test, or chi-square test, as appropriate.
Defined as women without a prior delivery at or beyond 20 weeks gestation
All maternal medical and obstetrical comorbidities defined as diagnosed clinically and documented in the medical record
Defined as estimated fetal weight by ultrasound of less than the tenth percentile for gestational age
Though the proportion of patients undergoing labor induction was numerically higher post-policy (43.6% vs 49.2%; p=0.05), risk of cesarean delivery was similar in both unadjusted and adjusted comparisons (Table 2). This was true both for the overall comparison and among only those women who attempted vaginal delivery. However, when vaginal delivery attempts were stratified by parity, risk of cesarean delivery was lower during the post-policy period for parous women (adjusted risk ratio [aRR] 0.64, 95% confidence interval 0.45–0.92) but not for nulliparous women (aRR 1.18, 95% confidence interval 0.94–1.48, p for interaction = 0.01).
Table 2.
Cesarean delivery rates and risk ratios for associations between policy implementation and cesarean delivery in all term births before or after policy implementation.
| Pre-policy (n=580) | Post-policy (n=630) | Unadjusted RR (95% CI) | Adjusted RR (95% CI) | |
| All deliveries | 241 (41.6) | 297 (47.1) | 1.13 (1.00–1.29) | 1.03a (0.92–1.14) |
| Parousb | 163 (40.8) | 203 (44.7) | 1.10 (0.94–1.28) | 0.96c (0.85–1.08) |
| Nulliparous | 78 (43.3) | 94 (53.4) | 1.23 (0.99–1.53) | 1.15d (0.93–1.42) |
| Patients attempting vaginal delivery | Pre-policy (n=456) | Post-policy (n=458) | Unadjusted RR (95% CI) | Adjusted RR (95% CI) |
| All vaginal delivery attempts | 117 (25.7) | 125 (27.3) | 1.06 (0.86–1.32) | 0.94a (0.77–1.14) |
| Parous | 52 (18.0) | 41 (14.0) | 0.78 (0.54–1.14) | 0.64c (0.45–0.92) |
| Nulliparous | 65 (38.9) | 84 (50.6) | 1.30 (1.02–1.66) | 1.18d (0.94–1.48) |
| With Induction of Labor | ||||
| Parous | 34 (24.3) | 31 (16.9) | 0.69 (0.45–1.07) | 0.62c (0.41–0.94) |
| Nulliparous | 50 (44.3) | 75 (59.5) | 1.35 (1.05–1.73) | 1.32d (1.04–1.68) |
| With Spontaneous Labor | ||||
| Parous | 18 (12.1) | 10 (9.3) | 0.77 (0.37–1.59) | 0.60e (0.29–1.27) |
| Nulliparous | 15 (27.8) | 9 (22.5) | 0.81 (0.40–1.66) | 0.90f (0.45–1.81) |
Abbreviations used: RR = risk ratio.
Data are presented as n (%) and risk ratio (95% confidence interval).
Adjusted model controlled for maternal age, race, parity, body mass index, prior cesarean, cervical ripening (yes/no), labor induction, and payor
Defined as having one or more prior deliveries at or beyond 20 weeks gestation
Adjusted model controlled for maternal age, race, body mass index, prior cesarean, cervical ripening, labor induction, and payor
Adjusted model controlled for maternal age, race, body mass index, cervical ripening, labor induction, and payor
Adjusted model controlled for maternal age, race, body mass index, prior cesarean, and payor
Adjusted model controlled for maternal age, race, body mass index, and payor
When the interactions with parity were examined separately among women with labor induction and those with spontaneous labor, parous women who underwent induction of labor had a significantly lower risk of cesarean delivery during the post-policy period compared with the pre-policy period (aRR 0.62, 95% confidence interval 0.41–0.94; Table 2). In contrast, nulliparous patients who underwent induction of labor had a significantly higher risk of cesarean delivery during the post-policy period compared with the pre-policy period (aRR 1.32, 95% confidence interval 1.04–1.68; Table 2; p for interaction = 0.01). Among women with spontaneous labor, the association between policy period and cesarean delivery did not differ significantly by parity (Table 2, p for interaction=0.69).
Regarding maternal morbidities, the unadjusted and adjusted risk ratios for blood transfusion were significantly higher in the post-policy group than the pre-policy group (Table 3). However, both the unadjusted and adjusted risk ratios for blood transfusion were non-significant and accompanied by wide confidence intervals when examining only patients who attempted vaginal delivery (Table 4). There were no other significant differences in maternal morbidities between the two groups, whether considering all patients (Table 3) or only those attempting vaginal delivery (Table 4). Likewise, the risk of composite neonatal morbidity and mortality was not statistically significantly different between groups in both unadjusted and adjusted comparisons (Tables 3 and 4). Statistically significant differences by parity were not observed for associations between the policy period and maternal and neonatal outcomes (p for interaction > 0.05).
Table 3.
Maternal and neonatal outcomes of patients with class III obesity who delivered at term before or after implementation of a policy for delivery at 39 weeks.
| Pre-Policy (n=580) | Post-Policy (n=630) | Unadjusted RR (95% CI) | Adjusted RR (95% CI)a | |
|---|---|---|---|---|
| Chorioamnionitisb | 3.8 | 3.2 | 0.84 (0.46–1.52) | 0.92 (0.51–1.65) |
| Endometritis | 1.7 | 1.6 | 0.92 (0.39–2.20) | 0.90 (0.37–2.17) |
| Wound Infection | 5.9 | 5.9 | 1.00 (0.64–1.57) | 0.96 (0.61–1.52) |
| ICU Admission | 0.9 | 0.5 | 0.55 (0.13–2.30) | 0.62 (0.15–2.59) |
| 3rd or 4th Degree Perineal Laceration | 0.7 | 0.3 | 0.46 (0.08–2.50) | - |
| Venous Thromboembolism | 0.0 | 0.0 | - | - |
| Postpartum Hemorrhage | 4.1 | 5.2 | 1.27 (0.76–2.12) | 1.19 (0.71–2.01) |
| Blood Transfusion | 1.0 | 3.7 | 3.53 (1.45–8.61) | 3.52 (1.38–8.97) |
| Stillbirth | 0.2 | 0 | - | - |
| Composite Neonatal Morbidity and Mortalityc | 7.8 | 9.2 | 1.19 (0.82–1.72) | 1.11 (0.76–1.63) |
Abbreviations used: RR = risk ratio.
Data are presented as proportion of n and risk ratio (95% confidence interval).
Some risk ratios are not calculable due to sparse data.
Adjusted model controlled for maternal age, race, parity, body mass index, prior cesarean, cervical ripening (yes/no), labor induction, and payor
All maternal outcomes defined as diagnosed clinically and documented in the medical record
Composite measure consisting of fetal or neonatal death; intubation, continuous positive airway pressure or high-flow nasal cannula for ventilation or cardiorespiratory support within the first 72 hours of life; Apgar score at five minutes of less than four; neonatal encephalopathy; seizures; sepsis; meconium aspiration syndrome; birth trauma [bone fractures, brachial plexus palsy, other neurologic injury, retinal hemorrhage, facial nerve injury]; intracranial or subgaleal hemorrhage; or hypotension requiring pressor support
Table 4.
Maternal and neonatal outcomes of patients with class III obesity attempting vaginal delivery who delivered at term before or after implementation of a policy for delivery at 39 weeks.
| Pre-Policy (n=456) | Post-Policy (n=458) | Unadjusted RR (95% CI) | Adjusted RR (95% CI)a | |
|---|---|---|---|---|
| Chorioamnionitisb | 4.9 | 4.2 | 0.86 (0.47–1.57) | 0.87 (0.48–1.58) |
| Endometritis | 1.8 | 1.6 | 0.87 (0.32–2.38) | 0.95 (0.35–2.59) |
| Wound Infection | 3.6 | 5.3 | 1.49 (0.80–2.77) | 1.36 (0.74–2.52) |
| ICU Admission | 0.7 | 0.4 | 0.66 (0.11–3.95) | - |
| 3rd or 4th Degree Perineal Laceration | 0.9 | 0.4 | 0.50 (0.09–2.70) | - |
| Venous Thromboembolism | 0.0 | 0.0 | - | - |
| Postpartum Hemorrhage | 4.4 | 6.2 | 1.39 (0.80–2.44) | 1.28 (0.73–2.26) |
| Blood Transfusion | 1.3 | 3.1 | 2.32 (0.90–5.99) | 2.24 (0.80–6.28) |
| Stillbirth | 0.22 | 0 | - | - |
| Composite Neonatal Morbidity and Mortalityc | 7.1 | 8.8 | 1.24 (0.80–1.94) | 1.15 (0.73–1.79) |
Data are presented as proportion of n and risk ratio (95% confidence interval).
Some risk ratios are not calculable due to sparse data.
Adjusted model controlled for maternal age, race, parity, body mass index, prior cesarean, cervical ripening (yes/no), labor induction, and payor
All maternal outcomes defined as diagnosed clinically and documented in the medical record
Composite measure consisting of fetal or neonatal death; intubation, continuous positive airway pressure or high-flow nasal cannula for ventilation or cardiorespiratory support within the first 72 hours of life; Apgar score at five minutes of less than four; neonatal encephalopathy; seizures; sepsis; meconium aspiration syndrome; birth trauma [bone fractures, brachial plexus palsy, other neurologic injury, retinal hemorrhage, facial nerve injury]; intracranial or subgaleal hemorrhage; or hypotension requiring pressor support
We also ascertained the number of patients in each group who had “isolated obesity”, meaning the absence of any other comorbidities that would affect timing of delivery (including diabetes, preeclampsia, gestational hypertension, chronic hypertension, and fetal growth restriction). There were 307 (52.9%) women with isolated obesity in the pre-policy group and 312 (49.5%) women with isolated obesity in the post-policy group. Results in this subset of patients were similar to those in the overall groups (Supplemental Tables S1–S4).
In addition, we performed a sensitivity analysis excluding patients who had a prior cesarean delivery. Results for cesarean rates were similar to those in the overall group. We also performed an analysis excluding patients who delivered in the early term period (37–38 weeks). We found that results restricted to deliveries at 39 weeks or later were similar to those in the overall analyses which included all term births (data not shown).
Discussion
In women delivering at 37 weeks or greater at our institution, a policy considering class III obesity an indication for delivery at 39 weeks did not affect either the overall cesarean rate or the rate among the subset of women attempting vaginal delivery. Furthermore, there were no significant differences in overall maternal or neonatal morbidity when comparing outcomes during the pre-policy and post-policy periods. However, in pre-specified secondary analyses stratified by parity, we found a decreased risk for cesarean delivery in parous women who underwent induction of labor in the post-policy period but an increased risk for cesarean delivery in nulliparous women who underwent induction of labor in the post-policy period.
Recognizing that women with class III obesity have a higher rate of conditions that may necessitate delivery before 40 weeks, we also examined outcomes in the subset of women with isolated obesity (i.e. those with no other comorbidities that would affect timing of delivery). We found that the outcomes in women with isolated obesity were similar to those in the overall groups, although these results should be interpreted with caution given the relatively small number of cases and outcomes in the group with isolated obesity.
Our data differ somewhat from that of Schuster et al,14 who examined 5000 randomly selected women and showed a decrease in cesarean rate after implementation of a policy that included delivery of patients with class III obesity by their estimated due date. That analysis did not stratify results by parity. Similarly, a retrospective study by Gibbs Pickens et al of over 160,000 women from a California birth database found that in both nulliparous and parous women with obesity, elective induction at 39 weeks was associated with fewer cesarean deliveries compared with women who were expectantly managed.15 A potentially important difference between our study and these two analyses is that our study included only women with class III obesity, while both the Schuster and Gibbs Pickens analyses also included women with class I and II obesity.
Our data are particularly relevant when viewed in light of the recently finished ARRIVE trial, which found that, compared with expectant management, induction of labor at 39 weeks in nulliparous low-risk women in the general population (not specifically obese) was associated with a lower rate of cesarean delivery and no adverse effects on maternal or neonatal morbidity.13 Given our finding that nulliparous women with class III obesity undergoing labor induction had a higher rate of cesarean delivery after institution of a policy to deliver at 39 weeks, we eagerly await further subgroup analyses from the ARRIVE trial regarding women with class III obesity. In fact, the secondary outcomes in our study were formulated to match those specified in the ARRIVE study (https://clinicaltrials.gov/ct2/show/NCT01990612) in order to facilitate comparison of our results with that anticipated secondary analysis of their data regarding class III obese gravidas.
We did find an increased proportion of patients with gestational hypertension in the post-policy group. This was unexpected, given that the two groups were similar in terms of other medical comorbidities. In addition, since the median gestational age at delivery was lower in the post-policy group, if anything we would have anticipated a lower rate of gestational hypertension in this group. One potential reason for this finding could be subtle practice changes in diagnosis of gestational hypertension related to publication of the Hypertension in Pregnancy document by the American College of Obstetricians and Gynecologists (ACOG) toward the end of our pre-policy period in 2013.16
The increased risk of blood transfusion post-policy initially might seem concerning. However, when considering the incorporation during the study period (beginning of 2015) of a new practice bundle regarding postpartum hemorrhage that has led to more diagnoses and more transfusions but fewer transfusions of more than four units of blood in our general obstetric population (institutional tracked data), we think that this finding could have been anticipated.
The rate of prior cesarean was higher in our post-policy group. The reason for this is unclear, however as a tertiary care referral center in a geographical area where few other centers offer trial of labor after cesarean, it is possible that changes in referral patterns may have contributed to this difference. Regardless of the reason, a higher rate of prior cesarean in the post-policy group should, if anything, bias our results toward a higher overall rate of cesarean delivery in the post-policy group, which we did not find.
The outcome of fetal growth restriction was less frequent than expected in our cohort, and in fact the pre-policy group had no cases of fetal growth restriction identified. This is a limitation of the study and likely reflects lack of documentation in the electronic medical record rather than true prevalence in our population. However, we think that it is unlikely that the cohorts would be differentially affected by this issue.
Although there was less than a two day difference in mean gestational age between the pre- and post-policy groups, the proportion of 39 week deliveries increased and the proportion of deliveries at 40 or more weeks decreased after policy implementation, demonstrating some compliance with this new policy. Clearly, there was some noncompliance with the policy since almost one-fifth of patients with class III obesity still reached a gestational age of at least 40 weeks after implementation. Due to the retrospective nature of the study, we could not ascertain whether this noncompliance was provider- or patient-related.
Our primary question addresses the impact of a policy shift to deliver at 39 weeks for the indication of class III obesity alone, however we included women who delivered in the early term period in our analyses since this change in management might also affect early term deliveries. When we performed a subgroup analysis of only women who delivered at 39 weeks and beyond, outcomes were similar to those in the overall group.
Although our policy change was aimed at reducing rates of stillbirth in women with class III obesity, our study was not powered to detect a difference in rates of stillbirth. With the thankfully low rate of that outcome, such a study would require an exceptionally large sample size. Given this, we chose cesarean delivery as our primary outcome since we reasoned that if detected, a difference in cesarean rate after policy implementation would have important implications for this population.
Though retrospective and at risk of potential biases inherent in such analyses, we think that our study has several strengths. One important strength of our study is that patients with medical comorbidities were included in our analysis, providing a more complete picture of outcomes in the overall obese obstetric population. In addition, we conducted individual patient medical chart review to obtain all of the data used in this analysis. We also adjusted for demographic differences between cohorts.
Because of the finding that a policy of delivery at 39 weeks in women with class III obesity may differentially affect the risk of cesarean in various subsets of patients and given the increased risk for complications in women who undergo cesarean delivery after a failed labor induction,17 a tool to calculate risk of cesarean in women with class III obesity is needed and could allow informed decisions about planned pre-labor cesarean versus labor induction, potentially decreasing morbidity.
Conclusion
The goal of our policy change was reduction in stillbirth, and our results suggest that any reduction in stillbirth rates attained by a policy of delivery at 39 weeks gestation for the indication of class III obesity may be achieved without a concomitant increase in overall cesarean delivery rate or maternal or neonatal morbidity. However, further investigation is warranted to determine whether there is a subset of patients who may have a higher risk for cesarean delivery with this type of policy.
Supplementary Material
Study Importance Questions.
It is well established that women with class III obesity have a higher risk for adverse pregnancy outcomes compared to women with normal weight, overweight, or lesser degrees of obesity; however, data are limited regarding the optimal timing of delivery for women with class III obesity
Our study demonstrates that a policy to deliver women with class III obesity at 39 weeks did not affect the overall rates of cesarean delivery or maternal or neonatal morbidity
However, we also found that nulliparous women had a higher rate of cesarean delivery after implementation of the policy
Additional research should focus on whether there is a subset of women who may be at higher risk for cesarean with a policy to deliver at 39 weeks for the indication of class III obesity
Acknowledgements
This work was presented in part at the Society for Maternal-Fetal Medicine’s 38th Annual Pregnancy Meeting in Dallas, TX, January 29-February 3, 2018.
Sources of Funding: Partial funding provided by National Institutes of Health, National Institute of General Medical Sciences [Grant 1 U54GM104938].
Footnotes
Conflicts of Interest: The authors declared no conflicts of interest.
References
- 1.Ogden CL, Carroll MD, Fryar CD, Flegal KM. Prevalence of Obesity Among Adults and Youth: United States, 2011–2014. NCHS Data Brief 2015;219:1–8 [PubMed] [Google Scholar]
- 2.Sibai BM, Ewell M, Levine RJ, Klebanoff MA, Esterlitz J, Catalano PM, et al. Risk factors associated with preeclampsia in healthy nulliparous women. The Calcium for Preeclampsia Prevention (CPEP) Study Group. Am J Obstet Gynecol 1997;177(5):1003–10 [DOI] [PubMed] [Google Scholar]
- 3.Weiss JL, Malone FD, Emig D, Ball RH, Nyberg DA, Comstock CH, et al. Obesity, obstetric complications and cesarean delivery rate--a population-based screening study. Am J Obstet Gynecol 2004;190(4):1091–7 [DOI] [PubMed] [Google Scholar]
- 4.Nohr EA, Bech BH, Davies MJ, Frydenberg M, Henrikson TB, Olsen J. Prepregnancy obesity and fetal death: a study within the Danish National Birth Cohort. Obstet Gynecol 2005;106(2):250–9 [DOI] [PubMed] [Google Scholar]
- 5.Huang DY, Usher RH, Kramer MS, Yang H, Morin L, Fretts RC. Determinants of unexplained antepartum fetal deaths. Obstet Gynecol 2000;95(2):215–21 [DOI] [PubMed] [Google Scholar]
- 6.Magann EF, Doherty DA, Chauhan SP, Klimpel JM, Huff SD, Morrison JC. Pregnancy, obesity, gestational weight gain, and parity as predictors of peripartum complications. Arch Gynecol Obstet, 2011;284(4):827–36 [DOI] [PubMed] [Google Scholar]
- 7.Salihu HM, Dunlop AL, Headayatzadeh M, Alio AP, Kirby RS, Alexander GR. Extreme obesity and risk of stillbirth among black and white gravidas. Obstet Gynecol 2007;110(3):552–7 [DOI] [PubMed] [Google Scholar]
- 8.Yao R, Ananth CV, Park BY, Pereira L, Plante LA; Perinatal Research Consortium. Obesity and the risk of stillbirth: a population-based cohort study. Am J Obstet Gynecol 2014;210(5):457 e1–9 [DOI] [PubMed] [Google Scholar]
- 9.Heffner LJ, Elkin E, Fretts RC. Impact of labor induction, gestational age, and maternal age on cesarean delivery rates. Obstet Gynecol 2003;102(2):287–93 [DOI] [PubMed] [Google Scholar]
- 10.Maslow AS, Sweeny AL. Elective induction of labor as a risk factor for cesarean delivery among low-risk women at term. Obstet Gynecol 2000;95(6 Pt 1):917–22 [DOI] [PubMed] [Google Scholar]
- 11.Stock SJ, Ferguson E, Duffy A, Ford I, Chalmers J, Norman JE. Outcomes of elective induction of labour compared with expectant management: population based study. BMJ 2012;344:e2838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Darney BG, Snowden JM, Cheng YW, Jacob L, Nicholson JM, Kaimal A, et al. Elective induction of labor at term compared with expectant management: maternal and neonatal outcomes. Obstet Gynecol 2013;122(4):761–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Grobman WA, Rice MM, Reddy UM, et al. Labor induction versus expectant management in low-risk nulliparous women. N Engl J Med 2018;379(6):513–523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schuster M, Madeueke-Laveaux OS, Mackeen AD, Feng W, Paglia MJ. The effect of the MFM obesity protocol on cesarean delivery rates. Am J bstet Gynecol 2016;215(4):492.e1–6 [DOI] [PubMed] [Google Scholar]
- 15.Gibbs Pickens CM, Kramer MR, Howards PP, Badell ML, Caughey AB, Hogue CJ. Term Elective Induction of Labor and Pregnancy Outcomes Among Obese Women and Their Offspring. Obstet Gynecol 2018;131(1):12–22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.American College of Obstetricians and Gynecologists; Task Force on Hypertension in Pregnancy. Hypertension in pregnancy. Report of the American College of Obstetricians and Gynecologists’ Task Force on Hypertension in Pregnancy. Obstet Gynecol 2013;122(5):1122–31 [DOI] [PubMed] [Google Scholar]
- 17.Subramaniam A, Jauk VC, Goss AR, Alvarez MD, Reese C, Edwards RK. Mode of delivery in women with class III obesity: planned cesarean compared with induction of labor. Am J Obstet Gynecol 2014;211(6):700.e1–9 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.