Abstract
Work relative value unit (wRVU) - based fee schedules are predominantly used by both the Center for Medicare and Medicaid Services (CMS) and private payers to determine the payments for physicians' clinical productivity. However, under the Affordable Care Act, CMS is transitioning into value-based payment structure that rewards patient-oriented outcomes and cost savings. Moreover, in the context of solid organ transplantation, physicians and surgeons conduct many activities that are neither billable nor accounted for in the wRVU models. New compensation models for transplant professionals must (i) justify payments for non-billable work related to transplant activity/procedures; (ii) capture the entire academic, clinical, and relationship-building work effort as part of RVU determination, and (iii) move towards a value-based compensation scheme that aligns the incentives for physicians, surgeons, transplant center, payers, and patients. In this review, we provide an example of redesigning RVUs to address these challenges in compensating transplant physicians and surgeons. We define a customized RVU (cRVU) for activities that typically do not generate wRVUs and create an outcome value unit (OVU) measure that incorporates outcomes and cost savings into RVUs to include value-based compensation.
INTRODUCTION:
Since their inception in 1988, relative value units (RVU) have become a widely accepted basis for ranking and evaluating the resources required and expended by physicians in providing each service. Both CMS and private payers use RVU-based fee schedules to determine the payments for physicians' work effort. The RVU rate, updated annually by the Center for Medicare and Medicaid Services (CMS), includes compensation for three types of resources: physician’s work (e.g., physician time), practice expenses (e.g., nonclinical labor and building space), and malpractice costs with geographic considerations in mind (e.g., malpractice insurance premiums).
The focus of this paper is work-RVUs (wRVU), which quantitates physicians’ effort based on time, technical skill, and cognition in providing a service. Simply put, work-RVUs (wRVU) are assigned to clinical activities; multiplying a dollar amount per wRVU by the number of RVUs performed by a physician (in direct patient care) determines the compensation for those clinical activities. Besides, a summation of wRVUs generated over a period is used as a standard to define overall physician productivity.
The origins of wRVU come from a study in which physicians evaluated patient vignettes in terms of work effort in comparison to some reference services. It is periodically updated based on the recommendations from the American Medical Association/Specialty Society Relative Value Scale Update Committee (RUC). The methodology evolved over the years and became the uniform approach to maintaining schedules for fee-for-service payments and ensuring clinical work is valued the same across services. The evolution of wRVU, however, did not parallel the shift from fee-for-service to value-focused healthcare.1 With the increasing regulatory emphasis on cost-efficient care, and the advent of new payment and delivery models such as accountable care organizations (ACO), there is a dire need for redefining what constitutes an RVU and aligning physician and payer incentives to deliver value. Transplantation, subject to federal regulation and public oversight, is uniquely positioned to address such a need and lead the way to value-based payments2 as it has been, for years, at the forefront of delivering value-driven, accountable, and team-based care.3, 4
Benefits and challenges of the RVU system
Provider compensation is widely based on the number of wRVUs generated as an indicator of the volume of the work performed, also referred to as clinical productivity. There exist several benefits of using wRVUs as a basis to compensate providers’ clinical effort. From the provider’s perspective, it encourages work and is generally perceived as fair because clinically productive providers receive higher compensation under such schema. From a hospital or system perspective, the wRVU metric has merit as it (i) provides a uniform and transparent metric of physician effort across many types of patient care, (ii) links clinical effort to payment, and (iii) has already overcome the hurdles that an alternative model would face, such as buy-in from payers, physicians and hospital managers.
Nonetheless, there exist key challenges to using wRVUs in compensating providers. The wRVUs may not fully capture labor-intensive tasks, often do not differentiate complex from non-complex patients, may not reward non-clinical activities such as education and research, and, entirely only, promote volume over value. Some challenges may arise with changing payment and delivery models that should be addressed.1 For instance, as physicians become aware of wRVU rates, clinical work that generates more wRVUs may be emphasized over work equally crucial to patients and payers, but associated with lower compensation. For example, conducting a procedure for differential diagnosis would generate revenue while spending additional time to understand patient preferences would not. Modifications to wRVU should be carefully designed to avoid the unintended effects such as “distorted RVUs,” which was exemplified in the shift of cardiac imaging from physician offices to hospitals as a result of reweighing of RVUs.1 Hence, as we move to a value-based scheme, aligning the incentives of physicians, payers, and patients is essential, and will likely require changes in wRVU-based compensation.
In the context of solid organ transplantation, with its unique relationship between institutions and physicians/surgeons, there are additional specific challenges.5 These include: (i) justifying payments for non-billable work related to transplant activity / procedures (satellite clinic visits, organ placement coordination, organ recovery including dry-runs, robotic surgery, additional work burden such as patient portals, publications, and teaching sessions), (ii) capturing the effort required of physicians/surgeons in support of the transplant center and infrastructure (academic, clinical, and relationship building) as part of RVU determination, and contributing to regional and national transplant governing bodies.6 We believe sufficient data and experience already exist to address these challenges in solid organ transplantation and provide an institution-based example of redesigning RVUs to quantitate better and compensate transplant services.
Transplant Physician and Surgeon Compensation Structure:
A variety of options exist to address the limitations in the wRVU-based payments for transplant providers. For example, transplant centers can withhold a portion of the overall physician/surgeon compensation or ancillary revenue generated from wRVU activities, and then redistribute the withheld part to value-generating activities. The redistribution can target billable activities to incentivize clinical work that improves patient outcomes, or it can focus on non-billable activities such as outreach, writing, or teaching. The challenge with this approach is convincing those who will observe a reduction in their incomes to support the non-clinical work of others. This approach is successful in some physician practices that generate significant ancillary revenue that can be used to create the pool. Another example is increasing the payments for wRVUs generated from high-value clinical activities (e.g., satellite clinic visits for providing convenient access to care, monitoring, and care coordination). Specific payment adjustments could be proportional to the impact of individual activities on outcomes or overall program success; hence, the per-RVU conversion rate would reflect the value of the activity. Abouljoud et al. propose recognizing and rewarding non-RVU generating activities through the use of “virtual RVUs.”6
Our proposed cRVU and OVU metrics are consistent with the concept of virtual RVUs but also promote the value-generating clinical effort. We offer a customized RVU (cRVU) for activities that typically do not generate wRVUs and create an outcome value unit (OVU) measure that incorporates outcomes and cost savings into RVUs based on value-based compensation. The newly developed cRVU corrects flaws in the wRVU while quantitating typically uncompensated work effort in an easily traceable and transparent fashion. Most transplant centers in the United States exist within academic medical centers; these new RVU metrics were developed with academic practices in mind.7-9 However, the proposed RVU metrics can be a roadmap for non-academic transplant centers that seek to compensate physicians/surgeons for non-clinical work as well as align their activities with the changing payment and delivery environment. Hence, some of the uncompensated work efforts are unique to transplant (e.g., reviewing organ offers and recovering organs) while others are common to most specialties (e.g., training residents and fellows, research & publications). We also note that the cRVU and OVU metrics we propose do not target activities that make clinical care possible, particularly those covered by practice expense RVUs.
Customized RVU (cRVU) and Outcome Value Units (OVU):
Creating cRVU and OVU has multiple advantages. Transplant surgeons and physicians engage in many activities, some of which (e.g., travel for organ recovery, set up and maintain satellite clinics, outreach referring physician visits, quality and safety process improvement, the UNOS data registry management, regulatory oversight, budget, and insurance contract reviews, and teaching), though non-billable, are critical to the success of the center. Promoting these activities that improve quality and value is essential in realizing not only the objectives of a transplant center but also enhancing the financial stability of the organization. Quantifying such activities through cRVU and OVU makes these activities transparent throughout the organization, consistent with the team approach so prevalent in transplantation. The payments associated with cRVU and OVU align the incentives of the physicians, surgeons, and the transplant center to work towards the common good while avoiding the detrimental perception of unequal pay for the work effort. The cRVU and OVU metrics are easy to tailor to ever-changing delivery and payment models and can facilitate meeting the needs of individual organizations. The separation of cRVU and OVU from wRVUs can also avoid the possible unintended effects of reweighing RVUs to compensate for distorted RVUs. Potential disadvantages to cRVU and OVU constructs include introducing incentives for non-patient care activities that can lead to less patient care activities being performed at transplant centers. Additionally, the new RVU metrics require more administrative effort among physicians/surgeons and center management to generate granular reporting and tracking of RVUs, a potential burden in an already documentation-heavy work environment.
Creating cRVU:
Designing cRVUs requires identification of what work activity is not captured in the current wRVU system. Examples of cRVUs involve: 1) for a transplant physician/surgeon (Table 1a-b) including teaching activities (lecturing/mentoring fellows, residents, and medical students), excess on call (higher than 5 days per month), co-authoring abstract and manuscript and/or book chapter writing, marketing and outreach visits, satellite start up and coverage, virtual (provider-patient interactions that occur via e-mail or through a Web-based portal) and/or telemedicine (store-and-forward, remote patient monitoring, real-time online encounter), being a principal or sub-investigator of a research study, patient identification/enrollment for research study, and supervising physician assistants and nurse practitioners; 2) for a transplant surgeon (Table 1c-d) comprising organ procurement, dry-runs, and utilization of robotic procedures; 3) non-face-to-face prolonged services (crediting for patient complexity during pre and post-transplant phases) before and/or after direct patient care (Table 1e) covering chart review, following up on patients’ test results, calling patients and meeting with their families, peer-to peer review, literature search, pre-procedure preparation, pre-authorization, coordination of care, updating referring physicians, and patient satisfaction. Each transplant center will incorporate different cRVUs into their physician/surgeon compensation to acknowledge the value of these essential cognitive clinical works depending on their institutions’ goals and needs. Then, this cRVUs are converted to compensation at a rate according to fair market value. The cRVU payment is based on direct patient care, on-call hourly or daily rates, or medical/surgical director hourly rates.
Table 1a.
Definition, rationale, and data source for customized relative value unit (cRVU) for a transplant physician/surgeon.
| Mnemonic | Definition of the Activity |
Activity Type/Time Spent |
cRVU | The Rationale for How cRVUs Are Calculated |
Sample Data Source |
|---|---|---|---|---|---|
| ATT | Manuscript development, research activity, teaching residents and fellows, clinical/regulatory meetings including patient selection, pathology, tumor board, radiology, QAPI | 30 min | 0.56 | RVU calculated on $106 per hour at a rate of $56 per RVU=1.12 RVU per hour or 0.56 RVUs per 30 min (based on CMS Medical Director RCE total August 22, 2014, for hourly rate and FMV source compensation per wRVU) | Fee ticket, sign-in sheets, physician calendars, time studies |
| MANPR | The primary author of manuscript or book chapter publication | Event | 48.00 | Calculated based on an average of 15 patients × New Patient visit code 99205 (RVUs 3.2) =48 RVU | E-copy of publications |
| MANCO | Co-author manuscript or book chapter publication | Event | 24.00 | Calculated based on an average of 15 patients × New Patient visit code 99205 (RVUs 3.2/2) =24 RVU | E-copy of publications |
| MRKT | Marketing and outreach. No additional if included in hours of medical director stipend | 30 min | 2.20 | RVU calculated on $214 per hour at a rate of $48.56 per RVU= 4.4 RVU per hour or 2.2 RVUs per 30 min (based on FMV source median salary and median wRVU) | Physician Calendars, fee tickets, Outreach coordinator activities |
| STBN | Satellite start-up bonus | Event | 48.00 | Calculated based on an average of 15 patients × New Patient visit code 9205 (RVUs 3.2) =48 RVU | EMR |
| NCALL | On-call transplant physician/surgeon | 1 day | 10.29 | On-call market rates $500 per day/48.56 per RVU=10.29 RVUs (FMV source data based on five days per month is considered excessive and earns RVUs | Call schedule |
| STO1 | Coverage of more than one Satellite clinic located more than 30 miles but less than 50 miles away from the center | 1 day | 9.18 | The calculated average of 15 patients × Modified New Patient visit code 99204 (RVUs 2.45*15*25%) | EMR |
| ST30 | Coverage of more than one Satellite clinic located more than 50 miles but less than 100 miles away from the center | 1 day | 18.35 | The calculated average of 15 patients × Modified New Patient visit code 99204 (RVUs 2.45*15 *50%) | EMR |
| ST100 | Coverage of more than one Satellite clinic located more than 100 miles away from the center | 1 day | 36.75 | The calculated average of 15 patients × Modified New Patient visit code 99204 (RVUs 2.45*15*100%) | EMR |
| PICRD | Principal investigator research study | New study | 26.78 | Based on $1500 per study $1550/$56 per RVU=26.78 RVUs | Study list/Physician CV |
| SICRD | Sub investigator research study | New study | 13.39 | Based on $750 per study $750/$56 per RVU=13.39 RVUs | Study list/Physician CV |
| IREO | Patient identification and selection for research studies | Clinic visit | 3.20 | Credit for the time required for patient identification and selection for the research study. Calculated by New Patient Code 99205 (RVU 3.2) | 1st research study patient clinic visit |
| IRE1 | Initial research patient enrollment study lasts <6 months | 1st clinic visit | 3.20 | Credit for patient complexity during the research study. Calculated by New Patient Code 99205 (RVU 3.2) | Research coordinator 1st clinic visit and study timeline |
| IRE2 | Initial research patient enrollment study lasts 6-18 months | 1st clinic visit | 6.40 | Credit for patient complexity during the research study. Calculated by New Patient Code 99205 (RVU 3.2) multiplier 2 | Research coordinator 1st clinic visit and study timeline |
| IRE3 | Initial research patient enrollment study lasts >18 months | 1st clinic visit | 11.80 | Credit for patient complexity during the research study. Calculated by New Patient Code 99205 (RVU 3.2) multiplier 3 | Research coordinator 1st clinic visit and study timeline |
| EVAL | Patient evaluations, waitlist management, and pre-annuals. 1 × each annually per patient | Clinic visit | 3.20 | Credit for patient complexity during pre-transplant evaluations, waitlist management, and annuals. Calculated by New Patient Code 99205 (RVU 3.2) | EMR |
| POOLT | Clinic visit | 1.60 | Credit for patient complexity post-transplant management. Calculated by New Patient Code 99205 (RVU 3.2/2) multiplier ½ | EMR | |
| NPSUP | Clinic visit | 1.00 | Income for NP supervision $3.00 per NP wRVU | EMR |
Abbreviations: RVU, relative value unit; wRVU, work relative value unit; CMS Center for Medicare and Medicaid; RCE, reasonable compensation equivalent; FMV, fair market value.
Table 1b.
Sample calculation for transplant physicians/surgeons' customized relative value unit (cRVU), not included in the benchmark for salary or work RVUs per month.
| Mnemonic* | Corresponding Activity |
Sample Count* | cRVU (per Count) |
cRVU Total (Sample Count cRVU) |
|---|---|---|---|---|
| ATT1 | Teaching | 5 | 0.56 | 2.80 |
| NCALL/HCALL/SURG | On-call (up to 5) | 5 | 8.90 | 0.00 |
| NCALL/HCALL/SURG | Additional On-call over five nights per month | 5 | 8.90 | 44.50 |
| MANCO | Co-author of manuscript/chapter | 1 | 24.00 | 24.00 |
| MRKT | Marketing and outreach | 10 | 1.55 | 15.50 |
| ST01 | Satellite clinic within the transplant center's service area (<30 miles) | 10 | 9.80 | 98.00 |
| ST30 | Satellite clinic within the transplant center's service area (30-50 miles) | 4 | 27.56 | 110.24 |
| ST50 | Satellite clinic within the transplant center's service area (50-100 miles) | 4 | 36.75 | 147.00 |
| ST100 | Satellite clinic outside the transplant center's service area (>100 miles) | 2 | 45.94 | 91.88 |
| VTMED | Non-billable virtual/telemedicine | 30 | 3.20 | 96.00 |
| PICRD | Principal investigator research study | 5 | 26.78 | 133.900 |
| SICRD | Sub investigator research study | 5 | 13.39 | 66.95 |
| IREO | Patient identification and selection for research studies | 10 | 3.20 | 32.0 |
| IRE1 | Initial research patient enrollment study lasts <6 months | 5 | 3.20 | 16.00 |
| IRE2 | Initial research patient enrollment study lasts 6-18 months | 5 | 6.40 | 32.00 |
| IRE3 | Initial research patient enrollment study lasts >18 months | 5 | 11.8 | 59 |
| NPSUP | Supervising a nurse practitioner per clinical visit | 100 | 1.6 | 160.00 |
Abbreviation: CPT4: Current Procedural Terminology, 4th Edition.
The sample count is based on academic physician/surgeon working a mid-size program (50-100 transplants per year).
Table 1c:
Definition, rationale, and data source for customized relative value unit (cRVU) for a transplant surgeon, customized relative value unit (cRVU).
| CPT4 Codes |
CPT4 Description Activity | RVU* | RVU Rationale | Sample Data Source |
|---|---|---|---|---|
| 32850 | Donor pneumonectomy, including cold preservation, lung procurement research only | 2.81 | Based on $160 payment, 160/$55.16 per wRVU | Fee ticket |
| 33940 | Donor cardiectomy, including cold preservation, heart procurement research only | 2.81 | Based on $160 payment, 160/$55.16 per wRVU | Fee ticket |
| 44132 | Donor enterectomy, including cold preservation, intestine procurement research only | 2.81 | Based on $160 payment, 160/$55.16 per wRVU | Fee ticket |
| 47133 | Donor hepatectomy, including cold preservation, liver procurement | 79.22 | Based on $4,370 payment, 4370/$55.16 per wRVU | Fee ticket |
| 48550 | Donor pancreatectomy, including cold preservation, pancreas procurement (with or without duodenal segment) | 30.09 | Based on $1,660 payment, 1,660/$55.16 per wRVU | Fee ticket |
| 50300 | Donor nephrectomy, including cold preservation, kidney procurement (unilateral or bilateral) | 22.66 | Based on $1,250 payment, 1,250/$55.16 per wRVU | Fee ticket |
| S2900 | Robotic-assisted surgery | 30% of wRVU | Credit for additional time (average 2 hrs.) and complexity associated with robotic surgery | EMR |
| Mnemonic | ||||
| DRYRU | Surgeons travel for organ procurement but no organs recovered (dry-run) | 11.33 | Based on $625 payment, 625/$55.16 per wRVU | Fee ticket |
Abbreviation: CPT4: Current Procedural Terminology, 4th Edition.
RVUs assigned to the CPT codes to capture work effort.
Table 1d.
Sample calculation for a transplant surgeon’s customized relative value unit (cRVU), not included in a benchmark for salary or work RVUs per month.
| CPT4 Codes and Mnemonic |
Description of the Activity |
Sample Count* |
cRVU (per Count) | cRVU Total (Count * cRVU) |
|---|---|---|---|---|
| 32850 | Lung procurement | 6 | 32.00 | 192.00 |
| 33940 | Heart procurement | 6 | 22.00 | 132.00 |
| 47133 | Liver procurement | 6 | 79.22 | 475.32 |
| 48550 | Pancreas procurement | 6 | 30.09 | 180.54 |
| 50300 | Kidney procurement | 6 | 22.66 | 135.96 |
| S2900 | Robotic-assisted surgery | 6 | 30% of wRVU value | |
| DRYRU | Travel- Dry run | 6 | 11.33 | 67.98 |
Abbreviations: CPT4: Current Procedural Terminology, 4th Edition
The sample count is based on the average number for an academic physician/surgeon working in a mid-size program (50-100 transplants per year).
Table 1e.
Sample customized relative value units (cRVU) for non-face-to-face prolonged services to credit for patient complexity (the part not captured with work relative value units - wRVUs) during pre and post-transplant phase.*
| Mnemonic | Description of the Activity | Sample Count** |
cRVU (per Count) |
cRVU Total (Count * cRVU) |
|---|---|---|---|---|
| EVAL | Pre-transplant evaluations, waitlist management, and pre-transplant annual visits | 40 | 3.2 | 128 |
| POOLT or POKT | Post-transplant follow-up visits management | 100 | 1.6 | 160 |
These services include a chart review, following up on patients' test results, calling patients and meeting with their families, peer-to-peer review, literature search, pre-procedure preparation, pre-authorization, coordination of care, updating referring physicians, curbside consulting to peers and referring doctors and patient satisfaction.
The sample counts are based on monthly average numbers for an academic physician/surgeon working in a mid-size program (50-100 transplants per year).
The cRVUs are given mnemonics to match the billing mnemonics used by the provider billing system, in our case Epic (https://www.epic.com). These cRVU mnemonics and values are added to the billing system for capturing the RVU activity (both wRVU and cRVU) into one comprehensive report that can be reviewed quarterly. Implementing the cRVUs requires training of the physicians/surgeons and billers. Any activity that does not get automatically generated from the EMR or billing system requires the physician/surgeon to document the activity and the billers to enter it into the billing system like any patient charge. Mandatory documentation for cRVUs includes fee ticket, EMR/registration, provider-billing system, call schedule, satellite schedule, manuscript and publications titles, and revenue payments not attached to wRVUs. The physician/surgeon only needs to complete the fee ticket, with support staff obtaining the rest of the documentation. Tables 1a and 1c show a detailed definition and rationale of cRVUs assigned to the non-billable activities. Compensation for this cRVUs is based on the fair market value for median physician/surgeon salaries and CMS Medical/Surgical Director Reasonable Compensation Equivalent (RCE).6, 10
Creating OVUs:
CMS implemented the population health management models with Accountable Care Organizations (ACO’s) that share financial savings and financial risks. ACO’s contract with members, which includes transplant physicians/surgeons, to directly impact activities most important to quality in patients they serve. OVUs are created to provide a methodology to define performance improvement targets, established and updated annually, to engage the transplant physician and surgeon in the ACO’s shared savings or revenue enhancement activities while addressing meaningful outcomes outside the typical payer incentives (Figure 1 and Table 2). OVUs can be considered in two main categories: 1) Outcomes metrics: clinical effectiveness (patient/graft survival rates as expected or above the average, organ acceptance rate as expected or above the average, decreased blood product utilization, less in-patient dialysis use, Hepatitis C screening and treatment, cancer surveillance protocol adherence), safety (high-risk organ utilization rate, waitlist mortality rate, etc.), and patient satisfaction (such as Press Ganey surveys); 2) Costs metrics including throughput efficiency (decreased length of stay, adherence to care bundles >90%, and clinical pathways such as delayed graft function utilization of services management) (revenue enhancement), timely radiological procedures (cost avoidance), living donor robotic procedure costs (cost savings), operating room time (cost-saving), overall cost per unit of care (transplant hospitalization cost to global reimbursement ratio calculated for individual patients taking into consideration payer and patient complexity). The two results of improved outcomes and financial benefit are always tied together. Real practice examples are provided in Figure 1a and Table 2.
Figure 1a.
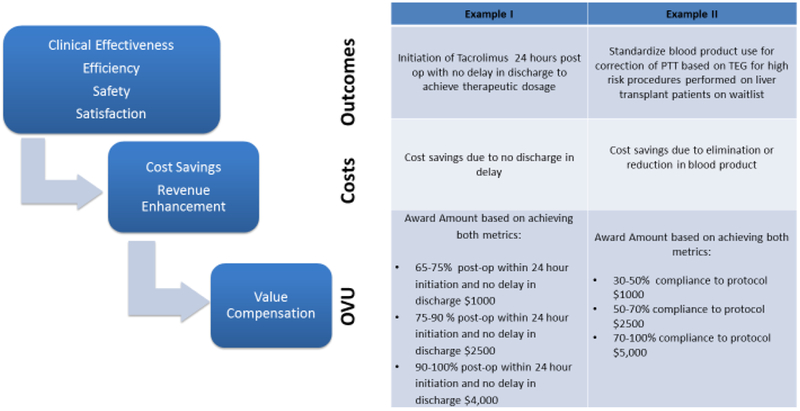
Example for an outcome value unit (OVU) construction.
Table 2.
Examples for Outcome-Value Units (OVUs) payments.
| Key Indicator Kidney/Liver Transplant Surgery (inpatient transplant surgery admission) |
Source | Award Amount Transplant Group |
|---|---|---|
| 1. Initiation of tacrolimus within 24 hours postoperative period with no delay in discharge to achieve tacrolimus therapeutic levels | Electronic Medical Record |
*65% 24-hour initiation of tacrolimus and no delay in discharge $1,000 or 27.78 OVU *75% 24-hour initiation of tacrolimus and no delay in discharge $2,500 or 69.45 OVU *≥90% 24-hour initiation of tacrolimus and no delay in discharge $4,000 or 111.11 OVU |
| Key Indicator Liver Transplant Patients Wait List Management |
Source | Award Amount Transplant Group |
| 1. Education of emergency room, catheter lab, and interventional radiology staff regarding new protocol for correcting platelet function and coagulation disorders based on thromboelastography (TEG) analysis for high-risk procedures | Sign-in sheet | *100% education to receive any award amount |
| 2. Standardize blood product use based on TEG for high-risk procedures performed on liver transplant patients on waitlist. | Electronic Medical Record |
*30% compliance to protocol $1,000 or 27.78 OVU *50% compliance to protocol $2,500 or 69.45 OVU *≥70% compliance to protocol $5,000 or 138.89 OVU |
One OVU generates $35.9996 based on the Medicare Physician Fee Schedule (MPFS).
These outcome/value changes, once implemented, are expected to be sustainable, but can recur as targets if critical to a transplant program’s success. OVU related compensation can be arbitrarily allocated among outcomes and cost-saving metrics ranging from 50/50 to 80/20 percentage ratio depending on transplant center preference. The OVUs can be kept separate for payment or, if implementing the pure RVU model, they may be added to the total RVUs that determine physician/surgeon compensation.
Incorporating cRVUs and OVUs into a Transplant Physician / Surgeon Compensation Model:
Our new compensation model (Table 3) is composed of four parts: 1) clinical productivity (wRVUs) generated by billing for providing patient care service and categorized in transplant service line analysis according to phases of the transplantation (see Tables 4 a and 4b for sample service line definitions for identifying how to capture all revenue associated with a service line); 2) non-billable work (cRVU, summarized in Tables 1a-e); 3) value-based work (OVUs) originating from achieving outcomes and cost-saving metrics; and 4) Medical and surgical directorship fee, hourly compensation per CMS Medical Director Reasonable Compensation Equivalent (RCE) and fair market value. Overall, total compensation generally encompasses wRVUs (50-55%), cRVUs (10-20%), OVUs (7-10%), and directorship fee (15-20%) if in a leadership role.
Table 3.
Sample* for a new annual compensation model for a transplant nephrologist:
| Compensation Components |
Sample Number of Units |
Compensation (% of total compensation) |
|
|---|---|---|---|
| Base salary* | $180,000 (49.2) | ||
| Clinical productivity (any wRVU billed above 3,500/year) | wRVUs** | 500 | $17,910 (4.9) |
| Non-billable work | cRVU*** | 1,200 | $67,200 (18.4) |
| Value based work | OVU** | 800 | $28,800 (7.9) |
| Medical directorship fee | Hourly compensation ($180/ hour) | 400 | $72,000 (19.7) |
| Total compensation | $365,910 (100) |
The sample counts are based on average numbers for an academic physician/surgeon working in a mid-size program (50-100 transplants per year).
One wRVU or OVU generates $35.9996 based on 2018 Medicare Physician Fee Schedule (MPFS) conversion factor.
One cRVU generates $56.0 based on fair market value.
Table 4a.
Kidney, simultaneous kidney-pancreas and kidney-liver service line analysis and their corresponding International Classification of Disease- 10th Revision-Clinical Modification (ICD-10-CM) codes.
| DEFINITIONS | |
|---|---|
| Phase and Codes | Data Location |
| Pre-transplant/Evaluation Services | |
| Kidney transplant acquisition salaries, benefits, medical director fees, operating costs | Cost Center (CC) Organ Acquisition Center (OAC) |
| Pancreas transplant acquisition salaries, benefits, medical director fees, operating costs | CC OAC |
| Exclude organ costs | Organ costs are pulled out of CC's and added to inpatient case costs |
| Pre-Transplant evaluation/Waitlist management - Outpatient revenue and direct and indirect expenses | Patient accounts |
| The fiscal year (FY) Evaluated patient list and waitlist patient names from Transplant EMR (EPIC Phoenix). All testing is done for FY | |
| Living Donor workup revenue and direct and indirect expenses | Z00.5 and FY patient names from Transplant electronic medical record (EMR) |
| Pre-Transplant Human Leukocyte Antigen (HLA) lab revenue and direct expenses | FY Evaluated patient list and waitlist patient names from Transplant EMR. All testing is done for FY |
| HLA outside revenue and direct expenses | CC Revenue |
| Total Pre-transplant | |
| Inpatient Phase (transplant event) | |
| Deceased Donor Kidney Transplant episode (hospital transplant event) | MS-DRG: 652 Kidney |
| Living Donor Kidney Transplant episode (hospital transplant event) | MS-DRG: 652 Kidney |
| Kidney-Pancreas Deceased Donor Transplant episode (hospital transplant event) | MS-DRG: 008 SPK (simultaneous kidney-pancreas), 010 Pancreas alone |
| Living Donor nephrectomy | Expenses under donor/recipient name. |
| Simultaneous Kidney/Liver (L/K) Transplant episode (hospital transplant event) | MS-DRG: 005 Liver transplant with major complicating co-morbidities (MCC). Medicare only recognizes the liver but pays for both organs in OAC |
| Transplant Patient List from Transplant EMR | |
| Inpatient Revenue | Patient accounts |
| Medicare Reimbursement | Obtain revenue from Cost Report Department |
| Organ Costs | Pull out organ costs from Transplant Department CCs |
| Inpatient Care Direct Expenses | Exclude entire organ acquisition charge on all recipient patient accounts as all expenses in organ costs or in transplant cost centers |
| Indirect Expenses | Formula provided by finance/expense allocation |
| Total Inpatient Phase (transplant event) | |
| Post-Transplant | |
| Outpatient Post Transplant Follow up Revenue and Direct and Indirect expenses | Patient Accounts |
| FY Post transplant patient list from Transplant EMR | |
| Diagnosis codes | |
| T86.10 | Unspecified complication of kidney transplant |
| T86.11 | Kidney transplant rejection |
| T86.12 | Kidney transplant failure |
| T86.13 | Kidney transplant infection |
| T86.19 | Other complications of Kidney transplant |
| Z49.83 | Pancreas transplant status |
| Z94.0 | Kidney transplant status |
| Z52.4 | Kidney donor status |
| Inpatient Post Transplant Readmissions Revenue and direct and indirect expenses | Patient Accounts |
| FY Post-transplant readmission patient list from Transplant EMR | |
| T86.11 | Kidney transplant rejection |
| T86.12 | Kidney transplant failure |
| T86.13 | Kidney transplant infection |
| T86.19 | Other complications of Kidney transplant |
| T86.899 | Complications pancreas transplant |
| FY Post-transplant readmission patient list from Transplant EMR | |
| Z49.83 | Pancreas transplant status |
| Z94.0 | Kidney transplant status |
| Z52.4 | Kidney donor status |
| Total Post Transplant | |
| Transplant Surgeon non Transplant Cases | |
| Inpatient and outpatient non transplant surgical cases revenue and direct and indirect expenses | Patient Accounts |
| Surgeon IDs or names | |
| Total Transplant Surgeon non Transplant Cases | |
| Non-Acquisition Expenses | |
| All direct expenses hitting this cost center including physician practice subsidy expenses for transplant work and global contracting distribution gain/loss | Transplant non-acquisition CCs capture marketing and physician subsidy expenses. Subsidy expense written off monthly to CCs includes contracting gain/loss |
| Total Non-Acquisition Expenses | |
| Total Kidney Transplant Service Line | |
Abbreviations: OAC= Organ Acquisition Cost Center; ICD-10-CM= International Classification of Disease- 10th Revision-Clinical Modification; CC = Cost center; FY = Fiscal year; K/L = Kidney / Liver; MS-DRG= Medicare Severity Diagnosis Related Group; HLA= Human Leukocyte Antigen; MCC = Major complicating co-morbidities.
Table 4b.
Liver transplant service line analysis and their corresponding International Classification of Disease- 10th Revision-Clinical Modification (ICD-10-CM) codes.
| DEFINITIONS | |
|---|---|
| Phase and Codes | Data Location |
| Pre-Transplant/Evaluation Services | |
| Liver Transplant Acquisition Salaries, benefits, Medical Director fees, operating costs | Cost Center (CC) Organ Acquisition Center (OAC) |
| Exclude organ costs | Organ costs are pulled out of OAC CC and added to inpatient care costs |
| Pre-Transplant Evaluation/Waitlist Management - Inpatient and Outpatient Revenue and direct and indirect expenses | Patient Accounts |
| Fiscal Year (FY) Evaluated patients list and waitlist patient names from Transplant Department electronic medical record (EMR) | |
| All inpatients admitted by transplant hepatologists revenue and direct and indirect expenses | Patient Accounts/ |
| Hepatologist IDs or names | |
| Inpatient and Outpatient Hepatology list provided by the Transplant Department | |
| Diagnosis codes | |
| Exclude Surgeons and transplant cases | |
| Pre-Transplant Management IP/OP (Hospitalists) | Inpatient and Outpatient Hepatology list provided by the Transplant Department |
| All inpatients referred for admission and clinically managed by hepatologists but admitted by Hospitalists/internists | Diagnosis codes |
| Exclude Surgeons and transplant cases | |
| Total Pre-Transplant/Evaluation Services | |
| Inpatient Phase Transplant Event | |
| Liver Transplant episode (hospital transplant event) | Medicare Severity Diagnosis Related Group (MS-DRG) 05 Liver Transplant with major complicating co-morbidities (MCC) and DRG 06 Liver transplant without MCC. |
| Transplant Patient List from Transplant EMR (EPIC Phoenix) | |
| Inpatient Revenue | Patient Accounts |
| Medicare Reimbursement | Obtain revenue from Cost Report department |
| Organ costs | Pull out organ costs from transplant dept CC or where organ costs are paid |
| Inpatient Care Direct Expenses | Exclude entire organ acquisition charge on all recipient patient accounts as all expenses in organ costs or transplant department CC |
| Indirect Expenses | Formula provided by finance/expense allocation |
| Inpatient Phase Kidney Liver Transplant Event | |
| Liver Transplant episode (hospital transplant event) | MS-DRG 05 Liver Transplant with MCC and DRG 06 Liver transplant without MCC. |
| Kidney Liver transplant episode | MS-DRG 05 Liver Transplant with MCC |
| Transplant Patient List from transplant department EMR (EPIC Phoenix) | |
| Inpatient Revenue | Patient Accounts |
| Medicare Reimbursement | Obtain revenue from Cost Report department |
| Organ costs | Pull out organ costs from transplant department CC or where organ costs are paid |
| Inpatient Care Direct Expenses | Exclude entire organ acquisition charge on all recipient patient accounts as all expenses in organ costs or transplant department CC |
| Indirect Expenses | The formula provided by finance/expense allocation |
| Total Inpatient Phase/Transplant Event | |
| Post-Transplant | |
| Post-Transplant Outpatient Revenue and direct and indirect expenses | Patient Accounts |
| Post-Transplant Inpatient Revenue and direct and indirect expenses | Patient Accounts |
| FY Post transplant patient list from transplant dept. EMR | |
| Diagnosis codes | |
| T86.40 | Unspecified complication of liver transplant |
| T86.41 | Liver transplant rejection |
| T86.42 | Liver transplant failure |
| T86.43 | Liver transplant infection |
| T86.49 | Other complications of liver transplant |
| Z09, Z48.298, Z48.23, Z94.4 | Post liver Fu |
| Z94.4 | Liver transplant status |
| Total Post Transplant | |
| Downstream Liver Disease or Liver Transplant Management. Out or Inpatient and outpatient primary surgeon cases | |
| Other system hospitals and facilities outpatient revenue and direct and indirect expenses | Patient Accounts |
| Outpatient Hepatology list provided by Transplant Department | |
| Diagnosis codes | |
| Include Surgeons and transplant cases | |
| Other system hospitals inpatient and outpatient surgical cases performed by Transplant Surgeons | Surgeon IDS assigned by the hospital or by name |
| Total Downstream | |
| Transplant Surgeon non-Transplant Cases | |
| Inpatient and Outpatient non transplant surgical cases revenue and direct and indirect expenses | Patient Accounts |
| Surgeon IDS assigned by the hospital or by name | |
| Exclude liver transplant inpatient and outpatient cases | |
| Total Downstream | |
| Liver Program Administration | |
| All expenses are hitting transplant department CCs, including physician practice expenses. Global Contracting gain/loss distribution is also included | CC marketing and Transplant Physician Practice subsidy expenses. Expense is written off monthly to CC. consists of the Global contracting gain/loss revenue |
| Total Liver Program Administration | |
| Outpatient/Specialty Pharmacy Revenue | |
| Medication Therapy Management Clinic Revenue and Direct Expenses related to Hepatitis C other Liver Disease Management Patients and Transplant Medications | CCs |
| Salary and Drug Direct Expenses related to transplant hospital management referrals | Transplant Surgeons, Transplant Hepatologists and Transplant ID ordering physicians |
| Total Outpatient/Specialty Pharmacy Revenue | |
| Total Liver Transplant Service Line | |
Abbreviations: OAC= Organ Acquisition Cost Center; ICD-10-CM= International Classification of Disease- 10th Revision-Clinical Modification; CC = Cost center; FY = Fiscal year; K/L = Kidney / Liver; MS-DRG= Medicare Severity Diagnosis Related Group; HLA= Human Leukocyte Antigen; MCC = Major complicating co-morbidities.
Funding for the proposed compensation model (transplant physicians/surgeons’ non-billable and value-based work) can originate from a shared revenue pool/group withhold (there can be many variations of how these are implemented ranging from the use of seed grants to settlement at the end of current year or next year), service line shared revenue when the health system owns all ancillaries, value-added/cost elimination, revenue enhancement, quality payment sharing, and mission-driven endowments. Specific funding considerations include (1) As organizations embrace value-based care models, there will be more opportunities to fund payment adjustments according to cRVU and OVU. For example, the expected success of the ACO model and cost savings brought by it can be a catalyst for the rearrangement of physician/surgeon compensation for a variety of specialties, including transplant.11 In an ACO setting, reductions in costs (as a result of related OVU incentives) can generate revenue to the ACO for shared savings between the center/hospital and physicians/surgeons under the ACO Medicare Shared Savings Program’s leniency of Stark restrictions. (2) Improvements in transplant outcomes/quality can lead to more referrals, a higher volume, and better contract terms with payers, in the long run, generating additional revenue; (3) Specific contractual agreements with private payers (e.g., under global contracts) to support alternative funding, applied already with some success.12-14 (4) Finally, transplant is among the few areas within a hospital that continues to receive cost-based reimbursement concerning the ratio of acquisition of organs for transplant to Medicare beneficiaries.15 Therefore, hospitals already receive compensation for some, but not all, of the activities we list in our tables as part of cRVU (e.g., pre-transplant patient evaluation). Such payments to hospitals may further facilitate the implementation of customized RVUs, particularly for specific measures that are captured by Medicare cost reports.
The proposed systematic framework in this manuscript is a possible first step for transplant centers in accounting for non-billable work and promoting value, though partly implemented in other forms. Many centers have adopted different methods for calculating non-billable time. Our proposed system has advantages as it uses mnemonics entered into the billing system or uses already created existing CPT codes to capture all the data in one place, which is the billing system. It minimizes the need for additional documentation as it uses data already being captured for most work and is objective. It is not developed for replacing but instead developed for enhancing a system already in place. The concepts can be adapted to fit any institution where gaps may exist in capturing time.
Our newly introduced RVU metrics constitute a balanced approach by capturing the teamwork implicit in transplantation while also recognizing individual productivity.2 Transplant centers can further customize the proposed cRVU or OVU metrics in parallel to their mission/vision and they can reweigh each aspect to fit different priorities. When implementing our framework, a transplant center using salary with bonuses can set expectations (i.e., a cap based on RVU metrics) and provide extra compensation to physicians/surgeons beyond those expectations or based on OVU (see Table 3).16 The highly dynamic nature of transplant and changing payment landscape may require changes in how wRVU, cRVU, and OVU is weighed in the overall physician/surgeon compensation and how it is modified over time. Moreover, adjustments can be made to meet the needs of individual institutions, academic or otherwise.
As noted earlier, the adoption of new RVU metrics will require additional reporting. Expert panels using a transparent process while administrators can randomly audit can assign RVU values. Some of the activities represented by cRVUs are already traced. In particular, organ offers can be tracked down through the UNet/DonorNet (powered with advanced data analytics) and the increased use of electronic health records (specifically for organs accepted for a patient) that could automatically capture needed information. Time studies for physicians/surgeons may also be of benefit and could potentially be utilized to lessen the reporting burden.
Physician compensation is a topic of high importance because it determines the ability of each center to retain talent and recruit new team members. From the surgical perspective, there is a great amount of non-billable work that is not compensated in a fee-for-service model. In this manuscript, we present a formula that allows physicians to document most of the non-billable work. Creating these categories and making compensation not dependent on wRVUs only would positively affect physician satisfaction and overall morale. For example, if a physician is out in the community marketing the transplant program, they can document this time as work and be compensated for their time. Another aspect is the ability to expand the transplant program services for cutting edge technologies that can enhance its marketability. In the surgeon’s case, the adoption of robotic donor nephrectomies, for example, is a way of creating value to the program but requires additional training and processes that are not captured by the wRVUs.
In conclusion, transplantation can be a leader in further developing value-based population management payment structures. Utilizing currently available data and norms, it is possible to augment wRVUs with additional metrics of non-clinical work of critical importance to patients and providers alike. Our proposed new transplant physician and surgeon compensation model can 1) provide a detailed and auditable record of non-billable work; 2) align incentives and goals for physician/surgeon and transplant center; 3) increase physician/surgeon satisfaction; and, ultimately 4) prioritize quality, not just quantity.
Acknowledgments
Funding:
This research is partly supported by the University of Texas Southwestern George O’Brien Kidney Research Core Center grant NIH P30DK079328.
Abbreviations:
- ACA
Affordable Care Act
- ACO
Accountable Care Organization
- CMS
Centers for Medicare and Medicaid Services
- EHR
Electronic Health Records
- FMV
Fair market value
- RCE
Reasonable compensation equivalent
- RVU
Relative value unit
- cRVU
Customized relative value unit
- OVU
Outcome value unit
- wRVU
Work relative value unit
Footnotes
Disclosure:
The authors of this manuscript have no conflicts of interest to disclose as described by the American Journal of Transplantation.
References:
- 1.Stecker EC, Schroeder SA. Adding value to relative-value units. N Engl J Med 2013;369:2176–9. [DOI] [PubMed] [Google Scholar]
- 2.Abecassis M, Pearson T. Fee-for-value and wRVU-based physician productivity-an emerging paradox. Am J Transplant 2015;15:579–80. [DOI] [PubMed] [Google Scholar]
- 3.Axelrod DA, Millman D, Abecassis MM. US Health Care Reform and Transplantation. Part I: overview and impact on access and reimbursement in the private sector. Am J Transplant 2010;10:2197–2202. [DOI] [PubMed] [Google Scholar]
- 4.Axelrod DA, Millman D, Abecassis MM. US Health Care Reform and Transplantation, Part II: impact on the public sector and novel health care delivery systems. Am J Transplant 2010;10:2203–7. [DOI] [PubMed] [Google Scholar]
- 5.Florence LS, Feng S, Foster CE 3rd, et al. Academic careers and lifestyle characteristics of 171 transplant surgeons in the ASTS. Am J Transplant 2011;11:261–71. [DOI] [PubMed] [Google Scholar]
- 6.Abouljoud M, Whitehouse S, Langnas A, et al. Compensating the transplant professional: time for a model change. Am J Transplant 2015;15:601–5. [DOI] [PubMed] [Google Scholar]
- 7.Regan L, Jung J, Kelen GD. Educational Value Units: A Mission-Based Approach to Assigning and Monitoring Faculty Teaching Activities in an Academic Medical Department. Acad Med 2016;91:1642–1646. [DOI] [PubMed] [Google Scholar]
- 8.Clyburn EB, Wood C, Moran W, et al. Valuing the education mission: implementing an educational value units system. Am J Med 2011;124:567–72. [DOI] [PubMed] [Google Scholar]
- 9.Mezrich R, Nagy PG. The academic RVU: a system for measuring academic productivity. J Am Coll Radiol 2007;4:471–8. [DOI] [PubMed] [Google Scholar]
- 10.Federal Register, Volume 79, Issue 163 (August 22, 2014). CMS Medical Director Reasonable Compensation Equivalent. https://www.govinfo.gov/content/pkg/FR-2014-08-22/html/2014-18545.htm accessed on December 25, 2018. [Google Scholar]
- 11.McWilliams JM, Hatfield LA, Landon BE, et al. Medicare Spending after 3 Years of the Medicare Shared Savings Program. N Engl J Med 2018;379:1139–1149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Song Z, Rose S, Safran DG, et al. Changes in health care spending and quality four years into global payment. N Engl J Med 2014;371:1704–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Adida E, Mamani H, Nassiri S. Bundled Payment vs. Fee-for-Service: Impact of Payment Scheme on Performance. Management Science 2017;63:1606–1624. [Google Scholar]
- 14.Ayvaci M CH, Kim Y, Raghunathan S. Payment mechanisms, incentives for adoption and value of health-information exchanges (HIE). Available at https://ssrn.com/abstract=2978862. SSRN Electronic Journal 2019:1–48.
- 15.Abecassis M. Organ acquisition cost centers Part I: medicare regulations--truth or consequence. Am J Transplant 2006;6:2830–5. [DOI] [PubMed] [Google Scholar]
- 16.Christianson JB ZD, White KM, Zeglin J. . Exploring alternative approaches to valuing physician services. A report from the University of Minnesota, Division of Health Policy and Management for the Medicare Payment Advisory Commission Volume 11-1, 2011:1–54. [Google Scholar]


