Highlights
-
•
A combination of proton therapy and deep inspiration breath-hold can reduce normal tissue dose.
-
•
The first patients treated showed clinically acceptable inter breath-hold variations.
-
•
The treatment strategy is robust and works well at a proton center.
Keywords: Radiotherapy, Hodgkin’s lymphoma, Proton therapy, Pencil beam scanning, Deep inspiration breath-hold
Abstract
Background
Most patients with Hodgkin’s lymphoma are young and have a favourable prognosis, therefore it is of high importance to decrease the radiation doses to normal tissues received during radiotherapy. A combination of proton therapy and deep inspiration breath-hold technique (DIBH) can improve the sparing effect and thereby reduce the risk of late effects.
Case presentation
The two first patient cases treated with proton therapy in DIBH at the Skandion Clinic, Uppsala, Sweden, are presented here. Proton treatment plans were compared to photon plans based on doses to target and organs at risk. Several CT scans were acquired during the treatment course and inter breath-hold variations were evaluated based on anatomical distances and dosimetric comparisons.
Conclusions
The results from our first patients treated with proton therapy in DIBH imply that the treatment strategy is robust and has the potential to reduce dose to normal tissue.
Introduction
In Sweden approximately 200 persons are diagnosed with Hodgkin’s lymphoma each year. The majority are adolescents or young adults, but the disease is also present in children and older persons [1]. Since most of the patients are young and the prognosis is very favourable, it is of high importance to minimize the long-term effects of the treatment [2].
Proton therapy for mediastinal tumours has the potential to reduce lung and heart doses compared to photon-based radiotherapy [3]. The combination of pencil beam scanning (PBS) proton therapy and deep inspiration breath-hold (DIBH) technique improves the sparing effect even further [4], [5] due to favourable anatomical changes compared to free breathing (FB). Furthermore, a successfully applied DIBH technique minimizes the effect of respiratory motion on range uncertainties and interplay effects [6], [7].
The Skandion Clinic, Uppsala, Sweden, offers advanced proton therapy to cancer patients from the whole country. This national project is run by the seven county councils with university hospitals and is based on a distributed competence concept. This means that immobilization, CT-scanning and treatment planning are performed at one of the university hospitals in Sweden, in this case Skåne University Hospital, while the treatment is given at the proton facility [8], [9]. This case report presents the first two Hodgkin’s lymphoma patients treated with PBS protons in DIBH at the Skandion Clinic.
Case report
Patients
This reporting was approved by the Ethics Board of Lund, Sweden (Dnr 2013/742).
Two patient cases, treated with proton therapy in DIBH between February 2018 and February 2019, are presented in this report. For details of patient characteristics, see Table 1. The selection, preparation and proton treatment procedures follow the national standard protocol.
Table 1.
Details about the two patients treated with PBS protons in deep inspiration breath-hold at the Skandion Clinic.
| Patient 1 | Patient 2 | |
|---|---|---|
| Age | 21 | 35 |
| Gender | Female | Female |
| Disease | HL (Stage IA) nodular sclerosis, bulky mediastine |
HL (Stage IIA) nodular sclerosis |
| Chemo therapy | Two cycles of ABVD, descaled to AVD (good responder) received for another two cycles |
Two cycles of ABVD |
| Dose | 29.75 Gy(RBE), 17 fx | 20 Gy(RBE), 10 fx |
| CTV volume | 125 cm3 | 72 cm3 |
Deep inspiration technique and CT imaging
CT images of the patients were acquired with Siemens SOMATOM Definition AS CT scanners (Siemens Medical Solutions, Erlangen, Germany), and the laser surface scanning system SentinelTM (C-rad Positioning AB, Uppsala, Sweden) was used to track the vertical chest wall motion in DIBH, using both audio and visual guidance. The residual chest wall motion within one breath-hold was limited to 3 mm by the gating window. Patients were trained to hold their breath for 20 seconds in order to acquire the CT scan within one breath-hold, and also limit the number of breath-holds required to deliver the fractional dose. To ensure DIBH reproducibility, the patients were guided to a large but comfortable and reproducible breath-hold amplitude (approximately 10 mm).
Several CT-series were acquired for each patient prior to treatment and during the course of treatment in order to ensure the patient’s ability to accurately reproduce the breath-hold amplitude, and to evaluate the inter breath-hold reproducibility:
-
-
Planning DIBH-CT and two low dose DIBH-CTs acquired at Skåne University Hospital prior to treatment.
-
-
Verification DIBH-CT and two low dose DIBH-CTs at the Skandion Clinic prior to treatment (for patient 1 only one DIBH-CT) and then a DIBH-CT once a week during the treatment course.
The low dose CT scans were acquired with the same DIBH technique as the standard DIBH-CTs used for treatment planning and were scanned immediately after the planning/verification DIBH CT was acquired, without any break. The CT images were acquired in a sequence of five DIBHs. The planning/verification CT was acquired during the first DIBH and the low dose CTs were acquired during the third and fifth DIBH. The low dose CT images were only used to evaluate breath-hold reproducibility and no recalculations of dose were performed based on them. The idea was to evaluate if the reproducibility of several anatomical measures was acceptable. The routine of acquiring two low dose scans prior to treatment at Skandion was established after the treatment course of patient 1, and therefore only one verification CT was acquired for this patient before treatment.
Contouring and treatment planning
The gross tumour volume (GTV) was delineated as the PET positive residual tumour and the clinical target volume (CTV) was defined as the original spread of the disease (including the GTV). It was verified that the CTV was encompassed in the two repeated DIBH-CT. Heart and lungs were delineated as organs at risk (OARs) and for patient 1 the breasts were also defined.
Varian Eclipse (Varian Medical Systems, Palo Alto, California) with the Proton Convolution Superposition algorithm (PCS, version 13.7) was used to create the proton plans. The proton beam (Ion Beam Applications, Belgium) delivers energies from 60 to 230 MeV. Proton plans were optimized in the interest of robustness:
-
-
Two anterior oblique fields with close gantry angles of 350° and 10° (Fig. 1) to achieve an almost volumetric repainting effect.
-
-
Range shifter (WET 3.5 cm) was used for both beams with a large airgap (>18 cm) to gain larger spot sizes and to eliminate risk of obscuring the field of view of the CatalystTM scanner system (C-rad Positioning AB, Uppsala, Sweden).
-
-
Field-specific targets were created from the CTV with a margin of 0.7 cm and range uncertainty of 4.5%, [10] and spot spacing of 0.7 cm (values normally used for proton plans in the thoracic region at our clinic)
-
-
Plans were single-field robust optimized (SFO) using the Nonlinear Universal Proton Optimizer (NUPO, Varian Eclipse) with perturbations up to 0.7 cm and 4.5% range uncertainty.
-
-
Plan robustness was evaluated with 0.5–0.6 cm setup uncertainty and 4.5% range uncertainty with a requirement that all perturbed dose distributions should reach D98% ≥ 95%.
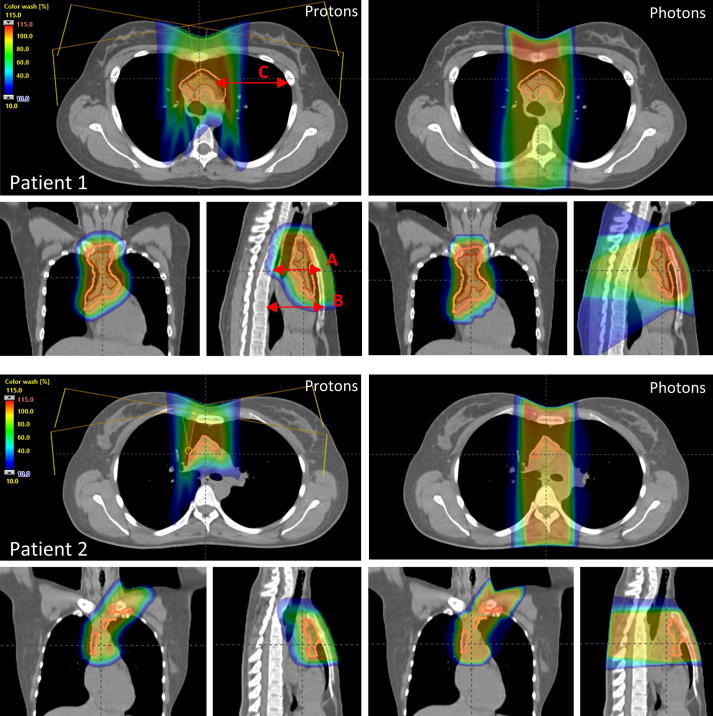
Fig. 1.
Proton (left) and photon (right) dose distributions for patient 1 (upper) and patient 2 (lower). CTV is marked in pink. Red arrows show examples of distances measured to evaluate inter breath-hold variation.
Photon treatment plans were created using Varian Eclipse with the Analytical Anisotropic Algorithm (AAA, version 13.6) and compared with proton plans according to our routines for selection of patients for protons. The photon plans were 3D conformal radiotherapy (3DCRT) with two 6 MV anterior-posterior/posterior-anterior (AP/PA) parallel opposed fields (gantry angles 0° and 180°) using a PTV margin of 8–10 mm, which is the treatment technique used in clinical practice at our centre.
Treatment preparation and verification
The optical surface scanning system CatalystTM [11] installed on the proton gantry was used for patient positioning in FB, using the reference surface acquired with the Sentinel system during the CT scanning, and also for tracking the DIBH respiratory motion. The baseline of the day, i.e. the signal expiration value in FB, was automatically calculated by the system and compared to the planned value. The patient position in DIBH was verified and potentially corrected for by using orthogonal X-ray images and a robotic couch with six degrees of freedom. During a few treatment fractions, the baseline value was considerably drifting (more than approx. 2 mm) and in those cases a new baseline was acquired after verification with new X-ray images. Audio instructions on when to inhale/exhale were given during the treatment, and both patients used video goggles for visual guidance of the breathing amplitude.
Verification of DIBH reproducibility
The total number of standard/low dose DIBH-CTs acquired were 4/2 for patient 1 and 3/4 for patient 2. The inter breath-hold variation was assessed by quantifying anatomical deviations between the CT images (standard and low dose protocol). Lung volumes and also well-defined distances (Fig. 1) in the thoracic area were compared. Two distances were measured in one sagittal image slice between the vertebra and sternum (distance A and B), and two distances were measured in two different axial slices (distances C and D, only C is shown in Fig. 1). To determine dosimetric effects, the original treatment plan was recalculated on the DIBH-CT verification images (standard dose protocol), and doses to the CTV and OARs were compared.
Results
Proton and photon treatment planning comparison
Dose distributions for the DIBH plans of the two patients are shown in Fig. 1. The percentage of the prescribed dose covering at least 98% of the CTV (D98%) and dose volume histogram (DVH) measures of OARs are presented in Table 2. Doses to OARs were generally lower for protons in comparison to photons. Robustness tests for the proton plans showed that the “worst” uncertainty curve had a D98% value of 96% and 95% for patients 1 and 2, respectively. No robustness tests were carried out for the photon plans, since this is normally not done for photon plans at our clinic.
Table 2.
Comparison of the percentage of the prescribed dose covering at least 98% of the CTV (D98%) and DVH values of organs at risk for proton and photon plans. V5Gy, Lungs - total lung volume receiving a dose of 5 Gy, D2%, Spinal cord - dose to 2% of spinal cord volume.
| Patient 1 |
Patient 2 |
|||
|---|---|---|---|---|
| DVH parameter | Protons | Photons | Protons | Photons |
| [%] | 98.0 | 95.0 | 96.9 | 96.7 |
| [Gy/Gy(RBE)] | 3.6 | 6.4 | 0.4 | 1.2 |
| [Gy/Gy(RBE)] | 3.4 | 5.3 | 1.4 | 2.5 |
| [%] | 17.9 | 26.8 | 8.9 | 11.7 |
| [Gy/Gy(RBE)] | 2.9 | 26.8 | 1.7 | 19.5 |
| [Gy/Gy(RBE)] | 2.3 | 2.6 | - | - |
| [Gy/Gy(RBE)] | 1.1 | 1.0 | - | - |
| [Gy/Gy(RBE)] | 5.0 | 8.4 | 0.1 | 0.8 |
| [Gy/Gy(RBE)] | 8.6 | 20.6 | 4.9 | 13.4 |
Verification of inter breath-hold variability
Table 3 shows the measured deviations in lung volumes and distances (Fig. 1) for all DIBH-CT verification images (both standard and low dose protocol) compared to the original DIBH-CT image. DVH measures for the CT verification recalculations (standard dose protocol only) compared to the original plan are also presented in the table.
Table 3.
The mean (maximal) deviations between distances (see schematic arrows in Fig. 1) and lung volumes measured in the DIBH-CT verification images (standard + low dose protocol) compared to the original DIBH-CT for the two patients. The mean (maximal) deviations (percentage points) of dose volume histogram measures for the dose distribution recalculations (standard dose protocol only) are also shown.
| Patient 1 | Patient 2 | |
|---|---|---|
| Geometrical measure | ||
| ΔA [mm] | 2.0 (3.9) | 0.9 (2.3) |
| ΔB [mm] | 2.0 (4.9) | 0.5 (1.4) |
| ΔC [mm] | 2.7 (5.3) | 1.0 (2.0) |
| ΔD [mm] | 1.5 (4.1) | 1.1 (1.6) |
| ΔLungVolume [%] | 5.3 (9.8) | 2.5 (6.3) |
| DVH parameter | ||
| [%] | 0.3 (0.3) | 0.6 (0.6) |
| [%] | 0.4 (0.6) | 0.1 (0.1) |
| [%] | 0.4 (0.6) | 1.7 (2.5) |
| [%] | 1.1 (1.9) | 0.2 (0.3) |
| [%] | 2.6 (3.6) | 1.0 (1.1) |
The number of breath-holds required to complete online imaging verification and to deliver the fractional dose was 5–7 for patient 1 and 3–5 for patient 2. The amount of breath-holds needed to deliver the treatment fraction depended on the patient’s own breathing technique and differed between the two cases. Patient 2 could hold her breath longer compared to patient 1, and hence fewer breath-holds were required to deliver the fractional dose. The mean (maximal) deviations in baseline value, i.e. the signal expiration value in FB, during the treatment fraction compared to the planned baseline were 3 (8) mm and 2 (4) mm for patients 1 and 2, respectively.
Discussion
In this case report, we describe the first PBS proton treatments of Hodgkin’s Lymphoma in DIBH technique at the Skandion Clinic, using an optical surface scanning system [12]. Our aim was a superior dose distribution and minimization of the effect of breathing motion by combining these two advanced treatment techniques. The PBS proton dose distribution presented here was superior compared to 3DCRT photons, the heart dose was reduced by 40–70% and the lung dose by 40%. This is consistent with earlier published findings [4], [5].
For both patient cases presented here, the anatomical distances measured to evaluate inter breath-hold variations showed that the mean deviations were generally within 2 mm. The maximal deviations were up to 5 mm for patient 1, but overall the variations were considered acceptable according to the robustness of the plan (robustness tests with 0.5–0.6 cm setup uncertainty). In addition, dosimetric evaluations on the repeated DIBH-CTs were also performed to determine if the treatment was clinically acceptable. Comparison of DVH metrics showed minor deviations both in D98% to CTV (below 0.6 percentage points) and doses to OARs (generally below 2 percentage points).
The results imply that the patients in this report were suitable for PBS proton therapy in DIBH. We want to emphasize the importance of careful evaluation of each patient’s case and performance; the tumour size and distribution in the aspect of complexity and motion, and whether plan quality and robustness criteria can be reached. In this study, only two patients were included with small target volumes located in the mediastinum. They were treated with rather simple treatment plans (SFO) during limited motion (in DIBH). Further investigations of larger volumes and more complex scenarios are needed to fully understand and fully use proton treatment in DIBH for Hodgkin’s Lymphoma patients. Larger volumes require longer delivery times and a greater number of breath-holds, which may worsen the breath-hold reproducibility. Furthermore, the patient’s ability to reproduce each DIBH is important, both in amplitude and in the breathing manoeuvre, and multiple DIBH-CT needs to be acquired to evaluate how this affects the dose distribution [13].
DIBH technique is a motion mitigation technique that, if successfully applied, creates an almost static geometrical situation [6], [7]. However, the reproducibility of the breath-hold may degrade the planned dose distribution caused by small anatomical changes and interplay effects. This has been one of the major concerns during the implementation of PBS treatments in DIBH. A pre-study was performed with the purpose of investigating the impact of DIBH variability on PBS proton delivery [14]. The results showed that averaged over the complete series of fractions, the deviations from the planned dose distribution are small; within 1% for the CTV. The pre-study thereby indicates that the DIBH technique is a suitable delivery mode for PBS proton therapy for mediastinal lymphoma.
Conclusion
Our experience from the first patients treated with PBS proton therapy in DIBH implies that combining protons and DIBH is a feasible treatment technique and works well at a proton centre. The results are encouraging and shows that this treatment strategy is robust and has the potential to reduce OAR doses.
Declaration of Competing Interest
The authors have no conflicts of interest to disclose.
References
- 1.Cancercentrum.se. (2019). National standard protocol for Hodgkins lymfom. [online] Available at: [Accessed 11 Jun. 2019]. https://www.cancercentrum.se/samverkan/cancerdiagnoser/blod-lymfom-myelom/lymfom-lymfkortelcancer/vardprogram/gallande-vardprogram-hodgkins-lymfom/.
- 2.Ng A., Bernardo M., Weller E., Backstrand K., Silver B., Marcus K. Long-term survival and competing causes of death in patients with early-stage Hodgkińs disease treated at age 50 or younger. J Clin Oncol. 2002;20:2101–2108. doi: 10.1200/JCO.2002.08.021. [DOI] [PubMed] [Google Scholar]
- 3.Tseng Y.D., Cutter D.J., Plastaras J.P. Evidence-based review on the use of proton therapy in lymphoma from the particle therapy cooperative group (PTCOG) lymphoma subcommittee. Int J Radiat Oncol Biol Phys. 2017;99:825–842. doi: 10.1016/j.ijrobp.2017.05.004. [DOI] [PubMed] [Google Scholar]
- 4.Edvardsson A. Comparative treatment planning study for mediastinal Hodgkińs lymphoma: Impact on normal tissue dose using deep inspiration proton and photon therapy. Acta Oncologica. 2019;58(1):95–104. doi: 10.1080/0284186X.2018.1512153. [DOI] [PubMed] [Google Scholar]
- 5.Rechner L.A., Maraldo M.V., Vogelius I.R. Life years lost attributable to late effects after radiotherapy for early stage Hodgkin lymphoma: the impact of proton therapy and/or deep inspiration breath-hold. Radiother Oncol. 2017;125:41–47. doi: 10.1016/j.radonc.2017.07.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schatti A., Zakova M., Meer D. The effectiveness of combined gating and re-scanning for treating mobile targets with proton spot scanning: An experimental and simulation-based investigation. Phys Med Biol. 2014;59:3813–3828. doi: 10.1088/0031-9155/59/14/3813. [DOI] [PubMed] [Google Scholar]
- 7.Dueck J., Knopf A.C., Lomax A. Robustness of the voluntary breath-hold approach for the treatment of peripheral lung tumors using hypofractionated pencil beam scanning proton therapy. Int J Radiat Oncol Biol Phys. 2016;95:534–541. doi: 10.1016/j.ijrobp.2015.11.015. [DOI] [PubMed] [Google Scholar]
- 8.Karlsson K., Björk-Eriksson T., Mattsson O. Distributed proton radiation therapy’’-A new concept for advanced competence support. Acta Oncologica. 2006;45:1094–1101. doi: 10.1080/02841860600897876. [DOI] [PubMed] [Google Scholar]
- 9.Witt Nyström P, Nyström H, PTC17-0228: Can the Swedish Model of Distributed Competence Serve as a Model for Other Proton Centres? 56th Annual Meeting of the Particle Therapy Cooperative Group (PTCOG) 8-13 May 2017
- 10.Paganetti H. Range uncertainties in proton therapy and the role of Monte Carlo simulations. Phys Med Biol. 2012;57(11):R99–R117. doi: 10.1088/0031-9155/57/11/R99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kugele M., Edvardsson A., Berg L. Dosimetric effects of intrafractional isocenter variation during deep inspiration breath-hold for breast cancer patients using surface-guided radiotherapy. J Appl Clin Med Phys. 2018;19:25–38. doi: 10.1002/acm2.12214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Enmark M., Lundkvist N., Fager M., Kugele M., Nyström H., Ceberg S. PTC17-0493: Clinical Commissioning of Gated Proton Pencil Beam Scanning. Additional Proceedings to the 56th Annual Meeting of the Particle Therapy Cooperative Group (PTCOG) Int J Particle Ther. 2017;4(2):177. [Google Scholar]
- 13.Chang J.Y., Zhang X., Knopf A. Consensus guidelines for implementing pencil beam scanning proton therapy for thoracic malignancies on behalf of PTCOG thoracic and lymphoma subcommittee. Int J Radiat Oncol Biol Phys. 2017;99:41–50. doi: 10.1016/j.ijrobp.2017.05.014. [DOI] [PubMed] [Google Scholar]
- 14.Enmark M., Olofsson J., Ceberg S., Jonsson J. [P205] The impact on pencil beam scanning (PBS) proton therapy for mediastinal lymphoma from deep inspiration breath-hold (DIBH) variability. Phys Med. 2018;52:159. [Google Scholar]