Abstract
Objective:
Sleep wake disturbances (SWD) are under-evaluated among children with acquired brain injury surviving critical care. We aimed to quantify severity, phenotypes, and risk factors for SWD.
Methods:
We performed a prospective cohort study of 78 children ≥3 years with acquired brain injury within 3 months of critical care hospitalization. Diagnoses included: traumatic brain injury (TBI, n=40); stroke (n=11); infectious or inflammatory (n=10); hypoxic ischemic (n=9); and other (n=8). Sleep Disturbances Scale for Children standardized T-scores measured SWD. Overall SWD were dichotomized as any total or subscale T-score ≥60. Any T-score ≥70 defined severe SWD. Subscale T-scores ≥60 identified SWD phenotypes.
Results:
SWD were identified in 44 (56%) children and were classified as severe in 36 (46%). SWD affected ≥33% of patients within each diagnosis and were not associated with severity of illness measures. The most common phenotype was disturbance in initiation and maintenance of sleep (47%), though 68% had multiple concurrent SWD phenotypes. One third of all patients had pre-admission chronic conditions, and this increased risk for SWD overall (43% versus 21%, p=.04) and in the TBI subgroup (52% versus 5%, p=.001).
Conclusion:
Over half of children surviving critical care with acquired brain injury have SWD. Most of these children have severe SWD independent of severity of illness measures. Many SWD phenotypes were identified, but most children had disturbance in initiation and maintenance of sleep. Our study underscores the importance of evaluating SWD after acquired brain injury.
Keywords: Pediatric, sleep, sleep wake disorders, critical care outcomes, brain injury
Introduction
Acquired brain injury from a neurologic diagnosis accounts for more than 20% of admissions to pediatric intensive care units.1,2 Each year tens of thousands of children require specialized pediatric neurocritical care (PNCC) to treat the primary neurologic insult and minimize secondary brain injury in an effort to improve outcomes.3 Despite specialized care, acquired brain injury is the leading cause of death and long-term morbidity among children requiring critical care.1,4,5 Chronic morbidities include physical, cognitive, emotional, and psychosocial impairments termed post-intensive care syndrome (PICS).6,7
Healthy sleep is vital for brain maturation and normal development, and is likely even more important after neurologic injury or illness given that sleep facilitates neuronal healing and reduces inflammation.8–12 Sleep wake disturbances (SWD) in otherwise healthy children are known to impair quality of life, reduce participation in social activities, and impair cognitive function.13–15 Many of the impairments found in children with SWD overlap with those of children with PICS. SWD including insomnia, somnolence, and sleep-related breathing disorders are reported in survivors of brain injury, but to date have been poorly quantified in children after critical care hospitalization.8,16,17 Our prior work showed SWD were a common subjective complaint in children with various neurologic diagnoses treated in a critical care follow-up clinic.18 Most research has focused on traumatic brain injury (TBI), and very few studies have reported SWD outcomes in children with injuries more severe than concussion.17 Those that included children hospitalized with mild complicated, moderate, or severe TBI requiring PNCC rarely used a validated sleep questionnaire19–22 and most were not originally designed for the purpose of collecting sleep data.19,22 Therefore, the severity of SWD and phenotypes of the SWD are largely under-evaluated and under-reported in prior studies limiting the ability to adequately identify risk factors and design targeted intervention studies.
To address these important knowledge gaps surrounding SWD in survivors with acquired brain injury, we evaluated SWD at two institutions with longitudinal critical care programs treating children in specialized multidisciplinary clinics. Based on our clinical experience, we hypothesized SWD would be prevalent and severe after acquired brain injury. We aimed to quantify overall SWD, severity and phenotypes of SWD, and risk factors for SWD after PNCC hospital discharge using a multidimensional sleep questionnaire.
Materials and Methods
Study Design
We evaluated SWD 1–3 months after hospital discharge (December 2017-October 2018) in a prospective cohort study of children ages 3–18 years with acquired brain injury. Evaluations were performed as part of routine clinical care in each institution’s coordinated follow-up clinic. More than two-thirds of all PNCC survivors complete a clinic visit and referral patterns and follow-up rates at each program have been previously described.18,23 The Institutional Review Board at each institution approved the study under a waiver of informed consent.
Population Characteristics
Both institutions are tertiary children’s hospitals and accredited Level 1 pediatric trauma centers with multidisciplinary critical care follow-up programs that include pediatric critical care, pediatric neurology, and pediatric neuropsychology faculty. Consecutive children who completed a follow-up visit were included. For the analysis, diagnoses were grouped into 5 unique subgroups: TBI; stroke (hemorrhagic and ischemic); infectious or inflammatory (meningitis, encephalitis, demyelinating); hypoxic ischemic (cardiac arrest, extracorporeal life support); and other (carbon monoxide, hemolytic uremic syndrome, severe sepsis, hippocampal necrosis after polypharmacy ingestion, refractory status epilepticus). The primary diagnosis was used in patients with multiple diagnoses (e.g. patients with seizures due to meningitis were classified as infectious).
Demographic and clinical characteristics were collected from electronic medical records. Pre-admission chronic conditions were grouped into system categories given the large number of individual diagnoses (Supplemental Table 1). Presence of any chronic condition was dichotomized for analysis. Pediatric Index of Mortality-2 score and critical care interventions (intubation, non-invasive ventilation, central venous catheterization, arterial catheter placement, intracranial pressure monitoring, continuous antiepileptic infusion, neurosurgical intervention, hemodynamic resuscitation or vasopressor use, and in-hospital cardiopulmonary resuscitation) were evaluated as markers of illness severity. Interventions were not counted if only used during operative management and were discontinued prior to return or admission to the pediatric intensive care unit (e.g. intubation during operation only). Functional assessments were made by attending physicians using the Functional Status Scale (FSS).24 Glasgow Coma Scale measured TBI severity (mild complicated 13–15, moderate 9–12, severe 3–8). Location and type of TBI and concurrent non-brain traumatic injuries were identified from radiology reports.
Outcomes
Sleep outcomes were measured at follow-up visits using the Sleep Disturbances Scale for Children (SDSC), a parent-reported 26-item validated multidimensional questionnaire for use in children ages 3–18 years.25,26 Each question is scored 1 to 5 with higher scores reflecting more disturbance. The SDSC provides 6 subscale scores and a total composite score that can each be converted to T-scores to reflect risk of clinical sleep disorders.25 In our study, SWD were defined as a T-score ≥60 in any of the SDSC total or subscale scores, corresponding to moderate or greater risk of clinical sleep disorders and ≥1 standard deviation (SD) from healthy population means.25 SWD group was used to compare demographic and clinical characteristics. Severe SWD were defined as T-scores ≥70 (≥2 SD from normal). Phenotypes of SWD were identified by the 6 SDSC subscales: disorders of initiation and maintenance of sleep (e.g. insomnia); sleep breathing disorders (e.g. sleep apnea); disorders of arousal (e.g. nightmares); sleep-wake transition disorders (e.g. sleep talking, bruxism); disorders of excessive somnolence (e.g. daytime sleepiness); sleep hyperhidrosis (e.g. night sweats).
Statistical Analysis
Descriptive statistics were used to describe the population including percent for categorical variables and median with interquartile range (IQR) for continuous variables as data were not normally distributed in our sample. SDSC total and subscale score mean and standard deviation (SD) for our cohort were compared with unpaired t-tests to prior published data on SDSC total and subscale means among healthy children (historical controls).25
Demographic and clinical characteristics were compared between dichotomized SWD groups. We used chi-square tests for categorical variables and Mann-Whitney U tests to compare continuous variables. Multiple logistic regression was used to identify variables associated with SWD among the overall cohort and results reported as adjusted Odds Ratio (aOR) with 95% Confidence Interval (CI). We controlled for diagnosis subgroup (“other” as reference diagnosis category), gender, age, Medicaid, non-white race, Hispanic ethnicity, and presence of any pre-admission chronic condition based on significance in the bivariate analysis (p<.05) and prior reports of risk factors for SWD in children.17 The full model results are reported (Supplemental Table 2) as it showed good calibration (Hosmer-Lemeshow p=.9) and discrimination (area under curve= .80) and outperformed reduced models (using area under the curve) derived from stepwise regression.
A descriptive analysis evaluated SWD phenotypes using SDSC subscales and SWD by diagnosis subgroup. A secondary analysis was performed to explore demographic and clinical variables by SWD group with the same tests as above for the TBI subgroup. Analyses were conducted using SPSS (version 24.0, Armonk, New York: IBM Corporation). All tests were two-tailed and significance defined as p<0.05. When multiple pairwise comparisons were made within variable groups, a Bonferroni adjustment was used to define significance level.
Results
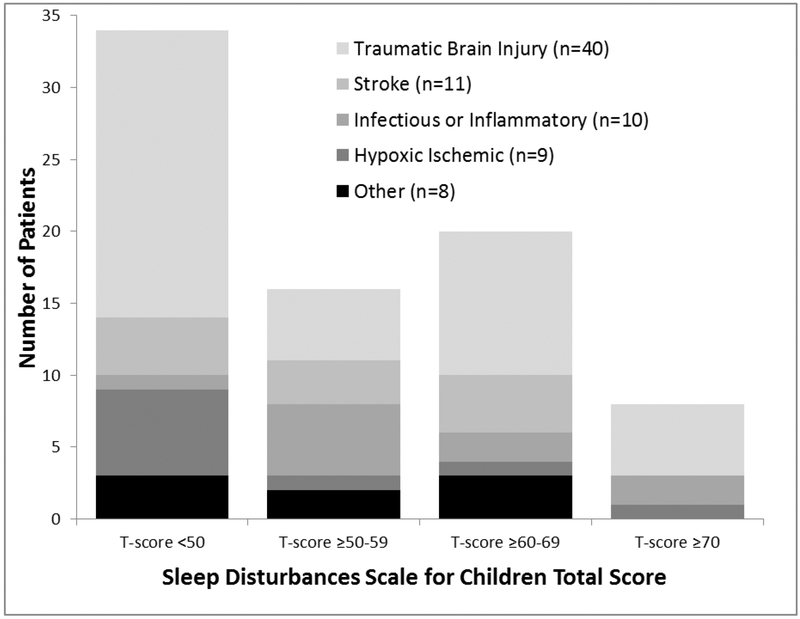
A total of 78 children were evaluated in clinic a median of 1.8 months (IQR 1.3, 2.8) post-injury. The majority of patients had TBI (n=40) followed by stroke (n=11), infectious or inflammatory disease (n=10), hypoxic ischemic injury (n=9), and other diagnoses (n=8). Table 1 shows demographic and clinical characteristics. Pre-admission chronic conditions were found in 26 (33%) patients and varied by diagnosis subgroup (Supplemental Table 1). Severity of illness and length of stay were variable, but two thirds required at least 1 critical care intervention and half were intubated (Table 1). No significant differences were found between institutions in diagnosis, severity, or any interventions. Average SDSC total score was 39.4 (SD 10.4) for the overall cohort and was significantly higher than the average for healthy children in published cohorts25 (35.1, SD 7.7; p<.001; Table 2). The distribution of standardized T-scores for the SDSC total score is shown in Figure 1.
Table 1.
Demographic and Clinical Characteristics by Sleep Wake Disturbance Group
| Characteristics | All N=78 (%) |
No SWD N=34 (%) |
SWD + N=44 (%) |
p-value |
|---|---|---|---|---|
| Age in years, Median (IQR) | 9.9 (6.8,14.1) | 8 (6,11) | 10.7 (7.6,15) | .03 |
| Male Gender | 47 (60%) | 18 (53%) | 29 (66%) | .35 |
| Pre-admission chronic condition | 26 (33%) | 7 (21%) | 19 (43%) | .04 |
| Race | .61 | |||
| White | 63 (81%) | 26 (77%) | 37 (84%) | |
| Black | 6 (8%) | 4 (12%) | 2 (5%) | |
| Other, multiple races, or unknown | 9 (12%) | 4 (12%) | 5 (11%) | |
| Hispanic Ethnicity | 13 (17%) | 4 (12%) | 9 (21%) | .38 |
| Medicaid Insurance | 35 (45%) | 17 (50%) | 18 (41%) | .42 |
| Diagnosis Category | .13 | |||
| Traumatic Brain Injury | 40 (51%) | 19 (56%) | 21 (48%) | |
| Stroke | 11 (14%) | 4 (12%) | 7 (16%) | |
| Infectious and Inflammatory | 10 (13%) | 1 (3%) | 9 (21%) | |
| Hypoxic Ischemic Injury | 9 (12%) | 6 (18%) | 3 (7%) | |
| Other | 8 (10%) | 4 (12%) | 4 (9%) | |
| Pediatric Index Mortality-2; Median (IQR) | −3.7(−4.1,−3) | −3.1(−4.1,−3) | −4 (−4,−3.1) | .49 |
| Intensive Care Interventions | ||||
| Monitoring only | 27 (35%) | 8 (24%) | 19 (43%) | .07 |
| Intubation | 39 (50%) | 19 (56%) | 20 (46%) | .36 |
| Non-invasive ventilation | 10 (13%) | 7 (21%) | 3 (7%) | .07 |
| Central venous line | 29 (37%) | 15 (44%) | 14 (32%) | .27 |
| Arterial line | 31 (40%) | 14 (41%) | 17 (39%) | .82 |
| Bolt | 5 (6%) | 1 (3%) | 4 (9%) | .27 |
| External Ventricular Drain | 6 (8%) | 2 (6%) | 4 (9%) | .60 |
| Infusion for seizure control | 12 (15%) | 4 (12%) | 8 (18%) | .44 |
| Neurosurgical intervention | 21 (27%) | 11 (32%) | 10 (23%) | .34 |
| Hemodynamic resuscitation or vasopressor | 25 (32%) | 12 (35%) | 13 (30%) | .59 |
| Cardiopulmonary resuscitation in-hospital | 8 (10%) | 5 (15%) | 3 (7%) | .26 |
| Inpatient Nutrition | .43 | |||
| Any Parenteral | 5 (6%) | 3 (9%) | 2 (5%) | |
| Any Nasogastric or Nasojejunal | 17 (22%) | 10 (29%) | 7 (15%) | |
| Oral only | 56 (72%) | 21 (62%) | 35 (80%) | |
| Inpatient consults | ||||
| Physical Therapy | 52 (67%) | 20 (59%) | 32 (73%) | .20 |
| Occupational Therapy | 47 (60%) | 19 (56%) | 28 (64%) | .49 |
| Speech Therapy | 20 (26%) | 9 (27%) | 11 (25%) | .88 |
| Psychology | 26 (33%) | 7 (21%) | 19 (43%) | .05 |
| Inpatient Rehabilitation Discharge | 11 (14%) | 7 (21%) | 4 (9%) | .15 |
| New Tracheostomy | 6 (8%) | 3 (9%) | 3 (7%) | >.99 |
| New Gastrostomy | 3 (4%) | 2 (6%) | 1 (2%) | .41 |
| Hours of Mechanical Ventilation, Median (IQR) n=39 | 16.7 (4, 37.2) | 17.4 (6.3,28) | 15.5 (3.1,35.8) | .68 |
| Hospital Length of Stay in Days Median (IQR) | 7.4 (2.1,20.8) | 6.8 (1.8,29.6) | 7.4 (2.8,16.7) | .61 |
| PICU Length of Stay in Days Median (IQR) | 2.8 (1.4,11.9) | 2.8 (1.0, 13.0) | 2.5 (1.5,7.9) | .78 |
| Clinic Functional Status Scale, Median (IQR) | 6 (6,7) | 6 (6,6) | 6 (6,7) | .30 |
IQR: Interquartile Range; PICU: Pediatric Intensive Care Unit
Values are prevalence or median when stated. Values in parentheses represent group percentage or IQR when stated. Mann Whitney U tests were used for continuous variables and chi-square tests for categorical variables.
Table 2.
Comparison of the Overall Acquired Brain Injury and Traumatic Brain Injury Cohorts to Healthy Controls Reported for the Sleep Disturbances Scale for Children
| SDSC scale | Healthy Control Sample25 N=1157 |
Overall cohort N=78 |
TBI subgroup N=40 |
|---|---|---|---|
| SDSC Total, Mean (SD) | 35.1 (7.7) | 39.4 (10.7)** | 38.6 (9.7)* |
| Disorders of Initiation and Maintenance of Sleep, Mean (SD) | 9.9 (3.1) | 13.2 (5.3)** | 12.7 (4.7)** |
| Sleep Breathing Disorder, Mean (SD) | 3.8 (1.5) | 3.9 (1.7) | 3.5 (1.0) |
| Disorders of Arousal, Mean (SD) | 3.3 (0.8) | 3.6 (1.7)* | 3.3 (1.0) |
| Sleep Wake Transition Disorders, Mean (SD) | 8.1 (2.4) | 8.7 (3.1)* | 8.8 (3.7) |
| Hypersomnolence, Mean (SD) | 7.1 (2.6) | 7.5 (2.5) | 7.6 (2.8) |
| Sleep Hyperhidrosis, Mean (SD) | 2.9 (1.7) | 2.5 (1.1) | 2.6 (1.0) |
TBI: Traumatic Brain Injury; SDSC: Sleep Disturbances Scale for Children; SD: Standard Deviation Healthy controls obtained from Bruni et al validation study25
p<0.001 when compared to healthy control populations in published literature;
p<0.05; comparisons with unpaired t-tests
Figure 1.
Distribution of standardized T-scores for the Sleep Disturbances Scale for Children total score is shown separated by primary diagnosis.
SWD were identified in 44 (56%) patients with acquired brain injury, and were severe in 36 (46%) patients. Table 1 shows demographic and clinical characteristics compared by SWD group. FSS at follow-up ranged from 6–12, and ≥75% had good functional outcomes (FSS=6–7). Older median age and presence of pre-admission chronic conditions were significantly associated with SWD. There was no association in bivariate analyses between SWD and institution or other demographic and clinical characteristics. Using multiple logistic regression controlling for demographic characteristics and diagnosis, presence of a pre-admission chronic condition was the only variable significantly associated with SWD, portending a 5-fold increased odds of SWD among the overall cohort (aOR 5.4; 95% CI 1.3–21.9).
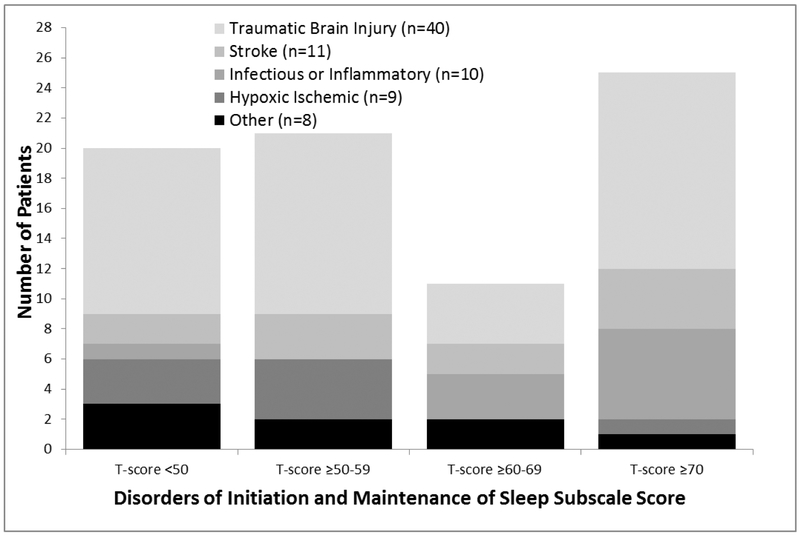
SWD Phenotypes
All SWD phenotypes measured by the SDSC were identified. Multiple SWD phenotypes were found in 30 (68%) of the 44 patients with SWD. Table 2 shows the overall cohort had significantly higher average scores in the total score and several subscales when compared to healthy children. Overall, the disorders of initiation and maintenance of sleep phenotype was most common with 37 (47%) patients having disturbance and 26 (33%) having severe disturbance (Figure 2). Sleep-wake transition disorders (n=18, 23%) and somnolence (n=15, 19%) were also prevalent phenotypes in the overall cohort. Sleep breathing disorder (n=8, 10%), arousal disorder (n=8, 10%), and hyperhidrosis (n=5, 6%) phenotypes were less common. Among patients with any SWD, 37 (84%) showed disturbance in the disorders of initiation and maintenance of sleep subscale.
Figure 2.
Distribution of standardized T-scores for the Disorders of Initiation and Maintenance of Sleep subscale is shown separated by primary diagnosis.
SWD by Diagnosis Group
Prevalence of SWD varied by diagnosis, but SWD were found in ≥33% in each subgroup. SWD were found in 9 (90%) patients with infectious and inflammatory diseases, 7 (64%) patients with stroke, 21 (53%) patients with TBI, 4 (50%) patients with other diagnoses, and 3 (33%) patients with hypoxic ischemic injury. The disorders of initiation and maintenance of sleep phenotype was most commonly disturbed among all diagnosis groups (Table 3).
Table 3.
Sleep Wake Disturbance Phenotypes by Diagnosis Group
| Phenotype | All N=78 |
TBI N=40 |
Stroke N=11 |
Infectious or Inflammatory N=10 |
Hypoxic Ischemic N=9 |
Other N=8 |
|---|---|---|---|---|---|---|
| Total Score | ||||||
| Median (IQR) | 36.5 (32,46) | 34 (30.5,45) | 42 (32.5,46) | 41.5 (37,47) | 32 (32,37) | 37 (33,46.5) |
| N (%) disturbance | 28 (36%) | 15 (38%) | 4 (36%) | 4 (40%) | 2 (22%) | 3 (38%) |
| N (%) severe | 8 (10%) | 5 (13%) | 0 | 2 (20%) | 1 (11%) | 0 |
| Disorders of Initiation and Maintenance of Sleep | ||||||
| Median (IQR) | 12 (9,16) | 11 (8.5,16.5) | 14 (10,17) | 16 (13,18) | 11 (8,12) | 11.5 (9,13.5) |
| N (%) disturbance | 37 (47%) | 17 (43%) | 6 (55%) | 9 (90%) | 2 (22%) | 3 (38%) |
| N (%) severe | 26 (33%) | 13 (33%) | 4 (36%) | 6 (60%) | 2 (22%) | 1 (13%) |
| Sleep Breathing Disorders | ||||||
| Median (IQR) | 3 (3,4) | 3 (3,4) | 3 (3,5) | 3.5 (3,6) | 3 (3,4) | 3.5 (3,4.5) |
| N (%) disturbance | 8 (10%) | 2 (5%) | 1 (9%) | 3 (30%) | 1 (11%) | 1 (13%) |
| N (%) severe | 4 (5%) | 1 (3%) | 1 (9%) | 1 (10%) | 1 (11%) | 0 |
| Disorders of Arousal | ||||||
| Median (IQR) | 3 (3,3) | 3 (3,3) | 3 (3,3) | 3 (3,5) | 3 (3,4) | 3 (3,4.5) |
| N (%) disturbance | 8 (10%) | 2 (5%) | 0 | 3 (30%) | 1 (11%) | 2 (25%) |
| N (%) severe | 8 (10%) | 2 (5%) | 0 | 3 (30%) | 1 (11%) | 2 (25%) |
| Sleep Wake Transition Disorders |
||||||
| Median (IQR) | 8 (7,10) | 7 (6,10.5) | 7 (6.5,8) | 9 (7,11) | 8 (7,10) | 9 (7,10) |
| N (%) disturbance | 18 (23%) | 10 (25%) | 1 (9%) | 4 (40%) | 2 (22%) | 1 (13%) |
| N (%) severe | 6 (8%) | 5 (13%) | 0 | 0 | 1 (11%) | 0 |
| Hypersomnolence | ||||||
| Median (IQR) | 7 (5,9) | 7 (5,9) | 7 (6.5,7.5) | 7.5 (5,9) | 6 (5,8) | 6 (5.5,9.5) |
| N (%) disturbance | 15 (19%) | 8 (20%) | 1 (9%) | 2 (20%) | 2 (22%) | 2 (25%) |
| N (%) severe | 7 (9%) | 6 (15%) | 0 | 1 (10%) | 0 | 0 |
| Sleep Hyperhidrosis | ||||||
| Median (IQR) | 2 (2,3) | 2 (2,3) | 2 (2,3.5) | 2 (2,2) | 2 (2,2) | 2 (2,3) |
| N (%) disturbance | 5 (6%) | 3 (8%) | 1 (9%) | 0 | 0 | 1 (13%) |
| N (%) severe | 1 (1%) | 0 | 1 (9%) | 0 | 0 | 0 |
Total and subscale scores from the Sleep Disturbances Scale for Children; Disturbance defined as T-score ≥60; Severe defined as T-score ≥70
More than 50% of TBI patients had SWD and showed significant differences from published results in healthy children (Table 2).25 No association between SWD and severity, mechanism, or location of TBI was found (Table 4). Type of intracranial injury was not statistically different between SWD groups. Pre-admission chronic conditions were strongly associated with SWD in the TBI population (52% with SWD versus 5% without, p=.001). The most prevalent pre-admission conditions identified in TBI were attention deficit hyperactivity disorder (ADHD) and behavioral disorders (n=5), but this was not statistically different between SWD groups. The disorders of initiation and maintenance of sleep subscale was disturbed in 17 (43%) TBI patients and severely disturbed in 13 (33%) patients. Sleep-wake transition disorders (25%) and somnolence (20%) phenotypes were also common. Phenotypes did not vary between mild complicated, moderate, and severe TBI patients.
Table 4.
Clinical Characteristics by Sleep Wake Disturbance Group among Traumatic Brain Injury Patients
| TBI patient characteristics | NoSWD N=19 (48%) |
+SWD N=21 (52%) |
Pvalue |
|---|---|---|---|
| Admission GCS median (IQR) | 12 (7.5,15) | 12 (9,15) | .83 |
| Severity of TBI | .86 | ||
| Mild Complicated | 8 (42%) | 10 (48%) | |
| Moderate | 5 (26%) | 6 (29%) | |
| Severe | 6 (32%) | 5 (24%) | |
| Age in years | 9.8 (6.2,12.9) | 10.1 (8, 13) | .31 |
| Pre-admission chronic condition | 1 (5%) | 11 (52%) | .001 |
| Any critical care intervention | 13 (68%) | 9 (43%) | .11 |
| Male gender | 11 (58%) | 17 (81%) | .11 |
| Mechanism | .26 | ||
| Motor vehicle occupant | 5 (15%) | 3 (7%) | |
| All-Terrain Vehicle | 1 (3%) | 1 (2%) | |
| Fall | 7 (21%) | 6 (14%) | |
| Auto-pedestrian or Auto-bicycle | 1 (3%) | 6 (14%) | |
| Bicycle or Scooter | 3 (9%) | 5 (11%) | |
| Penetrating | 2 (6%) | 0 | |
| Other traumatic injuries | 12 (63%) | 12 (57%) | .70 |
| Type of injurya | |||
| Skull fracture | 7 (37%) | 14 (66%) | .06 |
| Subdural | 5 (26%) | 7 (33%) | .63 |
| Epidural | 2 (11%) | 3 (14%) | .72 |
| Subarachnoid | 8 (42%) | 8 (38%) | .8 |
| Contusion | 10 (53%) | 12 (57%) | .78 |
| Diffuse axonal injury | 3 (16%) | 4 (19%) | .79 |
| Location of brain injurya | |||
| Frontal | 9 (47%) | 11 (52%) | .75 |
| Parietal | 8 (42%) | 10 (48%) | .73 |
| Temporal | 6 (32%) | 6 (29%) | .84 |
| Occipital | 5 (26%) | 8 (38%) | .43 |
| Loss of Consciousness | 10 (53%) | 12 (57%) | .16 |
| Other non-brain injuries | 12 (63%) | 12 (57%) | .7 |
| Inpatient rehabilitation discharge | 2 (11%) | 3 (14%) | .72 |
| Clinic Functional Status Scale, Median (IQR) | 6 (6,6) | 6 (6,6) | >.99 |
TBI: Traumatic Brain Injury; GCS: Glasgow Coma Scale; IQR: Interquartile Range
multiple responses possible in a single patient
Mann Whitney U tests were used for continuous variables and chi-square tests for categorical variables
Discussion
Among children with acquired brain injury treated in critical care follow-up clinics after discharge, SWD are highly prevalent and often severe. Risk of SWD was increased in children with pre-admission chronic conditions, but SWD were not associated with severity of injury measures. Many SWD phenotypes were found, some varying by diagnosis, and multiple SWD phenotypes co-existed in the majority of patients. The disorders of initiation and maintenance of sleep phenotype was most common and nearly universally identified in patients with SWD. These disturbances were also frequently severe and may serve as a target for future intervention studies seeking to improve outcomes in critical care survivors with acquired brain injury.
Our study adds to literature showing SWD are important outcomes in survivors of critical care and brain injury. To our knowledge, it is the first to describe SWD after many PNCC diagnoses. Case reports of SWD in children with stroke, meningitis, and hypoxic ischemic injury are reported, though SWD have not been systematically evaluated in these populations after critical care.27,28 Our rates of SWD among children with TBI are similar to prior reports showing high rates of somnolence, insomnia, and overall disturbances after pediatric TBI when compared to controls.17,19–22 One prior study used the SDSC in a PNCC population, showing significantly worse SWD in children after TBI compared to healthy controls, and reported similar total SDSC scores to our population.19 SWD are also reported in broader populations of children surviving critical care, with high rates similar to our study, and much higher than healthy children.29,30 Taken together, results highlight the importance of evaluating SWD in all PNCC survivors.
Our study additionally evaluated SWD phenotypes, showing the disorders of initiation and maintenance of sleep subscale was abnormal in most children with SWD after acquired brain injury. This subscale suggests insomnia or circadian rhythm disturbances are contributing to SWD in children surviving PNCC. Insomnia has been described in up to 60% of adults with TBI and after concussion.8 Poor sleep efficiency and impaired onset and maintenance was reported using actigraphy in 15 children with moderate and severe TBI consistent with insomnia.22 Circadian rhythm disturbances are less well described in the brain injury literature.8 Patients with visual impairment may be at increased risk of circadian disruption,31 though none of our patients had complete blindness or cortical visual impairment at follow-up. Hospitalized patients do have altered levels of melatonin and circadian rhythms while inpatient due to cares, medications, and persistently high ambient light levels,32,33 and patients with brain injury have greater alterations compared to other hospitalized patients.34,35 It is possible that children in our cohort have acquired circadian rhythm disturbance from brain injury compounded by the hospital environment, but more research is needed to distinguish these phenotypes and investigate the relative contribution of brain injury and the therapeutic environment. Both insomnia and circadian rhythm disturbances have been treated successfully in pediatric populations,36,37 but interventions to treat these SWD after critical care have not been studied.27,38,39 It remains unknown if interventions during or after hospitalization to improve sleep could augment recovery after discharge for pediatric acquired brain injury.
Risk of SWD was significantly increased with pre-admission chronic conditions in our cohort. We found similar rates of chronic conditions in PNCC patients as prior studies.3 Chronic conditions, such as epilepsy, asthma, ADHD, and autism are associated with SWD.37,40 We did not measure baseline SWD to determine effects of pre-injury SWD or potential association with pre-admission chronic conditions. A small number of our patients had any one of these individual chronic conditions limiting our ability to determine if specific pre-admission conditions were associated with SWD. One prior study did show children with TBI and concurrent ADHD had worse SWD than ADHD controls 1–4 years after injury.41 The acquired brain injury may compound pre-injury SWD or increase risk of SWD among those with pre-existing chronic conditions. However, most children in our study were previously healthy and prevalence of SWD was higher than reports in healthy children. This suggests the acquired brain injury and hospital course, rather than solely pre-admission conditions, explain our findings.
Older age was associated with SWD in bivariate analysis. Adolescents and teens are reported to have high rates of baseline SWD, which may explain the trend for increased SWD with older age in our study. Estimates show 30–40% of teenagers may have clinically important SWD at baseline, while estimates are lower in pre-school to adolescence.42 Older children may have more insight into problems sleeping, more effectively communicate problems to caregivers, or have behavioral differences in screen-time, caffeine intake, and sleep schedules contributing to these findings. Prior studies in TBI show inconsistent results with respect to age and SWD, and our analysis did not find age to be an independent risk factor when controlling for confounders in multivariable analysis. Additionally, most prior studies focus on narrower age ranges and have small sample sizes, thereby limiting direct comparison to our study.17,20–22,43
We found overall SWD were not associated with measures of severity of illness, including need for critical care interventions, functional outcome, or discharge to inpatient rehabilitation. Prior studies of heterogeneous pediatric critical care cohorts also failed to show associations between SWD and severity of illness markers or length of stay.29,30 While not associated with SWD in our study, some of the markers we used for severity of illness (e.g. critical care interventions) have been associated with delusional memories, delirium, and risk for post-traumatic stress,44–46 all of which may impact sleep. Evaluation of these important outcomes as mediators of SWD after discharge should be evaluated in future studies.
In the TBI subgroup, our study also found overall SWD were not associated with Glasgow Coma Scale on admission, loss of consciousness, or type or location of intracranial injury, and is consistent with prior work showing SWD are pervasive after all severities of TBI.8,17,19 We additionally found no difference in SWD phenotypes based on severity of TBI. While some adult studies suggest differences based on severity,8 prior literature in pediatric populations with injuries more severe than concussion are limited and have variable results. Osorio et al found increased daytime sleepiness in adolescents with moderate or severe TBI compared to mild complicated TBI.20 Shay et al evaluated young children and found no difference in daytime sleepiness based on severity of TBI, but did show increased bedtime resistance in patients with severe TBI.21 Daytime fatigue was also similar in children by TBI severity in other studies.47–49 Differences between available studies and our findings are likely explained by different populations, measurement tools, and limited sample sizes. Associations between sleep phenotypes and injury characteristics should be assessed in future studies with larger populations using validated measures of SWD to inform targeted intervention studies.
Given known associations between SWD and poor academic achievement, depression, and obesity in otherwise healthy children, SWD represent a substantial problem.13–15,37 SWD impair neuronal development and healing,9–12 a function even more critical in the developing brain and after injury. SWD offer a potentially modifiable target to improve recovery after acquired brain injury, and our results underscore the importance of systematically evaluating sleep in these children.
While our study includes data from two centers, our centers are unique in the presence of coordinated critical care follow-up programs. Most institutions do not have similar programs,5 and care of children with morbidities after brain injury is often left to general practitioners and subspecialists. Our unique clinical population limits generalizability, but our results show a need for increased awareness of SWD after acquired brain injury in PNCC survivors. Our study has several other limitations to consider including lack of pre-injury sleep measures, parent-reported questionnaires to define sleep outcomes, short-term follow-up, and lack of objective measures of SWD to supplement the questionnaire data. Prevalence of SWD in our study was high suggesting a large increase in prevalence even if baseline disturbances are present. Additionally, questionnaires may not capture the true prevalence of SWD relying on recall and estimation of events. The SDSC represents one of the only validated multidimensional tools to measure sleep in pediatric patients,50 but future studies should utilize objective measures like actigraphy and polysomnography to supplement patient and parent report. Our follow-up evaluations were limited to 1–3 months after discharge, so the trajectory of SWD after PNCC remains largely unknown, though studies in TBI have documented persistence of SWD several years after injury.17,51 Despite these limitations, our study highlights an important problem in survivors with acquired brain injury for which future research is needed.
Conclusion
SWD are an important morbidity affecting more than 50% of children surviving critical care with acquired brain injury in the months after discharge, and are frequently severe. Phenotypes consistent with insomnia or circadian rhythm disturbances were most common, but all SWD phenotypes were found in our cohort. SWD can impair physical, cognitive, and psychosocial functions, and our study showed SWD were pervasive in all diagnoses and regardless of severity of acute injury. This underscores the importance of evaluating SWD after discharge. More research is needed to identify effective interventions to prevent and treat SWD and determine if treating SWD can also augment recovery from acquired brain injury in other important domains.
Supplementary Material
Acknowledgments:
This research was made possible with support from the Oregon Clinical and Translational Research Institute (OCTRI), grant number UL1RR024140 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research
Funding source: Dr. Williams is supported by the Agency for Healthcare Research and Quality, grant number K12HS022981. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality. Dr. McEvoy is supported by the National Heart Lung Blood Institute, R01 HL105447 with co-funding from the Office of Dietary Supplement, R01H L129060 and UG3OD023288. Dr. Lim is supported with resources and the use of facilities at the VA Portland Health Care System and VA Career Development Award #IK2 BX002712 to MML. Interpretations and conclusions are those of the authors and do not represent the views of the U.S. Department of Veterans Affairs or the United States Government. Dr. Shea is supported by the National Institutes of Health grants R01-HL125893, R01-HL125893–03S1, R01-HL142064, and R01 HL140577, as well as the Oregon Institute of Occupational Health Sciences via funds from the Division of Consumer and Business Services of the State of Oregon (ORS 656.630). Dr. Guilliams is supported by the National Institute of Neurologic Disorders and Stroke grant number K23NS099472. Dr. Piantino is supported by the National Heart, Lung and Blood Institute grant number K12HL133115.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures: The authors have no conflicts of interest or financial relationships relevant to this article to disclose
References
- 1.Moreau JF, Fink EL, Hartman ME, et al. Hospitalizations of children with neurologic disorders in the United States. Pediatr Crit Care Med 2013;14:801–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wainwright MS, Grimason M, Goldstein J, et al. Building a pediatric neurocritical care program: a multidisciplinary approach to clinical practice and education from the intensive care unit to the outpatient clinic. Semin Pediatr Neurol 2014;21:248–54. [DOI] [PubMed] [Google Scholar]
- 3.Williams CN, Piantino J, McEvoy C, Fino N, Eriksson CO. The Burden of Pediatric Neurocritical Care in the United States. Pediatric neurology 2018;89:31–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pollack MM, Holubkov R, Funai T, et al. Pediatric intensive care outcomes: development of new morbidities during pediatric critical care. Pediatr Crit Care Med 2014;15:821–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fink EL, Kochanek PM, Tasker RC, et al. International Survey of Critically Ill Children With Acute Neurologic Insults: The Prevalence of Acute Critical Neurological Disease in Children: A Global Epidemiological Assessment Study. Pediatr Crit Care Med 2017;18:330–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Watson RS, Choong K, Colville G, et al. Life after Critical Illness in Children-Toward an Understanding of Pediatric Post-intensive Care Syndrome. J Pediatr 2018;198:16–24. [DOI] [PubMed] [Google Scholar]
- 7.Herrup EA, Wieczorek B, Kudchadkar SR. Characteristics of postintensive care syndrome in survivors of pediatric critical illness: A systematic review. World J Crit Care Med 2017;6:124–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sandsmark DK, Elliott JE, Lim MM. Sleep-Wake Disturbances After Traumatic Brain Injury: Synthesis of Human and Animal Studies. Sleep 2017;40:1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Volk C, Huber R. Sleep to grow smart? Arch Ital Biol 2015;153:99–109. [DOI] [PubMed] [Google Scholar]
- 10.Ringli M, Huber R. Developmental aspects of sleep slow waves: linking sleep, brain maturation and behavior. Prog Brain Res 2011;193:63–82. [DOI] [PubMed] [Google Scholar]
- 11.Jan JE, Reiter RJ, Bax MC, Ribary U, Freeman RD, Wasdell MB. Long-term sleep disturbances in children: a cause of neuronal loss. Eur J Paediatr Neurol 2010;14:380–90. [DOI] [PubMed] [Google Scholar]
- 12.Kocevska D, Muetzel RL, Luik AI, et al. The Developmental Course of Sleep Disturbances Across Childhood Relates to Brain Morphology at Age 7: The Generation R Study. Sleep 2017;40:1–9. [DOI] [PubMed] [Google Scholar]
- 13.Chang CH, Chen SJ, Liu CY. Pediatric sleep apnea and depressive disorders risk: A population-based 15-year retrospective cohort study. PLoS One 2017;12:e0181430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gozal D, Kheirandish-Gozal L. Neurocognitive and behavioral morbidity in children with sleep disorders. Curr Opin Pulm Med 2007;13:505–9. [DOI] [PubMed] [Google Scholar]
- 15.Owens JA. Neurocognitive and behavioral impact of sleep disordered breathing in children. Pediatr Pulmonol 2009;44:417–22. [DOI] [PubMed] [Google Scholar]
- 16.Williams CN, Lim MM, Shea SA. Sleep disturbance after pediatric traumatic brain injury: critical knowledge gaps remain for the critically injured. Nat Sci Sleep 2018;10:225–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gagner C, Landry-Roy C, Laine F, Beauchamp MH. Sleep-Wake Disturbances and Fatigue after Pediatric Traumatic Brain Injury: A Systematic Review of the Literature. J Neurotrauma 2015;32:1539–52. [DOI] [PubMed] [Google Scholar]
- 18.Williams CN, Kirby A, Piantino J. If You Build It, They Will Come: Initial Experience with a MultiDisciplinary Pediatric Neurocritical Care Follow-Up Clinic. Children (Basel) 2017;4:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fischer JT, Hannay HJ, Alfano CA, Swank PR, Ewing-Cobbs L. Sleep disturbances and internalizing behavior problems following pediatric traumatic injury. Neuropsychology 2018;32:161–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Osorio MB, Kurowski BG, Beebe D, et al. Association of daytime somnolence with executive functioning in the first 6 months after adolescent traumatic brain injury. PM R 2013;5:554–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shay N, Yeates KO, Walz NC, et al. Sleep problems and their relationship to cognitive and behavioral outcomes in young children with traumatic brain injury. J Neurotrauma 2014;31:1305–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sumpter RE, Dorris L, Kelly T, McMillan TM. Pediatric sleep difficulties after moderate-severe traumatic brain injury. J Int Neuropsychol Soc 2013;19:829–34. [DOI] [PubMed] [Google Scholar]
- 23.Dodd JN, Hall TA, Guilliams K, et al. Optimizing Neurocritical Care Follow-Up Through the Integration of Neuropsychology. Pediatric neurology 2018;89:58–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pollack MM, Holubkov R, Glass P, et al. Functional Status Scale: new pediatric outcome measure. Pediatrics 2009;124:e18–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bruni O, Ottaviano S, Guidetti V, et al. The Sleep Disturbance Scale for Children (SDSC). Construction and validation of an instrument to evaluate sleep disturbances in childhood and adolescence. J Sleep Res 1996;5:251–61. [DOI] [PubMed] [Google Scholar]
- 26.Romeo DM, Bruni O, Brogna C, et al. Application of the sleep disturbance scale for children (SDSC) in preschool age. Eur J Paediatr Neurol 2013;17:374–82. [DOI] [PubMed] [Google Scholar]
- 27.Keegan LJ, Reed-Berendt R, Neilly E, Morrall MC, Murdoch-Eaton D. Effectiveness of melatonin for sleep impairment post paediatric acquired brain injury: evidence from a systematic review. Dev Neurorehabil 2014;17:355–62. [DOI] [PubMed] [Google Scholar]
- 28.Schmidt H, Cohrs S, Heinemann T, et al. Sleep disorders are long-term sequelae of both bacterial and viral meningitis. J Neurol Neurosurg Psychiatry 2006;77:554–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Als LC, Picouto MD, Hau SM, et al. Mental and physical well-being following admission to pediatric intensive care. Pediatr Crit Care Med 2015;16:e141–9. [DOI] [PubMed] [Google Scholar]
- 30.Colville GA, Pierce CM, Peters MJ. Self-Reported Fatigue in Children Following Intensive Care Treatment. Pediatr Crit Care Med 2019;20:e98–e101. [DOI] [PubMed] [Google Scholar]
- 31.Uchiyama M, Lockley SW. Non-24-Hour Sleep-Wake Rhythm Disorder in Sighted and Blind Patients. Sleep Med Clin 2015;10:495–516. [DOI] [PubMed] [Google Scholar]
- 32.Tan X, van Egmond L, Partinen M, Lange T, Benedict C. A narrative review of interventions for improving sleep and reducing circadian disruption in medical inpatients. Sleep Med 2018:epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 33.Kudchadkar SR, Aljohani OA, Punjabi NM. Sleep of critically ill children in the pediatric intensive care unit: a systematic review. Sleep Med Rev 2014;18:103–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Grima NA, Ponsford JL, St Hilaire MA, Mansfield D, Rajaratnam SM. Circadian Melatonin Rhythm Following Traumatic Brain Injury. Neurorehabil Neural Repair 2016;30:972–7. [DOI] [PubMed] [Google Scholar]
- 35.Marseglia L, D’Angelo G, Manti S, et al. Melatonin Secretion Is Increased in Children with Severe Traumatic Brain Injury. Int J Mol Sci 2017;18:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Abdelgadir IS, Gordon MA, Akobeng AK. Melatonin for the management of sleep problems in children with neurodevelopmental disorders: a systematic review and meta-analysis. Archives of disease in childhood 2018;103:1155–62. [DOI] [PubMed] [Google Scholar]
- 37.Ophoff D, Slaats MA, Boudewyns A, Glazemakers I, Van Hoorenbeeck K, Verhulst SL. Sleep disorders during childhood: a practical review. Eur J Pediatr 2018;177:641–8. [DOI] [PubMed] [Google Scholar]
- 38.Bogdanov S, Naismith S, Lah S. Sleep outcomes following sleep-hygiene-related interventions for individuals with traumatic brain injury: A systematic review. Brain Inj 2017;31:422–33. [DOI] [PubMed] [Google Scholar]
- 39.Galland BC, Elder DE, Taylor BJ. Interventions with a sleep outcome for children with cerebral palsy or a post-traumatic brain injury: a systematic review. Sleep Med Rev 2012;16:561–73. [DOI] [PubMed] [Google Scholar]
- 40.Delahaye J, Kovacs E, Sikora D, et al. The relationship between Health-Related Quality of Life and sleep problems in children with Autism Spectrum Disorders. Research in Autism Spectrum Disorders 2014;8:292–303. [Google Scholar]
- 41.Ekinci O, Okuyaz C, Gunes S, et al. Sleep and quality of life in children with traumatic brain injury and ADHD. Int J Psychiatry Med 2017;52:72–87. [DOI] [PubMed] [Google Scholar]
- 42.Archbold KH, Pituch KJ, Panahi P, Chervin RD. Symptoms of sleep disturbances among children at two general pediatric clinics. J Pediatr 2002;140:97–102. [DOI] [PubMed] [Google Scholar]
- 43.Beebe DW, Krivitzky L, Wells CT, Wade SL, Taylor HG, Yeates KO. Brief report: parental report of sleep behaviors following moderate or severe pediatric traumatic brain injury. J Pediatr Psychol 2007;32:845–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Colville G, Kerry S, Pierce C. Children’s factual and delusional memories of intensive care. Am J Respir Crit Care Med 2008;177:976–82. [DOI] [PubMed] [Google Scholar]
- 45.Patel AK, Bell MJ, Traube C. Delirium in Pediatric Critical Care. Pediatr Clin North Am 2017;64:1117–32. [DOI] [PubMed] [Google Scholar]
- 46.Rennick JE, Rashotte J. Psychological outcomes in children following pediatric intensive care unit hospitalization: a systematic review of the research. J Child Health Care 2009;13:128–49. [DOI] [PubMed] [Google Scholar]
- 47.Crichton AJ, Babl F, Oakley E, et al. Prediction of Multidimensional Fatigue After Childhood Brain Injury. J Head Trauma Rehabil 2017;32:107–16. [DOI] [PubMed] [Google Scholar]
- 48.Crichton A, Anderson V, Oakley E, et al. Fatigue Following Traumatic Brain Injury in Children and Adolescents: A Longitudinal Follow-Up 6 to 12 Months After Injury. J Head Trauma Rehabil 2017. [DOI] [PubMed] [Google Scholar]
- 49.van Markus-Doornbosch F, de Kloet AJ, Berger MA, Lambregts SA, Wolterbeek R, Vliet Vlieland TP. Factors related to fatigue after paediatric acquired brain injury (ABI). Brain Inj 2016;30:1533–41. [DOI] [PubMed] [Google Scholar]
- 50.Spruyt K, Gozal D. Pediatric sleep questionnaires as diagnostic or epidemiological tools: a review of currently available instruments. Sleep Med Rev 2011;15:19–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Aaro Jonsson CC, Emanuelson IM, Charlotte Smedler A. Variability in quality of life 13 years after traumatic brain injury in childhood. Int J Rehabil Res 2014;37:317–22. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.