Abstract
Objective
To examine the prevalence of youth meeting the 24-hour healthy movement guidelines [i.e., ≥60-min of moderate-to-vigorous physical activity (MVPA), ≤2-hours of screen-time, age-appropriate sleep duration], and which combination of meeting these guidelines was most associated with bodyweight status, in a nationally representative US sample.
Study design
Cross-sectional data from the 2016-2017 National Survey of Children’s Health were used. A multinomial regression model of body weight status was generated (underweight, overweight, obese, versus healthy weight) and then stratified by sex. Analyses were adjusted for potential confounders.
Results
The sample (n=30,478) was 50.4% female, 52.4% white, and mean age was 13.85 years (SD=2.28); 15% percent were obese, and 15.2% were overweight. Overall, 9.4% met all three of the 24-hour healthy movement guidelines, 43.6% met two, 37.9% met one, and 9.1% met none. Meeting zero guidelines (vs. 3) was associated with the greatest likelihood of overweight (aOR=1.85, 95% CI=1.31-2.61), and obesity (aOR=4.25, 95% CI=2.87-6.31). Females (aOR=4.97, 95% CI=2.59-9.53) had higher odds of obesity than males (aOR=3.99, 95% CI=2.49-6.40) when zero (vs 3) guidelines were met. Meeting the MVPA guideline, either alone or in combination with screen-time or sleep duration (versus all 3), was associated with the lowest odds for overweight and obesity in the full sample.
Conclusion
Meeting all movement guidelines was associated with the lowest risk for obesity, particularly in females. Meeting the MVPA guideline may be a priority to prevent overweight and obesity in youth.
Keywords: 24-hour healthy movement, screen-time, sleep, physical activity
Sedentary behavior, physical activity, and sleep duration are co-dependent behaviors that fall on a movement/non-movement continuum, and together account for the 24-hour daily cycle.(1) Recommendations for healthy 24-hour time use posit that children (age 6-12 years) sleep 9 to 12 hours and adolescents (age 14-18 years) sleep 8 to 10 hours a night, and that both groups accumulate at least one hour of moderate to vigorous intensity physical activity and limit screen-time (ie, leisure time screen use) to 2 hours within a 24-hour period.(1, 2) The consideration of movement behaviors across the 24-hour period represents a more integrated behavioral paradigm, and a departure from traditional models that considered health risk behaviors as independent entities to be intervened upon singularly. Central to the integrated 24-hour movement paradigm is the concept that meeting recommendations for all three movement behaviors may have a greater association with beneficial health outcomes than meeting a single guideline.
Emerging data show that between 2-17% of youth,(3-9) and a greater proportion of male versus female, and younger (i.e., 5-11 years old) versus older (i.e., 12-17 years old) youth, meet all three healthy 24-hour time-use guidelines.(4) Meeting all (versus 0-2) guidelines has been associated with significantly better cardiometabolic indicators (e.g., lower BMI z-score, more favorable waist circumference, higher aerobic fitness), (3, 10, 11) as well as superior global cognition.(8) A curvilinear relationship has also been reported between healthy 24-hour time-use guidelines and obesity whereby meeting the physical activity guideline disproportionately reduced the odds of obesity as compared with the other guidelines.(7) Research has begun to extend the 24-hour movement framework to American youth, demonstrating only 5% of youth concurrently met the three guidelines.(5) To address some of these knowledge gaps, it is the purpose of this study to examine which combination of these guidelines may be most strongly associated with cardiometabolic outcomes such as overweight and obesity in male and female youth residing in the United States. Answers to these questions could inform more efficient, targeted interventions based on the healthy 24-hour framework to curb the obesity epidemic.
Methods
This cross-sectional study utilized nationally representative, de-identified data from the 2016-2017 National Survey of Children’s Health (NSCH) combined dataset. The NSCH is jointly sponsored by the National Center for Health Statistics at the Centers for Disease Control and Prevention and the Maternal and Child Health Bureau (both US). The 2016-2017 NSCH includes a probability sample of non-institutionalized youth aged 0 to 17 years in the United States (N=71,811). In 2016, the survey was updated and conducted either online or by mail (paper) based instruments by the US Census Bureau. Households were randomly contacted to identify households with children younger than the age of 18 years. If a household had more than one child, one was randomly selected, and parents/guardians completed the questionnaire. Parent, proxy reporting has shown validity for the assessment of constructs such as youth health related quality of life and physical activity by some (12) (13), but not all (14) reports. The weighted survey response rate was 40.7% and 37.4% for the 2016 and 2017 data collections, respectively. Further information about the 2016-2017 NSCH combined dataset can be found in the US Census Bureau’s fast facts document.(15) The National Center for Health Statistics Research Ethics Review Board and the National Opinion Research Center Institutional Review Board (both US) approved all the study procedures. Informed consent was collected from all parents or guardians.
Physical activity was assessed using one question: “During the past week, on how many days did this child exercise, play a sport, or participate in physical activity for at least 60 minutes?” Response options were “0 days”, “1-3 days”, “4-6 days”, and “every day.” A dichotomous variable was created where responses of “every day” were coded as “meeting physical activity guidelines,” and all other responses were coded as “not meeting physical activity guidelines.”(16)
Screen-time was assessed using one question: “On an average weekday, about how much time does this child usually spend in front of a TV watching TV programs, videos, or playing video games?” Responses were: “none”, “1 hour”, “2 hours”, “3 hours”, and “4 or more hours”. A dichotomous variable was created where responses of “none”, “1 hour” and “2 hours” were collapsed into “2 or less hours”, and all other responses were categorized as “more than 2 hours”, in alignment with 24-hour movement guidelines.(1, 17)
To assess sleep, parents were asked “During the past week, how many hours of sleep did this child get on an average weeknight?”. Potential responses included “less than 6 hours,” “6 hours,” “7 hours,” “8 hours,” “9 hours,” “10 hours,” and “11 or more hours.” Consistent with the National Sleep Foundation guidelines for healthy sleep duration, responses of 8, 9, or 10 hours for 14-17 years old, and 9 hours or more for 10-13 years old youth were coded as “meeting sleep guidelines” and all other responses were coded as “not meeting sleep guidelines.”(2)
In the NSCH, body mass index (BMI) is calculated based on parent-reported height and weight. Centers for Disease Control and Prevention (CDC) sex-specific BMI-for-age categories are provided in the NSCH data set, including: (a) underweight as less than 5th percentile, (b) normal weight as 5th percentile to less than 85th percentile, (c) overweight as 85th to <95th percentile, and (d) obese as greater or equal to 95th percentile.(18)
Adolescents’ ethnicity, sex, household income level, and parental education were included as covariates for this analysis, as they are potentially related to engagement in health behaviors(19, 20) and body weight.(20) Household income was represented by four categories of percent of federal poverty level (FPL) based on the Department of Health and Human Services guidelines; 0%-199% FPL, 200%-299% FPL, 300%-399% FPL, and 400% FPL or greater.(10) Parental education was recorded as the highest degree or year of school completed by the parent.
Statistical analyses
Youth (n = 33,245) without disabilities and aged between 10 and 17 years old were selected from the combined NSCH 2016-2017 dataset. Cases with missing or invalid question responses (n=2,767) were listwise removed; the final sample included 30,478 cases with complete responses. Using the data analysis plan from NSCH, data were analyzed in two steps. First, a frequency table and 95% confidence interval (CI) was created to present participant demographics, body weight status, and number of 24-hour movement guidelines met (0-3). Next, to estimate the odds of being overweight, or obese as a function of meeting each possible configuration of the guidelines, a multinomial logistic regression model of body weight status was generated (underweight, overweight, obese, versus healthy weight) for the complete sample and then stratified by sex. Within each bodyweight status model, “Meeting all three guidelines” was used as the reference category. Analyses were adjusted for participants’ ethnicity, sex, household income levels, and parental education. To account for the sampling plan of NSCH, the data analyses were conducted using the Complex Samples module of SPSS (Ver. 25, IBM; Armonk, NY). Results were considered statistically significant at the .05 level.
Results
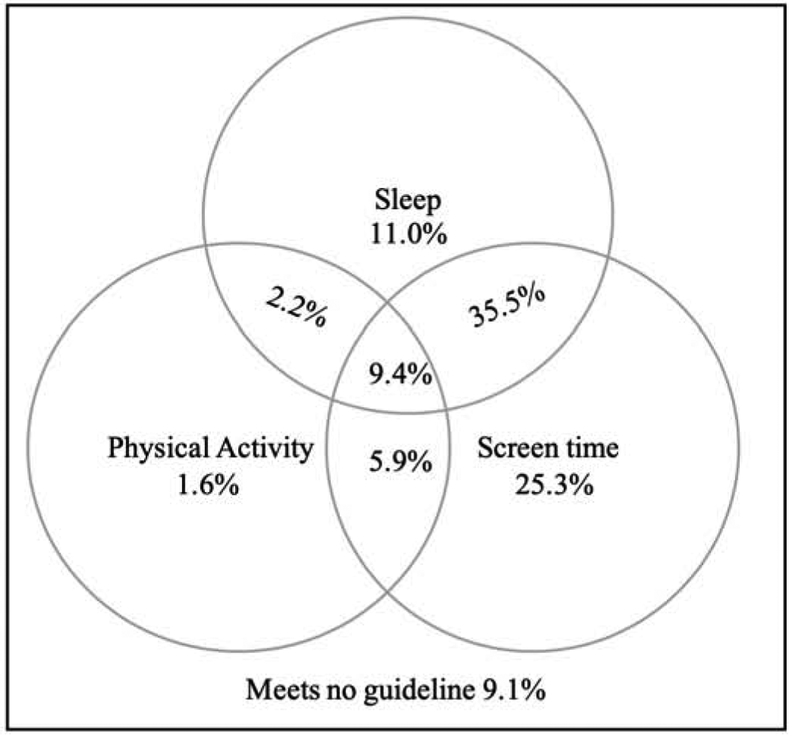
Of the analytic sample (n=30,478), the mean age was 13.85 years (SD=2.28) and 50.4% [95% CI=49.3-51.8] were female. Over one-half of the sample was white (52.4%; 95% CI=51.1-53.8), and 38.9% [95% CI=37.5-40.4%] were at 0-199% of the FPL. Fifteen percent of the sample were obese [95% CI=13.9-16.2], and a further 15.2% [95% CI= 14.2-16.3] were overweight. A large proportion of youth did not meet the physical activity (80.9%, 95% CI= 79.8-82.0), but met screen-time (76.2%, 95% CI=75.0-77.4) and sleep (58.1%, 95% CI=56.7-59.4) guidelines. Overall, 9.4% [95% CI= 8.7-10.2] of the sample met all three of the 24-hour healthy movement guidelines, 43.6% [95% CI= 42.3-45.0] met two, 37.9% [95% CI= 36.6-39.2] met one, and 9.1% [95% CI= 8.3-9.9] met none (Figure and Table 1). A multinomial regression model of the bodyweight status outcome was run, with the categories of underweight, overweight, and obese compared with healthy weight. Each possible combination of the 24-hour healthy movement guidelines was used as the independent variables of interest; meeting all three of the 24-hour movement guidelines provided the comparison within each model (Table 2). Due to low prevalence of underweight, the results focused on overweight, and obese compared with healthy weight status.
Figure.
Percentage of Youth (10-17 Years) Meeting 24-Hour Movement Guidelines (N = 30,478)
Table 1.
Demographic Characteristics of Youth from 2016-2017 National Survey of Children’s Health
| Age range | 10-17 years old N=30,478 |
Female n=15,524 |
Male n=14,954 |
|---|---|---|---|
| Age (y), mean (SD) | 13.85 (2.28) | 13.86 (2.29) | 13.84 (2.28) |
| Birth Sex (%, 95%CI) | |||
| Male | 49.6% (48.2-50.9%) | — | — |
| Female | 50.4% (49.3-51.8%) | — | — |
| Ethnicity (%, 95%CI) | |||
| Asian | 4.6% (4.1-5.1%) | 5.0% (4.3-5.8%) | 4.2% (3.6-5.0%) |
| Black | 13.1% (12.1-14.2%) | 13.1% (11.7-14.8%) | 12.9% (11.5-14.4%) |
| Hispanic | 24.5% (23.1-26.0%) | 23.7% (21.7-25.8%) | 25.1% (23.0-27.4%) |
| White, non-Hispanic | 52.4% (51.1-53.8%) | 52.4% (50.5-54.3%) | 52.8% (50.8-54.8%) |
| Others/multiracial, non-Hispanic | 5.4% (4.9-5.8%) | 5.8% (5.2-6.6%) | 5.0% (4.4-5.6%) |
| Household poverty level based on CHIP | |||
| 0-199% FPL | 38.9% (37.5-40.4%) | 39.5% (37.5-41.5%) | 37.9% (35.9-40.0%) |
| 200-299% FPL | 15.2% (14.3-16.2%) | 14.9% (13.7-16.3%) | 15.6% (14.1-17.1%) |
| 300-399% FPL | 12.5% (11.7-13.4%) | 12.1% (11.1-13.0%) | 13.1% (11.8-14.6%) |
| 400% FPL or greater | 33.3% (32.2-34.4%) | 33.5% (32.0-35.1%) | 33.4% (31.8-35.0%) |
| Weight status (%, 95%CI) | |||
| Underweight | 6.0% (5.5-6.6%) | 5.2% (4.5-5.9%) | 6.8% (6.0-7.8%) |
| Healthy weight | 63.8% (62.4-65.1%) | 66.2% (64.3-68.1%) | 61.2% (59.2-63.2%) |
| Overweight | 15.2% (14.2-16.3%) | 15.8% (14.3-17.4%) | 14.8% (13.4-16.2%) |
| Obese | 15.0% (13.9%-16.2%) | 12.9% (11.5-14.3%) | 17.2% (15.5-19.0%) |
| Physical activity participation (%, 95%CI) | |||
| Less than 60 min/day | 80.9% (79.8-82.0%) | 85.4% (84.0-86.7%) | 76.4% (74.6-78.0%) |
| 60 min or more/day | 19.1% (18.0-20.2%) | 14.6% (13.3-16.0%) | 23.6% (22.0-25.4%) |
| Average weeknight sleep (%, 95%CI) | |||
| Below age-appropriate hours | 41.9% (40.6-43.3%) | 42.7% (40.8-44.6%) | 41.0% (39.0-43.0%) |
| Meet age-appropriate hours | 58.1% (56.7-59.4%) | 57.3% (55.4-59.2%) | 59.0% (57.0-61.0%) |
| Weekday screen-time viewing (%, 95%CI) | |||
| 2 hours or less/day | 76.2% (75.0-77.4%) | 80.4% (78.7-81.9%) | 72.2% (70.4-73.9%) |
| More than 2 hours/day | 23.8% (22.6-25.0%) | 19.6% (18.1-21.3%) | 27.8% (26.1-29.6%) |
| 24-hour movement guideline (%, 95%CI) | |||
| Meet 0 guidelines | 9.1% (8.3-9.9%) | 8.2% (7.1-9.4%) | 10.0% (9.0-11.0%) |
| Meet 1 guideline | 37.9% (36.6-39.2%) | 38.7% (36.9-40.6%) | 36.8% (34.8-38.8%) |
| Meet 2 guidelines | 43.6% (42.3-45.0%) | 45.7% (43.9-47.6%) | 41.7% (39.8-43.7%) |
| Meet 3 guidelines | 9.4% (8.7-10.2%) | 7.4% (6.5-8.4%) | 11.5% (10.5-12.7%) |
CI: confidence interval; SD: standard deviation; CHIP: Children’s Health Insurance Program; FPL: Federal Poverty Level
Table 2.
Adjusted Odds Ratio Estimates Weight Status from 2016-2017 National Survey of Children’s Health
| Adjusted Odds Ratio (95% CI) | |||
|---|---|---|---|
| Body weight statusa | 10-17 years old (N=30,478)b | Female (n=15,524)c | Male (n=14,954)c |
| Overweight [vs. Healthy Weight] | n=4,283 | n=2,169 | n=2,114 |
| Meets none of the guidelines | 1.85 (1.31 - 2.61) ** | 1.62 (0.93 - 2.81) | 2.00 (1.31 - 3.07) ** |
| Meets screen time guideline alone | 1.39 (1.02 - 1.89) * | 1.16 (0.71 - 1.88) | 1.60 (1.10 - 2.34) * |
| Meets sleep guideline alone | 1.51 (1.07 - 2.14) * | 1.40 (0.79 - 2.47) | 1.56 (1.04 - 2.34) * |
| Meets screen time, sleep guidelines | 1.38 (1.02 - 1.86) * | 1.22 (0.75 - 1.98) | 1.46 (1.03 - 2.08) * |
| Meets physical activity guideline alone | 0.81 (0.41 - 1.60) | 0.29 (0.10 - 0.85) * | 1.28 (0.57 - 2.87) |
| Meets physical activity, screen time guidelines | 0.91 (0.61 - 1.37) | 0.64 (0.34 - 1.22) | 1.17 (0.70 - 1.94) |
| Meets physical activity, sleep guidelines | 1.48 (0.60 - 3.70) | 1.11 (0.50 - 2.48) | 1.78 (0.58 - 5.47) |
| Meets all three guidelines | 1 (referent) | 1 (referent) | 1 (referent) |
| Obese [vs. Healthy Weight] | n=3,663 | n=2,143 | n=1,520 |
| Meets none of the guidelines | 4.25 (2.87 - 6.31) ** | 4.97 (2.59 - 9.53) ** | 3.99 (2.49 - 6.40) ** |
| Meets screen time guideline alone | 2.07 (1.43 - 3.02) ** | 2.22 (1.28 - 3.84) ** | 2.10 (1.27 - 3.48) ** |
| Meets sleep guideline alone | 2.57 (1.71 - 3.86) ** | 3.39 (1.84 - 6.23) ** | 2.17 (1.28 - 3.67) ** |
| Meets screen time, sleep guidelines | 1.85 (1.30 - 2.64) ** | 2.11 (1.22 - 3.65) ** | 1.76 (1.12 - 2.76) * |
| Meets physical activity guideline alone | 1.35 (0.59 - 3.13) | 2.64 (0.70 - 9.90) | 0.90 (0.36 - 2.25) |
| Meets physical activity, screen time guidelines | 1.35 (0.82 - 2.22) | 1.56 (0.69 - 3.52) | 1.27 (0.68 - 2.36) |
| Meets physical activity, sleep guidelines | 1.47 (0.58 - 3.74) | 0.63 (0.23 - 1.68) | 1.56 (0.57 - 4.30) |
| Meets all three guidelines | 1 (referent) | 1 (referent) | 1 (referent) |
“Healthy weight” is used as a reference category for the multinomial logistic regression analysis.
Model adjusted for parental education, household poverty level, ethnicity and sex.
Model adjusted for parental education, household poverty level, and ethnicity.
p < 0.05,
p < 0.01.
In the multinomial model of overweight status, compared with youth who met all three 24-hour movement guidelines, the odds of overweight was significantly higher among youth who met no guideline (aOR = 1.85, 95% CI: 1.31-1.89), met the screen-time guideline alone (aOR = 1.39, 95% CI: 1.02-1.89), met the sleep guideline alone (aOR = 1.51, 95%CI: 1.07-2.14), or met the screen-time and sleep guidelines concurrently (aOR = 1.38, 95%CI: 1.02-1.86). Among male youth, meeting no guideline (aOR = 1.85, 95% CI: 1.31-1.89), the sleep guideline alone (aOR = 1.51, 95%CI: 1.07-2.14), the screen-time guideline alone (aOR = 1.39, 95% CI: 1.02-1.89), or the screen-time and sleep guidelines concurrently (aOR = 1.38, 95%CI: 1.02-1.86) was associated with a significantly higher odds of being overweight, than meeting all three guidelines. Among female youth, meeting the physical activity guideline alone (aOR = 0.29, 95%CI: 0.10-0.85) was associated with a significantly lower odds of being overweight than meeting all three 24-hour movement guidelines.
In the multinomial model of obese bodyweight status, compared with youth who met all three 24-hour movement guidelines, the odds of obesity was significantly higher among those who met no guideline (aOR = 4.25, 95%CI: 2.87-6.31), the sleep guideline alone (aOR = 2.57, 95%CI: 1.71-3.86), the screen-time guideline alone (aOR=2.07, 95%CI: 1.43-3.02), and or the screen-time and sleep guideline concurrently (aOR=1.85, 95%CI: 1.30-2.64). In the sex-stratified models, the same findings held for males and females. Notably, in the full sample and sex-stratified models, meeting the physical activity guidelines alone or meeting a combination of physical activity and another guideline (i.e. screen-time or sleep) versus meeting all three guidelines, was not associated with a significantly higher odds of obesity.
Discussion
The conceptualization of 24-hour healthy movement behaviors (i.e., ≥60-min of moderate-to-vigorous physical activity, ≤2-hours of screen-time, age-appropriate sleep duration/each day) as co-dependent and integrated entities represents an important paradigm advancement for health behavior change. A growing literature has shown that a minority (2-17%) of youth meet all three 24-hour healthy movement behaviors,(3-8, 21) but that meeting all guidelines is significantly associated with better cardiometabolic and cognitive health.(3, 8, 10, 11) The current study supports and extends this work by showing that meeting none of the guidelines procured the highest odds for overweight (aOR=1.85, 95% CI=1.31-2.61) and obesity (aOR=4.25, 95% CI=2.87-6.31), but that meeting the moderate-to-vigorous physical activity guideline, either independently, or in combination with the screen-time or sleep duration guideline, was associated with the lowest odds for overweight or obesity among US youth. A second key finding of this study was that the odds of obesity were considerably higher in female (aOR=4.97, 95% CI=2.59-9.53) versus male (aOR=3.99, 95% CI=2.49-6.40) youth who met none of the guidelines versus those who met all three.
Approximately one in three youth in this sample were either obese or overweight. These rates converge with data from the NHANES survey where 18.5% of youth were reported obese (22) and 16.6% overweight.(23) Our finding that meeting the physical activity guideline either alone, or in combination with the screen-time or sleep duration guidelines procured the lowest odds for overweight and obesity, converges with previous work conducted outside the US.(3, 7, 24, 25) Numerous of studies have shown youth who participate in regular physical activity (including sports teams) to have a lower body mass index, and to be less likely to be overweight or obese.(26) This relationship is likely attributable to the higher level of energy expenditure incurred with increased activity.(26) Indirect mechanisms to explain this relationship include the reduced energy intake observed in active youth exposed to food stimuli (i.e., the transient anorexigenic effect of activity),(27, 28) and being in a family or school context that promotes increased levels of habitual activity.(21, 29)
From a 24-hour healthy movement behavior perspective, it could be argued that habitually meeting the physical activity guideline is supported by also meeting the screen-time and sleep duration guidelines. Support for this premise comes from cross-sectional data showing that youth who regularly meet sleep duration guidelines are more physically active and have lower rates of obesity.(30, 31) In a recent study that examined the temporal and bidirectional relationship between objectively measured sleep, sedentary behavior, and physical activity, results showed that higher levels of physical activity were associated with subsequently better sleep, whereas increased sedentary behavior was associated with poorer subsequent sleep.(32) The complex temporal and reciprocal relationships between the 24-hour movement behaviors across childhood and adolescent maturation phases is still poorly understood. Elucidating these relationships, and their association with different measures of body fatness, is necessary for informing targeted intervention approaches to increase the proportion of youth meeting these guidelines.
Females who met zero of the 24-hour healthy movement guideline (vs. meeting all 3) had a five-fold increased odds (aOR=4.97) of obesity, whereas their male counterparts had a four-fold increased odds (aOR= 3.99). Moreover, females who met the physical activity guideline alone had a 71% reduced odds, of being overweight as compared with females who met all three guidelines. These data underscore how important meeting the physical activity and screen-time recommendations are for female youth to maintain a healthy weight. Yet, substantially fewer female youth meet physical activity recommendations than males, and the disparity only increases with age.(33) International data show that in early childhood, males accrue significantly more screen-time per day than females;(34) however, female adolescents may experience disproportionately more negative mental health effects from their screen-time, including depressive symptoms and anxiety.(35) Given the negative association between depressive symptomology and habitual physical activity,(36) screen-time may be particularly deleterious to physical activity levels in female youth. Taken together, these data highlight the importance of considering the range of movement behaviors, and introduce the need to consider sex-differences in the relative importance of the different 24-hour movement behaviors to body fatness.
Strengths of this study include the inclusion of a large national representative sample. These data should be interpreted with consideration of some methodological limitations including the fact that the data were cross-sectional, parent and self-reported, and that the analysis did not consider other social and environmental factors that also relate to body mass index.(21, 29) A limitation is related to the missing responses, although accounting for fewer than 10% of the total analyzed sample, minorities and those with lower income were overrepresented compared with the analyzed completed ones. That the assessment of screen-time did not take mobile phone or computer use into account, is another limitation. These results underscore the importance of the 24-hour healthy movement perspective, and identify meeting the physical activity guideline as being critical to healthy weight in youth. Further research needs to elucidate the reciprocal and temporal relationship between 24-hour healthy movement behaviors, and multi-level approaches to increase the proportion of youth meeting these guidelines that are critical to achieving a healthy weight.
Supplementary Material
Acknowledgements
We thank Yatzka Hernandez, Research Manager at the University of Delaware’s Department of Behavioral Health and Nutrition, who provided administrative support in the submission of this manuscript.
Supported by the National Institute On Minority Health And Health Disparities of the National Institutes of Health (R01MD012734 and R21AG056765 [to F.P.]), and by an Institutional Development Award (IDeA) Center of Biomedical Research Excellence from the National Institute of General Medical Sciences of the National Institutes of Health (P20GM113125 [to F.P.]). The study sponsor had no role in the study design, data collection, analysis, interpretation of data, the writing of this report, or the decision to submit this manuscript for publication. The authors declare no conflicts of interest.
Abbreviations:
- NSCH
National Survey of Children’s Health
- BMI
Body Mass Index
- CI
Confidence Interval
- OR
Odds Ratio
- aOR
Adjusted Odds Ratio
- SD
Standard Deviation
- FPL
Federal Poverty Level
- CHIP
Children’s Health Insurance Program
Footnotes
Data Statement: The NSCH data used for this study are publicly available.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Tremblay MS, Carson V, Chaput JP, Connor Gorber S, Dinh T, Duggan M, et al. Canadian 24- Hour Movement Guidelines for Children and Youth: An Integration of Physical Activity, Sedentary Behaviour, and Sleep. Appl Physiol Nutr Metab. 2016;41:S311–27. [DOI] [PubMed] [Google Scholar]
- 2.Hirshkowitz M, Whiton K, Albert SM, Alessi C, Bruni O, DonCarlos L, et al. National Sleep Foundation’s updated sleep duration recommendations: final report. Sleep Health. 2015;1:233–43. [DOI] [PubMed] [Google Scholar]
- 3.Carson V, Chaput JP, Janssen I, Tremblay MS. Health associations with meeting new 24-hour movement guidelines for Canadian children and youth. Prev Med. 2017;95:7–13. [DOI] [PubMed] [Google Scholar]
- 4.Roberts KC, Yao X, Carson V, Chaput JP, Janssen I, Tremblay MS. Meeting the Canadian 24- Hour Movement Guidelines for Children and Youth. Health Rep. 2017;28:3–7. [PubMed] [Google Scholar]
- 5.Knell G, Durand CP, Kohl HW 3rd, Wu IHC, Pettee Gabriel K. Prevalence and Likelihood of Meeting Sleep, Physical Activity, and Screen-Time Guidelines Among US Youth. JAMA Pediatr. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Healy S, Aigner CJ, Haegele JA, Patterson F. Meeting the 24-hr movement guidelines: An update on US youth with autism spectrum disorder from the 2016 National Survey of Children’s Health. Autism Res. 2019;12:941–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Roman-Vinas B, Chaput JP, Katzmarzyk PT, Fogelholm M, Lambert EV, Maher C, et al. Proportion of children meeting recommendations for 24-hour movement guidelines and associations with adiposity in a 12-country study. Int J Behav Nutr Phys Act. 2016;13:123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Walsh JJ, Barnes JD, Cameron JD, Goldfield GS, Chaput JP, Gunnell KE, et al. Associations between 24 hour movement behaviours and global cognition in US children: a cross-sectional observational study. Lancet Child Adolesc Health. 2018;2:783–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Janssen I, Roberts KC, Thompson W. Adherence to the 24-Hour Movement Guidelines among 10- to 17-year-old Canadians. Health Promot Chronic Dis Prev Can. 2017;37:369–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.U.S. Department of Health and Human Services. 2019 Poverty Guidelines: OFFICE OF THE ASSISTANT SECRETARY FOR PLANNING AND EVALUATION; 2019. [Available from: https://aspe.hhs.gov/2019-poverty-guidelines.
- 11.Katzmarzyk PT, Staiano AE. Relationship Between Meeting 24-Hour Movement Guidelines and Cardiometabolic Risk Factors in Children. J Phys Act Health. 2017;14:779–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Varni JW, Limbers CA, Burwinkle TM. Parent proxy-report of their children’s health-related quality of life: an analysis of 13,878 parents’ reliability and validity across age subgroups using the PedsQL 4.0 Generic Core Scales. Health Qual Life Outcomes. 2007;5:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chaumeton N, Duncan SC, Duncan TE, Strycker LA. A measurement model of youth physical activity using pedometer and self, parent, and peer reports. Int J Behav Med. 2011;18:209–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Koning M, de Jong A, de Jong E, Visscher TLS, Seidell JC, Renders CM. Agreement between parent and child report of physical activity, sedentary and dietary behaviours in 9–12-year-old children and associations with children’s weight status. BMC Psychol. 2018;6:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.United States Census Bureau. National Survey of Children’s Health (NSCH) 2019. [Available from: https://www.census.gov/programs-surveys/nsch.html.
- 16.US Department of Health and Human Services. Physical Activity Guidelines for Americans. Washington, DC: US Department of Health and Human Services; 2018. [Google Scholar]
- 17.Chaput JP, Carson V, Gray CE, Tremblay MS. Importance of all movement behaviors in a 24 hour period for overall health. Int J Environ Res Public Health. 2014;11:12575–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.WHO Expert Committee. Physical status: the use and interpretation of anthropometry. Geneva: World Health Organization; 1995. Contract No.: WHO Technical Report Series 854. [PubMed] [Google Scholar]
- 19.Lenhart C, Hanlon A, Kang Y, Daly B, Brown M, Patterson F. Gender Disparity in Structured Physical Activity and Overall Activity Level in Adolescence: Evaluation of Youth Risk Behavior Surveillance Data. ISRN Public Health. 2012;2012. [Google Scholar]
- 20.Belcher BR, Berrigan D, Dodd KW, Emken BA, Chou CP, Spruijt-Metz D. Physical activity in US youth: effect of race/ethnicity, age, gender, and weight status. Med Sci Sports Exerc. 2010;42:2211–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Donnelly JE, Greene JL, Gibson CA, Smith BK, Washburn RA, Sullivan DK, et al. Physical Activity Across the Curriculum (PAAC): a randomized controlled trial to promote physical activity and diminish overweight and obesity in elementary school children. Prev Med. 2009;49:336–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hales CM, Carroll MD, Fryar CD, Ogden CL. Prevalence of Obesity Among Adults and Youth: United States, 2015–2016. NCHS Data Brief. 2017:1–8. [PubMed] [Google Scholar]
- 23.Hales CM, Fryar CD, Carroll MD, Freedman DS, Ogden CL. Trends in Obesity and Severe Obesity Prevalence in US Youth and Adults by Sex and Age, 2007–2008 to 2015–2016. JAMA. 2018;319:1723–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Laurson KR, Lee JA, Gentile DA, Walsh DA, Eisenmann JC. Concurrent Associations between Physical Activity, Screen Time, and Sleep Duration with Childhood Obesity. ISRN Obes. 2014;2014:204540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Laurson KR, Lee JA, Eisenmann JC. The cumulative impact of physical activity, sleep duration, and television time on adolescent obesity: 2011 Youth Risk Behavior Survey. J Phys Act Health. 2015;12:355–60. [DOI] [PubMed] [Google Scholar]
- 26.Olds TS, Ferrar KE, Schranz NK, Maher CA. Obese adolescents are less active than their normal-weight peers, but wherein lies the difference? J Adolesc Health. 2011;48:189–95. [DOI] [PubMed] [Google Scholar]
- 27.Fearnbach SN, Masterson TD, Schlechter HA, Ross AJ, Rykaczewski MJ, Loken E, et al. Impact of imposed exercise on energy intake in children at risk for overweight. Nutr J. 2016;15:92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Thivel D, Rumbold PL, King NA, Pereira B, Blundell JE, Mathieu ME. Acute post-exercise energy and macronutrient intake in lean and obese youth: a systematic review and meta-analysis. Int J Obes (Lond). 2016;40:1469–79. [DOI] [PubMed] [Google Scholar]
- 29.Sigmund E, Sigmundova D, Badura P, Madarasova Geckova A. Health-related parental indicators and their association with healthy weight and overweight/obese children’s physical activity. BMC Public Health. 2018;18:676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kim Y, Umeda M, Lochbaum M, Stegemeier S. Physical Activity, Screen-Based Sedentary Behavior, and Sleep Duration in Adolescents: Youth Risk Behavior Survey, 2011–2013. Prev Chronic Dis. 2016;13:E131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Miller MA, Kruisbrink M, Wallace J, Ji C, Cappuccio FP. Sleep duration and incidence of obesity in infants, children, and adolescents: a systematic review and meta-analysis of prospective studies. Sleep. 2018;41. [DOI] [PubMed] [Google Scholar]
- 32.Master L, Nye RT, Lee S, Nahmod NG, Mariani S, Hale L, et al. Bidirectional, Daily Temporal Associations between Sleep and Physical Activity in Adolescents. Sci Rep. 2019;9:7732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Katzmarzyk PT, Lee IM, Martin CK, Blair SN. Epidemiology of Physical Activity and Exercise Training in the United States. Prog Cardiovasc Dis. 2017;60:3–10. [DOI] [PubMed] [Google Scholar]
- 34.Ng KW, Augustine L, Inchley J. Comparisons in Screen-Time Behaviours among Adolescents with and without Long-Term Illnesses or Disabilities: Results from 2013/14 HBSC Study. Int J Environ Res Public Health. 2018;15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Twenge JM, Martin GN, Campbell WK. Decreases in psychological well-being among American adolescents after 2012 and links to screen time during the rise of smartphone technology. Emotion. 2018;18:765–80. [DOI] [PubMed] [Google Scholar]
- 36.Miller M Understanding Depression: Harvard Medical School Special Health Report. Boston, MA: Harvard University Medical School; 2008. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.